Abstract
A new technique for performing gonioscopy that facilitates finding Schwalbe´s line, and lowers the amount of time and light that enters through the pupil is presented. The technique is an alternative to the classic corneal wedge technique and is feasible in the horizontal quadrants without further adjustments to the slit lamp, in contrast to the tilting usually needed for these quadrants. Clinical photos and online videos are presented.
How to cite this article
Albis-Donado O, Ortiz-Arismendi GE, Bhartiya S. New Gonioscopy Technique for Finding Schwalbe's Line: The Ortiz Maneuver. J Curr Glaucoma Pract 2023;17(1):37-39.
Keywords: Angle measurement, Glaucoma, Gonioscopy, New technique
Assessment of the anterior chamber angle is an integral part of the glaucoma work-up, and gonioscopy, despite being a qualitative and subjective assessment that is prone to inter-examiner variability, remains the gold standard. Newer anterior segment imaging techniques include ultrasound biomicroscopy, anterior segment optical coherence tomography, Scheimpflug photography, and scanning peripheral anterior chamber depth analyzer. All of these imaging modalities provide a wealth of information about the anterior chamber angle, as also a quantitative assessment of the angle structures. All of these also have their inherent drawbacks, and none of these techniques has gained acceptance as a substitute for gonioscopy since, despite their advances, they mostly remain as improved, objective, and quantifiable Van Herick's.1–6
Gonioscopy remains invaluable for the diagnosis of neovascularization, pseudoexfoliation, pigmentation, angle recession, cyclodialysis clefts, and peripheral anterior synechiae. It is a contact procedure, and despite inherent potential confounding angle distortion by goniolens contact and the use of broad slit or room illumination, it remains invaluable in the management of glaucoma.
Schwalbe's line is the peripheral termination of the cornea, where Descemet's membrane ends, and is the most important landmark for ascertaining angle width. Eyes with closed angles, hazy corneas, and pigmentation anterior to Schwalbe's line may often be mistaken as open angles.4 It is therefore advised that Schwalbe's line must be identified first during a gonioscopic evaluation, followed by identification of the other angle structures.
In eyes with abnormal (both, absent or heavy) pigmentation, Schwalbe's line is often difficult to identify during gonioscopy. In such cases, the corneal wedge, or parallelepiped technique helps in identifying the anterior border of the trabecular meshwork. This technique requires considerable practice, and tilting of the slit lamp to evaluate the nasal and temporal quadrants of the angle, making the evaluation slow, cumbersome, and technically difficult.
The new technique obviates the use of the tilting of the slit lamp and has been found to have a flatter learning curve for residents and fellows alike. This review on the novel ophthalmic technique for identification of Schwalbe's line aims to make gonioscopy easier and faster for the glaucoma practitioner.
Applied Anatomy of the Anterior Chamber Angle
The angle structures from anterior to posterior as identified during gonioscopy are Schwalbe's line, anterior nonpigmented trabecular meshwork, posterior pigmented trabecular meshwork, scleral spur, ciliary body band, and the iris root inserting into the ciliary body.
Telling apart the two portions of the trabecular meshwork is important for correctly performing argon-laser trabeculoplasty, and identifying Schwalbe's line is essential for performing selective trabeculoplasty on the trabecular meshwork, and not on peripheral pigmented endothelium of some eyes with very closed angles.
Understanding angle anatomy is even more important for being able to perform correctly many of the classic and newer glaucoma ab-interno surgical procedures, from goniotomy to I-stent®, Trabectome®, Aquesys®, Xen®, and Hydrus® procedures.
The Classic Corneal Wedge Technique
The width of the slit beam is reduced to a minimum, and the beam is laterally displaced from the path of the oculars by 30–45° for examining the superior and inferior angles, but for examining the nasal and temporal portions the slit beam must be used horizontally and the whole illumination rotation arm must be inclined vertically away from the oculars, so the beam also has about 30° of inferior or superior displacement (Fig. 1).
Figs 1A to C.
(A) Slit-lamp in primary position, the illumination rotation arm is aimed directly at the eye, 0° of rotation of the slit control knob (blue arrow); (B) Slit-lamp in a tilted position, with the slit control knob (blue arrow), rotated 90° so the beam is horizontal, necessary for performing the corneal wedge technique in both nasal and temporal quadrants since it displaces the beam about 30° from the horizontal plane; (C) the picture illustrates the difficulty for a full-tilt during horizontal gonioscopy, since the illumination piece's cables touch the upper part of the head-support frame and the patient, leaving little space for the examiner's hand too
The displaced beam is then projected onto the cornea. Through the gonioscope, a “Y” shaped illuminated band of light is noted (Fig. 2). This consists of two separate corneal reflections, which constitute the two prongs of the “Y,” illuminating the inner and outer aspects of the cornea. The band from the outer surface of the cornea is broader and less sharp, while the sharper reflection comes from the inner corneal surface. The reflection from the inner corneal surface curves along with the corneoscleral interface at the limbus to meet the first line at the point where the cornea ends and the meshwork begins. The stem of the “Y” illuminates the trabecular meshwork, the scleral spur, the ciliary band, and the last fold of the iris as a continuous line in open angles, and as a discontinuous line in progressively occludable angles. The corneal wedge is the space between the two prongs of the “Y,” and their intersection with its stem delineates Schwalbe's line.
Fig. 2.
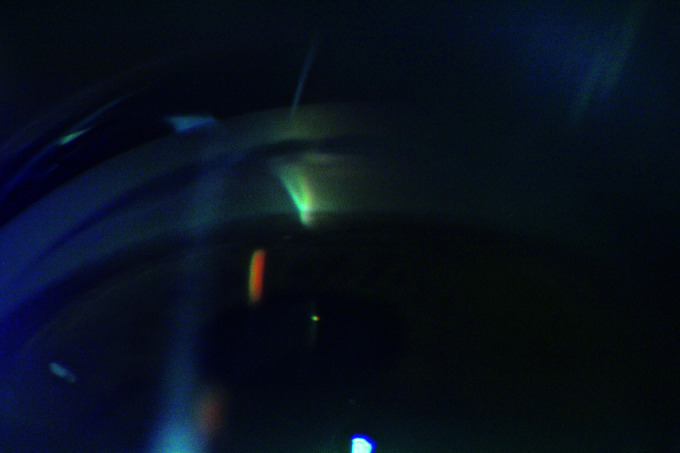
Corneal wedge technique in an open-angle. The inner portion of the beam is brighter and sharper and joins the outer portion of the beam at Schwalbe´s line. Some of the light goes through the pupil in this example and seems to be preventing further mydriasis from narrowing the angle. In this technique, the beam should be shortened in order to avoid this bias
New Technique of Identification of Schwalbe's Line
A newer and simpler technique was developed by Dr. Ortiz-Arismendi, which makes the identification of Schwalbe's line a faster and less tedious procedure. In this method, there is no need to move the illumination rotation arm of the slit lamp. Instead, the slit's inclination is modified to 45° by using the slit controller in Haag-Streit-type lamps, or the drum in Zeiss-type lamps (Figs 3A and B).
Figs 3A and B.
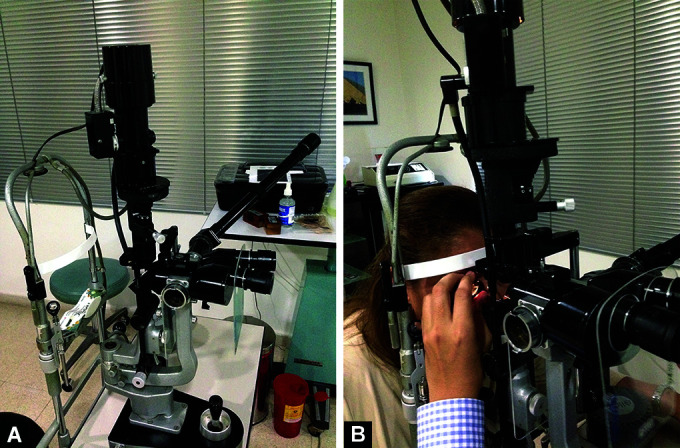
(A) The illumination rotation arm remains in primary position, but the inclination of the slit controller knob is rotated 45° to the left, making the slit take an oblique orientation, like a slash “/.”; (B) The examiner can comfortably fit his hand between the illumination arm and the patient, the primary position will also avoid the cumbersome inclination needed for the classic technique. In this example, the slit controller knob is rotated 45° to the right, and the slit beam is oriented as an inverted slash “\”
While using a 4-mirror goniolens with this oblique beam we will see an inverted V in the superior mirror (inferior quadrant), a V in the inferior mirror, a < in the left mirror (temporal for oculus dexter and nasal for oculus sinister), and a > for the right mirror. When using a Goldman type of lens the same image will be seen when the mirror is rotated into the corresponding position and the tip of the V will always be on the cornea.
One of the lines will be brighter and longer, this is the oblique and direct beam of light that will illuminate all the angle structures, beginning on the iris root, then the ciliary body band, the scleral spur, the trabecular meshwork, Schwalbe's line, and corneal endothelium. The second and softer beam of light will begin at the endothelium and, with a perpendicular orientation to the trabecular meshwork, will stop at Schwalbe's line. Since the two beams are geometrically separated they are more easily differentiated from each other, even when the beams are relatively broad, making photography and video of the angle less dependent on the exposure and sensitivity of the recording imaging device (Figs 4A and B).
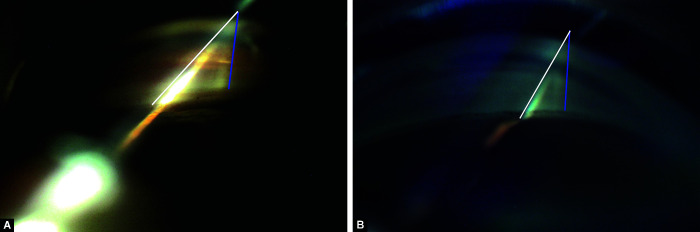
Figs 4A and B.
(A) The Ortiz maneuver in an open-angle. The inverted V has a sharper and brighter inner portion traveling through all angle structures (parallel to the white line) and the external portion (to the right, in blue) is blurrier and ends at Schwalbe´s line; (B) In a narrow-angle, the inner portion (in white) of the slit beam seems to “jump” when it passes from the iris root to the upper portion of the trabecular meshwork and corneal endothelium. The softer external beam ends at Schwalbe´s line (in blue), which is pigmented in this clinical example
The most striking change in gonioscopy is the ease of detecting the correct position of Schwalbe's line in both horizontal meridians, without having to move any other part of the slit lamp. Doing dark-room gonioscopy with this method helps to better see details of the changes in iris position relative to the trabecular meshwork when changing from a broad beam that causes the pupil to shrink, to a very thin and almost inexistent line of light and mydriatic pupil. This technique also has the advantage of permitting the use of a long slit-beam, since the inclination of the beam will prevent most of the light from entering through the pupil.
Conclusion
The new gonioscopic technique facilitates a more thorough angle examination, increasing precision by permitting an easier, faster way of identifying Schwalbe's line, even in the temporal and nasal quadrants, without having to make further adjustments in the slit lamp. The separation of the two components of the light beam allows for the use of broader slits, and therefore better-illuminated photographs and videos, making documentation of angle findings a more repeatable process than with the conventional, time-tested but cumbersome technique.
Video examples of closed and open angles using the Ortiz maneuver are available online at the journal´s website.
Orcid
Oscar Albis-Donado https://orcid.org/0000-0002-8438-4464
Footnotes
Source of support: Nil
Conflict of interest: Dr Shibal Bhartiya is associated as the Executive Editor of this journal and this manuscript was subjected to this journal's standard review procedures, with this peer review handled independently of this Executive Editor and her research group.
References
- 1.Dellaporta A. Historical notes on gonioscopy. Surv Ophthalmol. 1975;20:137–149. doi: 10.1016/0039-6257(75)90021-1. [DOI] [PubMed] [Google Scholar]
- 2.Terry JE. Gonioscopy: evaluation and interpretation. J Am Optom Assoc. 1977;48:1415–1423. 925300 [PubMed] [Google Scholar]
- 3.Prokopich CL, Flanagan JG. Gonioscopy: evaluation of the anterior chamber angle Part II. Ophthalmic Physiol Opt. 1997;17(Suppl 1):S9–S13. doi: 10.1016/s0275-5408(96)00073-7. [DOI] [PubMed] [Google Scholar]
- 4.Thomas R, Thomas S, Chandrashekar G. Gonioscopy. Indian J Ophthalmol. 1998;46(4):255–261. 10218313 [PubMed] [Google Scholar]
- 5.Prata TS, Dorairaj S, De Moraes CG, et al. Indentation slit lamp-adapted optical coherence tomography technique for anterior chamber angle assessment. Arch Ophthalmol. 2010;128:646–647. doi: 10.1001/archophthalmol.2010.51. [DOI] [PubMed] [Google Scholar]
- 6.Park SB, Sung KR, Kang SY, et al. Assessment of narrow angles by gonioscopy, Van Herick method and anterior segment optical coherence tomography. Jpn J Ophthalmol. 2011;55(4):343–350. doi: 10.1007/s10384-011-0036-0. [DOI] [PubMed] [Google Scholar]