Abstract
Objectives:
Evidence suggests a cross-sectional association between personality traits and suicidal ideation in LLD. Yet, it’s unclear how personality may influence suicidal ideation over time in LLD, or whether such an association would be moderated by psychosocial and biological individual differences. The present study had three aims: 1) to examine whether personality traits increase suicidal ideation in LLD over time, 2) to understand whether this relationship is influenced by subjective social support, and 3) to determine whether the potential relationship between social support, personality, and suicidal ideation is different for men and women.
Design:
Participants were enrolled in the Duke University Neurocognitive Outcomes of Depression in the Elderly (NCODE), a longitudinal investigation of the predictors of poor illness course in LLD. Patients were initially enrolled in the NCODE study between December 1994 and June 2000 and were followed for an average of six years.
Setting:
NCODE operates in a naturalistic treatment milieu.
Participants:
112 participants aged 60 and older with a current diagnosis of major depressive disorder.
Measurements:
Annual assessments of depression, suicidal ideation, and social support (measured with the Duke Social Support Index). Participants also completed the NEO Personality Inventory-Revised (NEO-PI-R) providing measures of the five major personality dimensions (neuroticism, extraversion, openness, conscientiousness, agreeableness).
Results:
Univariate logistic generalized linear mixed modeling (GLMM) analyses revealed that higher levels of depression at baseline, less subjective social support, higher neuroticism, and lower extraversion were significantly associated with an increased likelihood of suicidal ideation over time. While the relationship between these dimensions and suicidal ideation were no longer significant in multivariate analyses, there was a significant moderating effect of social support on the association between suicidal ideation and certain neuroticism and extraversion personality facets. Decreased subjective social support was associated with an increased likelihood of suicidal ideation in LLD patients with high (but not low) impulsiveness and low (but not high) gregariousness and positive emotions. Across all models, social support was beneficial to women, but not men, in decreasing the likelihood of future suicidal ideation.
Conclusions:
Changes in social support may contribute to suicidal ideation in older depressed adults with certain personality traits. Irrespective of personality traits, changes in social support had a significant effect on the suicidal ideation of women but not men. These relationships were apparent even when controlling for depression severity, age, and history of suicide attempt.
Introduction
Suicidal ideation increases the risk of suicide attempt in some older adults. One study found that 53% of older adults who died by suicide had reported either passive (e.g., life-weariness or death ideation) or more active (e.g., thoughts of taking one’s own life) suicidal ideation in the year before death (1). It is troubling to further consider that passive ideation – potentially ubiquitous among older adults with major depression or late-life depression (LLD) (2) – may convey an increased likelihood of future suicide in the absence of more active suicidal ideation (3). Both clinical (4) and epidemiological (5) studies suggest that passive ideators do not differ from active ideators in terms of prior number or the future likelihood of suicide attempts. Understanding longitudinal contributors to passive and active suicidal ideation in LLD may help inform suicide prevention strategies for older adults.
Three studies have examined the cross-sectional association between suicidal ideation and personality traits in older adults with LLD (see Szucs et al. (6) for a recent review). These studies have measured personality with the main dimensions of the Five Factor Model of Personality (7) (neuroticism, extraversion, openness to experience, conscientiousness, and agreeableness). Compared to LLD patients without suicidal ideation, two studies found that LLD patients with suicidal ideation reported higher neuroticism (reflecting emotional instability and proneness to psychological distress) and openness (reflecting attentiveness to inner feelings, curiosity, and preference for variety)(8, 9), with one study finding evidence of reduced agreeableness (reflecting egocentricity, guardedness, cynicism) in ideators compared to non-ideators (9). By contrast, LLD ideators and non-ideators did not differ in respect to conscientiousness (where high scoring individuals are confident, diligent, well-organized, and deliberate) and extraversion (where high scores reflect preferences for social interaction and the tendency to experience positive emotion) (8, 9). However, the extraversion facets of warmth and positive emotions were associated with less suicidal ideation (10) and depressive symptoms (11) in LLD.
Subjective satisfaction with available social support is an interpersonal state that has been repeatedly associated with decreased suicidal ideation in older adults (12–14). Three lines of evidence suggest social support may interact with personality dimensions, particularly neuroticism and extraversion, to moderate suicidal ideation in LLD. First, neuroticism and extraversion are associated with longitudinal changes to social support and depression symptoms in LLD (15, 16). Second, subjective social support was negatively correlated with depression in elders with low neuroticism, whereas elders high in this trait did not experience a reduction in depression as subjective social support increased (17). Third, lower subjective social support, subjective sense of being a burden, and diminished fear of death were associated with a history of suicide attempts in younger psychiatric outpatients high in the neuroticism facet of impulsiveness, but no such relationship between interpersonal states and suicide attempts were found in patients with low impulsiveness (18). The potential complex interactions between subjective social support, neuroticism, and extraversion on suicidal ideation in LLD have not been tested.
The association between personality, subjective social support, and suicidal ideation may be different for men and women. The perception of diminished social support is a predictor of suicidal ideation in women but not men (19). This is consistent with the notion that women place greater value on social connectedness (20) and score higher on extraversion and agreeableness than men (7). Furthermore, high extraversion and low neuroticism is correlated with social support in women but not men (21). While neuroticism generally seems to increase the probability of major depression, this relationship is stronger for women compared to men (22), and potentially mediated by different biological substrates (23).
In the current study, we hypothesized that LLD patients with high neuroticism and high openness would have an increased likelihood of suicidal ideation over time. By contrast, patients high in agreeableness and extraversion would have a reduced likelihood of suicidal ideation over time. We were less clear about the longitudinal main effects of conscientiousness, but included this dimension in an attempt to comprehensively examine personality and suicidal ideation in LLD. We further hypothesized that the relationship between certain personality dimensions and suicidal ideation would be moderated by changes to subjective social support. Specifically, increased social support would decrease the likelihood of suicidal ideation in patients with high neuroticism and extraversion, but no such relationship would be found in patients low in these dimensions. We also explored the relationship between suicidal ideation, social support, and individual facets of neuroticism and extraversion considering specific facets of these dimensions have been previously linked to suicidal ideation. Finally, we explored whether the potential effect of personality dimensions and social support on suicidal ideation would be different for men and women.
Methods
Participants
Participants age 59+ were enrolled in the Neurocognitive Outcomes of Depression in the Elderly (NCODE) study at Duke University Medical Center. The present study includes a subset of participants who agreed to participate in an ancillary study of personality between February 1998 and February 2001. These participants were initially enrolled in the NCODE study between December 1994 and June 2000. Depending on when each participant entered the study and when they completed the NEO-PI-R, longitudinal depression and social support data could predate personality assessment by between 0 and 63 months. Personality traits are therefore treated as a stable retrospective measure in this study and are used in the analysis of suicidal ideation data potentially collected earlier. Participants met Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria for a current episode of major depressive disorder as established by a geriatric psychiatrist. Exclusion criteria included the presence of another major psychiatric illness (except comorbid anxiety disorders), dementia at baseline, and other neurological illnesses. All participants provided informed consent before beginning any study procedures. The NCODE study was approved by the Duke University Health System Institutional Review Board.
Longitudinal Assessment
The NCODE study used a naturalistic treatment approach based on treatment guidelines established by the Duke Affective Disorders Program. Treatment modalities available included antidepressant medications, electro-convulsive therapy, and individual and group cognitive-behavioral psychotherapy. Patients’ depressive symptoms (including suicidal ideation) were evaluated when clinically indicated, and at least every three months while they were in the study. However, for the current study, we only included annual depression evaluations so as to match the timing of other annual assessments. The current study includes all depressed participants’ assessment within 10 years from enrollment.
Measurements
Personality Assessment.
The 240 item NEO-PI-R derives five dimensions of personality traits including neuroticism, extraversion, openness, conscientiousness, and agreeableness. Each factor has six facets. T scores were used in the analyses of main personality effects and were derived from normative transformations of raw scores provided in the NEO-PI-R manual (7). Whereas there are no scientifically validated thresholds for personality scales, we used a T-score of ≥ 55 to define high levels of personality traits. In older adults, this cut-score has been associated with a greater likelihood of cognitive decline and poor depression treatment response (15), as well as an increased likelihood of incident depression and mortality (24, 25).
Suicidal Ideation.
Suicidal ideation was assessed using the suicidal thoughts item (Item 10) from the Montgomery Asberg Depression Rating Scale or MADRS (26). Geriatric psychiatrists assessed participants’ level of suicidal thoughts over the past seven days on a scale ranging from 0 to 6. The following anchors were provided: 0 (Enjoys life or takes it as it comes), 2 (Weary of life; only fleeting suicidal thoughts), 4 (Probably better off dead; suicidal thoughts are common, and suicide is considered as a possible solution, but without specific plans or intention), and 6 (Explicit plans for suicide when there is an opportunity; active preparations for suicide). Ratings of ≥ 2 were used to define the presence of suicidal ideation.
Depression Severity.
The remaining MADRS items were summed to create a total depression score ranging from 0 to 54. Typically, scores of 0–6 on the MADRS indicate remitted depression, 7–19 mild depression, 20–34 moderate depression, and 35–60 severe depression.
Social Support:
Data on social support were collected annually. The perceived social support scale included 10-items derived from a prior factor analysis of the 35-item Duke Social Support Index (27, 28). Individual items reflect social isolation, the extent to which patient feels listened to, and relationship satisfaction. Higher scores indicate greater perceived social support (scales ranges from 0–30).
Statistical Analyses
For our main analyses, separate generalized linear mixed models (GLMM) were used to examine the relationships between the five major personality dimensions, perceived social support, sex, and suicidal ideation over 10 years while adjusting for potential confounders. Here, the dependent variable is presence vs. absence of suicide ideation (presence defined as MADRS ≥ 2) at any follow-up time point in the 10 year span. All logistic GLMM models included random intercept and time (since first evaluation in years). Each predictor of interest was first examined in separate logistic GLMMs. Next, the effect of each personality dimension was evaluated in separate logistic GLMM with main effects of personality, time, sex, and perceived social support (a time-varying variable), and two-way interactions of 1) perceived social support by high-low personality dimension scores and 2) perceived social support by sex. Additionally, baseline age, marital status, depression severity, and history of suicide attempt were included as covariates. Other two-way and higher order interactions were also considered. Multivariate analyses were then conducted on the facets of neuroticism and extraversion. For these analyses, whenever a specific personality facet was in the GLMM, the global personality dimension score was calculated as the total dimension score minus the items of the facet specific to that model. Inclusion of a global dimension score in the model allowed us to compare effects of specific facets with the overall dimension. As a sensitively analysis, we conducted analyses using both continuous and high/low personality and found that the results were robust. Differences where a dichotomized predictor was not significant while the same continuous predictor was significant was only observed on one occasion as described below. SAS 9.4 was used for all analyses.
Results
Table 1 includes demographic and clinical characteristics of 248 depressed NCODE participants recruited between February 1998 and 2001 who did and did not participate in the current study. The current sample includes NEO-PI-R completers (n=112). NCODE patients who completed and refused to complete (n=22) the NEO-PI-R did not significantly differ from one another in demographic and clinical characteristics (see Table 1). Reasons for refusal to complete the NEO-PI-R were not recorded. Furthermore, of the 248 NCODE subjects recruited between 1998–2001, reasons were not recorded as to why the remaining 114 subjects were not approached to complete the NEO-PI-R. Compared to those who completed the NEO (n=112), those who were not asked to complete the NEO (n=114) were older, less educated, and scored lower on the MMSE. There was a larger proportion of women, widowers, and Black elders in the latter group as well. In terms of longitudinal data, the NEO-PI-R completers were administered an average of 6.8 (SD = 2.8) MADRS and subjective social support assessments over a mean of 6.2 years (SD = 3.0). Participants were administered their initial MADRS an average of 19.6 months (SD = 14.5) before completing the NEO-PI-R, with 50% of participants completing the MADRS between six and 30 months.
Table 1.
Baseline Demographic and Clinical Characteristics of Depressed NCODE Participants Recruited Between 1998 and 2001 Who Did and Did Not Complete the NEO-PI-R.
| Variable | NEO-PI-R Completers (n=112) | Refused NEO-PI-R (n=22) | Not Approached with NEO-PI-R (n=114) | Results of 3 group ANOVA / χ2 / Exact test |
|---|---|---|---|---|
| Age*** | 67.8 (6.1) [59–83] | 69.2 (7.3) [60–81] | 72.4 (8.2) [59–91] | Welch F(2.0,58.3) = 11.68, p <.0001 |
| Education** | 13.9 (2.7) [7–17] | 13.0 (2.51) [7–17] | 12.6 (2.9) [11–19] | Welch F(2.0,62.9) = 5.06, p = .0092 |
| Gender* | 62% Female | 68% Female | 79% Female | χ2 (2) = 8.16, p = 0.0169 |
| Race* | 89.3% White 4.5% Black 0.9% Asian 5.4% Other |
86.4% White 14.0% Black 0% Asian 0% Other |
76.3% White 16.7% Black 2.6% Asian 4.4%Other |
Exact test, 0.0493 |
| Marital Status ** | 61.6% Married 3.6% Separated 17.0% Divorced 17.0% Widowed 0.9% Never married |
50.0% Married 4.6% Separated 9.1% Divorced 31.8% Widowed 4.6% Never married |
46.5% Married 3.5% Separated 7.9% Divorced 39.5% Widowed 2.6% Never married |
Exact test, 0.0070 |
| MMSE *** | 28.2 (2.6) [11–30] | 27.7 (2.0) [22–30] | 26.6 (3.6) [9–30] | F(2,245) = 8.63, p = 0.0002 |
| NEO-PI-R T scores | Mean (SD) [% > 55] | - | - | - |
| Neuroticism | 54.7 (11.7) [44%] | - | - | - |
| Extraversion | 45.2 (9.4) [13%] | - | - | - |
| Openness | 45.6 (11.4) [24%] | - | - | - |
| Agreeableness | 54.3 (9.2) [46%] | - | - | - |
| Conscientiousness | 43.9 (11.4) [18%] | - | - | - |
| MADRS Total | 26.9 (6.9) [13–50] | 28.4 (9.3) [16–53] | 28.6 (8.3) [10–52] | F(2,245) = 1.41, p = 0.2453 |
| Suicidal Ideation (% ≥ 2 on MADRS #10) | 48.2% | 36.4% | 50.9% | χ2 (2) = 1.56, p = 0.4589 |
| History of Suicide Attempt | 11.6% | 0% | 7.0% | χ2 (2) = 3.77, p = 0.1519 |
| Perceived Social Support (/30) | 23.7 (3.8) [11–28] | 22.3 (4.5) [12–28] | 22.6 (4.2) [11–28] | F(2,238) = 2.38, p = 0.0948 |
Note. Data are means, (standard deviation), and [range] unless otherwise noted; MADRS = Montgomery-Asberg Depression Rating Scale, MMSE = Mini-Mental State Exam.
p < .05,
p < .01
p < .001 post-hoc comparison of NEO-PI-R completers with those patients not approached with NEO-PI-R. Post-hoc comparisons did not reveal significant group differences between NEO-PI-R completers and those who refused NEO-PI-R, or between those who refused NEO-PI-R and those who were not approached with NEO-PI-R.
Suicidal ideation was present in 56% of the current sample at baseline. Of those patients reporting suicidal ideation at baseline, 76% (n=48) reported having fleeting life weariness or less severe thoughts of suicidal ideation on MADRS Item 10 (i.e., a score of two or three). The frequent occurrence of suicidal ideation, but without a plan or intent, was reported in 22% (n=14) of subjects (i.e., a score of four or five on MARDS Item 10). One subject had made explicit plans or active preparations for suicide at baseline (a score of six on Item 10). Twelve percent of the entire sample (n=13) had a history of attempted suicide. Attempters versus non-attempters did not significantly differ on reported suicidal ideation at baseline (69% of attempters and 55% of non-attempters had at least fleeting suicidal ideation on MADRS Item 10; χ2 (df = 1) = 1.01, p = 0.31). Attempters did report decreased social support and higher neuroticism at baseline compared to non-attempters (Social Support; attempters M = 20.92 ± 4.39, non-attempters M = 24.02 ± 3.55, t (df = 108) = −2.87, p < .05; Neuroticism T Score; attempters M = 60.98 ± 11.53, non-attempters M = 53.89 ± 11.48, t (df = 110) = 2.09, p < .05). Attempters and non-attempters did not significantly differ on the other four personality dimensions at baseline (results not shown).
Univariate Analyses
Univariate logistic GLMM analyses revealed that higher levels of depression at baseline, less subjective social support, and higher neuroticism were significantly associated with an increased likelihood of suicidal ideation over time (see Table 2). Lower continuous measured extraversion – but not low extraversion defined as T <=55 - was also significantly associated with an increased likelihood of suicidal ideation. Longer years in the study (presumably reflective of treatment) was also significantly associated with a decreased likelihood of suicidal ideation over time. Age, openness, agreeableness, and conscientiousness were not associated with the likelihood of suicidal ideation in univariate models. There was a non-significant association for women to experience an increased likelihood of suicidal ideation when compared to men, and patients with a history of suicide attempt to experience an increased likelihood of suicidal ideation when compared to those without an attempt history.
Table 2.
Univariate Predictors of Suicidal Ideation Over Time.
| Predictor | Suicidal Ideation | |
|---|---|---|
| Odds Ratio (95% CI) | Type III F Test | |
| Time | 0.582 (0.501, 0.676) | F(1,110) = 51.36, p < 0.001 |
| Age | 0.999 (0.947, 1.054) | F(1,542) = 1.04, p = 0.309 |
| Gender | 1.952 (0.998, 3.817) | F(1,542) = 3.25, p = 0.072 |
| Depression | 1.073 (1.018, 1.130) | F(1,542) = 7.69, p = 0.006 |
| History Suicide Attempt | 2.609 (0.979, 6.953) | F(1,542) = 3.69, p = 0.055 |
| Subjective Social Support | 0.771 (0.713, 0.834) | F(1,518) = 27.42, p < 0.001 |
| Neuroticism Continuous T Neuroticism T <= 55 |
1.037 (1.008, 1.066) 0.423 (0.221, 0.807) |
F(1,542) = 6.54, p =
0.011 F(1,542) = 6.85, p = 0.009 |
| Extraversion Continuous T Extraversion T <= 55 |
0.945 (0.912, 0.978) 2.013 (0.721, 5.616) |
F(1,542) = 10.44, p =
0.001 F(1,542) = 1.79, p = 0.181 |
| Openness Continuous T Openness T <= 55 |
0.984 (0.956, 1.013) 1.107 (0.513, 2.390) |
F(1,542) = 1.22, p =
0.270 F(1,542) = 0.07, p = 0.795 |
| Agreeableness Continuous
T Agreeableness T <= 55 |
0.988 (0.954, 1.024) 0.885 (0.460, 1.704) |
F(1,542) = 0.42, p =
0.515 F(1,542) = 0.13, p = 0.715 |
| Conscientiousness Continuous
T Conscientiousness T <= 55 |
0.993 (0.965, 1.021) 1.122 (0.478, 2.635) |
F(1,542) = 0.24, p =
0.625 F(1,542) = 0.07, p = 0.791 |
Note. 112 subjects, who underwent annual assessments upwards of 10 years since first depression evaluation (average 6.2 ± 3.0 assessments). Analyses included logistic generalized linear mixed models (GLMM) with random intercept and time.
Multivariate Analyses
The three-way interaction term of personality dimension, subjective social support, and sex was not statistically significant (for any of the major dimensions) and was removed from the final set of GLMM multivariate models. Likewise, the two-way interactions of sex by personality dimension, time by personality dimension, and time by sex, were also not statistically significant in any model, and were removed. Marital status did not affect suicide ideation, either on its own or in any two-way interaction combination, and was removed. The final logistic GLMM models therefore included the time-invariant predictors of sex, baseline age, baseline depression severity, baseline history of suicide attempt, personality dimension, as well as the time varying subjective social support predictor, and the two-way interactions of subjective social support by personality dimension and subjective social support by sex. Analyses using continuous and dichotomized personality dimension scores were not significantly different and only the analyses with dichotomized variables are presented below.
Contrary to our hypotheses, in the separate multivariate logistic GLMM models: 1) none of the five personality dimensions demonstrated a statistically significant main effect on the likelihood of suicidal ideation and 2) subjective social support did not moderate the effect of any of the five personality dimensions on the likelihood of suicidal ideation (see Table 3). By contrast, the interaction of social support and sex was a significant predictor in each of the five models. Baseline depression severity, but not age or history of suicide attempt, was also significantly associated with an increased likelihood of suicidal ideation across the majority of the final logistic GLMM models (with the exception of the model containing openness).
Table 3.
Multivariate Associations Between Five-Factor Personality Dimensions and Suicidal Ideation Over Time.
| Neuroticism | Extraversion | Openness | Agreeableness | Conscientiousness | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | Type III F Test | OR (95% CI) | Type III F Test | OR (95% CI) | Type III F Test | OR (95% CI) | Type III F Test | OR (95% CI) | Type III F Test | |
| Age | 0.961 (0.909, 1.015) | F = 2.04, p = 0.1538 |
0.962 (0.911, 1.017) | F = 1.87, p = 0.1718 |
0.961 (0.910, 1.016) | F = 1.94, p = 0.1645 |
0.965 (0.912, 1.022) | F = 1.51, p = 0.2198 |
0.964 (0.912, 1.019) | F = 1.65, p = 0.1993 |
| Sex | - | F = 6.84, p = 0.0092 |
- | F = 5.52, p = 0.0191 |
- | F = 6.79, p = 0.0094 |
- | F = 6.76, p = 0.0096 |
- | F = 6.49, p = 0.0111 |
| History Suicide Attempt | 0.972 (0.337, 2.804) | F = 0.00, p = 0.9586 |
0.855 (0.305, 2.397) | F = 0.09, p = 0.7650 |
0.809 (0.290, 2.257) | F = 0.16, p = 0.6850 |
0.738 (0.256, 2.122) | F = 0.32, p = 0.5721 |
0.809 (0.289, 2.263) | F = 0.16, p = 0.6856 |
| Depression Baseline | 1.081 (1.023, 1.142) | F = 7.81, p = 0.0054 |
1.068 (1.011, 1.127) | F = 5.65, p = 0.0178 |
1.067 (1.010, 1.127) | F = 5.43, p = 0.0202 |
1.066 (1.009, 1.127) | F = 5.25, p = 0.0223 |
1.074 (1.016, 1.135) | F = 6.40, p = 0.0117 |
| Personality Dimension (T > 55) | - | F = 0.06, p = 0.8017 |
- | F = 1.37, p = 0.2423 |
- | F = 0.11, p = 0.7434 |
- | F = 1.71, p = 0.1909 |
- | F = 0.01, p = 0.9395 |
| Time | 0.579 (0.489, 0.686) | F = 40.75, p < 0.0001 |
0.565 (0.473, 0.675) | F = 40.64, p < 0.0001 |
0.571 (0.479, 0.681) | F = 39.97, p < 0.0001 |
0.575 (0.483, 0.684) | F = 39.90, p < 0.0001 |
0.568 (0.476, 0.678) | F = 40.05, p < 0.0001 |
| Social Support | - | F = 9.67, p = 0.0020 |
- | F=1.06, p = 0.3035 |
- | F = 8.73, p = 0.0033 |
- | F = 9.92, p = 0.0017 |
- | F = 8.93, p = 0.0029 |
| Social Support by Low (L) and High (H) Personality Dimension | L: 0.861 (0.754, 0.982) H: 0.863 (0.761, 0.979) |
F = 0.00, p = 0.9750 |
L: 0.834 (0.754, 0.922) H: 1.008 (0.735, 1.382) |
F = 1.26, p = 0.261 |
L: 0.842 (0.758, 0.935) H: 0.858 (0.717, 1.027) |
F = 0.04, p = 0.8511 |
L: 0.798 (0.707, 0.901) H: 0.912 (0.789, 1.054) |
F = 2.12, p = 0.1461 |
L: 0.851 (0.767, 0.945) H: 0.840 (0.696, 1.013) |
F = 0.02, p = 0.8966 |
| Social Support by Sex (W=Women, M=Men) | W: 0.772 (0.696, 0.857) M: 0.962 (0.825, 1.122) |
F = 5.50, p = 0.0194 |
W: 0.829 (0.694, 0.990) M: 1.014 (0.827, 1.422) |
F = 4.42, p = 0.0359 |
W: 0.759 (0.681, 0.846) M: 0.952 (0.801, 1.131) |
F = 5.48, p = 0.0196 |
W: 0.761 (0.686, 0.845) M: 0.956 (0.811, 1.127) |
F = 5.48, p = 0.0196 |
W: 0.759 (0.672, 0.857) M: 0.941 (0.800, 1.109) |
F = 5.22, p = 0.0227 |
Note. 112 subjects, who underwent annual assessments upwards of 10 years since first depression evaluation (average 6.2 ± 3.0 assessments). Analyses included logistic generalized linear mixed models (GLMM) with random intercept and time. F test df = 516 or 515 for main predictors and interactions, df = 110 for linear time. The dependent variable is the presence vs. absence of suicidal ideation at any follow-up point in the 10 year span. Odds Ratios of individual terms included in interactions are not included.
Examination of the multivariate analyses at the facet level for neuroticism and extraversion revealed a moderating effect of social support on one facet of neuroticism and two facets of extraversion (see Table 4). When adjusting for age, history of attempted suicide, depression severity, and other facets of neuroticism, decreased subjective social support was associated with an increased likelihood of suicidal ideation in LLD patients high in the neuroticism impulsiveness facet, but changes in social support had no effect on the likelihood of suicidal ideation in those patients low in impulsiveness. When adjusting for age, history of attempted suicide, depression severity, and other facets of extraversion, decreased subjective social support increased the likelihood of suicidal ideation in LLD patients low in the gregariousness and positive emotion facets, but changes in social support had no effect on the likelihood of suicidal ideation in those patients high in these facets. Figure 1 illustrates the association between social support, suicidal ideation, and the facets of impulsiveness (Figure 1a), gregariousness (Figure 1b), and positive emotions (Figure 1c). For example, as seen in Figure 1a, a moderately depressed patient with low social support and high impulsiveness has almost double the probability of experiencing suicidal ideation compared to a moderately depressed patient with low social support and low impulsiveness. Furthermore, as social support increases and approaches the average levels for this sample (e.g., score of 23 on the Duke Social Support Index), the probability of suicidal ideation in patients with high impulsiveness decreases and is roughly equivalent to that of patients with low impulsiveness. None of the other neuroticism and extraversion facets demonstrated a statistically significant association with the likelihood of suicidal ideation either independently or through an interaction with social support (see supplementary tables). The interaction of social support and sex remained a significant predictor in each of the separate facet models.
Table 4.
Multivariate Associations Between Facets of Neuroticism and Extraversion and Suicidal Ideation Over Time.
| Predictors | Impulsiveness (Neuroticism) | Gregariousness (Extraversion) | Positive Emotions (Extraversion) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | Type III F Test | OR (95% CI) | Type III F Test | OR (95% CI) | Type III F Test | |
| Age | 0.958 (0.907, 1.012) | F= 2.38, p = 0.124 |
0.969 (0.914, 1.026) | F= 1.19, p = 0.276 |
0.965 (0.912, 1.022) | F= 1.50, p = 0.222 |
| Sex | - | F= 6.95, p = 0.009 |
- | F= 4.78, p = 0.029 |
- | F= 5.32, p = 0.021 |
| History Suicide Attempt | 0.747 (0.262, 2.128) | F= 0.30, p = 0.584 |
0.887 (0.312, 2.525) | F= 0.05, p = 0.822 |
0.823 (0.287, 2.358) | F= 0.13, p = 0.717 |
| Depression Baseline | 1.073 (1.017, 1.132) | F= 6.61, p = 0.010 |
1.073 (1.015, 1.133) | F= 6.27, p = 0.013 |
1.073 (1.014, 1.135) | F= 5.95, p = 0.015 |
| Global Personality Dimension^ | 1.015 (0.997, 1.034) | F= 2.57, p = 0.110 |
0.994 (0.968, 1.021) | F= 0.20, p = 0.652 |
0.995 (0.967, 1.023) | F= 0.15, p = 0.701 |
| Personality Facet (T ≥ 55) | - | F= 2.99, p = 0.084 |
- | F= 3.80, p = 0.052 |
- | F= 3.92, p = 0.048 |
| Time | 0.549 (0.455, 0.662) | F= 40.09, p <.001 |
0.560 (0.468, 0.671) | F= 40.78, p <.001 |
0.569 (0.477, 0.678) | F= 40.42, p <.001 |
| Social Support | - | F= 10.23, p = 0.002 |
- | F= 3.71, p = 0.055 |
- | F= 0.27, p = 0.602 |
| F= 4.37, p = 0.037 |
F= 4.02, p = 0.045 |
F = 4.14, p = 0.042 |
||||
| Social Support Increase / High Facet | 0.767 (0.657, 0.894) | 0.998 (0.830, 1.200) | 1.062 (0.843, 1.486) | |||
| F= 5.88, p = 0.016 |
F= 3.92, p = 0.048 |
F= 4.10, p = 0.044 |
||||
| Social Support* Increase / Men | 0.948 (0.809, 1.110) | 0.987 (0.831, 1.172) | 1.062 (0.869, 1.299) | |||
Notes. 112 subjects, who underwent annual assessments upwards of 10 years since first depression evaluation (average 6.2 ± 3.0 assessments). Analyses included logistic generalized linear mixed models (GLMM) with random intercept and time. The dependent variable is the presence vs. absence of suicidal ideation at any follow-up point in the 10 year span. Odds Ratios of individual terms included in interactions are not included.
Global Personality Dimension = total dimension score – facet items specific to that analysis (i.e., for impulsiveness analysis, global neuroticism = total neuroticism items – 8 impulsiveness subscale items). F test df = 516 for main predictors and interactions in the impulsiveness model, df = 515 for main predictors and interactions in the extraversion facet models, df = 110 for linear time.
Figure 1.
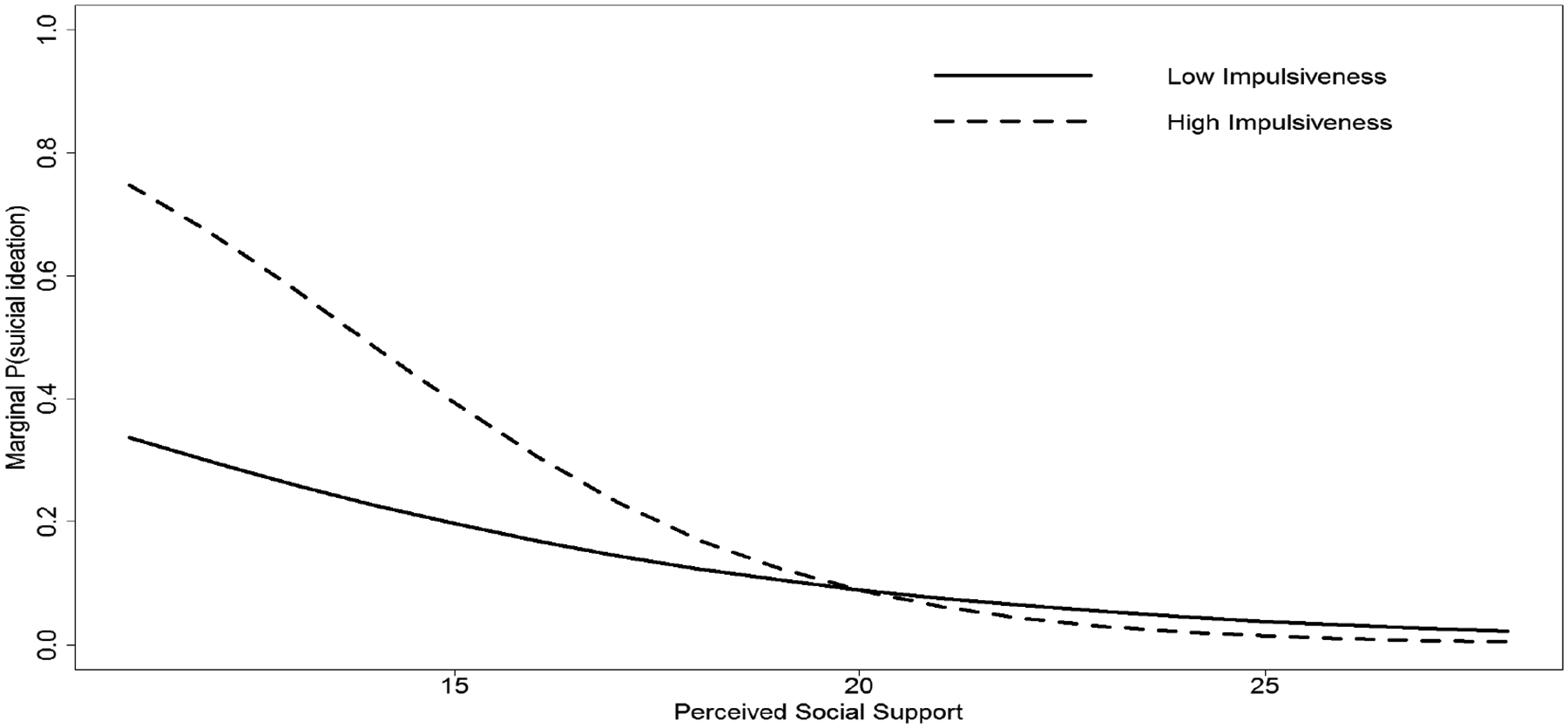
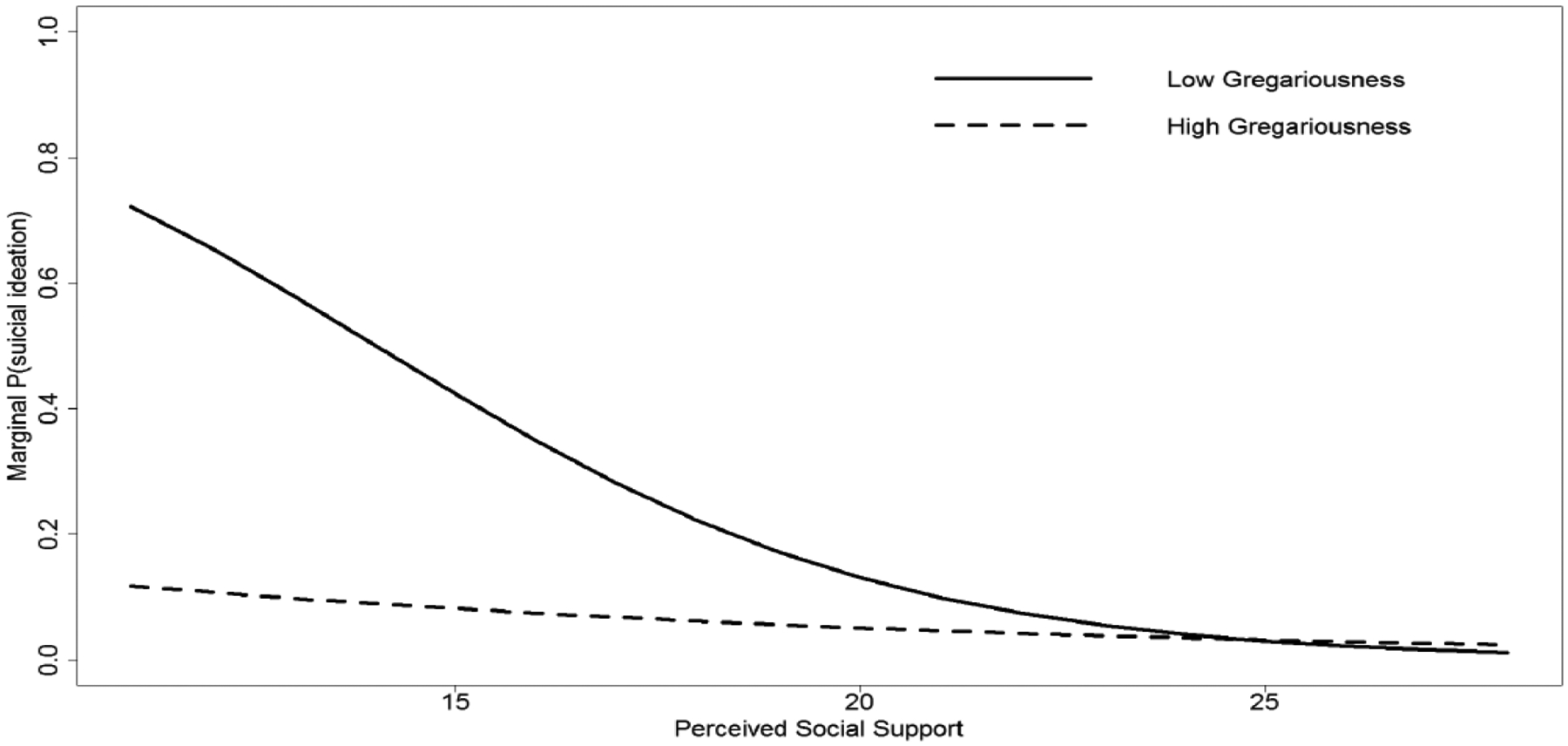
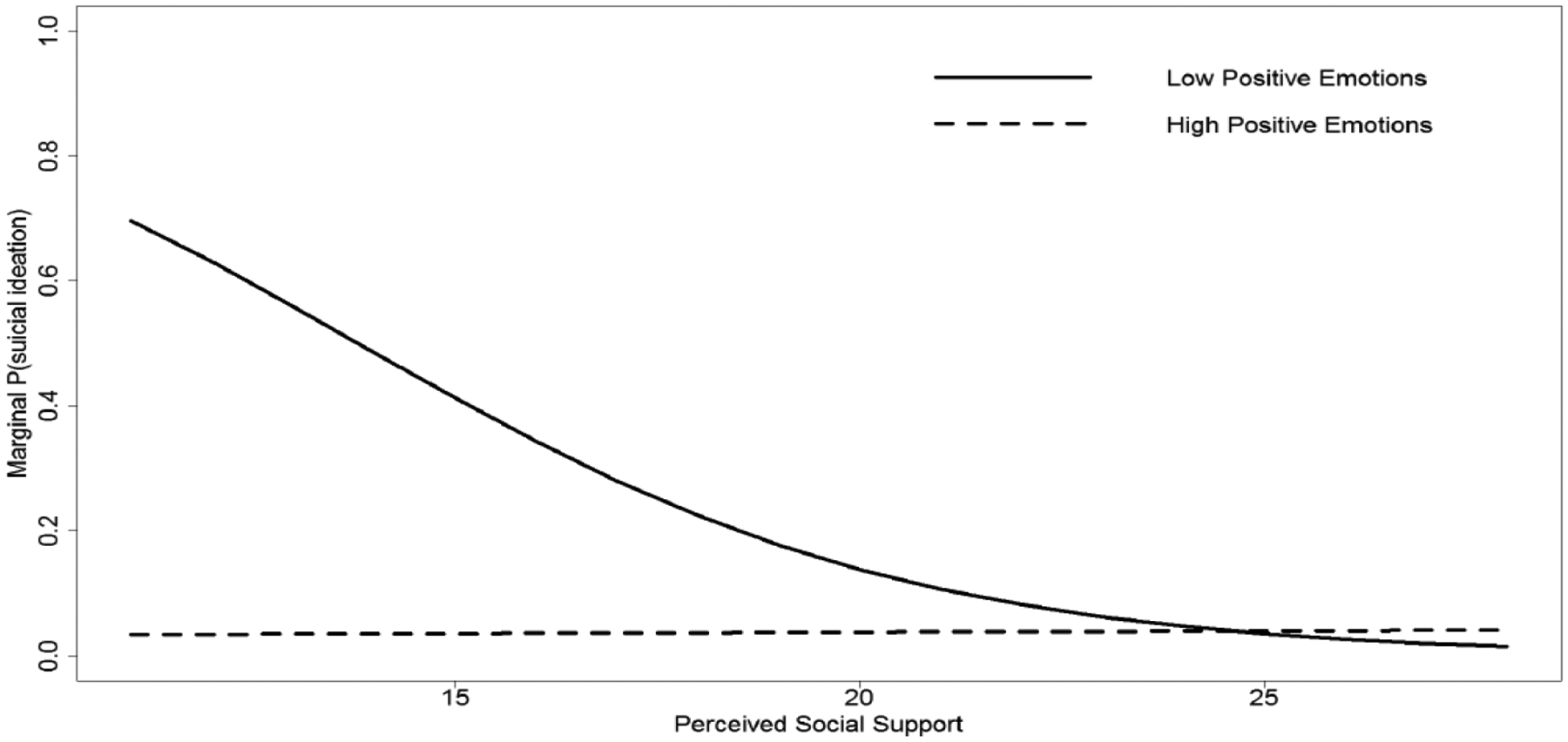
Figure 1a. Predicted probability of suicidal ideation based upon neuroticism facet of impulsiveness and perceived social support.
Figure 1b. Predicted probability of suicidal ideation based upon extraversion facet of gregariousness and perceived social support.
Figure 1c. Predicted probability of suicidal ideation based upon extraversion facet of positive emotions and perceived social support.
Note. These figures illustrate estimated probability for new data based upon a single follow-up time point. Marginal probability is estimated since random effect and autocorrelation have been ignored. The exact covariates used to depict the figure above included: 68 years of age, female sex, no previous suicide attempt, baseline MADRS without item 10 score = 25, 5 years after baseline. In addition, for Figure 1a NEO-PI-R neuroticism raw score without impulsiveness raw score = 83, Figure 1b NEO-PI-R extraversion raw score without gregariousness raw score = 83, NEO-PI-R extraversion raw score without positive emotions raw score = 83.
Conclusions
We found high neuroticism and low extraversion were independent predictors of prospective suicidal ideation in a sample of patients with LLD. While the relationship between these dimensions and the likelihood of suicidal ideation were no longer significant when other variables commonly associated with suicidal ideation were added to the model, multivariate analyses at the facet level did reveal a moderating effect of social support on impulsiveness, gregariousness, and positive emotions. Decreased subjective social support was associated with an increased likelihood of suicidal ideation in LLD patients with high (but not low) impulsiveness and low (but not high) gregariousness and positive emotions. Elsewhere, across all the models, social support by sex was a significant interaction term, indicating social support was beneficial to women, but not men, in decreasing the likelihood of future suicidal ideation.
The standard interpretation of high scores on NEO-PI-R impulsiveness facet refers to an inability to control cravings and urges. High scores on this scale seem to suggest an individual who is emotionally reactive, as this facet loads on the same factor as other impulsivity questionnaires related to “negative urgency” or the tendency to act rashly in response to negative emotion (29). Therefore, one explanation of the current findings is that depressed older adults with higher impulsiveness may be more inclined to experience death-related thoughts when faced with any stressor, whether it be social or otherwise. In one sample of older adults with LLD and co-morbid personality disorders, emotional coping in response to non-specific stressful events (or focusing on the negative emotions associated with the stressors) was associated with increased suicidal ideation (30). Alternatively, the experience of social disconnectedness or so-called “thwarted belongingness” may specifically trigger suicidal ideation in LLD (31), particularly in those with high impulsiveness who may have a stronger limbic response to threatening social stimuli (32).
We also found that the likelihood of suicidal ideation in LLD patients who reported high trait positive emotions and gregariousness was not influenced by changes in subjective social support. This was contrary to our expectation that patients low in gregariousness (traditionally meaning patients who prefer social isolation and are less interested in social stimulation) would not be impacted by subjective changes in social support. One possible interpretation of these findings is that depressed elders low in extraversion facets may experience thoughts related to death as a result of increased loneliness; one recent study of depressed older adults found lower extraversion scores were correlated with increased loneliness, particularly in women (33). We unfortunately did not measure loneliness in the current study so as to include this covariate in our models. Our findings might also simply suggest that patients who are low in gregariousness may still find social interactions rewarding. Hooker et al. found that adults with lower (but not higher) extraversion responded faster to a reward learning paradigm that used happy faces as the conditioned stimulus (34). Extraversion in this study was also negatively correlated with amygdala activity during happy versus neutral learning trials, suggesting subjects low in extraversion responded with greater amygdala activity and were more aroused in the presence of positive social stimuli (34). The presence of social support may therefore provide a positive arousing and emotionally salient experience. The lack of this positive arousal may be especially detrimental to depressed individuals low in extraversion who exhibit hypoactivation in emotional regulation and reward brain regions (35).
Contrary to our hypothesis, we did not find evidence of a different relationship between personality, subjective social support, and suicidal ideation in men and women. There was an interaction between sex and social support, however, such that subjective social support in women, but not men, was associated with a decreased likelihood of experiencing future suicidal ideation. Distinct associations between social support and suicide have been observed in younger men and women with major depression. Park et al.(36) found that lower subjective social support (i.e., the belief that you have someone who is supportive of your opinions and your actions) was associated with suicidal ideation in women but not men. By contrast, a lower number of friends was associated with suicidal ideation in men, but not women. Together, these findings suggest the quality rather than the quantity of social relationships has a greater impact on the suicide ideation of women compared to men. Additional studies are needed to better understand sex differences in social support and the trajectory of depression and suicide ideation in LLD.
These findings need to be interpreted within the context of some limitations. First, the majority of these data were collected some time ago, and we cannot determine the reasons subjects either refused to complete or were not approached with the NEO-PI-R. While there were no meaningful differences between those who completed and refused to complete the NEO-PI-R, those subjects who were not approached with the questionnaire were older, less educated, and had lower baseline cognitive functioning. Caution should therefore be used in generalizing the findings above to depressed elders with lower cognitive functioning, and further studies should seek to understand how personality, cognitive status, and social support may interact to impact the likelihood of suicidal ideation. In addition, the majority of NCODE participants who experienced suicidal ideation at baseline reported life weariness or death ideation and not more severe suicidal ideation. It is unclear whether similar associations would be found in depressed elders experiencing active thoughts of self-harm. Another limitation is that we only had retrospective information on suicide attempts at the time of baseline and not longitudinal prospective information. We also did not formally assess for the new onset of alcohol/substance abuse diagnoses at follow-up. Personality was also treated as a retrospective measure and therefore assumed to remain relatively stable from the time cognition and mood were first assessed and the time the NEO-PI-R was added to the NCODE protocol. This is consistent with the general stability of personality dimensions following treatment of major depression and the high test–retest reliability of the five dimensions when the retest interval spans an average of 10 years (37), although modest changes to personality do occur over the lifespan (38). Finally, although we attempted to limit our analyses of personality facets a priori, the current study still included a large number of hypothesis tests without correction for multiple comparisons. Considering the possibility of Type I error, these analyses should be considered tentative, particularly secondary outcomes at the facet level. Furthermore, while statistically significant, the overall effect sizes noted in this study were modest. These findings warrant replication and further exploration.
In conclusion, increased neuroticism, decreased extraversion, and decreased social support were independent predictors of increased suicidal ideation in older adults with LLD followed an average of six years later. Certain neuroticism and extraversion traits also interacted with changes in social support to contribute to suicidal ideation. Furthermore, across all the models, social support by sex was a significant interaction term, indicating social support was beneficial to women, but not men, in reducing the likelihood of suicidal ideation.
Supplementary Material
Acknowledgments
The work was supported by NIH grant R01 MH108578 and R01 MH108560.
Footnotes
No Disclosures to Report.
References
- 1.Waern M, Beskow J, Runeson B, et al. : Suicidal feelings in the last year of life in elderly people who commit suicide. Lancet 1999; 354:917–918 [DOI] [PubMed] [Google Scholar]
- 2.Rushing NC, Corsentino E, Hames JL, et al. : The relationship of religious involvement indicators and social support to current and past suicidality among depressed older adults. Aging Ment Health 2013; 17:366–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barry LC: Passive Suicidal Ideation in Older Adults: Implications for Suicide Prevention. Am J Geriatr Psychiatry 2019; [DOI] [PubMed] [Google Scholar]
- 4.Szanto K, Reynolds CF 3rd, Frank E, et al. : Suicide in Elderly Depressed Patients: Is Active vs. Passive Suicidal Ideation a Clinically Valid Distinction? Am J Geriatr Psychiatry 1996; 4:197–207 [DOI] [PubMed] [Google Scholar]
- 5.Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, et al. : Estimating risk for suicide attempt: are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. J Affect Disord 2011; 134:327–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Szucs A, Szanto K, Aubry JM, et al. : Personality and Suicidal Behavior in Old Age: A Systematic Literature Review. Front Psychiatry 2018; 9:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa PT,McCrae RR: NEO PI-R professional manual, Odessa Florida, Psychological Assessment Resources, 1992 [Google Scholar]
- 8.Heisel MJ, Duberstein PR, Conner KR, et al. : Personality and reports of suicide ideation among depressed adults 50 years of age or older. J Affect Disord 2006; 90:175–180 [DOI] [PubMed] [Google Scholar]
- 9.Duberstein PR, Conwell Y, Seidlitz L, et al. : Personality traits and suicidal behavior and ideation in depressed inpatients 50 years of age and older. J Gerontol B Psychol Sci Soc Sci 2000; 55:P18–26 [DOI] [PubMed] [Google Scholar]
- 10.Useda JD, Duberstein PR, Conner KR, et al. : Personality and attempted suicide in depressed adults 50 years of age and older: a facet level analysis. Compr Psychiatry 2004; 45:353–361 [DOI] [PubMed] [Google Scholar]
- 11.Hirsch JK, Duberstein PR, Chapman B, et al. : Positive affect and suicide ideation in older adult primary care patients. Psychol Aging 2007; 22:380–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alexopoulos GS, Bruce ML, Hull J, et al. : Clinical determinants of suicidal ideation and behavior in geriatric depression. Arch Gen Psychiatry 1999; 56:1048–1053 [DOI] [PubMed] [Google Scholar]
- 13.Rowe JL, Conwell Y, Schulberg HC, et al. : Social support and suicidal ideation in older adults using home healthcare services. Am J Geriatr Psychiatry 2006; 14:758–766 [DOI] [PubMed] [Google Scholar]
- 14.O’Riley AA, Van Orden KA, He H, et al. : Suicide and death ideation in older adults obtaining aging services. Am J Geriatr Psychiatry 2014; 22:614–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manning KJ, Chan G,Steffens DC: Neuroticism Traits Selectively Impact Long Term Illness Course and Cognitive Decline in Late-Life Depression. Am J Geriatr Psychiatry 2017; 25:220–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cukrowicz KC, Franzese AT, Thorp SR, et al. : Personality traits and perceived social support among depressed older adults. Aging Ment Health 2008; 12:662–669 [DOI] [PubMed] [Google Scholar]
- 17.Oddone CG, Hybels CF, McQuoid DR, et al. : Social support modifies the relationship between personality and depressive symptoms in older adults. Am J Geriatr Psychiatry 2011; 19:123–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anestis MD,Joiner TE: Examining the role of emotion in suicidality: negative urgency as an amplifier of the relationship between components of the interpersonal-psychological theory of suicidal behavior and lifetime number of suicide attempts. J Affect Disord 2011; 129:261–269 [DOI] [PubMed] [Google Scholar]
- 19.Donker T, Batterham PJ, Van Orden KA, et al. : Gender-differences in risk factors for suicidal behaviour identified by perceived burdensomeness, thwarted belongingness and acquired capability: cross-sectional analysis from a longitudinal cohort study. BMC Psychol 2014; 2:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fiori KL,Denckla CA: Social support and mental health in middle-aged men and women: a multidimensional approach. J Aging Health 2012; 24:407–438 [DOI] [PubMed] [Google Scholar]
- 21.Kitamura T, Watanabe K, Takara N, et al. : Precedents of perceived social support: personality, early life experiences and gender. Psychiatry Clin Neurosci 2002; 56:169–176 [DOI] [PubMed] [Google Scholar]
- 22.Kendler KS, Myers J,Prescott CA: Sex differences in the relationship between social support and risk for major depression: a longitudinal study of opposite-sex twin pairs. Am J Psychiatry 2005; 162:250–256 [DOI] [PubMed] [Google Scholar]
- 23.Sutin AR, Beason-Held LL, Dotson VM, et al. : The neural correlates of Neuroticism differ by sex prospectively mediate depressive symptoms among older women. J Affect Disord 2010; 127:241–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weiss A, Sutin AR, Duberstein PR, et al. : The personality domains and styles of the five-factor model are related to incident depression in Medicare recipients aged 65 to 100. Am J Geriatr Psychiatry 2009; 17:591–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Costa PT Jr., Weiss A, Duberstein PR, et al. : Personality facets and all-cause mortality among Medicare patients aged 66 to 102 years: a follow-on study of Weiss and Costa (2005). Psychosom Med 2014; 76:370–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Montgomery SA,Asberg M: A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134:382–389 [DOI] [PubMed] [Google Scholar]
- 27.Koenig HG, Westlund RE, George LK, et al. : Abbreviating the Duke Social Support Index for use in chronically ill elderly individuals. Psychosomatics 1993; 34:61–69 [DOI] [PubMed] [Google Scholar]
- 28.Landerman R, George LK, Campbell RT, et al. : Alternative models of the stress buffering hypothesis. Am J Community Psychol 1989; 17:625–642 [DOI] [PubMed] [Google Scholar]
- 29.Whiteside SP,Lynam DR: The Five Factor Model and impulsivity: using a structural model of personality to understand impulsivity. Pers Individ Dif 2001; 30:669–689 [Google Scholar]
- 30.Cukrowicz KC, Ekblad AG, Cheavens JS, et al. : Coping and thought suppression as predictors of suicidal ideation in depressed older adults with personality disorders. Aging Ment Health 2008; 12:149–157 [DOI] [PubMed] [Google Scholar]
- 31.Van Orden KA, Witte TK, Cukrowicz KC, et al. : The interpersonal theory of suicide. Psychol Rev 2010; 117:575–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vanyukov PM, Szanto K, Siegle GJ, et al. : Impulsive traits and unplanned suicide attempts predict exaggerated prefrontal response to angry faces in the elderly. Am J Geriatr Psychiatry 2015; 23:829–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schutter N, Koorevaar L, Holwerda TJ, et al. : ‘Big Five’ personality characteristics are associated with loneliness but not with social network size in older adults, irrespective of depression. Int Psychogeriatr 2019; 1–11 [DOI] [PubMed] [Google Scholar]
- 34.Hooker CI, Verosky SC, Miyakawa A, et al. : The influence of personality on neural mechanisms of observational fear and reward learning. Neuropsychologia 2008; 46:2709–2724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Tol MJ, Veer IM, van der Wee NJ, et al. : Whole-brain functional connectivity during emotional word classification in medication-free Major Depressive Disorder: Abnormal salience circuitry and relations to positive emotionality. Neuroimage Clin 2013; 2:790–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Park S, Hatim Sulaiman A, Srisurapanont M, et al. : The association of suicide risk with negative life events and social support according to gender in Asian patients with major depressive disorder. Psychiatry Res 2015; 228:277–282 [DOI] [PubMed] [Google Scholar]
- 37.Terracciano A, Costa PT Jr., McCrae RR: Personality plasticity after age 30. Pers Soc Psychol Bull 2006; 32:999–1009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Terracciano A, McCrae RR, Brant LJ, et al. : Hierarchical linear modeling analyses of the NEO-PI-R scales in the Baltimore Longitudinal Study of Aging. Psychol Aging 2005; 20:493–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


