Abstract
988, a national mental health emergency hotline number, went live throughout the United States in July 2022. 988 connects callers to the 988 Crisis & Suicide Lifeline, previously known as the National Suicide Prevention Lifeline. The transition to the three-digit number aimed to respond to a growing national mental health crisis and to expand access to crisis care. We examined preparedness throughout the U.S. for the transition to 988. In February and March 2022, we administered a national survey of state, regional, and county behavioral health program directors. Respondents (n = 180) represented jurisdictional coverage of 120 million Americans. We found that communities throughout the U.S. appeared ill-prepared for rollout of 988. Fewer than half of respondents reported their jurisdictions were ‘somewhat’ or ‘very’ prepared for 988 in terms of financing (29%), staffing (41%), infrastructure (41%), or service coordination (47%). Counties with higher representation of Hispanic/Latinx individuals were less likely to report being prepared for 988 in terms of staffing (OR: 0.62, 95 %CI: 0.45, 0.86) and infrastructure (OR: 0.68, 95 %CI: 0.48, 0.98). In terms of existing services, sixty percent of respondents reported a shortage of crisis beds and fewer than half reported availability of short-term crisis stabilization programs in their jurisdictions. Our study highlights components of local, regional, and state behavioral health systems in the U.S. that require greater investments to support 988 and mental health crisis care.
Keywords: 988, Hotline, Mental health, Behavioral health, Suicide, Crisis care
1. Introduction
In July 2022, a new crisis hotline number—988—went into effect throughout the United States. This three-digit number connects callers to an existing network of call centers at the 988 Suicide & Crisis Lifeline (Lifeline), previously known as the National Suicide Prevention Lifeline. (Vibrant Emotional Health, 2022) The transition from a lengthier 1–800 number to 988 was intended, in part, to address a rising epidemic of mental health emergencies. Suicide is now the second leading cause of death among adolescents and young adults in the U.S. (Nimh, 2022) One in every 10 visits to an emergency department is related to mental health. (Santillanes et al., 2020) 988 provides an opportunity to expand access to and reduce stigma surrounding crisis services.
988 is an important piece in a broader continuum of crisis care in which jurisdictions often struggle with capacity. Crisis services, according to national guidelines established by the Substance Abuse and Mental Health Services Administration (SAMHSA), should be timely, local, and supported by call centers that are staffed 24/7/365. (Samhsa, 2020) whether jurisdictions have adequate funding, staffing, and infrastructure to meet these goals remains an open question. Using data from a national survey we conducted ahead of the launch of 988, this study provides an overview of system preparedness for 988—as reported by behavioral health administrators who represent more than one-third of the U.S. population.
2. Methods
Between February 8 and March 18, 2022, we conducted a national survey of state, regional, and county behavioral health program directors on preparedness for 988. We contacted directors in every state and U.S. territory, as well as county and regional behavioral health directors for which we could find publicly available information (n = 690). Participants were invited to complete a confidential 21-item survey and offered a $10 gift card. Questions on preparedness corresponded to a four-point Likert scale: “not at all,” “a little bit,” “somewhat,” “very.” Other questions followed “yes,” “no,” “I don’t know” formatting.
We measured 988 preparedness with respect to four domains: strategic planning and financing, staffing, infrastructure, and service coordination. Planning and financing were intended to identify whether agencies had developed planning and budgeting targets as well as vehicles to finance the institutionalization of operations; staffing pertained to the training, configuration, and volume of personnel to field 988 calls and administrate operations; infrastructure pertained to development and maintenance of physical and organizational structures corresponding to 988; and service coordination pertained to harmonization of service providers to work effectively in executing 988-related activities. Without strong infrastructure, financing, staffing, and service coordination, jurisdictions are likely to be unprepared for 988. These four domains of preparedness, and measures within each, were selected based on a review of national guidelines chronicled by SAMHSA, CrisisNow, and the National Association of Mental Health Program Directors (NAMHPD). (SAMHSA, 2020, Crisis Services Task Force, 2016, National Association of State Mental Health Program Directors, 2021) The survey was reviewed by experts across academic and governmental organizations with relevant expertise in crisis hotlines. A full version of the survey can be found in the Appendix.
We also gathered county-level characteristics to identify potential correlates of 988 preparedness. These characteristics were selected based on literature linking sociodemographic and economic characteristics to mental health care and/or telehealth availability. (Hodgkinson et al., 2017, Colon-Rivera and Dixon, 2020, Cortelyou-Ward et al., 2020, Cummings et al., 2013) Specifically, we cataloged urbanicity, health provider professional area (HPSA) designation, median household income, and racial/ethnic composition from the Health Resources and Services Administration (Hrsa, 2020) and the U.S. Census Bureau. (Bureau UC, 2022) We defined urbanicity based on the 2010 Census Bureau’s urban-rural classification. We assessed counties’ racial/ethnic composition by percent of residents who are Black and Hispanic/Latinx.
We calculated one-way frequencies for each set of survey responses. We also conducted multivariable logistic regression analyses to examine county-level correlates of preparedness—one regression for each of the four domains. The dependent variable (“preparedness”) was coded as “1” if respondents endorsed they were “somewhat” or “very” prepared, and “0” if respondents endorsed “not at all” or “a little” prepared. Fixed effects were defined as county-level characteristics (i.e., urbanicity, HPSA designation, median household income, racial/ethnic composition), based on our a priori expectations in accordance with previous literature. Standard errors were clustered at the state level. All statistical analyses were conducted in Stata 17, using a standard two-sided alpha level of 0.05.
As a diagnostic function, we examined variance inflation factors (VIFs) for evidence of multicollinearity among independent variables. In no instance was VIF greater than or equal to 5, the typical threshold for potential multicollinearity. (Marcoulides and Raykov, 2019) We also examined potential for misspecification using Stata’s linktest. (Pregibon, 1980) For all four models, p < 0.10. Study procedures and protocols were approved by RAND’s Institutional Review Board.
3. Results
The survey was completed by 180 respondents, including 16 state directors and 134 county/regional directors. Thirty respondents did not report their title. Respondents represented approximately 120.1 million Americans.
Nearly all respondents (97%) felt that 988 preparedness was “somewhat” or “very” important. However, fewer than half reported being “somewhat” or “very” prepared in terms of financing, staffing, infrastructure, or service coordination (Fig. 1). A minority of all respondents indicated they had been involved in the development of a strategic plan (41%) or a budget (16%) for 988 support. Although all state directors’ agencies had a strategic plan, only half had a budget to support 988. 31% of county or regional agencies had a strategic plan and 6% had a budget.
Fig. 1.
Respondents’ self-reported preparedness in Feb-Mar 2022 for the rollout of 988. Legend. For responses to strategic planning and financing categories, individuals were first asked if they had a strategic plan or budget. If they responded ‘yes’, they were then asked about specific components of these.
With regard to strategic planning, a minority of respondents had a strategic plan with details on operating a 24/7 call center (34%), coordinating 988–911 (27%), or marketing 988 (24%) (Fig. 1). With regard to financing, only 12% of respondents had sufficient funding for 24/7 call center operations, and <9% reported sufficient funding for 988-related personnel, clinical services, or infrastructure.
Among those with a strategic plan (n = 73; data not shown), a majority indicated that details on a 24/7 call center (84%) and 988–911 coordination (67%) were included in the plan. Among those with a budget to support 988 (n = 29; data not shown), a majority (72%) reported sufficient funding for 24/7 call center operations, but fewer than half reported sufficient funding for 988-related personnel, clinical services, or infrastructure.
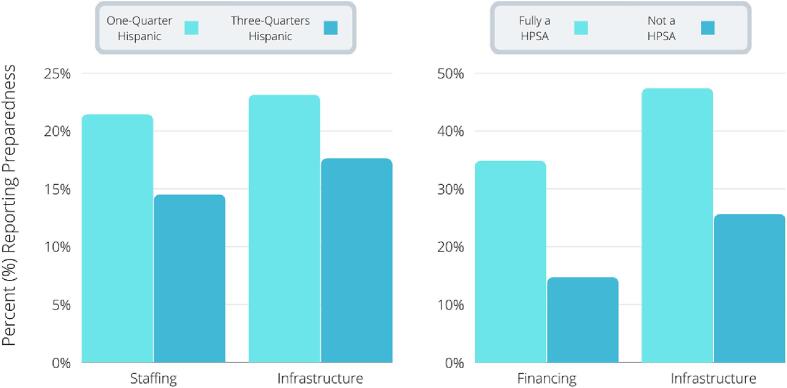
Multivariable regression analyses (full results displayed in online supplement) indicated counties with a larger share of Hispanic residents were less likely to endorse preparedness (i.e., indicate they were “somewhat” or “very” prepared) in terms of staffing or infrastructure. As shown in Fig. 2, counties that were three-quarters Hispanic would be expected to have a 32% lower probability of endorsing preparedness for financing 988 (15% vs. 21%) and 24% lower probability endorsing preparedness for infrastructure (18% vs. 23%), compared to counties that were only one-quarter Hispanic (p < 0.05). Conversely, counties designated as HPSAs were 85% more likely to endorse preparedness in terms infrastructure (47% vs. 26%) and more than twice as likely to endorse preparedness in terms of financing (35% vs. 15%), compared to those without the designation (p < 0.05).
Fig. 2.
County-level preparedness in Feb-Mar 2022 for the rollout of 988—by racial/ethnic composition and HPSA designation. Legend. Regression-adjusted values representing the probability that a respondent would endorse preparedness for 988 on a particular topic (staffing, infrastructure, financing) as a function of their county’s characteristics. “HPSA” stands for “mental health professional shortage area.”
In terms of existing hotline services (data not shown), most respondents had a call center operating prior to the launch of 988 (85%) that was available 24/7 (63%) and employed by paid rather than exclusively volunteer personnel (76%) who received standardized suicide intervention training (59%). However, fewer than half (48%) identified their jurisdictions’ hotline as part of the Lifeline network to which 988 calls are connected. We also found that fewer than half of these hotlines supported text (41%) or online chat (19%).
In terms of existing crisis care services (data not shown), sixty percent reported a shortage of crisis stabilization beds in their community. A minority of respondents’ jurisdictions had short-term crisis stabilization (48%), crisis residential treatment (26%), or mental health urgent care units (28%). Respondents also indicated their jurisdictions’ major entry points to crisis care. A majority reported an emergency department (93%), followed by an outpatient mental health clinic or community mental health center (77%) and a mobile crisis response team (59%).
4. Discussion
This survey, which gauged preparedness for 988 among 180 mental health program directors throughout the U.S., demonstrates that respondents appreciated the importance of 988; however, a preponderance felt they lacked the necessary resources to support its success. Our analysis at the county level indicated that communities with a larger share of Hispanic residents were considerably less likely to report preparedness in terms of staffing or infrastructure. This observation corresponds with prior research documenting lesser availability of community mental health facilities serving this demographic group. (Cummings et al., 2013) In contrast, counties designated as HPSAs reported being more prepared. While this may seem surprising, rural communities have more experience using telehealth as a mode of service delivery, to which 988 is akin.
Although 85% of respondents indicated the existence of a hotline in their jurisdiction, fewer than half confirmed these hotlines were part of the Lifeline network—to which 988 calls are connected. For individuals who dial 988 in counties with no local Lifeline call center, their calls are less likely to reach local responders who may have greater awareness of community-based services. Additionally, fewer than half of local hotlines appear to have text or chat components. With disproportionately high rates of suicide observed among adolescents and young adults, (Miron et al., 2019) digital interfaces like these are critical. Finally, sixty percent of respondents reported a shortage of crisis beds and fewer than half reported the availability of short-term crisis stabilization programs. With the expected increase in calls to the Lifeline compared to pre-988 levels (Vibrant Emotional Health, 2020) and the potential for increased demand in crisis services, this indicates a need for wider investment in the crisis care system as a whole.
COVID-19 relief funds and recent legislation have provided opportunities to expand crisis response in the U.S. For example, the 2020 Coronavirus Aid, Relief, and Economic Security (CARES) Act set aside $50 million for SAMHSA to spend on suicide prevention and an additional $100 million in flexible spending to address mental health challenges. (National Conference of State Legislatures, 2020) Whether this funding is enough to transform the mental health crisis system—and 988 in particular—is an open question. Strengthening crisis care will require ongoing investments, not just initial capital. Additional investments could include sustainable financing mechanisms such as local surcharges like those levied throughout the country to support 911. (National Emergency Number Association, 2021).
This study has limitations. Our survey response rate was in-line with similar types of services in the past; however, this rate of 26% implies our findings are limited to a self-selected sample that might differ from a random cross-section throughout the country. Nevertheless, our findings provide insights on jurisdictions representing more than one-third of the U.S. population, and we therefore perceive the findings as valuable in their own right. We also note that we were unable to validate the expertise of respondents beyond identifying their roles as directors and lead administrators of public behavioral health agencies. Lastly, the survey was conducted in February and March 2022, and it is conceivable that jurisdictions have made progress in preparations since this time.
5. Conclusions
For mental health crisis systems to flourish, evidence indicates that 988 will need to be integrated into a broader continuum of care. (Hogan and Goldman, 2021) This includes alternatives to emergency departments such as mental health urgent care centers, crisis residential treatment programs, and mobile crisis response teams. (Waters, 2021) Building up this infrastructure is likely to take time, implying that 988 and its impacts are likely to evolve over months and years. Policymakers and administrators should therefore continue to routinely gather information on preparedness and implementation—including the dimensions we assessed on planning, financing, infrastructure, and service coordination.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
This work was funded by the Sozosei Foundation (#01.2021.11.01). The funder was not involved in the conceptualization, development, analysis, or writing of any of the content in this report, or the decision to submit the article for publication. The authors have no financial disclosures to report.
We thank Shreya Huilgol, Jonah Kushner, and Fernando Esteves for assistance in identifying directors. We thank Brian Hepburn for identification and engagement of potential respondents, as well as Emily Lowrie and Emily Leckman-Westin for their support. We thank Deborah Kim, Josh Wolf, and Rosa Elena Garcia, and Ingrid Estrada-Darley at RAND for survey programming and administration. In addition, we thank Madelyn Gould and Laura Evans for providing feedback on drafts of the survey instrument. Finally, we thank Paul Koegel, Jeanne Ringel, Rajeev Ramchand, and Jeremy Goldbach for thoughtful suggestions.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102208.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Bureau UC. Population and Housing Unit Estimates. Census.gov. Accessed April 12, 2022. https://www.census.gov/popest.
- Colon-Rivera H., Dixon L.B. Mental Health Services in Rural Areas. PS. 2020;71(9):984–985. doi: 10.1176/appi.ps.71903. [DOI] [PubMed] [Google Scholar]
- Cortelyou-Ward K., Atkins D.N., Noblin A., Rotarius T., White P., Carey C. Navigating the Digital Divide: Barriers to Telehealth in Rural Areas. Journal of Health Care for the Poor and Underserved. 2020;31(4):1546–1556. doi: 10.1353/hpu.2020.0116. [DOI] [PubMed] [Google Scholar]
- Crisis Services Task Force. Crisis Now: Transforming Services Is Within Our Reach. Educational Development Center, Inc; 2016.
- Cummings J.R., Wen H., Ko M., Druss B.G. Geography and the Medicaid Mental Health Care Infrastructure: Implications for Health Care Reform. JAMA Psychiatry. 2013;70(10):1084–1090. doi: 10.1001/jamapsychiatry.2013.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkinson S., Godoy L., Beers L.S., Lewin A. Improving Mental Health Access for Low-Income Children and Families in the Primary Care Setting. Pediatrics. 2017;139(1):e20151175. doi: 10.1542/peds.2015-1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan M.F., Goldman M.L. New Opportunities to Improve Mental Health Crisis Systems. Psychiatr Serv. 2021;72(2):169–173. doi: 10.1176/appi.ps.202000114. [DOI] [PubMed] [Google Scholar]
- HRSA. Area Health Resources Files. Published 2020. Accessed January 20, 2021. https://data.hrsa.gov/topics/health-workforce/ahrf.
- Marcoulides K.M., Raykov T. Evaluation of Variance Inflation Factors in Regression Models Using Latent Variable Modeling Methods. Educ Psychol Meas. 2019;79(5):874–882. doi: 10.1177/0013164418817803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miron O., Yu K.H., Wilf-Miron R., Kohane I.S. Suicide Rates Among Adolescents and Young Adults in the United States, 2000–2017. JAMA. 2019;321(23):2362–2364. doi: 10.1001/jama.2019.5054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of State Mental Health Program Directors. Crisis Now | Transforming Crisis Services. Published 2019. Accessed July 28, 2021. https://crisisnow.com/.
- National Conference of State Legislatures. COVID-19 Stimulus Bill: What It Means for States. National Conference of State Legislatures; 2020. Accessed December 10, 2021. https://www.ncsl.org/Portals/1/Documents/statefed/COVID-19-Stimulus-Bill_3-27-20.pdf.
- National Emergency Number Association. 9-1-1 Surcharge - User Fees by State. Published 2021. Accessed April 28, 2022. https://www.nena.org/page/911RateByState.
- NIMH. Mental Health Information - Suicide. Published 2022. Accessed April 19, 2022. https://www.nimh.nih.gov/health/statistics/suicide.
- Pregibon D. Goodness of Link Tests for Generalized Linear Models. Journal of the Royal Statistical Society Series C (Applied Statistics). 1980;29(1):15–114. doi: 10.2307/2346405. [DOI] [Google Scholar]
- SAMHSA. National Guidelines for Behavioral Health Crisis Care: Best Practice Toolkit. SAMHSA; 2020. Accessed February 1, 2022. https://www.samhsa.gov/sites/default/files/national-guidelines-for-behavioral-health-crisis-care-02242020.pdf.
- Santillanes G., Axeen S., Lam C.N., Menchine M. National trends in mental health-related emergency department visits by children and adults, 2009–2015. The American Journal of Emergency Medicine. 2020;38(12):2536–2544. doi: 10.1016/j.ajem.2019.12.035. [DOI] [PubMed] [Google Scholar]
- Vibrant Emotional Health. 988 Serviceable Populations and Contact Volume Projections.; 2020. https://www.vibrant.org/wp-content/uploads/2020/12/Vibrant-988-Projections-Report.pdf?_ga=2.62739180.1718066263.1611784352-1951259024.1604696443.
- Vibrant Emotional Health. 988 and the National Suicide Prevention Lifeline. Accessed February 1, 2022. https://www.vibrant.org/wp-content/uploads/2020/07/988_two_pager_2021-2.pdf.
- Waters R. Enlisting Mental Health Workers, Not Cops. In Mobile Crisis Response. Health Affairs. 2021;40(6):864–869. doi: 10.1377/hlthaff.2021.00678. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.