Abstract
Objective Treatment of palmar midcarpal instability (PMCI) remains controversial and children can develop PMCI from asymptomatic hypermobility. Recently, case series have been published regarding the use of arthroscopic thermal shrinkage of the capsule in adults. Reports of the use of the technique in children and adolescents are rare, and there are no published case series.
Methods In a tertiary hand center for children's hand and wrist conditions, 51 patients were treated with arthroscopy for PMCI between 2014 and 2021. Eighteen out of 51 patients carried additional diagnosis of juvenile idiopathic arthritis (JIA) or a congenital arthritis. Data were collected including range of movement, visual analog scale (VAS) at rest and with load, and grip strength. Data were used to determine the safety and efficacy of this treatment in pediatric and adolescent patients.
Results Mean follow-up was 11.9 months. The procedure was well tolerated and no complications were recorded. Range of movement was preserved postoperatively. In all groups VAS scores at rest and with load improved. Those who underwent arthroscopic capsular shrinkage (ACS) had significantly greater improvement in VAS with load, compared with those who underwent arthroscopic synovectomy alone ( p = 0.04). Comparing those treated with underlying JIA versus those without, there was no difference in postoperative range of movement, but there was significantly greater improvement for the non-JIA group in terms of both VAS at rest ( p = 0.02) and VAS with load ( p = 0.02). Those with JIA and hypermobility stabilized postoperatively, and those with JIA with signs of early carpal collapse and no hypermobility achieved improved range of movement, in terms of flexion ( p = 0.02), extension ( p = 0.03), and radial deviation ( p = 0.01).
Conclusion ACS is a well-tolerated, safe, and effective procedure for PMCI in children and adolescents. It improves pain and instability at rest and with load, and offers benefit over open synovectomy alone. This is the first case series describing the usefulness of the procedure in children and adolescents, and demonstrates effective use of the technique in experienced hands in a specialist center.
Level of Evidence This is a Level IV study.
Keywords: adolescence, arthroscopy, capsular shrinkage, juvenile idiopathic arthritis, midcarpal instability, synovectomy
Midcarpal instability is a relatively rare cause of pain and instability in the wrist that was first described by Mouchet and Belot in 1934. 1 In 1981, Lichtman et al published a series of 10 patients with volar sagging and a painful snap related to progressive ulnar deviation of the radiocarpal joint: the so-called “catch-up clunk.” 2 Subsequently, the concept of midcarpal instability has been included in the description of carpal instability nondissociative manifesting as abnormal kinematics between carpal rows. The definition has attracted debate, as the condition in reality manifests with instability of the proximal carpal row, and there is potential for a contribution from instability within the same carpal row to exacerbate the problem. The diagnosis remains clinical, and the pathophysiology remains poorly understood. The term “ulnar” or “palmar” midcarpal instability describe the same pattern, and evolved from anatomic studies demonstrating laxity of the ulnar part of the arcuate (triquetro-hamate-capitate) ligament permitting palmar subluxation of the distal row. 3
Assessment, investigation, and treatment of palmar midcarpal instability (PMCI) remain subject to debate, and have been described for adult patients only. Most authors advocate a period of nonoperative treatment of 3 to 6 months including activity modification, splints including ulnar boost splints designed to support the supinated carpus, and proprioception and strengthening exercises, with a limited role for steroid injection. 4 5 Should nonoperative measures fail, an array of surgical techniques have been described, including historically partial wrist fusion, or ligament reconstruction and reinforcement via tendon transfer or tenodesis. These have variable reported results in the literature, and a recent vogue has arisen for arthroscopic capsular shrinkage (ACS), as a less invasive and lower morbidity option with quick recovery and good subjective patient-reported and objective outcomes. 6 7 The volar wrist ligaments are intimately related to the capsule, and despite the procedure title the intention is to shrink the ligaments themselves, as opposed to applying thermal instruments to the capsule which risks perforation and damage to the structures more superficial to it.
The senior author's practice involves children's hand surgery in a tertiary center treating rheumatological inflammatory as well as posttraumatic conditions. We describe our experience with the use of arthroscopy and thermal capsular shrinkage in 51 children and adolescents.
Patients and Methods
Between June 2014 and July 2021, 51 children and adolescents were treated with wrist arthroscopy by the senior author. The mean age was 15.0 years (range 8.9–18.4 years). Forty-six patients were female, and there were five males. Preoperatively, all patients were diagnosed as having PMCI on account of symptoms described, with a positive ulnar shift test or palmar midcarpal drawer test. There were no cases of static deformity. Almost half (20/51) of patients described a minor traumatic episode as heralding the onset of symptoms, with examination findings suggestive of hypermobility.
Initial treatment of these patients was nonoperative, mainly through proprioceptive neuromuscular exercises. 8 9 However, in children who continued to be symptomatic after a period of 6 months' nonoperative treatment, an arthroscopic assessment was offered, with synovectomy if applicable, and shrinkage. In this cohort we have included a group of children without a history of trauma, but with underlying juvenile idiopathic arthritis (JIA). They underwent arthroscopic synovectomy (AS) for either painful preexisting hypermobility, or early signs of carpal collapse due to ligament laxity and so were also offered ACS.
Indications for surgery, additional findings at arthroscopy, and procedures conducted are displayed in Tables 1 2 3 . Synovitis was found and debrided in almost all (46/51) cases. ACS was performed in more than ¾ (45/51) of cases. Pre- and postoperative data were collected via hand therapy regarding range of movement (ROM), grip strength, and visual analog scale (VAS) for pain at rest and with load. In the absence of validated outcome questionnaires in children, patients were asked for a subjective opinion regarding the outcome of surgery and improvement of symptoms. This subjective information is not included in the analysis on account of the likely bias associated with its reporting, but it has informed and influenced our decision making as our treatment pathways have evolved.
Table 1. Diagnoses.
| Diagnosis | Number | % |
|---|---|---|
| Symptomatic hypermobility after trauma | 20 | 39 |
| Juvenile idiopathic arthritis | 17 | 33 |
| Symptomatic hypermobility without trauma | 10 | 20 |
| Hypermobility + dorsal ganglion | 3 | 6 |
| Congenital arthritis | 1 | 2 |
| Total cases | 51 |
Table 2. Intraoperative findings.
| Intraoperative finding | Number of cases | % Prevalence |
|---|---|---|
| Synovitis | 46 | 90 |
| Scapholunate pathology | 25 | 49 |
| Triangular fibrocartilage complex (TFCC) pathology | 21 | 41 |
| Lunotriquetral pathology | 17 | 33 |
| Chondromalacia | 11 | 22 |
| Global laxity | 9 | 18 |
| Dorsal ganglion | 5 | 10 |
| Dorsal and volar ganglion | 1 | 2 |
| Long radiolunate ligament pathology | 1 | 2 |
Table 3. Intraoperative treatment.
| Treatment | Number of cases | % Prevalence |
|---|---|---|
| Synovectomy | 46 | 90 |
| Shrinkage | 45 | 88 |
| Biopsies | 20 | 39 |
| Ganglionectomy | 7 | 14 |
| Triangular fibrocartilage complex (TFCC) debridement | 6 | 12 |
| Plica resection | 3 | 6 |
| Steroid injection | 2 | 4 |
Surgical Technique
Examination under anesthesia followed by wrist arthroscopy was performed under general anesthesia and regional block, or regional block alone, via a traction tower set up using finger traps with use of a tourniquet. Standard ¾, ⅘, and/or 6R radiocarpal portals (i.e., between the 3rd and 4th extensor compartments, the 4th and 5th compartments, or radial to the 6th compartment), and midcarpal radial and midcarpal ulnar portals were used. Arthroscope size was proportional to the size of the child, with a 1.9-mm scope being more common in 8- to 12-year-old children, and 2.4-mm in 12- to 16-year-old adolescents. Arthroscopy will detect characteristic findings in hypermobility such as a “ballroom view” of the scapho-trapezium-trapezoid joint ( Fig. 1A ), bulging scapholunate (SL) ligament from a radiocarpal view ( Fig. 1B ), and gapping or a step off at the SL or lunotriquetral intervals from a midcarpal view ( Fig. 1C ). Where indicated, AS ( Figs. 2 3 4 ) was performed with a 2.5-mm shaver (CONMED, Florida, United States), and thermal capsular shrinkage ( Figs. 2 3 4 ) was performed with a 30-degree radiofrequency probe (CONMED Edge Bipolar RF system). From the radiocarpal joint shrinkage was applied to the radioscaphocapitate (RSC), long and short radiolunate, and ulnotriquetral ligaments volarly. The distal RSC and triquetro-capitate ligaments were treated through the midcarpal portals ( Figs. 2 3 4 ).
Fig. 1.
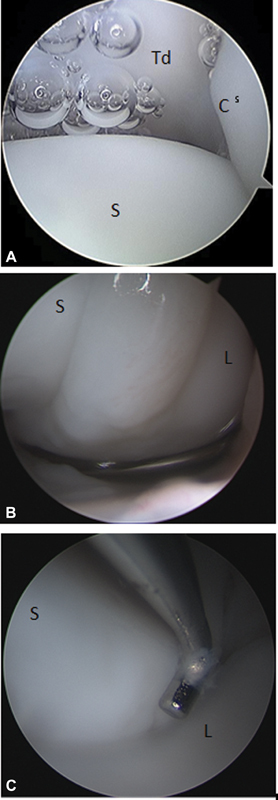
( A ) A so-called “ballroom view” of the scapho-trapezium-trapezoid (STT) joint in a 14-year-old with hypermobility noticing increasing space and air bubbles floating at the highest point in the midcarpal joint almost like a chandelier in a ballroom. (S = scaphoid, C = capitate, Td = trapezoid). ( B ) Radiocarpal view of the right wrist in a 14-year-old with hypermobility demonstrating a bulging scapholunate ligament with radius at the bottom. (S = scaphoid, L = lunate). ( C ) Midcarpal view in the same patient demonstrating a probe in the scapholunate interval showing no major steps or gaps (S = scaphoid, L = lunate).
Fig. 2.
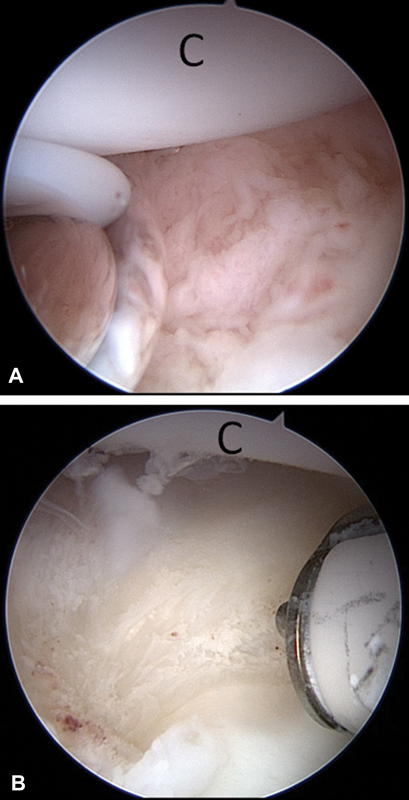
( A ) Active synovitis and hypermobility secondary to juvenile idiopathic arthritis (JIA) prior to synovectomy and shrinkage in a 15-year-old girl. Midcarpal view with capitate (C) on top. ( B ) Same patient and view after synovectomy and shrinkage (C = capitate).
Fig. 3.
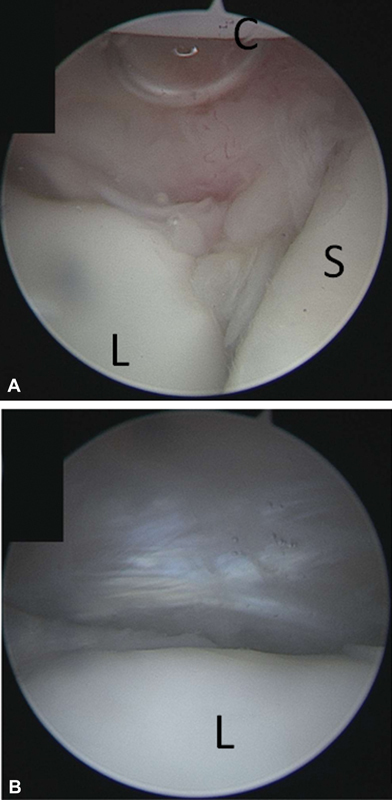
( A ) Chronic synovitis seen in this midcarpal view of the space of Poirier prior to synovectomy and shrinkage in an 11-year-old girl with juvenile idiopathic arthritis (JIA) (S = scaphoid, C = capitate, L = lunate). ( B ) Same patient after synovectomy and shrinkage in the same midcarpal view (L = lunate).
Fig. 4.
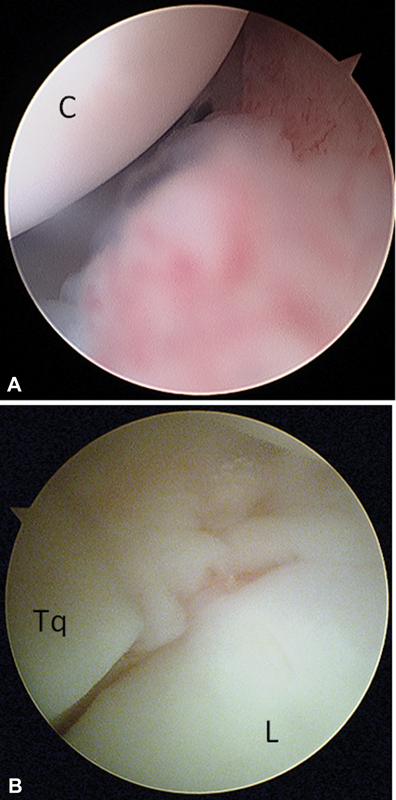
( A ) Active midcarpal synovitis in a 14-year-old with hypermobility as seen in this midcarpal view with the capitate (C) in the upper left corner. ( B ) Chronic midcarpal lunotriquetral synovitis in a 15-year-old male as seen in this midcarpal view with the lunate (L) in the lower right corner and the triquetrum (Tq) in the lower left.
In addition, further treatment was performed in some cases based on additional intraoperative findings ( Table 3 ). Dorsal shrinkage, which has been advocated in some circumstances, was not conducted. 7 Postoperatively, the wrist was immobilized in plaster for 6 weeks followed by splinting for a further 4 weeks and therapy.
Results
Complete data sets were available for 45 of the 51 patients. In three cases this was due to incomplete data (most commonly grip strength measurements) collected at follow-up, mostly on account of the coronavirus disease 2019 pandemic. All data available, including partial data sets, were included in analysis. Mean follow-up was 1 year (11.9 months, range 2–29 months). Data were analyzed using the Anderson–Darling calculation which confirmed normal distribution. Student's t -test analysis was used to identify any significant differences in outcome between those who underwent ACS and those who did not, and those with a diagnosis of JIA or congenital disorder, and those without ( Tables 4 5 6 7 ). The procedure was well tolerated, with significant improvement in all outcomes identified ( Table 4 ).
Table 4. A comparison of preoperative and postoperative function.
| Group | VAS rest | VAS load | Grip | Extension | Flexion | Radial | Ulnar | Supination | Pronation | |
|---|---|---|---|---|---|---|---|---|---|---|
| Juvenile idiopathic arthri | Preop | 2.2 | 4.6 | 0.6 | 72.9 | 80.6 | 29.0 | 30.6 | 87.8 | 87.8 |
| Post | 0.2 | 1.0 | 0.9 | 73.2 | 83.6 | 31.8 | 31.8 | 90.0 | 90.0 | |
| Change | –2.1 | –3.6 | 0.3 | 0.3 | 3.1 | 2.8 | 1.3 | 2.2 | 2.2 | |
| p -Value | 0.007 | 0.000 | 0.115 | 0.1 | 0.163 | 0.161 | 0.388 | 0.152 | 0.015 | |
| Hypermobility after trauma | Preop | 2.9 | 6.3 | 0.7 | 75.3 | 84.7 | 30.7 | 33.8 | 89.4 | 90.0 |
| Postop | 0.2 | 0.7 | 1.0 | 78.0 | 83.8 | 29.0 | 34.6 | 90.0 | 90.0 | |
| Change | –2.7 | –5.6 | 0.3 | 2.7 | –0.9 | –1.7 | 0.8 | 0.6 | 0.0 | |
| p -Value | 0.000 | 0.000 | 0.047 | 0.170 | 0.400 | 0.126 | 0.364 | 0.085 | 0.500 |
Abbreviation: VAS, visual analog scale.
Table 5. Change in outcome with ACS.
| Change post operatively | Extension | Flexion | Radial deviation | Ulnar deviation | Supination | Pronation | VAS rest | VAS load | Grip gain |
|---|---|---|---|---|---|---|---|---|---|
| Without ACS (6) | 0.0 | 6.0 | 2.0 | 0.0 | 0.0 | 0.0 | –2.4 | –3.2 | +30.0% |
| With ACS (45) | 3.3 | 0.4 | –2.4 | 1.5 | 2.1 | 0.0 | –2.4 | –5.3 | +30.1% |
| p -Value | 0.334 | 0.236 | 0.114 | 0.373 | 0.324 | N/A | N/A | 0.0495 | Too few values |
Abbreviations: ACS, arthroscopic capsular shrinkage; N/A, not available; VAS, visual analog scale.
Table 6. Change in outcomes in JIA versus hypermobility without JIA patients.
| Change postop | VAS rest | VAS load | Extension | Flexion | Radial deviation | Ulnar deviation | Supination | Pronation | Grip strength |
|---|---|---|---|---|---|---|---|---|---|
| JIA (18) | –1.5 | –3.8 | 2.5 | 3.3 | 0.4 | –1.3 | 0.0 | 0.0 | +13.5% |
| Hypermobility without JIA (33) | –2.8 | –5.6 | 3.1 | 0.2 | –1.5 | 2.0 | 0.6 | 0.0 | +30.3% |
| p -Value | 0.024 | 0.019 | 0.460 | 0.250 | 0.190 | 0.150 | 0.200 | 0.500 | 0.434 |
Abbreviations: JIA, juvenile idiopathic arthritis; VAS, visual analog scale.
Table 7. Change in outcomes in JIA with impending collapse versus JIA with hypermobility.
| Change post op | Extension | Flexion | Radial deviation | Ulnar deviation | Supination | Pronation | VAS rest | VAS load |
|---|---|---|---|---|---|---|---|---|
| JIA without hypermobility but early signs of carpal collapse (13) | 8.8 | 8.8 | 3.8 | –0.6 | 0.0 | 0.0 | –1.6 | –3.6 |
| JIA with hypermobility (5) | –10.0 | –7.5 | –6.3 | –2.5 | 0.0 | 0.0 | –1.3 | –4.3 |
| p -Value | 0.007 | 0.011 | 0.005 | 0.377 | N/A | N/A | 0.371 | 0.323 |
Abbreviations: JIA, juvenile idiopathic arthritis; N/A, not available; VAS, visual analog scale.
Shrinkage versus No Shrinkage
There was no significant loss of ROM in either the ACS (45 patients) or non-ACS group (6 patients) ( Table 5 ). In both groups there was improvement in VAS at rest and load. While there was no difference between the groups for VAS scores at rest, there was a statistically significant improvement in VAS with load in favor of the ACS group (–3.2 without ACS and N5.3 with ACS, p = 0.05; Table 5 ). In those cases where ACS was not performed (six cases) a synovectomy was conducted in all cases. In two cases a steroid injection was also delivered, in one case a chondral flap was debrided and in one case a lesion of the triangular fibrocartilage complex was treated.
Hypermobility in JIA versus Hypermobility without JIA
Data were also analyzed to identify whether there were differences between those who had JIA or congenital arthritis (18 patients), and those who did not (33 patients). There was no difference in postoperative ROM, but there was significantly greater improvement for the non-JIA group in terms of both VAS at rest (–1.5 for JIA, –2.8 for non-JIA, p = 0.02) and VAS with load (–3.8 for JIA, –5.6 for non-JIA, p = 0.02) ( Table 6 ).
JIA with Hypermobility versus JIA with Early Signs of Carpal Collapse
Data were then analyzed to identify differences for those patients with JIA and hypermobility (5 patients), as compared with those with JIA but no hypermobility (13 patients). Within the JIA hypermobility group, there was surgical intent to tighten the lax capsule, and so a degree of stability is a goal of surgery. Within the JIA without hypermobility group there was concern about impending carpal collapse. The therapeutic aim was to perform synovectomy and then assess ligamentous stability. If there was laxity after synovectomy (11 out of 13 patients), then capsular shrinkage was indicated and was performed.
There was an improvement in ROM for those wrists which were not hypermobile but had preoperatively early signs of carpal collapse, which potentially can be seen as a result of the synovectomy. We achieved the desired stability in those which were hypermobile, as per the treatment aims. This difference reached significance for extension, flexion, and radial deviation ( Table 6 ), but there was no significant difference in VAS scores at rest or with load ( Table 7 ).
Complications
Complications were not seen in this cohort. However, in one patient with Stickler syndrome there was prolonged stiffness which took some months to settle. This patient had complex additional medical needs that required frequent treatment. Unfortunately, this meant that commitment and compliance with postoperative physical therapy was difficult. Extended therapy showed at final follow-up at 11 months that ROM had returned to preoperative levels. Two patients from the synovectomy without ACS cohort later complained of symptomatic hypermobility and were successfully treated with ACS, as described in the “Discussion” section.
Discussion
Evaluation of the Painful Wrist in the Pediatric Population
Painful wrist in the growing child or adolescent is a common presentation. The treatment is challenging as it is difficult to know if it is related to true pathology or an episodic phase in the child's growth. This becomes even more challenging in symptomatic midcarpal hypermobility because laxity is very common in most teenagers and managing this controversial problem with wrist surgery is a potentially fraught endeavor. Presentation, diagnosis, and treatment pathways are all subject to continued debate. Additional factors should be considered in the treatment of midcarpal hypermobility/instability in children and adolescents. A balance must be struck between time away from education, and addressing the need of a developing child to participate in symptom-free activities with their peers to facilitate physiological and psychological development. The patient's own perceptions of the limitations imposed on them by their symptoms will vary widely from patient to patient, and application of a blanket treatment algorithm is not possible in such circumstances.
In the evaluation of PMCI there is an important difference in our clinical finding of hypermobility, and the patient's perceived wrist instability. The subjective sensation of instability may present following a trauma which is often innocuous in nature, or a time of increased physiological load such as writing during examination periods. The balance of intrinsic and extrinsic constraints may be upset by a period of inactivity related to pain or immobilization, and abnormal kinematics may result, leading to both instability and pain as the proximal row subluxates. In our practice the presence of JIA has an additional contribution, as synovitis may stretch delicate capsular and ligamentous structures, and pain may limit the potential for conventional therapy.
For those who fail nonoperative treatment of PMCI, ACS with or without synovectomy if required, and followed by a period of immobilization, offers a safe and effective method of improving balance and allowing return to symptom-free activity. Multiple therapeutic targets are often present ( Tables 2 and 3 ). 10 At arthroscopy the joint space is capacious and synovitic ( Fig. 4 ), ligamentous laxity ( Fig. 1 ) and often associated ganglia or midcarpal fibrous bands are present. The shrinkage technique targets the volar capsule including the RSC, the long and short radiolunate, and ulnotriquetral ligaments. The distal RSC and triquetro-capitate ligaments are treated through the midcarpal portals ( Figs. 2 3 4 ).
Juvenile Idiopathic Arthritis
JIA (17 patients) or congenital arthritis (Stickler syndrome in one case) patients represented two-fifths (18/51) of our cohort. This is a heterogeneous group, and management can be challenging. Several treatment options have been described in an attempt to prevent or delay the characteristic deformity onset. AS has demonstrated good benefit in previously published studies, although ours is the largest cohort of wrist arthroscopy patients. 11 12 We previously reported a review of current literature on the benefits of AS which revealed a paucity of evidence for the use of AS in JIA. 13 In general, published case series involving adult patients demonstrated the technique to be safe with good effects on pain and wrist function. 11 13 14 15 Our results demonstrate that the JIA and congenital arthritis population can still expect good outcomes from ACS. Unpublished data from our institution also suggest that AS can be a useful treatment option for JIA that is refractory to medical treatment, but where there are no concerns with regard to stability. The improvements are more modest than in those patients without such diagnoses which seem to improve more impressively. This is likely to be on account of progression of the underlying disease process, but should not preclude the use of this treatment in view of our demonstrated benefit. The procedure of ACS in these cases is intended to delay disease progression due to increasing laxity of ligaments, rather than establish cure, and careful counseling is recommended to inform patient expectations.
We present both JIA and nonarthritis-related hypermobility cases in this article because our intention is to demonstrated safety and efficacy of the technique. Ligaments and capsule subjected to chronic synovitis are likely to become attenuated by the inflammatory process, which is not globally the case for the hypermobility group. We appreciate the cohort demonstrates some heterogeneity as a result, and for that reason we have conducted subgroup analysis to establish differences in outcome: improvements were seen across the range of indications.
Comparison with Previously Published Data
ACS in other joints has led to concerning loss of ROM and potential later arthrosis, which our data suggest do not apply the same procedure in children's wrists. The wrist may be considered unique as postoperative splinting is technically easy and does not confer significant functional loss to patients during the splinting period. 6 The procedure is considered more acceptable to patients and families as a result. In a small cohort series of 13 adult patients (average age 28) almost all patients improved significantly at a mean of 42 months' follow-up. 7 No complications were reported. The same group recently reported 12-year follow-up of 12 patients (14 wrists) demonstrating resolution of instability in 9 out of 12. 16
It should be noted, however, that published outcomes are variable. In one series of 16 adult patients with symptomatic PMCI (average age 33), 5 were treated with arthroscopic thermal capsular shrinkage. 4 Recurrence occurred in two patients who went on to have a pisiform-based split flexor carpi ulnaris tendon graft to reconstruct the dorsal radiocarpal ligament via a bone tunnel in the triquetrum, and then attached to Lister's tubercle.
The applicability to children of the adult data describing ACS for PMCI remains unclear. In 2011, one series reported 34 cases in which wrist arthroscopy had been used in children and adolescents (mean age 14.6 years) for a variety of indications including one case of midcarpal instability. 14 No intraoperative complications related to arthroscopy were reported, although complications related to combined procedures including dome osteotomy were recognized.
The senior authors previously reviewed literature concerning the use of wrist arthroscopy and synovectomy in patients with JIA. 13 There was a paucity of available evidence in JIA, although extensive data to support the use of open synovectomy and AS in rheumatoid arthritis in adults was available. Open synovectomy for JIA was advocated in multiple level IV studies with results suggesting relief of pain and improved function could be reliably expected. Additionally, there is good evidence to support the use of arthroscopy of the knee, hip, shoulder, and elbow in JIA.
Evolution of the Technique
PMCI was diagnosed preoperatively in all patients based on clinical assessment. Early on in the series ACS was applied only where laxity was present at arthroscopic examination or following the treatment of other intraoperative findings, for example, synovectomy. In two cases patients in the non-JIA cohort who had not undergone capsular shrinkage complained of symptomatic PCMI during follow-up. Both of these patients presented in the early stages of the senior author's practice evolution, and had been treated with synovectomy only following the identification of synovitis intraoperatively. Both were in their late teenage years and could no longer undergo surgery in our children's institution at the time of symptom deterioration. As a result, both were referred to local adult services, and in both cases ACS was performed with complete resolution of symptoms. This is an illustration of the utility of the procedure, as synovectomy alone had proved insufficient. Following their treatment the senior author's practice evolved always to involve ACS for the treatment of similar presentations.
Although both dorsal and volar ligaments are important in maintaining full mechanical control of PMCI, it has been our experience that only volar structures require thermal shrinkage. There have been informal, unpublished reports of extensor tendon rupture from dorsal shrinkage due to the thin dorsal capsule. Dorsal shrinkage was not used in our series, and this reduces the risk of inadvertent tendon disruption, while still achieving excellent outcomes.
Evaluation of the Technique
Interpretation of the success of a procedure in children and adolescents presents certain challenges. Our experience suggests the overwhelming majority of patients are pleased with the outcome of surgery, and those with bilateral symptoms will often request contralateral surgery after their rehabilitation is complete. Capturing such subjective data are difficult, and established scores such as Disabilities of the Arm, Shoulder and Hand and Patient-Reported Wrist Evaluation lose validity in the pediatric population. These measures are designed for adults and many of the activities they examine are not relevant to children. Instead, we have found that our patients engage well with VAS sampling, and we are encouraged by the improvement in both VAS for pain and for load following our interventions.
ACS is not a universal panacea and caution should be exercised in its consideration in the presence of objective imaging findings, such as significant flexion of the proximal row seen as a nonreducible volar intercalated segment instability deformity ( Fig. 5 ). For correctable deformities we would still consider ACS, but careful patient counseling is required regarding the possible temporary nature of symptom improvement, and that more durable soft tissue reconstruction or partial arthrodesis techniques may be required in adult life.
Fig. 5.

Lateral radiograph demonstrating irreducible volar intercalated segment instability (VISI) for which we would not consider arthroscopic capsular shrinkage (ACS).
Limitations of this Study
Our data are limited by being a single-center, single-surgeon experience. Additionally, there were some missing outcome data due to the coronavirus pandemic and the analysis described above is reliant on the data available. We are further limited by a lack of validated patient-reported outcome measures for the child and adolescent population, although we have found VAS to be a reliable predictor of progression in this age group.
Conclusion
The treatment of symptomatic midcarpal hypermobility and instability in pediatric hand surgery requires a careful tailored approach. Although our data demonstrate the success of ACS as a minimally invasive treatment, care should be taken into assessing both physical and psychological aspects at presentation. Once other causes for the wrist pain have been ruled out and the symptomatic midcarpal hypermobility has been treated nonoperatively for 3 to 6 months, our cohort series shows that an arthroscopic approach with ACS works very well in both posttraumatic children as well as in JIA. It should be emphasized that it should only be performed in centers with extensive experience in wrist arthroscopy in general, and in the technique of ligament/capsular shrinkage in particular.
Conflict of Interest None declared.
Note
The cases described in this article were treated by thesenior author, Miss K. Oestreich, at Birmingham Women's and Children's Hospital.
References
- 1.Mouchet A, Belot J. Poignet à ressaut: subluxation mediocarpienne en avant. Bull Mem la Soc Natl Chir. 1934;60:1243–1244. [Google Scholar]
- 2.Lichtman D, Bruckner J, Culp R, Alexander C E. Palmar midcarpal instability: results of surgical reconstruction. J Hand Surg Am. 1981;6(06):515–523. doi: 10.1016/0363-5023(93)90366-B. [DOI] [PubMed] [Google Scholar]
- 3.Lichtman D M, Bruckner J D, Culp R W, Alexander C E. Palmar midcarpal instability: results of surgical reconstruction. J Hand Surg Am. 1993;18(02):307–315. doi: 10.1016/0363-5023(93)90366-B. [DOI] [PubMed] [Google Scholar]
- 4.Ho P-C, Tse W-L, Wong C W. Palmer midcarpal instability: an algorithm of diagnosis and surgical management. J Wrist Surg. 2017;6(04):262–275. doi: 10.1055/s-0037-1606379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jing S S, Smith G, Deshmukh S. Demystifying palmar midcarpal instability. J Wrist Surg. 2021;10(02):94–101. doi: 10.1055/s-0040-1714688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgin R PC, Hargreaves D G. Midcarpal instability: the role of wrist arthroscopy. Hand Clin. 2017;33(04):717–726. doi: 10.1016/j.hcl.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Hargreaves D G. Arthroscopic thermal capsular shrinkage for palmar midcarpal instability. J Wrist Surg. 2014;3(03):162–165. doi: 10.1055/s-0034-1384838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia-Elias M. The non-dissociative clunking wrist: a personal view. J Hand Surg Eur Vol. 2008;33(06):698–711. doi: 10.1177/1753193408090148. [DOI] [PubMed] [Google Scholar]
- 9.Hagert E, Lluch A, Rein S. The role of proprioception and neuromuscular stability in carpal instabilities. J Hand Surg Eur Vol. 2016;41(01):94–101. doi: 10.1177/1753193415590390. [DOI] [PubMed] [Google Scholar]
- 10.Lindau T R. The role of arthroscopy in carpal instability. J Hand Surg Eur Vol. 2016;41(01):35–47. doi: 10.1177/1753193415616276. [DOI] [PubMed] [Google Scholar]
- 11.Toledo M M, Martini G, Gigante C, Da Dalt L, Tregnaghi A, Zulian F. Is there a role for arthroscopic synovectomy in oligoarticular juvenile idiopathic arthritis? J Rheumatol. 2006;33(09):1868–1872. [PubMed] [Google Scholar]
- 12.Evans D M, Ansell B M, Hall M A. The wrist in juvenile arthritis. J Hand Surg [Br] 1991;16(03):293–304. doi: 10.1016/0266-7681(91)90057-u. [DOI] [PubMed] [Google Scholar]
- 13.Vermaak P V, Southwood T R, Lindau T R, Jester A, Oestreich K. Wrist arthroscopy in juvenile idiopathic arthritis: a review of current literature and future implications. J Wrist Surg. 2018;7(03):186–190. doi: 10.1055/s-0038-1639508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farr S, Grill F, Girsch W. Wrist arthroscopy in children and adolescents: a single surgeon experience of thirty-four cases. Int Orthop. 2012;36(06):1215–1220. doi: 10.1007/s00264-011-1428-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee H I, Lee K H, Koh K H, Park M J. Long-term results of arthroscopic wrist synovectomy in rheumatoid arthritis. J Hand Surg Am. 2014;39(07):1295–1300. doi: 10.1016/j.jhsa.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 16.Ricks M, Belward P, Hargreaves D. Long-term results of arthroscopic capsular shrinkage for palmar midcarpal instability of the wrist. J Wrist Surg. 2021;10(03):224–228. doi: 10.1055/s-0040-1722331. [DOI] [PMC free article] [PubMed] [Google Scholar]


