Abstract
Community-engaged research (CEnR) is a powerful tool to create sustainable and effective change in health outcomes. CEnR engages community members as equal partners, amplifying their voices and priorities by including them throughout the research process. Such engagement increases the relevance and meaning of research, improves the translation of research findings into sustainable health policy and practice, and ultimately enhances mutual trust among academic, clinical, and community partners for ongoing research partnership. There are a number of key principles that must be considered in the planning, design, and implementation of CEnR. These principles are focused on inclusive representation and participation, community empowerment, building community capacity, and protecting community self-determination. Although vascular surgeons may not be equipped to address these issues from the ground up by themselves, they should work with a team who can help them incorporate these elements into their CEnR project designs and proposals. This may be best accomplished by collaborating with researchers and community-based organizations who already have this expertise and have established social capital within the community. This article describes the theory and principles of CEnR, its relevance to vascular surgeons, researchers, and patients, and how using CEnR principles in vascular surgery practice, research, and outreach can benefit our patient population, with a specific focus on reducing disparities related to amputation.
Keywords: Community engagement, Community engaged research, Vascular surgery, Amputation disparities, Health disparities
1. Introduction
Community-engaged research (CEnR) approaches are grounded in the principles and practices of community engagement. Specifically, CEnR engages community members as equal partners, amplifying their voices and priorities by including them throughout the research process. Such engagement increases the relevance and meaning of research, improves the translation of research findings into sustainable health policy and practice, and ultimately enhances mutual trust between academic, clinical, and community partners for ongoing research partnership [1].
CEnR recognizes that lifestyles, behaviors, and the incidence and outcomes of illness are shaped by social, physical, and policy environments, and that disparities in health outcomes result from inequities in these environments [2]. If health is socially determined, then health issues are best addressed by engaging community partners, among others, who can bring their own perspectives and understanding of community life and health issues to interventions and solutions [3]. Amputation disparities are a clear example of the impact of both social and physical environmental inequities on health and, as such, have the potential to be impacted substantially by interventions that use CEnR approaches.
In this article, we describe the theory and principles of CEnR, its relevance to vascular surgeons, researchers, and patients, and how using CEnR principles in vascular surgery practice, research, and outreach can benefit our patient population, with a specific focus on reducing disparities related to amputation.
2. Background
2.1. Key concepts of community engagement and CEnR
Much like surgery, community engagement is a complex blend of science and art—science, as it relates to community health sciences and research methodology, and art, as it relates to understanding culture; interpersonal skill sets; community objectives; and sensitivity to and appreciation for the needs of others as individuals and organizations. Some key concepts to understand when approaching community engagement come from the field of community organizing. Community organizing is focused on bringing a community together to pursue social action, and is rooted in fairness, justice, empowerment, participation, and self-determination [4–7]. CEnR applies these concepts in the following ways:
by being representative in community engagement—this requires being inclusive in the definition of community and seeking to engage community members across the full spectrum of a community, not only those that are most empowered to engage [8];
by sharing power and resources with community partners so that they develop sustainable skills, resources, and structures to improve their own health (ie, capacity building); and
by focusing on authentically raising community voices and priorities with the understanding that every community has the right and power to act in its own self-interest (ie, self-determination).
Community engagement and CEnR take time and effort in order to build a truly collaborative relationship between an institution and a community. As illustrated in Figure 1, the relationship often evolves across a continuum from a consultative capacity to a cooperative one and, ultimately, to a collaborative level with strong, equal partnership among entities.
Fig. 1 –
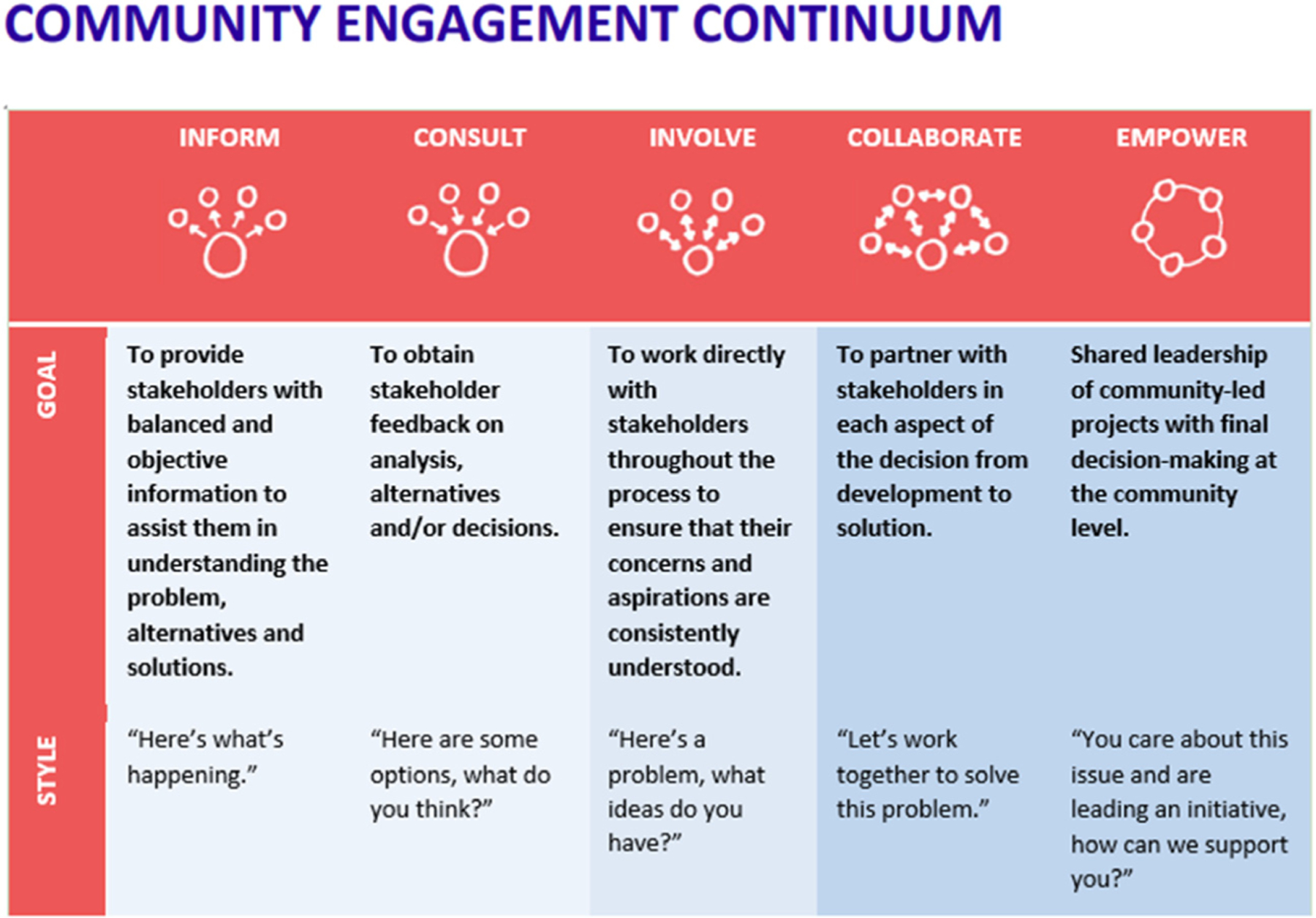
The community engagement continuum. Level of community engagement is a fluid process that should progress as relationships between researchers and communities evolve. From the Tamarack Institute-Community Engagement Continuum (adapted from the IAP2 Public Participation Spectrum), adapted with permission [9].
2.1.1. Definition of community
A community is composed of a variety of individuals who typically share social ties and, possibly, similar perspectives. A community may encompass a geographic location or specific setting (physical or virtual) or may bring together a group of people with a specific background, orientation, or disease process. A work environment may also be considered a community (such as a clinic) and bring together people who may not have otherwise been part of the same community. Individuals may identify as a member of more than one community, and their connection to different communities may shift over time. In medical research, there is a tendency to consider any population of interest as a community, but that is not necessarily the case, and it is important to allow community members to self-identify. It should also be understood that membership in certain communities may have benefits, but may also confer risk (particularly in marginalized communities, such as people who use drugs, immigrant populations, or people of certain sexual or gender orientations) and it is important to be aware of those possibilities and sensitive to them when engaging. CEnR involves collaboration with a wide range of community members and leaders, often described as stakeholders (Fig. 2) [10] and it is important to be thoughtful and inclusive when engaging stakeholders in order to truly perform representative CEnR.
Fig. 2 –
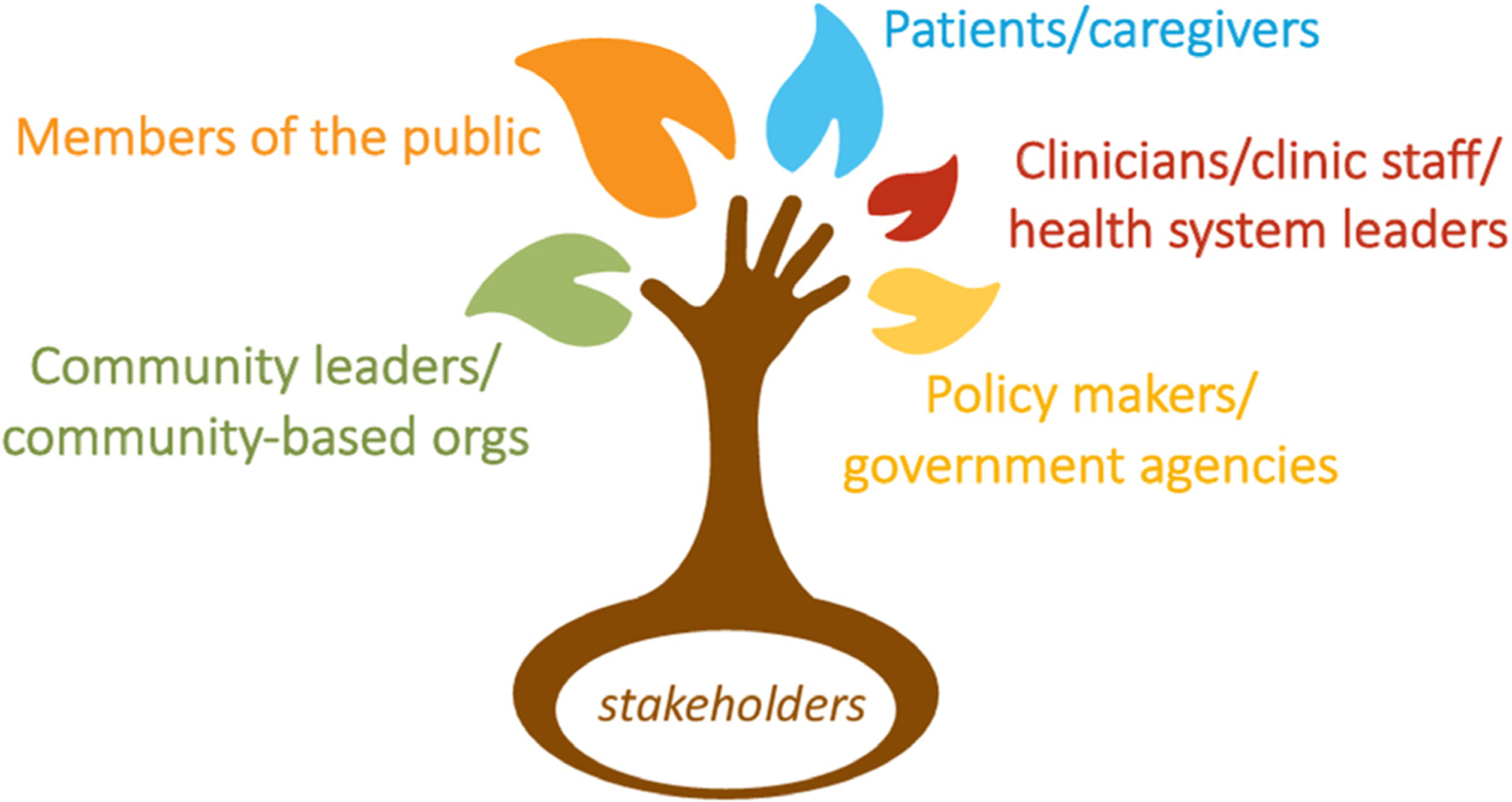
Who gets to be part of a community? Engaging a diverse group of community members is crucial to the success of community engagement. Design by PresentationGo.com. Content from Ackerman [10].
2.2. Health models and frameworks for the practice of CEnR
It is beyond the scope of this article to fully detail the health promotion and research models used in the practice of community engagement and CEnR. However, a brief description of several key related concepts is merited. these include the social-ecological model of health, the social determinants of health, community-based participatory research, and practice-based research.
2.2.1. The social-ecological model
The social-ecological model (Fig. 3) provides distinct areas for health promotion and intervention planning [11]. The social-ecological model is based on the ecological perspective of health [12], which posits that the health of an individual is affected at multiple and interacting levels. Thus, effective and sustainable health promotion and interventions should involve multiple levels and consider the interactions between them. The levels include the individual level (eg, genetics, biology, age, and health history), the relationship or intrapersonal level (eg, close personal relationships, such as family and close friend groups), the community level (eg, the multiple spheres in which people live their lives and experience social relationships, including school, workplace, and neighborhood), and finally the societal level (eg, the power structures that impact behavior and environment, including culture, social norms, and policy) [3]. CEnR uses this model to work with community partners to make relevant changes at multiple levels in order to make changes in health outcomes and reduce disparities.
Fig. 3 –
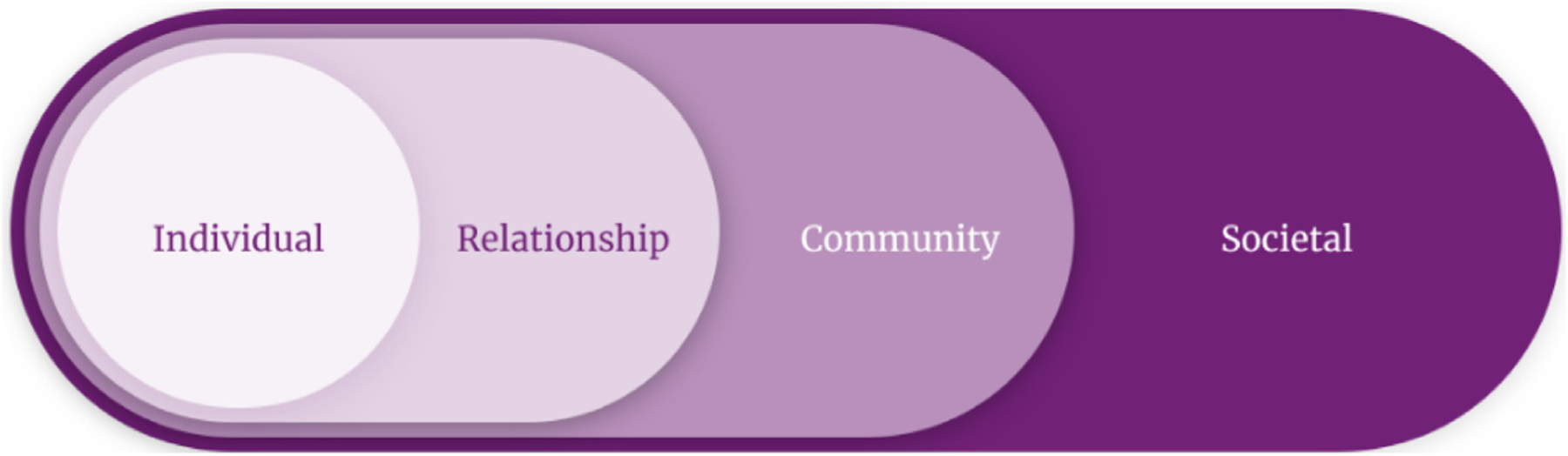
The social-ecological model. the social-ecological model operationalizes the ecological perspective of health, which posits that the health of an individual is affected at multiple and interacting levels. From Centers for Disease Control and Prevention [11].
2.2.2. The social determinants of health
Closely connected to the social-ecological model, are the social determinants of health (SDOH)—”the conditions and environments in which people are born, live, learn, work, play, worship and age” (Fig. 4) [11,13–15]. SDOH examples include access to healthy food, a safe and clean environment, education, quality health care, reliable transportation, stable housing, and economic stability. These factors comprise up to 75% of the risk factors that impact health over the course of a person’s lifetime [16,17]. Most vascular diseases are the result of untreated or poorly treated chronic disease processes that are inextricably intertwined with SDOH inequities. As such, vascular patients are a vulnerable group that stand to benefit substantially from community engagement and CEnR approaches that incorporate an appreciation of the realities of where and how patients and providers live. This can be done most effectively by engaging their voices through CEnR.
Fig. 4 –
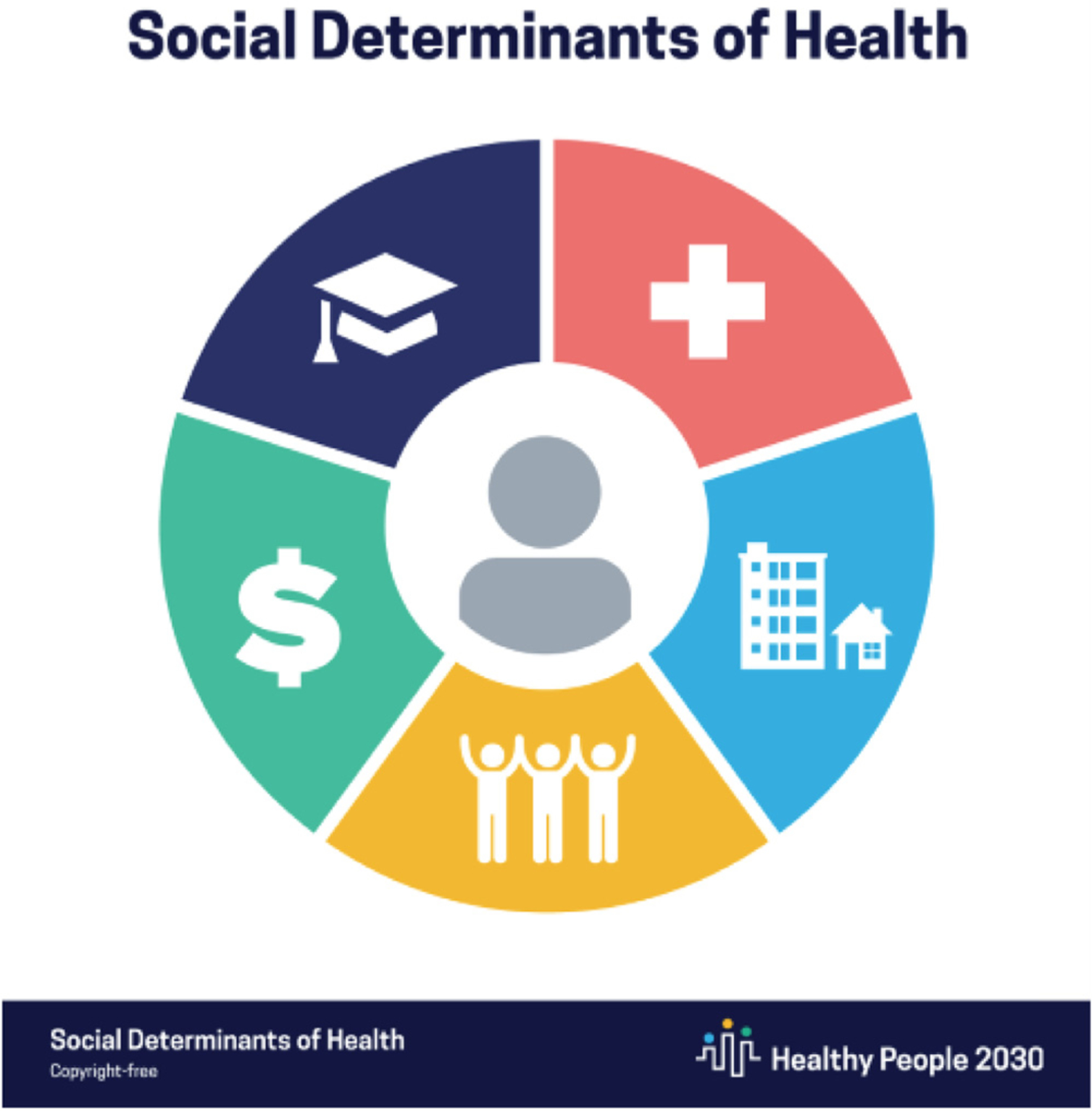
The social determinants of health. The social determinants of health are defined as “the conditions and environments in which people are born, live, learn, work, play, worship and age” and comprise up to 75% of the risk factors that impact health over the course of a person’s lifetime. From US Department of Health and Human Services, Office of Disease Prevention and Health Promotion [15].
2.2.3. Community-based participatory research
Community-based participatory research (CBPR) (Fig. 5) is a conceptual framework that embodies the fullest actualization of community member participation in research. CBPR is a form of CEnR in which community members identify a health priority in their community and seek out researchers to partner with to solve the problem. It moves beyond the scope of a particular research project to a larger-scale and sustainable collaborative effort focused on social and environmental changes to solve health problems and eliminate disparities [18,19]. Although CBPR is often beyond the level of engagement for vascular surgery researchers, there are many concepts within the framework that can be applied to CEnR at any level.
Fig. 5 –
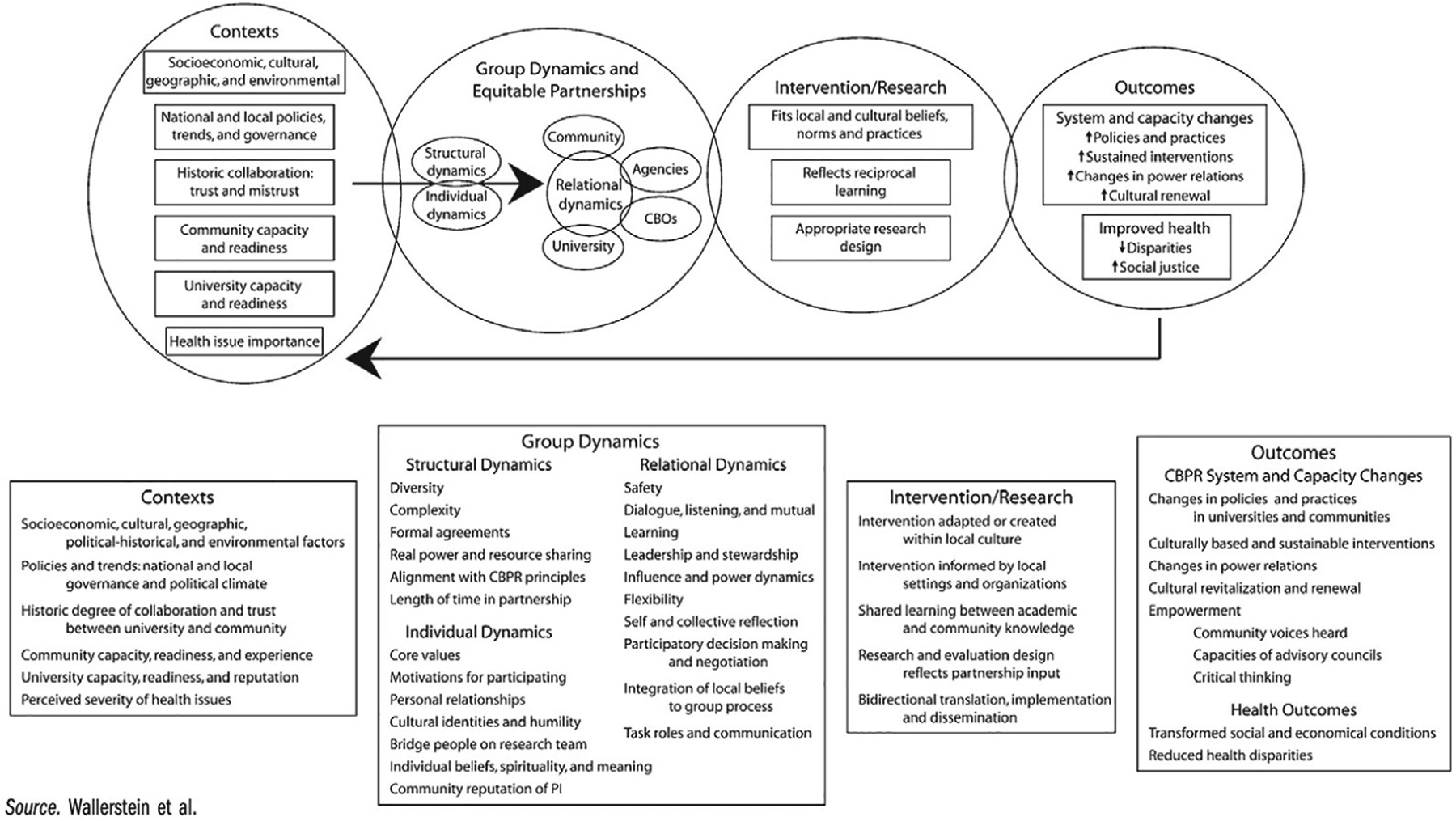
The community-based participatory research (CBPR) conceptual model. This conceptual model addresses four dimensions of CBPR and outlines the potential relationships between each. From Wallerstein and Duran [7], adapted with permission.
2.2.4. Practice-based research
Practice-based research (PBR) applies CEnR and community outreach principles to research within clinical practices. Of particular relevance to vascular surgeons, PBR views clinical practices as either a part of a community or a community in and of itself (including physicians, nurses, office staff, and patients) [20,21]. This model allows academic researchers to work with community members (both directly and through a partner clinical practice) at multiple levels. Figure 6 provides a conceptual model of a PBR project focused on diabetes in a rural, Hispanic/Latino/x community. This figure highlights the multiple aspects of community that are engaged for a PBR project to be successful.
Fig. 6 –
Practice-based research engaging the community. Practice-based research networks (PBRNs) directly engage the medical practice community (solid line) and community members (dashed line). PBRNs may engage the community members through the practice (dotted line). A community may be geographic-, demographic-, disease-specific, or a combination. Numerous other communities exist and may be engaged directly or through the practice (shaded area). From Westfall et al [21], reprinted with permission.
Vascular surgeons are well positioned to participate in PBR. Their clinical expertise gives them a unique perspective with regard to problems that arise in routine practice that create gaps between evidence-based care and actual care; and whether treatment and interventions with proven efficacy are likely to be effective in the real-world clinical setting. PBR also provides vascular surgeons with opportunities to better understand the dynamics of the clinical encounter, such as patient–physician communication, patient preference elicitation, and patient-centered outcomes to improve individual patient care [22]. By capitalizing on those spheres of influence, vascular surgeons can bridge and accelerate the link between research discoveries and clinical care in a way that is most relevant and beneficial to patients and surgical practice.
3. Considerations for performing CEnR as a vascular surgeon
3.1. Principles for planning, design, and implementation of CEnR
There are a number of key principles that must be considered in the planning, design, and implementation of CEnR. Although vascular surgeons may not be equipped to address these issues from the ground up by themselves, they should work with a team who can help them incorporate these elements into their CEnR project designs and proposals. This may be best accomplished by collaborating with researchers, practitioners, and community-based organizations who already have this expertise and have established social capital within the community. The principles are summarized as follows [3]:
- What to consider before engagement
- Define the purpose of community engagement for the project and the intended community.
- Learn about the community’s history, demographic composition, culture, social networks, and economic conditions.
- What to consider for engagement to occur
- Go to the community to build trust and establish relationships.
- Foster community self-determination.
- What to consider for engagement to be successful
- Facilitate collaborative, equitable community partnerships.
- Respect community diversity and culture.
- Identify and build on the community’s strengths, expertise, and resources to develop capacity and promote sustainability.
- Maintain flexibility to allow for changes in the community engagement process.
- Commit to long-term collaboration to maintain trust and sustain progress.
3.2. Expertise required to conduct CEnR in vascular surgery
The science of CEnR draws on the expertise of a number of fields, for example, anthropology, sociology, psychology, public health, and health disparities research. It also requires basic familiarity with multiple research methods, including outcomes research, quantitative research, qualitative research, mixed methods research, implementation science, and evaluation science. Given that it is impractical to build individual capacity in all of these areas, researchers leading a CEnR project should assemble a multidisciplinary team that has combined expertise in these subject areas. Crucially, project leaders must possess adequate knowledge and ability to lead their team in a truly collaborative fashion that fosters trust, respect, and appropriate collaboration from all of the disciplines and perspectives involved.
The art of CEnR requires the ability to communicate across a broad spectrum of people—not only research team personnel, but also community organizers, stakeholders, and lay community members—in an authentic and effective way. This may not be the primary strength of every vascular surgeon aspiring to perform CEnR and, if that is the case, it is important to have a member of the team who possesses that skill and is empowered to serve in that role.
3.3. Positionality and reflexivity in CEnR
Positionality and reflexivity are crucial concepts for understanding and applying CEnR approaches. Positionality involves understanding that one’s own race and ethnicity, cultural background, skin color, sexual orientation, ability, gender, and the intersection of these various social identities gives them greater or lesser access to social power and shapes their perspectives on the world around them [23]. Even if a person does not come from a position that traditionally confers power and privilege, their achievements and current work environment (eg, at a large academic institution) are still an important component of their identity as researcher. Thus, positionality must be acknowledged and integrated into research design, implementation, and interpretation in a way that maximizes equity. Statements of positionality by the research team are often considered a requirement in qualitative research articles, as it plays an integral role in how data are interpreted [24]. Reflexivity represents the examination and awareness of one’s identities and positionality and how they can manifest in the research they do. Reflexivity is especially critical when approaching a community for partnership in CEnR [25]. For example, the power differential between an academic researcher and community provider, or scientist and lay community member, must be considered when approaching potential community partners. Historically marginalized community members may have significant and understandable trust issues when approached by researchers who are members of groups that have played a role in marginalizing that community. That is why it is so important for researchers to demonstrate appropriate sensitivity and sociocultural humility, understand the role of power and privilege in collaborative partnerships, and have a plan for power sharing before initiating engagement.
With that in mind, the authors would like to state their own positionality as it pertains to this article:
S.D.M. is a White woman born and raised by Jewish immigrant parents in an urban community in Montreal, Quebec, Canada. She practices vascular surgery at a quaternary care center in Morgantown, WV and has been working with rural communities since 2017.
C.A.P is a Black woman born and raised in Detroit, MI, who is currently an integrated vascular surgery trainee at Michigan Medicine, an academic, tertiary care center in Ann Arbor, MI.
L.M.D. is a White woman born and raised in an Italian culture by Christian parents in Montreal, Quebec, Canada. She works as a vascular surgeon in an urban quaternary care center in Montreal.
L.Y. is a White woman born and raised in West Virginia. She is the Director of the Pocahontas County Family Resource Network located in Marlinton, WV. She has experience planning, developing, and sustaining community engagement efforts in rural Pocahontas County for 14 years.
K.K. is a White woman practicing vascular surgery in a tertiary center in Tulsa, OK, and is employed by the University of Oklahoma in an academic setting.
L.N.O is a Mexican-American women born to migrant farm workers on the border in South Texas. She is a private practice surgeon in San Antonio, TX and founder of the SAVE Clinic, which addresses health inequities. She operates at five metropolitan hospitals.
M.P. is a Black woman born and raised in the Southern United States. She and her siblings were the first in her family born with all of their civil rights. She is a practicing internist and health equity researcher in an academic medical center in Chicago, IL.
G.D. is a White woman born and raised in the suburban northeast United States, who has practiced CEnR with a focus on rural health disparities for more than 2½ decades.
4. The role of community-engaged research and outreach to reduce amputation disparities
4.1. Amputation disparities and CEnR
Amputation is a devastating but preventable complication of diabetes and peripheral artery disease (PAD). It is also a marker for severe and poorly managed cardiovascular disease; 50% to 74% of patients with diabetes and PAD who undergo amputation die at 5 years due to cardiac or cerebrovascular complications [26,27]; this is a prognosis worse than most forms of cancer. Amputations are highly preventable, a foot ulcer precedes 85% of amputations [28] and diabetes-related amputations have been consistently found to be preventable with access to high-quality medical, podiatric, and vascular care [28,29]. As such, disparities in amputation rates have been adopted as a leading health indicator and national objective for achieving equity in the treatment of diabetes across the United States [22,30]. Although the risk for amputation is highest in communities with higher levels of diabetes, cardiovascular disease, and tobacco use, it is also disproportionately higher in communities affected by high economic hardship and chronic external stressors [31,32]. Multiple studies have identified variation in amputation risk based on socioeconomic, racial, ethnic, and geographic (rural/urban) status [31,33–38]. Amputation disparities are therefore particularly well suited to CEnR approaches, as they tend to occur at higher rates in certain community settings, and are closely related to inequities related to the SDOH. Therefore, engaging community members as partners in order to assess contextual issues related to diabetes and vascular care within the community and creating meaningful strategies to address them are particularly beneficial for amputation prevention interventions.
4.2. Examples of CEnR addressing amputation disparities from the existing literature
Currently, there is little evidence regarding community-engaged interventions in the vascular surgery literature. However, such interventions have long been implemented in a number of chronic diseases, such as cardiovascular disease, diabetes, and others. Some examples of effective interventions include patient education and self-management approaches for high-risk patients with hypertension; focused outreach through community health representatives for patients with diabetes; community engagement to enhance stroke preparedness among high-risk communities; and community-wide integrated, comprehensive cardiovascular risk reduction programs in low-income rural communities [39–42].
Although addressing general cardiovascular risk factors is important for tackling the upstream contributors of vascular disease, interventions focused on vascular disease itself are also needed. Research on PAD and diabetes-related amputation is particularly well suited to CEnR. Compared with other atherosclerotic disease processes, such as stroke and coronary artery disease, there is a lack of awareness among the public and providers about PAD [43]. This lack of awareness extends beyond the clinical implications of PAD, such as increased risk of stroke, heart attack, and death, to the economic burden and significant impact on patient quality of life that occurs when PAD progresses to revascularization, months of wound care, and then amputation. CEnR interventions represent an opportunity to address critical gaps in amputation through primary and secondary prevention to mitigate amputation disparities. Through thoughtful collaborations among clinicians, public health experts, patients, community members, and policy makers, local infrastructure can be developed to support delivery of culturally relevant PAD and diabetes-related foot care to those in greatest need [44].
4.3. Examples of amputation prevention interventions using community-engaged approaches
Although not yet published in the literature, many of the authors of this article are conducting work that uses CEnR approaches to reduce amputation disparities. Next, we present four case studies illustrating this work and the CEnR principles used.
4.3.1. A community-engaged approach to implement an amputation prevention intervention in a high-risk rural community in West Virginia (S.D.M.)
4.3.1.1. Background
Appalachia is a highly rural region with higher overall cardiovascular disease deaths, diabetes prevalence rates, and tobacco use than the rest of the United States [45–49]. West Virginia, a highly rural state, is the only state fully within Appalachia [50]. Current amputation interventions focus little on community context and individual-level factors that play crucial roles in the development of foot complications, including amputation. This PBR project uses CEnR approaches to effectively implement evidence-based amputation interventions in rural West Virginia.
4.3.1.2. Methods
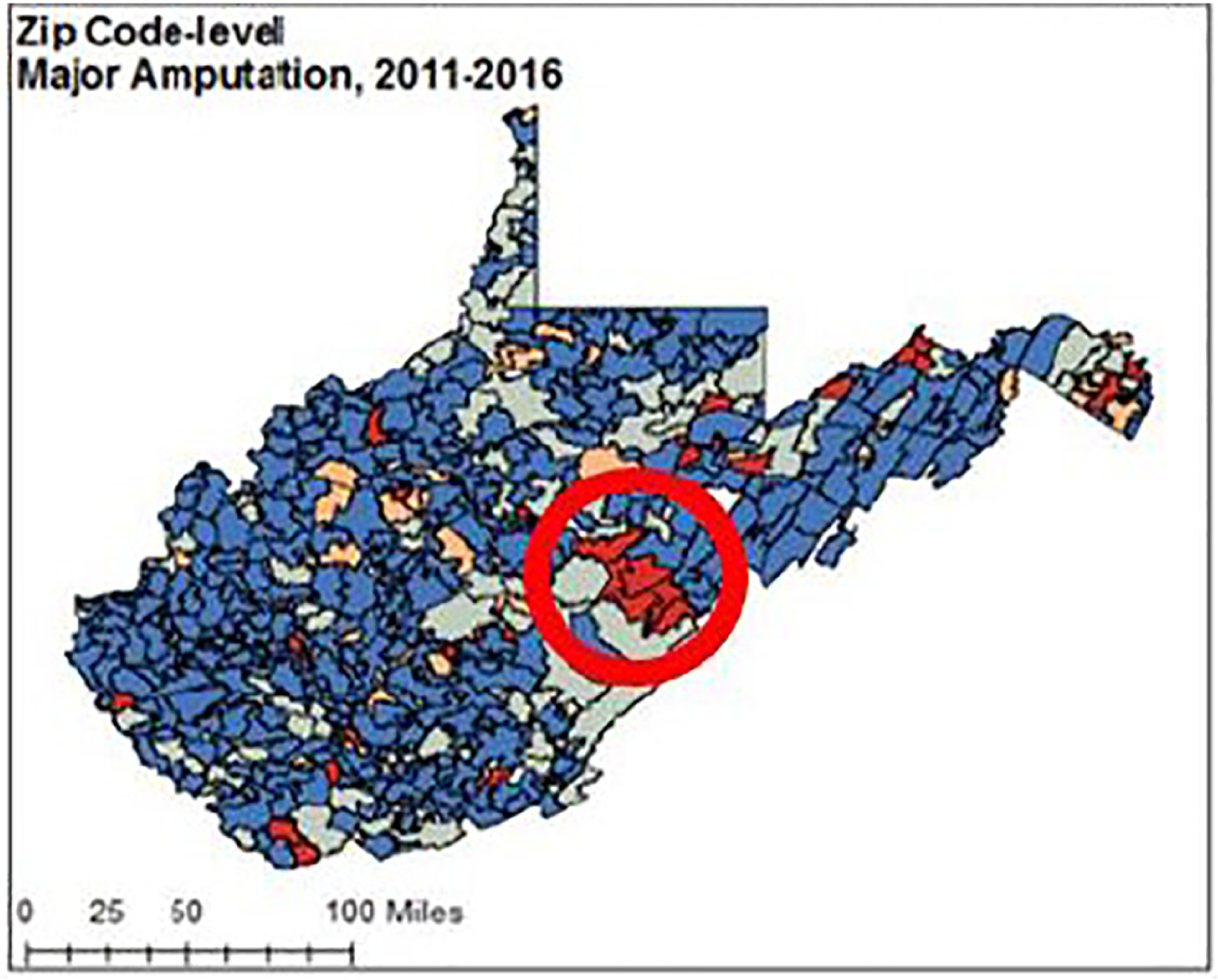
The project team includes individuals with clinical, epidemiological, and intervention expertise with a shared agenda, that is, to address WV amputation disparities using CEnR. The first project step was to use a mixed-methods approach to gain a thorough understanding of the epidemiology and etiology of amputations across the state. First, we identified a WV “geographic hotspot” (ie, community area) disproportionately affected by amputation using high-granularity Geographic Information Systems (GIS) to identify clusters of high-risk ZIP codes (Fig. 7) [36]. Next, we identified risk factors for amputation by analyzing a large WV dataset and followed up with qualitative interviews with people with amputations and providers—focusing on the high-risk areas identified by GIS—and informed by the risk factors identified in the database analysis. A mixed-methods analysis of the quantitative and qualitative data was performed, and the results were then translated into accessible language and disseminated to key stakeholders in the affected communities. This was accomplished by coordinating meetings with local public health departments, city councils, local clinics, major community organizers, and any other stakeholders identified through these meetings. Resulting community conversations led to the development of the project plan, which ultimately became a PBR project that sought to adapt evidence-based interventions for amputation prevention to local clinics [51–55]. Further community engagement was accomplished through site visits, focus groups with community clinic partners, and the creation of a project advisory board composed of members who provide care to patients in the community with diabetes. In addition to the project advisory board, a community advisory board eventually developed to address community interest in developing population-level approaches to diabetes prevention and diabetes care delivery within the community.
Fig. 7 –
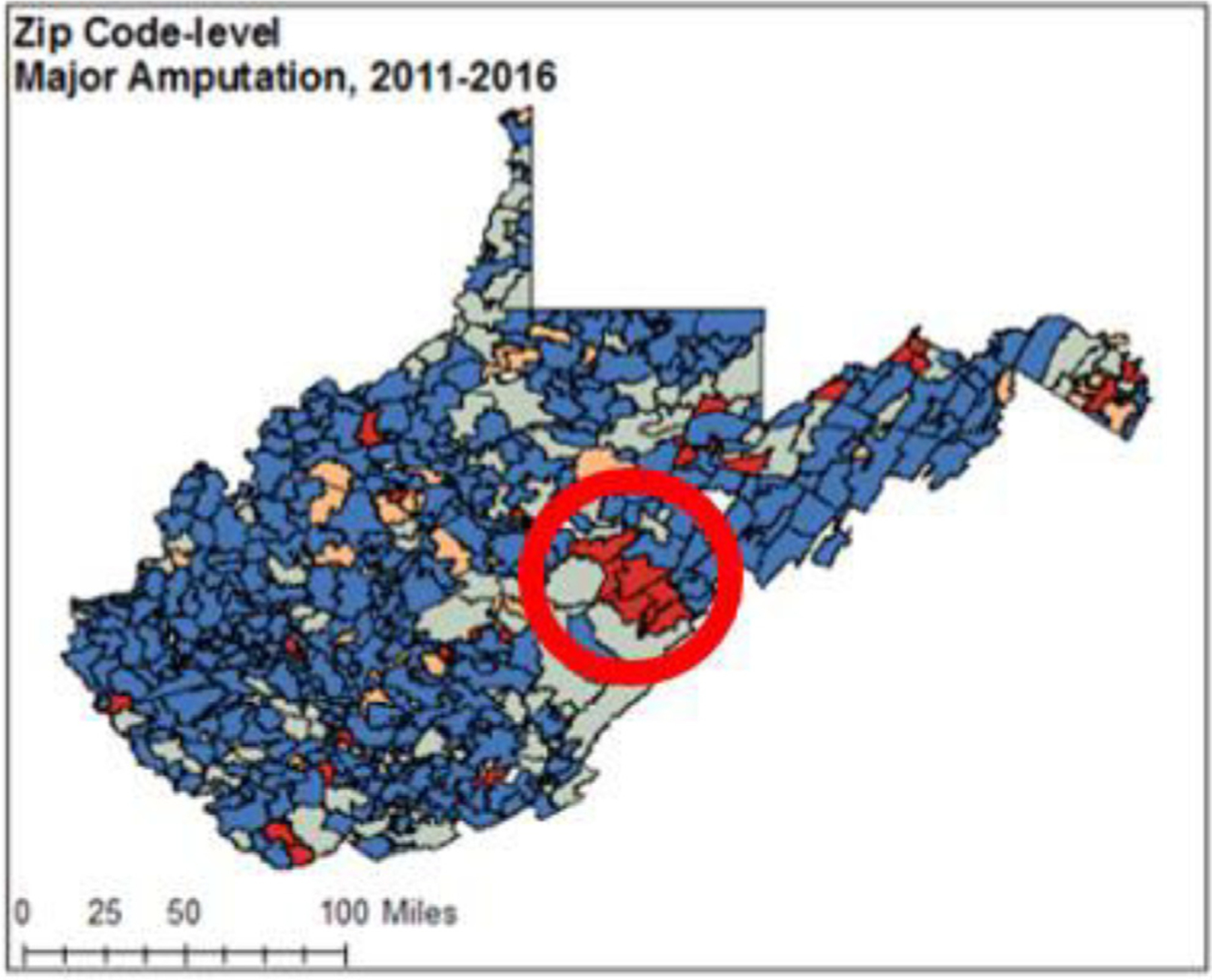
Risk for amputation in West Virginia. ZIP code–level model-fitted relative risk estimates for major amputation in West Virginia 2011 – 2016, adjusting for covariates. Highlighting a high-risk cluster in Pocahontas County. From Minc et al [36], reprinted with permission.
4.3.1.3. Comments on the community engagement aspects of this project
Identifying our community and going there in person to meet and translate, disseminate, and discuss data with key stakeholders was critical to building the foundation for our project. The community is 3 hours south of the West Virginia University flagship hospital (and approximately 3 hours from a tertiary-level center) and driving to and from the area can sometimes be difficult due to road conditions. However, the act of “showing up” has been crucial to the success of this project for several reasons. First, witnessing the day-to-day challenges and opportunities of the community helped to reduce the research team’s own biases about high-risk rural communities, specifically in terms of seeing first-hand the challenges that patients face regularly in accessing vascular care, but also in terms of understanding the strength, capability, and structures that already exist within the community. Second, our presence demonstrated a level of authenticity and dedication to community partners that we felt was very important for the project. It should be emphasized however, that this “act of showing up,” is not meant to be performative (ie, showing up and expecting the community members to be grateful for your presence), but demonstrates the appropriate level of respect that should be given to a partner who is allowing you to enter their “home” as a guest, and is providing their own time, resources, and expertise to a project. Finally, CEnR approaches are reflected throughout the research design of the project. This has been achieved through careful planning to include community input and collaboration in several key areas, including community assessment, intervention adaptation, implementation and assessment, and results dissemination. This careful, collaborative planning is a critical component of CEnR.
4.3.2. Working with primary care providers to care for those at risk for amputations in Oklahoma using a PBR model (K.K.)
4.3.2.1. Background
4.3.2.1.1. Values and a goal.
The University of Oklahoma-Tulsa vascular surgery’s mission is to improve vascular health in Oklahoma, with the goal to reduce our state’s amputation rate. During every meeting, every invited presentation, every introduction, we define this goal.
4.3.2.2. Methods
4.3.2.2.1. Using the expertise of others.
We began by creating a diverse team with experience in quantitative analytics, multidisciplinary clinical work, and qualitative principles. In addition, we joined forces with the Oklahoma Primary Healthcare Improvement Collaborative, who had successfully completed projects that aligned directly with our values of improving cardiovascular care with primary care practices and focusing on patient-centered outcomes [56]. As we have developed, we have added expertise in implementation science, cultural competency, and social work.
4.3.2.2.2. Inquiry.
Through inquiry, the picture of Oklahoma’s vascular health began to form. Oklahomans rate significantly higher in years of life lost per 100,000 persons than the US rate due to cardiovascular disease [57]. Oklahoma is unique in many ways, with significant representation from populations at risk for amputations, including American Indians, the uninsured, and persons living in rural areas (which represents 34% of Oklahomans) [58,59]. In addition, Oklahoma ranks 50th in overall state health system performance and scores in the bottom quartile in access to care, healthy lives, and health equity [60]. There is also evidence of limited access to specialty care, with only 12 board-certified vascular surgeons practicing in Oklahoma in 2019 (unpublished data) for a population of 4 million people. Furthermore, amputation rates in Oklahoma have one of the greatest increases of any state over the last 10 years [61]. We evaluated amputation rates in our state based on different geographic regions, patient sociodemographic characteristics, and insurance status. In tandem, we conducted surveys across the state with primary care practices and conducted interviews with people with amputations and primary care providers to elucidate perceptions about amputation prevention and the reasons for limb preservation failures. These efforts to understand where Oklahoma stands in vascular health and amputations have created a foundation for further outreach.
4.3.2.2.3. Outreach.
The community outreach portion of our work includes observing and educating primary care practices, conducting free noninvasive vascular screening, providing and distributing educational materials, and developing partnerships. This work has been intentionally fluid and conducted with inquiry as we partner with clinical practices and patients, with aspirations to build trust and commitment. We hope to gain a better understanding of challenges facing primary care practices, to collaborate and create effective educational programs, and begin a responsive referral network that can empower the primary care practices to be confident and effective in their care of patients at risk for amputation.
4.3.2.3. Comments on the community engagement aspects of this project
As the project has progressed, the element of the unexpected and stirring within the community has fostered collaboration with tribal nations, media attention, delivering Grand Rounds, and meeting community advocates in a small room with a round table. We believe these are the intangibles that will push the goal forward to create change.
4.3.3. A community-engaged intervention to implement an amputation prevention intervention in Montreal, Quebec (L.D.)
4.3.3.1. Background
In Quebec, more than 675,000 people live with diabetes and the prevalence of diabetes has increased 42% between 2001 and 2019 [62]. Optimizing interdisciplinary care coordination for patients with diabetes and vascular-related foot complications is a top priority for provincial action to transform health care quality. The focus of this project was to understand the unique epidemiological landscape of amputations in Quebec, pair this with the lived experiences of stakeholders, and use this information to implement interdisciplinary amputation prevention teams across the province.
4.3.3.2. Methods
4.3.3.2.1. Epidemiology.
Our first goal was to establish a better understanding of the epidemiology of amputations in Quebec. In collaboration with Institut National d’Excellence en Santé et en Services Sociaux and l’Institut Universitaire de Cardiologie et de Pneumologie de Québec, we calculated crude and age-standardized annual incidence rates of primary lower extremity amputation associated with diabetes or PAD among hospitalized adults 40 years or older. The results demonstrated that, in 2019, the crude rate of primary lower extremity amputation was 116.0 per 100,000 with 84.8 and 21.9 per 100,000 being minor and major, respectively. Unfortunately, there is a paucity of available data on the epidemiology of amputation in Canada, and it is not possible to compare these findings with other population data reported in the literature [63]. The next stage for this project is to perform a geospatial analysis to identify geospatial hotspots for lower extremity amputation in the province of Quebec.
4.3.3.2.2. Development of partnerships and community support.
Our team has established partnerships with patients, caregivers, providers, and decision makers across disciplines and across Quebec. Partners have included patients who have undergone limb preservation procedures or amputations, caregivers of those impacted by amputation, nurses, wound care specialists, plastic surgeons, vascular surgeons, interventional radiologists, vascular medicine specialists, and lawyers with expertise in social justice. The latter group was of particular importance to ensure that the project moves forward with a lens toward equity and an understanding of how to create lasting change on a social-political level. We have also created a community advisory board of patients, caregivers, providers, and decision makers across le Réseau Universitaire Intégré de Santé et Services Sociaux. We have local champions within each Réseau Universitaire Intégré de Santé et Services Sociaux across specialties involved in the care of patients with amputation prevention, as well as partners developed in our community engagement strategy. We have also partnered with community organizations who assist some of the most vulnerable populations in Montreal and Quebec, that is, persons living in homelessness and Indigenous populations.
4.3.3.3. Comments on the community engagement aspects of this project
Identifying key stakeholders and community partners, developing and fostering those relationships, and meeting to understand individual and community needs was key for our project development. The act of having face-to-face contact on a regular basis, “showing up,” and listening has been crucial to the success of the initial phases of this project. Having stakeholders engaged early (ie, during the brainstorming and project development phase) encouraged communal goals and “buy-in,” and sustained motivation to continue contributing throughout the project. Having research team members present for monthly project updates, and ongoing listening to local needs has demonstrated dedication to the communal goal of improving health care quality and tackling major social, structural and environmental barriers to preventive foot care. Although this case study is in its initial phases, using a CEnR approach has already delivered benefits in terms of community and patient engagement.
4.3.4. Community engagement in private practice: The San Antonio Vascular and Endovascular Clinic (L.O.)
4.3.4.1. Background
In contrast to the previous case studies, the San Antonio Vascular and Endovascular Clinic (SAVE) is an example of a community-based private vascular surgery practice that uses community engagement methods outside of academia to address amputation disparities in an underserved community.
The SAVE clinic is located in San Antonio, TX, which comprises >70% of Bexar County. Amputation rates due to diabetes in Bexar County are >30% higher than the Texas state-wide rate; within the county’s 71 ZIP codes, 9 ZIP codes have greater than double the state-wide rate. In addition, these 9 ZIP codes have a predominantly Hispanic/Latino/x population and have a higher prevalence of PAD risk factors (eg, diabetes and obesity), higher poverty rates, and worse socioeconomic conditions relative to other Bexar County ZIP codes [64].
4.3.4.2. Methods
4.3.4.2.1. Establishing clinic locations with community partners.
In establishing clinic locations, the decision was made to have one primary full-time clinic and several part-time clinics to increase access to care in those ZIP codes with the highest amputation rates. Although the acquisition of a primary location is a normal internal business process, the identification of the part-time clinics required identifying and networking with other private practices within the high-risk ZIP codes to explore the possibility of part-time lease arrangements. These other practices not only represented potential access points for patients to SAVE, but also potential collaborative partners in basic amputation prevention, including podiatrists, orthopedic surgeons, and primary care physicians.
4.3.4.2.2. Engagement with local elected officials.
In an ongoing engagement effort, SAVE attends formal meetings with local elected officials, including city council members, county commissioners, state representatives and senators, and mayors of San Antonio and other municipalities. The goal of these meetings was to improve the elected offices’ awareness and knowledge regarding clinical and socioeconomic factors contributing to amputation rates, and to explore potential solutions that can be supported by the office. In September 2022, SAVE partnered with the 7 San Antonio city council districts representing the highest amputation rates to conduct PAD screening events, which included resources regarding common SDOH. Forty percent of the 174 PAD screenings were abnormal, indicating that the city council district offices were able to effectively reach their constituents in need of this service.
4.3.4.2.3. Staff engagement with patients and integrating community health workers.
In response to the overwhelming SDOH barriers faced by high-risk patients. SAVE staff members have been trained to provide additional support to help patients overcome these issues. For example, patients frequently cite transportation issues as reasons for delayed or discontinued health care and many are unaware of transportation benefits included in their health insurance plans or are unable to navigate the process to arrange for transportation services. In response to this, employees were trained on methods to help patients obtain transportation to clinic sites and to easily identify transportation resources to help patients learn how to obtain transportation for future appointments. In addition, SAVE has employed a community health worker (CHW) to help patients navigate additional challenges and improve adherence to treatment and medication plans. A CHW is a lay member of the community who shares ethnicity, language, socioeconomic status, and life experiences with the community members they serve [65,66]. CHWs commonly offer interpretation and translation services, provide culturally appropriate health education and information, give informal counseling and guidance on health behaviors, and advocate for individual and community health needs. CHWs have been shown to improve adherence to medication regimens by improving patient satisfaction with medication information [67], and through coaching on medication safety behaviors [68]. CHWs also offer support to help patients at high risk for amputation in several situations, including obtaining high-cost medications (such as certain anticoagulation, antiplatelet, and cholesterol medicines) for free or at highly discounted rates, navigating access to other specialists or health care resources, and obtaining affordable health insurance or government support.
4.3.4.3. Comments on the community engagement aspects of this project
The SAVE clinic uses a number of community engagement approaches in a private practice setting, including using multiple levels of the social-ecological model (eg, engaging community health workers and policy makers) to improve the health of the community, and building a practice with an appreciation for barriers related to the SDOH. As a community-based practice, however, it is limited from a research perspective, and would benefit from collaboration with an academic partner to evaluate outcomes and disseminate findings to other vascular surgeons.
4.4. Case study lessons and steps to take action
Although each of the presented cases come from very diverse settings, there are a number of overarching themes that run through each project. These themes can be summarized into action points that can be applied to other CEnR projects focused on amputation prevention.
4.4.1. Work with multidisciplinary teams
All of the projects required the expertise of team members from multiple academic disciplines and skill sets in order to obtain rigorous quantitative and qualitative data, organize, engage and collaborate with community members, and design and implement interventions. Building and leading a multidisciplinary team is a key component for any CEnR project leader.
4.4.2. Identify your community
As discussed, the risk of amputation tends to be higher in certain communities compared to others. A key component of all of the studies discussed was the use of epidemiologic methodologies to identify high-risk areas for amputation in order to focus project resources in those areas.
4.4.3. Mobilize community members
Once “hot spots” were identified, project teams focused on disseminating those data directly to community stakeholders in order to mobilize community partners. This is crucial in order to build project advisory boards with members that are able to meaningfully engage in identifying approaches to address the issue.
4.4.4. Assess community risk factors, needs, and resources—with a specific focus on SDOH
A comprehensive assessment of the etiology of amputation within the community, as well as gaining a deep understanding of existing community needs, resources, and perceptions surrounding amputations is critical. In the discussed cases, this was achieved mainly using mixed methods (ie, quantitative and qualitative) approaches. Qualitative approaches are particularly important in elevating the voices of those that are directly impacted by amputation and for illuminating quantitative findings.
4.4.5. Moving forward with community members
All of the projects we discussed used community engagement principles in order to design, implement, and assess their amputation prevention interventions. Meaningful engagement of community members at all steps of the project is essential in order to build effective and sustainable projects.
4.5. CEnR limitations
Although CEnR has the potential to address health disparities and improve outcomes, this approach does have limitations. CEnR can be a slow and winding process and requires moving at the speed of trust. This is because the hallmark of CEnR is community–academic collaboration or partnership, which takes time to cultivate and sustain. In addition, the process of identifying problems relevant to the community and generating solutions is often marked by trial and error, which can also be time-intensive. Another issue is related to expectations regarding the speed and timelines of CEnR projects. From a research funding perspective, non-CEnR timelines cannot be applied generically to CEnR, which can make funding mechanisms difficult to navigate. In addition, community partners who do not have experience working with researchers may have variable expectations for deliverables and markers of productivity [69]. All of these issues can be resolved with careful communication at every stage of the project and should be put in writing for the sake of clarity whenever possible.
Another limitation of CEnR is inherent in its strength. At its core, CEnR shifts the focus to addressing community relevant needs and contextualizes interventions. Although the local specificity of interventions is a strength, it potentially limits generalizability to other communities, which may be facing different issues and have different capacities or even willingness to engage in research efforts [70].
5. Perspective from a community partner on CEnR in rural communities (L.Y.)
Rural communities are often perceived as tranquil, serene, isolated, and beautiful places to live. We are often envied for the lack of traffic and hustle in our daily lives. Although this is often true, we also experience higher levels of poverty, unemployment, and lack basic needs, such as access to healthy, affordable food. Local culture provides a sense of identity for rural communities and residents. This identity facilitates common understanding, traditions, and values that are all central to the identification of plans of action to improve well-being. Culture contributes to building a sense of local identity and solidarity.
Services in rural communities are often provided in overlapping and confusing delivery systems that leave our residents resentful and resistant. In addition, rural and disenfranchised populations tire of becoming “test subjects” for researchers and pilot projects that result in publications and data, but do not enact meaningful change in the community. Researchers can navigate this resentment by being “guests” in these communities. A deliberate effort to demonstrate honor for the opportunity to work in rural communities can facilitate your work. It is important to remember that others have come before you and may have left without fostering trust and collaboration. It is the job of each new researcher to repair damage that they did not create and work to ensure relationships remain intact after the project ends. A successful researcher will foster change by the community and for the community, supported by people with resources to help. Habits for successful community engagement include:
Seek first to understand, then be understood. Be sensitive to the needs of others as individuals and organizations, as well as circumstances that shaped community perspective and culture before you, remembering that no community wants to be known for health inequalities.
Build relationships based on trust and clear communication. “Communities” will both form and disband, it is okay. Be open and transparent as people engage and disengage during the process. They often talk to other stakeholders, so be consistent and truthful with messaging.
Focus on being representative and participatory; the more people who give opinions, the better the results. Community engagement is more labor-intensive than is often realized and requires investment in time and resources. It is helpful to identify a “champion” who can inspire and call others to action. Shining the spotlight on this champion is a great way to lead from behind.
Look outside your project’s scope to see how you can benefit community efforts that directly or indirectly dovetail into your mission. Taking this extra step to help others be successful sends a powerful message. This work calls for sympathy and empathy. If done right, the return on invest will be huge.
When there are successful breakthroughs, celebrate and share the excitement.
6. Conclusions
CEnR is a powerful tool to create sustainable and effective change in health outcomes, amplify the voices of patients and community members, and create meaningful translatable research. It is a particularly relevant approach for research focused on addressing amputation disparities, as it provides a mechanism to identify and address the SDOH and the pertinent barriers of care in communities that struggle with high amputation rates. Vascular surgeons who are interested in pursuing CEnR or community engagement are encouraged to consider the principles and action items discussed in this article, as well as collaborations with others with experience in the field before engaging. CEnR requires time, collaboration, and thoughtful work for success, but the exponential rewards for researchers, community members, and, most importantly, our patients, will elevate vascular care in our communities.
Acknowledgments
Samantha D. Minc is supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (K23DK128569) and the Society for Vascular Surgery Foundation/American College of Surgeons. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Society for Vascular Surgery Foundation, or the American College of Surgeons. Kelly Kempe is supported by the Volunteers in Service To All (VISTA) grant from the Society for Vascular Surgery Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Society for Vascular Surgery Foundation. Geri Dino is supported by the Centers for Disease Control and Prevention’s Cooperative Agreement Number U48-DP-006391 for The West Virginia Prevention Research Center. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Laura Young is supported by a grant from the West Virginia Department of Health and Human Services/Bureau of Children and Families (WVDHHR/BCF). The content is solely the responsibility of the author and does not necessarily represent the official views of the WVDHHR/BCF.
Footnotes
Declaration of Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
REFERENCES
- [1].Cashman SB, Adeky S, Allen AJ 3rd, et al. The power and the promise: working with communities to analyze data, interpret findings, and get to outcomes. Am J Public Health 2008;98:1407–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].The root causes of health inequity. Communities in Action: Pathways to Health Equity. National Academies Press; 2017. p. 99–184. [PubMed] [Google Scholar]
- [3].Clinical and Translational Science Awards Consortium Community Engagement Key Function Committee Task Force on the Principles of Community Engagement. Principles of Community Engagement. National Institutes of Health; 2011. [Google Scholar]
- [4].Alinsky SD. Citizen Participation and Community Organization in Planning and Urban Renewal. Industrial Areas Foundation; 1962. [Google Scholar]
- [5].Chávez V, Minkler M, Wallerstein N, et al. Community organizing for health and social justice. In: Cohen L, Chavez VC, Chehimi S, editors. Prevention Is Primary: Strategies for Community Well-Being. 2nd ed.. John Wiley and Sons; 2007. p. 87–112. [Google Scholar]
- [6].Freire P Pedagogy of the Oppressed. Herder and Herder; 1970. [Google Scholar]
- [7].Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract 2006;7:312–23. [DOI] [PubMed] [Google Scholar]
- [8].Michener L, Cook J, Ahmed SM, et al. Aligning the goals of community-engaged research: why and how academic health centers can successfully engage with communities to improve health. Acad Med 2012;87:285–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].TOOL: Engagement Continuum. Tamarack Institute. Accessed December 31, 2022. https://www.tamarackcommunity.ca/library/the-engagement-continuum
- [10].Ackerman S Introduction to community engaged-research, module 1. Community-Engaged Research. UCSF Implementation Science Program University of California San Franscisco; 2022. [Google Scholar]
- [11].The Social-Ecological Model A Framework for Prevention. Centers for Disease Control and Prevention; 2007. Published Accessed October 18, 2022 https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html.
- [12].National Cancer Institute Theory at a Glance: A Guide for Health Promotion Practice. US Department of Health and Human Services. Public Health Service, National Institutes of Health, National Cancer Institute; 1995. [Google Scholar]
- [13].Bierman AS, Dunn JR. Swimming upstream. Access, health outcomes, and the social determinants of health. J Gen Intern Med 2006;21:99–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Social Determinants of Health: Know What Affects Health. Centers for Disease Control and Prevention. Published 2018. Accessed July 22, 2018. https://www.cdc.gov/socialdeterminants/.
- [15].Healthy People 2030. US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Accessed December 21, 2022. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
- [16].Lowry M Want healthier communities?. Address social factors. American Public Health Association; 2018. Voices. Published 2018. Accessed August 21 http://www.publichealthnewswire.org/?p=20607. [Google Scholar]
- [17].Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014;129(2):19–31 suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health 2010;100(1):S40–6 suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998;19:173–202. [DOI] [PubMed] [Google Scholar]
- [20].Andersson N Participatory research-a modernizing science for primary health care. J Gen Fam Med 2018;19:154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Westfall JM, Fagnan LJ, Handley M, et al. Practice-based research is community engagement. J Am Board Fam Med 2009;22:423–7. [DOI] [PubMed] [Google Scholar]
- [22].Healthy People 2020. US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Updated November 27, 2018. Accessed November 27, 2018. https://www.healthypeople.gov/node/4121/data_details
- [23].Altman MR, Kantrowitz-Gordon I, Moise E, et al. Addressing Positionality within case-based learning to mitigate systemic racism in health care. Nurse Educ 2021;46:284–9. [DOI] [PubMed] [Google Scholar]
- [24].Malterud K Qualitative research: standards, challenges, and guidelines. Lancet 2001;358(9280):483–8. [DOI] [PubMed] [Google Scholar]
- [25].Muhammad M, Wallerstein N, Sussman AL, et al. Reflections on researcher identity and power: the impact of positionality on community based participatory research (CBPR) processes and outcomes. Crit Sociol (Eugene) 2015;41:1045–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Aulivola B, Hile CN, Hamdan AD, et al. Major lower extremity amputation: outcome of a modern series. Arch Surg 2004;139:395–9 discussion 399. [DOI] [PubMed] [Google Scholar]
- [27].Armstrong DG, Swerdlow MA, Armstrong AA, et al. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 2020;13:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care 1990;13:513–21. [DOI] [PubMed] [Google Scholar]
- [29].Armstrong DG, Wrobel J, Robbins JM. Guest editorial: are diabetes-related wounds and amputations worse than cancer? Int Wound J 2007;4:286–7. [DOI] [PubMed] [Google Scholar]
- [30].Healthy People 2030: Reduce the rate of foot and leg amputations in adults with diabetes - D-08. US Department of Health and Human Services: Office of Disease Prevention and Promotion. Accessed October 22, 2022. https://health.gov/healthypeople/objectives-and-data/browse-objectives/diabetes/reduce-rate-foot-and-leg-amputations-adults-diabetes-d-08/data
- [31].Tseng CL, Helmer D, Rajan M, et al. Evaluation of regional variation in total, major, and minor amputation rates in a national health-care system. Int J Qual Health Care 2007;19:368–76. [DOI] [PubMed] [Google Scholar]
- [32].Healthy Chicago 2.0 Partnering to improve Health Equity, 2016–2020. Chicago Department of Public Health; 2016. [Google Scholar]
- [33].Feinglass J, Abadin S, Thompson J, et al. A census-based analysis of racial disparities in lower extremity amputation rates in Northern Illinois, 1987–2004. J Vasc Surg 2008;47 1001–7; discussion 1007. [DOI] [PubMed] [Google Scholar]
- [34].Stevens CD, Schriger DL, Raffetto B, et al. Geographic clustering of diabetic lower-extremity amputations in low-income regions of California. Health Aff (Millwood) 2014;33:1383–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Margolis DJ, Hoffstad O, Nafash J, et al. Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care 2011;34:2363–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Minc SD, Hendricks B, Misra R, et al. Geographic variation in amputation rates among patients with diabetes and/or peripheral arterial disease in the rural state of West Virginia identifies areas for improved care. J Vasc Surg 2020;71:1708–17 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].McGinigle KL, Kalbaugh CA, Marston WA. Living in a medically underserved county is an independent risk factor for major limb amputation. J Vasc Surg 2014;59:737–41. [DOI] [PubMed] [Google Scholar]
- [38].Arya S, Binney Z, Khakharia A, et al. Race and socioeconomic status independently affect risk of major amputation in peripheral artery disease. J Am Heart Assoc 2018;7(2):e007425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Record NB, Onion DK, Prior RE, et al. Community-wide cardiovascular disease prevention programs and health outcomes in a rural county, 1970–2010. JAMA 2015;313:147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Zoellner J, Connell C, Madson MB, et al. HUB city steps: a 6-month lifestyle intervention improves blood pressure among a primarily African-American community. J Acad Nutr Diet 2014;114:603–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Trevisi L, Orav JE, Atwood S, et al. Community outreach for Navajo people living with diabetes: who benefits most? Prev Chronic Dis 2020;17:E68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Skolarus LE, Zimmerman MA, Bailey S, et al. Stroke ready intervention: community engagement to decrease prehospital delay. J Am Heart Assoc 2016;5(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Hirsch AT, Criqui MH, Treat-Jacobson D, et al. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA 2001;286:1317–24. [DOI] [PubMed] [Google Scholar]
- [44].McGinigle KL, Minc SD. Disparities in amputation in patients with peripheral arterial disease. Surgery 2021;169:1290–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Harris JK, Beatty K, Leider JP, et al. The double disparity facing rural local health departments. Annu Rev Public Health 2016;37:167–84. [DOI] [PubMed] [Google Scholar]
- [46].Peacock JM, Keo HH, Duval S, et al. The incidence and health economic burden of ischemic amputation in Minnesota, 2005–2008. Prev Chronic Dis 2011;8(6):A141. [PMC free article] [PubMed] [Google Scholar]
- [47].National Diabetes Statistics Report. Estimates of Diabetes and its Burden in the United StatesUS Department of Health and Human Services. Centers for Disease Control and Prevention; 2014. Published 2014. Accessed August 7, 2018 https://www.cdc.gov/diabetes/data/statistics/statistics-report.html.
- [48].Interactive Atlas of Heart Disease and Stroke Centers for Disease Control and Prevention; 2018. Accessed November 6 https://nccd.cdc.gov/DHDSPAtlas/Default.aspx?state=WV.
- [49].State Tobacco Activities Tracking and Evaluation (STATE) system. Centers for Disease Control and Prevention. Published 2018. Accessed June 9, 2020 https://nccd.cdc.gov/STATESystem/rdPage.aspx?rdReport=OSH_STATE.Highlights&rdRequestForwarding=Form.
- [50].Marshall J, Thomas L, Lane N, et al. Health Disparities in Appalachia. PDA Inc; August 2017. [Google Scholar]
- [51].Sanders LJ, Robbins JM, Edmonds ME. History of the team approach to amputation prevention: pioneers and milestones. J Vasc Surg 2010;52(3) 3S–16S, suppl. [DOI] [PubMed] [Google Scholar]
- [52].Khan T, Shin L, Woelfel S, et al. Building a scalable diabetic limb preservation program: four steps to success. Diabet Foot Ankle 2018;9(1):1452513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Patout CA Jr, Birke JA, Horswell R, et al. Effectiveness of a comprehensive diabetes lower-extremity amputation program in a predominantly low-income African-American Population. Diabetes Care 2000;23:1339–42. [DOI] [PubMed] [Google Scholar]
- [54].Rith-Najarian S, Branchaud C, Beaulieu O, et al. Reducing lower-extremity amputations due to diabetes. Application of the staged diabetes management approach in a primary care setting. J Fam Pract 1998;47:127–32. [PubMed] [Google Scholar]
- [55].Driver VR, Madsen J, Goodman RA. Reducing amputation rates in patients with diabetes at a military medical center: the limb preservation service model. Diabetes Care 2005;28:248–53. [DOI] [PubMed] [Google Scholar]
- [56].Chou AF, Homco JB, Nagykaldi Z, et al. Disseminating, implementing, and evaluating patient-centered outcomes to improve cardiovascular care using a stepped-wedge design: healthy hearts for Oklahoma. Bmc Health Serv Res 2018;18(1):404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Mokdad AH, Ballestros K, Echko M, et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 2018;319:1444–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].US Census Bureau. Native American Population 2020 US Census Bureau; 2020. Published 2020Accessed February 17 http://worldpopulationreview.com/states/native-american-population/.
- [59].Conway D, Mykyta L. Decline in share of people without health insurance driven by increase in public coverage in 36 states. US Census Bureau 2022. Published Accessed November 23, 2022 https://www.census.gov/library/stories/2022/09/uninsured-rate-declined-in-28-states.html. [Google Scholar]
- [60].Scorecard on State Health System Performance The Commonwealth Fund; 2022. Published 2019. Accessed October 18 https://www.commonwealthfund.org/publications/scorecard/2019/jun/2019-scorecard-state-health-system-performance-deaths-suicide.
- [61].Harding JL, Andes LJ, Rolka DB, et al. National and state-level trends in nontraumatic lower-extremity amputation among U.S. Medicare beneficiaries with diabetes, 2000–2017. Diabetes Care 2020;43:2453–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Institut National de santé Publique de Québec. Portrait du diabète dans la population québécoise âgée d’un an et plus de 2001 à 2019–2022.
- [63].Kayssi A, de Mestral C, Forbes TL, et al. A Canadian population-based description of the indications for lower-extremity amputations and outcomes. Can J Surg 2016;59:99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Olin A Map of Houston Area’s Distressed and Prosperous ZIP Codes Shows Ongoing and Growing Inequality. Rice University; 2022. Published 2020Accessed October 18 https://kinder.rice.edu/urbanedge/map-houston-areas-distressed-and-prosperous-zip-codes-shows-ongoing-and-growing#:~:text=The%20ZIP%20code%20is%2071.2%25%20white.%20At%20%2427%2C500%2C,which%20is%20twice%20that%20of%20whites%20or%20Blacks. [Google Scholar]
- [65].West JF. To fight bad suga’, or diabetes, my neighborhood needs more health educators. Health Aff (Millwood) 2013;32:184–7. [DOI] [PubMed] [Google Scholar]
- [66].McCloskey J Promotores as partners in a community-based diabetes intervention program targeting Hispanics. Fam Community Health 2009;32:48–57. [DOI] [PubMed] [Google Scholar]
- [67].Hofer R, Choi H, Mase R, et al. Mediators and moderators of improvements in medication adherence. Health Educ Behav 2017;44:285–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Wang CJ, Fetzer SJ, Yang YC, et al. The impacts of using community health volunteers to coach medication safety behaviors among rural elders with chronic illnesses. Geriatr Nurs 2013;34:138–45. [DOI] [PubMed] [Google Scholar]
- [69].Berge JM, Mendenhall TJ, Doherty WJ. Using community-based participatory research (CBPR) to target health disparities in families. Fam Relat 2009;58:475–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Wilson MG, Lavis JN, Travers R, et al. Community-based knowledge transfer and exchange: helping community-based organizations link research to action. Implement Sci 2010;5:33. [DOI] [PMC free article] [PubMed] [Google Scholar]


