Abstract
This study used a population-based individual patient data set that included diagnoses of COVID-19 to determine whether there was a temporal association between COVID-19 and type 1 diabetes in children.
The incidence of type 1 diabetes in children increased during the COVID-19 pandemic,1,2,3,4 but studies have not discriminated between children with and without infection. We analyzed a large population-based, individual-patient data set that included diagnoses of COVID-19 to determine whether there was a temporal association between COVID-19 and type 1 diabetes in children.
Methods
The Bavarian Association of Statutory Health Insurance Physicians (BASHIP) processes claims data for all statutorily insured patients in Bavaria, Germany (approximately 85% of the total Bavarian population). Anonymized data of all children born between 2010 and 2018 and observed through December 2021 in the BASHIP database were included in this analysis. Diagnoses of medically attended COVID-19 and type 1 diabetes according to International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes were recorded in quarterly (3-month) calendar intervals without information about the exact date of diagnosis. For COVID-19, disease codes indicating whether COVID-19 was virus confirmed (polymerase chain reaction positive) were entered by clinicians.
The incidence rate of type 1 diabetes was compared in 2018-2019 vs 2020-2021. Time-dependent Cox models, adjusted for children’s sex and age, were used to determine risk of type 1 diabetes associated with a COVID-19 diagnosis on a quarterly basis in 2020-2021. A sensitivity analysis was performed excluding COVID-19 diagnoses without virus confirmation. The binomial test was used to compare groups and the Mann-Whitney U test to compare age distributions. Statistical analyses were conducted using R software (version 4.1.2; R Project for Statistical Computing). Statistical significance was determined at the 5% level (2-sided). Data release was approved by the BASHIP according to German guidelines for secondary data analysis.
Results
Of 1 181 878 children with medical claims data, 1242 received a diagnosis of type 1 diabetes through December 2019. Of the remaining 1 180 636 children without prevalent type 1 diabetes at the start of 2020, 195 795 (16.6%; 93 529 girls [47.8%]) had a diagnosis of COVID-19 (57 646 virus confirmed [29.4%]) between January 2020 and December 2021 (Table). The frequency of a first diagnosis of COVID-19 ranged from 0.18% in January to March 2020 to 4.79% in October to December 2021. The frequency was higher in boys (16.8%) than girls (16.4%) (P < .001) and in children younger than the median age of 6.5 years (18.6%) compared with older children (14.6%) (P < .001).
Table. Characteristics of Children Included in a Study of COVID-19 and Type 1 Diabetes.
| 2018-2019 | 2020-2021 | P valuea | ||
|---|---|---|---|---|
| No COVID-19 diagnosis | COVID-19 diagnosis | |||
| Total, No. (%) | 1 181 096 | 984 841 (83.4) | 195 795 (16.6) | |
| Sex, No. (%) | ||||
| Girls | 572 073 (48.4) | 478 295 (48.6) | 93 529 (47.8) | <.001 |
| Boys | 609 023 (51.6) | 506 546 (51.4) | 102 266 (52.2) | |
| Age | ||||
| Median (IQR), yb | 4.5 (2.5-6.8) | 6.8 (4.5-8.8) | 6.0 (4.0-8.5) | <.001 |
| ≤6.5 y, No. (%) | 826 805 (70.0) | 484 426 (49.2) | 110 454 (56.4) | <.001 |
| >6.5 y, No. (%) | 354 791 (30.0) | 500 415 (50.8) | 85 341 (43.6) | |
P values were for comparisons between children with and without a COVID-19 diagnosis.
Age was on January 1, 2019, for the 2018-2019 period and on January 1, 2020, for the 2020-2021 period.
The incidence rate of type 1 diabetes was 29.9 (95% binomial CI, 27.7-32.2; 705 cases) per 100 000 person-years between January 2020 and December 2021 vs 19.5 (95% CI, 17.8-21.4; 460 cases) between January 2018 and December 2019 (P < .001) (Figure). The incidence rate of type 1 diabetes during the pandemic was 28.5 (95% CI, 26.3-30.9; 620 cases) per 100 000 person-years in the absence of a preceding or concurrent COVID-19 diagnosis. In comparison, the incidence rate of type 1 diabetes was 55.2 (95% CI, 37.1-81.5; 27 cases) per 100 000 person-years in the same quarter as the COVID-19 diagnosis (P < .001 vs COVID-19 negative). The incidence rate was 38.8 (95% CI, 25.6-58.1; 25 cases) in the next 2 quarters (P = .16) and 50.7 (95% CI, 34.3-74.4; 28 cases) in later quarters (6-15 months after COVID-19 infection; P = .004). The age- and sex-adjusted hazard ratio for type 1 diabetes development in 2020-2021 was 1.57 (95% CI, 1.32-1.88; P < .001) with any COVID-19 diagnosis and 1.69 (95% CI, 1.31-2.18; P < .001) when only virus-confirmed cases were considered.
Figure. Incidence Rates for Type 1 Diabetes in Children With and Without a COVID-19 Diagnosis.
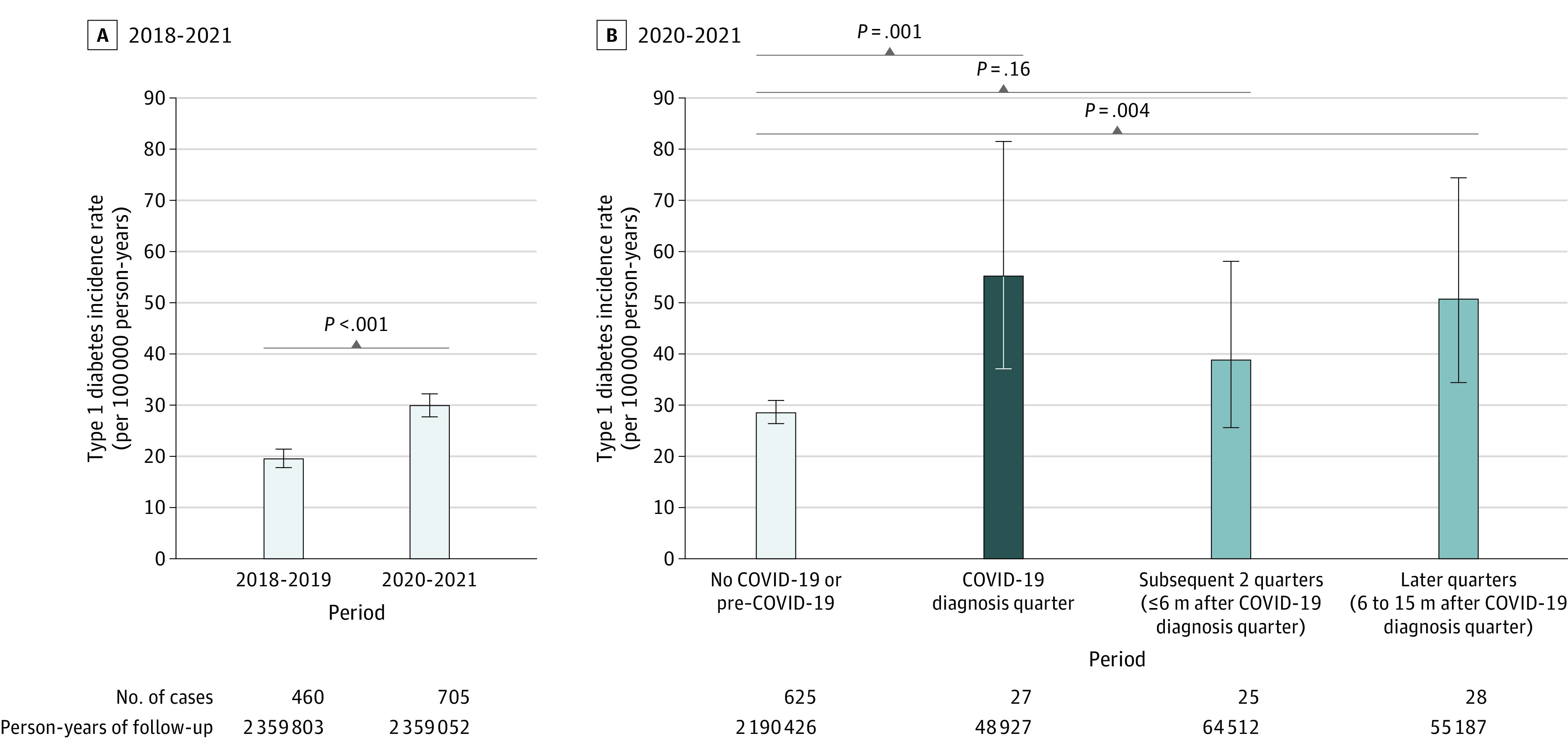
A, Incidence rate of type 1 diabetes before the pandemic (2018-2019) and during the pandemic (2020-2021) for 1 181 096 children with medical insurance claims data. B, For children in the pandemic period, the incidence rate of type 1 diabetes is shown from January 2020 to December 2021 in the absence of a preceding or concurrent COVID-19 diagnosis (light blue bar), during the quarter with the COVID-19 diagnosis (dark blue bar), and for the 2 quarters (6 calendar months) and subsequent quarters (6 to 15 calendar months) after the COVID-19 diagnosis quarter (blue bars). The number of cases of type 1 diabetes and the person-years of follow-up per group are indicated. Error bars indicate 95% binomial CIs of the respective incidence rate estimate.
Discussion
A diagnosis of COVID-19 in children was associated with an increased incidence of type 1 diabetes since 2020 in Bavaria. The findings suggest that SARS-CoV-2 infection contributed to the observed increase in type 1 diabetes incidence during the pandemic. Undiagnosed infection, which represents the majority of SARS-CoV-2 antibody–positive children,5 could also have contributed to the moderately increased incidence of type 1 diabetes observed in children without a COVID-19 diagnosis. Possible mechanisms include initiation of autoimmunity or acceleration of disease progression. Study limitations include the quarterly collection of data, which did not allow the determination of whether type 1 diabetes was diagnosed before or after COVID-19 when they occurred in the same quarter; missing viral confirmation in 70% of the diagnosed children; insufficient numbers of cases to allow subgroup comparisons; and potential confounding or selection biases. Further studies are required to determine whether vaccination should be considered in children at risk for type 1 diabetes.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Senior Editor.
Data Sharing Statement
References
- 1.Gottesman BL, Yu J, Tanaka C, Longhurst CA, Kim JJ. Incidence of new-onset type 1 diabetes among us children during the COVID-19 global pandemic. JAMA Pediatr. 2022;176(4):414-415. doi: 10.1001/jamapediatrics.2021.5801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamrath C, Rosenbauer J, Eckert AJ, et al. Incidence of type 1 diabetes in children and adolescents during the COVID-19 pandemic in Germany: results from the DPV Registry. Diabetes Care. 2022;45(8):1762-1771. doi: 10.2337/dc21-0969 [DOI] [PubMed] [Google Scholar]
- 3.McKeigue PM, McGurnaghan S, Blackbourn L, et al. Relation of incident type 1 diabetes to recent COVID-19 infection: cohort study using e-health record linkage in Scotland. Diabetes Care. 2022;dc220385. doi: 10.2337/dc22-0385 [DOI] [PubMed] [Google Scholar]
- 4.Zhang T, Mei Q, Zhang Z, et al. Risk for newly diagnosed diabetes after COVID-19: a systematic review and meta-analysis. BMC Med. 2022;20(1):444. doi: 10.1186/s12916-022-02656-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hippich M, Sifft P, Zapardiel-Gonzalo J, et al. A public health antibody screening indicates a marked increase of SARS-CoV-2 exposure rate in children during the second wave. Med. 2021;2(5):571-572. doi: 10.1016/j.medj.2021.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement


