Abstract
Introduction and importance
Spontaneous perforation of the biliary tree, resulting in retroperitoneal biloma in adults is an extremely rare condition, and may unfold to a potentially fatal outcome, particularly when the diagnosis and definitive treatment are delayed.
Case presentation
We report a case of a 69-year-old male who presented to the emergency room with abdominal pain, localized to the right quadrants, associated with jaundice and dark-coloured urine. Abdominal imaging including CT scan, ultrasound and magnetic resonance cholangiopancreatography (MRCP) revealed a retroperitoneal fluid collection, a distended gallbladder with wall thickening and lithiasis, as well as a dilated common bile duct (CBD) with choledocholithiasis. The analysis of the retroperitoneal fluid obtained by CT-guided percutaneous drainage was consistent with biloma. A combined approach of biloma percutaneous drainage and endoscopic retrograde cholangiopancreatography (ERCP)-guided stent placement in the CBD with biliary stones removal was successful in the management of this patient, despite the fact that the perforation site could not be detected.
Clinical discussion
The diagnosis of biloma is based mainly on clinical presentation and abdominal imaging. If urgent surgical intervention is not indicated, pressure necrosis and perforation of the biliary tree may be avoided by timely percutaneous aspiration of the biloma and ERCP to remove the impacted stones in the biliary tree.
Conclusion
Biloma should be considered in the differential diagnosis of a patient presenting with right upper quadrant or epigastric pain and an intra-abdominal collection on imaging. Efforts should be made in order to offer a prompt diagnosis and treatment to the patient.
Keywords: Retroperitoneal space, Rupture, Spontaneous, Choledocholithiasis, Bile ducts
Highlights
-
•
Spontaneous rupture of the biliary tree in adults is very rare.
-
•
Biloma can present as right upper quadrant pain and an intra-abdominal collection.
-
•
Retroperitoneal biloma warrants prompt management.
1. Introduction
Spontaneous rupture of the biliary tree is a very rare entity and more common in the paediatric population, generally in association with congenital biliary anomalies [1], [2]. In the adult population, the most common etiologic factors of the bile duct and gallbladder perforation include blunt or penetrating abdominal traumas, hepatobiliary surgery and instrumentations [3], [4].
A biloma is a collection of bile outside the biliary tree, that can be either intra- or extrahepatic [4]. Clinical presentation may range from an insidious course, where painless abdominal distension and increasing jaundice are the main symptoms, to an acute presentation with fulminant biliary peritonitis, septic shock and multi-organ failure [3], [5].
Therefore, due to its rarity, biliary perforation requires a high index of suspicion. A prompt diagnosis and treatment are of main importance, since this entity may have a high mortality rate, particularly when the definitive treatment is delayed [5].
Here, we report a 69-year-old male patient with a spontaneous retroperitoneal biloma as a result of choledocholithiasis, that was successfully managed by a multidisciplinary team with percutaneous drainage and endoscopic biliary decompression in the context of a public hospital.
This work has been reported in line with the updated SCARE guidelines [6].
2. Case report
A 69-year-old Caucasian male with no significant past medical history nor chronic medication presented to the emergency room with constant right-sided abdominal pain for four days. The pain was described as mild to moderate and associated with constipation and dark-coloured urine. The patient denied the experience of fever, chills, nausea, recent weight loss or abdominal trauma. On physical examination, there was evidence of jaundice and distended abdomen, with no tenderness upon palpation. Laboratory workup was significant for elevated bilirubin level, hepatic cytolysis and cholestasis, without increased inflammation markers [aspartate aminotransferase: 196 U/L (normal: 13-38 U/L), alanine aminotransferase: 664 U/L (10-49 U/L), alkaline phosphate level: 193 U/L (46-116 U/L), gamma-glutamyl transferase: 186 U/L (<73 U/L), total bilirubin: 10,02 mg/dL (0.2–1.1 mg/dL), direct bilirubin: 6,81 mg/dL (<0.3 mg/dL)].
Abdominal ultrasound (US) revealed a distended gallbladder with wall thickening, containing sludge and microlithiasis, as well as a dilated common bile duct (CBD) of 9,6 mm and intrahepatic ducts with no identifiable obstacle or free peritoneal fluid.
The patient was then hospitalized for further investigation of the aetiology of the obstructive jaundice.
Computed tomography (CT) scan of the abdomen and pelvis was performed 4 days after initial admission and revealed a fluid collection anterior to the psoas muscle, below the inferior pole of the right kidney as well as a densification of the right perirenal fat with extension to its hilum and to the inferior vena cava, associated with findings of urothelial thickening (Fig. 1).
Fig. 1.
(A, B): Abdominal CT scan revealing a fluid collection anterior (white arrows) to the right psoas muscle and densification of the right perirenal fat; (C): CBD dilation (arrow head).
On day 12, the patient experienced worsening of the abdominal pain, with tenderness upon palpation of the right upper quadrant, but no fever, associated with increased inflammation markers [white blood cell count: 23 × 109/L (4.1–11.1 × 109/L); C-reactive protein: 35.84 mg/dL (<0.5 mg/dL)], and negative blood cultures. A control CT scan of the abdomen revealed spread of the retroperitoneal fluid collection (Fig. 2) and the patient was started on an empiric antibiotic regimen with vancomycin and piperacillin-tazobactam, with subsequent improvement of the abdominal pain.
Fig. 2.
(A, B): Control abdominal CT scan revealing spread of the retroperitoneal collection (white arrow); (C): sagittal plane showing extensive fluid collection anterior to the psoas muscle.
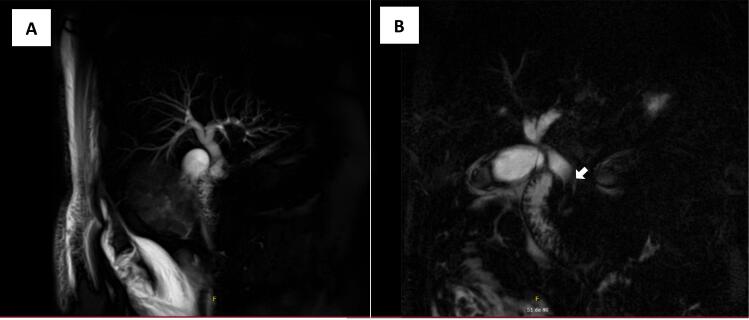
On day 18, he was submitted to a magnetic resonance cholangiopancreatography (MRCP) of the abdomen, which did not identify the rupture site, but revealed the presence of various subtraction images in the distal third of the CBD, compatible with choledocholithiasis (Fig. 3).
Fig. 3.
(A, B): Magnetic resonance cholangiopancreatography (MRCP) of the abdomen revealing the presence of various subtraction images in the distal third of the CBD, compatible with choledocholithiasis (white arrow).
Given the insufficient control of the clinical situation, in spite of the supportive treatment, with intravenous antibiotics and analgesics, it was decided to do a diagnostic CT-guided percutaneous fluid aspiration on day 25. The macroscopic aspect of the fluid revealed that it was bilious in origin, with negative cytology for malignant cells.
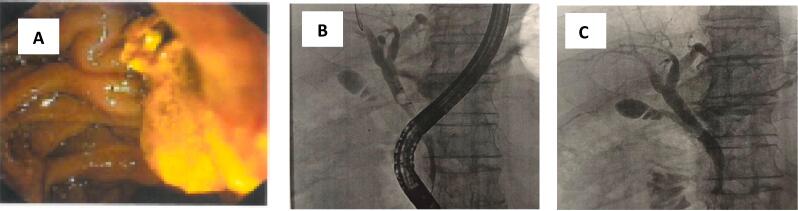
Endoscopic retrograde cholangiopancreatography (ERCP) was performed on day 27, and it did not identify the presence of any contrast extravasation but permitted extraction of some biliary stones and placement of a stent in the CBD. An external drainage tube was then placed on the retroperitoneal collection on day 31 (Fig. 4). The patient underwent an additional cycle of targeted antibiotic, with meropenem, given the isolation of extended spectrum beta-lactamase -producing Klebsiella pneumoniae in the bile acquired from the drainage tube, with a favourable outcome, and was discharged at day 57. The drainage tube was left in situ for 70 days, and it drained a total of 6890 mL of bile.
Fig. 4.
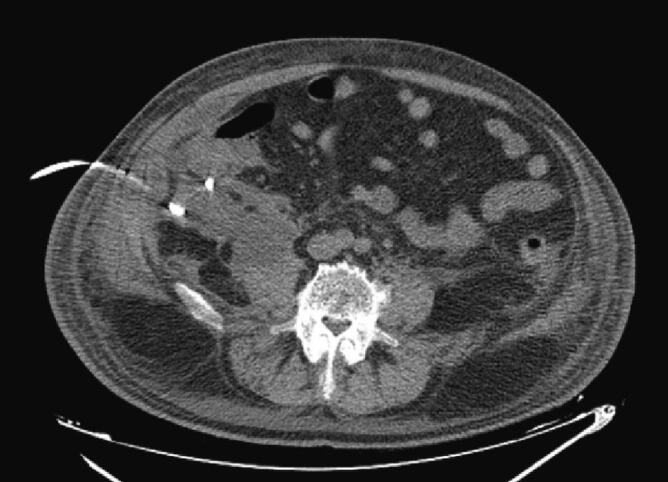
CT-guided percutaneous drainage with tube placement.
After the patient was discharged, he had to undergo two additional ERCP (Fig. 5), with lithotripsy to remove the remaining calculus. Finally, the patient underwent an elective laparoscopic cholecystectomy with intraoperative cholangiogram eight months after the initial presentation, with findings of scleroatrophic gallbladder and numerous adhesions and fibrosis, in order to prevent the possibility of repeated impaction of calculus in the biliary ducts. Histopathologic examination of the resected tissues revealed an acute-on-chronic cholecystitis.
Fig. 5.
Last ERCP after hospital discharge. (A): Biliary stone removal; (B): cholangiography before calculi removal; (C): cholangiography at the end of the procedure.
The patient remains asymptomatic after 10 months of follow-up.
3. Discussion
Perforations of the biliary tree in adults are extremely rare and are mainly caused by iatrogenic injury or severe abdominal trauma [7]. However, there are a small collection of cases of spontaneous biloma, reported in the literature. The most common spontaneous perforation site of the biliary tract is the gallbladder and is typically caused by cholecystitis and cholelithiasis [2]. The pathophysiology of the spontaneous perforation of the biliary tree remains to be completely elucidated, but some mechanisms have already been proposed, namely: erosion of the bile duct wall by biliary stones; persistently increased intraductal pressure due to an obstruction of the distal bile duct; thrombosis of a vessel supplying the bile duct wall or even intramural infection of the duct as a result of cholangitis [2]. As previously mentioned, the clinical presentation of biloma is extremely variable, ranging from non-specific abdominal pain to severe biliary sepsis, depending upon the location, size and aetiology of the biloma, frequently delaying the diagnosis [4], [7].
The diagnosis of a biloma is based on the clinical presentation and in the radiological abdominal imaging. The abdominal US is usually the initial imaging in the evaluation of RUQ (right upper quadrant) pain, and it is capable of evaluating the presence of biloma and sometimes the underlying pathology and excluding differential diagnosis, such as hematoma, seroma, liver abscess, cysts or pseudocysts [7], [8]. On the other hand, CT plays a crucial role, since it can define the collection and the integrity of the retroperitoneal organs with more accuracy. Percutaneous aspiration under radiologic guidance, as well as ERCP can aid both in diagnosis and treatment. Indeed, impacted stones in the biliary tree need to be extracted to avoid pressure necrosis and spontaneous perforation, and can be complemented with biliary stent placement [5]. Although it was not available in this case, the hepatobiliary iminodiacetic acid scan is considered to be the most effective diagnostic imaging modality in the identification of bile leak [5].
Emergent surgical intervention is necessary in hemodynamically unstable patients, presenting with septic shock, biliopleural fistula, biliary peritonitis or bilhemia [4]. The goals of surgical management are to ease the abdominal contamination with infected bile by draining the peritoneal cavity, restoring the patency of the biliary tract, surgical closure of the perforation and T-tube drainage, as well as treating the underlying biliary pathologic features [5], [9]. In some instances, the perforation site cannot be repaired due to the surrounding inflammation [5], [9].
On the other hand, some bilomas can be managed only with surveillance with no intervention, particularly those that are small in size and asymptomatic [7], [10]. However, most cases require treatment. In fact, in symptomatic stable patients whose clinical condition warrants a conservative approach the management goals also include draining the bile collection and decompressing the biliary tree, with efforts to find the leakage site [9]. However, ERCP and stent placement should only be used as temporizing measures to manage the acute obstructive phase [5]. Definitive surgical intervention must follow initial biliary decompression to avoid complications [5] and to prevent the possibility of repeated impaction of calculus in the biliary ducts.
In this article, we report a case of a spontaneous retroperitoneal biloma, in a patient with choledocholithiasis, in which the diagnosis was made when the fluid aspirated from the retroperitoneal collection was identified as bile. After the definitive diagnosis, it was decided to leave an external drainage tube on the retroperitoneal collection and to perform an ERCP, in order to remove the biliary stones and decompress the biliary tree. The site of rupture or leakage could not be identified on MRCP or ERCP and the patient's condition gradually improved on conservative management, so surgery was deferred. This case portrays the difficulty of the diagnosis, given its rarity and the scarcity of information about the appropriate management. Notwithstanding, this case presentation displays that in selected patients a conservative approach is safe and preferable, given the possible morbimortality associated with an urgent surgical intervention [4], [7], [10].
4. Conclusion
Spontaneous perforation of the biliary tree, resulting in a retroperitoneal biloma in adults is an extremely rare condition. Therefore, it is a condition that needs a high index of suspicion, when a patient presents with RUQ or epigastric pain, and a prompt diagnosis and treatment are of main importance.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval is exempt/waived at our institution.
Funding
None.
Guarantor
Maria Adriano Costa.
Research registration number
N/A.
CRediT authorship contribution statement
Maria Adriano Costa: Conceptualization, Methodology, Writing - Original draft. Leonor Sardo: Supervision. Alice Pimentel, Sofia Dias da Silva, Rui Moreira, Joana Noronha: Writing - Review & editing.
All authors read and approved the final manuscript.
Conflicts of interest
None.
Contributor Information
Maria Adriano Costa, Email: maria.costa.72444@chbv.min-saude.pt.
Alice Pimentel, Email: Maria.Pimentel.70978@chbv.min-saude.pt.
Sofia Dias da Silva, Email: Sofia.Silva.71127@chbv.min-saude.pt.
Leonor Sardo, Email: leonorcostasardo@gmail.com.
Rui Moreira, Email: rufisamo@yahoo.com.
Joana Noronha, Email: Joana.Noronha.11295@chbv.min-saude.pt.
References
- 1.Malik H.S., Cheema H.A., Fayyaz Z., Hashmi M.A., Parkash A., Waheed N., Mushtaq I., Anjum N. Spontaneous perforation of bile duct, clinical presentation, laboratory work up, treatment and outcome. J. Ayub Med. Coll. Abbottabad. 2016;28(3):518–522. PMID: 28712226. [PubMed] [Google Scholar]
- 2.Ishii K., Matsuo K., Seki H., et al. Retroperitoneal biloma due to spontaneous perforation of the left hepatic duct. Am. J. Case Rep. 2016;17:264–267. doi: 10.12659/AJCR.897612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yaşar N.F., Yaşar B., Kebapçi M. Spontaneous common bile duct perforation due to chronic pancreatitis, presenting as a huge cystic retroperitoneal mass: a case report. Cases J. 2009;2(9) doi: 10.4076/1757-1626-2-6273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yousaf M.N., D'Souza R.G., Chaudhary F., et al. Biloma: a rare manifestation of spontaneous bile leak. Cureus. 2020;12(5) doi: 10.7759/cureus.8116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atwez A., Augustine M., Nottingham J.M. Non-traumatic perforation of common hepatic duct: case report and review of literature HP. Int. J. Surg. Case Rep. 2017;41:188–190. doi: 10.1016/j.ijscr.2017.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. International Journal of Surgery. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Bas G., Okan I., Sahin M., Erylmaz R., Isk A. Spontaneous biloma managed with endoscopic retrograde cholangiopancreatography and percutaneous drainage: a case report. J. Med. Case Rep. 2011:5. doi: 10.1186/1752-1947-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blake-Siemsen J.C., Kortright-Farías M. Spontaneous retroperitoneal biloma: a case report. Cirugia Cirujanos (Eng. Ed.) 2017;85(6):552–556. doi: 10.1016/j.circir.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Kang S., Han H., Min S.K., Lee H.K. Nontraumatic perforation of the bile duct in adults. Arch. Surg. 2004;139(10):1083–1087. doi: 10.1001/archsurg.139.10.1083. [DOI] [PubMed] [Google Scholar]
- 10.Lee J.H., Suh J.I. A case of infected biloma due to spontaneous intrahepatic biliary rupture. Korean J. Intern. Med. 2007;22(3):220–224. doi: 10.3904/kjim.2007.22.3.220. [DOI] [PMC free article] [PubMed] [Google Scholar]