Abstract
Background
Antimicrobial resistance (AMR) has been deepening in the layer poultry sector in Zambia partly due to the inappropriate use of antimicrobials. Escherichia coli (E. coli), a commensal and zoonotic bacterium, can potentially be a source of AMR.
Objectives
This study assessed the phenotypic AMR profiles of E. coli isolated from the apparent health-laying hens in Lusaka and Copperbelt provinces of Zambia.
Methods
A cross-sectional study was conducted between September 2020 and April 2021 in which 365 cloacal swabs were collected from 77-layer farms based in Lusaka and Copperbelt provinces of Zambia. E. coli isolation and identification were done using cultural and biochemical properties and confirmed using the 16S rRNA gene sequencing. Antimicrobial susceptibility testing (AST) was done using the Kirby–Bauer disc-diffusion method. Data analysis was done using WHONET 2020 and Stata v.16.1.
Results
Of the 365 samples, E. coli was isolated from 92.9% (n = 339). The AMR was detected in 96.5% (n = 327) of the isolates, of which 64.6% (n = 219) were multidrug-resistant (MDR). E. coli was highly resistant to tetracycline (54.6%) and ampicillin (54%) but showed low resistance to meropenem (0.9%), ceftazidime (6.2%) and chloramphenicol (8.8%).
Conclusion
This study found a high prevalence of E. coli resistant to some commonly used antibiotics in poultry, which is a public health concern because of the potential contamination of eggs and layers of chicken meat that enter the food chain. Urgent attention is needed, including strengthening antimicrobial stewardship and surveillance programmes in layer poultry production in Zambia.
Introduction
Antimicrobial resistance (AMR) has increased in poultry over the past decade due to the inappropriate use of antimicrobial agents.1–4 Antimicrobial agents have primarily been used for improved egg production, growth promotion, prophylaxis, metaphylaxis and therapeutics in the poultry industry.5–8 The use of antimicrobials in poultry production can be attributed to the increased demand for poultry products such as chicken meat and eggs.9,10 This has contributed to the continuous exposure of poultry microorganisms to antimicrobials and, thus, the development of AMR.11,12Escherichia coli (E. coli) are among the commensal or pathogenic microorganisms isolated from poultry that have become resistant to common antibiotics used in human and animal health.13–16E. coli causes infections such as urinary tract infections, bloodstream infections, sepsis and meningitis.17–19
In the poultry sector, the effect of AMR can cause economic losses due to challenges in containing antimicrobial-resistant infections, increased mortality, costs associated with the disposal of carcasses and the compromise on safety and security.20 In the public sector, AMR leads to increased medical costs, prolonged hospital stays and increased mortality.21–23 If this problem is not addressed, it is estimated to cause 10 million human deaths globally by the year 2050.24–26
Imprudent use of antimicrobials among poultry farmers worldwide have contributed to the emergence and spread of AMR.27–30 Studies have shown that most poultry farmers are unaware of the implications of inappropriate use of antimicrobials that leads to AMR.31–33 The ease of access to antibiotics without prescriptions has contributed to their inappropriate use.31,34 Poultry farmers’ high antibiotic demand often drives this to enhance production.3,31,34 This issue has been exacerbated by the ready availability and sale of antibiotics in drug stores and through street vendors.34,35 Additionally, antibiotics are incorrectly used in poultry to treat viral infections.36 Consequently, some poultry farmers administer lower doses of antibiotics to their chickens and usually stop before the course is completed, provided their birds look in fair health.8
At a global level, antimicrobial-resistant E. coli has been isolated from poultry.37–40E. coli was reportedly resistant to antimicrobials, including tetracycline, trimethoprim, ampicillin and gentamicin.36,41,42 Alongside the reported AMR profiles of E. coli, there are reports of multidrug-resistant (MDR) E. coli isolated from poultry.41,43,44 This is of public health concern and puts pressure on animal and human health prescribers when choosing antibiotics to prescribe for a particular condition. Additionally, antimicrobial-resistant E. coli can be transmitted from poultry to humans and cause infections that may be difficult or impossible to treat.15,45–48 As this problem can affect both humans and animals, there is a need to enhance the one health approach to address it.49–52
In Africa, some reports have been documented on the resistance patterns of E. coli isolated from poultry in some studies.16,53–58E. coli resistant to ampicillin, tetracycline, cotrimoxazole, ciprofloxacin and gentamicin has been identified. Besides, MDR E. coli isolated from poultry was reported from different studies, with 76% in Bangladesh,15 78.1% in Ethiopia,59 98.1% in Nigeria60 and 86.76% in Tanzania.53 This reported resistance to antimicrobials highlights the need for the prudent use in poultry farming.
In Zambia, antimicrobial-resistant E. coli have been isolated from humans,61,62 broiler chickens,63,64 dairy65 and wildlife and livestock.66 In broilers, E. coli, was observed to be resistant to tetracycline, ampicillin, cotrimoxazole and ciprofloxacin, whereas, in dairy, it was resistant to tetracycline, ampicillin, cotrimoxazole and ciprofloxacin.65 Besides, E. coli isolates from wildlife and livestock were highly resistant to ampicillin (27%), ceftazidime (14.3%), cefotaxime (9.5%) and kanamycin (9.5%).66 In these animal species, a prevalence of 36.5% MDR was reported in broilers63% and 18.8% in wildlife.66 However, the study of the prevalence and AMR profiles of E. coli isolated from laying hens in Zambia was not reported prior to this study.
The reported AMR in Zambia requires enhancement and implementation strategies to address this problem. Among the proposed strategies, the Zambia Multi-sectoral National Action Plan (NAP) on AMR, launched in 2017, aimed at addressing this problem in humans and animals.67,68 The NAP on AMR was developed in line with the Global Action Plan on AMR to successfully prevent and treat infections across all populations with safe and effective medicines and reduce AMR.69 The NAP on AMR strives to address AMR in animals and humans by increasing awareness and knowledge of AMR among different populations and promoting the rational use of antimicrobials.67 Alongside this, strengthening antimicrobial stewardship (AMS) and surveillance programmes are critical in addressing AMR across humans and animals.67,69–74 This study assessed the AMR profiles of E. coli isolated from laying hens in Lusaka and Copperbelt provinces of Zambia.
Materials and methods
Study design, site and population
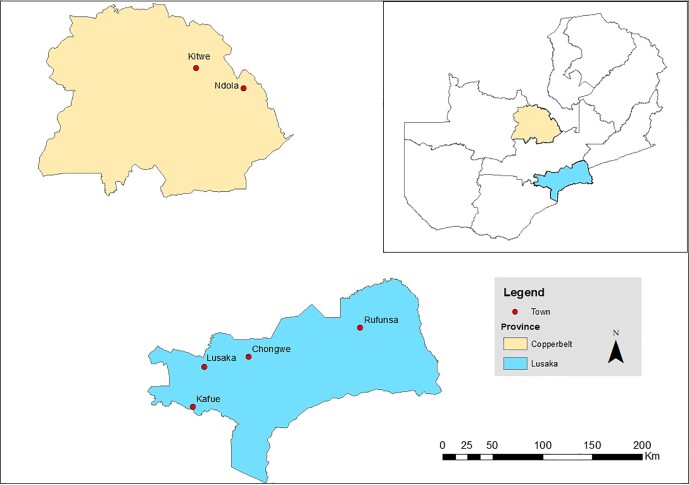
A cross-sectional study was conducted in layer farms of Lusaka and Copperbelt provinces from September 2020 to April 2021. The two provinces contribute (75%) to poultry production in the country.75 On the basis of information from the Poultry Association of Zambia, Lusaka province contributes 50% while Copperbelt province contributes 25% to poultry production.75 The study sites are shown in Figure 1.
Figure 1.
Map of Zambia indicating the study sites in Lusaka and Copperbelt provinces (ARCGis: 2021).
Study population and sampling
This study enrolled layer poultry farmers after obtaining informed consent. The study participants were poultry farmers who were rearing laying hens and resided in Zambia's Lusaka and Copperbelt provinces. A multi-stage sampling method was used to select six districts, farms and later laying hens from the poultry houses. All layers in the production age were sampled randomly to increase the chances of all hens being selected. However, laying hens that were on antibiotic treatment or sick during data collection were excluded from the study. We used registers from the District Veterinary Offices and the Poultry Association of Zambia to identify the layer poultry farmers. Farm visits were conducted with the help of Veterinary Assistants. The layer poultry farms were categorized into small-scale (farmers rearing up to 1000 hens), medium-scale (farmers rearing 1001 to 10 000 hens) and large-scale (farmers rearing greater than 10 000 hens). On the basis of the registers from the District Veterinary Offices and the Poultry Association of Zambia, active layer poultry farmers were estimated to be 96, i.e. 56 from Lusaka and 40 from the Copperbelt province. A recent study also reported this estimated population of layer poultry farms.31 Before sampling, the sample size was estimated using Ausvet Epitools (https://epitools.ausvet.com.au/) at a 95% confidence level, 50% estimated proportion and a 5% desired precision, as reported in a similar poultry study.76 Because there were few layer poultry farms that were identified and active in rearing laying hens, we conducted a complete enumeration to recruit all the farmers, which resulted in the recruitment of 77-layer poultry farms.
At each farm, laying hens were randomly sampled per 25 m2 (sampling unit) from each poultry house. A cloacal swab was collected from each laying hen per sampling unit and pre-enriched in 10 millilitres (mL) of buffered peptone water (BPW) broth (Oxoid, Basingstoke, UK). The pre-enriched samples were then transported within eight hours of collection to the Public Health Laboratory at the School of Veterinary Medicine at University of Zambia, for processing and analysis. A total of 365 cloacal swab samples were collected and processed for E. coli isolation.
Isolation and identification of E. coli isolates
To isolate E. coli, the samples were incubated in the pre-enriched BPW broth at 37˚C for 16–24 hours. Aliquots of the pre-enriched broth were then spread and cultured on MacConkey agar (Oxoid, Basingstoke, UK) plates and incubated aerobically at 37˚C for 24 hours. The pink-coloured (lactose fermenting) colonies were sub-cultured on Eosin Methylene Blue (EMB) agar (Oxoid, Basingstoke, UK) plates and incubated aerobically for an additional 24 hours. The green metallic colonies on EMB were presumed E. coli and were sub-cultured on nutrient agar (Oxoid, Basingstoke, UK) plates and incubated aerobically for 24 hours. The E. coli colonies appeared large, thin, circular and greyish-white on nutrient agar. Further identification of the isolates was made using the Analytical Profile Index (API 20E) (Biomerieux®, Inc., 100 Rodolphe Street, Durham, NC 27712, USA) test kit. We stored the presumptive E. coli isolates in 10% glycerol at −20˚C before further analysis.
Confirmation of E. coli isolates
The presumptive E. coli isolates were sequenced using 16S rRNA as described for E. coli.77 The boiling method was used to extract DNA from presumptive E. coli isolates, as was used in a similar study.78 Each pure colony was suspended in 200 µL of nuclease-free water and heated at 95°C for 5 minutes. The suspension was centrifuged at 6000 g for 2 minutes at four °C to extract the DNA. Polymerase Chain Reaction (PCR) was used for DNA amplification using Taq polymerase, and the uidA F (Forward) primers (5′-CGGAAGCAACGCGTAAACTC-3′) and uidA R (Reverse) primers (5′-TGAGCGTCGCAGAACATTACA-3′) (Sigma-Aldrich, Merck, Germany) in a thermo-cycler. The PCR conditions were; initial denaturation 95°C for 3 minutes, and 40 cycles of 95°C for 45 seconds, 55°C for 45 seconds and 72°C for 60 seconds. The final extension was at 72°C for 5 minutes and held at 4°C. After that, the amplicons were run on 1.5% agarose gels by gel electrophoresis in 1X tris-acetate EDTA (TAE) buffer at 100 volts for 30 minutes. The gels were then stained with ethidium bromide and read on a BioDoc-IT™ Imaging System Trans-illuminator to confirm the amplifications of the uidA target region.
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing (AST) was done using a panel of 13 antibiotics by the Kirby disc-diffusion method. The AST procedure was done as described in other studies.79–81 The antibiotic discs (Oxoid, Basingstoke, Hampshire, UK) that were used included amoxicillin/clavulanic acid (20/10 µg), ampicillin (10 µg), cefepime (30 µg), cefotaxime (30 µg), ceftazidime (30 µg), chloramphenicol (30 µg), ciprofloxacin (5 µg), gentamicin (10 µg), meropenem (10 µg), nalidixic acid (30 µg), nitrofurantoin (300 µg), tetracycline (30 µg) and trimethoprim/sulfamethoxazole (1.25/23.75 µg).
The bacterial suspension was prepared and turbidity adjusted to 0.5 McFarland standard, after which it was inoculated onto Mueller-Hinton Agar (Oxoid, Basingstoke, Hampshire, UK) petri dishes and incubated at 37°C for 16–24 hours. The zones of inhibition were measured in millimetres using a Vernier calliper, and results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) 2020 guidelines as susceptible (S), intermediate (I) and resistant.82 We used E. coli ATCC 25922 for quality control.
Data process and analysis
Data analysis used Stata version 16.1/BE (Stata Corp., College Station, TX, USA) and WHONET 2020. The zones of inhibition were interpreted using the CLSI 2020 guidelines and interpreted as susceptible (S), intermediate (I) and resistant (R). Frequencies and percentages are presented in Tables 1 and 2.
Table 1.
Distribution of samples collected from laying hens
| Province | District | Number of farms sampled, n (%, 95% CI) | Number of samples collected | Samples that yield E. coli isolates | Positivity rates (%) |
|---|---|---|---|---|---|
| Lusaka | Chongwe | 17 (22.1; 14.0–33.0) | 103 | 96 | 93.2 |
| Kafue | 20 (26.0; 17.2–37.1) | 81 | 68 | 84.0 | |
| Lusaka | 5 (6.49;2.67–14.9) | 34 | 34 | 100 | |
| Rufunsa | 3 (3.90; 1.23–11.7) | 7 | 7 | 100 | |
| Copperbelt | Kitwe | 22 (28.6; 19.4–39.9) | 94 | 88 | 93.6 |
| Ndola | 10 (13.0; 7.03–22.7) | 46 | 46 | 100 | |
| Total | 77 | 365 | 339 |
Table 2.
AMR patterns of Escherichia coli isolates (n = 365)
| Antibiotic name | % R | % I | % S | % R 95%CI |
|---|---|---|---|---|
| Amoxicillin/Clavulanic acid | 25 (7.4) | 32 (9.4) | 282 (83.2) | 13.1–21.3 |
| Ampicillin | 183 (54.0) | 40 (11.8) | 116 (34.2) | 48.5–59.4 |
| Cefotaxime | 103 (30.4) | 39 (11.5) | 197 (58.1) | 25.6–35.6 |
| Ceftazidime | 21 (6.2) | 29 (8.6) | 289 (85.3) | 4.0–9.5 |
| Cefepime | 21 (6.2) | 61 (18.0) | 257 (75.8) | 4.0–9.5 |
| Chloramphenicol | 30 (8.8) | 18 (5.3) | 291 (85.8) | 6.1–12.5 |
| Ciprofloxacin | 86 (25.4) | 80 (23.6) | 173 (51.0) | 20.9–30.4 |
| Gentamicin | 29 (8.6) | 69 (20.4) | 241 (71.1) | 5.9–12.2 |
| Meropenem | 3 (0.9) | 15 (4.4) | 321 (94.7) | 0.2–2.8 |
| Nitrofurantoin | 41 (12.1) | 72 (21.2) | 226 (66.7) | 8.9–16.2 |
| Tetracycline | 184 (54.3) | 52 (15.3) | 103 (30.4) | 49.1–59.9 |
| Trimethoprim/Sulfamethoxazole | 90 (26.5) | 12 (3.5) | 237 (69.9) | 22.0–31.6 |
| Nalidixic acid | 82 (24.2) | 58 (17.1) | 199 (58.7) | 19.8–29.2 |
Note. R = Resistant, I = Intermediate, S = Susceptible, 95% CI = 95% confidence interval.
Ethical approval
We obtained ethical clearance from the ERES Converge Ethics Committee with a protocol ID: reference no. 2019-Dec-004. Permission to conduct the research in the selected sites was also obtained from the Zambia National Health Research Authority. Additionally, we obtained further permission to collect data in layer poultry farms from the Lusaka and Copperbelt Provincial and District Veterinary Offices. Finally, we obtained informed consent from the layer poultry farmers to collect samples from their laying hens.
Results
Seventy-seven layer poultry farms from six districts across Lusaka and Copperbelt provinces were enrolled in this study from which 365 cloacal swabs were collected from the laying hens. Of the 365 cloacal swab samples, 339 tested positive for E. coli, resulting in a 92.9% positivity rate (Table 1).
E. coli isolates were highly resistant to tetracycline (54.6%) and ampicillin (54.0%) while highly susceptible to meropenem (94.7%), chloramphenicol (85.8%) and ceftazidime (85.3%) as depicted in Table 2.
Multidrug-resistant, extensively drug-resistant and pan-drug-resistant E. coli
Overall, 12/339(3.54%; 95% CI: 1.93–6.27) of the isolates were susceptible to all antibiotics, while 327/339 (96.5; 95% CI: 93.73%–98.07%) were resistant to at least one antibiotic. A total of 219/339 (64.6%; 95% CI: 59.22–69.64) isolates were MDR and resistant to three or more antibiotics from different classes. Of these isolates, 25/339 (7.37%; 95% CI: 4.92–10.83) were possible XDR isolates. However, no PDR isolates were recorded.
Overall, layer poultry farms obtained MDR isolates from 75/77(97.4%; 95% CI: 89.9–99.4). All the farms (45/45) from Lusaka province and 30/32 (93.8%; 95% CI: 77.4–98.5) from the Copperbelt province recorded MDR isolates.
The most MDR pattern was seen with resistance to AMP, CTX and CIP, while the least frequent pattern was seen with resistance to AMP, CTX, FEP and CHL (Table 3).
Table 3.
Selected common and less common MDR patterns of Escherichia coli
| Antimicrobial combination | Number of isolates | Number of antimicrobial classes |
|---|---|---|
| AMC, AMP, CTX, CIP | 4 | 3 |
| AMC, AMP, CTX, FEP, CIP | 4 | 3 |
| AMC, AMP, CTX, CAZ, CIP | 3 | 3 |
| AMC, AMP, CTX, FEP, CHL, CIP | 4 | 4 |
| AMP, CTX, CAZ, FEP, CIP | 6 | 3 |
| AMP, CTX, FEP, CHL | 2 | 3 |
| AMP, CTX, FEP, CIP | 12 | 3 |
| AMP, CTX, CHL, CIP | 4 | 4 |
| AMP, CTX, CHL | 3 | 3 |
| AMP, CTX, CIP | 19 | 3 |
| AMP, CAZ, FEP, CIP | 3 | 3 |
| AMP, CAZ, CIP | 5 | 3 |
| AMP, CHL, CIP | 5 | 3 |
| AMC, AMP, CTX, CAZ, FEP, CHL, CIP | 5 | 4 |
| AMC, AMP, CTX, CAZ, FEP, CIP | 6 | 3 |
Note: AMC = Amoxicillin/clavulanic acid; AMP = Ampicillin; CTX = Ceftriaxone; FEP = Cefepime; CHL = Chloramphenicol; CIP = Ciprofloxacin; CAZ = Cefpodoxime.
Discussion
In this study, we assessed the AMR profiles of E. coli isolated from laying hens in selected districts of Lusaka and Copperbelt provinces in Zambia. Our study found a high isolation rate of 92.9%, with a 96.5% prevalence of E. coli resistant to at least one antibiotic. Additionally, 64.6% of the isolates were MDR. This study found that most E. coli isolates were highly resistant to tetracycline (54.6%), ampicillin (54.0%), cefotaxime (30.4%), trimethoprim-sulfamethoxazole (26.5%), ciprofloxacin (25.4%) and nalidixic acid (24.2%). Conversely, E. coli was highly susceptible to meropenem (94.7%), chloramphenicol (85.8%), ceftazidime (85.3%), amoxicillin-clavulanic acid (83.2%) and cefepime (75.8%).
The present study found a high E. coli isolation rate of 92.9%. The isolation rate of E. coli in our study was similar to (93%) what was reported in Sierra Leone.83 However, our isolation rate was slightly higher than (86%) what was reported in broiler chickens in Bangladesh.15 Other studies have reported even higher isolation rates, including 100% in Tanzania,53 99% in the USA84 and 94% in Nepal.85 The high isolation rate of E. coli reported in our study and similar studies could be due to adherence to the microbiology isolation protocols that resulted in increased bacteria recovery. This level of isolation rate makes E. coli a suitable microorganism to evaluate the AMR prevalence and profiles in many production systems, including layer poultry farms. However, lower isolation rates have been reported in other studies, such as a study in Bangladesh that used frozen chicken samples.41 The differences in sample sources may account for these variations in isolation rates.
The highest resistance of E. coli to antibiotics was observed with tetracyclines. A previous study conducted from commercial farms in the Chisamba district of Zambia reported a 100% resistance of E. coli to tetracycline.86 Another recent study in Zambia found high (87.9%) resistance of E. coli to tetracycline.87 The ease of access to tetracyclines in Zambia's poultry industry without prescriptions may contribute to AMR.88 Our findings corroborate observations from other studies conducted on poultry.13,41,55,59,89 The misuse of tetracyclines in poultry for growth promotion, improved egg production, prophylaxis and treatment of diseases has contributed to the resistance of E. coli to these drugs.90–93 However, by contrast, a study in Bangladesh found that E. coli isolated in poultry were highly resistant to levofloxacin.15 These discrepancies may be due to differences in poultry disease burdens and the availability of particular poultry antimicrobials across countries. Furthermore, the ease of access to common antibiotics such as tetracyclines, quinolones and penicillins for use in poultry has contributed to development and spread of AMR.42,53
Our study found that E. coli was also highly resistant to ampicillin. Our findings are similar to a study that was conducted in poultry farms in Zambia.87 Additionally, our findings are consistent with those reported in other studies.14,53,60,85,94 The resistance of E. coli to ampicillin may indicate the misuse of penicillins in the poultry sector. Additionally, studies in humans have also reported high resistance of E. coli to ampicillin.61,62,95,96 The resistance rate reported in our study is higher than that reported in a study that was done in the USA97 and in Sierra Leone.83
This study found that E. coli was resistant to cefotaxime, a third-generation cephalosporin. A similar resistance rate to cefotaxime has been reported in Bangladesh,15 and resistance to ceftiofur, another third-generation cephalosporin, was reported in China.98 Studies suggest that increased resistance of E. coli to third-generation cephalosporins may be associated with the administration of beta-lactams, which may result in the production of extended spectrum beta-lactamases.98–100 In human medicine, third-generation cephalosporins such as cefotaxime and ceftriaxone are ‘Watch group’ antibiotics and should only be used when the ‘Access (to first-line) group’ have failed.101 However, there is evidence that antibiotics such as ceftriaxone or cefotaxime are usually prescribed inappropriately, thereby increasing the risk of bacterial resistance to cephalosporins.102–104
In Zambia, the misuse of enrofloxacin, a quinolone commonly used in poultry, is evidenced by the resistance rates of E. coli to ciprofloxacin and nalidixic acid in our present study, a recent comparable study87 and the ease of access to poultry antibiotics,33,88 in Zambia. This finding aligns with similar resistance patterns of E. coli to quinolones reported in other studies.15,16,44,85,105 The misuse of enrofloxacin in the poultry sector may contribute to the resistance of E. coli and other microorganisms to this drug, as well as other quinolones.106 This highlights the importance of prudent use of antimicrobials in the poultry sector to prevent the development and spread of AMR that would subsequently compromise the treatment of human infections.
Our study found high resistance (96.5%) of E. coli to at least one of the tested antibiotics, similar to a study done in China, where 94% of E. coli isolates were resistant to at least one antibiotic.44 This high resistance may be partially attributed to the inappropriate use of antibiotics in poultry.33 The detection of 64.6% MDR E. coli in our study is a public health concern requiring urgent attention and control of antibiotic use in poultry. Similar findings were reported in other studies. An earlier study from three commercial poultry farms in Zambia showed that 4.8% of E. coli were MDR,86 while higher levels of MDR E. coli have been reported in broiler chickens in Bangladesh (100%),41 95.7% in Austria,107 86.76% in Tanzania,53 76% in Bangladesh,15 71% in Nepal,85 56.3% Nigeria108 and 44% in Ireland.37 The treatment failure of poultry diseases due to MDR microorganisms can cause farmers to seek more options of the available antimicrobials that can further increase the selection pressure of AMR and make the treatment of infections even more difficult or impossible.109–111 The occurrence of MDR isolates in our study, as well as in other studies, highlights the need to intensify biosecurity measures in poultry10,108,112–117 and for more robust AMS and surveillance programmes to address AMR.118–125
This study highlights the AMR profiles of E. coli isolated from laying hens from Zambia’s two provinces that produce the largest number of poultry products. However, this study focused on one priority microorganism and does not give a clear picture of the resistance patterns of other priority microorganisms isolated from poultry.
Conclusion
This study found a high resistance of E. coli to antibiotics commonly used in both poultry and humans in Zambia. The presence of MDR isolates is a significant public health concern because of the potential risk of transmission of AMR from chickens and eggs to humans. The regulation of antibiotic use in poultry is critical in addressing this issue. To combat this problem, there is a need to increase education and awareness among poultry farmers and veterinary drug dispensers on the rational use of antimicrobials, biosecurity measures, vaccinations and AMR. Furthermore, a multifaceted response, implementation and strengthening of AMS and surveillance programmes in poultry should be promoted to reduce the development and spread of AMR.
Acknowledgements
We are grateful to the layer poultry farmers for allowing us to conduct this study on their farms. Further, we pass our thanks to the Lusaka and Copperbelt Provincial and District Veterinary Offices for giving us permission to conduct this study in their veterinary camps. We also acknowledge the technical support that was rendered to us by the laboratory staff members in the Department of Disease Control, School of Veterinary Medicine at the University of Zambia.
Contributor Information
Steward Mudenda, Department of Pharmacy, School of Health Sciences, University of Zambia, Lusaka, Zambia; Department of Disease Control, School of Veterinary Medicine, University of Zambia, Lusaka, Zambia.
Sydney Malama, Department of Biological Sciences, School of Natural Sciences, University of Zambia, Lusaka, Zambia.
Musso Munyeme, Department of Disease Control, School of Veterinary Medicine, University of Zambia, Lusaka, Zambia.
Scott Kaba Matafwali, Clinical Research Department, Faculty of Infectious and Tropical Diseases, London School of Hygiene & Tropical Medicine, London, UK.
Penjaninge Kapila, Department of Disease Control, School of Veterinary Medicine, University of Zambia, Lusaka, Zambia.
Patrick Katemangwe, Department of Disease Control, School of Veterinary Medicine, University of Zambia, Lusaka, Zambia.
Geoffrey Mainda, Department of Veterinary Services, Central Veterinary Research Institute, Ministry of Fisheries and Livestock, Lusaka, Zambia.
Andrew Nalishuwa Mukubesa, Department of Disease Control, School of Veterinary Medicine, University of Zambia, Lusaka, Zambia.
Mwendalubi Albert Hadunka, Department of Animal Health, Centre for Infectious Disease Research in Zambia (CIDRZ), Lusaka, Zambia.
John Bwalya Muma, Department of Disease Control, School of Veterinary Medicine, University of Zambia, Lusaka, Zambia.
Funding
This study was completed as part of a research project by a PhD student.
Transparency declarations
All authors have declared no conflict of interest.
References
- 1. de Mesquita Souza Saraiva M, Lim K, do Monte DFMet al. . Antimicrobial resistance in the globalized food chain: a one health perspective applied to the poultry industry. Brazilian J Microbiol 2022; 53: 465–86. 10.1007/s42770-021-00635-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jibril AH, Okeke IN, Dalsgaard Aet al. . Association between antimicrobial usage and resistance in Salmonella from poultry farms in Nigeria. BMC Vet Res 2021; 17: 234. 10.1186/s12917-021-02938-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tangcharoensathien V, Chanvatik S, Sommanustweechai A. Complex determinants of inappropriate use of antibiotics. Bull World Health Organ 2018; 96: 141–4. 10.2471/BLT.17.199687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mudenda S, Matafwali SK, Malama Set al. . Prevalence and antimicrobial resistance patterns of Enterococcus species isolated from laying hens in Lusaka and Copperbelt provinces of Zambia: a call for AMR surveillance in the poultry sector. JAC-Antimicrobial Resist 2022; 4: dlac126. 10.1093/jacamr/dlac126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Plata G, Baxter NT, Susanti Det al. . Growth promotion and antibiotic induced metabolic shifts in the chicken gut microbiome. Commun Biol 2022; 5: 293. 10.1038/s42003-022-03239-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gupta CL, Blum SE, Kattusamy Ket al. . Longitudinal study on the effects of growth-promoting and therapeutic antibiotics on the dynamics of chicken cloacal and litter microbiomes and resistomes. Microbiome 2021; 9: 178. 10.1186/s40168-021-01136-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rahman MRT, Fliss I, Biron E. Insights in the development and uses of alternatives to antibiotic growth promoters in poultry and swine production. Antibiotics 2022; 11: 766. 10.3390/antibiotics11060766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pokharel S, Shrestha P, Adhikari B. Antimicrobial use in food animals and human health: time to implement ‘one health’ approach. Antimicrob Resist Infect Control 2020; 9: 181. 10.1186/s13756-020-00847-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Van Boeckel TP, Brower C, Gilbert Met al. . Global trends in antimicrobial use in food animals. Proc Natl Acad Sci U S A 2015; 112: 5649–54. 10.1073/pnas.1503141112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kiambi S, Mwanza R, Sirma Aet al. . Understanding antimicrobial use contexts in the poultry sector: challenges for small-scale layer farms in Kenya. Antibiotics 2021; 10: 106. 10.3390/antibiotics10020106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mehdi Y, Létourneau-Montminy MP, Lou GMet al. . Use of antibiotics in broiler production: global impacts and alternatives. Anim Nutr 2018; 4: 170–8. 10.1016/j.aninu.2018.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mwikuma G, Kainga H, Kallu SAet al. . Determination of the prevalence and antimicrobial resistance of Enterococcus faecalis and Enterococcus faecium associated with poultry in four districts in Zambia. Antibiotics 2023; 12: 657. 10.3390/antibiotics12040657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jahantigh M, Samadi K, Dizaji REet al. . Antimicrobial resistance and prevalence of tetracycline resistance genes in Escherichia coli isolated from lesions of colibacillosis in broiler chickens in Sistan, Iran. BMC Vet Res 2020; 16: 267. 10.1186/s12917-020-02488-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mensah GI, Adjei VY, Vicar EKet al. . Safety of retailed poultry: analysis of antibiotic resistance in Escherichia coli from raw chicken and poultry fecal matter from selected farms and retail outlets in Accra, Ghana. Microbiol Insights 2022; 15: 117863612210932. 10.1177/11786361221093278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hussain A, Shaik S, Ranjan A, et al. . Risk of transmission of antimicrobial resistant Escherichia coli from commercial broiler and free-range retail chicken in India. Front Microbiol 2017; 8: 2120. 10.3389/fmicb.2017.02120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vounba P, Arsenault J, Bada-Alambédji Ret al. . Prevalence of antimicrobial resistance and potential pathogenicity, and possible spread of third-generation cephalosporin resistance, in Escherichia coli isolated from healthy chicken farms in the region of Dakar, Senegal. PLoS ONE 2019; 14: e0214304. 10.1371/journal.pone.0214304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Braz VS, Melchior K, Moreira CG. Escherichia coli as a multifaceted pathogenic and versatile bacterium. Front Cell Infect Microbiol 2020; 10: 548492. 10.3389/fcimb.2020.548492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Daga AP, Koga VL, Soncini JGMet al. . Escherichia coli bloodstream infections in patients at a university hospital: virulence factors and clinical characteristics. Front Cell Infect Microbiol 2019; 9: 191. 10.3389/fcimb.2019.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Aworh MK, Kwaga J, Okolocha Eet al. . Prevalence and risk factors for multi-drug-resistant Escherichia coli among poultry workers in the federal capital territory, Abuja, Nigeria. PLoS ONE 2019; 14: e0225379. 10.1371/journal.pone.0225379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mellata M. Human and avian extraintestinal pathogenic Escherichia coli: infections, zoonotic risks, and antibiotic resistance trends. Foodborne Pathog Dis 2013; 10: 916–32. 10.1089/fpd.2013.1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ikuta KS, Swetschinski LR, Robles Aguilar Get al. . Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the global burden of disease study 2019. Lancet 2022; 400: 2221–48. 10.1016/S0140-6736(22)02185-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Murray CJ, Ikuta KS, Sharara Fet al. . Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 2022; 399: 629–55. 10.1016/S0140-6736(21)02724-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tacconelli E, Pezzani MD. Public health burden of antimicrobial resistance in Europe. Lancet Infect Dis 2019; 19: 4–6. 10.1016/S1473-3099(18)30648-0 [DOI] [PubMed] [Google Scholar]
- 24. de Kraker MEA, Stewardson AJ, Harbarth S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med 2016; 13: e1002184. 10.1371/journal.pmed.1002184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pulingam T, Parumasivam T, Gazzali AMet al. . Antimicrobial resistance: prevalence, economic burden, mechanisms of resistance and strategies to overcome. Eur J Pharm Sci 2022; 170: 106103. 10.1016/j.ejps.2021.106103 [DOI] [PubMed] [Google Scholar]
- 26. Hillock NT, Merlin TL, Turnidge Jet al. . Modelling the future clinical and economic burden of antimicrobial resistance: the feasibility and value of models to inform policy. Appl Health Econ Health Policy 2022; 20: 479–86. 10.1007/s40258-022-00728-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Alhaji NB, Haruna AE, Muhammad Bet al. . Antimicrobials usage assessments in commercial poultry and local birds in north-central Nigeria: associated pathways and factors for resistance emergence and spread. Prev Vet Med 2018; 154: 139–47. 10.1016/j.prevetmed.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 28. Bamidele O, Amole TA, Oyewale OAet al. . Antimicrobial usage in smallholder poultry production in Nigeria. Vet Med Int 2022; 2022: 7746144. 10.1155/2022/7746144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Malijan GM, Howteerakul N, Ali Net al. . A scoping review of antibiotic use practices and drivers of inappropriate antibiotic use in animal farms in WHO Southeast Asia region. One Heal 2022; 15: 100412. 10.1016/j.onehlt.2022.100412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kainga H, Phonera MC, Chikowe Iet al. . Determinants of knowledge, attitude, and practices of veterinary drug dispensers toward antimicrobial use and resistance in main cities of Malawi: a concern on antibiotic stewardship. Antibiotics 2023; 12: 149. 10.3390/antibiotics12010149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mudenda S, Malama S, Munyeme Met al. . Awareness of antimicrobial resistance and associated factors among layer poultry farmers in Zambia: implications for surveillance and antimicrobial stewardship programs. Antibiotics 2022; 11: 383. 10.3390/antibiotics11030383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nhung NT, Chansiripornchai N, Carrique-Mas JJ. Antimicrobial resistance in bacterial poultry pathogens: a review. Front Vet Sci 2017; 4: 126. 10.3389/fvets.2017.00126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chilawa S, Mudenda S, Daka Vet al. . Knowledge, attitudes, and practices of poultry farmers on antimicrobial use and resistance in Kitwe, Zambia: implications on antimicrobial stewardship. Open J Anim Sci 2022; 13: 60–81. 10.4236/ojas.2023.131005 [DOI] [Google Scholar]
- 34. Xu J, Sangthong R, McNeil Eet al. . Antibiotic use in chicken farms in northwestern China. Antimicrob Resist Infect Control 2020; 9: 10. 10.1186/s13756-019-0672-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Al Masud A, Rousham EK, Islam MAet al. . Drivers of antibiotic use in poultry production in Bangladesh: dependencies and dynamics of a patron-client relationship. Front Vet Sci 2020; 7: 78. 10.3389/fvets.2020.00078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Agyare C, Etsiapa Boamah V, Ngofi Zumbi C, et al. . Antibiotic use in poultry production and its effects on bacterial resistance. Antimicrobial Resistance—A Global Threat. IntechOpen, 2018; 33–51. [Google Scholar]
- 37. Byrne N, O’Neill L, Dίaz JACet al. . Antimicrobial resistance in Escherichia coli isolated from on-farm and conventional hatching broiler farms in Ireland. Ir Vet J 2022; 75: 7. 10.1186/s13620-022-00214-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Abo-Amer AE, Shobrak MY, Altalhi AD. Isolation and antimicrobial resistance of Escherichia coli isolated from farm chickens in Taif, Saudi Arabia. J Glob Antimicrob Resist 2018; 15: 65–8. 10.1016/j.jgar.2018.05.020 [DOI] [PubMed] [Google Scholar]
- 39. Boulianne M, Arsenault J, Daignault Det al. . Drug use and antimicrobial resistance among Escherichia coli and Enterococcus spp. isolates from chicken and turkey flocks slaughtered in Quebec, Canada. Can J Vet Res 2016; 80: 49–59. [PMC free article] [PubMed] [Google Scholar]
- 40. Agunos A, Arsenault RK, Avery BPet al. . Changes in antimicrobial resistance levels among Escherichia coli, Salmonella, and Campylobacter in Ontario broiler chickens between 2003 and 2015. Can J Vet Res 2018; 82: 163–77. [PMC free article] [PubMed] [Google Scholar]
- 41. Parvin MS, Talukder S, Ali MYet al. . Antimicrobial resistance pattern of Escherichia coli isolated from frozen chicken meat in Bangladesh. Pathogens 2020; 9: 420. 10.3390/pathogens9060420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Koirala A, Bhandari P, Shewade HDet al. . Antibiotic use in broiler poultry farms in Kathmandu valley of Nepal: which antibiotics and why? Trop Med Infect Dis 2021; 6: 47. 10.3390/tropicalmed6020047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rahman MM, Husna A, Elshabrawy HAet al. . Isolation and molecular characterization of multidrug-resistant Escherichia coli from chicken meat. Sci Rep 2020; 10: 21999. 10.1038/s41598-020-78367-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yassin AK, Gong J, Kelly Pet al. . Antimicrobial resistance in clinical Escherichia coli isolates from poultry and livestock, China. PLoS ONE 2017; 12: e0185326. 10.1371/journal.pone.0185326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Stromberg ZR, Johnson JR, Fairbrother JMet al. . Evaluation of Escherichia coli isolates from healthy chickens to determine their potential risk to poultry and human health. PLoS ONE 2017; 12: e0180599. 10.1371/journal.pone.0180599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mitchell NM, Johnson JR, Johnston Bet al. . Zoonotic potential of Escherichia coli isolates from retail chicken meat products and eggs. Appl Environ Microbiol 2015; 81: 1177–87. 10.1128/AEM.03524-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Meena PR, Yadav P, Hemlata Het al. . Poultry-origin extraintestinal Escherichia coli strains carrying the traits associated with urinary tract infection, sepsis, meningitis and avian colibacillosis in India. J Appl Microbiol 2021; 130: 2087–101. 10.1111/jam.14905 [DOI] [PubMed] [Google Scholar]
- 48. Mellata M, Johnson JR, Curtiss R. Escherichia coli isolates from commercial chicken meat and eggs cause sepsis, meningitis and urinary tract infection in rodent models of human infections. Zoonoses Public Health 2018; 65: 103–13. 10.1111/zph.12376 [DOI] [PubMed] [Google Scholar]
- 49. Queenan K, Häsler B, Rushton J. A one health approach to antimicrobial resistance surveillance: is there a business case for it? Int J Antimicrob Agents 2016; 48: 422–7. 10.1016/j.ijantimicag.2016.06.014 [DOI] [PubMed] [Google Scholar]
- 50. Nowbuth A, Asombang A, Tazikeng Net al. . Antimicrobial resistance in Zambia: a systematic review. Int J Infect Dis 2022; 116: S17–8. 10.1016/j.ijid.2021.12.042 [DOI] [Google Scholar]
- 51. Castillo AK, Espinoza K, Chaves AFet al. . Antibiotic susceptibility among non-clinical Escherichia coli as a marker of antibiotic pressure in Peru (2009–2019): one health approach. Heliyon 2022; 8: e10573. 10.1016/j.heliyon.2022.e10573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Velazquez-Meza ME, Galarde-López M, Carrillo-Quiróz Bet al. . Antimicrobial resistance: one health approach. Vet World 2022; 15: 743–9. 10.14202/vetworld.2022.743-749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kiiti RW, Komba E V, Msoffe PLet al. . Antimicrobial resistance profiles of Escherichia coli isolated from broiler and layer chickens in Arusha and Mwanza, Tanzania. Int J Microbiol 2021; 2021: 6759046. 10.1155/2021/6759046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ngai DG, Nyamache AK, Ombori O. Prevalence and antimicrobial resistance profiles of Salmonella species and Escherichia coli isolates from poultry feeds in Ruiru Sub-County, Kenya. BMC Res Notes 2021; 14: 41. 10.1186/s13104-021-05456-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mgaya FX, Matee MI, Muhairwa AP, et al. . Occurrence of multidrug-resistant Escherichia coli in raw meat and cloaca swabs in poultry processed in slaughter slabs in Dar Es Salaam, Tanzania. Antibiotics 2021; 10: 343. 10.3390/antibiotics10040343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Alonso CA, Zarazaga M, Ben Sallem Ret al. . Antibiotic resistance in Escherichia coli in husbandry animals: the African perspective. Lett Appl Microbiol 2017; 64: 318–34. 10.1111/lam.12724 [DOI] [PubMed] [Google Scholar]
- 57. Amer MM, Mekky HM, Amer AMet al. . Antimicrobial resistance genes in pathogenic Escherichia coli isolated from diseased broiler chickens in Egypt and their relationship with the phenotypic resistance characteristics. Vet World 2018; 11: 1082–8. 10.14202/vetworld.2018.1082-1088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Osman KM, Kappell AD, Elhadidy M, et al. . Poultry hatcheries as potential reservoirs for antimicrobial-resistant Escherichia coli: a risk to public health and food safety. Sci Rep 2018; 8: 5859. 10.1038/s41598-018-23962-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sarba EJ, Kelbesa KA, Bayu MDet al. . Identification and antimicrobial susceptibility profile of Escherichia coli isolated from backyard chicken in and around ambo, central Ethiopia. BMC Vet Res 2019; 15: 85. 10.1186/s12917-019-1830-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Aworh MK, Kwaga JKP, Hendriksen RSet al. . Genetic relatedness of multidrug resistant Escherichia coli isolated from humans, chickens and poultry environments. Antimicrob Resist Infect Control 2021; 10: 1–13. 10.1186/s13756-021-00930-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Bumbangi FN, Llarena A-K, Skjerve Eet al. . Evidence of community-wide spread of multi-drug resistant Escherichia coli in young children in Lusaka and Ndola districts, Zambia. Microorganisms 2022; 10: 1684. 10.3390/microorganisms10081684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Chiyangi H, Muma B, Malama Set al. . Identification and antimicrobial resistance patterns of bacterial enteropathogens from children aged 0–59 months at the University Teaching Hospital, Lusaka, Zambia: a prospective cross-sectional study. BMC Infect Dis 2017; 17: 117. 10.1186/s12879-017-2232-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Muligisa-Muonga E, Mainda G, Mukuma Met al. . Antimicrobial resistance of Escherichia coli and Salmonella isolated from retail broiler chicken carcasses in Zambia. J Epidemiol Res 2021; 6: 35–43. 10.5430/jer.v6n1p35 [DOI] [Google Scholar]
- 64. Phiri N, Mainda G, Mukuma Met al. . Antibiotic-resistant Salmonella species and Escherichia coli in broiler chickens from farms, abattoirs, and open markets in selected districts of Zambia. J Epidemiol Res 2020; 6: 13–21. 10.5430/jer.v6n1p13 [DOI] [Google Scholar]
- 65. Mainda G, Bessell PB, Muma JBet al. . Prevalence and patterns of antimicrobial resistance among Escherichia coli isolated from Zambian dairy cattle across different production systems. Sci Rep 2015; 5: 26589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Kabali E, Pandey GS, Munyeme Met al. . Identification of Escherichia coli and related enterobacteriaceae and examination of their phenotypic antimicrobial resistance patterns: a pilot study at a wildlife-livestock interface in Lusaka. Zambia. Antibiotics 2021; 10: 238. 10.3390/antibiotics10030238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Republic of Zambia NAP on AMR . Multi-sectoral national action plan on antimicrobial resistance. Gov Repub Zambia 2017: 1–79. https://www.afro.who.int/publications/multi-sectoral-national-action-plan-antimicrobial-resistance-2017-2027 [Google Scholar]
- 68. Kapona O. Zambia Successfully launches the first multi-sectoral national action plan on antimicrobial resistance (AMR). Heal Press Zambia Bull 2017; 1: 5–7. [Google Scholar]
- 69. World Health Organization . Global action plan on antimicrobial resistance. World Heal Organ 2015: 1–28. https://apps.who.int/iris/handle/10665/193736 [DOI] [PubMed]
- 70. CDC 2022 . Combating Antimicrobial Resistance in People and Animals: A One Health Approach. Centers for Disease Control Prevention. https://www.cdc.gov/onehealth/in-action/combating-ar-in-people-and-animals.html.
- 71. Guardabassi L, Butaye P, Dockrell DHet al. . One health: a multifaceted concept combining diverse approaches to prevent and control antimicrobial resistance. Clin Microbiol Infect 2020; 26: 1604–5. 10.1016/j.cmi.2020.07.012 [DOI] [PubMed] [Google Scholar]
- 72. White A, Hughes JM. Critical importance of a one health approach to antimicrobial resistance. Ecohealth 2019; 16: 404–9. 10.1007/s10393-019-01415-5 [DOI] [PubMed] [Google Scholar]
- 73. Espinosa-Gongora C, Jessen LR, Dyar OJet al. . Towards a better and harmonized education in antimicrobial stewardship in European veterinary curricula. Antibiotics 2021; 10: 364. 10.3390/antibiotics10040364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Dyar OJ, Huttner B, Schouten Jet al. . What is antimicrobial stewardship? Clin Microbiol Infect 2017; 23: 793–8. 10.1016/j.cmi.2017.08.026 [DOI] [PubMed] [Google Scholar]
- 75. Krishnan SB, Peterburs T. Zambia Jobs in Value Chains: Opportunities in Agribusiness. World Bank, 2017; 1–50. https://openknowledge.worldbank.org/handle/10986/27007 [Google Scholar]
- 76. Odoch T, Wasteson Y, L’Abée-Lund Tet al. . Prevalence, antimicrobial susceptibility and risk factors associated with non-typhoidal Salmonella on Ugandan layer hen farms. BMC Vet Res 2017; 13: 365. 10.1186/s12917-017-1291-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Al Azad MAR, Rahman MM, Amin Ret al. . Susceptibility and multidrug resistance patterns of Escherichia coli isolated from cloacal swabs of live broiler chickens in Bangladesh. Pathogens 2019; 8: 118. 10.3390/pathogens8030118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ievy S, Islam MS, Sobur MA, et al. . Molecular detection of avian pathogenic Escherichia coli (APEC) for the first time in layer farms in Bangladesh and their antibiotic resistance patterns. Microorganisms 2020; 8: 1021. 10.3390/microorganisms8071021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Hudzicki J. Kirby-Bauer disk diffusion susceptibility test protocol author information. Am Soc Microbiol 2012: 1–13. [Google Scholar]
- 80. Jorgensen JH, Turnidge JD. Kirby-Bauer disk diffusion susceptibility test protocol. Kirby-Bauer-Disk-Diffusion-Susceptibility-Test-Protocol 2015: 1–14. [Google Scholar]
- 81. Bauer AW, Kirby WM, Sherris JCet al. . Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol 1966; 45: 493–6. 10.1093/ajcp/45.4_ts.493 [DOI] [PubMed] [Google Scholar]
- 82. CLSI . Performance Standards for Antimicrobial Susceptibility Testing—Thirtieth-Edition: M100. 2020.
- 83. Mansaray AHD, Yankson DPY, Johnson RABet al. . Bacterial isolates and antibiotic resistance of Escherichia coli isolated from fresh poultry excreta used for vegetable farming in Freetown, Sierra Leone. Int J Environ Res Public Health 2022; 19: 5405. 10.3390/ijerph19095405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Lebert L, Martz SL, Janecko Net al. . Prevalence and antimicrobial resistance among Escherichia coli and Salmonella in Ontario smallholder chicken flocks. Zoonoses Public Health 2018; 65: 134–41. 10.1111/zph.12381 [DOI] [PubMed] [Google Scholar]
- 85. Koju P, Shrestha R, Shrestha Aet al. . Antimicrobial resistance in E. coli isolated from chicken cecum samples and factors contributing to antimicrobial resistance in Nepal. Trop Med Infect Dis 2022; 7: 249. 10.3390/tropicalmed7090249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Mtonga S, Nyirenda SS, Mulemba SSet al. . Epidemiology and antimicrobial resistance of pathogenic E. coli in chickens from selected poultry farms in Zambia. J Zoonotic Dis 2020; 2021: 18–28. [Google Scholar]
- 87. Mwansa M, Mukuma M, Mulilo Eet al. . Determination of antimicrobial resistance patterns of Escherichia coli isolates from farm workers in broiler poultry production and assessment of antibiotic resistance awareness levels among poultry farmers in Lusaka. Zambia. Front Public Heal 2023; 10: 998860. 10.3389/fpubh.2022.998860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Mudenda S, Mukosha M, Godman Bet al. . Knowledge, attitudes and practices of community pharmacy professionals on poultry antimicrobial dispensing, use and resistance in Zambia: implications on antibiotic stewardship and WHO AWaRe classification of antibiotics. Antibiotics 2022; 11: 1210. 10.3390/antibiotics11091210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hanson R, Kaneene JB, Padungtod P, et al. . Prevalence of Salmonella and E. coli, and their resistance to antimicrobial agents, in farming communities in northern Thailand. Southeast Asian J Trop Med Public Health 2002; 33Suppl: 120–6. [PubMed] [Google Scholar]
- 90. Marinho CM, Santos T, Gonçalves Aet al. . A decade-long commitment to antimicrobial resistance surveillance in Portugal. Front Microbiol 2016; 7: 1650. 10.3389/fmicb.2016.01650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kamini MG, Keutchatang FT, Mafo HYet al. . Antimicrobial usage in the chicken farming in yaoundé, Cameroon: a cross-sectional study. Int J Food Contam 2016; 3: 10. https://doi.org/https://doi.org/10.1186/s40550-016-0034-610.1186/s40550-016-0034-6 [Google Scholar]
- 92. Azabo R, Mshana S, Matee M, et al. . Antimicrobial usage in cattle and poultry production in Dar es Salaam, Tanzania: pattern and quantity. BMC Vet Res 2022; 18: 7. https://doi.org/https://doi.org/10.1186/s12917-021-03056-910.1186/s12917-021-03056-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Granados-Chinchilla F, Rodríguez C. Tetracyclines in food and feeding stuffs: from regulation to analytical methods, bacterial resistance, and environmental and health implications. J Anal Methods Chem 2017; 2017: 1315497. 10.1155/2017/1315497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Dela Peña LBRO, Nacario MAG, Bolo NRet al. . Multiple antibiotic resistance in Escherichia coli isolates from fecal and water sources in Laguna lake, Philippines. Water (Basel) 2022; 14: 1517. [Google Scholar]
- 95. Wu D, Ding Y, Yao Ket al. . Antimicrobial resistance analysis of clinical Escherichia coli isolates in neonatal ward. Front Pediatr 2021; 9: 670470. 10.3389/fped.2021.670470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Puvača N, de Frutos RL. Antimicrobial resistance in Escherichia coli strains isolated from humans and pet animals. Antibiotics 2021; 10: 1–19. 10.3390/antibiotics10010069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Khong MJ, Snyder AM, Magnaterra AKet al. . Antimicrobial resistance profile of Escherichia coli isolated from poultry litter. Poult Sci 2023; 102: 102305. 10.1016/j.psj.2022.102305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Liao M, Wu J, Li Yet al. . Prevalence and persistence of ceftiofur-resistant Escherichia coli in a chicken layer breeding program. Animals (Basel) 2023; 13: 90. 10.3390/ani13010090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Dierikx CM, Van Der Goot JA, Smith HEet al. . Presence of ESBL/AmpC -producing Escherichia coli in the broiler production pyramid: a descriptive study. PLoS ONE 2013; 8: e79005. 10.1371/journal.pone.0079005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Yamba K, Lukwesa-Musyani C, Samutela MTet al. . Phenotypic and genotypic antibiotic susceptibility profiles of gram-negative bacteria isolated from bloodstream infections at a referral hospital, Lusaka, Zambia. PLoS Glob Public Heal 2023; 3: e0001414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Hsia Y, Lee BR, Versporten Aet al. . Use of the WHO access, watch, and reserve classification to define patterns of hospital antibiotic use (AWaRe): an analysis of paediatric survey data from 56 countries. Lancet Glob Heal 2019; 7: e861–71. 10.1016/S2214-109X(19)30071-3 [DOI] [PubMed] [Google Scholar]
- 102. Kalungia AC, Mukosha M, Mwila Cet al. . Antibiotic use and stewardship indicators in the first- and second-level hospitals in Zambia: findings and implications for the future. Antibiotics 2022; 11: 1626. 10.3390/antibiotics11111626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Mudenda S, Chomba M, Chabalenge Bet al. . Antibiotic prescribing patterns in adult patients according to the WHO AWaRe classification: a multi-facility cross-sectional study in primary healthcare hospitals in Lusaka, Zambia. Pharmacol Pharm 2022; 13: 379–92. 10.4236/pp.2022.1310029 [DOI] [Google Scholar]
- 104. Mudenda S, Nsofu E, Chisha Pet al. . Prescribing patterns of antibiotics according to the WHO AWaRe classification during the COVID-19 pandemic at a teaching hospital in Lusaka, Zambia: implications for strengthening of antimicrobial stewardship programmes. Pharmacoepidemiology 2023; 2: 42–53. 10.3390/pharma2010005 [DOI] [Google Scholar]
- 105. Talebiyan R, Kheradmand M, Khamesipour Fet al. . Multiple antimicrobial resistance of Escherichia coli isolated from chickens in Iran. Vet Med Int 2014; 2014: 491418. 10.1155/2014/491418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Gouvêa R, Dos Santos FF, De Aquino Met al. . Fluoroquinolones in industrial poultry production, bacterial resistance and food residues: a review. Brazilian J Poult Sci 2015; 17: 1–10. 10.1590/1516-635x17011-10 [DOI] [Google Scholar]
- 107. Hess C, Troxler S, Jandreski-Cvetkovic D, et al. . Escherichia coli isolated from organic laying hens reveal a high level of antimicrobial resistance despite no antimicrobial treatments. Antibiotics 2022; 11: 467. 10.3390/antibiotics11040467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Adebowale O, Makanjuola M, Bankole Net al. . Multi-drug resistant Escherichia coli, biosecurity and anti-microbial use in live bird markets, Abeokuta. Nigeria. Antibiotics 2022; 11: 253. 10.3390/antibiotics11020253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Uddin TM, Chakraborty AJ, Khusro Aet al. . Antibiotic resistance in microbes: history, mechanisms, therapeutic strategies and future prospects. J Infect Public Health 2021; 14: 1750–66. 10.1016/j.jiph.2021.10.020 [DOI] [PubMed] [Google Scholar]
- 110. Harada K, Asai T. Role of antimicrobial selective pressure and secondary factors on antimicrobial resistance prevalence in Escherichia coli from food-producing animals in Japan. J Biomed Biotechnol 2010; 2010: 180682. 10.1155/2010/180682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Magiorakos AP, Srinivasan A, Carey RBet al. . Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 2012; 18: 268–81. 10.1111/j.1469-0691.2011.03570.x [DOI] [PubMed] [Google Scholar]
- 112. Moje N, Waktole H, Kassahun Ret al. . Status of animal health biosecurity measures of dairy farms in urban and peri-urban areas of central Ethiopia. Front Vet Sci 2023; 10: 1086702. 10.3389/fvets.2023.1086702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Tilli G, Laconi A, Galuppo Fet al. . Assessing biosecurity compliance in poultry farms: a survey in a densely populated poultry area in north east Italy. Animals (Basel) 2022; 12: 1409. 10.3390/ani12111409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Alhaji NB, Odetokun IA. Assessment of biosecurity measures against highly pathogenic avian influenza risks in small-scale commercial farms and free-range poultry flocks in the northcentral Nigeria. Transbound Emerg Dis 2011; 58: 157–61. 10.1111/j.1865-1682.2010.01195.x [DOI] [PubMed] [Google Scholar]
- 115. Ismael A, Abdella A, Shimelis Set al. . Assessment of biosecurity status in commercial chicken farms found in Bishoftu town, Oromia regional state, Ethiopia. Vet Med Int 2021; 2021: 5591932. 10.1155/2021/5591932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Selaledi LA, Hassan ZM, Manyelo TGet al. . The current status of the alternative use to antibiotics in poultry production: an African perspective. Antibiotics 2020; 9: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Gray P, Jenner R, Norris Jet al. . Antimicrobial prescribing guidelines for poultry. Aust Vet J 2021; 99: 181–235. 10.1111/avj.13034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Godman B, Egwuenu A, Haque Met al. . Strategies to improve antimicrobial utilization with a special focus on developing countries. Life 2021; 11: 528. 10.3390/life11060528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Schnall J, Rajkhowa A, Ikuta Ket al. . Surveillance and monitoring of antimicrobial resistance: limitations and lessons from the GRAM project. BMC Med 2019; 17: 176. 10.1186/s12916-019-1412-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Tacconelli E, Sifakis F, Harbarth Set al. . Surveillance for control of antimicrobial resistance. Lancet Infect Dis 2018; 18: e99–106. 10.1016/S1473-3099(17)30485-1 [DOI] [PubMed] [Google Scholar]
- 121. Cox JA, Vlieghe E, Mendelson Met al. . Antibiotic stewardship in low- and middle-income countries: the same but different? Clin Microbiol Infect 2017; 23: 812–8. 10.1016/j.cmi.2017.07.010 [DOI] [PubMed] [Google Scholar]
- 122. van Dijck C, Vlieghe E, Cox JA. Antibiotic stewardship interventions in hospitals in low-and middle-income countries: a systematic review. Bull World Health Organ 2018; 96: 266–80. 10.2471/BLT.17.203448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Khan X, Rymer C, Ray Pet al. . Quantification of antimicrobial use in Fijian livestock farms. One Heal 2021; 13: 100326. 10.1016/j.onehlt.2021.100326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Goutard FL, Bordier M, Calba Cet al. . Antimicrobial policy interventions in food animal production in South East Asia. BMJ 2017; 358: j3544. 10.1136/bmj.j3544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Donado-Godoy P, Castellanos R, León Met al. . The establishment of the Colombian Integrated Program for Antimicrobial Resistance Surveillance (COIPARS): a pilot project on poultry farms, slaughterhouses and retail market. Zoonoses Public Health 2015; 62: 58–69. 10.1111/zph.12192 [DOI] [PubMed] [Google Scholar]