Abstract
Background
The COVID-19 pandemic significantly increased depression prevalence in general population. However, the relationship between persistent dysfunctional thinking associated with COVID-19 (perseverative-cognition) and depression, and its potential moderators are understudied. We aimed to examine the association between COVID-19 perseverative-cognition and depression, and the moderating effect of potential risk and protective factors on this association in general public during the peak of fifth COVID-19 wave in Hong Kong.
Methods
This survey recruited 14,269 community-dwelling adults between March 15–April 3, 2022 to investigate association between COVID-19 perseverative-cognition and depression, and the moderating effect of resilience, loneliness and three coping strategies (including emotion-focused, problem-focused and avoidant coping) on this association, using hierarchical regression models and simple slope analyses. COVID-19 perseverative cognition was assessed by the Obsession with COVID-19 Scale (OCS) and depressive symptoms were measured by the Patient Health Questionnaire-9 (PHQ-9).
Results
Perseverative-cognition was positively associated with depression severity. Resilience, loneliness and three coping strategies moderated the association between perseverative-cognition and depression. Specifically, greater resilience and emotion-focused coping ameliorated the association between perseverative-cognition and depression, while higher levels of loneliness, avoidant and problem-focused coping accentuated such association.
Limitations
Cross-sectional design precluded establishing causality among variables.
Conclusion
This study affirms that COVID-19 perseverative-cognition is significantly related to depression. Our findings indicate the potential critical role of enhanced personal resilience and social support, and adoption of emotion-focused coping in mitigating negative effect of COVID-19 related maladaptive thinking on depression severity, thereby facilitating development of targeted strategies to reduce psychological distress amidst the prolonged pandemic.
Keywords: COVID-19, Depression, Persistent dysfunctional thinking, Loneliness, Resilience, Coping styles
1. Introduction
Coronavirus disease (COVID-19) imposes public health crisis and disruptive impacts on individuals and society at large locally and globally. Despite continuous and stringent public health and social measures, Hong Kong (HK) experienced the fifth wave of COVID-19 following the emergence of the Omicron variant in December 2021, with the 7-day rolling average of COVID-related deaths having reached 3.73 per 1000 people at the peak, the highest worldwide (Cheung et al., 2022; Lee, 2022). It is acknowledged the prolonged COVID-19 pandemic is associated with a sense of uncontrollability and uncertainty. Repetitive exposure to such continual and ongoing stressful encounters may result in perseverative cognition, which is persistent dysfunctional and disturbing thinking manifested in worry and rumination (Brosschot et al., 2006). Perseverative cognition has been robustly implicated in the onset of depression (Michl et al., 2013; Watkins and Roberts, 2020). Substantial evidence has shown an increased prevalence of depression in the general public during the pandemic (Bueno-Notivol et al., 2021; Wu et al., 2021). However, there is a paucity of research examining the role of COVID-19 perseverative cognition and other vulnerability factors in the emergence of depressive symptoms within a socio-ecological framework (Bronfenbrenner and Evans, 2000), which is a proposed meta-paradigm conceptualizing depression, taking into consideration multi-level correlates at the individual and societal levels including important risk and protective factors such as resilience, loneliness, and coping strategies.
Resilience is the inter- and intra-personal capacity to bounce back from stress in an adversity-adaption dyad (Luthar, 2015). Literature revealed a protective effect of resilience against depression (Chmitorz et al., 2021; Luthar, 2015). High degree of resilience is also found to reduce depressive symptoms (Anyan et al., 2017; da Silva-Sauer et al., 2021) and mitigate the effect of pandemic-related stress on negative mental health outcomes (Chan et al., 2021; Havnen et al., 2020). Conversely, it is acknowledged that loneliness (or lack of social support) is closely linked to occurrence and exacerbation of depression (Ibarra-Rovillard and Kuiper, 2011; Thoits, 2011). Recent COVID-19 studies also showed that greater perceived social support was associated with fewer depressive symptoms (Grey et al., 2020; Probst et al., 2020). Alternatively, previous studies consistently demonstrated a strong association between coping behaviors and depression (Langlois, 2013; Morrow and Nolen-Hoeksema, 1990), but most focused only on maladaptive coping. In fact, coping behaviors have been broadly conceptualized into three major categories including problem-focused, emotion-focused and avoidant coping strategies (Coolidge et al., 2000; Litman, 2006). Recent data suggested that pandemic-related stress may interact with maladaptive coping strategies to influence depressive symptom severity (Reid et al., 2022; Wang et al., 2022). Notably, few studies have been conducted to concurrently investigate resilience, loneliness and coping strategies and their relationship with depression during the pandemic.
In the current study, we aimed to examine the relationship between COVID-19 perseverative cognition and depressive symptoms in a large sample of community-dwelling adults during the peak of the fifth wave of COVID-19 in HK. We evaluated the potential moderating role of resilience, loneliness and three coping strategies (problem-focused, emotion-focused and avoidant coping) on the association between COVID-19 perseverative cognition and depression. Based on prior research, we hypothesized that COVID-19 perseverative cognition would be positively related to depressive symptom severity. We anticipated that resilience, loneliness and coping strategies would moderate the relationship between COVID-19 perseverative cognition and depression. Specifically, resilience and adoption of emotion- and problem-focused coping were hypothesized to ameliorate the negative impact of dysfunctional thinking on depression, while loneliness and avoidant coping were expected to increase the adverse effect of dysfunctional thinking on depression.
2. Method
2.1. Participants and procedure
This cross-sectional survey aimed to recruit community-dwelling adults in HK from March 15 to April 3, 2022, during which the city was experiencing the peak of the fifth COVID-19 wave. It was estimated that approximately half of the population (3.6 million) have contracted the infection during the fifth wave by mid-March (“Modelling the fifth wave”, 2022), and public health containment and social-distancing measures were further tightened in response to the surge of COVID cases (Burki, 2022). We adopted snowballing sampling technique for data collection, with an online anonymous self-rated questionnaire being administered on a Qualtrics survey platform (https://www.qualtrics.com). Virtual snowballing sampling is a commonly-used recruitment strategy during COVID-19 pandemic (e.g., García-Fernández et al., 2022; Roy et al., 2020; Wang et al., 2020), which enables researchers to obtain a large sample within a short period of time and to minimize the interference of stringent control measures on data collection. The survey was disseminated through social media platforms (e.g., Facebook, Instagram, Twitter, WhatsApp), universities (via emails), and the Hong Kong Public Opinion Research Institute (HKPORI) which sent email invitations with survey link to the members of its probability- and non-probability- based online panels of adult HK residents. HKPORI is a well-established survey agency which has executed numerous independent public surveys for academic institutions and government departments in HK (HKPORI, 2022). Respondents were encouraged to forward the survey link to their social networks for study participation. Survey participation was on a voluntary basis and informed consent was obtained before questionnaire assessment. The survey took around 20 min to complete. The study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW). Individuals who aged ≥18 years and resided in HK during the study period were eligible for survey participation. The survey received 20,971 responses. Respondents who did not provide consent or failed to complete the questionnaire items on the core measures of the current study (i.e., depression, COVID-19 perseverative cognition, resilience, loneliness and coping strategies) were excluded. A total of 14,269 respondents constituted the final sample for the current analysis.
2.2. Study assessment
The survey questionnaire comprised four sections including socio-demographic characteristics, psychological distress and symptom profiles, coping strategies and resilience/loneliness, and COVID-19 related factors. In the current analysis, we focused on and reported basic socio-demographic variables including age, gender, educational level and household income, and the following core measures:
2.2.1. Depressive symptoms
Depressive symptoms were assessed using the Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) on a 4-point Likert scale (0 [never] to 3 [nearly every day]). A higher score indicates a greater symptom severity. The Chinese version of PHQ-9 demonstrated satisfactory psychometric properties (Yu et al., 2012), and Cronbach's α coefficient of the scale was 0.899 in our study, indicating good internal consistency.
2.2.2. COVID-19 perseverative cognition
Persistent maladaptive thinking patterns associated with COVID-19 (or termed COVID-19 perseverative cognition henceforth) were measured by the Obsession with COVID-19 Scale (OCS; Lee, 2020). This 4-item scale was specifically developed for measuring the frequency of persistent and disturbing thinking about COVID-19, within a 2-week time-frame on a 5-point Likert scale (0 [not at all] to 4 [nearly every day]). The OCS has been translated in different language versions and has consistently demonstrated a unidimensional construct with solid reliability and validity (e.g., Andrade et al., 2022; Ashraf et al., 2022; Caycho-Rodríguez et al., 2022; Choi et al., 2022; Chen et al., 2021), and was positively associated with psychological distress and functional impairment. A validated Chinese version of OCS (Chen et al., 2021; Lee, 2020) was employed in this study and yielded Cronbach's α coefficient of 0.790, indicating satisfactory internal consistency.
2.2.3. Resilience
Resilience was measured using the 6-item Brief Resilience Scale (BRS; Smith et al., 2008) on a 5-point Likert scale (1 [strongly disagree] to 5 [strongly agree]), with a higher score indicating greater resilience. The Chinese version of BRS (Hsin, 2020) demonstrated good validity and Cronbach's α coefficient of the scale was 0.869 in this study.
2.2.4. Loneliness
A UCLA 3-item Loneliness Scale (Hughes et al., 2004) was applied to measure loneliness on a 3-point Likert scale (1 [hardly ever] to 3 [often]), with a higher score indicating greater loneliness. The Chinese version of the scale (Liu et al., 2020) has satisfactory psychometric properties and yielded Cronbach's α coefficient of 0.833 in our study.
2.2.5. Coping strategies
Participants' coping strategies were assessed by an adapted Chinese version of the Coping Orientation to Problems Experienced Inventory–Brief (Brief-COPE; Carver, 1997; Ye, 2008) on a 4-point Likert scale (0 [never] to 3 [always]). The 14 items of the adapted Brief-COPE were grouped into 3 copying styles based on a previous factor-analytic study (Dias et al., 2012), namely emotion-focused, problem-focused and avoidant coping for subsequent analysis. A higher item sum score indicates higher level of engagement in that particular coping style. In this study, Cronbach's α coefficient of the scale was 0.798.
2.3. Statistical analysis
We first performed correlation analyses to examine the associations among the core study variables of depression, COVID-19 perseverative cognition, resilience, loneliness, and three types of coping styles. Relationships of depression severity with demographic characteristics of age, gender, educational level and household income were assessed using an independent-sample t-test or analysis of variance as appropriate. Demographic variables that were significantly related to depression were then included in regression analyses as covariates. To test the moderating effect of (i) resilience, (ii) loneliness, and (iii) coping strategies on the association between COVID-19 perseverative cognition and depression, three sets of hierarchical regression analyses were conducted. For each set of regression analyses, demographic covariates, OCS score and a moderator(s) (i.e., resilience, loneliness or three types of coping strategies) were added in the first step of the regression model to estimate the amount of variance of depression (as a dependent variable) that could be accounted for by these variables. Then, an interaction term for the moderator and OCS score was entered in the next step of the regression model (note: for coping strategies, a total of three interaction terms were added in the model). Simple slope analyses were conducted for significant interaction terms to examine the strength of the association between COVID-19 perseverative cognition and depression at high (1 SD above the mean) and low (1 SD below the mean) levels of the moderator. To avoid multicollinearity, all of the core study variables were centred before the analysis, and the interaction terms were generated using the centred variables. Statistical analysis was performed on R (version 4.1.2), and statistical significance was set at p < 0.05.
3. Results
3.1. Sample characteristics and correlations between study variables
Of the 14,269 participants, 30.2 %, 36.6 % and 33.2 % aged 18–39 years, 40–59 years and ≥60 years, respectively. A total of 7540 (52.8 %) were women, and 64.5 % (n = 5063) of the study sample attained tertiary educational level or above (Table 2). The average PHQ-9 score of the total sample was 6.58 (SD = 5.96), and 24.6 % (n = 3510) met the clinical cut-off of PHQ-9 score ≥10, indicating having probable depression. As shown in Table 1 , all of the core study variables, namely depressive symptoms, COVID-19 perseverative cognition, resilience, loneliness and three coping strategies, were significantly correlated with each other. Concerning the relationships between depression and demographics, younger age group (18–39 years), female gender, attainment of secondary educational level or below, and lower monthly household income were significantly associated with more severe depression (Table 2 ).
Table 2.
Differences in depressive symptom severity stratified by demographic characteristics.
| N | Depressiona |
P | Partial ƞ2 | 95 % CI for Mean |
||
|---|---|---|---|---|---|---|
| Mean (SD) | Lower limit | Upper limit | ||||
| Age | <0.001 | 0.083 | ||||
| 18–39 years | 4307 | 8.82 (6.42) | 8.63 | 9.00 | ||
| 40–59 years | 5227 | 6.62 (5.72) | 6.47 | 6.78 | ||
| 60 years or above | 4735 | 4.51 (4.94) | 4.37 | 4.65 | ||
| Gender | <0.001 | 0.005 | ||||
| Male | 6729 | 6.09 (5.91) | 5.94 | 6.23 | ||
| Female | 7540 | 6.94 (5.92) | 6.80 | 7.07 | ||
| Educational levels | <0.001 | 0.007 | ||||
| Secondary level or below | 9206 | 6.96 (6.15) | 6.83 | 7.08 | ||
| Tertiary level or above | 5063 | 5.89 (5.51) | 5.75 | 6.04 | ||
| Monthly household incomeb | <0.001 | 0.007 | ||||
| HDK25,000 or below | 6550 | 7.11 (6.26) | 6.96 | 7.26 | ||
| Above HKD25,000c | 7719 | 6.13 (5.65) | 6.01 | 6.26 | ||
CI: confidence intervals; HKD: Hong Kong dollars.
Depressive symptom severity was measured by Patient Health Questionnaire (PHQ-9).
As of 29 Jan, 2023, 1 HKD = 0.13 USD.
The median of monthly household income is HKD27,100 according to the Hong Kong Census and Statistics Department April–June 2022.
Table 1.
Correlations between study variables.a
| Variables | Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|
| (1) Depressive symptoms | 6.58 (5.96)⁎, ⁎⁎ | – | |||||
| (2) COVID-19 perseverative cognition | 4.17 (3.57) | 0.42⁎⁎⁎ | – | ||||
| (3) Resilience | 3.29 (0.76) | −0.55⁎⁎⁎ | −0.37⁎⁎⁎ | – | |||
| (4) Loneliness | 4.47 (1.71) | 0.53⁎⁎⁎ | 0.30⁎⁎⁎ | −0.46⁎⁎⁎ | – | ||
| (5) Emotion-focused coping | 10.22 (2.98) | 0.09⁎⁎⁎ | 0.08⁎⁎⁎ | 0.06⁎⁎⁎ | 0.13⁎⁎⁎ | – | |
| (6) Problem-focused coping | 6.37 (2.08) | 0.18⁎⁎⁎ | 0.13⁎⁎⁎ | −0.06⁎⁎⁎ | 0.16⁎⁎⁎ | 0.70⁎⁎⁎ | – |
| (7) Avoidant coping | 10.43 (2.80) | 0.52⁎⁎⁎ | 0.38⁎⁎⁎ | −0.40⁎⁎⁎ | 0.44⁎⁎⁎ | 0.45⁎⁎⁎ | 0.53⁎⁎⁎ |
COVID: coronavirus; SD: standard deviation.
Spearman-ranked correlation analyses were performed.
P < 0.05.
P < 0.01.
P < 0.001.
3.2. Moderating effect of resilience, loneliness and coping strategies on the association between COVID-19 perseverative cognition and depression
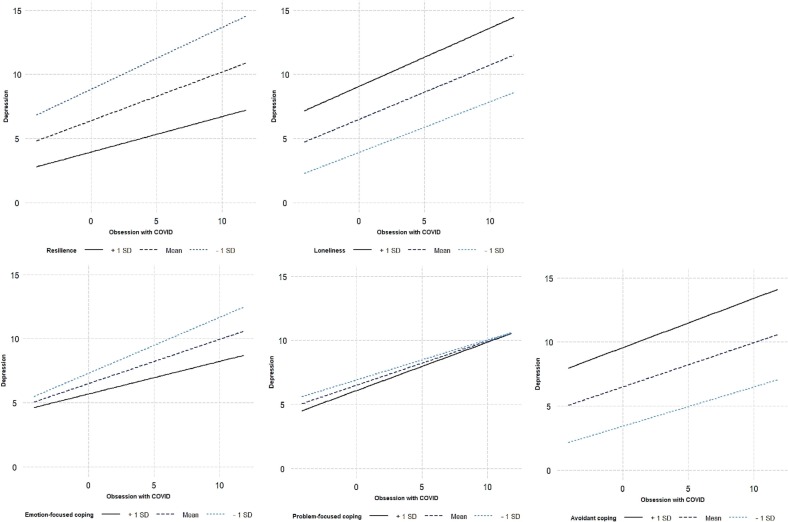
As shown in Table 3 , COVID-19 perseverative cognition was positively associated with depression in all regression models. The interaction terms of COVID-19 perseverative cognition with resilience, loneliness, and the three coping strategies were all found to be significant. The moderating effect was further examined by simple slope regression analyses, which showed that the association between COVID-19 perseverative cognition and depression was significant at both high and low levels of resilience, loneliness, emotion-focused coping, problem-focused coping and avoidant coping (Table 4 ). Specifically, the association between COVID-19 perseverative cognition and depression was stronger at low level than at high level of resilience (Low: b simple = 0.482; High: b simple = 0.276) and emotion-focused coping (Low: b simple = 0.435; High: b simple = 0.254). Conversely, the relationship between COVID-19 perseverative cognition and depression was stronger at high level than at low level of loneliness (High: b simple = 0.455; Low: b simple = 0.393), problem-focused coping (High: b simple = 0.380; Low: b simple = 0.312) and avoidant coping (High: b simple = 0.718; Low: b simple = 0.306) (Tale 4). The results of the simple slope analyses are depicted in Fig. 1 .
Table 3.
Multiple regression analyses of moderation effect of resilience, loneliness and coping strategies on relationship between COVID-19 perseverative cognition and depression.
| Moderators | Variablesa | Estimate | SE | t | 95 % CI for estimate |
P | ΔR2 | F | P for ΔF | |
|---|---|---|---|---|---|---|---|---|---|---|
| LL | UL | |||||||||
| Resilience | Step 1: IV | 0.376 | 1412.36 | <0.001 | ||||||
| Age | −1.357 | 0.05 | −26.35 | −1.458 | −1.256 | <0.001 | ||||
| Gender | −0.184 | 0.08 | −2.28 | −0.341 | −0.026 | 0.023 | ||||
| Highest education level | −0.183 | 0.08 | −2.17 | −0.349 | −0.018 | 0.030 | ||||
| Monthly household income | −0.375 | 0.08 | −4.56 | −0.536 | −0.214 | <0.001 | ||||
| OCS score | 0.404 | 0.01 | 33.90 | 0.381 | 0.427 | <0.001 | ||||
| Resilience | −3.224 | 0.06 | −56.53 | 3.336 | −3.112 | <0.001 | ||||
| Step 2: Interaction term | 0.004 | 1232.40 | <0.001 | |||||||
| OCS score × Resilience | −0.136 | 0.01 | −9.78 | −0.163 | −0.108 | <0.001 | ||||
| Loneliness | Step 1: IV | 0.403 | 1580.47 | <0.001 | ||||||
| Age | −1.391 | 0.05 | −27.77 | −1.490 | −1.293 | <0.001 | ||||
| Gender | −0.079 | 0.08 | −1.00 | −0.233 | 0.076 | 0.318 | ||||
| Highest education level | −0.334 | 0.08 | −4.05 | −0.496 | −0.172 | <0.001 | ||||
| Monthly household income | −0.488 | 0.08 | −6.08 | −0.645 | −0.330 | <0.001 | ||||
| OCS score | 0.431 | 0.01 | 37.62 | 0.408 | 0.453 | <0.001 | ||||
| Loneliness | 1.519 | 0.02 | 62.92 | 1.471 | 1.566 | <0.001 | ||||
| Step 2: Interaction term | 0.001 | 1357.00 | 0.002 | |||||||
| OCS score × Loneliness | 0.018 | 0.01 | 3.17 | 0.007 | 0.030 | 0.002 | ||||
| Coping strategies | Step 1: IV | 0.408 | 1205.58 | <0.001 | ||||||
| Age | −1.352 | 0.05 | −26.76 | −1.451 | −1.253 | <0.001 | ||||
| Gender | −0.220 | 0.08 | −2.73 | −0.378 | −0.062 | 0.006 | ||||
| Highest education level | −0.309 | 0.08 | −3.71 | −0.472 | −0.146 | <0.001 | ||||
| Monthly household income | −0.640 | 0.08 | −8.00 | −0.797 | −0.483 | <0.001 | ||||
| OCS score | 0.354 | 0.01 | 30.04 | 0.331 | 0.377 | <0.001 | ||||
| Emotion-focused coping | −0.268 | 0.02 | −14.21 | −0.305 | −0.231 | <0.001 | ||||
| Problem-focused coping | −0.199 | 0.03 | −7.08 | −0.254 | −0.144 | <0.001 | ||||
| Avoidant coping | 1.104 | 0.02 | 63.02 | 1.069 | 1.138 | <0.001 | ||||
| Step 2: Interaction term | 0.002 | 883.30 | <0.001 | |||||||
| OCS score × Emotion-focused coping | −0.030 | 0.01 | −5.90 | −0.041 | −0.020 | <0.001 | ||||
| OCS score × Problem-focused coping | 0.015 | 0.01 | 1.98 | 0.001 | 0.031 | 0.047 | ||||
| OCS score × Avoidant coping | 0.014 | 0.01 | 3.44 | 0.006 | 0.022 | 0.001 | ||||
COVID: coronavirus; IV: independent variables; LL: lower limit; OCS: Obsession with COVID-19 Scale; SE: standard error; UL: upper limit.
Standardized values of OCS score (for COVID-19 perseverative cognition), resilience, loneliness and coping strategies by centring were used in all inferential analyses.
Table 4.
Conditional effect of resilience, loneliness and coping strategies on the relationship between COVID-19 perseverative cognition and depression.a
| Moderators | Conditional effect of moderators | Estimateb | SE | t | 95 % CI for estimate |
P | |
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| Resilience | +1 SD | 0.276 | 0.02 | 15.65 | 0.242 | 0.311 | <0.001 |
| −1 SD | 0.482 | 0.01 | 33.67 | 0.454 | 0.510 | <0.001 | |
| Loneliness | +1 SD | 0.455 | 0.01 | 32.89 | 0.428 | 0.482 | <0.001 |
| −1 SD | 0.393 | 0.02 | 23.71 | 0.360 | 0.425 | <0.001 | |
| Emotion-focused coping | +1 SD | 0.254 | 0.02 | 12.72 | 0.215 | 0.293 | <0.001 |
| −1 SD | 0.435 | 0.02 | 22.89 | 0.398 | 0.473 | <0.001 | |
| Problem-focused coping | +1 SD | 0.380 | 0.02 | 18.79 | 0.340 | 0.420 | <0.001 |
| −1 SD | 0.312 | 0.02 | 15.58 | 0.273 | 0.351 | <0.001 | |
| Avoidant coping | +1 SD | 0.718 | 0.02 | 46.38 | 0.687 | 0.748 | <0.001 |
| −1 SD | 0.306 | 0.02 | 16.99 | 0.271 | 0.341 | <0.001 | |
COVID: coronavirus; IV: independent variables; LL: lower limit; OCS: Obsession with COVID-19 Scale; SE: standard error; UL: upper limit.
Standardized values of OCS score (for COVID-19 perseverative cognition), resilience, loneliness and coping strategies by centring were used in all inferential analyses.
Beta (bsimple) indicated the strength of the moderation effect.
Fig. 1.
Simple slope analysis of the moderating effect of resilience, loneliness and coping strategies on the relationship between COVID-19 perseverative cognition (as measured by Obsession with COVID-19 Scale, OCS) and depression.
COVID: coronavirus; SD: standard deviation.
4. Discussion
The current study aimed to examine, first, the association between COVID-19 perseverative cognition and depressive symptoms, and second, the moderating effect of resilience, loneliness, and coping strategies on this association among community-dwelling adults during the peak of fifth COVID-19 wave in HK. To our knowledge, this is the first study to systematically evaluate resilience, loneliness, and coping strategies in the moderation analyses of the relationship between COVID-19 perseverative cognition and depression. Previous research primarily assessed one of these three variables on its association with pandemic-related stress and depression (or other mental health outcomes). In line with our first hypothesis and the results of a prior study (O'Connor et al., 2022), we observed that COVID-19 perseverative cognition was positively associated with depressive symptom severity. Repetitive COVID-19 waves are continual and ongoing stressful encounters, which create discrepancies between individuals' current and desired states. This may lead to rumination about how to reduce such discrepancies (Carver and Scheier, 1981). Yet, discrepancy between prolonged pandemic situation and the desired state (i.e., complete control of COVID-19 situation) is unlikely to be readily resolved, resulting in the development of depression (Michl et al., 2013) and other internalizing psychopathology (Aldao et al., 2010). Alternatively, individuals who experience COVID-19 perseverative cognition may also have higher propensity to engage in perseverative thoughts about other stressors and daily hassles. As substantial evidence has demonstrated a strong link between perseverative cognition in general and depression (Michl et al., 2013), further investigation is required to disentangle potential independent effect of COVID-19 specific and general (non-pandemic-related) perseverative thoughts on depression severity.
Our moderation analyses revealed that higher level of resilience ameliorated the association between depression and COVID-19 perseverative cognition, while higher level of loneliness magnified such association. Our findings are thus generally in keeping with earlier pandemic studies which demonstrated the moderating role of resilience (Chan et al., 2021; Havnen et al., 2020) and loneliness (Hou et al., 2021; Mäkiniemi et al., 2021; Probst et al., 2020) in developing depression. Under the socioecological conceptual framework (Bronfenbrenner and Evans, 2000), resilience and social support empower individuals with personal strength in the presence of external resources during COVID-19. Recent data noticed that a significant proportion of individuals experienced high degree of loneliness during the pandemic (Tso and Park, 2020). Our results highlight the critical role of enhancing resilience (e.g., practicing self-care and cultivating community) and social support (i.e., reduced sense of loneliness) to alleviate the adverse pandemic-related impact on mental health status in the general public (Ke et al., 2022; Rosenberg, 2020).
We observed that greater engagement in emotion-focused coping buffered the effect of COVID-19 perseverative cognition on depression. Our result echoes with the literature indicating emotion-focused coping as a moderator in the relationship between heightened stress and negative mental health outcomes (Austenfeld and Stanton, 2004; Cheng et al., 2022; Lin et al., 2010). This is also consistent with recent studies which found that positive reappraisal, a key component of emotion-focused coping, represented a protective factor against development of psychological distress during COVID-19 (Ke et al., 2022; Riepenhausen et al., 2022). It is recognized that adoption of effective emotion-focused coping enables individuals to re-evaluate the circumstances, activate the resources, and may even discover positive values in an otherwise challenging situation (Austenfeld and Stanton, 2004). Conversely, greater use of avoidant coping strategies was found to amplify the impact of COVID-19 perseverative cognition on depression. In fact, past studies demonstrated that avoidant coping exacerbated the influence of perceived stress on psychological distress (e.g., Blalock and Joiner, 2000). It is posited that avoidant coping, including behavioral and mental disengagement from stressors, precludes habituation and engagement of useful coping resources to take place, thereby contributing to emergence of depression (Langlois, 2013).
Of note, we found that greater engagement in problem-focused coping accentuated rather than attenuated the effect of COVID-19 perseverative cognition on depressive symptom severity. This is contrary to our hypothesis and findings of several past studies which suggested that problem-focused coping had a buffering effect on the impact of stress on depression during the pandemic (Ciuhan et al., 2022; Tang et al., 2022). However, our analysis revealed that problem-focused coping was only marginally significant (p = 0.047) in moderating the association between COVID-19 perseverative cognition and depression. Simple slope analyses also showed that high and low levels of engagement of problem-focused coping in fact exerted similar magnitude of effect on the relationship between COVID-19 perseverative cognition and depression (albeit slightly greater in the former than in the latter; High: bsimple = 0.380; Low: bsimple = 0.312). Our results on the moderating role of problem-focused coping should therefore be treated with caution. Alternatively, more prolonged and stricter public health and social policies have been adopted in HK compared to most other regions of the world during the pandemic to contain COVID-19 in the territory. The fifth COVID-19 wave has triggered further tightening of control measures in this highly densely-populated city (Burki, 2022). Given the unpredictable nature of COVID-19 and the accompanied sense of uncontrollability, positive effect of individuals' problem-focused coping would be significantly compromised (Lazarus and Folkman, 1984a) and are very likely insufficient to provide an appropriate solution to the pandemic-related health and social ramifications. This may thus result in poor adjustment and increased psychological distress among those who have actively pursued problem-solving strategies in such a low-control stress situation (Terry and Hynes, 1998). In contrast, more extensive use of emotion-focused coping (e.g., encouraging to express the worry, enhance emotional awareness, regulation and making sense of emotional experience) (Greenberg, 2004), in a low-control stress situation is associated with better adjustment (Lazarus and Folkman, 1984b) and reduces the likelihood of developing depression. Notwithstanding, owing to the paucity of existing data, more research is warranted to identify effective coping strategies to reduce the adverse psychological impact associated with prolonged pandemic.
The study findings have several important implications in public health perspective and psychiatric service delivery to address the adverse impact of pandemic on mental health. Our results underscore the importance of promoting individuals' resilience, enhancing social support and encouraging adoption of emotion-focused coping strategies to effectively mitigate the negative influence of COVID-19 perseverative cognition on depression severity. For instance, interventions including guided self-help, psychological treatments such as brief cognitive-behavioral therapy or mindfulness practice, virtual peer-support group and engagement with community-based support programs (Cuijpers et al., 2010; Suresh et al., 2021; Tran et al., 2020) could help foster resilience and reduce levels of loneliness. Moreover, increased utilization of telemedicine for mental health evaluation and treatment could minimize barriers of restricted access to adequate psychiatric care amidst the peak of pandemic due to tightening of social-distancing measures (Wind et al., 2020).
The main strengths of the study include a large sample size and evaluation of a comprehensive set of relevant moderators, i.e., loneliness, resilience and coping strategies, on the association between COVID-19 perseverative cognition and depression. The study has several methodological limitations. First, the cross-sectional survey design precludes us from establishing causal relationship between the study variables. Prospective research is required to clarify how resilience, loneliness and coping strategies interact with COVID-19 perseverative cognition and depression and moderate the relationship between these two symptom variables over time. Second, our study did not include measures assessing trait levels of perseverative cognition (e.g., Perseverative Thinking Questionnaire, PTQ; Ehring et al., 2011). Hence, we were not able to clarify accurately to what extent the reported association between COVID-19 perseverative cognition and depression is independently attributable to pandemic-specific thoughts and the general process of perseverative thinking. Third, the snowballing sampling strategy is non-probabilistic in nature and may compromise the representativeness of the sample and study results. Additionally, the questionnaire was distributed and administered online, people with limited access to smartphone or computers would be excluded from the survey, resulting in some selection bias. Fourth, psychological symptom assessment was based on participants' self-reporting, which may not well align with the corresponding rating instruments administered by mental health professionals.
In conclusion, our results indicated that persistent dysfunctional thinking related to COVID-19 was associated with more severe depression among community-dwelling adults amidst the peak of the fifth wave of pandemic. Resilience, loneliness and different coping styles exhibited varying moderating effects on the association between COVID-19 perseverative cognition and depression. Strategies strengthening personal resilience and social support, as well as adoption of emotion-focused coping may offer buffering effect against COVID-19 related stressors and maladaptive thinking on the development of depression. Further investigation verifying the critical role of these studied moderators in a longitudinal perspective, incorporating other potential moderating variables such as cognitive flexibility and personality traits for more comprehensive analysis, and evaluating the effectiveness of interventions targeting at resilience, loneliness and coping styles would facilitate development of effective strategies to minimize negative mental health outcomes in the face of prolonged and fluctuating pandemic, as well as future public mental health crises (Holmes et al., 2020).
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
Funding
The study was supported by the Hong Kong Research Grants Council (grant number: 10617014). Additional financial support to undertake this research was provided by the State Key Laboratory of Brain & Cognitive Sciences, the University of Hong Kong.
CRediT authorship contribution statement
The authors confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We understand that the Corresponding Author is the sole contact for the Editorial process. He is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
Declaration of competing interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Acknowledgements
We thank the Hong Kong Public Opinion Research Institute to support the study. We are also grateful to the individuals who participated in the study.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Aldao A., Nolen-Hoeksema S., Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Andrade E.F., Pereira L.J., Orlando D.R., Peixoto M.F.D., Lee S.A., Castelo P.M. Validation of the Brazilian Portuguese version of the Obsession with COVID-19 Scale (BP-OCS) using a large university sample in Brazil. Death. Stud. 2022;46:1073–1079. doi: 10.1080/07481187.2021.1879319. [DOI] [PubMed] [Google Scholar]
- Anyan F., Worsley L., Hjemdal O. Anxiety symptoms mediate the relationship between exposure to stressful negative life events and depressive symptoms: a conditional process modelling of the protective effects of resilience. Asian J. Psychiatr. 2017;29:41–48. doi: 10.1016/j.ajp.2017.04.019. [DOI] [PubMed] [Google Scholar]
- Ashraf F., Lee S.A., Elizabeth Crunk A. Factorial validity of the Urdu version of the Obsession with COVID-19 Scale: preliminary investigation using a university sample in Pakistan. Death. Stud. 2022;46:1059–1064. doi: 10.1080/07481187.2020.1779436. [DOI] [PubMed] [Google Scholar]
- Austenfeld J.L., Stanton A.L. Coping through emotional approach: a new look at emotion, coping, and health-related outcomes. J. Pers. 2004;72:1335–1364. doi: 10.1111/j.1467-6494.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- Blalock J.A., Joiner T.E., Jr. Interaction of cognitive avoidance coping and stress in predicting depression/anxiety. Cognit. Ther. Res. 2000;24:47–65. [Google Scholar]
- Bronfenbrenner U., Evans G.W. Developmental science in the 21st Century: emerging questions, theoretical models, research designs and empirical findings. Soc. Dev. 2000;9:115–125. [Google Scholar]
- Brosschot J.F., Gerin W., Thayer J.F. The perseverative cognition hypothesis: a review of worry, prolonged stress-related physiological activation, and health. J. Psychosom. Res. 2006;60:113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021;21 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burki T. Hong Kong’s fifth COVID-19 wave—the worst yet. Lancet Infect. Dis. 2022;22:455–456. doi: 10.1016/S1473-3099(22)00167-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol' too long: consider the brief cope. Int. J. Behav. Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver C.S., Scheier M.F. Springer; New York: 1981. Attention and Self-regulation: A Control-theory Approach to Human Behaviour. [Google Scholar]
- Caycho-Rodríguez T., Vilca L.W., Carbajal-León C., et al. Obsession with Covid-19 in Peruvian police and armed forces: validation of the obsession with Covid-19 Scale in Spanish using SEM and IRT models. Death Stud. 2022;46:2145–2155. doi: 10.1080/07481187.2021.1900453. [DOI] [PubMed] [Google Scholar]
- Chan A.C.Y., Piehler T.F., Ho G.W.K. Resilience and mental health during the COVID-19 pandemic: findings from Minnesota and Hong Kong. J. Affect. Disord. 2021;295:771–780. doi: 10.1016/j.jad.2021.08.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J.H., Tong K.K., Su X., Yu E.W. Yat, Wu A.M.S. Measuring COVID-19 related anxiety and obsession: validation of the Coronavirus Anxiety Scale and the Obsession with COVID-19 Scale in a probability Chinese sample. J. Affect. Disord. 2021;295:1131–1137. doi: 10.1016/j.jad.2021.08.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng W.L.S., Young P.M.C., Luk K.K.H. Moderating role of coping style on the relationship between stress and psychological well-being in Hong Kong nursing students. Int. J. Environ. Res. Public Health. 2022;19:11822. doi: 10.3390/ijerph191811822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung P.H., Chan C.P., Jin D.Y. Lessons learned from the fifth wave of COVID-19 in Hong Kong in early 2022. Emerg. Microbes Infect. 2022;11:1072–1078. doi: 10.1080/22221751.2022.2060137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmitorz A., Neumann R.J., Kollmann B., et al. Longitudinal determination of resilience in humans to identify mechanisms of resilience to modern-life stressors: the longitudinal resilience assessment (LORA) study. Eur. Arch. Psychiatry Clin. Neurosci. 2021;271:1035–1051. doi: 10.1007/s00406-020-01159-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi E., Lee J., Lee S.A. Validation of the Korean version of the obsession with COVID-19 scale and the Coronavirus anxiety scale. Death Stud. 2022;46:608–614. doi: 10.1080/07481187.2020.1833383. [DOI] [PubMed] [Google Scholar]
- Ciuhan G.C., Nicolau R.G., Iliescu D. Perceived stress and wellbeing in Romanian teachers during the COVID-19 pandemic: the intervening effects of job crafting and problem-focused coping. Psychol. Sch. 2022;59:1844–1855. doi: 10.1002/pits.22728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coolidge F.L., Segal D.L., Hook J.N., Stewart S. Personality disorders and coping among anxious older adults. J. Anxiety Disord. 2000;14:157–172. doi: 10.1016/s0887-6185(99)00046-8. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Donker T., van Straten A., Li J., Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol. Med. 2010;40:1943–1957. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- da Silva-Sauer L., Lima T.R.G., da Fonsêca É.K.G., de la Torre-Luque A., Yu X., Fernández-Calvo B. Psychological resilience moderates the effect of perceived stress on late-life depression in community-dwelling older adults. Trends Psychol. 2021;29:670–683. [Google Scholar]
- Dias C., Cruz J.F., Fonseca A.M. The relationship between multidimensional competitive anxiety, cognitive threat appraisal, and coping strategies: a multi-sport study. Int. J. Sport Exerc. Psychol. 2012;10:52–65. [Google Scholar]
- Ehring T., Zetsche U., Weidacker K., Wahl K., Schönfeld S., Ehlers A. The Perseverative Thinking Questionnaire (PTQ): validation of a content-independent measure. J. Behav. Ther. Exp. Psychiatry. 2011;42:225–232. doi: 10.1016/j.jbtep.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Fernández L., Romero-Ferreiro V., López-Roldán P.D., et al. Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol. Med. 2022;52:195–197. doi: 10.1017/S0033291720002019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg L.S. Emotion-focused therapy. Clin. Psychol. Psychother. 2004;11:3–16. doi: 10.1002/cpp.624. [DOI] [PubMed] [Google Scholar]
- Grey I., Arora T., Thomas J., Saneh A., Tomhe P., Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havnen A., Anyan F., Hjemdal O., Solem S., Riksfjord M.G., Hagen K. Resilience moderates negative outcome from stress during the COVID-19 pandemic: a moderated mediation approach. Int. J. Environ. Res. Public Health. 2020;17:6461. doi: 10.3390/ijerph17186461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong Kong Public Opinion Research Institute HKPOP Panel 2022. https://www.pori.hk/panel.html?lang=en./
- Hou J., Yu Q., Lan X. COVID-19 infection risk and depressive symptoms among young adults during quarantine: the moderating role of grit and social support. Front. Psychol. 2021;11 doi: 10.3389/fpsyg.2020.577942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsin Y.Z. National Pingtung University; Taiwan: 2020. Reliability and Validity of the Brief Resilience Scale. (Master thesis) [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res. Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibarra-Rovillard M.S., Kuiper N.A. Social support and social negativity findings in depression: perceived responsiveness to basic psychological needs. Clin. Psychol. Rev. 2011;31:342–352. doi: 10.1016/j.cpr.2011.01.005. [DOI] [PubMed] [Google Scholar]
- Ke G.N., Grajfoner D., Wong R.M.M., Carter S., Khairudin R., Lau W.Y., Kamal K.A., Lee S.C. Building the positive emotion-resilience-coping efficacy model for COVID-19 pandemic. Front. Psychol. 2022;13 doi: 10.3389/fpsyg.2022.764811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9 validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langlois J.C. Alliant International University; San Diego, California: 2013. The Influence of Avoidance Coping and Stressors on Depression Risk. (Doctoral Thesis) [Google Scholar]
- Lazarus R.S., Folkman S. Springer; New York: 1984. Appraisal, Coping, and Adaptational Outcomes. [Google Scholar]
- Lazarus R.S., Folkman S. Springer; New York: 1984. The Concept of Coping. [Google Scholar]
- Lee S.A. How much “thinking” about COVID-19 is clinically dysfunctional? Brain Behav. Immun. 2020;87:97–98. doi: 10.1016/j.bbi.2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P. Covid-19 in data: 7 charts showing Hong Kong's deadly Omicron outbreak. 2022. https://hongkongfp.com/2022/03/12/covid-19-in-data-6-charts-showing-hong-kongs-deadly-omicron-outbreak/
- Lin H.S., Probst J.C., Hsu Y.C. Depression among female psychiatric nurses in southern Taiwan: main and moderating effects of job stress, coping behaviour and social support. J. Clin. Nurs. 2010;19:2342–2354. doi: 10.1111/j.1365-2702.2010.03216.x. [DOI] [PubMed] [Google Scholar]
- Litman J.A. The COPE inventory: dimensionality and relationships with approach- and avoidance-motives and positive and negative traits. Pers. Individ. Differ. 2006;41:273–284. [Google Scholar]
- Liu T., Lu S., Leung D.K.Y., et al. Adapting the UCLA 3-item loneliness scale for community-based depressive symptoms screening interview among older Chinese: a cross-sectional study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-041921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar S.S. Developmental Psychopathology. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 2015. Resilience in development: a synthesis of research across five decades; pp. 739–795. [Google Scholar]
- Mäkiniemi J.P., Oksanen A., Mäkikangas A. Loneliness and well-being during the Covid-19 pandemic: the moderating roles of personal, social and organizational resources on perceived stress and exhaustion among Finnish university employees. Int. J. Environ. Res. Public Health. 2021;18:7146. doi: 10.3390/ijerph18137146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michl L.C., McLaughlin K.A., Shepherd K., Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: longitudinal evidence in early adolescents and adults. J. Abnorm. Psychol. 2013;122:339–352. doi: 10.1037/a0031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modelling the fifth wave of COVID-19 in Hong Kong 2022. https://www.med.hku.hk/en/news/press/20220210-modelling-the-omicron-fifth-wave/ [DOI] [PMC free article] [PubMed]
- Morrow J., Nolen-Hoeksema S. Effects of responses to depression on the remediation of depressive affect. J. Pers. Soc. Psychol. 1990;58:519–527. doi: 10.1037//0022-3514.58.3.519. [DOI] [PubMed] [Google Scholar]
- O'Connor D., Wilding S., Ferguson E., et al. Effects of COVID-19-related worry and rumination on mental health and loneliness during the pandemic: longitudinal analyses of adults in the UK COVID-19 mental health & wellbeing study. J. Ment. Health. 2022 doi: 10.1080/09638237.2022.2069716. (Online ahead of print) [DOI] [PubMed] [Google Scholar]
- Probst T., Budimir S., Pieh C. Depression in and after COVID-19 lockdown in Austria and the role of stress and loneliness in lockdown: a longitudinal study. J. Affect. Disord. 2020;277:962–963. doi: 10.1016/j.jad.2020.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid C., Beckstead J., Salinas-Miranda A. COVID-19 stress, social support, and coping in international students during the COVID-19 pandemic: a moderated analysis on anxiety and depression. J. Am. Coll. Heal. 2022 doi: 10.1080/07448481.2022.2089044. (Online ahead of print) [DOI] [PubMed] [Google Scholar]
- Riepenhausen A., Veer I.M., Wackerhagen C., et al. Coping with COVID: risk and resilience factors for mental health in a German representative panel study. Psychol. Med. 2022 doi: 10.1017/S0033291722000563. (Online ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg A.R. Cultivating deliberate resilience during the coronavirus disease 2019 pandemic. JAMA Pediatr. 2020;174:817–818. doi: 10.1001/jamapediatrics.2020.1436. [DOI] [PubMed] [Google Scholar]
- Roy D., Tripathy S., Kar S.K., Sharma N., Verma S.K., Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. Int. J. Behav. Med. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Suresh R., Alam A., Karkossa Z. Using peer support to strengthen mental health during the COVID-19 pandemic: a review. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.714181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y.L., Benfante A., Graupner L., et al. Emergency stress, hardiness, coping strategies and burnout in health care and emergency response workers during the COVID-19. Pandemic Front. Psychol. 2022;13 doi: 10.3389/fpsyg.2022.918788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry D.J., Hynes G.J. Adjustment to a low-control situation: reexamining the role of coping responses. J. Pers. Soc. Psychol. 1998;74:1078–1092. [Google Scholar]
- Thoits P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011;52:145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Tran B.X., Hoang M.T., Vo L.H., Le H.T., Nguyen T.H., Vu G.T., Latkin C.A., Ho C.S.H., Ho R.C.M. Telemedicine in the COVID-19 pandemic: motivations for integrated, interconnected, and community-based health delivery in resource-scarce settings? Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.564452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tso I.F., Park S. Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: a case study of Hong Kong. Psychiatry Res. 2020;293:113423. doi: 10.1016/j.psychres.2020.113423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Zhang Y., Ding W., et al. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur. Psychiatry. 2020;63 doi: 10.1192/j.eurpsy.2020.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D.K., Liu X.H., Xiao J.H., et al. Hope during the COVID-19 epidemic decreased anxiety and depression symptoms mediated by perceived stress: coping style differences among patients with COVID-19. Curr. Med. Sci. 2022;42:885–894. doi: 10.1007/s11596-022-2624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins E.R., Roberts H. Reflecting on rumination: consequences, causes, mechanisms and treatment of rumination. Behav. Res. Ther. 2020;127 doi: 10.1016/j.brat.2020.103573. (103573–28) [DOI] [PubMed] [Google Scholar]
- Wind T.R., Rijkeboer M., Andersson G., Riper H. The COVID-19 pandemic: the 'black swan' for mental health care and a turning point for e-health. Internet Interv. 2020;20 doi: 10.1016/j.invent.2020.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye S. University of Hong Kong; Pokfulam Road, Hong Kong SAR: 2008. A Longitudinal Study of Subjective Well-being Among Chinese University Students: The Roles of Personality, Attribution, and Coping. (Doctoral Thesis) [Google Scholar]
- Yu X., Tam W.W.S., Wong P.T.K., Lam T.H., Stewart S.M. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr. Psychiatry. 2012;53:95–102. doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.