Abstract
Background
Pregnant persons are at increased risk of severe coronavirus disease 2019 (COVID-19) and adverse obstetric outcomes. Understanding maternal antibody response, duration, and transplacental transfer after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and COVID-19 vaccination is important to inform public health recommendations.
Methods
This prospective observational cohort study included 351 pregnant people who had SARS-CoV-2 infection or COVID-19 vaccination during pregnancy. Immunoglobulin (Ig) G and IgM to SARS-CoV-2 S1 receptor binding domain were measured in maternal and cord blood. Antibody levels and transplacental transfer ratios were compared across (1) disease severity for those with SARS-CoV-2 infection and (2) infection versus vaccination.
Results
There were 252 individuals with SARS-CoV-2 infection and 99 who received COVID-19 vaccination during pregnancy. Birthing people with more severe SARS-CoV-2 infection had higher maternal and cord blood IgG levels (P = .0001, P = .0001). Median IgG transfer ratio was 0.87–1.2. Maternal and cord blood IgG were higher after vaccination than infection (P = .001, P = .001). Transfer ratio was higher after 90 days in the vaccinated group (P < .001). Modeling showed higher amplitude and half-life of maternal IgG following vaccination (P < .0001). There were no significant differences by fetal sex.
Conclusions
COVID-19 vaccination in pregnancy leads to higher and longer lasting maternal IgG levels, higher cord blood IgG, and higher transfer ratio after 90 days compared with SARS-CoV-2 infection. Greater infection severity leads to higher maternal and cord blood antibodies. Maternal IgG decreases over time following both vaccination and infection, reinforcing the importance of vaccination, even after infection, and vaccine boosters for pregnant patients.
Keywords: SARS-CoV-2, COVID-19, vaccination, pregnancy, antibody
There are higher and longer lasting antibodies in pregnant persons and higher antibody levels in cord blood after COVID-19 vaccination compared with SARS-CoV-2 infection, especially in cases of lower disease severity. Antibody levels wane over time following vaccination and infection.
Pregnant persons with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection are at higher risk of severe coronavirus disease 2019 (COVID-19), including hospitalization, intensive care, and death [1–3]. Furthermore, adverse perinatal outcomes such as increased risk of preterm birth, preeclampsia, and stillbirth have been observed with SARS-CoV-2 infection in pregnancy, particularly in moderate–severe disease [1, 3–6]. While the pathophysiological mechanisms leading to increased morbidities in pregnancy are not fully understood, a growing body of literature provides evidence that COVID-19 vaccinations are both safe [7–9] and efficacious [10, 11] in pregnancy. Thus, there is an urgent recommendation to protect pregnant persons from COVID-19 through vaccination [12].
Due to the novel nature of SARS-CoV-2 and exclusion of pregnant patients from initial vaccine trials, the immunologic response in infection and vaccination has been studied through observational studies. SARS-CoV-2 infection in pregnancy generates antibody responses over many weeks [13–17]. In nonpregnant adults, disease severity is associated with antibody levels, which decrease over time after an initial peak [18, 19]. However, is a paucity of information about the duration of antibody titers over time and how pregnancy-specific factors such as fetal sex impact maternal immunologic response to SARS-CoV-2 infection [20]. Vaccine hesitancy in pregnancy remains, and there are limited data on vaccination of pregnant persons following recovery from prior infection.
Maternal antibody response also correlates with infant passive immunity; thus, vaccination during pregnancy remains an important prevention strategy to promote infant health [21]. Transplacental antibody transfer has been shown in the setting of SARS-CoV-2 infection and mRNA vaccination during pregnancy, with varying reported transfer ratios (0.3–1.3) [14, 22–26] and concerns about impaired transplacental transfer after infection [13, 27]. With respect to COVID-19 vaccination, 2 doses of mRNA vaccine [24, 26, 28] and vaccination earlier in pregnancy are associated with higher transfer ratios [29, 30]. Yet, few studies have addressed the duration of vaccine-induced antibody response in pregnancy or have compared vaccine-induced antibodies with natural infection.
We investigated maternal anti-spike protein (S1) receptor binding domain (RBD) immunoglobulin (Ig) G and IgM in pregnant people and umbilical cord blood (herein referred to as infant) at the time of delivery in a large cohort with either SARS-CoV-2 infection or mRNA vaccination in pregnancy. We aimed to specifically assess the association between timing/severity of infection and both maternal and infant antibody levels. In addition, we aimed to compare antibody levels at delivery between pregnant people who were infected with SARS-CoV-2 and those with COVID-19 vaccination.
METHODS
Study Design and Patient Cohort
This is a prospective observational cohort study of pregnant people who delivered at Northwestern Medicine Prentice Women's Hospital in Chicago, Illinois, USA (April 2020–July 2021). Individuals who had SARS-CoV-2 infection or received COVID-19 vaccination during pregnancy were identified via the electronic medical record (EMR). Maternal SARS-CoV-2 infection during pregnancy was defined as either a positive SARS-CoV-2 polymerase chain reaction (PCR) result or provider documentation of a positive test. Demographic and clinical data, including COVID-19 symptoms, laboratory abnormalities, imaging, clinical course, and treatment, were collected through EMR review. SARS-CoV-2 infection severity was defined according to National Institutes of Health criteria as asymptomatic, mild, moderate, severe, and critical [31].
Vaccination date and type were taken from the EMR that interfaces with the Illinois Comprehensive Automated Immunization Registry Exchange (I-CARE). Timing of SARS-CoV-2 infection or vaccination (first dose) was determined by gestational age, utilizing the clinically defined estimated due date [32]. For asymptomatic patients (e.g., who tested positive on routine PCR screening upon admission to Labor and Delivery), the specific timing of infection could not be accurately determined. Thus, for analyses related to timing of infection, these individuals were excluded. Timing from event (infection vs vaccine) to delivery is termed “latency.” We excluded patients who were both vaccinated and had a SARS-CoV-2 infection in pregnancy. This study was approved by the Institutional Review Board of Northwestern University (reference number STU00212232) with a waiver of informed consent obtained prior to initiation of this research.
For all analyses, statistical significance was defined as P <.05. Corrections were not made for multiple comparisons. Analyses were conducted using STATA/IC version 16.0 (StataCorp), R software (R Foundation for Statistical Computing), and Python 3.10.1 (Python Software Foundation).
Maternal and Infant Antibody Detection
After birth, maternal blood and cord blood were retrieved from the clinical laboratory. A maternal specimen is sent to a blood bank for all pregnant people upon admission to Labor and Delivery; cord blood is sent based on maternal blood type (O, Rh-, or positive blood group antibodies). Plasma was separated and stored at −80°C. SARS-CoV-2 IgM and IgG were measured in maternal and infant plasma using the Access SARS-CoV-2 IgG and IgM Antibody tests (DXI Platform; Beckman Coulter) in the Northwestern Memorial Hospital College of American Pathologists/Clinical Laboratory Improvement Amendments (CAP/CLIA)–certified laboratory. The chemiluminescent assay reports quantitative antibodies to the SARS-CoV-2 spike protein S1 RBD in arbitrary units (AU)/mL, with values of 1 or higher being positive. Antibody transfer ratio was calculated as infant IgG divided by maternal IgG concentrations.
Statistical Analysis: SARS-CoV-2 Severity
Demographics, clinical characteristics, maternal and infant IgG at delivery, and IgG transfer ratio were compared between those with SARS-CoV-2 infection across strata of severity. Locally weighted smoothing (LOESS) was applied for univariate regression analysis fitting of antibody plots with respect to latency time.
Differences across severity with respect to latency were evaluated using 2 methods. First, latency from infection was dichotomized at 90 days and median antibody levels were compared across severity subgroups using Kruskal-Wallis analysis of variance (ANOVA). Ninety days was used for clinical relevance (the time frame that reinfection is deemed less likely) [33, 34]. This analysis was performed separately for maternal IgG and infant IgG. Second, mathematical modeling of maternal antibody durability was conducted using amplitude over time by previously described methods [35] (code available at https://github.com/jagstein/antibody_kinetics). This approach assumes 2 antibody secreting populations, 1 with a long half-life (llp) and the other with a short half-life (slp). In this model, the following equation is used:
where IgGt is the IgG level at a latency of t days; amplitude is a measure of intensity; shortprop is the proportion of the IgG-secreting population that is short-lived, hlshort is the half-life of the short-lived population, hlIgG is the half-life of IgG, and hllong is the half-life of the long-lived population. The proportion of IgG-secreting cells that are long-lived is not directly estimated but is simply the proportion of IgG-secreting cells that are not short lived (1−shortprop). Five-fold cross-validation was performed 20 times with shuffling of the IgG analyte (maternal) and categories (mild, moderate, severe, vaccinated). Amplitudes of subcategories were compared using t tests to report statistically significant differences in antibody kinetics between subgroups.
Statistical Analysis: SARS-CoV-2 Infection Versus Vaccination
A similar approach was used to compare characteristics, antibody levels, and transfer ratio in SARS-CoV-2 infection versus vaccination during pregnancy. Univariate LOESS was used for regression analysis of maternal and infant IgG. In addition, latency from either infection or vaccination was dichotomized at 90 days and median antibody levels were compared across subgroups within each latency stratum using Mann-Whitney U tests. Differences in maternal IgG kinetics were also evaluated using the mathematical modeling approach described above. In patients with multiple inoculations, incorporation of a second stimulus/secretion curve did not improve accuracy and so was not further pursued.
Statistical Analysis: Sex as a Biological Variable
Median maternal IgG, infant IgG, and transfer ratios were compared across infant sex using Mann-Whitney U tests. These analyses were repeated separately for those with SARS-CoV-2 infection and who received COVID-19 vaccination.
RESULTS
Study Population and Characteristics
There were 351 pregnant people and 357 infants in the study. Of pregnant people, 252 were diagnosed with SARS-CoV-2 infection and 99 received COVID-19 vaccination during pregnancy. Maternal and neonatal characteristics are reported in Table 1.
Table 1.
Patient Demographics and Delivery Outcomes
| Characteristics | Total Cohort | SARS-CoV-2 Infection | COVID-19 Vaccine | P a |
|---|---|---|---|---|
| Maternal, n | 351 | 252 | 99 | |
| Age, mean (SD), y | 32.5 (5.7) | 31.7 (5.9) | 34.1 (4.9) | <.001 |
| ȃRace | .002 | |||
| ȃWhite | 183 (52.1) | 109 (43.3) | 74 (74.8) | |
| ȃBlack | 31 (8.8) | 29 (11.5) | 2 (2.0) | |
| ȃAsian | 15 (4.3) | 8 (3.2) | 7 (7.1) | |
| ȃOther | 102 (29.1) | 92 (36.5) | 10 (10.1) | |
| ȃUnknown | 20 (5.7) | 14 (5.6) | 6 (6.1) | |
| ȃLatinx | 122 (35.8) | 115 (46.6) | 7 (7.5) | <.001 |
| Public insurance | 113 (32.2) | 109 (43.3) | 4 (4.0) | <.001 |
| Multiple gestations | 5 (1.4) | 4 (1.6) | 1 (1.0) | |
| Preterm birth | 37 (10.5) | 32 (12.7) | 5 (5.1) | .035 |
| Nulliparous | 129 (35.8) | 105 (41.7) | 24 (24.2) | .002 |
| Comorbidities | ||||
| ȃAsthma | 40 (11.4) | 35 (13.9) | 5 (5.1) | .024 |
| ȃDiabetes | 28 (8.0) | 25 (9.9) | 3 (3.0) | .03 |
| ȃObesity | 185 (52.7) | 156 (61.9) | 29 (29.3) | <.001 |
| ȃTobacco use | 32 (9.1) | 28 (11.1) | 4 (4.0) | .04 |
| ȃChronic hypertension | 7 (1.99) | 7 (2.78) | 0 | .19 |
| Gestational age at exposure, mean (SD), wks | 29.6 (8.9) | 29.0 (9.9) | 31.3 (5.3) | .62 |
| Infant, n | 357 | 256 | 101 | |
| ȃSex (female) | 181 (50.7) | 134 (52.3) | 47 (46.5) | .38 |
| ȃCord blood available | 298 (83) | 234 (91) | 64 (63) |
Data are presented as n (%) unless otherwise indicated.
Abbreviations: COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SD, standard deviation.
Significant differences between the SARS-CoV-2 infection and COVID-19 vaccination groups for maternal age, race/ethnicity, public insurance, parity, asthma, obesity, diabetes, and tobacco use in our cohort, representative of national trends [36].
Maternal Disease Severity
Of those with SARS-CoV-2 infection, severity categories were 64 (26%) asymptomatic, 140 (56%) mild disease, 32 (13%) moderate disease, and 12 (5%) severe/critical disease (Supplementary Table 1). The majority of pregnant people were symptomatic at diagnosis: 83% (20/24) in the first trimester, 95% (59/62) in the second trimester, and 65% (105/162) in the third trimester. There was no statistically significant difference in median latency based on severity (mild: 65.5 days; interquartile range [IQR]: 25–124 days); moderate: 70.5 days; IQR: 27–128 days; severe/critical: 60 days; IQR: 13–104 days; P = .67). Of pregnant people with infection, 63% had a positive IgG (>1 AU/mL) at delivery with a median of 1.67 AU/mL (IQR: 0.45–6.24), which was similar for the subset with symptomatic infection (66% positive IgG; median: 1.71 AU/mL; IQR: 0.60–7.79). Infant IgM was positive in 4 infants (range: 1.1–3.6 AU/mL). Infant IgG following maternal infection was positive in 58% (median IgG: 1.28 AU/mL; IQR: 0.37–5.86). In the subset with symptomatic infection, 63% of infants had positive IgG (median: 1.69 AU/mL; IQR: 0.56–7.94).
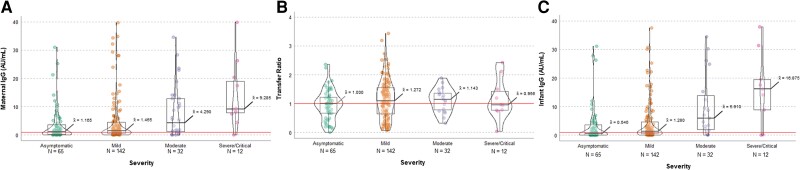
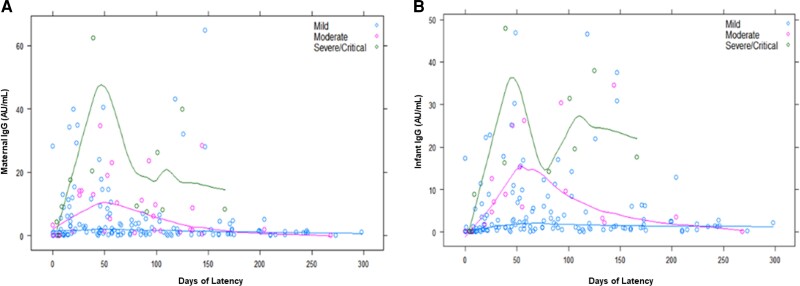
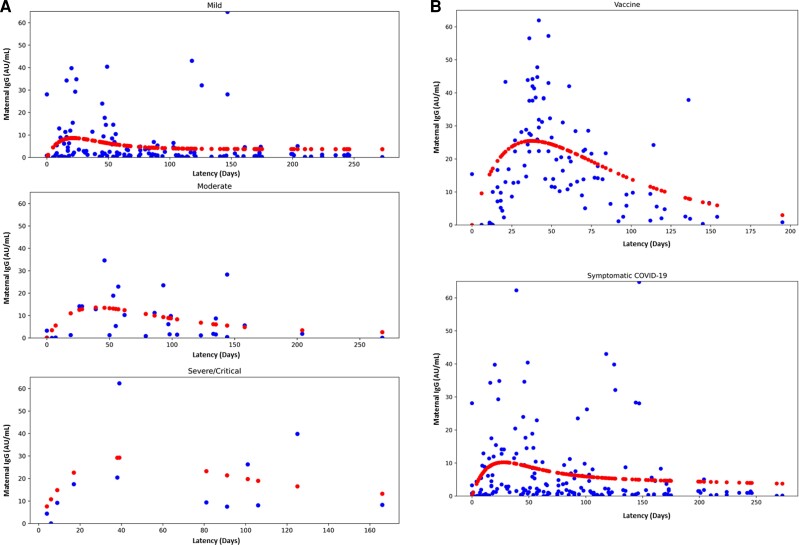
Pregnant people with greater severity of SARS-CoV-2 infection were more likely to have higher maternal and infant IgG levels (P = .0001 and P = .0001) (Figure 1). More severe infection was also more likely to result in positive maternal IgG (asymptomatic 55% vs mild 61% vs moderate 78% vs severe 92%; P = .02), a trend that was also reflected in infant IgG levels (asymptomatic 45% vs mild 60% vs moderate 79% vs severe/critical 80%; P = .026). Median IgG transfer ratio ranged from 0.87 to 1.2 and was not significantly different across severity categories (P = .29). The LOESS plots in Figure 2 show the best-fit trend of maternal IgG and infant IgG for patients with symptomatic SARS-CoV-2 infection with respect to latency. Dichotomizing latency to fewer and more than 90 days (Supplementary Table 2), median maternal IgG levels were higher after more severe infection after 90 days of latency (P < .001) but did not reach statistical significance at 90 days or fewer (P = .085). Similarly, infant IgG was significantly higher with greater severity when infection was more than 90 days prior to delivery (P = .004) but not significantly different if latency was 90 days or fewer (P = .21). Transfer ratios were not significantly different across severity groups (P = .78 for ≤ 90-day latency and P = .67 for >90-day latency). Mathematical modeling demonstrated significantly higher maternal IgG amplitude and longer-half life with greater disease severity (P < .0001 across severity categories and in individual comparisons of mild vs moderate, moderate vs severe, mild vs severe). Models are displayed in Figure 3A.
Figure 1.
Antibody data by severity of maternal SARS-CoV-2 infection. A, Maternal IgG, *P = .0001. B, Transfer ratio (infant IgG:maternal IgG), P = NS. C, Infant IgG, *P = .0001 across disease maternal disease severity categories. Comparison by Kruskal-Wallis ANOVA. Abbreviations: ANOVA, analysis of variance; AU, arbitrary units; IgG, immunoglobulin G; NS, not significant; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Figure 2.
Antibody levels by severity of maternal SARS-CoV-2 infection with respect to latency from SARS-CoV-2 infection to delivery. A, Maternal IgG. B, Infant IgG. Severity: green = severe, pink = moderate, blue = mild. Locally weighted smoothing (LOESS) was applied for univariate regression analysis fitting of antibody plots with respect to latency time. Abbreviations: AU, arbitrary units; IgG, immunoglobulin G; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Figure 3.
Mathematical models of maternal IgG level. Mathematical models of maternal IgG level (A) across severity categories and (B) vaccination versus symptomatic SARS-CoV-2 infection. Blue = individual data points, red = kinetics model. Abbreviations: AU, arbitrary units; COVID-19, coronavirus disease 2019; IgG, immunoglobulin G; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
SARS-CoV-2 Infection and Vaccination
Significant differences were noted in maternal age, race/ethnicity, public insurance, parity, asthma, obesity, diabetes, tobacco use, and preterm birth (P = .035) among the SARS-CoV-2 infection group compared with the vaccinated group (Table 1). Sixty-four percent of vaccinations were Pfizer NT162b2, 32% had Moderna mRNA-1273, and 4% were unknown. The first dose was during the second trimester for 17% and during the third trimester for 83% of patients. Twenty patients (20% of the vaccinated group) received only 1 dose of vaccine prior to delivery. The median latency between SARS-CoV-2 infection and delivery was 66 days (IQR: 25–124), whereas the latency between first-dose vaccination and delivery was 46 days (IQR: 33–71) (P = .007).
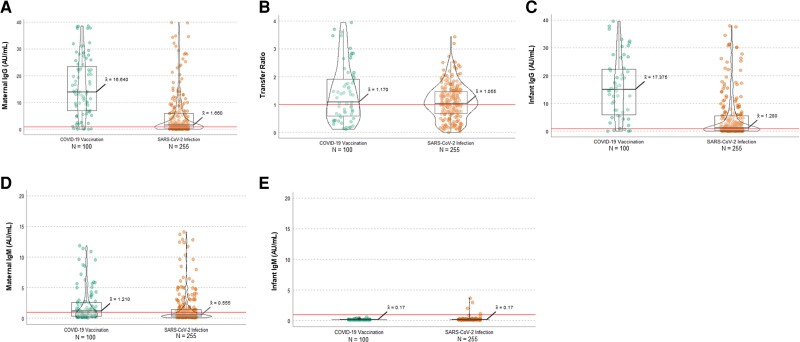
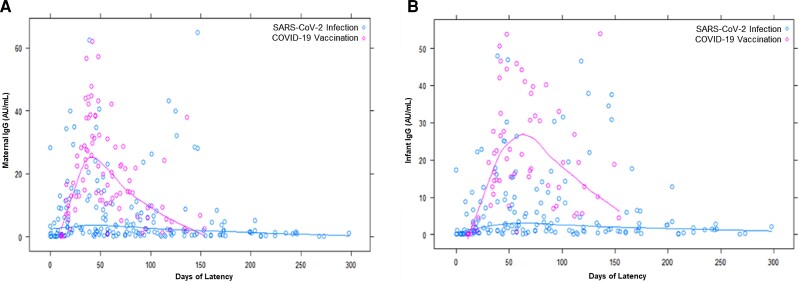
The majority of vaccinated individuals (92%) had positive maternal IgG levels (median: 16.64 AU/mL; IQR: 8.58–28.53) and 89% had positive infant IgG (median: 17.38 AU/mL; IQR: 7.60–31.26). Overall, maternal IgG levels were higher in the vaccinated group compared with the infection group (16.64 vs 1.66; P = .001) as were infant IgG levels (17.6 vs 1.28 AU/mL; P = .001). Maternal IgM was slightly higher in the vaccinated group (IgM: 1.21 vs 0.56 AU/mL; P = .001). There was no difference in infant IgM levels (0.17 vs 0.17 AU/mL; P = 1.00). Four infants of mothers with SARS-CoV-2 infection and no infants of mothers who received vaccination had positive IgM levels. Patients who were vaccinated during pregnancy were more likely to have maternal IgG levels greater than 1 AU/mL compared with those with SARS-CoV-2 infection (92% vs 63%; P < .001), a trend reflected in infant IgG as well (90% of vaccination group vs 58% of infection group; P < .001). Figure 4 demonstrates the distribution of maternal IgG, infant IgG, and transfer ratio following infection and vaccination, respectively. LOESS plots in Figure 5 show best-fit curves for maternal IgG and infant IgG in the vaccinated and SARS-CoV-2 infection groups by latency. Vaccinated individuals had higher maternal IgG and infant IgG levels that are longer lasting, although there was a downward trend after approximately day 50 and they were notably low by approximately 150 days from exposure.
Figure 4.
Antibody data in vaccination versus SARS-CoV-2 infection. A, Maternal IgG, *P = .001. B, Transfer ratio (infant IgG:maternal IgG), P = NS. C, Infant IgG, *P = .001. D, Maternal IgM, *P = .001. E, Infant IgM, P = 1.0. Comparisons were made using Mann-Whitney U tests. Abbreviations: AU, arbitrary units; COVID-19, coronavirus disease 2019; IgG, immunoglobulin G; IgM, immunoglobulin M; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Figure 5.
Antibody levels for vaccinated and SARS-CoV-2 infection groups with respect to latency from exposure (first vaccine, infection) to delivery. A, Maternal IgG. B, Infant IgG. Category: pink = vaccination, blue = SARS-CoV-2 infection. Locally weighted smoothing (LOESS) was applied for univariate regression analysis fitting of antibody plots with respect to latency time. Abbreviations: AU, arbitrary units; COVID-19, coronavirus disease 2019; IgG, immunoglobulin G; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Median maternal IgG was significantly higher at delivery in the vaccinated group across latency time frames (≤ 90 days: 20.40 vs 2.67; P = .001; >90 days: 5.17 vs 1.21; P < .001). Similarly, infant IgG was significantly higher in the vaccinated group (≤ 90 days: 19.79 vs 1.82; P < .001; >90 days: 12.57 vs 1.36; P < .001). Transfer ratios were not significantly different if latency was 90 days or fewer (0.92 vs 0.94; P = .66) but were higher if more than 90 days had passed since infection or vaccination (2.84 vs 1.37; P < .001). Mathematical modeling demonstrated significantly higher maternal IgG amplitude and longer-half life in vaccinated people compared with infection (P < .0001). Models are displayed in Figure 3B.
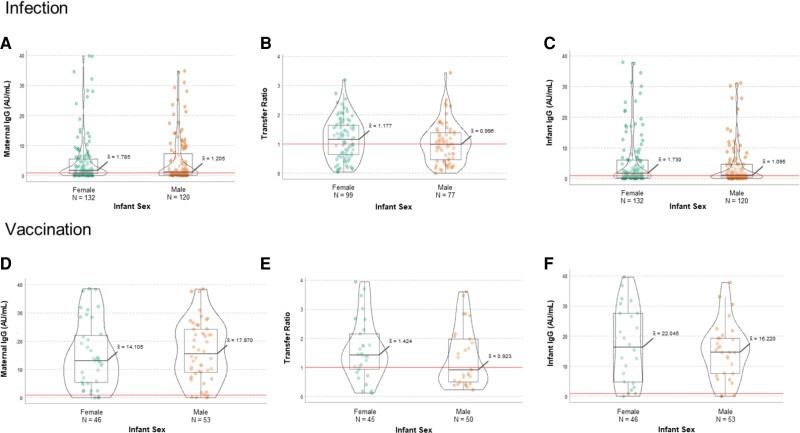
Comparison With Respect to Fetal Sex
There were no statistically significant differences by fetal sex in maternal IgG, infant IgG, or transfer ratio in either the vaccinated group or infection group or in pooled analysis of the entire cohort (combining vaccination and infection) (Supplementary Table 3, Figure 6).
Figure 6.
Antibody data by fetal sex. SARS-CoV-2 infection: A, Maternal IgG; B, transfer ratio (infant IgG:maternal IgG); C, infant IgG. Vaccination: D, Maternal IgG; E, transfer ratio; F, infant IgG by fetal sex (female vs male). All comparisons P = NS using Mann-Whitney U tests. Abbreviations: AU, arbitrary units; IgG, immunoglobulin G; NS, not significant; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
DISCUSSION
In this prospective observational cohort study, we addressed maternal and infant antibody levels and transplacental transfer following SARS-CoV-2 infection and vaccination, particularly with respect to latency. Given the potential adverse maternal and obstetric effects of SARS-CoV-2 infection, the goal of vaccination is to optimally protect the pregnant person. Thus, it is imperative to understand the durability of protection after SARS-CoV-2 infection and COVID-19 vaccination. Additionally, because infants younger than 6 months of age are vulnerable and require a unique vaccination strategy, antibody transfer to the fetus is an important strategy to optimize protection in infancy. Recent data demonstrated decreased hospitalizations among infants younger than 6 months whose mother received COVID-19 vaccination during pregnancy [37].
There are limited data on immune response in relation to disease severity in pregnant people. Prior work by Flannery et al [14] noted that mothers with moderate–critical illness had higher maternal and infant IgG, but the differences were not statistically significant. Our data demonstrate through stratified analysis and modeling that greater severity of infection is associated with higher and longer lasting maternal antibody levels and higher cord blood IgG. Antibody levels decrease over time, particularly after mild infection in nonpregnant individuals [38, 39]. In our study, pregnant persons with SARS-CoV-2 infection had a clear increase in IgG with a peak approximately 6 weeks from first vaccination and then a significant decrease by 4–5 months. People with asymptomatic and mild infection yielded lower antibody levels sooner. These data emphasize the need for vaccination as a protective strategy for pregnant people, even after natural SARS-CoV-2 infection during pregnancy.
There is evolving recent literature about the timing of vaccination in pregnancy and duration of antibody response. Our study demonstrates that vaccination induces higher and longer lasting antibody levels in pregnant persons and their newborns than SARS-CoV-2 infection, while also avoiding potential complications of COVID-19. The timing of vaccination, duration of response, and transplacental transfer to infant have shown various results across studies, including the highest delivery antibodies after early third-trimester vaccination [29, 30, 40]. Our data, although limited to the second and third trimester, show evidence that vaccination results in superior maternal and infant antibody levels compared with infection, and that this difference is pronounced, along with a significant difference in transfer ratio, in the setting of longer latency. Nevertheless, there are decreasing antibody levels over time and thus this study reinforces the potential importance and current recommendation of boosting maternal immunity with an additional dose if many months have passed since the primary vaccine series.
In translational work by Bordt et al [20], mothers carrying male fetuses had lower maternal IgG and transfer ratio following third-trimester SARS-CoV-2 infection than pregnancies with female fetuses. The possibility that fetal sex modifies maternal antibody response or placental transfer is intriguing. Our data, however, did not find any statistically significant differences in maternal IgG level or transfer ratio according to fetal sex after SARS-CoV-2 infection or vaccination, in overall analysis and stratified analysis limited to third-trimester infection. Further dedicated work is needed in this area. It is also of note that no infants of mothers who received vaccination had positive IgM and a few infants had low positive IgM following maternal SARS-CoV-2 infection (asymptomatic–mild, 0–49 days prior to delivery). Infants with positive IgM had negative SARS-CoV-2 PCR testing. Thus, these results may reflect intrauterine vertical transmission, albeit rare, versus likely false-positive results [41].
The strengths of this study include the following: (1) the large cohort of samples from pregnant people and umbilical cord following vaccination or infection during pregnancy, (2) accurate detailed clinical information about infection severity and timing, and (3) a consistent platform for anti-S1 RBD. Additionally, the mathematical modeling approach to maternal antibody kinetics adds to the statistical validity of severity and vaccine versus natural infection comparisons. Limitations include the 1 time point of antibody measurements at delivery, single center, and latency for the vaccination group being shorter than for the infection group. Additionally, our LOESS regressions were limited to univariate analyses to avoid overfitting models and could not include clinical covariates in multivariable-adjusted models. Circulating anti-S1 RBD antibody is also only 1 measure of protection and does not account for aspects of immunologic memory. Although we did not measure neutralizing antibody, anti-S IgG correlates closely with neutralizing activity patterns [18, 40]. In addition, given the time frame of this cohort, the effects of booster vaccination during pregnancy and SARS-CoV-2 infection after prior vaccination are not assessed.
In conclusion, COVID-19 vaccination in pregnancy leads to higher and longer lasting maternal IgG and higher infant IgG levels than natural SARS-CoV-2 infection. Vaccination results in higher transplacental antibody transfer ratios than infection after longer latency. Severity of infection is also associated with higher and longer lasting antibodies. Maternal IgG antibody levels decrease over time in pregnant patients following both vaccination and natural infection, reinforcing the importance of (1) vaccination even after infection and (2) a potential booster dose if many months have elapsed from the initial series or in the context of new variants, to optimize protection of pregnant individuals and their infants.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Contributor Information
Sebastian Otero, Ann & Robert H. Lurie Children's Hospital of Chicago and Stanley Manne Children's Research Institute, Chicago, Illinois, USA.
Emily S Miller, Department of Obstetrics and Gynecology, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA.
Ashwin Sunderraj, Department of Pediatrics, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA.
Elisheva D Shanes, Department of Pathology, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA.
Allie Sakowicz, Department of Obstetrics and Gynecology, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA.
Jeffery A Goldstein, Department of Pathology, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA.
Leena B Mithal, Ann & Robert H. Lurie Children's Hospital of Chicago and Stanley Manne Children's Research Institute, Chicago, Illinois, USA; Department of Pediatrics, Northwestern University Feinberg School of Medicine, Chicago, Illinois, USA.
Notes
Acknowledgments. The authors thank the staff of the Northwestern Prentice Women's Hospital Obstetric COVID Unit, the Northwestern Memorial Hospital Blood Bank, and the Northwestern Memorial Hospital Chemistry Lab, for sample processing and antibody assays that helped make this study possible. They also acknowledge contributions of students and research staff who participated in data collection: Antonia Willnow, Rebecca Ebbott, Raveena Aggarwal, Hooman Azad, Chiedza Mupanomunda, Alexandra Isaia, and Allaa Fadl-Alla.
Financial support. This work was supported by funding from Friends of Prentice (to J. A. G., E. D. S., E. S. M., and L. B. M.) and the Stanley Manne Children's Research Institute (to L. B. M). Investigators are supported by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health (grant number K23 AI139337; to L. B. M.) and the National Institute of Biomedical Imaging and Bioengineering at the National Institutes of Health (grant number K08 EB030120; to J. A. G.). The project benefited from institutional resources supported by the National Center for Advancing Translational Sciences (UL1TR001422).
Potential conflicts of interest. J. A. G. reports grants from Friends of Prentice and the National Institutes of Health (NIH; K08 EB030120). L. B. M. reports support from Friends of Prentice and NIH (K23 AI139337) and a Stanley Manne Children's Research Institute grant. E. S. M. and E. D. S. also report being co-investigators on a Friends of Prentice grant. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Woodworth KR, Olsen EO, Neelam V, et al. Birth and infant outcomes following laboratory-confirmed SARS-CoV-2 infection in pregnancy—SET-NET, 16 jurisdictions, March 29-October 14, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1635–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zambrano LD, Ellington S, Strid P, et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22-October 3, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1641–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Metz TD, Clifton RG, Hughes BL, et al. Association of SARS-CoV-2 infection with serious maternal morbidity and mortality from obstetric complications. JAMA 2022; 327:748–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Karasek D, Baer RJ, McLemore MR, et al. The association of COVID-19 infection in pregnancy with preterm birth: a retrospective cohort study in California. Lancet Reg Health Am 2021; 2:100027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lai J, Romero R, Tarca AL, et al. SARS-CoV-2 and the subsequent development of preeclampsia and preterm birth: evidence of a dose-response relationship supporting causality. Am J Obstet Gynecol 2021; 225:689–693, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DeSisto CL, Wallace B, Simeone RM, et al. Risk for stillbirth among women with and without COVID-19 at delivery hospitalization—United States, March 2020-September 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1640–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention . COVID-19 vaccines while pregnant or breastfeeding. Updated 14 July 2022. Available at: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html. Accessed 15 July 2022.
- 8. Shimabukuro TT, Kim SY, Myers TR, et al. Preliminary findings of mRNA COVID-19 vaccine safety in pregnant persons. N Engl J Med 2021; 384:2273–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kharbanda EO, Haapala J, DeSilva M, et al. Spontaneous abortion following COVID-19 vaccination during pregnancy. JAMA 2021; 326:1629–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lipkind HS, Vazquez-Benitez G, DeSilva M, et al. Receipt of COVID-19 vaccine during pregnancy and preterm or small-for-gestational-age at birth—eight integrated health care organizations, United States, December 15, 2020-July 22, 2021. MMWR Morb Mortal Wkly Rep 2022; 71:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Goldshtein I, Nevo D, Steinberg DM, et al. Association between BNT162b2 vaccination and incidence of SARS-CoV-2 infection in pregnant women. JAMA 2021; 326:728–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Morgan JA, Biggio JR Jr, Martin JK, et al. Maternal outcomes after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in vaccinated compared with unvaccinated pregnant patients. Obstet Gynecol 2022; 139:107–9. [DOI] [PubMed] [Google Scholar]
- 13. Edlow AG, Li JZ, Collier AY, et al. Assessment of maternal and neonatal SARS-CoV-2 viral load, transplacental antibody transfer, and placental pathology in pregnancies during the COVID-19 pandemic. JAMA Netw Open 2020; 3:e2030455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Flannery DD, Gouma S, Dhudasia MB, et al. Assessment of maternal and neonatal cord blood SARS-CoV-2 antibodies and placental transfer ratios. JAMA Pediatr 2021; 175:594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cosma S, Carosso AR, Corcione S, et al. Longitudinal analysis of antibody response following SARS-CoV-2 infection in pregnancy: from the first trimester to delivery. J Reprod Immunol 2021; 144:103285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Legros V, Denolly S, Vogrig M, et al. A longitudinal study of SARS-CoV-2-infected patients reveals a high correlation between neutralizing antibodies and COVID-19 severity. Cell Mol Immunol 2021; 18:318–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang K, Long QX, Deng HJ, et al. Longitudinal dynamics of the neutralizing antibody response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Clin Infect Dis 2021; 73:e531–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bordt EA, Shook LL, Atyeo C, et al. Maternal SARS-CoV-2 infection elicits sexually dimorphic placental immune responses. Sci Transl Med 2021; 13:eabi7428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Munoz FM, Jamieson DJ. Maternal immunization. Obstet Gynecol 2019; 133:739–53. [DOI] [PubMed] [Google Scholar]
- 20. Rottenstreich A, Zarbiv G, Oiknine-Djian E, Zigron R, Wolf DG, Porat S. Efficient maternofetal transplacental transfer of anti- severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike antibodies after antenatal SARS-CoV-2 BNT162b2 messenger RNA vaccination. Clin Infect Dis 2021; 73:1909–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gray KJ, Bordt EA, Atyeo C, et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol 2021; 225:303.e1–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mithal LB, Otero S, Shanes ED, Goldstein JA, Miller ES. Cord blood antibodies following maternal coronavirus disease 2019 vaccination during pregnancy. Am J Obstet Gynecol 2021; 225:192–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Song D, Prahl M, Gaw SL, et al. Passive and active immunity in infants born to mothers with SARS-CoV-2 infection during pregnancy: prospective cohort study. BMJ Open 2021; 11:e053036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Beharier O, Plitman Mayo R, Raz T, et al. Efficient maternal to neonatal transfer of antibodies against SARS-CoV-2 and BNT162b2 mRNA COVID-19 vaccine. J Clin Invest 2021; 131:e154834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Atyeo C, Pullen KM, Bordt EA, et al. Compromised SARS-CoV-2-specific placental antibody transfer. Cell 2021; 184:628–642.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Atyeo C, DeRiso EA, Davis C, et al. COVID-19 mRNA vaccines drive differential antibody fc-functional profiles in pregnant, lactating, and nonpregnant women. Sci Transl Med 2021; 13:eabi8631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang YJ, Murphy EA, Singh S, et al. Association of gestational age at coronavirus disease 2019 (COVID-19) vaccination, history of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, and a vaccine booster dose with maternal and umbilical cord antibody levels at delivery. Obstet Gynecol 2022; 139:373–80. [DOI] [PubMed] [Google Scholar]
- 28. Rottenstreich A, Zarbiv G, Oiknine-Djian E, et al. The effect of gestational age at BNT162b2 mRNA vaccination on maternal and neonatal SARS-CoV-2 antibody levels. Clin Infect Dis 2022; 75:e603–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. National Institutes of Health . COVID-19 treatment guidelines: clinical spectrum of SARS-CoV-2 Infection. 2021. Available at: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-spectrum/. Accessed 15 July 2022.
- 30. Committee opinion no 700: methods for estimating the due date. Obstet Gynecol 2017; 129(5):e150–4. [DOI] [PubMed]
- 31. Dan JM, Mateus J, Kato Y, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science 2021; 371:eabf4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention . Science Brief: SARS-CoV-2 infection-induced and vaccine-induced immunity. Updated 29 October 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/vaccine-induced-immunity.html. Accessed 15 July 2022. [PubMed]
- 33. White M, Idoko O, Sow S, et al. Antibody kinetics following vaccination with MenAfriVac: an analysis of serological data from randomised trials. Lancet Infect Dis 2019; 19:327–36. [DOI] [PubMed] [Google Scholar]
- 34. Centers for Disease Control and Prevention . COVID Data Tracker: pregnancy data. Available at: https://covid.cdc.gov/covid-data-tracker/#pregnancy-data. Accessed 15 July 2022.
- 35. Halasa NB, Olson SM, Staat MA, et al. Maternal vaccination and risk of hospitalization for COVID-19 among infants. N Engl J Med 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Long QX, Tang XJ, Shi QL, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med 2020; 26:1200–4. [DOI] [PubMed] [Google Scholar]
- 37. Choe PG, Kim KH, Kang CK, et al. Antibody responses 8 months after asymptomatic or mild SARS-CoV-2 infection. Emerg Infect Dis 2021; 27:928–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kugelman N, Nahshon C, Shaked-Mishan P, et al. Maternal and neonatal SARS-CoV-2 immunoglobulin G antibody levels at delivery after receipt of the BNT162b2 messenger RNA COVID-19 vaccine during the second trimester of pregnancy. JAMA Pediatr 2022; 176:290–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Joseph NT, Dude CM, Verkerke HP, et al. Maternal antibody response, neutralizing potency, and placental antibody transfer after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Obstet Gynecol 2021; 138:189–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Collier AY, McMahan K, Yu J, et al. Immunogenicity of COVID-19 mRNA vaccines in pregnant and lactating women. JAMA 2021; 325:2370–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Prabhu M, Murphy EA, Sukhu AC, et al. Antibody response to coronavirus disease 2019 (COVID-19) messenger RNA vaccination in pregnant women and transplacental passage into cord blood. Obstet Gynecol 2021; 138:278–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.