Abstract
Clinical practice guidelines (CPGs) provide recommendations to clinicians based on current medical knowledge to guide and reduce variability in clinical care. With advances in nutrition science research, CPGs increasingly include dietary guidance; however, the degree of consistency in dietary recommendations across CPGs has not been investigated. Using a systematic review approach adapted for meta-epidemiologic research, this study compared dietary guidance from current guidelines developed by governments, major medical professional societies, and large health stakeholder associations owing to their often well-defined and standardized processes for guideline development. CPGs making recommendations for dietary patterns and food groups or components for generally healthy adults or those with prespecified chronic diseases were eligible. Literature from January 2010 to January 2022 was searched in 5 bibliographic databases and augmented by searches in point-of-care resource databases and relevant websites. Reporting followed an adapted PRISMA statement and included narrative synthesis and summary tables. Seventy-eight CPGs for major chronic conditions (autoimmune, 7; cancers, 5; cardiovascular-related, 35; digestive, 11; diabetes, 12; weight-related, 4; or multiple, 3) and general health promotion (n = 1) were included. Nearly, all (91%) made dietary pattern recommendations, and approximately half (49%) endorsed patterns centered on plant foods. Overall, CPGs were most closely aligned in promoting consumption of major plant food groups (vegetables = 74% of CPGs, fruit = 69%, whole grains = 58%), whereas discouraging intake of alcohol (62%) and salt or sodium (56%). CVD and diabetes CPGs were similarly aligned with additional messaging to consume legumes/pulses (60% of CVD CPGs; 75%, diabetes), nuts and seeds (67%, CVD), and low-fat dairy (60%, CVD). Diabetes guidelines discouraged sweets/added sugars (67%) and sweetened beverages (58%). This alignment across CPGs should boost clinician confidence in relaying such dietary guidance to patients in accordance with their relevant CPGs.
This trial was registered at the International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/prospero; PROSPERO 2021) as CRD42021226281.
Keywords: practice guideline, best practice, point-of-care systems, diet, healthy diet, health promotion, chronic disease, systematic review, meta-epidemiological
Statement of Significance.
This is the first study, to our knowledge, to compare dietary recommendations across current clinical practice guidelines for multiple major chronic diseases that are of concern globally. The results show that guidelines aimed at preventing, managing, or treating major chronic diseases are closely aligned in their recommendations for daily intake of plant sources of food with limited consumption of alcohol and salt or sodium; thus, clinicians should feel confident making these recommendations in accordance with their respective practice guidelines.
Introduction
A suboptimal diet is responsible for more deaths globally than any other risk factors, such as tobacco smoking. According to a 2019 systematic analysis of dietary risks in 195 countries, more than half of these diet-related deaths were attributed to nonoptimal intake of whole grains, fruit, and sodium [1]. Conversely, in the United States, high-quality diets are associated with a significantly lower risk of all-cause mortality and major chronic diseases [2]. Owing to the known importance of diet adequacy and quality, many countries have outlined dietary guidance for general health promotion in food-based dietary guidelines (FBDGs), such as the Dietary Guidelines for Americans (DGA) [3]. Recent evidence suggests that these national FBDGs are globally aligned in much of their guidance [4]. Such consistent messaging can promote greater confidence in, and compliance with, guideline recommendations. This is valuable because adherence to FBDGs has been associated with desirable outcomes in multiple domains such as a better quality of life [5,6] and mental health [7], healthy weight maintenance, and lower risk of major chronic diseases [for example, CVD, type 2 diabetes (T2D), multiple cancers [2,[8], [9], [10]]] and all-cause mortality [2,9,11].
National FBDGs provide dietary recommendations to prevent malnutrition and promote health [12], and they are typically aimed at broad, generally healthy populations. By contrast, clinical practice guidelines (CPGs) are prescriptive documents that guide providers in clinical decision making [13], and they may or may not include dietary recommendations. Developed by government agencies, institutions, professional societies, governing boards, or expert panels, CPGs are based on the latest medical evidence, and their purpose is to optimize patient care and help reduce variability in the diagnosis, treatment, and management of specific clinical circumstances or conditions [14]. Aiming to increase the rigor and trustworthiness of CPGs, the Institute of Medicine of the National Academies (now the National Academy of Medicine) conducted a study of best methods for developing guidelines and published a set of standards in 2011 [14]. Because of their visibility and clout in clinical settings, many governments, major medical professional societies, and large health stakeholder associations now follow such rigorous and transparent methods when developing and updating their guidelines.
To improve patient health outcomes, dietary guidance is included among other lifestyle recommendations in many current CPGs [15,16]. The degree of consistency in dietary messaging across CPGs overall and within targeted areas is not yet known, but close alignment could enhance confidence in their dietary recommendations. Previously, patients have reported feeling confused by conflicting nutrition messaging [[17], [18], [19]], and physicians, whose counsel is often sought for dietary guidance [20], typically receive little to no nutrition education during medical schooling [21]. Therefore, investigating the alignment of dietary guidance among CPGs and elucidating dietary recommendations largely supported by these evidence-based documents could benefit both patients and clinicians those who guide and develop clinical care policies.
Objective and scope
The primary objective of this research was to conduct a meta-epidemiologic study [22] (with guidelines as the unit of analysis) to compare dietary recommendations from CPGs developed by governments, major medical professional societies, and large health stakeholder associations promoting general health or aiming to improve health for adults with prespecified chronic diseases (CVD, T2D, cancer, autoimmune diseases, chronic obstructive pulmonary disease, digestive diseases, and weight-related conditions). Related to this objective, it is the position of the American College of Lifestyle Medicine (ACLM) that an eating plan based predominantly on a variety of minimally processed vegetables, fruit, whole grains, legumes, nuts, and seeds is recommended for the treatment, reversal, and prevention of lifestyle-related chronic diseases [23], such as T2D [24]. Therefore, a secondary objective of this study is to assess alignment between dietary recommendations from global CPGs and the ACLM dietary position statement that was developed from evidence-based research and clinical expertise.
This report includes an assessment of dietary messaging consistency across CPGs overall and dietary recommendation summaries for populations with the aforementioned prespecified chronic diseases. Primary dietary outcomes of interest were dietary patterns, food groups, and food components, and secondary outcomes were macronutrient and micronutrient recommendations. This review included a summary of the quality of guideline development methodology and reporting by reviewed CPGs; however, we did not assess the evidence used to develop the CPGs, nor did we formally evaluate certain aspects of quality such as composition of guideline development groups or grading of evidence to support CPG recommendations.
Methods
This meta-epidemiologic study used a systematic review approach following the National Academy of Medicine’s Standards for Systematic Reviews [25]. However, a risk-of-bias assessment was not completed because bias was not pertinent to this review’s research question, as per the meta-epidemiologic study guidelines by Murad and Wang [22]. Results are reported according to the said guidelines [22], which include an adapted PRISMA statement [26]. Before data extraction, a study protocol was published on the International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/prospero; PROSPERO 2021 CRD42021226281).
Data sources and searches
In consultation with a research librarian, we developed a search strategy to identify the most recent release of all published major stakeholder guidance documents (CPGs, FBDGs, consensus statements, and position statements), which included diet or nutrition recommendations. Publications by individual authors or small organizations were ineligible. The search was implemented in Embase, CINAHL, and Ovid platform databases such as MEDLINE, Healthstar, and Global Health. The initial searches were restricted to publications dating from 1 January, 2010 to 18 November, 2020, and an updated search was conducted to include publications up to 18 January, 2022. The complete MEDLINE search strategy is included in Supplemental Data. To capture relevant gray literature, we performed a hand search for potentially relevant guidance documents from BMJ Best Practice, ClinicalKey, and DynaMed point-of-care resource databases, and we manually searched for guidance documents published on relevant stakeholder websites. The hand search was conducted for documents published from January 2010 through February 2022, and the latest versions of updated documents were sought up to 11 February, 2022. Duplicate citations were removed in EndNote and the online Rayyan application [27] before screening.
Study selection
Two independent investigators screened all titles and abstracts in Rayyan and assessed full-text articles for study eligibility criteria presented in Table 1. Disagreements between the investigators were resolved by consensus or team discussion. Guidance documents aimed at the general free-living adult population (age: ≥18 y) or free-living adults with the prespecified chronic diseases were eligible for consideration if they were available in English and included meaningful diet or nutrition recommendations. Meaningful recommendations specified individual foods, components, ingredients, food groups, or dietary patterns. Guidance documents making vague recommendations (for example, “healthy diet” without description) or focused on supplements, enteral or parenteral nutrition, or micronutrients or macronutrients without the aforementioned meaningful recommendations were excluded.
TABLE 1.
Eligibility criteria for guidance documents included in this meta-epidemiologic study
| Category | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Study design | Any guidance documents with nutrition recommendations1
|
Any clinical study or case study Letters to the editor Protocols Background reading Any reviews:
|
| Date of publication | January 2010–February 2022 | Before 2010 |
| Publication status | Articles published in peer-reviewed journals Guidance documents published on websites of major medical professional societies, governments, or large health stakeholder associations |
Articles not published in peer-reviewed journals or on websites of major medical professional societies, governments, or large health stakeholder associations |
| Authors/publishers | Major medical professional societies Governments Large health stakeholder associations |
Individual authors Small or niche organizations |
| Language of publication | English language | Non-English languages |
| Country | No restriction | NA |
| Population | Free-living humans | Non–free-living humans (for example, residential care) Animals |
| Age of study participants | Adults (18+ y) | Infants/young children (0–3 y) Children/adolescents (>3 to <18 y) |
| Health status of population | Generally healthy (document focus is on general health promotion) Chronic diseases or specific health conditions limited to the following:
|
Pregnant or lactating women Illness other than the specified chronic diseases Other health conditions (for example, sepsis) Accident victims |
| Intervention or exposure | Guidance or recommendations (for example, increase, decrease, exclude, or include specific quantities) for the following:
|
No real guidance or recommendation for diet Only talks about micronutrients (for example, sodium and fiber) without any mention of the inclusion criteria Only talks about macronutrients without any mention of the inclusion criteria Only talks about supplements or enteral/parenteral nutrition Primary focus is nutrients only (even if specific foods are mentioned) |
Only the clinical practice guidelines found eligible for this meta-epidemiological study are within the scope of this report.
We identified numerous eligible guidance documents of a diverse nature, so this report addressed only the CPGs included in our meta-epidemiologic study (from here on, referred to as CPGs or guidelines). These were documents specified as practice guidelines in titles or author descriptions and/or documents using prescriptive language to guide practitioners in patient care decisions. Consensus statements, position statements, and FBDGs, which do not use prescriptive language, are outside the scope of this report so are listed among excluded publications.
Data extraction
We developed standardized data extraction forms for CPG characteristics, dietary recommendations, and quality of methodology and reporting. All data were extracted by 1 investigator and checked by a second. Disagreements between the investigators were resolved by consensus, a third investigator, or team discussion.
Data extracted for characteristics included country or region of development, author/publisher name and type (major medical professional society, large health stakeholder association, or government), primary aim of the guideline, and target population (based on age group, health status, and specific condition or disease). Data were extracted for dietary guidance that specified dietary patterns (for example, Mediterranean and calorie-restricted), food groups (for example, vegetables and dairy), and food components (for example, fruit juice and added sugar). Recommendations for specific macronutrients and micronutrients were also noted. Recommended items not clearly fitting into predefined categories were discussed in group meetings, and appropriate definitions and categories were determined by consensus. For example, recommendations for “refined carbohydrates” were interpreted by the group to mean refined grains. “Spreads” or “spread fats” were interpreted as solid fats and were included with the “butter or other animal fats” food components. “White meat” was included with the “lean meat” food group, and “simple sugars” were included with the food component, “added sugars.”
Guideline quality
We adapted relevant portions of the Appraisal of Guidelines for Research & Evaluation Instrument (AGREE II) [28] to extract data on methodologic and reporting quality in the reviewed CPGs. These included whether the guideline was an original or update; methods for gathering supporting evidence (for example, systematic review); methods for establishing recommendations (for example, formal or informal consensus); whether supporting evidence was clearly presented and connected with recommendations; source(s) of funding and role of funder(s) in guideline development; and whether the conflicts of interest of the guideline committee members were disclosed and mitigated. When guideline development methods were not clearly reported, we searched related publications and websites of guideline publishers and sponsors for these details.
Data synthesis and analysis
Individual CPG characteristics have been narratively synthesized and presented in tables. Summary tables and figures are also presented to highlight commonalities and differences among dietary recommendations from the reviewed guidelines and to elucidate methodologic and reporting quality. Where possible, figures organize the results by health conditions to facilitate subgroup comparisons.
Recommendations for dietary patterns were categorized by name (for example, the American Heart Association diet) or description (for example, low-sodium). For food group and component recommendations, we interpreted the original language in each guideline and categorized recommendations as “include/increase” or “exclude/decrease/limit.” Recommendations advocating “moderate” consumption were categorized as include/increase, whereas language indicating “low” or “low-to-moderate” intake were categorized as exclude/decrease/limit. When guidelines only mentioned serving sizes without descriptive language, serving sizes presented with symbols indicating limitations (< or ≤) were categorized as exclude/decrease/limit, whereas all others (>, ≥, or exact servings, for example, 1–2 cups/d or 2 oz/d) were categorized as include/increase. Specific nutrient recommendations were not the primary focus of this review, but macronutrient and micronutrient recommendations were tallied to identify nutrients of interest or concern. Summary statistics were calculated using the Microsoft Excel for Microsoft 365 MSO (version 2202 Build 16.0.14931.20128; 64-bit).
Results
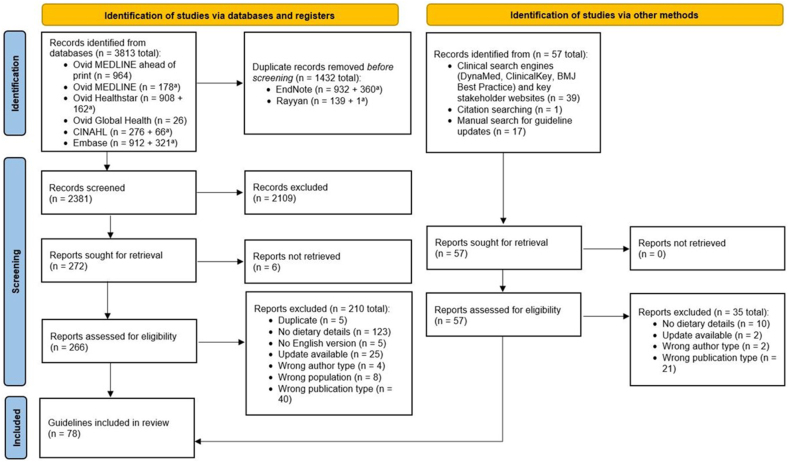
The initial and updated database searches identified 2381 unique publications, and other searches identified 57 additional unique publications. After initial screening excluded 2109 publications, 323 full-text reports were found and assessed for eligibility. Of these, 78 CPGs were included in this review, and their characteristics are presented in Supplemental Table 1. The search strategy and selection process are presented in Figure 1, and Supplemental Table 2 lists the excluded full-text guidelines with exclusion reasons.
FIGURE 1.
PRISMA flowchart of search strategy and selection process. aResults from the updated search. BMJ Best Practice; CINAHL Database.
Guideline characteristics
The characteristics of the 78 CPGs included in this meta-epidemiologic study are summarized in Table 2. The included CPGs were published between 2010 and 2021 (77% published after 2014). The guidelines were mostly written for countries in North America (41%), Europe (29%), and Asia (18%), but 4 CPGs (5%) were written for multicontinent or global populations. Figure 2 presents a map of the represented countries. Most of the guidelines (83%) came from major medical professional societies, with 12% coming from governments and 5% from large health stakeholder associations. This review focused on guidelines written for adults, which included those aged ≥18 y (64% of the included guidelines) and seniors aged ≥55 y (4%). Guidelines written for adults and children or adolescents (32%) were also included, but only the recommendations specific to adults or individuals of any age were considered for this study.
TABLE 2.
Summary of characteristics for 78 included clinical practice guidelines
| Characteristics | Guidelines (n) | % |
|---|---|---|
| Year published | ||
| 2021 | 8 | 10 |
| 2020 | 10 | 13 |
| 2019 | 10 | 13 |
| 2018 | 14 | 18 |
| 2017 | 7 | 9 |
| 2016 | 4 | 5 |
| 2015 | 7 | 9 |
| 2014 | 7 | 9 |
| 2013 | 3 | 4 |
| 2012 | 5 | 6 |
| 2011 | 0 | 0 |
| 2010 | 3 | 4 |
| Study location | ||
| Africa | 1 | 1 |
| Asia | 17 | 22 |
| Europe | 23 | 29 |
| North America | 32 | 41 |
| South America | 1 | 1 |
| International | 4 | 5 |
| Authors/publishers type | ||
| Government | 9 | 12 |
| Large health stakeholder association | 4 | 5 |
| Major medical professional society | 65 | 83 |
| Target age group | ||
| Adults (18+ y) | 50 | 64 |
| Mixed age group (adults and children/adolescents) | 25 | 32 |
| Seniors only (55+ y) | 3 | 4 |
| Target health status1 | ||
| Autoimmune diseases | 7 | 9 |
| Cancer, any type | 6 | 8 |
| CVD or related | 38 | 49 |
| Diabetes, type 2 | 15 | 19 |
| Digestive | 11 | 14 |
| General health promotion | 1 | 1 |
| Weight | 5 | 6 |
Three guidelines targeted diseases from multiple categories, so the total percentage for this section is >100%. See Table 1 for specific health conditions included in each disease category.
FIGURE 2.
Location of the target populations for 78 included clinical practice guidelines.
Guidelines for general health promotion or the prespecified major chronic diseases were eligible, but only 1 CPG (1%) for general health—particularly for individuals aged older than 65 y [29]—met the inclusion criteria. No eligible guidelines addressed chronic obstructive pulmonary disease. Nearly half of the included guidelines (49%) focused on the prevention, management, or treatment of CVD or related conditions (for example, hypertension). Other preidentified conditions of interest were T2D (a focus of 19% of included CPGs), digestive diseases (14%) such as irritable bowel syndrome (IBS), autoimmune diseases (9%) such as celiac disease and inflammatory bowel disease (IBD), cancers of any kind (8%), and weight-related conditions (6%) such as overweight, obesity, or weight loss. Although many CPGs offered guidance on multiple related health conditions, such as weight loss in a population with CVD, the aims of these CPGs were clearly focused on a single condition; however, 3 included CPGs (4%) covered >1 major chronic disease [[30], [31], [32]].
Guideline quality
To identify CPGs with the greatest likelihood of sound and transparent methodologies, this meta-epidemiologic study solely reviewed guidelines developed by governments, major medical professional societies, and large health stakeholder associations. Therefore, risk of bias in the development of the guidelines was not a primary focus of this study so was not assessed. Despite this, methodologic and reporting quality was not assumed to be high among the guidelines, so key features of quality deemed relevant by the investigators were assessed using criteria adapted from the AGREE II [28] appraisal tool for guidelines, as presented in Table 3.
TABLE 3.
A summary of financial support and conflicts of interest reported by 78 included clinical practice guidelines
| Category | Guidelines (n) | % |
|---|---|---|
| Status of guideline and update process | ||
| Original, and no mention of future update | 10 | 13 |
| Original, but plans to update in future | 7 | 9 |
| Update and describes update process | 24 | 31 |
| Update and no description of update process | 25 | 32 |
| Unclear | 12 | 15 |
| How was evidence gathered to support recommendations? | ||
| Systematic review—comprehensive (for example, 2+ databases, hand search, experts consulted) | 39 | 50 |
| Systematic review—not comprehensive or not clear (for example, 1 database, no hand search, no experts consulted) | 17 | 22 |
| Informal review (for example, hand search only or insufficient detail) | 8 | 10 |
| Not described | 14 | 18 |
| What methods were used to form recommendations? | ||
| Formal consensus (for example, Delphi method, Glaser techniques) | 15 | 19 |
| Informal consensus or not clear (for example, standard method not mentioned) | 24 | 31 |
| Voting system | 14 | 18 |
| Not described | 25 | 32 |
| Does the guideline clearly present supporting evidence for nutrition recommendations? | ||
| No | 13 | 17 |
| Yes | 65 | 83 |
| Was a funding source named or no funding declared? | ||
| No | 31 | 40 |
| Yes | 47 | 60 |
| Does the guideline state that the views of the funding body have not influenced the content of the guideline? | ||
| No, but funding source was not reported | 31 | 40 |
| No | 29 | 37 |
| Yes | 10 | 13 |
| Not applicable (no funding) | 8 | 10 |
| Were competing interests of guideline development group members disclosed? | ||
| No | 11 | 14 |
| Yes | 67 | 86 |
| Was an attempt made to reduce the effect of competing interests? (for example, excluding certain members from developing guidelines) | ||
| No (disclosed but not mitigated) | 18 | 23 |
| Yes | 21 | 27 |
| Unclear (not addressed) | 39 | 50 |
Overall, the 78 reviewed CPGs provided a high degree of transparency in reporting guideline development processes. Of the 8 criteria reviewed, 76% of the CPGs provided details on ≥6 criteria, whereas 8% of the CPGs provided details on 2 or fewer criteria. Only 2 CPGs included no description of the guideline development process [33,34]. The CPGs commonly lacked a clear statement that views of the funding body had not influenced the guideline content (77% not reporting), where 40% of the CPGs provided no statement at all about funding or support. Although most CPGs (86%) clearly reported competing interests, half gave no details regarding whether or how attempts were made to reduce the effect of competing interests in guideline development.
Other results indicated that 22% of the included guidelines were original documents, 63% were updates to previous guidelines, and the original/update status was unclear for the remaining 15%. Including both original guidelines and updates, 40% reported plans for future updating. Evidence for recommendations in the guidelines was gathered using various methods, but most (72%) conducted some form of systematic reviews. The processes used to form recommendations from gathered evidence also varied, but one-third of the guidelines (32%) failed to report sufficient details for this criterion. CPGs specifying methods reported formal consensus through Delphi [35] or Glaser-like [36] techniques (19%), informal consensus (that is, no mention of specific or recognized techniques, or insufficient detail; 31%), or a voting system (18%). Most included guidelines (83%) clearly presented descriptive supporting evidence (not just citations) for recommendations.
Overall dietary recommendations
The primary aim of this meta-epidemiologic study was to compare CPG recommendations for overall dietary patterns, major food groups, and prespecified food components commonly addressed in nutrition science research and clinical settings. A secondary aim was to identify the number of guidelines making recommendations for macronutrients (carbohydrates, protein, and lipids), related nutrients (for example, fiber and FAs), energy, and micronutrients (for example, specific vitamins). Overall results for these primary and secondary aims are described further under separate headings for dietary patterns, food groups, food components, and nutrients. An additional section summarizes the primary aim results by specific health outcomes.
Dietary patterns
Nearly all included CPGs (91%) recommended a specific dietary pattern, and 33 dietary patterns were specified altogether (Table 4). These included popular or commercial diets (for example, Ornish and Zone); diets associated with national guidelines (for example, DGA and Nordic Diet) or association guidelines (for example, American Heart Association and European Association for the Study of Diabetes Guidelines); and diets defined by intended outcomes (for example, heart-healthy and therapeutic lifestyle changes diet), specific food characteristics [for example, low-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), gluten-free, plant-based], or nutrients (for example, low-sodium, high-fiber, lipid monitoring). The most frequently recommended dietary patterns were Mediterranean (33% of guidelines), Dietary Approaches to Stop Hypertension (DASH; 26%), and a “healthy diet” (24%) or similarly named pattern (for example, balanced diet, healthful eating plan, and healthy eating pattern). The definitions of Mediterranean-style and DASH diets varied somewhat, but 1 guideline summarized Mediterranean diets as being rich in vegetables, whole grains, and olive oil and DASH diets as rich in fruit, vegetables, and low-fat dairy, whereas being low in saturated fat, total fat, cholesterol, red meat, salt, sweets, and sugar-containing beverages [37]. Guidelines that specifically named healthy diets as a dietary pattern (not just describing a healthy diet) were included in this category. These guidelines defined healthy diets using different approaches such as naming specific foods or food groups [38,39], specifying nutrients of interest or concern [40,41], or by emphasizing calorie balance and/or nutrient intake to maintain optimal weight [34,42]. Another 5 dietary patterns recommended by 10%–15% of the included guidelines were low-fat or lipid monitoring (14%), low-sodium (13%), high-fiber (12%), plant-based (12%), and vegetarian diets (10%). Although 38% of the guidelines recommended a single dietary pattern, 53% recommended multiple dietary patterns.
TABLE 4.
A summary of dietary pattern recommendations from 78 included clinical practice guidelines1
| Recommended dietary patterns | Guidelines (n) | % |
|---|---|---|
| American College of Cardiology or AHA | 5 | 6 |
| Alternative Healthy Eating Index | 1 | 1 |
| DASH | 20 | 26 |
| European Association for the Study of Diabetes Guidelines | 1 | 1 |
| Fasting | 1 | 1 |
| Gluten-free | 5 | 6 |
| Healthy diet2 | 19 | 24 |
| Heart-healthy or cardioprotective | 3 | 4 |
| High-carbohydrate | 1 | 1 |
| High-fiber | 9 | 12 |
| High-potassium | 1 | 1 |
| High-protein | 3 | 4 |
| Japan diet | 1 | 1 |
| Low-FODMAP | 6 | 8 |
| Low-GI or GL | 5 | 6 |
| Low-CHO or CHO monitoring | 5 | 6 |
| Low-cholesterol | 3 | 4 |
| Low-fat or lipid monitoring | 11 | 14 |
| Low-saturated fat | 4 | 5 |
| Low-sodium | 10 | 13 |
| Lyon | 1 | 1 |
| Mediterranean | 26 | 33 |
| No named dietary patterns | 7 | 9 |
| Nordic | 2 | 3 |
| Ornish | 1 | 1 |
| Plant-based | 9 | 12 |
| Portfolio | 3 | 4 |
| Reduced-calorie | 7 | 9 |
| Therapeutic lifestyle changes diet | 2 | 3 |
| USDA or Dietary Guidelines for Americans food pattern | 3 | 4 |
| Vegan | 3 | 4 |
| Vegetarian | 8 | 10 |
| Volumetric | 1 | 1 |
| Zone | 1 | 1 |
FODMAP, fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
Forty-one guidelines recommended multiple dietary patterns, so the percentage column total is >100%.
The healthy diet category was assigned only to guidelines recommending a healthy diet by name (for example, healthy diet, balanced diet, healthful eating plan, and healthy eating pattern). Guidelines describing only the contents of what might be interpreted as a healthy diet were categorized according to any specified dietary pattern or as “no named dietary pattern.”
Food groups
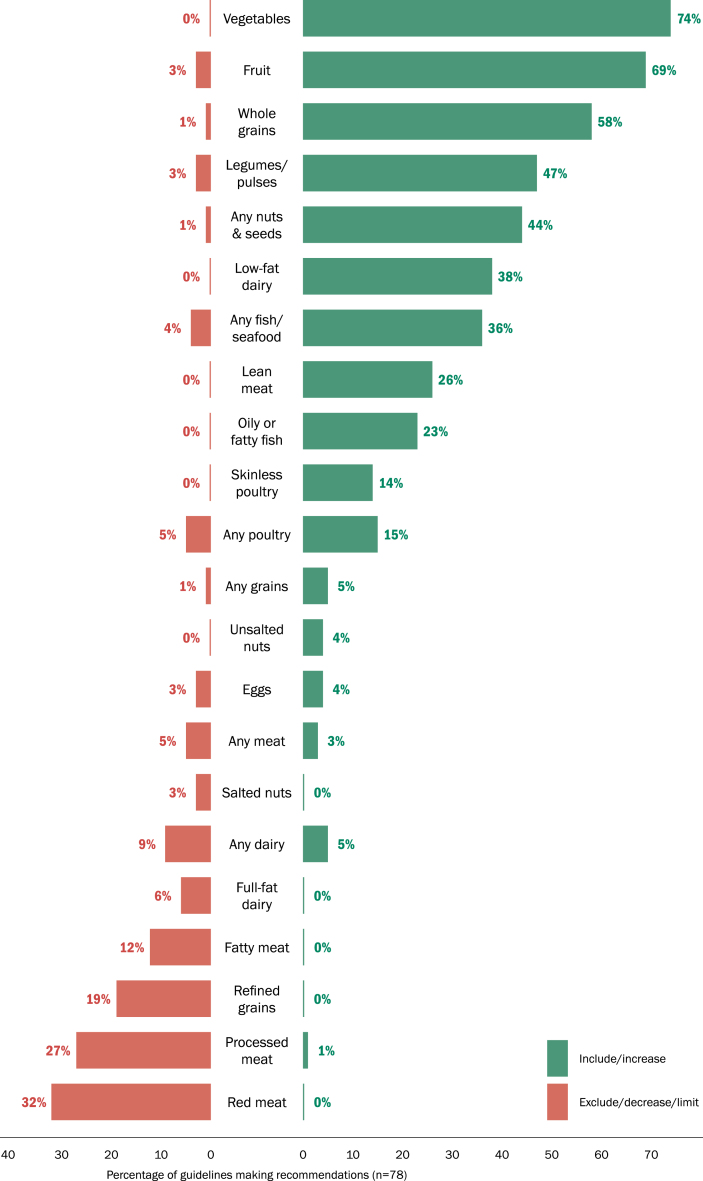
Of the 78 included CPGs, most (83%) made food group recommendations, and these were categorized in this study as recommendations to include/increase (that is, encouraged intake) or exclude/decrease/limit (that is, discouraged intake). Fifteen food groups were prespecified for the analysis as follows: all meat, red meat and pork, poultry, fish/seafood, processed meat, eggs, any dairy, low-fat dairy, full-fat dairy, fruit and vegetables, legumes/pulses, any grains, whole grains, refined grains, and nuts and seeds. “Other” food groups or food group–related items were also captured, and for those “other” recommendations made by multiple guidelines, additional food group categories were formed post hoc. These new food groups included lean meat, fatty meat, skinless poultry, oily or fatty fish, unsalted nuts, and salted nuts. Because some of these categories were related to prespecified categories, we revised the prespecified food groups as all meat, fish/seafood, and nuts and seeds, to “any meat,” “any fish/seafood,” and “any nuts and seeds” (all unspecified). In addition, no guidelines specified pork in recommendations, so the red meat and pork category was later reduced to the red meat category. Figure 3 presents the results for food group recommendations made by the included CPGs.
FIGURE 3.
Food group recommendations made by the included clinical practice guidelines.
More than half of the reviewed CPGs encouraged intake of 3 food groups: vegetables (74% of CPGs), fruit (69%), and whole grains (58%). More than 20% of the CPGs also encouraged intake of legumes/pulses (47%), any nuts and seeds (44%), low-fat dairy (38%), any fish/seafood (36%), lean meat (26%), and oily or fatty fish (23%). However, for some of these same food groups, between 1% and 5% (n = 1–4) of the included CPGs discouraged intake. In particular, 3 guidelines for populations with CVD and 1 guideline for overweight/obesity recommended low-to-moderate intake of dairy, fish, and poultry [33,43] (one of these stipulated fish intake ≥2 times/wk [33]) or specified ≤2 servings/d [44] or <6 oz/d [45] of meat, poultry, and fish. Two guidelines for Japanese populations with diabetes (type 1 and/or type 2) recommended fruit intake be limited to ≤1 unit of fructose (fruit) [38] or 1 unit (80 kcal)/d, given that fruits currently on markets often contain a large amount of sugar because of selective breeding [46]. Three guidelines for populations with IBS recommended a low-FODMAP dietary pattern. These guidelines discouraged consumption of insoluble fiber from sources such as beans, nuts, and grains [47] or whole grains [48], and they discouraged intake of foods with high oligosaccharide content (for example, legumes, chickpeas, and lentils [49]). None of the reviewed CPGs explicitly recommended to include/increase intake of fatty meat, red meat, full-fat dairy, refined grains, or salted nuts.
Although few of the reviewed CPGs made explicit recommendations to exclude/decrease/limit any food groups, >20% recommended excluding red meat (32%) and processed meat (27%). Intake of 2 other food groups was discouraged by >10% of reviewed CPGs, and these were refined grains (19%) and fatty meat (for example, high-fat meats, fatty cuts of meat, meat fat, or organ meats; 12%). None of the reviewed CPGs explicitly discouraged intake of lean meat, skinless poultry, oily or fatty fish, low-fat dairy, vegetables, or unsalted nuts.
Some food groups had mixed recommendations with the percentage of CPGs encouraging or discouraging intake differing ≤5%. These included any dairy (5% encouraged; 9% discouraged), eggs (4% encouraged; 3% discouraged), any meat (3% encouraged; 5% discouraged), and any grains (5% encouraged; 1% discouraged, for populations with IBS [47]).
Food components
As with food groups, 83% of the reviewed CPGs included ≥1 food component (or item) recommendation, which we categorized as include/increase or exclude/decrease/limit based on the language or serving sizes presented in the CPGs (see Food groups section for examples). The prespecified food components of interest were any beverages, fruit juice, sugar-sweetened beverages (SSBs), alcohol, water, processed foods (for example, chips, pastries, and fast food), added sugar, vegetable oils, butter and other animal fats, and salt. Other food components were also captured, and any other components mentioned by multiple guidelines were added to data extraction forms post hoc. These were soy protein or products, sweets (including products with added sugar), tropical vegetable/plant oils, and wine or red wine. Because some of these other components were related to the prespecified categories, the prespecified categories were adjusted as follows: sweets and added sugars (including products with added sugar) were combined into a single category, and the vegetable oil category was changed to vegetable/plant oils (nontropical). In addition, the salt category was later combined with recommendations for sodium because recommendations about salt typically referred to sodium in the diet. The results for the food component recommendations are presented in Figure 4.
FIGURE 4.
Food component recommendations made by the included clinical practice guidelines.
Recommendations encouraging intake of food components were scarce, but 2 components were mentioned by >10% of the reviewed CPGs. Intake of vegetable/plant oils (in general or as specified) was encouraged by 35% of the guidelines, with many specifying types of oils such as olive (17%), canola (3%), or nontropical vegetable/plant oils (4%). Another 5% specified to avoid or limit tropical plant oils (for example, palm oil and coconut oil). Intake of soy protein or soy products (for example, tofu and edamame) was encouraged by 18% of the reviewed CPGs.
Guidelines widely discouraged intake of multiple food components. More than half discouraged alcohol (62%) and salt or sodium (56%) intake, and more than one-third discouraged SSBs (36%) and sweets or added sugar (36%). Two other commonly discouraged food components were processed foods (19%) and butter and other animal fats (18%).
Beyond alcohol and SSBs, few CPGs made recommendations for beverages. Although water consumption was encouraged by 6% of the CPGs and discouraged by none, the opposite was true for caffeine (0% encouraged; 6% discouraged). Two other categories with mixed recommendations were fruit juice (4% encouraged; 6% discouraged) and wine or red wine (3% encouraged; 3% discouraged).
Nutrients
Nearly all reviewed CPGs mentioned ≥1 macronutrient (91%) in their dietary or nutrition recommendations, where the most (78%) mentioned lipids, and more than half mentioned carbohydrates (59%) or protein (54%). Four guidelines (5%; 1 each for CVD [50], diabetes [39], obesity [37], and cancer [51]) recommended limiting or minimizing intake of refined carbohydrates. Intake of protein from plant or vegetable sources was encouraged by the 18% of CPGs, whereas recommendations for animal sources of protein were mixed (5% encouraged; 4% discouraged). Five CPGs for populations with celiac disease [[52], [53], [54], [55], [56]] recommended complete avoidance of gluten, but gluten was not mentioned by any other CPG.
Macronutrient components mentioned in >20% recommendations included fiber (73% of the CPGs), SFAs (46%), dietary cholesterol (37%), unsaturated FAs (MUFA and/or PUFA; 29%), trans-fats (24%), and ω-3 FAs (23%). Other macronutrient components mentioned in recommendations were calories or energy, low-glycemic or high-GI carbohydrates, complex carbohydrates, soluble or insoluble fiber, and other FAs (for example, ω-6 FAs, ALA, EPA, and DHA). Of the 31 guidelines making recommendations for vegetable/plant oils (nontropical or tropical) and/or butter and other animal fats, 74% also addressed unsaturated, saturated, and/or trans-fats. Twenty of these guidelines (65%) encouraged intake, and 1 guideline (3%) discouraged intake, of nontropical vegetable/plant oils, which are high in unsaturated FAs. Conversely, 13 of these guidelines (42%) discouraged intake (none encouraged intake) of butter and other animal fats and/or tropical vegetable/plant oils, which are high in saturated FAs.
Dietary recommendations by health outcome
Most CPGs included in this meta-epidemiologic study (96%) focused on populations with conditions related to a single major health outcome of interest (general health promotion, autoimmune diseases, cancers, CVD, digestive conditions, T2D, and weight-related conditions), but 3 CPGs focused on 2 or more chronic diseases (Supplemental Table 1) [[30], [31], [32]]. To identify commonalities among dietary recommendations for specific populations, results from the CPGs aimed at single health outcomes (n = 75) are summarized below and in Supplemental Figures 1 and 2.
Cardiovascular disease and related conditions
Thirty-five CPGs were focused on populations with CVD and/or related conditions such as acute MI, atherosclerotic CVD, acute coronary syndrome, CAD, chronic heart failure, stroke, transient ischemic attack, stable ischemic heart disease, dyslipidemia, hypercholesterolemia, and arterial hypertension. Of these 35 CPGs, 66% recommended multiple dietary patterns to support the health of individuals with cardiovascular conditions, and 4 specific dietary patterns were mentioned by >25% of the CPGs. These were Mediterranean (46% of these CPGs), DASH (43%), low-sodium (26%), and healthy (26%) dietary patterns. There was strong consensus among these CPGs regarding food groups to include or increase in the diet (Supplemental Figure 3). Most guidelines encouraged intake of fruit (89% of the CPGs), vegetables (89%), whole grains (80%), any nuts and seeds (66%), legumes/pulses (60%), and low-fat dairy (60%). Intake of any fish/seafood was encouraged by 49% of these CPGs, whereas 40% recommended intake of oily or fatty fish specifically. As with the overall study findings, few CPGs discouraged intake of any food groups, but those most frequently discouraged were red meat (37%), processed meat (31% of these CPGs), refined grains (23%), and fatty meat (20%). There was also strong consensus around limiting or excluding intake of alcohol (83% of these CPGs) and salt or sodium (80%) and other discouraged food components were SSBs (43%), sweets or added sugar (43%), butter and other animal fats (29%), and processed foods (29%) (Supplemental Figure 4). Nearly half (46%) recommended vegetable or plant oils be included/increased in the diet, and 26% encouraged intake of soy protein or soy products.
Type 2 diabetes
A total of 12 CPGs focused on populations with diabetes, such that all 12 addressed populations with T2D, and 8 also addressed those with type 1 diabetes. Two of the CPGs were directed at diabetes management in chronic kidney disease or kidney transplant patients, and 2 offered guidelines for individuals with prediabetes. All 12 of these CPGs recommended ≥1 dietary pattern, and 50% recommended >1 pattern to support the health of individuals with diabetes. Dietary patterns that were recommended by ≥25% of these CPGs were healthy (42%), Mediterranean (42%), DASH (25%), and plant-based diet (25%). Similar to the aforementioned reporting, there was strong consensus to include/increase intake of vegetables (92%), and at least half also encouraged intake of legumes/pulses (75%), fruit (67%), whole grains (67%), any fish/seafood (50%), and any nuts and seeds (50%). The most commonly discouraged food groups were processed meat (42%), red meat (25%), and refined grains (25%) (Supplemental Figure 5). Food components encouraged by ≥2 of these CPGs were vegetable/plant oils (33%) and soy protein or soy products (17%) (Supplemental Figure 6). Unsurprisingly, most CPGs discouraged populations with diabetes from consuming salt or sodium (83%), sweets or added sugar (67%), alcohol (58%), and SSBs (58%). One quarter of the CPGs also discouraged intake of processed foods (25%) (Supplemental Figure 5).
Digestive conditions
Altogether, 11 of the CPGs included in this study were written for populations with digestive conditions including chronic constipation (n = 2), chronic gastritis (n = 1), colonic diverticular disease (n = 1), diarrhea in cancer patients (n = 1), or IBS (n = 6). These CPGs made much less extensive dietary recommendations than the CPGs focused on CVD and diabetes. Only these 4 dietary patterns were recommended to support digestive health: low-FODMAP (45%; all were CPGs for IBS), high fiber (36%), healthy (18%; n = 2), and vegetarian (9%; n = 1). Six of the CPGs (55%) made food group recommendations, and just 3 food groups were mentioned by >1 CPG. These included fruit (27% encouraged), vegetables (27% encouraged), and legumes/pulses (9% encouraged; 18% discouraged, for populations with IBS [47,49]). Similarly, few food component recommendations were made for those with digestive conditions. Food components mentioned by >1 CPG were alcohol (27% discouraged), water (18% encouraged), and salt or sodium (9% allowed; 9% discouraged).
Autoimmune diseases
Seven CPGs addressed populations with autoimmune conditions. Five CPGs were aimed at populations with celiac disease and recommended gluten-free dietary patterns, where 1 additionally recommended high-fiber diets. One CPG addressing IBD, Crohn disease, and ulcerative colitis recommended a low-FODMAP diet and specified a high-protein diet for those with active IBD or Crohn disease. The remaining CPG addressed populations with IBD and recommended diets rich in fruit, vegetables, and ω-3 FAs, and low in ω-6 FAs. Just 3 food groups and no food components were mentioned by >1 of these CPGs. Recommendations were to include/increase vegetables (57% of the CPGs), fruit (43%), and whole grains (29%).
Cancers
Five CPGs addressed populations with cancer (any cancer, n = 1; colorectal cancer, n = 2; lung cancer, n = 1), or cancer survivors (n = 1). Dietary patterns recommended by these CPGs included a low-fat diet (n = 1), a low-carbohydrate diet (n = 1), and the USDA MyPlate recommendations (n = 1). The 2 other CPGs did not specify dietary patterns, but 1 recommended diets rich in fruit and nonstarchy vegetables and low in red and processed meat, whereas the other recommended diets high in vegetables, fruit, and whole grains and low in saturated fats, red meats, and alcohol. Three of these CPGs (60%) encouraged intake of fruit, vegetables, and whole grains, whereas 2 of these same CPGs (40%) encouraged intake of any poultry and any fish/seafood. All 5 CPGs discouraged intake of red meat, and 4 (80%) discouraged intake of processed meat for populations with colorectal or lung cancer and cancer survivors. Food components mentioned by >1 CPG were alcohol (60% discouraged) and SSBs (40% discouraged).
Weight
Four CPGs focused on populations with overweight and/or obesity. Each recommended multiple dietary patterns including Mediterranean-style (100% of these CPGs), low-carbohydrate (75%), reduced-calorie (75%), DASH (50%), high-protein (50%), and vegetarian diets (50%), among others (each recommended by just 1 CPG). Food groups encouraged by >1 CPG were fruit (75% of these CPGs), low-fat dairy (75%), vegetables (75%), lean meat (50%), and legumes/pulses (50%). Intake of red meat and refined grains was discouraged by 2 (50%) of these CPGs. No food components were encouraged by >1 CPG, but 3 CPGs (75%) discouraged intake of alcohol, SSBs, and sweets or added sugar, whereas 2 (50%) discouraged intake of salt or sodium.
General health promotion
The only eligible CPG for general health promotion was directed at older people in Finland [29]. It recommended a balanced diet aligned with the DGA and Nordic Nutritional Recommendations with <10% of energy from SFAs and 20%–30% of energy from MUFAs and PUFAs.
Discussion
Summary of findings
Clinicians rely on practice guidelines to provide evidence-based recommendations from the most current and rigorous medical research. Such guidelines help steer and support clinicians’ diagnoses, management, and treatment of medical conditions, and following these guidelines can help reduce variability in optimizing patient care. The field of lifestyle medicine emphasizes nutrition as foundational to treatment. Therefore, identifying commonalities among guidelines’ dietary recommendations can support diet as an important lifestyle treatment component and can bolster clinicians’ confidence in executing the dietary guidance.
To this end, we systematically reviewed and compared dietary recommendations of current CPGs from major medical professional societies, large health stakeholder associations, and governments across the globe to illuminate recurrent and divergent themes. The reviewed guidelines primarily focused on major chronic diseases with only 1 guideline aimed at general health promotion in older adults. Guidelines on CVD, diabetes, and various digestive conditions were most prevalent with few guidelines focused on populations with cancers or weight-related conditions. Our informal quality assessment identified transparent reporting of guideline development processes and competing interests but less transparency for how competing interests were managed and how guideline development was funded. Guideline recommendations were primarily based on systematic reviews, and recommendation language was largely decided by consensus or voting processes. All but 13 CPGs clearly presented supporting evidence for dietary recommendations. From these findings, we feel confident that the reviewed CPG recommendations are generally trustworthy and sufficiently evidence based.
Dietary patterns were mentioned in nearly all reviewed guidelines, with more than half recommending multiple dietary patterns. Although this suggests different styles of eating may support positive health outcomes, half of the guidelines recommended dietary patterns known to be rich in unrefined plant foods and low in more refined and animal-based foods. These were Mediterranean, DASH, plant-based, vegetarian, and vegan dietary patterns. Overall, the guidelines were aligned on recommendations to consume vegetables and fruit and to limit intake of alcohol. Most guidelines supported intake of whole grains and limited salt or sodium, and many encouraged intake of legumes/pulses and any nuts and seeds. Recommendations for all other major food groups and components were more varied, but approximately one-third encouraged intake of low-fat dairy, fish/seafood, lean meats, and nontropical vegetable oils, whereas nearly one-third discouraged intake of red and processed meats, SSBs, and sweets or added sugars.
Trends in recommendations for specific chronic diseases varied somewhat from the overall recommendations. For instance, similar to the overall trends, 50% or more of the guidelines on CVD and diabetes encouraged intake of vegetables, fruit, and whole grains; however, most of these guidelines further promoted legumes/pulses, and approximately half encouraged intake of any nuts/seeds and any fish/seafood. Although the guidelines for CVD and diabetes were aligned in recommending limited intake of alcohol and salt/sodium, CVD guidelines more often encouraged low-fat dairy intake, whereas most diabetes guidelines emphasized limited intake of sweets or added sugars and SSBs.
The importance of consistent messaging across CPGs becomes clear in the context of typical US dietary intakes. On an average, American adults consume fewer vegetables, fruits, whole grains, and legumes than the DGA standards [3]. Suboptimal and low-quality dietary intakes play a key role in developing chronic diseases highlighted in the reviewed guidelines [1,2]. Thus, it is essential that consistent messaging around healthy eating be at the forefront of medical treatment, as performed in the field of lifestyle medicine.
Comparisons with existing literature
Similar to our findings, a recent global review of 90 FBDGs found a high level of consistency in recommendations to consume abundant fruit and vegetables, to include legumes in the diet, and to limit sugar and salt [4]. The FBDG review also reported that one-third of the guidelines recommended lean meat or meat with fat removed, 27% supported fish consumption, and 23% recommended limiting or moderating meat consumption. In contrast to this study, the review of FBDGs reported high consistency in recommendations to include starchy staples (mentioned in just 2 CPGs in our review) and animal-sourced foods (as 1 of the 4 or 5 recommended food groups) but to avoid excessive intake of fats/oils (as indicated by small proportions on food guide graphics such as food pyramids). In this study, 78% of the reviewed guidelines mentioned fat in their recommendations, but only 14% recommended a low-fat dietary pattern. One-third of our reviewed guidelines promoted intake of nontropical vegetable oils rich in unsaturated fats, whereas nearly 20% discouraged intake of butter and other animal fats or tropical plant oils, which are all high in SFAs. Similar to our review, the FBDG review found recommendations for dairy, red meat, fats and oils, and nuts were more variable across guidelines and were often unclear as to whether these foods should be included with moderation or limited in the diet.
Differences between our findings and the global review of FBDGs could be due to several factors, but the primary difference is likely target population. National FBDGs are aimed at the general population and/or healthy members of the general population, and FBDGs target general health promotion and prevention of disease. CPGs are typically aimed at populations with specific medical conditions and can address diagnosis, management, and treatment of disease in addition to general health promotion and disease prevention. This source of discrepant recommendations is clear even within our review where guidelines targeting different chronic diseases emphasized different dietary patterns, food groups, and food components. Furthermore, with the rapid advancement of nutrition science over recent decades, evidence-based recommendations for dietary practices can become outdated if not regularly updated. Although both types of guidance documents generally include plans for updating, national FBDGs are often updated every 5 or 10 y, whereas some CPGs are updated annually or as soon as new meaningful evidence emerges. Accordingly, the global FBDG review included all FAO repository guidelines that spanned from 1986 to 2017; however, our review included the most recently revised CPGs published in peer-reviewed journals or stakeholder websites since 2010. Of the 78 guidelines we reviewed, 54% were updated or original guidelines published in the last 5 y (since 2017), thus representing more recent scientific evidence. The FBDG study reviewed relevant information provided in English on the FAO site by 90 countries [4]. Our review included only guidelines published in English, resulting in representation from 18 individual countries (mostly in North America or Europe) plus regional guidelines for Asian, Australian, European, or global populations. Finally, national FBDGs for general populations are expected to vary between countries owing to differences in agriculture, culture, economics, and food production [57]. CPGs targeting specific medical conditions (that is, more restricted populations) may be less subject to these differences. However, some guidelines in our review clearly pointed to cultural and regional considerations in their recommendations. As noted previously, 1 diabetes guideline from Japan recommended limited intake of fruit owing to higher sugar content from selective breeding [46], and another Japanese guideline for CVD prevention recommended a low-salt Japanese dietary pattern (that is, lean meats, reduced butter and other animal fats, and consumption of soy, fish, vegetables, seaweed, mushrooms, fruit, and unpolished grains) [58].
Despite these differences, both global FBDGs and CPGs for adults with major chronic diseases reviewed in this study show clear consensus support for consuming fruit, vegetables, legumes/pulses, and whole grains while limiting intake of salt or sodium.
Implications
The public discourse around nutrition is increasingly noisy and confusing as various experts and pseudo-experts populate the internet with information of varying quality [19]. In the United States, the rising prevalence of overweight/obesity and associated chronic conditions constitute a growing public health threat, and the need to address these conditions is urgent [59]. Many patients have nutrition questions related to these conditions, and they look to their medical providers for guidance [20]. However, the dissemination of public health recommendations on diet as part of medical treatment can be hampered by providers’ lack of familiarity with nutrition guidelines or lack of confidence in delivering nutrition advice in patient encounters [21]. This large meta-epidemiologic study captured dietary recommendations from the most current versions of CPGs published in the last decade. By comparing and summarizing dietary recommendations made for general health promotion or the prevention, management, and/or treatment of major chronic diseases in adults, the results from this study can inform many clinician–patient discussions involving nutrition and can increase clinician confidence in making evidence-based and consensus supported recommendations related to patient health outcomes.
Although the bulk of CPGs included in this study were from North America and Europe, the inclusion of guidelines from various countries and regions around the globe increases the generalizability of our findings, which suggest clear consensus that fruit, vegetables, and whole grains are essential dietary components supporting human health, whereas intake of alcohol and salt or sodium should be limited. These findings support both the ACLM’s dietary position statement [23] and its recent expert consensus statement that the most effective dietary intervention for achieving T2D remission is whole, plant-based foods with minimal consumption of meat and other animal products [60]. Conversely, findings from this study did not support popular trends such as low-carbohydrate, high-protein, Paleo, or ketogenic diets, which may emphasize intake of animal-sourced foods but restricting whole grains, beans, and/or fruit. Research on these diets is still emerging, but current evidence suggests these extreme macronutrient diets may propagate divergence from dietary reference intakes [61] and dietary guidelines [62] and may increase cardiovascular disease risk factors [[63], [64], [65]]. Therefore, clinicians should practice caution when communicating with patients interested in adopting these or other dietary patterns inconsistent with most recommendations for chronic disease. As the practice of lifestyle medicine continues to grow, the use of food as medicine will play an increasingly important role in medical practice and treatment of chronic disease [66], and clinicians should feel confident in recommending dietary changes aligned with those consistently found across guidelines.
Strengths and limitations
Despite implementing a broad search for relevant guidelines, only 1 CPG aimed at general health promotion, and few CPGs directed at weight-related conditions (n = 4), cancers (n = 5), and autoimmune diseases (n = 7) were eligible for inclusion. However, the inclusion of 35 guidelines for CVD and related conditions, in addition to >10 guidelines for populations with diabetes and digestive conditions, strengthens confidence in the consistency of dietary recommendations made by CPGs for these chronic diseases. Furthermore, nearly all eligible CPGs were from high-income and upper middle–income countries, so the findings from this review have limited implications for low-income and lower middle–income countries.
A major limitation of this study was the lack of detailed dietary recommendations among many included guidelines. This was unsurprising because few included guidelines were written expressly to address patients’ dietary or nutritional needs. Although several guidelines offered clear descriptions of dietary patterns, some mentioned only the name of a pattern without further details. Serving sizes and frequency of intake were also rarely outlined in food group or component recommendations, thus quantity or proportion of these items encouraged in the diet was not always clear. With these limitations, this study focused on summarizing recommended content rather than quantities of intake. Comparing recommendations across guidelines with inconsistent details also necessitated a simplified approach to categorize intake as positive (include/increase) or negative (exclude/decrease/limit). For health outcomes with substantial evidence supporting clear connections to dietary intake (for example, hypertension and sodium intake), a more nuanced summary of recommendations would prove valuable (for example, excluding salt altogether compared with limiting intake to specific quantities). For clinicians or patients with such needs, we encourage readers to seek out the individual guidelines related to their specific health concerns.
In conclusion, this meta-epidemiologic study compared dietary and nutrition recommendations from CPGs published by global professional organizations for the promotion of health and the reduction of chronic diseases in patient populations. Most guidelines had strong methodology and reporting, but some lacked clarity on management of competing interests, funding, and supporting evidence for dietary recommendations. To improve rigor and further increase the trustworthiness of CPG recommendations, future guideline developers should follow published standards for methodology and reporting [14]. The reviewed guidelines aimed at preventing, managing, or treating major chronic diseases were closely aligned in their dietary recommendations for daily intake of plant sources of food (especially fruit, vegetables, and whole grains), with limited consumption of alcohol and salt or sodium. Based on the current evidence, clinicians should feel confident making these recommendations in accordance with their respective practice guidelines. Guidelines for chronic disease prevention and health promotion may become more aligned on specific dietary patterns and food groups as the growing evidence base further elucidates their effect on human health. The identification of consensus among guidelines can provide clarity for health care practitioners and policymakers.
Acknowledgments
We thank Research & Instruction Librarian, Amy LaVertu, for assisting with the search strategy and Kara Staffier for assisting with manuscript preparation.
The authors’ responsibilities were as follows: DMG, MCK, and MDT: conceived the research; KCC and MCK: designed the research; KCC, MCK, BKK, and SSA: analyzed and interpreted the data; KCC, DMG, and MCK: drafted the manuscript; and all authors: collected data and critically revised, read, and approved the final version of the manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.advnut.2023.03.007.
Funding
This project was supported by the American College of Lifestyle Medicine (ACLM). ACLM staff were involved in the design, analysis, and interpretation of data.
Author disclosures
MCK, MDT, and KCC were supported by the American College of Lifestyle Medicine (ACLM). DMG has received funding for consulting services from Game Changers Institute, TrueNorth Health Foundation, Wellness Foundry, Trail Butter, and the ACLM. All other authors report no conflicts of interest within the 5 y before publication.
Data availability
The MEDLINE search strategy and a table of characteristics of included studies has been made available in the Supplementary Data. Search strategies for additional databases can be obtained by contacting the corresponding author Dr. Micaela Karlsen.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Afshin A., Sur P.J., Fay K.A., Cornaby L., Ferrara G., Salama J.S., et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwingshackl L., Bogensberger B., Hoffmann G. Diet quality as assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: an updated systematic review and meta-analysis of cohort studies. J. Acad. Nutr. Diet. 2018;118(1):74–100.e11. doi: 10.1016/j.jand.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Agriculture . 9th Edition. Dietary guidelines for Americans; 2020. U.S. Department of Health and Human Services. 2020-2025. USDA/DHHS. [Google Scholar]
- 4.Herforth A., Arimond M., Álvarez-Sánchez C., Coates J., Christianson K., Muehlhoff E. A global review of food-based dietary guidelines. Adv. Nutr. 2019;10(4):590–605. doi: 10.1093/advances/nmy130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Govindaraju T., Sahle B.W., McCaffrey T.A., McNeil J.J., Owen A.J. Dietary patterns and quality of life in older adults: a systematic review. Nutrients. 2018;10(8):971. doi: 10.3390/nu10080971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evers I., Heerings M., de Roos N.M., Jongen P.J., Visser L.H. Adherence to dietary guidelines is associated with better physical and mental quality of life: results from a cross-sectional survey among 728 Dutch MS patients. Nutr. Neurosci. 2022;25(8):1633–1640. doi: 10.1080/1028415X.2021.1885240. [DOI] [PubMed] [Google Scholar]
- 7.Lassale C., Batty G.D., Baghdadli A., Jacka F., Sánchez-Villegas A., Kivimäki M., et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol. Psychiatry. 2019;24(7):965–986. doi: 10.1038/s41380-018-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen S.H., Overvad K., Hansen C.P., Dahm C.C. Adherence to national food-based dietary guidelines and incidence of stroke: a cohort study of Danish men and women. PLOS ONE. 2018;13(10) doi: 10.1371/journal.pone.0206242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voortman T., Kiefte-de Jong J.C., Ikram M.A., Stricker B.H., van Rooij F.J.A., Lahousse L., et al. Adherence to the 2015 Dutch dietary guidelines and risk of non-communicable diseases and mortality in the Rotterdam Study. Eur. J. Epidemiol. 2017;32(11):993–1005. doi: 10.1007/s10654-017-0295-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kohler L.N., Garcia D.O., Harris R.B., Oren E., Roe D.J., Jacobs E.T. Adherence to diet and physical activity cancer prevention guidelines and cancer outcomes: a systematic review. Cancer Epidemiol. Biomarkers Prev. 2016;25(7):1018–1028. doi: 10.1158/1055-9965.Epi-16-0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ewers B., Marott J.L., Schnohr P., Nordestgaard B.G., Marckmann P. Non-adherence to established dietary guidelines associated with increased mortality: the Copenhagen General Population Study. Eur. J. Prev. Cardiol. 2021;28(11):1259–1268. doi: 10.1177/2047487320937491. [DOI] [PubMed] [Google Scholar]
- 12.Cámara M., Giner R.M., González-Fandos E., López-García E., Mañes J., Portillo M.P., et al. Food-based dietary guidelines around the world: a comparative analysis to update AESAN scientific committee dietary recommendations. Nutrients. 2021;13(9) doi: 10.3390/nu13093131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenfeld R.M., Nnacheta L.C., Corrigan M.D. Clinical consensus statement development manual, Otolaryngol. Head Neck Surg. 2015;153(Suppl 2):S1–S14. doi: 10.1177/0194599815601394. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine . The National Academies Press; Washington, DC: 2011. Clinical practice guidelines we can trust. [Google Scholar]
- 15.Rock C.L., Thomson C., Gansler T., Gapstur S.M., McCullough M.L., Patel A.V., et al. American Cancer Society guideline for diet and physical activity for cancer prevention, CA Cancer. J. Clin. 2020;70(4):245–271. doi: 10.3322/caac.21591. [DOI] [PubMed] [Google Scholar]
- 16.American Diabetes Association, 5 Lifestyle management: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Suppl 1):S46–S60. doi: 10.2337/dc19-S005. [DOI] [PubMed] [Google Scholar]
- 17.Vijaykumar S., McNeill A., Simpson J. Associations between conflicting nutrition information, nutrition confusion and backlash among consumers in the UK. Public Health Nutr. 2021;24(5):914–923. doi: 10.1017/s1368980021000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark D., Nagler R.H., Niederdeppe J. Confusion and nutritional backlash from news media exposure to contradictory information about carbohydrates and dietary fats. Public Health Nutr. 2019;22(18):3336–3348. doi: 10.1017/s1368980019002866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spiteri Cornish L., Moraes C. The impact of consumer confusion on nutrition literacy and subsequent dietary behavior. Psychol. Market. 2015;32(5):558–574. doi: 10.1002/mar.20800. [DOI] [Google Scholar]
- 20.Adams K.M., Kohlmeier M., Powell M., Zeisel S.H. Nutrition in medicine: nutrition education for medical students and residents. Nutr. Clin. Pract. 2010;25(5):471–480. doi: 10.1177/0884533610379606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crowley J., Ball L., Hiddink G.J. Nutrition in medical education: a systematic review. Lancet Planet. Health. 2019;3(9):e379–e389. doi: 10.1016/S2542-5196(19)30171-8. [DOI] [PubMed] [Google Scholar]
- 22.Murad M.H., Wang Z. Guidelines for reporting meta-epidemiological methodology research. Evid. Based Med. 2017;22(4):139–142. doi: 10.1136/ebmed-2017-110713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American College of Lifestyle Medicine announces dietary lifestyle position statement for treatment and potential reversal of disease. PRWeb; 2018. https://www.prweb.com/releases/american_college_of_lifestyle_medicine_announces_dietary_lifestyle_position_statement_for_treatment_and_potential_reversal_of_disease/prweb15786205.htm [Internet] [September 25, 2018, April 6, 2023]. Available from: [September 25, 2018, April 6, 2023]. Available from: [Google Scholar]
- 24.Kelly J., Karlsen M., Steinke G. Type 2 diabetes remission and lifestyle medicine: a position statement from the American College of Lifestyle Medicine. Am. J. Lifestyle Med. 2020;14(4):406–419. doi: 10.1177/1559827620930962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Institute of Medicine (US) National Academies Press; Washington, DC: 2011. Committee on Standards for Systematic Reviews of Comparative Effectiveness Research, Finding what works in health care: standards for systematic reviews. [PubMed] [Google Scholar]
- 26.Moher D., Liberati A., Tetzlaff J., Altman D.G. PRISMA Group, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoffmann-Eßer W., Siering U., Neugebauer E.A., Brockhaus A.C., Lampert U., Eikermann M. Guideline appraisal with AGREE II: systematic review of the current evidence on how users handle the 2 overall assessments. PLOS ONE. 2017;12(3) doi: 10.1371/journal.pone.0174831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suominen M.H., Jyvakorpi S.K., Pitkala K.H., Finne-Soveri H., Hakala P., Mannisto S., et al. Nutritional guidelines for older people in Finland. J. Nutr. Health Aging. 2014;18(10):861–867. doi: 10.1007/s12603-014-0509-1. [DOI] [PubMed] [Google Scholar]
- 30.Grundy S.M., Stone N.J., Bailey A.L., Beam C., Birtcher K.K., Blumenthal R.S., et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082–e1143. doi: 10.1161/CIR.0000000000000625. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cosentino F., Grant P.J., Aboyans V., Bailey C.J., Ceriello A., Delgado V., et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD) Eur. Heart J. 2020;41(2):255–323. doi: 10.1093/eurheartj/ehz486. 2019. [DOI] [PubMed] [Google Scholar]
- 32.Wolfram G., Bechthold A., Boeing H., Ellinger S., Hauner H., Kroke A., et al. Evidence-based guideline of the German Nutrition Society: fat intake and prevention of selected nutrition-related diseases. Ann. Nutr. Metab. 2015;67(3):141–204. doi: 10.1159/000437243. [DOI] [PubMed] [Google Scholar]
- 33.El-Deeb M.H., Sulaiman K.J., Al-Riyami A.A., Mohsin N., Al-Mukhaini M., Al-Lamki M., et al. Oman Heart Association guidelines for the management of hypertension: practical recommendations from the Oman Heart Association (OHA), High Blood Press. Cardiovasc. Prev. 2015;22(1):83–97. doi: 10.1007/s40292-014-0074-z. 2015. [DOI] [PubMed] [Google Scholar]
- 34.Špinar J., Vítovec J., Hradec J., Málek I., Meluzín J., Špinarová L., et al. Czech Society of Cardiology guidelines for the diagnosis and treatment of chronic heart failure 2011, Cor. Vasa. 2012;54(2):E113–E134. [Google Scholar]
- 35.Barrett D., Heale R. What are Delphi studies? Evid. Based Nurs. 2020;23(3):68–69. doi: 10.1136/ebnurs-2020-103303. [DOI] [PubMed] [Google Scholar]
- 36.Fink A., Kosecoff J., Chassin M., Brook R.H. Consensus methods: characteristics and guidelines for use. Am. J. Public Health. 1984;74(9):979–983. doi: 10.2105/ajph.74.9.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garvey W.T., Mechanick J.I., Brett E.M., Garber A.J., Hurley D.L., Jastreboff A.M., et al. Reviewers of the AACEOCPG. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr. Pract. 2016;22(Suppl 3):1–203. doi: 10.4158/EP161365.GL. [DOI] [PubMed] [Google Scholar]
- 38.Araki E., Goto A., Kondo T., Noda M., Noto H., Origasa H., et al. Japanese clinical practice guideline for diabetes 2019. Diabetol. Int. 2020;11(3):165–223. doi: 10.1007/s13340-020-00439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Boer I.H., Caramori M.L., Chan J.C.N., Heerspink H.J.L., Hurst C., Khunti K., et al. KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;98(4):S1–S115. doi: 10.1016/j.kint.2020.06.019. [DOI] [PubMed] [Google Scholar]
- 40.Mach F., Baigent C., Catapano A.L., Koskinas K.C., Casula M., Badimon L., et al. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020;41(1):111–188. doi: 10.1093/eurheartj/ehz455. 2019. [DOI] [PubMed] [Google Scholar]
- 41.Hua Q., Fan L., Li J. Joint Committee for Guideline Revision. 2019 Chinese guideline for the management of hypertension in the elderly. J. Geriatr. Cardiol. 2019;16(2):67–99. doi: 10.11909/j.issn.1671-5411.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MacLeod J., Franz M.J., Handu D., Gradwell E., Brown C., Evert A., et al. Academy of Nutrition and Dietetics nutrition practice guideline for type 1 and type 2 diabetes in adults: nutrition intervention evidence reviews and recommendations. J. Acad. Nutr. Diet. 2017;117(10):1637–1658. doi: 10.1016/j.jand.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 43.The Management of Adult Overweight and Obesity Work Group . Department of Veterans Affairs and Department of Defense; 2020. VA/DoD clinical practice guideline for the management of adult overweight and obesity; pp. 1–147. [Google Scholar]
- 44.Ibrahim M.M. The Egyptian hypertension society: Egyptian hypertension guidelines, Egypt. Heart J. 2014;66(2):79–132. [Google Scholar]
- 45.Rabi D.M., McBrien K.A., Sapir-Pichhadze R., Nakhla M., Ahmed S.B., Dumanski S.M., et al. Hypertension Canada’s 2020 Comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can. J. Cardiol. 2020;36(5):596–624. doi: 10.1016/j.cjca.2020.02.086. [DOI] [PubMed] [Google Scholar]
- 46.Tajima N., Noda M., Origasa H., Noto H., Yabe D., Fujita Y., et al. Evidence-based practice guideline for the treatment for diabetes in Japan 2013. Diabetol. Int. 2015;6(3):151–187. [Google Scholar]
- 47.Pietrzak A., Skrzydło-Radomańska B., Mulak A., Lipiński M., Małecka-Panas E., Reguła J., et al. Guidelines on the management of irritable bowel syndrome: in memory of Professor Witold Bartnik. Prz. Gastroenterol. 2018;13(4):259–288. doi: 10.5114/pg.2018.78343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lacy B.E., Pimentel M., Brenner D.M., Chey W.D., Keefer L.A., Long M.D., et al. ACG clinical guideline: management of irritable bowel syndrome. Am. J. Gastroenterol. 2021;116(1):17–44. doi: 10.14309/ajg.0000000000001036. [DOI] [PubMed] [Google Scholar]
- 49.Song K.H., Jung H.K., Kim H.J., Koo H.S., Kwon Y.H., Shin H.D., et al. Clinical practice guidelines for irritable bowel syndrome in Korea, 2017 revised edition. J. Neurogastroenterol. Motil. 2018;24(2):197–215. doi: 10.5056/jnm17145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arnett D.K., Blumenthal R.S., Albert M.A., Buroker A.B., Goldberger Z.D., Hahn E.J., et al. ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019;74(10):e177–e232. doi: 10.1016/j.jacc.2019.03.010. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leong K., Hartley J., Karandikar S. Association of Coloproctology of Great Britain & Ireland (ACPGBI): guidelines for the management of cancer of the colon, rectum and anus (2017)—follow up, lifestyle and survivorship. Colorectal Dis. 2017;19(Suppl 1):67–70. doi: 10.1111/codi.13706. [DOI] [PubMed] [Google Scholar]
- 52.Al-Toma A., Volta U., Auricchio R., Castillejo G., Sanders D.S., Cellier C., et al. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. U. Eur. Gastroenterol. J. 2019;7(5):583–613. doi: 10.1177/2050640619844125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sood A., Ahuja V., Kedia S., Midha V., Mahajan R., Mehta V., et al. Diet and inflammatory bowel disease: the Asian Working Group guidelines. Indian J. Gastroenterol. 2019;38(3):220–246. doi: 10.1007/s12664-019-00976-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Remes-Troche J.M., Uscanga-Domínguez L.F., Aceves-Tavares R.G., Calderón de la Barca A.M., Carmona-Sánchez R.I., Cerda-Contreras E., et al. Clinical guidelines on the diagnosis and treatment of celiac disease in Mexico. Rev. Gastroenterol. Mex (Engl Ed). 2018;83(4):434–450. doi: 10.1016/j.rgmx.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 55.Bai J.C., Ciacci C. World Gastroenterology Organisation global guidelines: celiac disease February 2017. J. Clin. Gastroenterol. 2017;51(9):755–768. doi: 10.1097/mcg.0000000000000919. [DOI] [PubMed] [Google Scholar]
- 56.Ludvigsson J.F., Bai J.C., Biagi F., Card T.R., Ciacci C., Ciclitira P.J., et al. Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut. 2014;63(8):1210–1228. doi: 10.1136/gutjnl-2013-306578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dwyer J.T. In: Present knowledge in nutrition. Erdman J., Macdonald I., Zeisel S., editors. Elsevier; 2012. Dietary standards and guidelines: similarities and differences among countries; pp. 1110–1134. [Google Scholar]
- 58.Kinoshita M., Yokote K., Arai H., Iida M., Ishigaki Y., Ishibashi S., et al. Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases 2017. J. Atheroscler. Thromb. 2018;25(9):846–984. doi: 10.5551/jat.GL2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hales C.M., Carroll M.D., Fryar C.D., Ogden C.L. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1–8. [PubMed] [Google Scholar]
- 60.Rosenfeld R.M., Kelly J.H., Agarwal M., Aspry K., Barnett T., Davis B.C., et al. Dietary interventions to treat type 2 diabetes in adults with a goal of remission: an expert consensus statement from the American College of Lifestyle Medicine. Am. J. Lifestyle Med. 2022;16(3):342–362. doi: 10.1177/15598276221087624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karlsen M., Livingston K., Agoulnik D., Miki A., Lichtenstein A., Folta S., et al. Theoretical intakes of modern-day paleo diets: comparison to U.S. dietary reference intakes. Curr. Dev. Nutr. 2021;5(Suppl 2):420. doi: 10.1093/cdn/nzab038_032. [DOI] [Google Scholar]
- 62.Churuangsuk C., Lean M.E.J., Combet E. Carbohydrate knowledge, dietary guideline awareness, motivations and beliefs underlying low-carbohydrate dietary behaviours. Sci. Rep. 2020;10(1) doi: 10.1038/s41598-020-70905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dinu M., Pagliai G., Angelino D., Rosi A., Dall’Asta M., Bresciani L., et al. Effects of popular diets on anthropometric and cardiometabolic parameters: an umbrella review of meta-analyses of randomized controlled trials. Adv. Nutr. 2020;11(4):815–833. doi: 10.1093/advances/nmaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Freire R. Scientific evidence of diets for weight loss: different macronutrient composition, intermittent fasting, and popular diets. Nutrition. 2020;69 doi: 10.1016/j.nut.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 65.Elidottir A.S., Halldorsson T.I., Gunnarsdottir I., Ramel A. Dietary intake and cardiovascular risk factors in icelanders following voluntarily a low carbohydrate diet. PLOS ONE. 2016;11(8) doi: 10.1371/journal.pone.0156655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Witkamp R.F., van Norren K. Let thy food be thy medicine….when possible. Eur. J. Pharmacol. 2018;836:102–114. doi: 10.1016/j.ejphar.2018.06.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The MEDLINE search strategy and a table of characteristics of included studies has been made available in the Supplementary Data. Search strategies for additional databases can be obtained by contacting the corresponding author Dr. Micaela Karlsen.