Abstract
Objective
Describe the epidemiological profile and social-economic burden that hydrocephalus patients represent to the national public health system, using data available at the online database of the Brazilian Health Ministry (DataSUS).
Methods
This is a populational study based on descriptive statistics of all clinical and surgical appointments included in the DataSUS database. Data included herein were collected between 2015 and 2021 and subdivided into three main groups, related to hydrocephalus incidence and mortality, hospitalizations, and financial costs.
Results
In the study period, 3993 new cases of congenital hydrocephalus were diagnosed, with 6051 deaths overall. The mortality rate in the country was 1.5/100000 live births and the prevalence was 0.374/100000 inhabitants. The number of hospitalizations resulting from treatment procedures and complications of hydrocephalus was 137,880 and there was a reduction of up to 27.2% during the SARS-CoV-2 pandemics concerning previous years. Total costs for hydrocephalus management in the country amounted to 140,610,585.51 dollars.
Conclusions
Hydrocephalus has a significant impact on public health budgets and pediatric mortality rates; however, it is probably underestimated, due to the paucity of demographic data and epidemiological studies in Latin America and, specifically, in Brazil. The dataSUS also has several limitations in accessing certain data related to hydrocephalus, making it difficult to have a more assertive understanding of the disease in Brazil. The results of this study provide important guidance for future research projects in clinical and experimental hydrocephalus and also the creation of public policies for better governance and care of hydrocephalus patients.
KEYWORDS: Epidemiology, Hydrocephalus, National registry
Introduction
Hydrocephalus is a neurological disease characterized by disturbances in cerebrospinal fluid (CSF) circulation, caused by overproduction, lack of resorption, or obstruction to its normal pathways.1,2 The etiology is associated with genetic and environmental factors and, can be secondary to several pathological conditions including Central Nervous System malformations, congenital infections, hemorrhages, and tumors, among others.3 The mainstay of treatment for hydrocephalus is surgery, most often ventriculoperitoneal shunt and endoscopic third ventriculostomy.4,5
There are many complications of shunt surgery (30-40% of patients), notably within the first six post-operative months. Obstruction, disconnection, migration, along with infections, are the most common causes. Although infection rates have been reduced, morbidity and mortality remain high. Also, shunts have late complications (biodegradation), which might require reoperations and prolonged in-hospital stay.2 Therefore, the financial burden can be quite steep, considering the need for intensive care therapy and the replacement of the shunt system.4
In Brazil, the management of hydrocephalus can be done either in the private or public sector. The public system is called Sistema Unico de Saude (SUS), which was implemented on September 19th, 1990 after Organic Law number 8080. It has many public health tools, the most important of which is a Department of Information Technology named DataSUS, to form structured information systems that integrate all SUS data and improve public health management. With several regional offices in close contact with local providers, health services and technical cooperation are encouraged.6
Considering that there is a lack of epidemiological data about hydrocephalus in Brazil, a thorough assessment of the national database would afford valuable perceptions that could work as a guide for future policies and investments in public health. The goal of this study is to characterize the epidemiological profile and social-economic burden that hydrocephalus represents to the SUS, using information available at DataSUS.
Methods
This is a populational study, based on descriptive statistics, to outline the demographics and treatment variables (including complications) of hydrocephalus in Brazil. All data included were obtained from DataSUS (available at http://www2.datasus.gov.br), whose server is classified and organized according to the International Statistical Classification of Diseases and Related Health Problems, 10th review (ICD-10), and is supplied by the public and private institutions affiliated with the SUS, through regulated forms. As all information is in the online public domain, approval by an ethics committee is not required. This study was divided into three subgroups: 1. Vital Statistics: anomalies or congenital defects diagnosed in live births (2015-2019); 2. Vital Statistics: mortality (2015-2019); and 3. Healthcare Data and Hospitalizations (2015-2021) (Fig. 1). The expenditure values obtained were calculated in Brazilian currency (R$) and converted into dollars according to the previous annual average real-dollar R$= $3.32 (2015); $3.49 (2016); $3.19 (2017); $3.62 (2018); $=3.92 (2019); $=5.06 (2020); $=5.32 (2021).
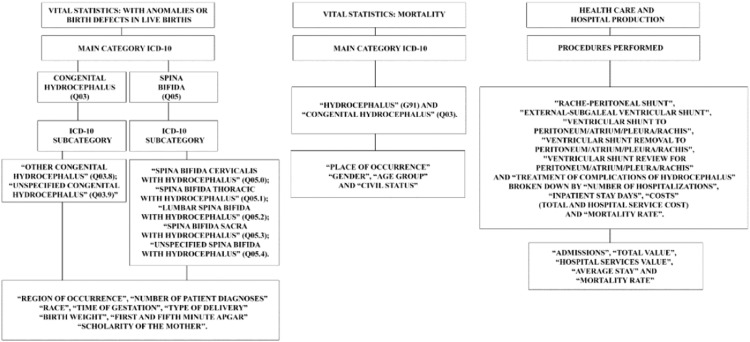
Fig. 1.
Flowchart of the strands and their access in DataSUS. Based on each aspect, diagnoses were used according to their main categories and subcategories according to the ICD-10 classification.
Results
Vital statistics: Anomalies or congenital defects diagnosed in live births
Geographic regions
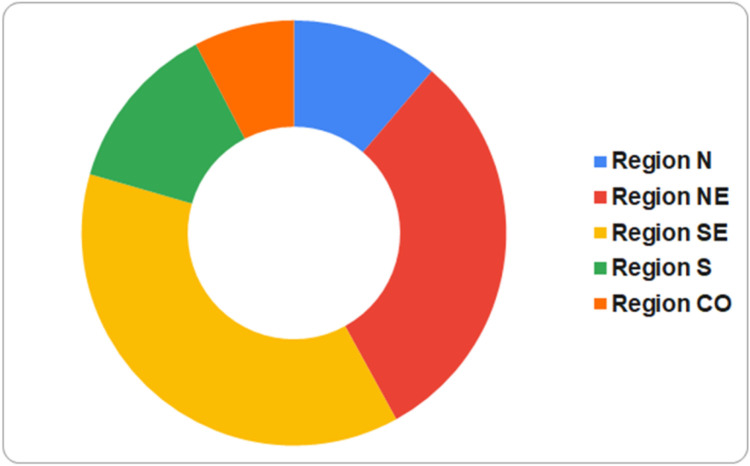
The authors identified 3993 live births diagnosed with at least one of the congenital hydrocephalus classifications. The overall prevalence was 0.374 per 100.000 inhabitants (Fig. 2). The southeastern (SE) region was the one with the highest number of cases, followed by the northeastern (NE), south (S), midwest (CO), and north (N). However, the N region has the highest incidence rate (0.475 cases/year), notably the state of Acre (0.662 cases/year), which had the highest rate. With a rate of 0.426, the NE came second, then the CO (0.365), S (0.339), and SE, which, despite having a larger caseload, had the lowest incidence (0.334) (Supplementary material - Table 1).
Fig. 2.
Number of hydrocephalus cases available in dataSUS by Brazilian region from 2015 to 2019. N: North, NE: Northeast, SE: Southeast, S: South and CO: Midwest. The SE (37.5%) and NE (30.8%) regions had the highest number of cases in the period evaluated and the CO region had the lowest rates. (Ministry of Health - Live Births Information System - SINASC).
Hydrocephalus diagnoses according to ICD-10
Unspecified congenital hydrocephalus was the most frequent diagnosis at 74.9% (2992), followed by other congenital hydrocephalus at 10.3% (411). The authors also identified the association of spina bifida with hydrocephalus, as follows: 261 patients (6.5%) unspecified, 149 (3.7%) cervical, 102 (2.6%) lumbar, 49 (1.2) sacral and 29 (0.7%) thoracic. Furthermore, 59.9% (2390) patients were diagnosed only with hydrocephalus, whereas 20.3% (811) had two diagnoses, 7.7% (308) three, 3.8% (153) four, and 2.6% (105) five or more.
Ethnicity
The N region had the highest percentage of mixed African American patients (85.3%), the lowest of Caucasian (6.7%), also having 2.4% of black African, 6.2% of native Americans, and 1.1% with an unspecified ethnicity. The NE region had the following distribution: 76.1% (934) mixed African American, 7.8% (96) Caucasian, 5% (61) black African, 0.4% (5) Native American, 0.2% (2) Asian at 10.6% (130) of unspecified. In the CO, 51.8% (158) were mixed African American, 22.6% (69) Caucasian, 6.6% (20) Native American, 2.0% (6) Asian and 12,8% (39) unspecified. The SE region had 44.7% (669) of Caucasian patients, 44.3% (662) mixed African American, 8.6% (128) black African, 0.1% (1) native, 0.5% (7) Asian and 1,9% (29) unspecified. Lastly, 79.8% (441) as Caucasian, 15.7% (81) were mixed African American, 3.1% (16) black African, 0.4% (2) Asian, 0.2% (1) native and 0.8% (4) were unspecified in the S region.
Gestational aspects
Prematurity (birth before 37 weeks of pregnancy), occurred in 34.7% (1384), of which 80 (2%) were extreme prematurity (before 28 weeks). Delivery was most frequently via cesarean section 88.8% (3545), whilst vaginal delivery corresponded to 11% (447) of cases.
Birth weight and Apgar scores
Ninety-five (2.4%) weighed less than 999g at birth; 157 (3.9%) between 1000-1499g; 748 (18.7%) between 1500-2499g; 789 (19.8%) between 2500-2999g; 1688 (42.3%) between 3000-3999g; and 515 (12.9%) more than 4000g. The analysis of one-minute Apgar scores revealed that 55.6% (2223) of hydrocephalic children were born with depressed clinical responses, with scores ≤ 8. Around half of these children (1083 – 27.2%) didn't recover in the fifth minute and kept a score below 8. On the other hand, 1715 children (43%) in one-minute and 2849 (71.3%) in fifth-minute scores were born with good clinical status and had scores above 8.
Maternal educational level
This parameter was assessed as years spent in school: 19 (0.47%) mothers had no schooling whatsoever; 106 (2.65%) stayed 1-3 years in school; 766 (19.18%) between 4-7 years; 2422 (61,15%) between 8-11 years, which means they got to high school; 642 (16.07%) had over 12 years of schooling and 38 (0.95%) not informed. The NE region had the highest number of mothers who didn't get to high school (357), followed by the SE (241), N (125), S (107), and CO regions (65). Conversely, the SE (300) and NE (124) were the regions with the biggest quantity of mothers who went to college, particularly São Paulo (200), Bahia (33), and Ceará (23).
Vital statistics: Mortality rates
The coefficient of mortality was calculated using the Brazilian estimated population in 2017 as per the Brazilian Institute of Geography and Statistics (IBGE) Coordination Committee of Population and Social Indicators (COPIS).7 Overall, deaths caused directly by hydrocephalus in Brazil, comprised 6051 cases (Fig. 3), of which 3966 were cast as non-specified hydrocephalus and 2085 as congenital hydrocephalus; 259 were stillborn.
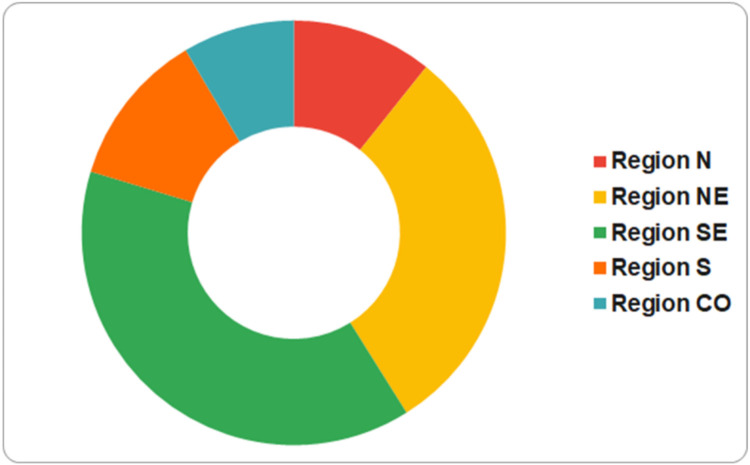
Fig. 3.
Total number of deaths from hydrocephalus and congenital hydrocephalus by Brazilian region from 2015 to 2019. N: North, NE: Northeast, SE: Southeast, S: South and CO: Midwest. The SE (38.6%) and NE (30.4%) regions were the ones with the highest number of deaths from hydrocephalus and congenital hydrocephalus in the studied period, according to DataSUS (Ministry of Health - Live Births Information System - SINASC).
The N region has the highest mortality rate (0.036/1000 inhabitants), followed by the NE and CO with 0.032. States with striking mortality coefficients include Amapá (0.064), Piauí (0.052), Roraima (0.048), and Paraíba (0.043). It is worth mentioning that the SE region, despite having the largest total death count (2264), had a lower mortality rate (0.027), second only to the S region (0.024); states with low mortality are Minas Gerais (0.025), São Paulo (0.027), Santa Catarina (0.023) and Rio Grande do Sul (0.020) (Supplementary material - Table 2).
Such deaths occurred most frequently in hospitals at 82,8% (5010), followed by household at 12,3% (746), other healthcare facilities 3,4% (206), other locations 1,1% (64), public roads 0,4% (22) and ignored in 0,1% (3). The proportions of in-hospital deaths were quite similar in all regions of the country: 83,8% (1957) SE; 83% (594) S; 82,7% (426) CO; 82,1% (1508) NE; and 80,9% (525) N, whereas the percentages of household deaths were: N 15,4% (100); NE 13,9% (255); S 12,4% (89); CO 12,4% (64); and SE 10,2% (238).
Gender
About the distribution of deaths: 53.4% males, 45.9% females, and 0.7% uninformed (N); 53.1% males, 46.8% females, and 0.1% uninformed (NE); 54.9% males, 44.9% females and 0.2% uninformed (SE); 54.6% males and 45.4% females (S); 52.3% males, 47.6% females and 0.1% uninformed (CO).
Age
The average national mortality rate for children was 0.10, which means that one child out of every 10000 live births dies due to hydrocephalus within their first year of life in Brazil. The N region had the highest mortality rate (0.18), followed by the NE (0.16) and CO (0.11). Significant lower rates were seen in the SE (0.07) and S (0.06). States with the highest infant mortality rates secondary to hydrocephalus were Roraima (0.22) and Amazonas (0.20), while Rio Grande do Sul (0.05) and Minas Gerais (0.07) had the lowest ones. Furthermore, 46.9% (145) of deaths in the N region were in children less than 9 years, and 19.7% (61) less than 1 year; in the state of Roraima, for instance, there were 17 deaths, of which 13 (76.5%) were under 9 years and 7 (41.2%) were under one year of age. The NE had rates of 34.7% (415) below 9 years and 15.3% (183) below 1 year, whereas the CO had a 13.4% (39) rate of deaths below one year, followed by the SE 6.7% (113) and S 2.9% (14). For comparison, mortality rates due to hydrocephalus in adults over 60 years old were, for the same period, 16.2% in the N, 20.4% NE, 35.3% CO, 53.6% S, and 44.3% SE regions.
Congenital hydrocephalus (as notified, and not including stillborns) accounted for 62.2% (213) in the N, notably the states of Rondônia (76.2%) and Amapá (68.2%), 52,4% in the NE (Sergipe 70%), 47.9% S, 48.7% SE and 47.1% in the CO.
Health care services: Hospital data
Admissions
A total of 137800 admissions due to hydrocephalus treatment and complications were listed. DataSUS does not distinguish patients individually, so this total number may refer to many admissions of a single patient. The SE region had 57557 (41.7%) admissions (32080 in the state of Sao Paulo alone, which comprise 23.3% of all hydrocephalus admissions, and Minas Gerais with 15040 admissions), followed by the NE 35386 (25.7%), S 25152 (18.3%), CO 10695 (7.7%) and N 9090 (6.6%) regions.
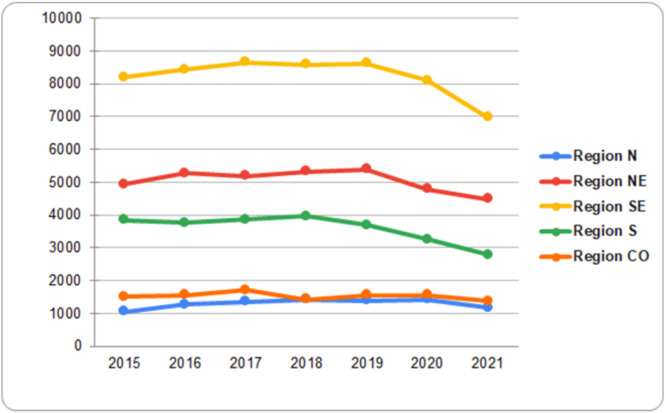
Between 2020 and 2021, admission statistics differed significantly, certainly due to SARS/CoV pandemic (Fig. 4). Considerable decreases were seen in the S region, which suffered the highest impact, with reductions of 15% (3250 admissions) and 27.2% (2782) in 2020 and 2021, respectively. Likewise, the SE had a reduction of 4.7% (8100) and 17.9% (6975), and the NE 8.3% (4790) and 14.3% (4475) for 2020 and 2021. Interestingly, in the year 2020, such differences were not found in the CO and N regions but, in 2021, admissions were 11.5% and 10.5% shorter, respectively (Supplementary material - Table 3).
Fig. 4.
Hospitalizations for treatment procedures and complications of hydrocephalus from 2015 to 2021. N: North, NE: Northeast, SE: Southeast, S: South and CO: Midwest. It is noted that the SE and NE regions had the highest hospitalization rates and the N region had the lowest. (Ministry of Health - Live Births Information System - SINASC).
Surgical admissions
As with the number of hospitalizations, DataSUS does not distinguish between patients individually, therefore, the number of procedures may refer to more than a single patient. The following surgical procedures were performed for treating hydrocephalus, according to the Brazilian Classification of Medical Procedures (CHBPM): ventriculoperitoneal/atrial/pleural shunt: 53067 notifications, external/subgaleal shunt: 50952, treatment of hydrocephalus complications: 23585, and lumboperitoneal shunt: 798. Also, there were 2079 e 7399 notifications, respectively, of shunt removal and shunt revisions.
Costs
Admissions
The total amount spent on hydrocephalus treatment in Brazil was $140,610,585.51. The SE region used the biggest fraction (44.9%), making up $63,171,293.12, followed by the NE ($31,703,993.37) and S regions ($27,464,330.00). The CO and N had the lowest expenditures, with $10,693,188.73 and $7,577,780.29, respectively.
Considering 137800 total admissions, and that all the budget would be completely spent on these, each one would cost, on average, $1,020.39. However, there are substantial disparities amongst regions. The SE region had an average cost of $1,097.54; S, $1,091.93; CO, $999.83; NE, $895.94; and N, $833.63. Nationally, the mean in-hospital period for hydrocephalus management is 11 days.
Complications of the treatment of hydrocephalus – Hospital costs and mortality
The cost of hospital-related services represents the direct expenses as indicated and approved by hospital boards and included in the database; therefore, it does not include indirect costs. Overall, $114,502,432.00 were spent on in-hospital treatment of hydrocephalus. Regional distribution was as follows: SE ($51,831,866.83), NE ($25,393,674.09), S ($22,627,306.77), CO ($8,687,450.52), and N ($5,962,133.79). Deduction of in-hospital costs for total costs allows for an assessment of indirect expenses; thus, 21.3% of total costs in the N region came from indirect expenses, in comparison with 19.8% in the NE, 18.6% CO, 17.9% SE, and 17.5% in the S region. Mean mortality rates for every 100 procedures performed to treat complications varied among regions: SE (15.3), CO (13.8), N (12.3), S (12,3), and NE (11.6) (Supplementary material - Table 4).
Discussion
Albeit the management of hydrocephalus has great medical and social relevance, due to its high prevalence and vast clinical repercussions, there is still a paucity of precise epidemiological information in Brazil. DataSUS has been created to gather data throughout the country, but insertion relies on local or regional personnel and is still underperformed, which hinders clear-cut analyses.
The present study has shown that the prevalence of congenital hydrocephalus in Brazil is 0.374 per 100000 inhabitants, which is quite below other populational estimates abroad.8, 9 The authors hypothesize that only a partial caseload has been contemplated, mainly due to the sub-notification but also to DataSUS limitations that do not allow us to distinguish post-hemorrhagic and post-infectious hydrocephalus. Such difficulties have been also described in another international study.8 Nonetheless, the global prevalence of hydrocephalus is approximately 80 cases for every 100000 individuals, including those with spina bifida and other causes of childhood hydrocephalus. In Latin America, the estimated incidence is 316 cases for every 100000 births.8, 9, 10
From an ethnical standpoint, the number of cases was proportional to ethnical distributions regional, which can be explained by historical issues such as colonization and internal migration patterns.11 Similarly, the study of Naftel et al.12 has not shown ethnical differences in the prevalence of hydrocephalus, concluding that cultural and social factors determine different standards of healthcare.8,9 Likewise, Attenello et al.13 have reported that African American patients had an increased likelihood of inpatient death (56%) and nonroutine discharge (30%) compared with white patients after CSF shunt procedures.
It wasn't possible to collect sufficient data regarding gestational age and diagnosis of hydrocephalus, but it is well-known that planned pregnancy and prenatal care have a clear impact on the outcome. Garne et al.,14 found that 61% of cases are diagnosed within the prenatal period, which might lead to higher rates of termination of pregnancy (TOP). Johnson et al.15 reported that termination of pregnancy is most common when hydrocephalus is diagnosed before 24 weeks of gestation since, after that, there is great variability in national law codes, which restrain termination. However, this fact must be considered and explains, in part, lower incidences of hydrocephalus in places where TOP is legally permitted.
The cesarean section was the most frequent delivery route (88.8%). Morgan et al.16 showed that such delivery for babies with ventriculomegaly can expedite clinical and surgical management. Its benefits have not been proven, since comorbidities, infection rates, and a need for repeat surgeries, were significantly high. Moritake et al.17 also reported that, although cesarean section was used more frequently, patients born by transvaginal delivery had fewer complications and better clinical courses. The authors claim that complications of the surgical procedure can be responsible for this, and even though cesarean sections are the favorite for cases with cephalopelvic disproportion because they most likely prevent traumatic and ischemic injury to the fetus, these benefits still lack clear scientific evidence.
The educational status of caretakers has a significant relationship with the diagnosis and treatment of hydrocephalus, allowing for adequate follow-up.8 In Brazil, predominantly, hydrocephalic children are taken care of by their mothers,18 which were shown to have unsatisfactory schooling levels: 78% didn't reach high school and only 16% went to college. Similar figures were reported by Naftel et al.12
Infant mortality is a strong social sustainability index for the assessment of the quality of life, healthcare, and public sanitation aspects.19 Brazilian regions with large mortality rates secondary to hydrocephalus also were the ones with higher general mortality rates, according to the Brazilian Ministry of Health bulletin of 2021,20 which confirms the importance of adequate local health and sanitary conditions.21,22 The majority of hydrocephalus-related deaths occurred inside hospitals, contrary to the study of Tully et al.,23 performed in the US.
The management of complications treatment, particularly shunt revisions, was responsible for a great number of admissions, due to high rates of shunt malfunction within the first post-operative year, but also in subsequent years, as the children would grow. Infections were also a frequent complication, estimated to affect one out of five individuals. On average, patients might experience a 2 to 4-fold increase in the risk of complications within the initial 10 years.8,12,24
Regarding financial burden, the total expenditure on procedures for treating hydrocephalus, reached $140 million, with a mean cost of $1,020.39 per hospital admission. An Australian study revealed a total cost of AUD$4.78 (mean 1.59 million/year) and a mean cost of AUD$9.753 per inpatient admission.25 In the US, admissions for hydrocephalus costs around $2 billion/year.9 Costs in Brazil are likely underestimated, due to the already-mentioned biases. The state of São Paulo came first in the number and cost of admissions, certainly because it is the most populous state, with better healthcare services.26,27
The authors noted a significant reduction in admissions between 2020 and 2021 in comparison with previous years, probably due to the SARS-CoV-2 pandemic. Lubansu et al.28 have observed similar data, with a considerable decline in neurosurgical procedures after the pandemic, raising concerns that the search for medical care and the realization of surgeries might have been delayed. Pricop et al.29 evaluated the adverse effects of the pandemic on hydrocephalus. The most deleterious impact was on patients who waiting for scheduled surgical procedures, without a definitive diagnosis or family support.
At the moment, there are no epidemiological data in the literature covering hydrocephalus in Brazil or any other specific Latin American country, only data from some services or local hospitals.30 Thus, this is the first work that surveys this information at the national level, exposing the regional differences in Brazil. However, taking into account the stipulated data for all the Latin America and other global data,8, 9, 10 it's possible to conclude that there's still a large underreporting of cases and procedures in Brazil, in addition to the impossibility of specifying data due to limitations of the DataSUS. The authors evidence regional discrepancies, upholding the fragile socioeconomic realm of the country regarding high-quality healthcare; also, the economic burden represented by hydrocephalus on public health has been demonstrated. For a complete observation of all the search engines that the authors did on the DataSUS platform and their results, the authors have inserted all the tables in the supplementary materials. Unfortunately, hydrocephalus remains a significant cause of infant mortality. All data presented herein can be useful in the elaboration of future policies and healthcare organization systems that manage hydrocephalus cases.
Funding
This research has not received any specific funding from agencies in the public, commercial or non-profit sectors.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jped.2022.10.008.
Appendix. Supplementary materials
References
- 1.Deren KE, Packer M, Forsyth J, Milash B, Abdullah OM, Hsu EW, et al. Reactive astrocytosis, microgliosis and inflammation in rats with neonatal hydrocephalus. Exp Neurol. 2010;226:110–119. doi: 10.1016/j.expneurol.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 2.Kahle KT, Kulkarni A V, Limbrick DD, Warf BC. Hydrocephalus in children. Lancet. 2016;387:788–799. doi: 10.1016/S0140-6736(15)60694-8. [DOI] [PubMed] [Google Scholar]
- 3.Cavalcanti DP, Salomão MA. Incidence of congenital hydrocephalus and the role of the prenatal diagnosis. J Pediatr (Rio J) 2003;79:135–140. [PubMed] [Google Scholar]
- 4.de Lima BO, Pratesi R. Endoscopic third ventriculostomy has no higher costs than ventriculoperitoneal shunt. Arq Neuropsiquiatr. 2014;72:524–527. doi: 10.1590/0004-282x20140070. [DOI] [PubMed] [Google Scholar]
- 5.Vogel TW, Bahuleyan B, Robinson S, Cohen AR. The role of endoscopic third ventriculostomy in the treatment of hydrocephalus Clinical article. J Neurosurg Pediatr. 2013;12:54–61. doi: 10.3171/2013.4.PEDS12481. [DOI] [PubMed] [Google Scholar]
- 6.Brasil. Ministério da Saúde [Internet]. Sobre o DATASUS. [cited 2022 Jan 31]. Available from: https://datasus.saude.gov.br/sobre-o-datasus/.
- 7.Coordenação de População e Indicadores Sociais (COPIS), IBGE [Internet]. Estimativas da População. [cited 2022 Jan 22]. Available from: https://www.ibge.gov.br/estatisticas/sociais/populacao/9103-estimativas-de-populacao.html?edicao=17283&t=downloads.
- 8.Tamber MS. Insights into the epidemiology of infant hydrocephalus. Childs Nerv Syst. 2021;37:3305–3311. doi: 10.1007/s00381-021-05157-0. [DOI] [PubMed] [Google Scholar]
- 9.Isaacs AM, Riva-Cambrin J, Yavin D, Hockley A, Pringsheim TM, Jette N, et al. Correction: age-specific global epidemiology of hydrocephalus: systematic review, metanalysis and global birth surveillance. PLoS One. 2019;14 doi: 10.1371/journal.pone.0210851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dewan MC, Rattani A, Mekary R, Glancz LJ, Yunusa I, Baticulon RE, et al. Global hydrocephalus epidemiology and incidence: systematic review and meta-analysis. J Neurosurg. 2019;130:1065–1079. doi: 10.3171/2017.10.JNS17439. [DOI] [PubMed] [Google Scholar]
- 11.Instituto Brasileiro de Geografia e Estatística: IBGE [Internet]. Desigualdades Sociais por Cor ou Raça no Brasil. [cited 2022 Jan 31]. Available from: https://www.ibge.gov.br/estatisticas/sociais/populacao/25844-desigualdades-sociais-por-cor-ou-raca.html?=&t=conceitos-e-metodos.
- 12.Naftel RP, Safiano NA, Falola M, Blount JP, Oakes WJ, Wellons JC. The association between race and frequent shunt failure: a single-center study. Clinical article. J Neurosurg Pediatr. 2013;11:552–557. doi: 10.3171/2013.1.PEDS12425. [DOI] [PubMed] [Google Scholar]
- 13.Attenello FJ, Ng A, Wen T, Cen SY, Sanossian N, Amar AP, et al. Racial and socioeconomic disparities in outcomes following pediatric cerebrospinal fluid shunt procedures. J Neurosurg Pediatr. 2015;15:560–566. doi: 10.3171/2014.11.PEDS14451. [DOI] [PubMed] [Google Scholar]
- 14.Garne E, Loane M, Addor MC, Boyd PA, Barisic I, Dolk H. Congenital hydrocephalus - prevalence, prenatal diagnosis and outcome of pregnancy in four European regions. Eur J Paediatr Neurol. 2010;14:150–155. doi: 10.1016/j.ejpn.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Johnson CY, Honein MA, Flanders WD, Howards PP, Rasmussen SA, Disabilities D. Pregnancy termination following prenatal diagnosis of anencephaly or spina bifida: a systematic review of the literature. Birth Defects Res A Clin Mol Teratol. 2012;94:857–863. doi: 10.1002/bdra.23086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morgan CD, Ladner TR, Yang GL, Moore MN, Parks RD, Walsh WF, et al. Early elective delivery for fetal ventriculomegaly: are neurosurgical and medical complications mitigated by this practice? Childs Nerv Syst. 2018;34:829–835. doi: 10.1007/s00381-017-3662-0. [DOI] [PubMed] [Google Scholar]
- 17.Moritake K, Nagai H, Nagasako N, Yamasaki M, Oi S, Hata T. Diagnosis of congenital hydrocephalus and delivery of its patients in Japan. Brain Dev. 2008;30:381–386. doi: 10.1016/j.braindev.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Tavares P de AJ, Ukawa TB, Hamamoto Filho PT, de Avila MAG. Evaluating educational material from the perspective of informal caregivers of children with hydrocephalus: a qualitative study. World Neurosurg. 2020;139:427–433. doi: 10.1016/j.wneu.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Paixão AN, Ferreira T. Determinantes da mortalidade infantil no Brasil. Inf Gepec. 2012;16:6–20. [Google Scholar]
- 20.Brasil. Ministério da Saúde, Secretaria de Vigilância em Saúde [Internet]. Boletim epidemiológico 37. [cited 2022 Jan 24]. Available from: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/boletins-epidemiologicos/edicoes/2021/boletim_epidemiologico_svs_37_v2.pdf.
- 21.Alves TF, Coelho AB. Infant mortality and gender in Brazil: an investigation using updated statistics. Cien Saude Colet. 2021;26:1259–1264. doi: 10.1590/1413-81232021264.04022019. [DOI] [PubMed] [Google Scholar]
- 22.Mombelli MA, Sass A, Molena CA, Téston EF, Marcon SS. Fatores de risco para mortalidade infantil em municípios do Estado do Paraná, de 1997 a 2008. Rev Paul Pediatr. 2012;30:187–194. [Google Scholar]
- 23.Tully HM, Doherty D, Wainwright M. Mortality in pediatric hydrocephalus. Dev Med Child Neurol. 2022;64:112–117. doi: 10.1111/dmcn.14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Health Service [Internet]. Complications Hydrocephalus. [cited 2022 Jan 25]. Available from: https://www.nhs.uk/conditions/hydrocephalus/complications/.
- 25.Pham AC, Fan C, Owler BK. Treating pediatric hydrocephalus in Australia: a 3-year hospital-based cost analysis and comparison with other studies: Clinical article. J Neurosurg Pediatr. 2013;11:398–401. doi: 10.3171/2013.1.PEDS12233. [DOI] [PubMed] [Google Scholar]
- 26.Instituto Brasileiro de Geografia e Estatística: IBGE [Internet]. Projeções da População do Brasil e Unidades da Federação por sexo e idade: 2010-2060. [cited 2022 31 Jan]. Available from: https://shre.ink/m7ju.
- 27.Macroplan Analytics [Internet]. Desafios da Gestão Municipal (DGM). 4 ed. [cited 2022 Jan 31]. Available from: https://www.macroplan.com.br/dgm2020/.
- 28.Lubansu A, Assamadi M, Barrit S, Dembour V, Yao G, El Hadwe S, et al. COVID-19 Impact on neurosurgical practice: lockdown attitude and experience of a European Academic Center. World Neurosurg. 2020;2507:1–9. doi: 10.1016/j.wneu.2020.08.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pricop DF, Subotic A, Anghelescu BA, Eagles M, Hamilton M, Roach P. Impacts of the COVID-19 pandemic on the healthcare provision and lived experiences of patients with hydrocephalus. J Patient Exp. 2022;9:2. doi: 10.1177/23743735221092555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jucá CE, Lins Neto A, de Oliveira RS, Machado HR. Treatment of hydrocephalus by ventriculoperitoneal shunt: analysis of 150 consecutive cases in the Hospital of the Faculty of Medicine of Ribeirão Preto. Acta Cir Bras. 2002;17:59–63. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.