Abstract
Background:
Given the high prevalence of depressive symptoms reported by adolescents and associated risk of experiencing psychiatric disorders as adults, differentiating the trajectories of the symptoms related to negative valence at an individual level could be crucial in gaining a better understanding of their effects later in life.
Methods:
A longitudinal deep learning framework is presented, identifying self-reported and behavioral measurements that detect the depressive symptoms associated with the Negative Valence System domain of the NIMH Research Domain Criteria (RDoC).
Results:
Applied to the annual records of 621 participants (age range: 12 to 17 years) of the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA), the deep learning framework identifies predictors of negative valence symptoms, which include lower extraversion, poorer sleep quality, impaired executive control function and factors related to substance use.
Limitations:
The results rely mainly on self-reported measures and do not provide information about the underlying neural correlates. Also, a larger sample is required to understand the role of sex and other demographics related to the risk of experiencing symptoms of negative valence.
Conclusions:
These results provide new information about predictors of negative valence symptoms in individuals during adolescence that could be critical in understanding the development of depression and identifying targets for intervention. Importantly, findings can inform preventive and treatment approaches for depression in adolescents, focusing on a unique predictor set of modifiable modulators to include factors such as sleep hygiene training, cognitive-emotional therapy enhancing coping and controllability experience and/or substance use interventions.
Keywords: Negative valence, Adolescents, Deep learning, RDoC
1. Introduction
During adolescence, the prevalence of major depressive disorder (MDD) increases dramatically from 8.4 % (13–14 years) to 15.4 % (17–18 years) (Merikangas et al., 2010). MDD in adolescence is associated with an increased risk for chronic and recurrent depression (Fombonne et al., 2001), anxiety disorders (Merikangas et al., 2010), sleep problems (Short et al., 2020), eating disorders (Holm-Denoma et al., 2014), substance use (Kessler et al., 2005), and suicide attempts, with trajectories extending into adulthood (Geoffroy et al., 2020). Given that depression exerts a major personal, societal, and economic burden (Petito et al., 2020; Mrazek et al., 2014), there is an urgent need to identify more accurate risk factors for the development of this disorder in youth.
Increased risk for depression in adolescence has been linked with multiple psychosocial and behavioral constructs interacting against the backdrop of a range of developmental changes. Examples of such risk factors are personality traits (Klinger-Koenig et al., 2018), exposure to stressful life events (McLaughlin et al., 2012), changes in social relationships and greater autonomy (Fredrick et al., 2018; Thoits, 2011), difficulties with health-promoting behaviors such as sleep (Lovato and Gradisar, 2014; Schulte et al., 2019), risky behaviors such as alcohol use (Danzo et al., 2017), and impaired cognitive function (problems of attention, executive function, and visual memory) (Snyder et al., 2019; Morea and Calvete, 2021; Matthews et al., 2008; Porter et al., 2003). Given the heterogeneity of these risk factors and the low diagnostic validity and specificity of the Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnostic criteria for adolescent MDD (Henje-Blom et al., 2014), there is a growing trend in psychiatry research (Insel, 2014) to look beyond rigid diagnostic criteria by mapping corresponding symptoms onto continua of human functioning defined by the Research Domain Criteria framework (NIMH Research Domain Criteria - RDoC) (Infurna et al., 2016). The six domains in the RDoC framework are Negative Valence Systems, Positive Valence Systems, Cognitive Systems, Systems for Social Processes, Arousal/Regulatory Systems and Sensorimotor Systems. Symptoms associated with these domains are captured by eight units of analyses: self-report, behavior, paradigms, genes, molecules, cells, circuits, and physiology. By associating domains with symptoms measured through units of analyses, the RDoC framework is designed to identify the underlying principle factors and functional systems that contribute to depressive symptoms and development of psychopathology (Henje-Blom et al., 2014).
Despite the clinical importance and considerable advances made in understanding adolescent depression, it remains inconclusive what are the principal factors and systems that underlie depressive symptoms in youth, with the literature linking them with a myriad of psychological predictors (Musliner et al., 2016). Longitudinal studies of adolescent depression have highlighted that a multitude of contextual factors influence the expression of depressive symptoms (Costello et al., 2008; Olino et al., 2010; Dekker et al., 2007). Within RDoC, the psychopathologies are considered as neurodevelopmental disorders where core disruptions in specific brain circuits manifest in disruptions across multiple physiological and psychological domains (Woody and Gibb, 2015). Built on this principle and considering the broader context of the heterogeneity of depressive symptoms during adolescent development, a longitudinal deep learning framework is proposed, which detects symptoms of the RDoC domain in individuals by recognizing complex patterns across a wide variety of measurements capturing self-reported psychological constructs and behaviors.
The Negative Valence Systems domain is constructed of five subdomains: Acute, Potential, and Sustained Threat, Loss, and Frustrative Non-reward (McKay and Tolin, 2017). These constructs are manifested in responses to aversive situations that are associated with the brain’s defensive mechanisms, high vigilance to uncertain harm, avoidance and deprivation (National Institute of Mental Health, 2011). This work focuses on these constructs because symptoms in the RDoC Negative Valence Systems domain are important correlates of MDD, including feelings of sadness, loss, and responses to frustrating and unpleasant situations, such as sustained anxiety, fear, and threat (Cuthbert and Insel, 2013). Youth experiencing these symptoms often exhibit negative attentional biases in their information processing, including giving lower valence ratings for emotional faces (Dai et al., 2016). There is some evidence for clinical divergence between symptoms both in adolescents (McMakin et al., 2012) and in adults (Medeiros et al., 2020), such as patients with symptoms of anhedonia responding differently to antidepressants than patients reporting symptoms of negative valence (Domschke et al., 2010).
While classical statistical models are designed to identify group differences of a priori, expert selected variables supporting a specific hypothesis (such as specific personality traits characteristic for those experiencing negative valence) the exploratory, data-driven nature of machine learning can handle heterogeneity across subjects and symptoms by performing hierarchical feature selection that enables identification of complex patterns detecting symptoms in individuals. This ability has made machine learning a popular tool for identifying risk factors of MDD (Nemesure et al., 2021). For example, Su et al. (2021) applied a longitudinal machine learning model to identify risk factors of MDD in an elderly population. Machine learning technology has also been used to forecast severe depressive states in individuals (Suhara et al., 2017).
In extension to these previous approaches, a longitudinal deep learning model is proposed that detects symptoms of negative valence being present at an assessment of an adolescent by training the data-driven approach on annually recorded self-reports and behavioral evaluations of 621 participants (age range: 12 to 17 years) of the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA). The deep learning model does so by explicitly accounting for age and mood history of the adolescent. A novel, general framework is then proposed to identify the complex patterns derived by deep learning models, which in our case detect symptoms of negative valence in individuals. Specifically, the measurements derived from the self-reports and behavioral assessments are divided into 8 categories (i.e., personality, life events, risk behavior, support, sleep, neuropsychological, substance use (including alcohol drinking), demographics) and then used by permutation testing to compute the significance of each category in detecting negative valence. By doing so, it is possible to relate the data-driven discoveries on detecting symptoms of negative valence at an individual assessment to group differences published in the adolescent literature.
2. Materials and methods
From November 2012 to October 2014, the NCANDA study (Brown et al., 2015) recruited 831 youths (ages 12 to 21 years at baseline) across five sites (University of California San Diego (UCSD), SRI International, Duke University Medical Center, University of Pittsburgh (UPMC), and Oregon Health & Science University (OHSU)), of which 621 were under 18 years (forming the sample analyzed here).
Participants provided written informed assent together with parental permission. The Institutional Review Boards (IRB) at each site approved data collection and use. Participants completed up to 7 assessments by age 17 years. The average time between assessments was 1.05 years. The data were part of the public data release NCANDA_PUBLIC_6Y_R-EDCAP_V01 (Pohl et al., 2022), whose collection and distribution were supported by NIH funding AA021697, AA021695, AA021692, AA021696, AA021681, AA021690, and AA02169.
For each assessment, symptoms of negative valence were measured using the Achenbach System of Empirically Based Assessments (ASEBA; (Achenbach and Rescorla, 2001)) administered as the Youth Self-Report (YSR; (Achenbach and Rescorla, 2001)). Each item of the YSR is assessed on a 3-point scale (0 = not true, 1 = sometimes true, 2 = often true, for the past 6 months).
To identify adolescents at risk for depression on a broad landscape, all RDoC dimensions of the Negative Valence Systems (fear, anxiety and loss) were represented, hence the criteria for negative valence were based on the anxious/depressed items of the YSR subscale and on the single item “often experience unhappiness, sadness, or depression”, representing the sadness construct (rated on a 3-point scale). The subscale is composed of 13 items, including being fearful/anxious, nervous/tense, and cries a lot. Normalized t-scores were calculated based on age and sex, and a dichotomized variable was created. Individuals were identified as experiencing symptoms associated with negative valence if their t-score was 65 or above (Achenbach and Rescorla, 2001) or if they scored higher than 0 on the single item. Among the 621 youth, the t-scores of assessments of 63 subjects were at the at-risk range (≥ 65) derived from the 13 anxious/depressed items on the YSR, while 39 subjects reported sadness at the single item “often experience unhappiness, sadness, or depression” at least in one assessment. Overall, 81 subjects satisfied either of the two criteria for exhibiting negative valence in at least one of their yearly assessments. Specifically, out of 1442 total assessments, the 81 subjects exhibited negative valence at 116 assessments. Youth with negative valence score below the threshold in all their assessments were categorized as controls.
At each assessment, participants completed a battery of psychological self-report and behavioral assessments, which covered 8 categories: personality, sleep, life events, Behavior Rating Inventory of Executive Function (BRIEF) (Gioia et al., 2000a, 2000b), neuropsychology battery, substance use, social support, and demographics. Demographics consisted of all variables listed in Table 1 except age, which was included in the model as a co-target within the longitudinal analyses. The remaining categories are described in detail in Section B of the Supplementary material.
Table 1.
Demographics of the NCANDA dataset.
| General | |
|---|---|
|
| |
| Sex (female/male) | 310/311 |
| Number of assessments | 3.20 ± 1.66 |
| Time between assessments in years | 1.05 ± 0.15 |
|
Baseline | |
| Age in years | 15.02 ± 1.69 |
| Pubertal Development Score (PDS) | 3.04 ± 0.69 |
| Body Mass Index (BMI; z-score) | 0.32 ± 1.01 |
| Parents education in years | 16.88 ± 2.46 |
|
Race/ethnicity | |
| Caucasian | 438 (70.53 %) |
| African-American | 81 (13.05 %) |
| Asian | 38 (6.12 %) |
| Other | 64 (10.31 %) |
| Hispanic | 74 (13.52 %) |
|
Site | |
| UCSD | 154 (24.80 %) |
| SRI International | 146 (23.51 %) |
| Duke | 137 (22.06 %) |
| OHSU | 108 (17.39 %) |
| UPMC | 76 (12.24 %) |
± denotes the average and standard deviation.
2.1. Deep learning and statistical analysis
A deep learning model is built to identify measures from the 8 categories (excluding those used for determining negative valence) that detected symptoms of negative valence at every assessment of an individual. First, missing measures at an assessment were replaced with those of the individual’s nearest assessment or with the mean of all participants if the measurement was never recorded for that individual (Little and Rubin, 2019). The resulting dataset was then used as the input of our longitudinal deep learning framework (Fig. 1(a)). The deep learning architecture consisted of a Fully Connected Layer (Goodfellow et al., 2016) and a Recurrent Neural Network with a gated mechanism called Gated Recurrent Unit (GRU) (Cho et al., 2014) (see Supplement Section A and Supplementary Fig. 1. for more details such as model optimization)).
Fig. 1.

Overview of the proposed pipeline. Annual assessments of 621 NCANDA youth split into control/negative valence cohorts were processed by a longitudinal neural network, which estimated the age and detected the negative valence symptoms of each individual at every assessment. Afterwards the measurements of each variable category were permuted and reassessed by the trained model to identify the significance of each category. Further, the individual measurements of the significant categories were ranked using the gradient magnitudes of the trained model. Finally, the measurements that contributed the most to detecting negative valence were correlated with the confidence scores.
All individual assessments were the input to the GRU layer, which identified the absence or presence of symptoms of negative valence at each assessment of a subject. As shown in Fig. 2, all individual assessments were the input to our neural network, which identified negative valence at each assessment by also considering all previous assessments of the subject. Simultaneously, the model estimated the subject’s age at every assessment using two fully connected layers (Fig. 2). This multitask learning approach ensured that the age of the subject played a crucial role in the identification model as adolescent subjects undergo major developmental changes during the age span of this study (i.e., 12 and 17 years), which are also reflected in longitudinal changes in the 126 model predictors (such as personality traits and life events). Furthermore, the baseline age of subjects at enrollment differed, therefore estimate the age implicitly aligned assessments across subjects during the training process. Our model was optimized by minimizing binary cross-entropy loss (Murphy, 2012) with respect to classifying assessments into being symptomatic or not and a mean-square error loss (Bishop and Nasrabadi, 2006) for regressing the age of the subject.
Fig. 2.
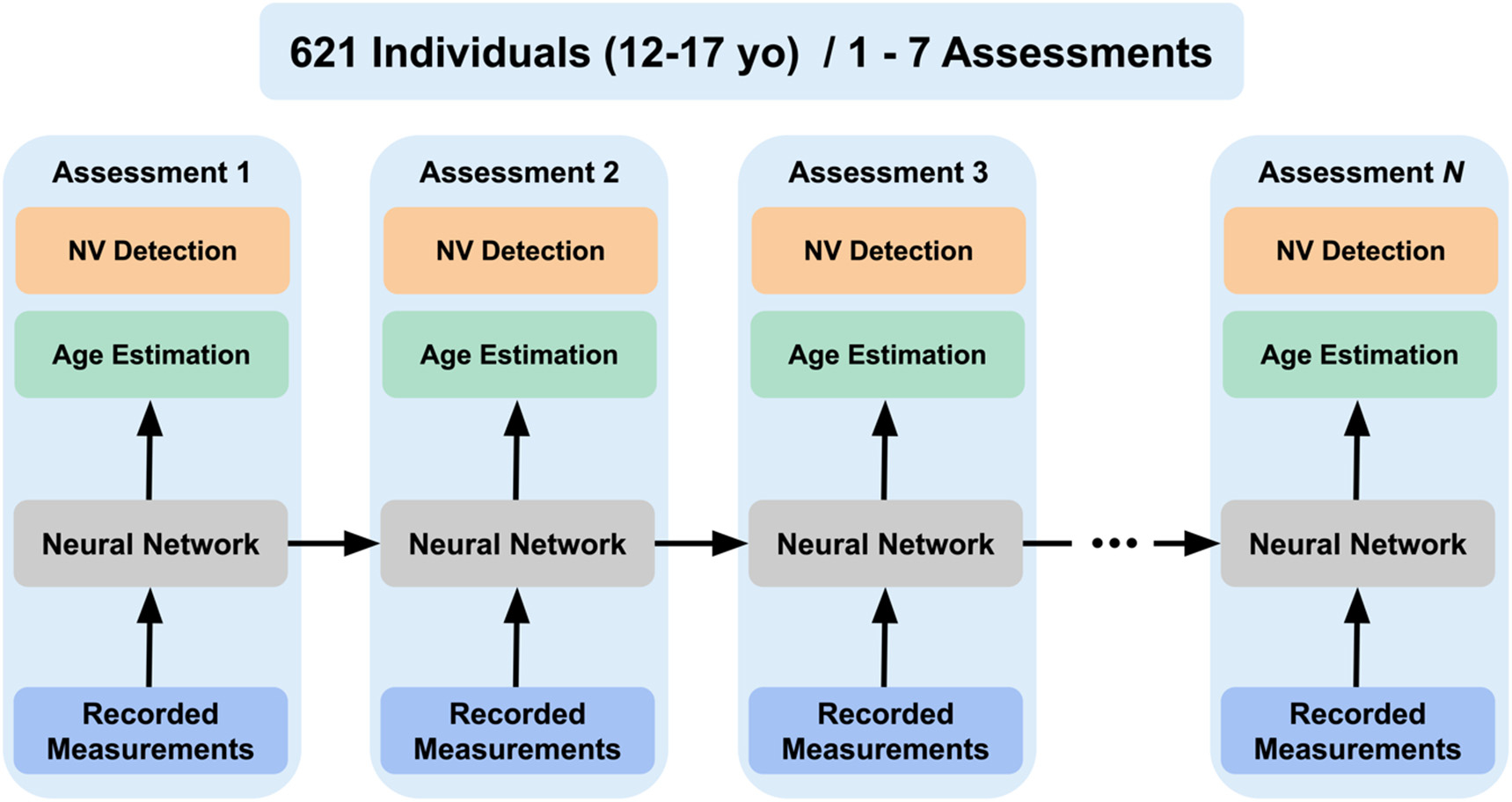
Graphical illustration of how the recurrent neural network identifies negative valence (NV detection) and estimates age at each assessment of a subject based on measurements recorded at that assessment and based on the analysis of prior time points. The analysis is flexible with respect to the number of assessments recorded for a subject, which ranged from 1 to 7 on the NCANDA data set.
The accuracy of the regressed age and confidence score (between 0 and 1) regarding the presence of negative valence at every assessment of a participant was determined via 5-fold stratified cross-validation (Arlot et al., 2010), i.e., dividing the participants into 5 folds, selecting 4 folds for training the model and one fold for testing the model, and repeating training and testing until each fold was used for testing. The reported balanced accuracy of the model was calculated over all assessments of all subjects in every test fold.
Next, the importance of each of the 8 categories in detecting symptoms of negative valence was determined via permutation testing (Good, 2006) (Fig. 1(b)). Permutation testing randomly rearranged the values of each measurement of a category among participants in the test set, applied the detection model to this data (including the 7 other categories), and recorded the resulting accuracy. This procedure was repeated 500 times to compute the percentage of trials (p-value) that resulted in balanced accuracy (BACC) (Brodersen et al., 2010) at least as high as the original (un-permutated) accuracy. The impact of the category on the detection process was then viewed as significant if the p-value was smaller than 0.05 (or <25 permutations with at least as high accuracy scores).
For each category that met the significance level, the influences of individual measurements of that category on detecting the symptom were determined by performing 100 runs of bootstrapping (Efron and Tibshirani, 1994) (Fig. 1(c)). Each run consisted of randomly selecting subjects (with replacement) from the 621 NCANDA subjects and then training the detection model on the resulting data set. The importance of a measurement in detecting symptoms was then quantified by its magnitude according to guided back-propagation (Springenberg et al., 2014). After completing the 100 runs, the contribution of measurements within each category was ranked according to their averaged magnitude across those runs.
The significance (p < 0.05) of the most important measurement of each category was determined by first computing for each participant its average and that of the confidence score score across all assessments (Fig. 1(d)). Next, the resulting average scores were Spearman correlated (Spearman, 1904) across all participants. In parallel, the Mann–Whitney U test (Mann and Whitney, 1947) examined the difference in the average measurement values between controls and the cohort of individuals reporting symptoms of negative valence. The effect size for the Mann–Whitney U test was captured by the rank-biserial correlation (r) (Wendt, 1972). To further investigate the impact of sex on our results, a secondary analysis was performed examining the potential mediation effect of the personality trait, emotional stability, between sex and negative valence (Baron and Kenny, 1986).
3. Results
The model was significant (p < 0.001) in detecting negative valence symptoms (BACC: 79.57 %). To further motivate the proposed deep model, the accuracy of our approach was compared to two common machine learning classifiers, i.e., random forest (Ho, 1995) (depth = 4, number of estimators = 200) and logistic regression (Bishop and Nasrabadi, 2006) (solver = Stochastic Average Gradient Descent, penalty = L2). For each approach, the balanced accuracy was computed using the same experimental setup (i.e., 5-fold cross-validation). The random forest achieved a balanced accuracy of 72.3 % which was slightly lower than logistic regression (balanced accuracy: 75.0 %). Both accuracy scores were significantly lower than the one of our deep model (p < 0.001 according to McNemar test (McNemar, 1947)).
Of significant importance for identifying negative valence (Table 2) were the categories of personality (p < 0.002), life events (p < 0.002), executive function (p < 0.002), sleep (p = 0.024), and substance use (p = 0.048). For these five categories, their three most important measurements are listed in Table 3. With respect to personality, traits of extroversion, emotional stability, and acceptance were the most important predictors for negative valence. Specifically, lower emotional stability was significantly correlated with the actual construct score used for identifying symptoms of negative valence (in Fig. 3). Regarding, the mediation effect of emotional stability, between sex and negative valence, our mediation analysis confirmed that the sex difference specific to symptoms of negative valence is mediated by emotional stability. When both sex and emotional stability are used to regress negative valence, the significant sex effect on negative valence disappears.
Table 2.
Eight predictor categories for symptoms of negative valence: p-values and difference statistics. The average difference and standard deviation in BACC were reported when the category was permuted compared to the unpermutated data (i.e., BACC of 79.57 %). Categories are ranked with respect to their p-values and difference if they had the same p-value. Bolding indicates statistically significant p-values (p < 0.05).
| Category | p-Value | Difference |
|---|---|---|
|
| ||
| Personality | <0.002 | −0.1517 ± 0.062 |
| Life events | <0.002 | −0.0427 ± 0.085 |
| BRIEF | <0.002 | −0.0417 ± 0.106 |
| Sleep | 0.024 | −0.0157 ± 0.093 |
| Substance use | 0.048 | −0.0097 ± 0.098 |
| Support | 0.432 | −0.0007 ± 0.079 |
| Neuropsych | 0.562 | +0.0013 ± 0.088 |
| Demographics | 0.764 | +0.0033 ± 0.096 |
Table 3.
The three most important measurements in categories crucial for detecting negative valence.
| Category | Negative valence |
|---|---|
|
| |
| Personality | Emotional Stability Extraversion Acceptance |
| Life events | Discrete Positive Controllable Events Sexual Abuse Chronic Negative Controllable Scale |
| BRIEF | Cognitive Shift t-score Behavioral Shift t-score Inhibit t-score |
| Sleep | Circadian Preference Weekend Sleep Duration Poor Sleep Quality |
| Substance Use | Cahalan Score Externalizing (Youth SSAGA) Family Substance Use |
Fig. 3.
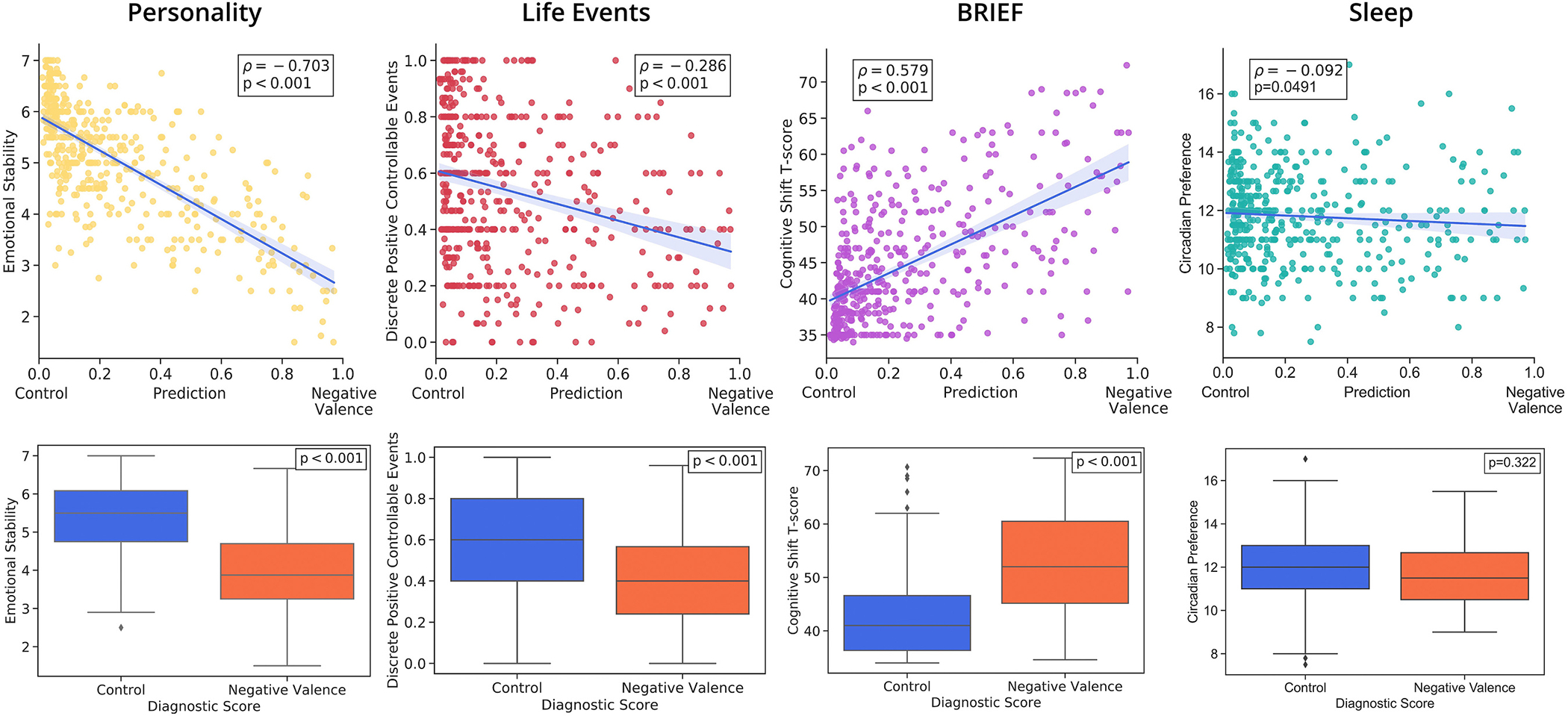
Top: Correlation between average confidence score and the average of the most important variable in each category that was crucial for detecting negative valence. Bottom: Distribution of those variables for individuals in the control cohort and for individuals reporting negative valence in at least one assessment (medians ± interquartile range (IQR) and outliers).
With respect to the category life events, negative life events, childhood sexual abuse and fewer positive life events were crucial predictors of negative valence, which was also significantly correlated with fewer positive controllable events (Fig. 3). Important measurements of executive function from the BRIEF were the higher cognitive shift t-score, inhibit, and behavioral shift t-scores. Finally, poor sleep quality was also important in identifying negative valence symptoms. Specifically, circadian preference (more eveningness) and weekday or weekend sleep duration were the most important predictors of negative valence symptoms (Fig. 3).
Those findings were confirmed when comparing the distribution of those measurements between controls and individuals reporting negative valence symptoms at least once. Specifically, participants with symptoms of negative valence reported significantly lower emotional stability (Mdn = 3.87) than did controls (Mdn = 5.5) (Mann-Whitney U = 25,857, n1(controls) = 381, n2(negative valence) = 81, p < 0.001) (see Fig. 3). Positive controllable events were also significantly lower in the cohort reporting negative valence symptoms (Mdn = 0.4) than in the controls (Mdn = 0.6) (Mann-Whitney U = 20,239, n1 = 381, n2 = 81, p < 0.001). Participants who reported negative valence symptoms also had significantly higher cognitive shift t-scores (Mdn = 52.0) than did controls (Mdn = 41.0) (Mann-Whitney U = 6172, n1 = 381, n2 = 81, p < 0.001). Both the emotional stability (r = 0.67) and cognitive behavioral shift (r = 0.60) had strong effects on the outcome, while the positive discrete controllable life events had only a small effect (r = 0.31).
4. Discussion
This paper proposed a novel approach for detecting negative valence symptoms in individual assessments of adolescents. Each assessment contained a variety of neuropsychological, emotional, personality, and behavioral factors. By considering the developmental changes occurring during adolescence, our data-driven, longitudinal approach detected symptoms of negative valence with relatively high accuracy and identified categories and corresponding measurements that seem to be closely linked to those symptoms. Strongest predictors were factors of personality, notably lower emotional stability, lower extraversion, and lower acceptance. These findings are consistent with previous group findings that link depression symptoms with low extraversion (Klinger-Koenig et al., 2018), especially the low positive emotionality component of extraversion (Watson et al., 2015). As stated in the emotion context-insensitivity (ECI) hypothesis (Rottenberg and Gotlib, 2004), personality traits could influence mood through altering reactivity to emotional cues, meaning that reduced sensitivity to the emotional context (both pleasant and unpleasant), or in other words, emotional withdrawal, is a risk factor for depression. Sensitivity to the emotional cues at the neural level, reflected in increased neural responses towards emotional stimuli in adolescence, has been shown to be associated with higher extraversion (Speed et al., 2015), suggesting that low extraversion reflects altered emotional processing and increased risk for depressive disorder.
Another important category for detecting native valence was negative life events with chronic negative events, childhood sexual abuse and fewer positive life events being the most crucial predictors within that category. Adverse life events have been linked to increased susceptibility to depression in youth (De Venter et al., 2013). A strong association between childhood sexual abuse and depression has also been widely reported (Jhang, 2020). In addition, meta-analyses (Humphreys et al., 2020; Infurna et al., 2016) addressing different types of traumatic life events point to the importance of more “silent” types of maltreatment, such as emotional abuse and neglect in adolescents in detecting depressive symptoms, which was not found. Adolescents might differ in their reactions to life events based on their control over the situation; emotional abuse can lead a child to experience feelings of powerlessness and have lower self-esteem, which are linked more strongly with depression than are other forms of maltreatment (Van Veen et al., 2013). In the extant literature, life events that fall beyond individual control are labeled as uncontrollable, while events influenced by the individuals are referred to as controllable (Marum et al., 2014). These findings highlight the importance of the potential control over the negative life event and support the formulation that the controllable events are more likely to increase the likelihood of psychiatric morbidity and exacerbate depressive symptom levels over time (Jhang, 2020).
A consistent association was found between depressive symptoms and executive dysfunction; lower inhibitory control and lower flexibility (cognitive and behavioral shift) were associated with negative valence. Impaired executive control over negative information may lead to increased negative cognition and prolonged negative affect, which in turn may increase the risk for depression. It should be noted that depression also predicts executive dysfunction, with a reciprocal relation (Gotlib and Joormann, 2010).
As expected, another important predictor of symptoms of negative valence identified by our deep learning approach were factors sleep, i.e., circadian preference towards eveningness, shortened sleep duration, and poor sleep quality. During puberty, adolescents tend to move towards later chronotypes (Roenneberg et al., 2004) and their sleep time is highly variable (Fuligni and Hardway, 2006), which increases their risk for sleep problems. Our finding that shorter sleep duration is associated with negative valence symptoms supports a strong body of research indicating shorter sleep duration in adolescents increases the risk for experiencing depression, anxiety, fatigue, and lower subjective well-being (Fuligni and Hardway, 2006). Shorter sleep duration is associated with a 55 % increased risk of mood difficulties (with strongest effects for reduced positive affect (Short et al., 2020; Blake et al., 2018). Given that sleep is a modifiable factor (Blake et al., 2018), improving sleep quality could be an essential intervention strategy to avoid the development of mood problems during adolescence. Our data support sleep as a protective factor against the emergence of negative effects, which could ultimately reduce the risk for depressive disorder. The current results are in line with the previous finding that circadian preference towards eveningness is related to poorer mental health and a higher prevalence of clinical depression (Kitamura et al., 2010), and extends these findings to show that they enable detection on an individual level and that eveningness is an important predictor for negative valence symptoms.
Substance use was also a risk factor for negative valence. The most important predictors in this category were elevated past alcohol use, having externalizing symptoms and family substance use history. There is a bidirectional relation between heavy alcohol use and depression, with shared risk factors; alcohol may be used to relieve negative feelings, but alcohol problems can also predispose adolescents to depression (Marmorstein, 2009; Hussong et al., 2017). Our findings are consistent with a meta-analysis of several studies showing that more frequent engagement in alcohol use and binge drinking is associated with higher levels of depression in adolescents (Cairns et al., 2014). Further, externalizing symptoms are commonly reported comorbidity factors of substance use (King et al., 2004; Hussong et al., 2011), and are related by definition to behavioral disinhibition problems. This correlation is driven by both common genetic liability (Kendler et al., 2003) and environmental factors (Kendler et al., 1997), especially a family history of substance use (Cservenka, 2016; Handley et al., 2011).
Surprisingly, sex (and other demographic factors) was not a significant predictor of negative valence. However, consistent with the literature (Hankin et al., 1998), our sample contains significantly more girls than boys reporting symptoms of negative valence (see Fig. 4). As confirmed by the mediation analysis, the sex difference specific to negative valence is mediated by emotional stability (the highest ranked predictor of negative valence). Furthermore, adolescent boys had significantly higher emotional stability (p < 0.001) than girls, as was previously reported by (McCrae et al., 2002; Klimstra et al., 2009), and were less likely to have high negative valence.
Fig. 4.
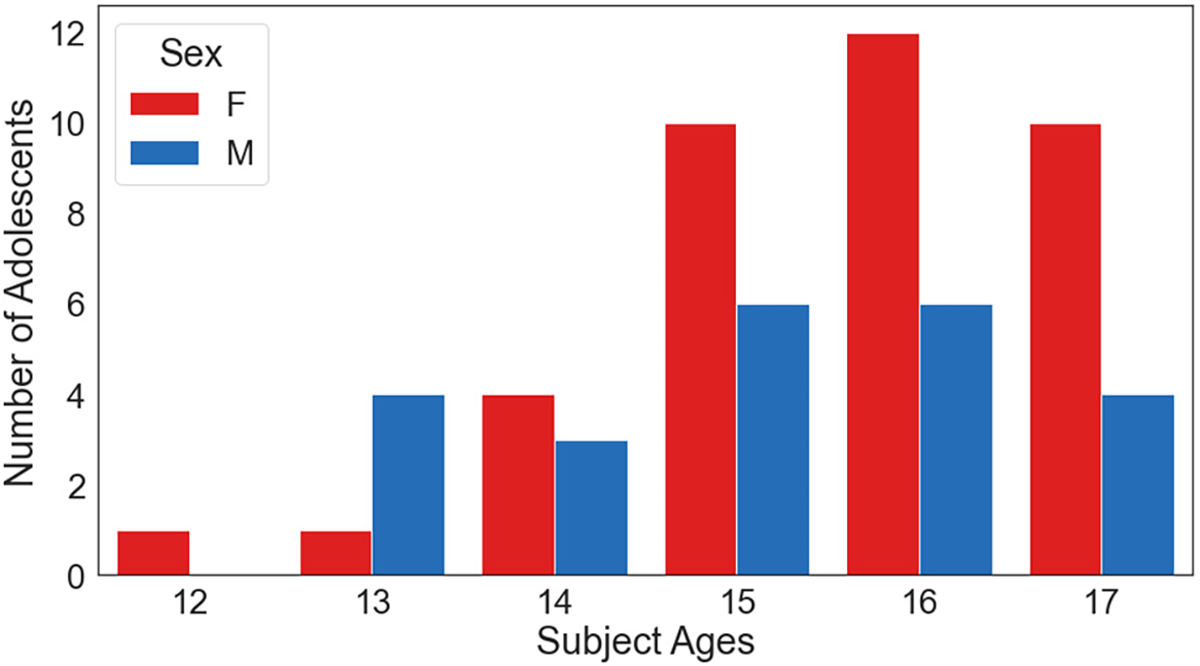
Number of male and female participants who endorsed negative valence across assessments between ages 12–17 years.
Among psychological factors considered by our model, social support, which was mainly measured in the context of school and community, has low power in detecting symptoms of negative valence. While social support can be beneficial and protective against depression (Cheng et al., 2008; Yu et al., 2016) in adults, adolescents might perceive the received support as controlling (Piko and Balázs, 2012) or as a source of conflict (Barrera et al., 1993). Indeed, the positive association between social support and well-being increases with age (Chu et al., 2010).
One important benefit of our novel longitudinal approach is that it incorporates within-person information. This approach detected negative valence at every assessment, as subjects can switch between reporting symptoms of negative valence at assessments and being symptom free at others. By doing so, the proposed model could inform clinicians about the individual-level potential risk based on the measurements recorded in an assessment. Also, possibly critical for clinical interventions is the ranking between the relevant predictors of symptoms of negative valence that our novel data-driven analysis provided.
While being comprehensive (with over 100 predictors considered) our analysis was not exhaustive so that there may be other factors that could be relevant for detecting negative valence symptoms. Another limitation of this study is the reliance on self-reported data for all variables other than the behavioral neuropsychology test performance measures. Furthermore, the examination of network-based brain activation patterns is needed to determine whether our results, based on self-report measures, are reflected in the subsequent neural substrates (potentially based on functional or resting-state MRI data) that underlie the negative valence symptoms. For example, examining pathways and functions that rely on the prefrontal cortex could be promising in this respect, given that the prefrontal cortex is still developing through early adolescence (Andersen and Teicher, 2008). These studies highlight that high-risk adolescents are characterized by altered cortical thickness in regions of the brain that are involved in cognitive control, emotional regulation, and in the default mode network, and suggest that alternative modeling focusing on the underlying neural representation will provide additional insights about the development of depression and characterization negative valence symptoms in adolescents.
Given that depression can manifest in different symptom profiles (Keller et al., 2007; Coryell et al., 1994) with moderate within-person consistency of symptoms (Oquendo et al., 2004), a symptom-level analysis is provided instead of using traditional diagnostic criteria. Here, the focus was specifically on the predictors of negative valence, which is a critical system implicated in depressive disorder as well as other psychiatric disorders, such as obsessive-compulsive disorder, PTSD, anxiety-related symptomology (McKay and Tolin, 2017), rumination (Owens and Gibb, 2017) and eating disorders (Vannucci et al., 2015). Future work is needed to examine predictors of other RDoC systems (such as positive valence systems) critical to the development of depression and other disorders. Determination of unique as well as overlapping predictors for the RDoC systems on subject level could then inform prevention and treatment of depression symptomatology in individuals.
5. Conclusion
In conclusion, this study aimed to increase our understanding of the risk effects of multiple psychosocial and behavioral factors on experiencing symptoms of negative valence symptoms. The deep learning analysis took advantage of the NCANDA longitudinal data set, tracking negative valence of 621 adolescents over 6 years. The relatively high accuracy in detecting symptoms of negative valence at individual assessments, along with the developmental aspect, emphasizes the benefits of the proposed model. This line of research has important implications for prevention and early diagnoses, reducing the potential predictors to a small set of risk factors that contribute to the general decline in mood and mental health in adolescence.
Supplementary Material
Acknowledgements
We thank the NIH NIAAA for funding and the NCANDA consortium (NIH funding AA021697, AA021695, AA021692, AA021696, AA021681, AA021690, and AA02169) for support of this project.
Funding
This study was supported by the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) project by means of research grants from the National Institute on Alcohol Abuse and Alcoholism (NIH NIAAA) AA021697 (PI: KMP), AA021696 (PI: FB), and K99 AA028840 (PI: QZ). The research was also supported by the Stanford Institute for Human-Centered Artificial Intelligence (HAI) Google Cloud Credit (PI: KMP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest
This research work was supported by NIH NIAAA and HAI grants. We declare no conflicts of interest.
CRediT authorship contribution statement
FB, KMP designed the study. OK, MP managed the literature searches and analyses. QZ, EA designed the statistical analysis, MP undertook the statistical analysis, and authors MP, OK, KMP, EA, QZ wrote the first draft of the manuscript. SP processed the data necessary for our analysis. IHG and EMO assisted with the preparation and proof-reading of the manuscript. All authors contributed to and have approved the final manuscript.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.06.002.
References
- Achenbach T, Rescorla L, 2001. Manual for the aseba school-age forms & profiles. In: Adverse Childhood Experiences International Questionnaire (ace-iq). University of Vermont Research Centre for Children, Youth and Families, Burlington, VT guidance for analysing ace-iq. world health organization; [Accessed: 2021-08-21]. (n.d.). [Google Scholar]
- Andersen SL, Teicher MH, 2008. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 31 (4), 183–191. [DOI] [PubMed] [Google Scholar]
- Arlot S, Celisse A, et al. , 2010. A survey of cross-validation procedures for model selection. Statistics Surveys 4, 40–79. [Google Scholar]
- Baron RM, Kenny DA, 1986. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51 (6), 1173. [DOI] [PubMed] [Google Scholar]
- Barrera M, Chassin L, Rogosch F, 1993. Effects of social support and conflict on adolescent children of alcoholic and nonalcoholic fathers. J. Pers. Soc. Psychol. 64 (4), 602–612. [DOI] [PubMed] [Google Scholar]
- Bishop CM, Nasrabadi NM, 2006. In: Pattern Recognition and Machine Learning, 4. Springer, New York, p. 738. No. 4. [Google Scholar]
- Blake MJ, Trinder JA, Allen NB, 2018. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin. Psychol. Rev. 63, 25–40. [DOI] [PubMed] [Google Scholar]
- Brodersen KH, Ong CS, Stephan KE, Buhmann JM, 2010. The balanced accuracy and its posterior distribution. In: 2010 20th International Conference on Pattern Recognition, pp. 3121–3124. [Google Scholar]
- Brown SA, Brumback T, Tomlinson K, Cummins K, Thompson WK, Nagel BJ, De Bellis MD, Hooper SR, Clark DB, Chung T, et al. , 2015. The national consortium on alcohol and neurodevelopment in adolescence (ncanda): a multisite study of adolescent development and substance use. J. Stud. Alcohol Drugs 76 (6), 895–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns KE, Yap MBH, Pilkington PD, Jorm AF, 2014. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 169, 61–75. [DOI] [PubMed] [Google Scholar]
- Cheng ST, Cheung KCC, Cheung CK, 2008. Peer victimization and depression among Hong Kong adolescents. J. Clin. Psychol. 64 (6), 766–776. [DOI] [PubMed] [Google Scholar]
- Cho K, Van Merrienboer B, Gulcehre C, Bahdanau D, Bougares F, Schwenk H, Bengio Y, 2014. Learning Phrase Representations Using rnn Encoder-Decoder for Statistical Machine Translation. arXiv preprint arXiv:1406.1078. [Google Scholar]
- Chu PS, Saucier DA, Hafner E, 2010. Meta-analysis of the relationships between social support and well-being in children and adolescents. J. Soc. Clin. Psychol. 29 (6), 624–645. [Google Scholar]
- Coryell W, Winokur G, Shea T, Maser JD, Endicott J, Akiskal HS, 1994. The long-term stability of depressive subtypes. Am. J. Psychiatry 151 (2), 199–204. [DOI] [PubMed] [Google Scholar]
- Costello DM, Swendsen J, Rose JS, Dierker LC, 2008. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. J. Consult. Clin. Psychol. 76 (2), 173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cservenka A, 2016. Neurobiological phenotypes associated with a family history of alcoholism. Drug Alcohol Depend. 158, 8–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert BN, Insel TR, 2013. Toward the future of psychiatric diagnosis: the seven pillars of rdoc. BMC Med. 11 (1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Q, Wei J, Shu X, Feng Z, 2016. Negativity bias for sad faces in depression: an event-related potential study. Clin. Neurophysiol. 127 (12), 3552–3560. [DOI] [PubMed] [Google Scholar]
- Danzo S, Connell AM, Stormshak EA, 2017. Associations between alcohol-use and depression symptoms in adolescence: examining gender differences and pathways over time. J. Adolesc. 56, 64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Venter M, Demyttenaere K, Bruffaerts R, 2013. The relationship between adverse childhood experiences and mental health in adulthood. A systematic literature review. Tijdschrift voor psychiatrie 55 (4), 259–268. [PubMed] [Google Scholar]
- Dekker MC, Ferdinand RF, Van Lang NDJ, Bongers IL, Van Der Ende J, Verhulst FC, 2007. Developmental trajectories of depressive symptoms from early childhood to late adolescence: gender differences and adult outcome. J. Child Psychol. Psychiatry 48 (7), 657–666. [DOI] [PubMed] [Google Scholar]
- Domschke K, Dannlowski U, Hohoff C, Ohrmann P, Bauer J, Kugel H, Zwanzger P, Heindel W, Deckert J, Arolt V, et al. , 2010. Neuropeptide y (npy) gene: impact on emotional processing and treatment response in anxious depression. Eur. Neuropsychopharmacol. 20 (5), 301–309. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani RJ, 1994. An introduction to the bootstrap. CRC Press. [Google Scholar]
- Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M, 2001. The maudsley long-term follow-up of child and adolescent depression: I. Psychiatric outcomes in adulthood. Br. J. Psychiatry 179 (3), 210–217. [DOI] [PubMed] [Google Scholar]
- Fredrick SS, Demaray MK, Malecki CK, Dorio NB, 2018. Can social support buffer the association between depression and suicidal ideation in adolescent boys and girls? Psychol. Sch. 55 (5), 490–505. [Google Scholar]
- Fuligni AJ, Hardway C, 2006. Daily variation in adolescents’ sleep, activities, and psychological well-being. J. Res. Adolesc. 16 (3), 353–378. [Google Scholar]
- Geoffroy M-C, Orri M, Girard A, Perret LC, Turecki G, 2020. Trajectories of suicide attempts from early adolescence to emerging adulthood: prospective 11-year follow-up of a Canadian cohort. Psychol. Med. 1–11. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L, 2000a. Behavior rating inventory of executive function: brief. In: Psychological Assessment Resources Odessa, FL. PAR, Inc. [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L, 2000b. Test review behavior rating inventory of executive function. Child Neuropsychol. 6 (3), 235–238. [DOI] [PubMed] [Google Scholar]
- Good PI, 2006. Permutation, Parametric, and Bootstrap Tests of Hypotheses. Springer Science & Business Media. [Google Scholar]
- Goodfellow I, Bengio Y, Courville A, Bengio Y, 2016. Deep Learning, Vol. 1. MIT Press, Cambridge. [Google Scholar]
- Gotlib IH, Joormann J, 2010. Cognition and depression: current status and future directions. Annu. Rev. Clin. Psychol. 6, 285–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley ED, Chassin L, Haller MM, Bountress KE, Dandreaux D, Beltran I, 2011. Do executive and reactive disinhibition mediate the effects of familial substance use disorders on adolescent externalizing outcomes? J. Abnorm. Psychol. 120 (3), 528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE, 1998. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J. Abnorm. Psychol. 107 (1), 128. [DOI] [PubMed] [Google Scholar]
- Henje-Blom E, Duncan LG, Ho TC, Connolly CG, LeWinn KZ, Chesney M, Hecht FM, Yang TT, 2014. The development of an rdoc-based treatment program for adolescent depression:“training for awareness, resilience, and action”(tara). Front. Hum. Neurosci. 8, 630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho TK, 1995. Random decision forests. Proceedings of 3rd international conference on document analysis and recognition 1, 278–282. [Google Scholar]
- Holm-Denoma JM, Hankin BL, Young JF, 2014. Developmental trends of eating disorder symptoms and comorbid internalizing symptoms in children and adolescents. Eat. Behav. 15 (2), 275–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, LeMoult J, Wear JG, Piersiak HA, Lee A, Gotlib IH, 2020. Child maltreatment and depression: a meta-analysis of studies using the childhood trauma questionnaire. Child Abuse Negl. 102, 104361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S, 2011. An internalizing pathway to alcohol use and disorder. Psychol. Addict. Behav. 25 (3), 390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Ennett ST, Cox MJ, Haroon M, 2017. A systematic review of the unique prospective association of negative affect symptoms and adolescent substance use controlling for externalizing symptoms. Psychol. Addict. Behav. 31 (2), 137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna MR, Reichl C, Parzer P, Schimmenti A, Bifulco A, Kaess M, 2016. Associations between depression and specific childhood experiences of abuse and neglect: a meta-analysis. J. Affect. Disord. 190, 47–55. [DOI] [PubMed] [Google Scholar]
- Insel TR, 2014. The nimh research domain criteria (rdoc) project: precision medicine for psychiatry. Am. J. Psychiatr. 171 (4), 395–397. [DOI] [PubMed] [Google Scholar]
- Jhang F-H, 2020. Uncontrollable and controllable negative life events and changes in mental health problems: exploring the moderation effects of family support and self-efficacy in economically disadvantaged adolescents. Child Youth Serv. Rev. 118, 105417. [Google Scholar]
- Keller MC, Neale MC, Kendler KS, 2007. Association of different adverse life events with distinct patterns of depressive symptoms. Am. J. Psychiatr. 164 (10), 1521–1529. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Davis CG, Kessler RC, 1997. The familial aggregation of common psychiatric and substance use disorders in the national comorbidity survey: a family history study. Br. J. Psychiatry 170, 541. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC, 2003. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch. Gen. Psychiatry 60 (9), 929–937. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE, 2005. Lifetime prevalence and age-of-onset distributions of dsmiv disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 62 (6), 593–602. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M, 2004. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction 99 (12), 1548–1559. [DOI] [PubMed] [Google Scholar]
- Kitamura S, Hida A, Watanabe M, Enomoto M, Aritake-Okada S, Moriguchi Y, Kamei Y, Mishima K, 2010. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiol. Int. 27 (9–10), 1797–1812. [DOI] [PubMed] [Google Scholar]
- Klimstra TA, Hale III WW, Raaijmakers QA, Branje SJ, Meeus WH, 2009. Maturation of personality in adolescence. J. Pers. Soc. Psychol. 96 (4), 898. [DOI] [PubMed] [Google Scholar]
- Klinger-Koenig J, Hertel J, Terock J, Voelzke H, Van der Auwera S, Grabe HJ, 2018. Predicting physical and mental health symptoms: additive and interactive effects of difficulty identifying feelings, neuroticism and extraversion. J. Psychosom. Res. 115, 14–23. [DOI] [PubMed] [Google Scholar]
- Little RJ, Rubin DB, 2019. Statistical Analysis With Missing Data, Vol. 793. John Wiley & Sons. [Google Scholar]
- Lovato N, Gradisar M, 2014. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med. Rev. 18 (6), 521–529. [DOI] [PubMed] [Google Scholar]
- Mann HB, Whitney DR, 1947. On a test of whether one of two random variables is stochastically larger than the other. Ann. Math. Stat. 18 (1), 50–60. [Google Scholar]
- Marmorstein NR, 2009. Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcohol. Clin. Exp. Res. 33 (1), 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marum G, Clench-Aas J, Nes RB, Raanaas RK, 2014. The relationship between negative life events, psychological distress and life satisfaction: a population-based study. Qual. Life Res. 23 (2), 601–611. [DOI] [PubMed] [Google Scholar]
- Matthews K, Coghill D, Rhodes S, 2008. Neuropsychological functioning in depressed adolescent girls. J. Affect. Disord. 111 (1), 113–118. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT Jr., Terracciano A, Parker WD, Mills CJ, De Fruyt F, et al. , 2002. Personality trait development from age 12 to age 18: longitudinal, cross-sectional, and cross-cultural analyses. J. Pers. Soc. Psychol. 83, 1456–1468. [PubMed] [Google Scholar]
- McKay D, Tolin DF, 2017. Empirically supported psychological treatments and the research domain criteria (RDoC). J. Affect. Disord. 216, 78–88. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC, 2012. Childhood adversities and first onset of psychiatric disorders in a national sample of us adolescents. Arch. Gen. Psychiatry 69 (11), 1151–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMakin DL, Olino TM, Porta G, Dietz LJ, Emslie G, Clarke G, Brent DA, 2012. Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor treatment–resistant depression. J. Am. Acad. Child Adolesc. Psychiatry 51 (4), 404–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNemar Q, 1947. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 12 (2), 153–157. [DOI] [PubMed] [Google Scholar]
- Medeiros GC, Rush AJ, Jha M, Carmody T, Furman JL, Czysz AH, Trombello JM, Cooper CM, Trivedi MH, 2020. Positive and negative valence systems in major depression have distinct clinical features, response to antidepressants, and relationships with immunomarkers. Depression and anxiety 37 (8), 771–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J, 2010. Lifetime prevalence of mental disorders in us adolescents: results from the national comorbidity survey replication–adolescent supplement (ncs-a). J. Am. Acad. Child Adolesc. Psychiatry 49 (10), 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morea A, Calvete E, 2021. Cognitive flexibility and selective attention’s associations with internalizing symptoms in adolescents: are they reciprocal? J. Youth Adolesc. 50 (5), 921–934. [DOI] [PubMed] [Google Scholar]
- Mrazek DA, Hornberger JC, Altar CA, Degtiar I, 2014. A review of the clinical, economic, and societal burden of treatment-resistant depression: 1996–2013. Psychiatr. Serv. 65 (8), 977–987. [DOI] [PubMed] [Google Scholar]
- Murphy KP, 2012. Machine Learning: A Probabilistic Perspective. MIT Press. [Google Scholar]
- Musliner KL, Munk-Olsen T, Eaton WW, Zandi PP, 2016. Heterogeneity in long-term trajectories of depressive symptoms: patterns, predictors and outcomes. J. Affect. Disord. 192, 199–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health, 2011. Definitions of the RDoC Domains and Constructs. https://www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/definitions-of-the-rdoc-domains-and-constructs.
- Nemesure MD, Heinz MV, Huang R, Jacobson NC, 2021. Predictive modeling of depression and anxiety using electronic health records and a novel machine learning approach with artificial intelligence. Sci. Rep. 11 (1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Klein DN, Lewinsohn PM, Rohde P, Seeley JR, 2010. Latent trajectory classes of depressive and anxiety disorders from adolescence to adulthood: descriptions of classes and associations with risk factors. Compr. Psychiatry 51 (3), 224–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Barrera A, Ellis SP, Li S, Burke AK, Grunebaum M, Endicott J, Mann JJ, 2004. Instability of symptoms in recurrent major depression: a prospective study. Am. J. Psychiatr. 161 (2), 255–261. [DOI] [PubMed] [Google Scholar]
- Owens M, Gibb BE, 2017. Brooding rumination and attentional biases in currently non-depressed individuals: an eye-tracking study. Cognit. Emot. 31 (5), 1062–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petito A, Pop TL, Namazova-Baranova L, Mestrovic J, Nigri L, Vural M, Sacco M, Giardino I, Ferrara P, Pettoello-Mantovani M, 2020. The burden of depression in adolescents and the importance of early recognition. J. Pediatr. 218, 265–267. [DOI] [PubMed] [Google Scholar]
- Piko BF, Balázs MÁ, 2012. Control or involvement? Relationship between authoritative parenting style and adolescent depressive symptomatology. Eur. Child Adolesc. Psychiatry 21 (3), 149–155. [DOI] [PubMed] [Google Scholar]
- Pohl KM, Sullivan EV, Podhajsky S, Baker FC, Brown SA, Clark DB, Colrain IM, DeBellis M, Goldston D, Nagel BJ, Nooner KB, Tapert SF, Pfefferbaum A, 2022. The NCANDA_PUBLIC_6Y_REDCAP_v01 Data Release of the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA). 10.7303/syn25606546. [DOI] [Google Scholar]
- Porter RJ, Gallagher P, Thompson JM, Young AH, 2003. Neurocognitive impairment in drug-free patients with major depressive disorder. Br. J. Psychiatry 182 (3), 214–220. [DOI] [PubMed] [Google Scholar]
- Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, Merrow M, 2004. A marker for the end of adolescence. Curr. Biol. 14 (24), R1038–R1039. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Gotlib IH, 2004. Socioemotional functioning in depression. In: Power Mick (Ed.), Mood Disorders: A Handbook of Science and Practice. Wiley, pp. 61–77. [Google Scholar]
- Schulte T, Hong J-Y, Sullivan EV, Pfefferbaum A, Baker FC, Chu W, Prouty D, Kwon D, Meloy MJ, Brumback T, et al. , 2019. Effects of age, sex, and puberty on neural efficiency of cognitive and motor control in adolescents. Brain Imaging Behav. 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short MA, Booth SA, Omar O, Ostlundh L, Arora T, 2020. The relationship between sleep duration and mood in adolescents: a systematic review and meta-analysis. Sleep Med. Rev. 52, 101311. [DOI] [PubMed] [Google Scholar]
- Snyder HR, Friedman NP, Hankin BL, 2019. Transdiagnostic mechanisms of psychopathology in youth: executive functions, dependent stress, and rumination. Cogn. Ther. Res. 43 (5), 834–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spearman C, 1904. The proof and measurement of association between two things. Am. J. Psychol. 15, 72–101. [PubMed] [Google Scholar]
- Speed BC, Nelson BD, Perlman G, Klein DN, Kotov R, Hajcak G, 2015. Personality and emotional processing: a relationship between extraversion and the late positive potential in adolescence. Psychophysiology 52 (8), 1039–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springenberg JT, Dosovitskiy A, Brox T, Riedmiller M, 2014. Striving for Simplicity: The All Convolutional Net. arXiv preprint arXiv:1412.6806. [Google Scholar]
- Su D, Zhang X, He K, Chen Y, 2021. Use of machine learning approach to predict depression in the elderly in China: a longitudinal study. J. Affect. Disord. 282, 289–298. [DOI] [PubMed] [Google Scholar]
- Suhara Y, Xu Y, Pentland AS, 2017. Deepmood: Forecasting depressed mood based on self-reported histories via recurrent neural networks. In: Proceedings of the 26th International Conference on World Wide Web, pp. 715–724. [Google Scholar]
- Thoits PA, 2011. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 52 (2), 145–161. [DOI] [PubMed] [Google Scholar]
- Van Veen T, Wardenaar K, Carlier I, Spinhoven P, Penninx B, Zitman F, 2013. Are childhood and adult life adversities differentially associated with specific symptom dimensions of depression and anxiety? Testing the tripartite model. J. Affect. Disord. 146 (2), 238–245. [DOI] [PubMed] [Google Scholar]
- Vannucci A, Nelson EE, Bongiorno DM, Pine DS, Yanovski JA, Tanofsky-Kraff M, 2015. Behavioral and neurodevelopmental precursors to binge-type eating disorders: support for the role of negative valence systems. Psychol. Med. 45 (14), 2921–2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Stasik SM, Ellickson-Larew S, Stanton K, 2015. Extraversion and psychopathology: a facet-level analysis. J. Abnorm. Psychol. 124 (2), 432. [DOI] [PubMed] [Google Scholar]
- Wendt HW, 1972. Dealing with a common problem in social science: a simplified rank-biserial coefficient of correlation based on the statistic. Eur. J. Soc. Psychol. 2, 463–465. [Google Scholar]
- Woody ML, Gibb BE, 2015. Integrating NIMH research domain criteria (RDoC) into depression research. Curr. Opin. Psychol. 4, 6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu C, Li X, Wang S, Zhang W, 2016. Teacher autonomy support reduces adolescent anxiety and depression: An 18-month longitudinal study. J. Adolesc. 49, 115–123. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


