ABSTRACT
Garré’s osteomyelitis, first described by Carl Garré in 1893, is a type of chronic osteomyelitis accompanied by hyperplastic periostitis. This condition affects relatively young patients and occurs in the fibula, femur, and other long bones as chronic non-purulent sclerosing osteomyelitis. Further, reactive periosteal bone formation develops due to chronic irritation or infection. In the maxillofacial region, it often occurs in the first molar region of the mandible due to caries and other similar causes, and it is rarely associated with impacted teeth. Herein, we present a 12-year-old female patient who primarily complained of swelling on the right side of the mandible. Despite taking antibiotics prescribed at local otolaryngologist, the swelling did not completely resolve. Thus, the patient was referred to the Department of Otorhinolaryngology at our hospital, where a dental-related disease was suspected. On a computed tomography scan, radiolucent findings were observed around the germ of the impacted wisdom tooth as well as hyperostosis in the lower jaw. Thus, Garré’s osteomyelitis was suspected. The patient received oral anti-inflammatory treatment by the incision prior to surgery. Thereafter, the tooth germ was enucleated and newly-formed bone, which was laterally located to the cortical bone of the mandible, was removed under the effect of general anesthesia. On computed tomography scan 9 months after the surgery, hyperostosis in the angle of the mandible disappeared. Thereafter, pain and swelling did not recur, and the patient was doing well.
Keywords: mandible, osteomyelitis, tooth germ
Garré’s osteomyelitis is a type of chronic osteomyelitis accompanied by hyperplastic periostitis. This condition affects relatively young patients and manifests as chronic non-purulent sclerosing osteomyelitis in the fibula, femur, and other long bones.1 Furthermore, reactive periosteal bone formation develops due to chronic irritation or infection. In the maxillofacial region, it often occurs in the first molar region of the mandible due to caries and other similar causes, and it is rarely associated with impacted teeth. The preferred treatment is extraction of the causal tooth and removal of hyperostotic region caused by periosteal reaction, and the outcome is generally favorable. In this report, we describe the case of pediatric Garré’s osteomyelitis caused by germ infection in the lower impacted wisdom tooth.
PATIENT REPORT
A 12-year-old female patient reported swelling in the right buccal region that had begun 3 weeks before her visit to our department. The patient consulted a local dentist, pediatrician, and otolaryngologist, and she was prescribed with antibiotics. Although the swelling subsided temporarily, it reoccurred after completing the course of antibiotic treatment. Hence, she was referred to the Department of Otorhinolaryngology/Head and Neck Surgery of our hospital. A dental-related disease was suspected, and she was referred to our department for treatment.
The patient’s previous medical or family history was not significant. Extraoral findings upon her initial visit revealed diffuse swelling in the buccal region on the right side (Fig. 1), and severe trismus with only 12 mm of maximum mouth opening. As intraoral findings, light swelling of the buccal gingiva in her lower right molars without fluctuation was noted. No evident caries was observed on the first and second molars on the lower right molars, and the electro-pulp test revealed a neural response of the pulp. The wisdom tooth in the right lower mandible did not erupt. According to the blood test results, the white blood cell count and C-reactive protein level were slightly elevated at 7.0 × 103/μL and 2.16 mg/dL, respectively. The bacterial culture test showed the presence of general oral bacteria. Panoramic radiography did not reveal evident caries that could be a source of infection. Nevertheless, impacted wisdom teeth with immature tooth roots were observed at the both sides of the mandible (Fig. 2). Computed tomography (CT) scan showed periosteal thickening of the right mandibular angle of the mandibular and cortical bone destruction (Figs. 3A and B). Bone scintigraphy was performed to rule out neoplastic lesions (Fig. 4). There was accumulation in the area corresponding to the right mandibular angle. However, there was no abnormal accumulation in the other region. Therefore, the patient was diagnosed with mandibular osteomyelitis caused by the right mandibular impacted wisdom tooth.
Fig. 1.
Clinical images revealed diffuse swelling of the right mandibular angle area.
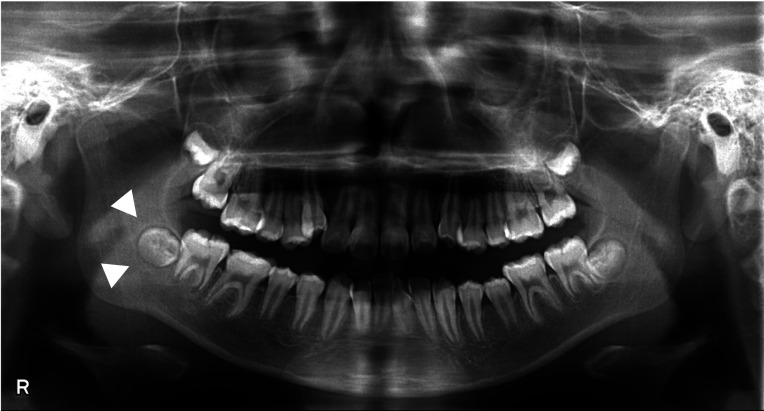
Fig. 2.
Orthopantomograph images. No evident caries, which can cause infection, were observed. Impacted wisdom teeth with immature tooth roots were observed in the lower right areas (arrowheads).
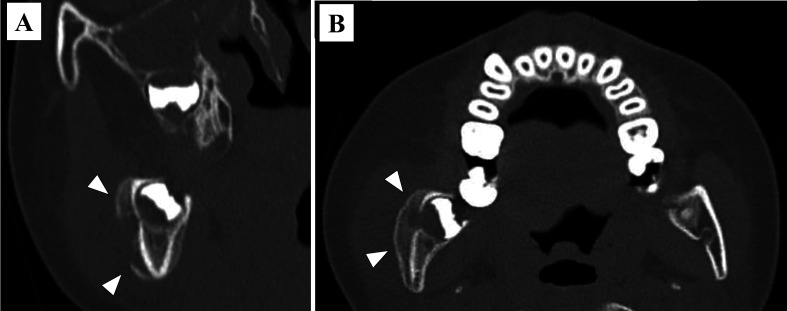
Fig. 3.
(A) Computed tomography coronal-section image. A radiograph revealed the presence of a fistula in the buccal cortical bone of the tooth germ of the third molar (arrowheads), and periosteal hyperostosis was observed on the outside. (B) Computed tomography sagittal plane image. Periosteal thickening of the right angle of the mandible was observed (arrowheads).
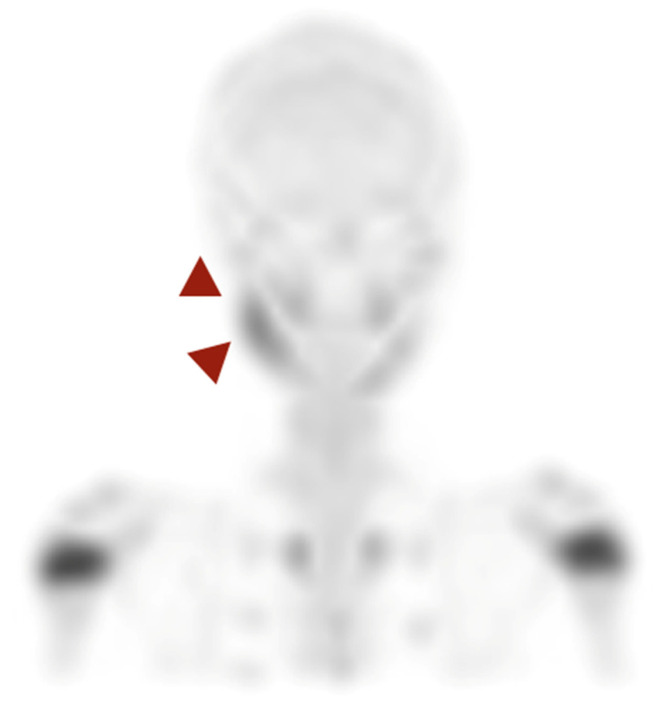
Fig. 4.
Bone scintigraphy. Accumulation was observed in the right mandibular angle equivalent section (arrowheads). Abnormal accumulation was not noted in other parts.
To reduce inflammation, PO AmpC 750 mg/day was administered for 1 week, and the swelling disappeared. Three months after the initial consultation, the patient underwent surgery under general anesthesia for removal of the newly formed bone to the cortical bone, and the dental germ from the wisdom tooth of the mandible was extracted to eliminate the source of infection (Fig. 5). There was no clear pus drainage from the wound, and cortical bone growth was observed. A diagnosis of chronic osteomyelitis was made based on the histopathological examination findings. The periosteal reaction observed preoperatively improved on CT scan 9 months after the surgery (Fig. 6). As bone growth disappeared after removing the source of infection, a final diagnosis of Garré osteomyelitis was made. Thereafter, no swelling was observed, and the patient progressed well.
Fig. 5.
Surgical image. No clear drainage of pus from the wound and cortical bone growth were observed.
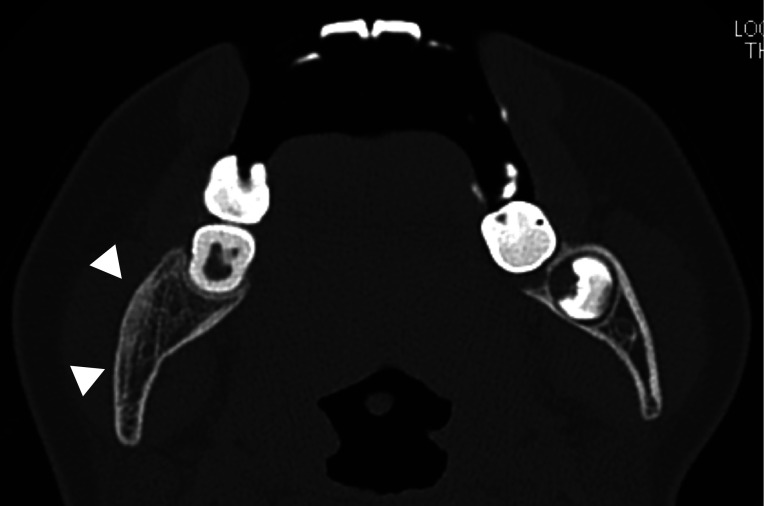
Fig. 6.
Computed tomography cross-section image 9 months after surgery. Periosteal thickening improved (arrowheads).
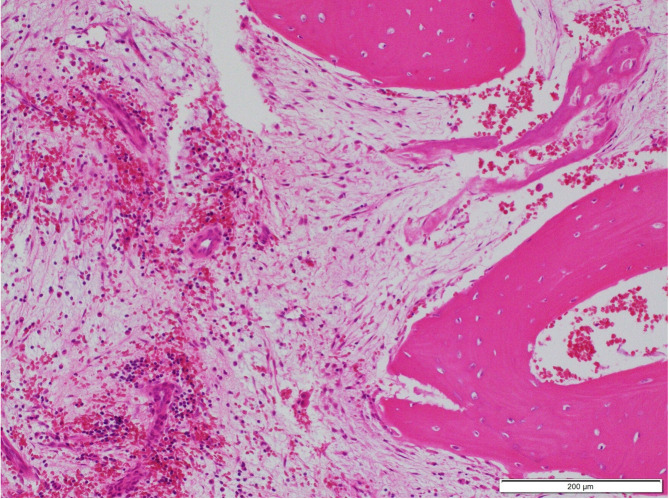
Histopathological findings
Osteocytes were observed in the lacuna, and fibrosis and hemorrhage between the bone trabeculae. Moreover, mild lymphocyte infiltration and chronic osteomyelitis occurred and bony trabeculae of the reactive bone arranged perpendicular to the bone surface. However, there was no jaw osteonecrosis (Fig. 7).
Fig. 7.
Histopathological images. Osteocytes were observed in the lacuna, and fibrosis and hemorrhage between the bone trabeculae. Further, mild lymphocyte infiltration and chronic osteomyelitis occurred and bony trabeculae of the reactive bone arranged perpendicular to the bone surface. However, there was no jaw osteonecrosis. Hematological and eosin staining. Bar = 200 μm.
DISCUSSION
In 1893, Garré reported about osteosclerotic osteomyelitis with specific presentations including non-purulent bone swelling and thickening of the femur, humerus, and other bones in young patients. In that study, osteomyelitis was found in 20 of 559 patients. However, there was no case of mandibular osteomyelitis.1 In 1955, Pell et al. presented a case of oromandibular osteomyelitis, which often occurs due to periapical lesions in the mandibular molar region of juvenile patients. This may be attributed to the significant osteogenic potential of the mandible and its dependence on the periosteum for blood supply and thick cortical bone. As this prevents bone marrow inflammation from spreading to the surrounding area, chronic outcome is more likely to occur.2 Eversole et al. showed that the diagnostic criteria for Garré’s osteomyelitis were facial asymmetry caused by local bone swelling, histopathological findings confirming a benign periosteal fibrous lesion, injury secondary to infection, trauma, or other stimuli, and ability to the bone completely or partially reshape after removing the excess bone.3 Biopsy is not necessary in the diagnosis of Garré’s osteomyelitis, except when the cause of infection is unknown.4, 5 Conventional radiographic or CT imaging is sufficient for diagnosis.5,6,7 In our case, preoperative biopsy was not necessary because bone scintigraphy showed no accumulation except of the right mandible and clear clinical and radiological features of Garré’s osteomyelitis. In the current case, swelling was observed in the lower right angle of the mandible, and chronic osteomyelitis was found on histopathological examination. Hence, the impacted wisdom tooth, which was considered the source of infection, was extracted. As hyperostosis disappeared, a final diagnosis of Garré’s osteomyelitis was made. Nortjé et al. analyzed 81 cases in which a periosteal reaction was observed with jaw osteomyelitis.8 In terms of causal tooth, bone augmentation due to in periosteal reaction occurred in the mandibular first molar (51.2%), mandibular second molar (13.2%), and mandibular second deciduous molar (8.5%). Garré’s osteomyelitis caused by germ infection in the mandibular wisdom teeth is an extremely rare condition.8,9,10,11 In the current case, the second molar on the lower right of the mandible partially erupted and a wisdom tooth was also affected. The reason for this could be that bacteria may have entered through the periodontal pocket of the second molar on the lower right of the mandible, causing an infection of the dental germ of the wisdom tooth. Therefore, in addition to removing the newly formed bone, we extracted the dental germ from the wisdom tooth, which was the causal tooth.
In terms of treatment, after extraction of the causal tooth and removal of the hyperostotic region caused by periosteal reaction, improvement was observed and the patient progressed well.7 However, some reports have shown that bone augmentation decreased with tooth extraction and curettage alone.9 Further, antibiotic administration and bone augmentation/reduction are sometimes conducted without extracting any teeth even if the source of infection is unclear.10 Imaging and biopsy should be performed to rule out differential diagnoses such as cortical hyperplasia, Ewing’s sarcoma, osteosarcoma, and cherubism.10, 12 In the current case, bone scintigraphy was performed to rule out the abovementioned conditions, and this procedure is considered necessary from a diagnostic point of view. Ewing’s sarcoma is similar to Garré’s osteomyelitis in terms of subperiosteal bone formation and appearance in young people. However, Ewing’s sarcoma differs from Garré’s osteomyelitis in that it produces osteophytes with a “sun ray” appearance, causing rapid bone enlargement and increased osteolytic reactions in the bone as well as the occurrence of frequent complications such as facial neuralgia and lip paresthesia.12, 13
Osteosarcoma can also produce a hard bone mass on the bone surface. However, it differs from Garré’s osteomyelitis in that it exhibits characteristic features of malignant tumors, such as new bone formation with a “sun ray” appearance and periosteal reactions in the form of a Codman triangle on radiography.12, 13 Cherubism is a painless, non-neoplastic disease that causes symmetrical and proliferative lesions in the upper and lower jaws.14
Here, we present a case of Garré’s osteomyelitis caused by germ infection in the right lower wisdom tooth, and a good outcome was achieved via tooth extraction, curettage, and bone augmentation removal.
Acknowledgments
Acknowledgments: We thank Dr. Hiroshi Miura of the Division of Pathology, Matsue Red Cross Hospital, for sharing their pathological expertise and helping in the preparation of this manuscript.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Garré C. Ueber besondere formen und folgezustande der akuten infektiosen osteomyelitis. Beitr Klin Dhir. 1893;10:241-98. German. [Google Scholar]
- 2.Pell GJ,Shafer WG,Gregory GT,Ping RS,Spear LB. Garré’s osteomyelitis of the mandible; report of case. J Oral Surg (Chic). 1955;13:248-52. [PubMed] [Google Scholar]
- 3.Eversole LR,Leider AS,Corwin JO,Karian BK. Proliferative periostitis of Garré: its differentiation from other neoperiostoses. J Oral Surg. 1979;37:725-31. [PubMed] [Google Scholar]
- 4.Suma R,Vinay C,Shashikanth MC. SubbaReddy VV. Garre’s sclerosing osteomyelitis. J Indian Soc Pedod Prev Dent. 2007;25:30-5. [PubMed] [Google Scholar]
- 5.Gonçalves M,Oliveira DP,Oya EO,Gonçalves A. Garre’s osteomyelitis associated with a fistula: a case report. J Clin Pediatr Dent. 2002;26:311-3. 10.17796/jcpd.26.3.v65535482m037304 [DOI] [PubMed] [Google Scholar]
- 6.Brazão-Silva M,Pinheiro T. The So-called Garrè’s osteomyelitis of jaws and the pivotal utility of computed tomography scan. Contemp Clin Dent. 2017;8:645-6. 10.4103/ccd.ccd_304_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakano H,Miki T,Aota K,Sumi T,Matsumoto K,Yura Y. Garré’s osteomyelitis of the mandible caused by an infected wisdom tooth. Oral Sci Int. 2008;5:150-4. 10.1016/S1348-8643(08)80021-3 [DOI] [Google Scholar]
- 8.Nortjé CJ,Wood RE,Grotepass F. Periostitis ossificans versus Garrè’s osteomyelitis. Oral Surg Oral Med Oral Pathol. 1988;66:249-60. 10.1016/0030-4220(88)90102-8 [DOI] [PubMed] [Google Scholar]
- 9.Tong ACK,Ng IOL,Yeung KMA. Osteomyelitis with proliferative periostitis: an unusual case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e14-9. 10.1016/j.tripleo.2006.03.025 [DOI] [PubMed] [Google Scholar]
- 10.Liu D,Zhang J,Li T,Li C,Liu X,Zheng J,et al. Chronic osteomyelitis with proliferative periostitis of the mandibular body: report of a case and review of the literature. Ann R Coll Surg Engl. 2019;101:328-32. 10.1308/rcsann.2019.0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park J,Myoung H. Chronic suppurative osteomyelitis with proliferative periostitis related to a fully impacted third molar germ: a report of two cases. J Korean Assoc Oral Maxillofac Surg. 2016;42:215-20. 10.5125/jkaoms.2016.42.4.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akgül HM,Çağlayan F,Günen Yılmaz S,Derindağ G. Garre’s Osteomyelitis of the Mandible Caused by Infected Tooth. Case Rep Dent. 2018;2018:1-4. 10.1155/2018/1409539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jundt G. Cherubism. In Barnes L, Eveson JW, eds; WHO Classification of Tumours, Pathology and Genetics of Head and Neck Tumours. IARC Press, Lyon, 2005, P325.
- 14.Papadaki ME,Lietman SA,Levine MA,Olsen BR,Kaban LB,Reichenberger EJ. Cherubism: best clinical practice. Orphanet J Rare Dis. 2012;7(suppl 1):S6. 10.1186/1750-1172-7-S1-S6 [DOI] [PMC free article] [PubMed] [Google Scholar]