Abstract
The COVID-19 pandemic prompted unexpected changes in the healthcare system. This current longitudinal study had 2 aims: 1) describe the trajectory of pandemic-associated stressors and patient-reported health outcomes among patients receiving treatment at a tertiary pain clinic over 2 years (May 2020 to June 2022); and 2) identify vulnerable subgroups. We assessed changes in pandemic-associated stressors and patient-reported health outcome measures. The study sample included 1270 adult patients who were predominantly female (74.6%), White (66.2%), non-Hispanic (80.6%), married (66.1%), not on disability (71.2%), college-educated (59.45%), and not currently working (57.9%). We conducted linear mixed effect modeling to examine the main effect of time with controlling for a random intercept. Findings revealed a significant main effect of time for all pandemic-associated stressors except financial impact. Over time, patients reported increased proximity to COVID-19, but decreased pandemic-associated stressors. A significant improvement was also observed in pain intensity, pain catastrophizing, and PROMIS-pain interference, sleep, anxiety, anger, and depression scores. Demographic-based subgroup analyses for pandemic-associated stressors revealed that younger adults, Hispanics, Asians, and patients receiving disability compensation were vulnerable groups either during the initial visit or follow-up visits. We observed additional differential pandemic effects between groups based on participant sex, education level, and working status. In conclusion, despite unanticipated changes in pain care services during the pandemic, patients receiving pain treatments adjusted to pandemic-related stressors and improved their health status over time. As the current study observed differential pandemic impacts on patient subgroups, future studies should investigate and address the unmet needs of vulnerable subgroups.
Perspective
Over a 2-year timeframe, the pandemic did not adversely influence physical and mental health among treatment-seeking patients with chronic pain. Patients reported small but significant improvements across indices of physical and psychosocial health. Differential impacts emerged among groups based on ethnicity, age, disability status, gender, education level, and working status.
Keywords: COVID-19 pandemic, chronic pain, racial disparities, physical health, pandemic stressors
The broad impacts of the COVID-19 pandemic on healthcare have persisted through years of intermittent lockdowns and the emergence of new variants of the SARS-CoV-2 virus. Initial changes in healthcare service delivery, most notably the widespread adoption of telehealth, have become the new normal for patients. In addition to indirect impacts on patient health, recent studies describe direct health impacts of COVID-19 including the development of pain symptoms 1 and prolonged symptomatology 2 in both specific subgroups and the global population at large. To date, evidence on the impact of COVID-19 among patients with pain is mixed. Emerging research from Italy, Canada, the United Kingdom, and the United States found adverse effects of the COVID-19 pandemic on patients with pain including increased pain, psychological distress, barriers to pain care during periods of lockdown and social distancing,3, 4, 5, 6 and disruptions to existing pain treatment.7, 8, 9 Conversely, there is encouraging evidence suggesting resilience among patients with chronic pain during the pandemic,10, 11 consistent with pre-pandemic findings on the resilience of patients with chronic pain.12, 13
Notably, there is increasing evidence of disproportionate impacts of the pandemic on specific subgroups and marginalized individuals. Evidence suggests that racial and ethnic minorities, older adults, and individuals with comorbid chronic health conditions are at increased risk of severe disease and death resulting from infection with the SARS-CoV-2 virus.14, 15, 16 The causes of these health disparities are still unclear but partly due to increased stress from systemic inequality, low socioeconomic status, and unequal access to healthcare.17, 18 Several studies have reported that disproportionate impacts of the pandemic extend to patients with chronic pain. Cross-sectional studies of individuals with chronic pain have found that women reported greater pain and negative mood related to the pandemic,19 individuals identifying as non-Hispanic Black reported increased pandemic-related disruptions to mood, sleep quality, and pain20; in addition, female sex, older age, and nonwhite race were associated with worse pain after the onset of the pandemic.5 Evidence also suggests that health disparities during the pandemic may exacerbate disparities in access to quality pain treatment.21 Taken together, these findings underscore the importance of examining subgroups and potential disparities in the impacts of the pandemic on individuals with chronic pain.
In the present study, we aimed to describe the trajectory of patients with chronic pain seeking treatment at a multidisciplinary pain clinic during the first 2 years (May 2020 to June 2022) of the COVID-19 pandemic. In a prior investigation, we reported that patients from this clinic were largely resilient in the first few months of the COVID-19 lockdown,22 as evidenced by unchanged pain intensity scores, and improvements in pain interference, physical function, sleep impairment, and emotional support. However, elevated pain catastrophizing scores were observed as cases of COVID-19 in San Mateo County, CA, USA increased in July 2020, suggesting the important role of time and pandemic-specific factors (eg, case counts, vaccinations, infection, lockdowns) on patients’ reported health and function. Accordingly, our present study aimed to 1) describe patients’ pandemic-associated stressors, in addition to physical and psychosocial health over the past 2 years, and; 2) characterize subgroup impacts of the pandemic, in light of growing evidence of disproportionate impacts on minorities. Consistent with results from our prior work, we hypothesized that patients with chronic pain presenting at a multidisciplinary pain clinic would report resilience and improvement across pandemic-related and Patient-Reported Outcomes Measurement Information System (PROMIS) outcomes over time, with notable differences across vulnerable subgroups of individuals.
Methods
Study Design and Participants
This observational cross-sectional retrospective cohort study was conducted at Stanford University’s Pain Management Center, a multidisciplinary pain clinic located in San Mateo County, Redwood City, CA, USA, between May 1, 2020, and June 19, 2022. Fig 1 depicts the timeline of the local COVID-19 pandemic. The first positive case was reported on February 21, 2020, and shelter-in-place order went into effect on March 16, 2020. Shortly after, the clinic started offering virtual visits and resumed in-person visits in June of 2020. From June of 2020 to the present, the clinic offers a hybrid of virtual and in-person visits. Since the first COVID-19 vaccine was available to local residents in December 2020, 81% of county residents age 16 and older received at least 1 COVID-19 vaccine within 6 months (May 27, 2021). This vaccination rate was higher than the US average (57%) by May 22, 2021.23, 24, 25 Healthcare workers started receiving vaccination on December 15, 2020, followed by older adults aged 65 or older on January 12, 2021, and adults aged 50 or older on April 1, 2021. The shelter-in-place order was lifted on June 15, 2021, and peak cases were observed on January 11, 2022. By June 19, 2022, 91.6% of San Mateo County residents received at least 1 dose of COVID-19 vaccine and 82.5% were fully vaccinated.
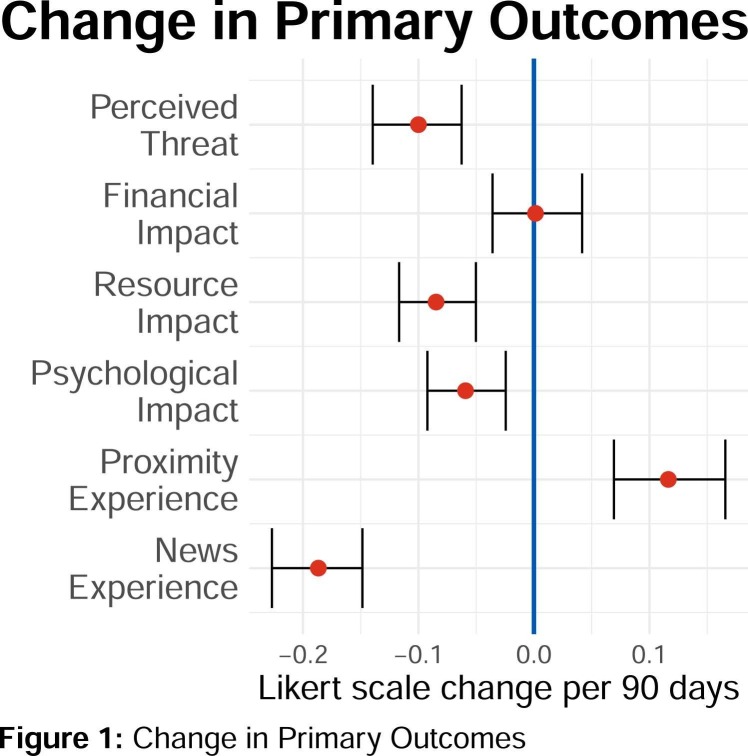
Figure 1.
Change in primary outcomes.
Study procedures included consecutive data collection from patient surveys collected during initial and follow-up visits to a tertiary pain clinic, and who agreed to complete additional surveys related to COVID-19. Data was collected for 26 months through CHOIR, a digital learning healthcare system, to characterize patients’ physical, psychological, and social function, in addition to COVID-19 impacts following the pandemic lockdown, enaction of the stay-at-home order in San Mateo County. This initial lockdown, which lasted from mid-March to late May 2020, restricted all private and public gatherings outside of single households and all travel not deemed essential. On April 17, 2020, the county-wide mask mandate rule was imposed on the public and workers. Then, a statewide mask mandate in public or high-risk settings was issued on June 18, 2020. This statewide mask mandate was lifted for vaccinated individuals in most settings since June 15, 2021. However, our pain management center has been maintaining the mask mandate for patients and healthcare workers since the reopening of the clinic for in-person visit in May 2020.26, 27 At the pain management clinic in which the present study took place, only virtual visits were offered in the first month of the study (May 2020), with in-person visits for medically necessary appointments resuming in June 2020.
The current study included 6575 surveys collected from 4127 patient participants during their clinic visit (virtual or in-person). The study survey was presented as optional, and patients who elected to participate were presented with an information sheet and an informed consent, which was signed digitally. The number of surveys per person ranged from 1 to 25, with 2842 (68.86%) participants completing 1 survey. To assess the impact of COVID-19 over time, our final study sample consisted of 1270 (30.77%) patient participants who were 18 years of age or older at the first survey and completed 2 to 9 surveys at least 30 days apart. The research was conducted in full compliance with the American Psychological Association’s Ethical Principles in treating human participants. Stanford University’s Institutional Review Board (IRB) approved the study procedures.
Measures
Demographics
Patient age, sex, race, ethnicity, education, marital status, disability status, and working status were retrieved from their clinic intake form. Participant race and ethnicity data were recorded using the following categories: Asian; Black or African American; Black, non-Hispanic; Other; Other, Hispanic; American Indian or Alaska Native; Native Hawaiian or Other Pacific Islander; White; White, non-Hispanic. Table 1 displays the correspondence between recorded and analyzed participant race and ethnicity categories.
Table 1.
Correspondence Between Recorded and Analyzed Participant Race and Ethnicity Categories
| participant race and ethnicity as analyzed | participant race and ethnicity as originally recorded |
|---|---|
| Asian | Asian |
| Black | Black or African American |
| Black, non-Hispanic | |
| Other | Other |
| Other, Hispanic | |
| American Indian or Alaska Native | |
| Native Hawaiian or Other Pacific Islander | |
| White | White |
| White, non-Hispanic | |
| Race Missing | |
| Unknown | |
| Patient Refused to Answer | |
| Race and Ethnicity Unknown | |
| Hispanic | Hispanic/Latino |
| Non-Hispanic | Non-Hispanic/Non-Latino |
| Ethnicity Missing | |
| Patient Refused | |
| Unknown |
COVID-Related Domains
We used a set of measures previously developed to assess social psychological aspects of the COVID-19 pandemic.28 Three measures assessed 6 domains related to COVID-19 impacts and experiences. Participants rated each statement on a Likert-type scale ranging from 1 (not true of me at all) to 7 (very true of me). The scores on the individual items were summed, and an average score was generated for each domain. Higher scores indicated higher endorsement of symptoms or impacts on each domain. These measures included the following:
Perceived Coronavirus Threat Questionnaire
Perceived Coronavirus Threat Questionnaire which consists of 3 items assessing perceived threat as related to COVID-19. An example item “Thinking about the Coronavirus (COVID-19) makes me feel threatened.”
Coronavirus Impacts Questionnaire
Coronavirus Impacts Questionnaire included 3 subscales assessing financial, resource and psychological impact. Each subscale consisted of 2 items assessing impacts of each domain. An example item from the Financial Impacts Scale “The Coronavirus (COVID-19) has impacted me negatively from a financial point of view,” and from the Psychological Impacts Scale “I have become depressed because of the Coronavirus (COVID-19).”
Coronavirus Experience Questionnaire
Coronavirus Experience Questionnaire included 2 subscales; each consists of 2 items. Proximity to Others Scale assessed the degree to which a respondent was close to others afflicted or exposed to COVID-19; and News Scale assessed the degree to which respondents watched news related to COVID-19. Example item from the Proximity to Others Scale, “I know someone who has been diagnosed with Coronavirus (COVID-19),” and from the News Scale “I watch a lot of news about the Coronavirus (COVID-19).”
Pain Intensity and Pain Body Map Segments
Pain intensity was assessed on a numerical rating scale (NRS). Respondents were asked to rate their average pain intensity over the previous 7 days on a scale of 0 (no pain) −10 (worst pain imaginable). Assessment of pain intensity using an NRS has been supported in prior studies.29 Patient self-reported the number of body segments in which chronic pain is experienced marked locations of pain on a reliable and valid CHOIR body map scheme that included 36 anterior and 38 posterior symmetrical body segments for a maximum total of 74 segments.30, 31
Pain Catastrophizing
The Pain Catastrophizing Scale (PCS) is a 13-item questionnaire that assesses distress regarding the cognition and emotion associated with actual or anticipated pain.32 The PCS comprises 3 subscales: rumination, magnification, and helplessness. Patients rate each item on a 5-point Likert Scale (0 = Not at all to 4 = All the time). The PCS has a minimum score of 0 and a maximum score of 52 with higher scores indicative of more catastrophic thinking.
The Patient-Reported Outcomes Measurement Information System
The PROMIS measures are well-validated and widely used to assess physical and psychosocial health status in patients with chronic illnesses, including chronic pain.33, 34, 35, 36, 37, 38 Detailed information about the measure development and validation is available at http://www.healthmeasures.net. All PROMIS measures in the current study were administered using computerized adaptive testing (CAT). T-scores were calculated for each patient (population M = 50, SD = 10).36 PROMIS CAT instruments were administered for pain domains (pain behavior, pain interference), physical health (fatigue, mobility, upper extremity, sleep disturbance), psychological health (anger, anxiety, depression, emotional support), and social health (social isolation, satisfaction with social roles and activities). Higher scores on each PROMIS measure generally indicate greater severity of each symptom domain. However, higher scores on PROMIS physical function, emotional support, and satisfaction with roles and activities indicate better health status in each domain.
Statistical Analyses
Demographics, timepoints, and outcomes were all examined for missingness and nonsensical inputs before analysis. Day 0 for all patients is defined as the day of their first survey. Analysis was limited to individuals who responded to 2 to 9 surveys, where each survey was at least 30 days apart from the next survey. We excluded patients who only responded to 1 survey. We instituted an upper cutoff at 9 because the number of patients dropped steeply after 9, and the patients who visited the pain clinic 10 or more times in the 26-month period represent a small portion of the clinical pain population (.25%). Surveys taken within 30 days were excluded to ensure capturing change over time without biasing the results with recent follow-up visits. All remaining surveys were included in the analysis if they contained valid timepoints and outcome measures, and missingness was permitted in demographic variables. Included and excluded patients were assessed using chi-squared tests (chisq.test) for categorical variables and Wilcox rank sum (kruskal.test) for the skewed continuous variables.
R 4.2.1 was used to analyze the study findings. Assumptions of normality were assessed by plotting the data, which revealed violations of normality. As such, Wilcoxon rank-sum tests were applied to test for differences between groups (wilcox.text). Bootstrapped standard errors (boot 1.3–28) were used to avoid problems with biased errors due to non-normally distributed residuals. All intervals reported are 95% confidence intervals as reported by SAS. An alpha of .05 for statistical significance was applied to describe the patient population over time. For primary and secondary aims, changes over time were modeled using mixed effect linear modeling (lme4 1.1–29) with a random intercept. For subgroup analyses, both between-group comparisons and within-group analyses were reported. Mixed effect modeling allows for the discovery of overall trends (fixed effects) while adjusting for individual differences at the initial visit (random effects) and is robust against missing data. A significant intercept value difference without a significant trend difference means that the subgroup values are different but parallel over time. A significant difference between intercept and trend could suggest converging or diverging subgroup trends. Finally, linear, quadratic, and cubic effects were assessed. In all cases, linear effects produced the lowest Bayesian Information Criterion (BIC) and were therefore retained. The fixed effects are reported below.
Results
Sample Characteristics
Of the 4127 patients that responded to at least 1 survey, 1270 patients met the inclusion criteria for the study and were included in the analysis. Table 2 describes the study sample, which was predominantly female (74.57%), middle aged (M = 55.52, SD = 15.47), White (66.22%), non-Hispanic (80.63%), married (66.14%), not receiving disability benefits (71.18%), not currently working (57.87%), with a college degree (59.45%). Half the patients (49.92%) identified 10 or fewer pain sites, 26.31% reported at least 20 pain sites, and 7.24% of patients identifying more than 40 pain sites. White, non-Hispanic, older, and female subgroups were overrepresented in our study sample (P = .053, P = .021, P < .001, and P = .035, respectively) relative to patients who responded to 1 survey and to patients who responded to 10 or more surveys, with the latter being a much smaller group.
Table 2.
Sample Characteristics
| characteristics | study population (n = 1270) |
|---|---|
| Age, Mean Years (SD) | 55.52 (15.47) |
| Age Categories, No. (%) | |
| 18-30 | 84 (6.61%) |
| 31-55 | 498 (39.21%) |
| 56-70 | 453 (35.67%) |
| 71+ | 235 (18.51%) |
| Pain Sites, No. (%) | |
| 1-10 | 634 (49.92%) |
| 11-20 | 302 (23.78%) |
| 21-40 | 242 (19.06%) |
| 41-60 | 66 (5.20%) |
| 61-74 | 26 (2.05%) |
| Sex, No. (%) | |
| Female | 947 (74.57%) |
| Male | 292 (22.99%) |
| Missing | 31 (2.44%) |
| Race, No. (%) | |
| Asian/Pacific Islander | 96 (7.56%) |
| Black | 41 (3.23%) |
| Other | 173 (13.62%) |
| White | 841 (66.22%) |
| Missing | 119 (9.37%) |
| Ethnicity, No. (%) | |
| Hispanic | 118 (9.29%) |
| Non-Hispanic | 1024 (80.63%) |
| Missing | 128 (10.08%) |
| Marital Status, No. (%) | |
| Married/Living Together | 840 (66.14%) |
| Single | 349 (27.48%) |
| Missing | 81 (6.38%) |
| Receiving Disability Benefits, No. (%) | |
| Yes | 292 (22.99%) |
| No | 904 (71.18%) |
| Missing | 74 (5.83%) |
| Education, No. (%) | |
| Less than High School | 25 (1.97%) |
| High School or Some College | 406 (31.97%) |
| 4-year College or More | 755 (59.45%) |
| Missing | 84 (6.61%) |
| Working Status, No. (%) | |
| Working | 456 (35.91%) |
| Not working | 735 (57.87%) |
| Missing | 79 (6.22%) |
COVID-19 Impacts on Patients With Chronic Pain Across Time
Patients’ Reports of Perceived Threat, Exposure to Pandemic News, Proximity to Persons With COVID-19, Financial, Resource, and Psychological Impacts Overtime (Primary Aim)
Across survey responses, on a response scale of 1 (not true of me at all) to 7 (very true of me), during their first visit patient ratings fell in the below average to average range on several indices: perceived threat (M = 3.89, SD = 2.11), exposure to pandemic news (M = 3.47, SD = 2.06), proximity experience (M = 1.52, SD = 1.52), financial impact (M = 2.77, SD = 2.19), resource impact (M = 2.36, SD = 1.83), and psychological impact (M = 2.73, SD = 1.88). Overall, patients experienced low to low-moderate levels of COVID-19-associated stressors during their initial clinic visit.
Results showed ( Table 3) that patient’s perceived COVID-19-associated stressors improved across 4 of the 6 COVID-19 outcomes over time. The reported β coefficients represent the average rate of change per 30 days after controlling for within-individual correlation. Mixed-effects analysis revealed significant fixed effects of time for perceived threat (β = −.033, P < .001), resource impact (β = −.027, P < .001), psychological impact (β = −.021, P < .001), proximity experience (β = .039, P < .001), and news experience (β = −.063, P < .001). The time effect was nonsignificant for financial impact (P = .946). The unit of these effects are Likert scale points per 30 days. The results from this analysis are displayed in Fig 1. Findings demonstrate that patient perceptions of threat, resource scarcity, psychological hardships, and news consumption decreased overtime while experiences of close proximity cases increased. Improvements on these indices ranged from 6.51% on perceived threat to 15.31% on news experience, with a 20.54% increase in proximity experience (Table 2). Finally, a mixed-effects linear regression was conducted to test if the decrease in psychological impact over time could be explained by baseline social isolation. This model showed that adding social isolation to the model did not significantly change our time coefficient, which indicates our findings in this domain are stable (−.000678 vs −.000668, 3.09% change).
Table 3.
COVID-19 Impacts on Patients With Chronic Pain Across Time
| variable | first visit*mean (sd) | last visit*mean (sd) |
first & last difference |
||
|---|---|---|---|---|---|
| value | percent | p-value† | |||
| Primary Outcomes | |||||
| Perceived Threat | 3.89 (2.11) | 3.64 (2.05) | −.25 | −6.51% | .002 |
| Financial Impact | 2.77 (2.19) | 2.80 (2.20) | .03 | 1.14% | .665 |
| Resource Impact | 2.36 (1.83) | 2.10 (1.65) | −.27 | −11.30% | <.001 |
| Psychological Impact | 2.73 (1.88) | 2.59 (1.82) | −.14 | −5.13% | .076 |
| Proximity Experience | 1.52 (1.52) | 1.83 (1.88) | .31 | 20.54% | <.001 |
| News Experience | 3.47 (2.06) | 2.94 (1.99) | −.53 | −15.31% | <.001 |
| Secondary Outcomes | |||||
| Pain | |||||
| Pain Intensity | 5.51 (2.02) | 5.24 (2.17) | −.27 | −4.95% | .001 |
| Pain Catastrophizing | 18.41 (12.16) | 16.07 (12.46) | −2.33 | −12.67% | <.001 |
| Pain Interference | 64.48 (6.96) | 63.53 (7.38) | −.95 | −1.48% | .001 |
| Physical | |||||
| Fatigue | 58.93 (10.22) | 58.58 (10.63) | −.35 | −.59% | .316 |
| Sleep Disturbance | 56.65 (8.88) | 55.84 (9.50) | −.81 | −1.43% | .012 |
| Upper Extremities | 39.01 (9.75) | 38.94 (9.96) | −.07 | −.18% | .884 |
| Mobility | 40.56 (8.98) | 40.65 (8.97) | .09 | .23% | .719 |
| Mental | |||||
| Depression | 54.38 (9.26) | 54.00 (9.47) | −.39 | −.71% | .308 |
| Anxiety | 55.47 (8.94) | 54.90 (9.59) | −.58 | −1.04% | .112 |
| Anger | 48.79 (9.73) | 47.55 (10.21) | −1.24 | −2.54% | .001 |
| Emotional Support | 51.86 (9.37) | 52.18 (9.59) | .32 | .62% | .484 |
| Social | |||||
| Social Roles & Activities | 41.74 (8.82) | 41.88 (8.81) | .14 | .35% | .422 |
| Social Isolation | 49.24 (9.31) | 49.30 (9.81) | .06 | .12% | .804 |
Bold values are statistically significant values.
Patients included in this study visited 2 to 9 times.
Wilcox rank-sum test.
Patients’ Report of Pain Intensity, Pain Catastrophizing, and PROMIS Outcomes Overtime (Secondary Aim)
During their initial visit, patients reported moderate pain intensity levels (M = 5.51, SD = 2.02); moderate levels of pain catastrophizing (M = 18.41, SD = 12.16), above average levels of pain interference (M = 64.48, SD = 6.96); and average levels of fatigue (M = 58.93, SD = 10.22), and sleep disturbance (M = 56.65, SD = 8.88). Notably, patient’s physical function levels were lower, as indexed by their upper extremities (M = 39.01, SD = 9.75) and mobility scores (M = 40.56, SD = 8.98) compared to the population mean. Finally, the means of psychosocial factors were all within one standard deviation of the population mean (Table 3). Overall, our study sample reported moderate pain intensity and pain interference, and limitations in physical function.
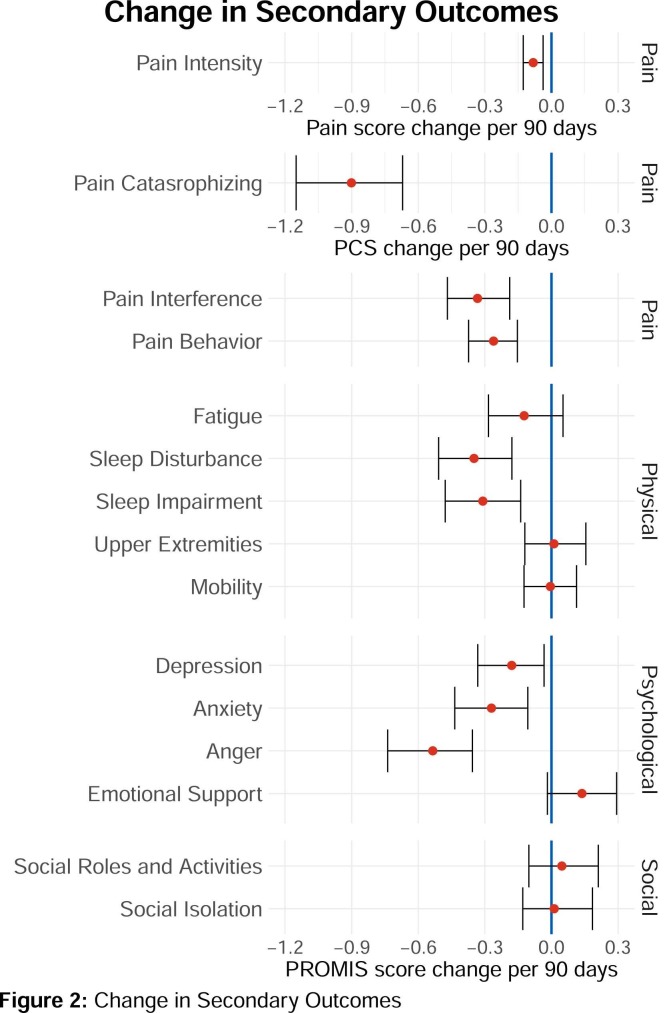
A mixed effect linear model was fit to examine changes in pain-related outcomes across time as indexed by measures of pain intensity and PROMIS outcomes. We observed significant improvements in the pain domain (pain intensity: β = −.027, P < .001; pain catastrophizing: β = −.303, P < .001; and pain interference: β = −.111, P < .001). In the physical health domain, and significant changes were observed only in sleep disturbance (β = −.117, P < .001). We observed significant improvements across the psychological domain (anxiety: β = −.090, P = .001; anger: β = −.177, P < .001; depression: β = −.060, P = .016). In the social domain, there were no significant changes (social roles and activities: β = .005, P = .908; social isolation: β = .002, P = .956; emotional support β = .045, P = .092). These results are illustrated in Fig 2. Overall, findings revealed that people receiving pain treatment showed improvements in pain, sleep, and psychological health overtime. These improvements were small, ranging from 1.43% on sleep disturbance to 4.9% on pain intensity (Table 2).
Figure 2.
Change in secondary outcomes.
Subgroup Differences (Age, Race/Ethnicity, Sex, Pain Sites, Receiving Disability Benefits, Education & Working Status) in Outcome Variables Over Time (Exploratory)
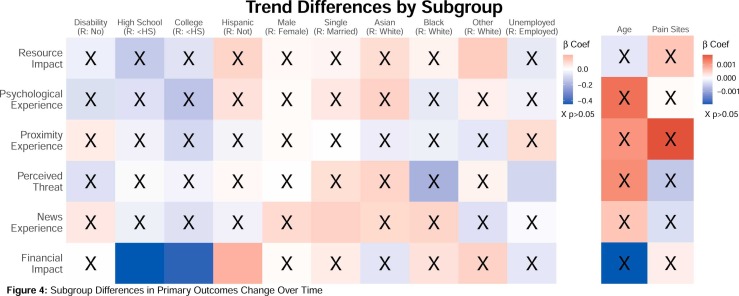
We conducted subgroup analyses for the 6 primary outcomes via mixed-effects linear models for age, race/ethnicity, sex, pain sites, receiving disability benefits, education and working status. We used a mixed effect model with intercepts to examine between-group differences in intercept ( Fig 3) and trends ( Fig 4). We have reported statistically significant β coefficients where intercept values are in Likert scale units and difference in trend values are in Likert scale units per 30 days.
Figure 3.
Subgroup differences in primary differences overall.
Figure 4.
Subgroup differences in primary differences overtime.
Findings revealed that younger adults experienced significantly higher financial impact (β = −.020, P < .001), resource impact (β = −.010, P < .001), psychological impact (β = −.011, P < .001), and proximity experience (β = −.007, P < .001) and less news experience (β = .029, P < .001) in the intercept. There was no evidence of statistically significant moderation effect by age over time on perceived threat, financial impact, resource impact, psychological impact, proximity experience, or news experience (ps>.50). These results suggest that younger people were initially more affected by the pandemic, but age did not significantly impact change over time.
For race and ethnicity, we analyzed our sample using White, Asian, Black, Other, Hispanic, and non-Hispanic subgroups based on patients’ originally recorded race and ethnicity identifications (Table 1). Asian patients (N = 96) reported a significantly higher perceived threat (β = .353, P = .002) and financial impact (β = 1.043, P < .001) compared to White patients, but their trend did not differ significantly from White patients over time. Black patients (N = 41) experienced significantly less psychological impact (β = −.425, P = .017) and proximity experience (β = −.321, P = .004), but their trend did not differ significantly from White patients over time. Patients in the Other subgroup (N = 173) reported significantly less news experience (β = −.325, P = .002) overall, and significantly less improvement in resource impact (β = .039, P = .031) over time compared to White patients. These subgroup findings suggest that, compared to White patients, Asian and Other patients experienced higher financial and resource burden during the pandemic, and Black patients reported less psychological impact and case exposure.
Hispanic patients (N = 118) reported a significantly higher perceived threat (β = .345, P = .009), financial impact (β = .296, P = .024), and resource impact (β = .390, P = .001), and less news experience (β = −.528, P < .001) compared to non-Hispanic patients. Over time, Hispanic patients also reported significantly less improvement in financial impact (β = .060, P = .019). These differences suggest that Hispanic patients may have been more impacted by the pandemic, especially in the beginning stages, and did not experience the same recovery as non-Hispanic patients in the financial impact domain.
For participant sex, male and female patients differed significantly in their intercept; males (N = 292) reported significantly higher news consumption (β = .438, P = .004), and females reported higher psychological impact (β = −.300, P < .001), perceived threat (β = −.351, P < .001), and resource impact (β = −.179, P = .008). Trends did not differ significantly by participant sex over time. These differences suggest that the pandemic impacts differed by participant sex depending on the domain of COVID-associated impacts.
Patients who reported receiving disability benefits (N = 292) reported significantly higher financial impact (β = .287, P = .001), resource impact (.504, P < .001), and psychological impact (.365, P < .001) compared to patients who did not report receiving disability benefits. Trends between these groups of patients did not differ significantly over time. Similarly, patients who reported more pain sites had significantly higher perceived threat (β = .011, P < .001), financial impact (β = .015, P < .001), resource impact (β = .015, P < .001) and psychological impact (β = .010, P = .002), and significantly less news experience (β = −.008, P = .011) at baseline. The significantly higher intercept values for patients receiving disability benefits suggest a higher pandemic impact on patients receiving disability benefits, but no significant difference in the slope suggest that the pandemic impact improves at the same rate between those receiving and not receiving disability benefits. Similarly, around 50% of patients identified 10 or fewer pain sites, and subgroup analyses revealed that those more pain sites had a higher pandemic impact at baseline, which improves at the same rate among those who had fewer pain sites.
Subgroup differences by education occurred in 2 outcomes’ intercept statistic. Patients with only a high school diploma (n = 406) experienced significantly more financial impact than patients with less than a high school diploma or a college degree (β = .753, P = .003). These higher education subgroups experienced significantly higher proximity experience (High School: β = .555, P < .001; College: β = .289, P = .009) compared to the less than high school group. Patients with less than a high school diploma (n = 25) experienced a significant increase in financial threat over time (β = .144, P = .011) which was not experienced by more educated patients (HS: β = −.138, P = .020; College: β = −.147, P = .011). These opposing results suggest that patients with fewer years of education were affected more financially over time, whereas patients with more years of education reported worse outcomes initially.
Nonworking patients (n = 735) reported significantly higher perceived threat (β = .146, P = .033), resource impact (β = .337, P < .001), and news experience (β = .281, P < .001). They also reported significantly less proximity experience (β = −.373, P < .001). Over time, patients who were not working reported a greater decrease in perceived threat (β = −.033, P = .021) while the trend for working patients alone becomes nonsignificant (β = −.015, P = .179). Significant subgroup differences suggest that nonworking patients were more impacted psychologically during the pandemic, and working patients came into more contact with cases.
Discussion
To our knowledge, this study is the first to assess the trajectory of COVID-19-specific experiences among patients with chronic pain over 2 years, and to identify patterns of differential impacts among subgroups. During their initial visit, patients reported low to moderate levels of COVID-associated stressors, as indexed by their scores on COVID-associated perceived threat, financial, resource, and psychological impacts. This finding may be in part due to negative impacts surfacing at a later stage in time, as some evidence from longitudinal case studies suggests worsening rates of psychological distress over time, even after lockdowns are lifted.39 Overall, patients reported below average levels of proximity experience, which is not surprising in light of social distancing and restrictions associated with the initial lockdown and shelter-in-place orders in California.
Patients also reported on their health status during their initial visit. On average, patients reported moderate levels of pain intensity and pain interference, which is inconsistent with research suggesting worsening pain reported by patients 3, 4, 5, 6 and physician observations.40 Pain levels in the current sample were congruent with prior findings among treatment-seeking patients at a tertiary pain clinic,41, 42, 43 suggesting that the pandemic did not result in immediate worsening of pain symptoms. Importantly, patients reported limitations in physical function, as indexed by upper extremity and mobility scores and that are 2 standard deviations below the population mean. This finding is consistent with prior research,3, 4, 5, 6 showing significant reduction in daily physical activity.44 It is likely exacerbated by limited access to many therapies for pain, including acupuncture, massage, physical therapy, rehabilitation therapy, and counseling services.45, 46 Thus, an important consideration for both patients and clinicians would be to potentially address ways to increase physical activities by providing patients with home-based activity or exercises. Additionally, reports of psychosocial factors were consistent with our previous study showing unchanged scores of depression, anxiety, anger, and social isolation after the pandemic.
Over the course of 2 years, mixed effect linear models revealed improvements in pain, psychological health (ie, anxiety, depression, and anger), and physical health (ie, sleep disturbance). This finding is a replication of our prior findings 22 and supports evidence of encouraging resilience among patients receiving treatment for pain conditions in the face of the COVID-19 pandemic. Improvements across some physical and psychosocial domains should be considered with our patients’ specific social context. Namely, most of our patients were married or living together, which may buffer the impacts of social threats that worsen psychosocial function among pain patients.47, 48, 49, 50, 51, 52, 53 Additionally, current findings showed improvement in pain catastrophizing as patients were receiving pain treatments over the course of the pandemic. Our prior findings showed that pain catastrophizing scores were higher in July 2020 (when new COVID-19 cases peaked in San Mateo County and adjacent Santa Clara County),22 suggesting that pain coping strategies may be more context-specific or susceptible to COVID-19 seasonal effects, but are addressable with pain treatments over time.
Subgroup analyses revealed that older age was associated with significantly lower COVID-related stressors. Despite age being a risk factor for acquiring COVID-19,14 it appears that older individuals were adjusting to the COVID-19 experience. In relation to psychological impact, it is possible that older individuals utilize better coping strategies, aligned with theories of socioemotional selectivity 54 and affect regulation.55 Namely, older adults may use more effective emotional regulation to alter their attention, beliefs and environments to maximize positive and dampen negative affect.56, 57, 58, 59, 54, 55 Older adults may be less concerned about financial and resource impacts, especially if they are retired or have stable income. Less financial/resource impact caused by the economic disruptions of COVID-19 is likely to directionally result in lower psychological impact. Finally, trend analyses showed that younger people were initially more affected by the pandemic, but improved equally over time, suggesting a pattern of adaptation.
For race and ethnicity, Asian patients reported a significantly higher perceived threat and financial impact. Hispanic patients reported a significantly higher perceived threat, resource and financial impact during their initial visit, and did not experience the same recovery as non-Hispanic patients in the financial impact domain. These findings are largely consistent with literature suggesting minoritized individuals reporting worse outcomes; physical and psychological health,20 and worse pandemic-related pain.5 Health disparities at large during the pandemic may exacerbate disparities in access to quality pain treatment,21 thus worsening the sense of insecurity related to resources among minoritized groups. Causes of these health disparities are still unclear but may be in part due to increased stress from systemic inequality, low socioeconomic status, and unequal access to healthcare.17, 18 For example, studies assessing the impact of the pandemic in Hispanic and Latino Americans have reported high rates of job loss, likely stemming from a lack of available sick days for essential workers,60 and resulting in increased food and resource insecurity.61 For Asian Americans, a marked increase in anti-Asian racial discrimination in the U.S. during the pandemic,62 with associated decrements in mental and physical well-being,63 may help contextualize the elevated reports of financial impact reported by Asian participants in our study.
For participant sex, females reported higher perceived threat, resource impact, and worse psychological health than males. These findings are consistent with research showing that women are vulnerable for pandemic-related threat,64, 65, 66, 67 which may explain their worsening psychological health during the pandemic. Additionally, research shows pandemic-related workload increases among women, including childcare or homeschooling,68 and an overall increase in the amount of housework.69 Other factors previously associated with worse outcomes among women during the pandemic include lower social stability and maladaptive emotional coping style,70 as well as insecure attachment style among women who gave birth during the pandemic.71 It is also possible that a lack of social access, support, and isolation may worsen psychosocial function 48, 49, 50, 51, 52, 72 disproportionately among women.
As expected, patients who were on disability or had more pain sites reported more financial/resource and psychological impacts of the pandemic compared to those with less disability or pain sites, yet all patients improved over the course of the pandemic. This finding is consistent with prior findings that even patients with moderate pain-related disability saw improvements over the course of the pandemic,73 possibly due to the limitations in activities necessitated by pandemic stay-at-home orders. Also, patients who were not employed reported worse pandemic impact, consistent with research among patients with cancer 74 and multiple sclerosis 75 which found that unemployment, and its associated financial costs, is related to worse quality of life and worse mental health. Among patients who reported that they were not currently working, a greater proportion reported exposure to potential COVID-19 cases, likely reflecting the disproportionate risk conferred to individuals deemed “essential workers” during the pandemic.76 The effects of the pandemic on the global workforce were complex and time-varying: some occupations (eg, in hospitality, tourism) became furloughed nearly overnight, while others (eg, in technology, healthcare) were either boosted or protected from layoffs. Collectively, our subgroup analyses suggest a complex set of relationships and subgroup-specific factors in addition to the multifaceted experience of chronic pain.
Limitations
Several limitations are worth noting. First, we did not correct for multiple testing given the exploratory nature of observational data, which is not meant to establish causality. Second, disparities found in subgroup analyses may be more prevalent because our sample is primarily White and non-Hispanic. Next, cell sizes in some subgroup analyses were small; however, these were exploratory and intended to inform future research. Selection bias is another potential limitation, as it is possible that the patients most severely impacted by the COVID-19 pandemic were not sampled because they did not access care at our clinic. Our study cohorts were recruited from a pain management clinic located in the San Francisco Bay Area. Regional variability in COVID-19 caseloads, mortality, and government-mandated lockdowns may influence the negative impacts of the pandemic on patients with pain. In San Mateo and Santa Clara Counties, there was an early high rate in COVID infections during the pandemic, but considerably fewer COVID-19 deaths compared to many other parts of the United States.77 As such, results may not generalize to other regions of the US or to other countries. Finally, some of the COVID-19-specific measures used in this study had not yet been validated due to the rapid emergence of the pandemic.
Conclusions
Overall, over a 2-year study timeframe, we found that the pandemic did not adversely influence markers of physical and mental health among patients seeking treatment for pain in our clinic. Our study sample also reported small but significant improvements across indices of physical and psychosocial health. These findings highlight the importance of providing pain care over the long course of the pandemic even when the healthcare system was substantially and rapidly changed with social distancing, mask mandates, vaccine availability, limited treatment options, and adoption of telehealth services. Findings also show differential pandemic impacts among marginalized groups, and suggest that more research is needed to better understand the unique and unmet needs of patients who are younger, women, not currently working, on disability, racial minorities, and those who report more widespread pain.
Author Contributions
All authors contributed to the conceptualization, analysis plan, and writing the manuscript. SJ and DY conducted the statistical analyses. All authors approved the final version.
Footnotes
Authors M.Z., S.J., S.A., D.Y., B.D., and S.M. have no conflicts of interest to declare. This work was supported by grant funding from the National Institute of Health: NIDA K23DA047473 (M.Z.) and NIDA K23DA048972 (D.Y.).
B.D. is chief science advisor at Applied VR. She has authored 4 pain treatment books for patients and clinicians and receives royalties for 3. B.D. is the principal investigator for pain research grants and awards from the NIH and the Patient-Centered Research Outcomes Research Institute. B.D. serves on the Board of Directors for the American Academy of Pain Medicine and the Institute for Brain Potential. B.D. is a scientific member of the NIH Interagency Pain Research Coordinating Committee, the Pain Advisory Group of the American Psychological Association, and is a former member of the Centers for Disease Control and Prevention (CDC) Opioid Workgroup (2020–2021).
Address reprint requests to Maisa S. Ziadni, PhD, Stanford School of Medicine, Division of Pain Medicine, Systems Neuroscience and Pain Lab, 1070 Arastradero Road, Suite 200, Palo Alto, CA 94304. E-mail: mziadni@stanford.edu
References
- 1.Weng L.-M., Su X., Wang X.-Q. Pain symptoms in patients with coronavirus disease (COVID-19): A literature review. J Pain Res. 2021;14:147. doi: 10.2147/JPR.S269206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sudre C.H., Murray B., Varsavsky T., Graham M.S., Penfold R.S., Bowyer R.C., Pujol J.C., Klaser K., Antonelli M., Canas L.S. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Consonni M., Telesca A., Grazzi L., Cazzato D., Lauria G. Life with chronic pain during COVID-19 lockdown: The case of patients with small fibre neuropathy and chronic migraine. Neurol Sci. 2021;42(2):389–397. doi: 10.1007/s10072-020-04890-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fallon N., Brown C., Twiddy H., Brian E., Frank B., Nurmikko T., Stancak A. Adverse effects of COVID-19-related lockdown on pain, physical activity and psychological well-being in people with chronic pain. Br J Pain. 2021;15(3):357–368. doi: 10.1177/2049463720973703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hruschak V., Flowers K.M., Azizoddin D.R., Jamison R.N., Edwards R.R., Schreiber K.L. Cross-sectional study of psychosocial and pain-related variables among patients with chronic pain during a time of social distancing imposed by the coronavirus disease 2019 pandemic. Pain. 2021;162(2):619–629. doi: 10.1097/j.pain.0000000000002128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zambelli Z., Fidalgo A.R., Halstead E.J., Dimitriou D. Acute impact of a national lockdown during the COVID-19 pandemic on wellbeing outcomes among individuals with chronic pain. J Health Psychol. 2021;27(5):1099–1110. doi: 10.1177/1359105321995962. 1359105321995962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lacasse A., Pagé M.G., Dassieu L., Sourial N., Janelle-Montcalm A., Dorais M., Nguefack H.L.N., Godbout-Parent M., Hudspith M., Moor G. Impact of the COVID-19 pandemic on the pharmacological, physical, and psychological treatments of pain: Findings from the Chronic Pain & COVID-19 Pan-Canadian Study. Pain Rep. 2021;6(1) doi: 10.1097/PR9.0000000000000891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pagé M.G., Lacasse A., Dassieu L., Hudspith M., Moor G., Sutton K., Thompson J.M., Dorais M., Montcalm A.J., Sourial N. A cross-sectional study of pain status and psychological distress among individuals living with chronic pain: The Chronic Pain & COVID-19 Pan-Canadian Study. Health Promot Chronic Dis Prev Can. 2021;41(5):141–152. doi: 10.24095/hpcdp.41.5.01. [DOI] [PubMed] [Google Scholar]
- 9.Serrano-Ibáñez E.R., Esteve R., Ramírez-Maestre C., Ruiz-Párraga G.T., López-Martínez A.E. Chronic pain in the time of COVID-19: Stress aftermath and central sensitization. Br J Health Psychol. 2021;26(2):544–552. doi: 10.1111/bjhp.12483. [DOI] [PubMed] [Google Scholar]
- 10.Flowers K.M., Colebaugh C.A., Hruschak V., Azizoddin D.R., Meints S.M., Jamison R.N., Edwards R.R., Schreiber K.L. Introversion buffers pandemic-related increases in chronic pain impact. J Pain. 2021;22(5):611–612. [Google Scholar]
- 11.Margolies S.O., Patidar S.M., Chidgey B.A., Goetzinger A., Sanford J.B., Short N.A. Growth in crisis: A mixed methods study of lessons from our patients with chronic pain during the COVID-19 pandemic. J Context Behav Sci. 2021;19:12–16. [Google Scholar]
- 12.Smith B.W., Zautra A.J. Vulnerability and resilience in women with arthritis: Test of a two-factor model. J Consult Clin Psychol. 2008;76(5):799. doi: 10.1037/0022-006X.76.5.799. [DOI] [PubMed] [Google Scholar]
- 13.Sturgeon J.A., Zautra A.J. Resilience: A new paradigm for adaptation to chronic pain. Curr Pain Headache Rep. 2010;14(2):105–112. doi: 10.1007/s11916-010-0095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carethers J.M. Insights into disparities observed with COVID-19. J Intern Med. 2021;289(4):463–473. doi: 10.1111/joim.13199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hooper M.W., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lopez L., Hart L.H., Katz M.H. Racial and ethnic health disparities related to COVID-19. JAMA. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- 17.Chowkwanyun M., Reed A.L., Jr Racial health disparities and Covid-19—Caution and context. N Engl J Med. 2020;383(3):201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 18.Geronimus A.T., Hicken M., Keene D., Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chatkoff D.K., Leonard M.T., Najdi R.R., Cruga B., Forsythe A., Bourgeau C., Easton H. A brief survey of the COVID-19 pandemic's impact on the chronic pain experience. Pain Manag Nurs. 2022;23(1):3–8. doi: 10.1016/j.pmn.2021.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mun C.J., Campbell C.M., McGill L.S., Aaron R.V. The early impact of COVID-19 on chronic pain: A cross-sectional investigation of a large online sample of individuals with chronic pain in the United States, April to May, 2020. Pain Med. 2021;22(2):470–480. doi: 10.1093/pm/pnaa446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dassieu L., Pagé M.G., Lacasse A., Laflamme M., Perron V., Janelle-Montcalm A., Hudspith M., Moor G., Sutton K., Thompson J.M. Chronic pain experience and health inequities during the COVID-19 pandemic in Canada: Qualitative findings from the chronic pain & COVID-19 pan-Canadian study. Int J Equity Health. 2021;20(1):1–13. doi: 10.1186/s12939-021-01496-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ziadni M.S., You D.S., Cramer E.M., Anderson S.R., Hettie G., Darnall B.D., Mackey S.C. The impact of COVID-19 on patients with chronic pain seeking care at a tertiary pain clinic. Sci Rep. 2022;12(1):1–10. doi: 10.1038/s41598-022-10431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Center CoSMJI. Getting vaccinated easier than ever; doses near 900,000; guidance on masks & gatherings: Update on county response to COVID-19 (May 20, 2021). Available at: https://www.smcgov.org/news/getting-vaccinated-easier-ever-doses-near-900000-guidance-masks-gatherings-update Accessed April 24, 2023.
- 24.Diesel J.S.N., Dasgupta S., Kriss J.L., Barry V., Esschert K.V., Whiteman A., Cadwell B.L., Weller D., Qualters J.R., Harris L., Bhatt A., Williams C., Fox L.M., Delman D.M., Black C.L., Barbour K.E. COVID-19 vaccination coverage among adults — United States, December 14, 2020–May 22, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:922–927. doi: 10.15585/mmwr.mm7025e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Health SMC. Vaccination totals & locations data (April 9, 2023). Available at: https://www.smchealth.org/data-dashboard/vaccination-totals-locations-data Accessed April 9, 2023.
- 26.Health CDoP. California Public Health Officials release guidance requiring Californians to wear face coverings in most settings outside the home (June 18, 2020). Available at: https://www.cdph.ca.gov/Programs/OPA/Pages/NR20-128.aspx Accessed April 9, 2023.
- 27.Health SMC. Health orders & updates from the health officer and the SMC (March 30, 2023). Available at: https://www.smchealth.org/health-orders-updates Accessed April 9, 2023.
- 28.Conway L.G., Woodard S.R., Zubrod A., Tiburcio M., Martínez-Vélez N.A., Sorgente A., Lanz M., Serido J., Vosylis R., Fonseca G. How culturally unique are pandemic effects?: Evaluating cultural similarities and differences in effects of age, biological sex, and political beliefs on COVID impacts. Front Psychol. 2022;13(937211):6436. doi: 10.3389/fpsyg.2022.937211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farrar J.T., Young J.P., Jr, LaMoreaux L., Werth J.L., Poole R.M. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 30.Cramer E., Ziadni M., Scherrer K.H., Mackey S., Kao M.-C. CHOIRBM: An R package for exploratory data analysis and interactive visualization of pain patient body map data. PLoS Comput Biol. 2022;18(10) doi: 10.1371/journal.pcbi.1010496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scherrer K.H., Ziadni M.S., Kong J.-T., Sturgeon J.A., Salmasi V., Hong J., Cramer E., Chen A.L., Pacht T., Olson G. Development and validation of the Collaborative Health Outcomes Information Registry body map. Pain Rep. 2021;6(1):1–12. doi: 10.1097/PR9.0000000000000880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan M.J., Bishop S.R., Pivik J. The pain catastrophizing scale: Development and validation. Psychol Assess. 1995;7(4):524–532. [Google Scholar]
- 33.Askew R.L., Cook K.F., Revicki D.A., Cella D., Amtmann D. Evidence from diverse clinical populations supported clinical validity of PROMIS pain interference and pain behavior. J Clin Epidemiol. 2016;73:103–111. doi: 10.1016/j.jclinepi.2015.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buysse D.J., Yu L., Moul D.E., Germain A., Stover A., Dodds N.E., Johnston K.L., Shablesky-Cade M.A., Pilkonis P.A. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33(6):781–792. doi: 10.1093/sleep/33.6.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cella D., Lai J.-S., Jensen S.E., Christodoulou C., Junghaenel D.U., Reeve B.B., Stone A.A. PROMIS fatigue item bank had clinical validity across diverse chronic conditions. J Clin Epidemiol. 2016;73:128–134. doi: 10.1016/j.jclinepi.2015.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cella D., Riley W., Stone A., Rothrock N., Reeve B., Yount S., Amtmann D., Bode R., Buysse D., Choi S. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cook K.F., Jensen S.E., Schalet B.D., Beaumont J.L., Amtmann D., Czajkowski S., Dewalt D.A., Fries J.F., Pilkonis P.A., Reeve B.B. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J Clin Epidemiol. 2016;73:89–102. doi: 10.1016/j.jclinepi.2015.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schalet B.D., Hays R.D., Jensen S.E., Beaumont J.L., Fries J.F., Cella D. Validity of PROMIS physical function measured in diverse clinical samples. J Clin Epidemiol. 2016;73:112–118. doi: 10.1016/j.jclinepi.2015.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patel K., Robertson E., Kwong A.S., Griffith G.J., Willan K., Green M.J., Di Gessa G., Huggins C.F., McElroy E., Thompson E.J. Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Netw Open. 2022;5(4) doi: 10.1001/jamanetworkopen.2022.7629. e227629–e227629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lynch M.E., Williamson O.D., Banfield J.C. COVID-19 impact and response by Canadian pain clinics: A national survey of adult pain clinics. Can J Pain. 2020;4(1):204–209. doi: 10.1080/24740527.2020.1783218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barad M.J., Sturgeon J.A., Hong J., Aggarwal A.K., Mackey S.C. Characterization of chronic overlapping pain conditions in patients with chronic migraine: A CHOIR study. Headache J Head Face Pain. 2021;61(6):872–881. doi: 10.1111/head.14129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gilam G., Cramer E.M., Webber K.A., Ziadni M.S., Kao M.-C., Mackey S.C. Classifying chronic pain using multidimensional pain-agnostic symptom assessments and clustering analysis. Sci Adv. 2021;7(37):eabj0320. doi: 10.1126/sciadv.abj0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taub C.J., Sturgeon J.A., Chahal M.K., Kao M.-C., Mackey S.C., Darnall B.D. Self-reported traumatic etiology of pain and psychological function in tertiary care pain clinic patients: A collaborative health outcomes information registry (CHOIR) study. Scand J Pain. 2020;20(3):499–509. doi: 10.1515/sjpain-2019-0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yamada M., Kimura Y., Ishiyama D., Otobe Y., Suzuki M., Koyama S., Kikuchi T., Kusumi H., Arai H. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: A cross-sectional online survey. J Nutr Health Aging. 2020;24(9):948–950. doi: 10.1007/s12603-020-1501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Blyth F.M., March L.M., Brnabic A.J., Cousins M.J. Chronic pain and frequent use of health care. Pain. 2004;111(1–2):51–58. doi: 10.1016/j.pain.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 46.Braunack-Mayer A.J., Street J.M., Rogers W.A., Givney R., Moss J.R., Hiller J.E. Including the public in pandemic planning: A deliberative approach. BMC Public Health. 2010;10(1):1–9. doi: 10.1186/1471-2458-10-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ashton-James C.E., Anderson S.R., Mackey S.C., Darnall B.D. Beyond pain, distress, and disability: The importance of social outcomes in pain management research and practice. Pain. 2022;163(3):e426–e431. doi: 10.1097/j.pain.0000000000002404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karayannis N.V., Baumann I., Sturgeon J.A., Melloh M., Mackey S.C. The impact of social isolation on pain interference: A longitudinal study. Ann Behav Med. 2019;53(1):65–74. doi: 10.1093/abm/kay017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parrish B.P., Zautra A.J., Davis M.C. The role of positive and negative interpersonal events on daily fatigue in women with fibromyalgia, rheumatoid arthritis, and osteoarthritis. Health Psychol. 2008;27(6):694. doi: 10.1037/0278-6133.27.6.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sturgeon J.A., Carriere J.S., Kao M.-C.J., Rico T., Darnall B.D., Mackey S.C. Social disruption mediates the relationship between perceived injustice and anger in chronic pain: A collaborative health outcomes information registry study. Ann Behav Med. 2016;50(6):802–812. doi: 10.1007/s12160-016-9808-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sturgeon J.A., Dixon E.A., Darnall B.D., Mackey S.C. Contributions of physical function and satisfaction with social roles to emotional distress in chronic pain: A Collaborative Health Outcomes Information Registry (CHOIR) study. Pain. 2015;156(12):2627. doi: 10.1097/j.pain.0000000000000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wolf L.D., Davis M.C. Loneliness, daily pain, and perceptions of interpersonal events in adults with fibromyalgia. Health Psychol. 2014;33(9):929. doi: 10.1037/hea0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ziadni M.S., You D.S., Sturgeon J.A., Mackey S.C., Darnall B.D. Perceived injustice mediates the relationship between perceived childhood neglect and current function in patients with chronic pain: A preliminary pilot study. J Clin Psychol Med Settings. 2021;28(2):349–360. doi: 10.1007/s10880-020-09722-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Löckenhoff C.E., Carstensen L.L. Socioemotional selectivity theory, aging, and health: The increasingly delicate balance between regulating emotions and making tough choices. J Pers. 2004;72(6):1395–1424. doi: 10.1111/j.1467-6494.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- 55.Staudinger UMB S. In: Handbook of Midlife Development. Lachman M.E., editor. John Wiley & Sons, Inc; Hoboken: 2001. A view on midlife development from life-span theory; pp. 3–39. [Google Scholar]
- 56.Carstensen L.L. In: Dweck J.H.C.S., editor. Cambridge University Press; Cambridge: 1998. A life-span approach to social motivation; pp. 341–364. (Motivation and Self-regulation Across the Life Span). [Google Scholar]
- 57.Carstensen L.L., Isaacowitz D.M., Charles S.T. Taking time seriously: A theory of socioemotional selectivity. Am Psychol. 1999;54(3):165. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- 58.Labouvie-Vief G. Ego processes in adulthood: A comment on Jane Loevinger. Psychol Inq. 1993;4(1):34–37. [Google Scholar]
- 59.Labouvie-Vief G., Medler M. Affect optimization and affect complexity: Modes and styles of regulation in adulthood. Psychol Aging. 2002;17(4):571–588. doi: 10.1037//0882-7974.17.4.571. [DOI] [PubMed] [Google Scholar]
- 60.Gonzalez D., Karpman M., Kenney G.M., Zuckerman S. Vol. 13. Urban Institute; Washington, DC: 2020. pp. 1–10. (Hispanic Adults in Families With Noncitizens Disproportionately Feel the Economic Fallout From COVID-19). [Google Scholar]
- 61.Rodriguez C., Crowder S.L., Rodriguez M., Redwine L., Stern M. Food insecurity and the hispanic population during the COVID-19 pandemic. Ecol Food Nutrition. 2021;60(5):548–563. doi: 10.1080/03670244.2021.1974014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cheng H.-L. Xenophobia and racism against Asian Americans during the COVID-19 pandemic: Mental health implications. J Interdiscip Perspect Scholarsh. 2020;3(1):1–4. [Google Scholar]
- 63.Lee S., Waters S.F. Asians and Asian Americans’ experiences of racial discrimination during the COVID-19 pandemic: Impacts on health outcomes and the buffering role of social support. Stigma Health. 2021;6(1):70. [Google Scholar]
- 64.Gázquez Linares J.J., Molero Jurado MdM Martos, Martínez Á., Jiménez-Rodríguez D., Pérez-Fuentes Md.C. The repercussions of perceived threat from COVID-19 on the mental health of actively employed nurses. Int J Mental Health Nurs. 2021;30(3):724–732. doi: 10.1111/inm.12841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lewis A., Duch R. Gender differences in perceived risk of COVID-19. Soc Sci Q. 2021;102(5):2124–2133. doi: 10.1111/ssqu.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nino M., Harris C., Drawve G., Fitzpatrick K.M. Race and ethnicity, gender, and age on perceived threats and fear of COVID-19: Evidence from two national data sources. SSM Popul Health. 2021;13(100717):1–8. doi: 10.1016/j.ssmph.2020.100717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yıldırım M., Güler A. Factor analysis of the COVID-19 Perceived Risk Scale: A preliminary study. Death Stud. 2022;46(5):1065–1072. doi: 10.1080/07481187.2020.1784311. [DOI] [PubMed] [Google Scholar]
- 68.Sevilla A., Smith S. Baby steps: The gender division of childcare during the COVID-19 pandemic. Oxf Rev Econ Policy. 2020;36(Suppl 1):S169–S186. [Google Scholar]
- 69.Hudde A., Hank K., Jacob M. Gender role attitudes cannot explain how British couples responded to increased housework demands during the COVID-19 pandemic. Socius. 2021;7(January-December 2021):1–21. [Google Scholar]
- 70.Di Blasi M., Albano G., Bassi G., Mancinelli E., Giordano C., Mazzeschi C., Pazzagli C., Salcuni S., Lo Coco G., Gelo O.C.G. Factors related to women’s psychological distress during the COVID-19 pandemic: Evidence from a Two-Wave Longitudinal Study. Int J Environ Res Public Health. 2021;18(21):11656. doi: 10.3390/ijerph182111656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ostacoli L., Cosma S., Bevilacqua F., Berchialla P., Bovetti M., Carosso A.R., Malandrone F., Carletto S., Benedetto C. Psychosocial factors associated with postpartum psychological distress during the Covid-19 pandemic: A cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):1–8. doi: 10.1186/s12884-020-03399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ziadni M.S., You D.S., Sturgeon J.A., Mackey S.C., Darnall B.D. Perceived injustice mediates the relationship between perceived childhood neglect and current function in patients with chronic pain: A preliminary pilot study. J Clin Psychol Med Settings. 2020:1–12. doi: 10.1007/s10880-020-09722-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Reed D.E., Cobos B., Lehinger E.A., Nabity P.S., Vail K.E., III, McGeary D.D. Pain-related disability, PTSD symptoms, and mood among a comorbid chronic pain and PTSD sample prior to and during the COVID-19 pandemic. J Health Psychol. 2022;27(6):1515–1532. doi: 10.1177/13591053211051821. [DOI] [PubMed] [Google Scholar]
- 74.Guo Y., Shen M., Zhang X., Xiao Y., Zhao S., Yin M., Bu W., Wang Y., Chen X., Su J. Unemployment and health-related quality of life in melanoma patients during the COVID-19 pandemic. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.630620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Motolese F., Rossi M., Albergo G., Stelitano D., Villanova M., Di Lazzaro V., Capone F. The psychological impact of COVID-19 pandemic on people with multiple sclerosis. Front Neurol. 2020;11 doi: 10.3389/fneur.2020.580507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lancet EBoT The plight of essential workers during the COVID-19 pandemic. Lancet. 2020;395(10237) doi: 10.1016/S0140-6736(20)31200-9. 1587–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.JHU. Coronavirus Resource Center: California State Overview (March 10, 2023). Available at: https://coronavirus.jhu.edu/region/us/california Accessed April 9, 2023.