Abstract
Background:
Cancers are a disease of growing public health importance in Africa, but cancer research capacity in the region is under-developed. The quest to foster and promote locally conceptualized and conducted oncology research in Africa have informed the African Research Group for Oncology’s (ARGO) research capacity building efforts in Nigeria.
Aim:
To evaluate the effectiveness of oncology research capacity building initiatives among Nigerian senior trainees and junior faculty physicians.
Subjects and Methods:
Panel study design was employed to study Nigerian senior trainees and junior faculty physicians who participated in two research capacity-building symposia. Data were collected pre-and immediate post-symposia, and three-month post first symposium. Changes in knowledge were assessed using Chi-Square; and level of confidence using Wilcoxon Signed Rank test. A p-value of <0.05 was considered statistically significant.
Results:
In the first symposium, the participants’ pass rate in the knowledge-based questions improved significantly from 9.8% to 46.7% to 81.5% at the baseline, immediate post-symposium, and three-month post-symposium respectively (p < 0.001). Likewise, participants’ level of confidence in carrying out certain research-related activities increased significantly after the second symposium (p < 0.001).
Conclusion:
The study concludes that building capacity for oncology research in low and- and middle-income countries is possible with focused symposia and educational programs.
Keywords: Cancers, capacity building, research
Introduction
The incidence of cancer in Africa is increasing, making it a major public health burden, and increasingly common cause of death.[1–3] However, cancer research capacity in the region remains under-developed and as such is an area of significant unmet need.[4] Research which is conceptualized, conducted, analyzed and published by Africans is central to meeting the health needs of the continent.[5] Building research capacity can promote problem solving, reduce the gap between evidence and practice, and promote health gains.[6] Research capacity building is defined as “the process by which individuals, organizations and societies develop the ability (individually and collectively) to perform research functions effectively, efficiently and sustainably, to define objectives and priorities, build sustainable institutions and bring solutions to key national problems.”[7] Building capacity for health research in low- and middle-income countries (LMICs) has also been identified not just as a driver of development and an essential component of strengthening healthcare system but also as a requirement for an efficient investment of limited resources.[8, 9]
Some of the unique challenges that LMICs face when undertaking healthcare-related research are a persistent scarcity of proficient researchers and competent interdisciplinary research teams, as well as limited research career opportunities and funding, among others.[8] These challenges are particularly obvious in cancer research, and contribute to a lack of local evidence necessary for driving change and improving outcomes.
In Nigeria, there is a clear need for training in oncology research. As in other LMICs, there appears to be a rising incidence of cancers in the country, although population-based cancer registry data is lacking in most states. Nigeria has committed to a National Cancer Control Plan (2018–2022) that includes scaling up cancer services, promoting earlier detection, and improving cancer outcomes. Achieving these ambitious goals will require training of oncologists and other physicians and healthcare providers not only in cancer care, but also in cancer research, monitoring and evaluation science. Supporting Nigerian physician scientists into the field of oncology is vital, and doing so requires opportunity for them to develop cancer-specific research skills and career pathways. The content of cancer-focused research training should include study design and methodology for carrying out cancer-focused epidemiological, translational, health services and clinical trials research. [1, 3] To the best of our knowledge, there is little oncology research capacity building currently taking place in Nigeria.
Based on the desire to proffer a solution to the shortage of oncology specialists and oncology researchers in Nigeria, the African Research Group for Oncology (ARGO), a consortium formed in 2013 through the collaborative efforts of surgeons at the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife, Nigeria and the Memorial Sloan Kettering Cancer Center (MSKCC), New York, United States of America, is focused on training and conducting cancer-related research by strengthening local research capacity. ARGO training initiatives include organizing symposia for physician-scientists with a special interest in oncology. The ultimate goal of these training initiatives is to improve the outcomes for cancer patients in Nigeria as well as other countries on the continent. One such training initiative was that supported by a grant from the US Civilian Research and Development Foundation (CRDF) in 2019. The goal was to create training that can foster cancer-focused health research capacity building among senior trainees and junior faculty physicians; which can as well be scaled up in the future. The objective of this study, conducted among the physician-scientists that attended ARGO onsite and online symposia, was to evaluate the effectiveness of the oncology research capacity building on them.
Material and Methods:
This study was conducted among senior trainees and junior faculty who participated in the two separate symposia (onsite and online) organized by ARGO one year apart. The first symposium was held between the 2nd and 3rd of October 2019 at the OAUTHC main auditorium, in Ile-Ife, Nigeria. The second symposium, held between 10th and 11th September 2020, was virtual via zoom owing to the COVID-19 pandemic gathering restrictions. The goal of these symposia was to create a platform to boost proficiency in the fundamentals of research so that each of the participants would be poised to participate as an investigator in on-going ARGO studies and as well be able to develop their independent research taking advantage of ARGO infrastructure. To meet this goal, a total of fifteen topics including fundamentals of research, mentorship and collaborative opportunity in research, basics of statistics, grant opportunities and grant management, to mention a few, were taken by different international and local faculty members.
Study Design and Study Population
Senior trainee and young faculty within three years post-fellowship program, drawn from some specialties involved in cancer care namely surgery, radiology, pathology, clinical and radiation oncology, and community medicine in the Nigerian ARGO collaborating institutions using panel study design, constituted the study population. The onsite symposium excluded faculty members in the selected departments who have spent more than three years post-residency training. However, the online symposium was attended by medical students, junior trainees and faculty members who have spent more than three years post-residency training, in addition to the original target population.
Sample Size and Sampling Technique
First symposium (October 2019):
Fifty eligible doctors were selected from the 25 ARGO collaborating institutions to attend the onsite symposium of which forty-seven attended the symposium. Using a convenience sampling method, a total of forty-one participants (87.2%) took part in the pre-symposium assessment, and forty-five (95.6%) completed an immediate post-symposium assessment questionnaire. Twenty-seven (57.5%) of participants present at the symposium were successfully contacted three months post-symposium through a social media platform (WhatsApp) created immediately after the symposium for further follow up.
Second symposium (September 2020):
Ninety-two potential participants registered through the online link sent to them via email addresses and the group WhatsApp. Eighty-eight (95.7%) completed the pre-symposium questionnaire, while fifty-three (57.6%) completed the post-symposium questionnaire, both hosted on survey monkey.
Data Collection
First symposium:
Data were collected using a self-administered questionnaire. The pre-symposium questionnaire comprised four sections: Section A socio-demographic variables; Section B participants’ previous research experience and grant management; Section C participants’ expectation from the symposium; and Section D participants’ knowledge in the fundamentals of research (study design, methodology and basic statistics).
The immediate post-symposium questionnaire comprised two main sections: Section A participants’ rating of how helpful/relevant each topic taken in the symposium was; Section B participants’ knowledge in the fundamentals of research (study design, methodology, and basic statistics) covered during the symposium. The knowledge-based questions contained in both pre- and post-symposium questionnaires were categorized into three domains namely epidemiological design, qualitative research, and basic statistics. These questions directly assessed the immediate impact of the symposium on the participants’ knowledge of the fundamentals of research and basic statistics.
The same set of questions assessing the participants’ knowledge of fundamentals of research were contained in the questionnaire administered via e-mail three months after the symposium to assess medium-term retention of the knowledge gained, in addition to other questions assessing participants’ progress in the area of conduct of research.
Second symposium:
Data were collected using a self-administered questionnaire hosted on survey monkey. The pre-symposium questionnaire comprised three sections: Section A socio-demographic variables, Section B questions that assessed participants’ previous research experience and mentorship while Section C assessed participants level of confidence in carrying out certain research-related activities such as generating a research question, choosing an appropriate research design, applying basic statistical tests, analyzing qualitative data, clinical trial study design, and interpretation, etc.
Data Analysis
Data were analyzed using IBM SPSS version 25 for windows (IBM SPSS Inc., Chicago, USA).
First symposium:
Categorical variables like socio-demographic variables, participants’ previous experience with research and grant management, and perceived usefulness of the lectures were summarized using frequency tables and chart. Knowledge scores at pre-symposium, immediate post-symposium, and three-month post-symposium assessments were compared using Chi-Square tests. P-value < 0.05 was considered to be statistically significant.
Second symposium:
Categorical variables like socio-demographic variables, participants’ previous experience with research, grant management and mentorship, and participants’ level of confidence in carrying out certain research-related activities before and after the symposium were likewise presented in tables. The difference in level of confidence was analyzed using Wilcoxon Signed Ranks Test
Ethical Consideration:
Ethical approval was sought and obtained from the Research and Ethics Committee of the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria. Informed consent was also sought and obtained from each participant. Confidentiality and data security were assured. Participation was made voluntary as each participant was at liberty to opt-out of the study at any point.
Results
First symposium:
The mean age of the forty-one participants that completed the pre-symposium questionnaire was 37.5 ± 3.5 years. The majority were males (70.7%). Only 26.8% of the participants had professional experience of greater than or equal to ten years post first medical degree. (see Table 1).
Table 1:
Participants’ Demographics
| Symposium 1 | Symposium 2 | ||
|---|---|---|---|
| Participants’ Demographics (n = 41) | Frequency (%) | Participants’ Demographics (n = 88) | Frequency (%) |
| Age Category (years) | (mean = 37.5 ± 3.5) | Age Category (years) | (mean = 37.4 ± 7.2) |
| 30–34 | 8 (19.5) | <30 | 12 (13.6) |
| 35–39 | 20 (48.8) | 30–34 | 8 (9.1) |
| 40–44 | 11 (26.8) | 35–39 | 35 (39.8) |
| ≥ 45 | 1 (2.4) | 40–44 | 22 (25.0) |
| Missing | 1 (2.4) | ≥ 45 | 9 (10.2) |
| Missing | 2 (2.3) | ||
| Sex | Sex | ||
| Female | 12 (29.3) | Female | 20 (22.7) |
| Male | 29 (70.7) | Male | 68 (77.3) |
| Professional cadre | Professional cadre | ||
| Consultant (Fellows) | 21 (51.2) | Consultant (Fellows) | 43 (48.9) |
| Senior registrar | 20 (48.8) | Senior registrar | 29 (33.0) |
| Others | 16 (18.2) | ||
| Years since after first medical degree | Years post fellowship (n = 41) | ||
| < 10 | 27 (65.9) | ≤ 3 | 27 (65.9) |
| ≥10 | 11 (26.8) | ≥ 4 | 14 (34.1) |
| Missing | 3 (7.3) | ||
| Types of degree | Years completed in residency (n = 29) | ||
| MBBS | 20 (48.8) | ≤ 3 | 4 (14.3) |
| Both (MBBS/Fellowship) | 21 (51.2) | ≥ 4 | 25 (86.2) |
| Any expectation for this conference? | Any expectation for this conference? | ||
| Yes | 38 (92.7) | Yes | 82 (93.2) |
| Missing | 3 (7.3) | Missing | 6 (6.8) |
A higher proportion of participants (78%) were interested in clinical research while 17.1% were interested in both clinical and translational types of research. The top three items identified by participants as obstacles to undertaking research included lack of mentorship (75.6%), lack of financial support for conducting research (56.7%), and lack of knowledge on research design, funding and grant management (46.3%). About 93% of participants had no previous experience in clinical trials, 65.9% had no previous experience with cancer-related epidemiological studies, 61% had no previous involvement or experience with manuscript writing and preparation, and about 95.1% did not have any prior experience with grant management. (see Table 2)
Table 2:
Participants’ Previous Experience with Research and Grant Management
| Symposium 1 | Symposium 2 | ||
|---|---|---|---|
| Previous Research Experience (n = 41) | Frequency (%) | Previous Research Experience (n = 88) | Frequency (%) |
| Types of research most interested in | Types of research most interested in | ||
| Clinical | 32 (78.0) | Basic science | 3 (3.4) |
| Translational | 1(2.4) | Clinical | 69 (78.4) |
| Clinical / Translational | 7 (17.1) | Translational | 8 (9.1) |
| Translational / Basic science | 1 (2.4) | Public & preventative | 6 (6.8) |
| Missing | 2 (2.3) | ||
| Previous experience in clinical research | Formal Research Degree | ||
| No | 9 (22.0) | No | 76 (86.4) |
| Yes | 32(78.0) | Yes | 12 (13.6) |
| Involvement with clinical trial design | Participated in 2019 ARGO Symposium | ||
| No | 38 (92.7) | No | 57 (64.8) |
| Yes | 3 (7.3) | Yes | 31 (35.2) |
| Involvement with epidemiological studies related to cancer | Participated in other cancer research course in the past 12mths | ||
| No | 27 (65.9) | No | 80 (90.9) |
| Yes | 14 (34.1) | Yes | 8 (9.1) |
| Involvement with the performance of diagnostic and screening tests | Hold Research Grants/Funding | ||
| No | 33 (80.5) | No | 84 (95.5) |
| Yes | 8 (19.5) | Yes | 4 (4.5) |
| Involvement with manuscript writing/preparation | Involvement with manuscripts writing | ||
| No | 25 (61.0) | No | 38 (43.2) |
| Yes | 16 (39.0) | Yes | 50 (56.8) |
| Number of manuscripts written annually (n = 16) | Number of manuscripts written in the past year (n = 50) | ||
| ≤ 2 | 10 (62.5) | ≤ 2 | 26 (52.0) |
| 3 or more | 5 (31.3) | 3 or more | 19 (38.0) |
| Missing | 1 (6.3) | Missing | 5 (10.0) |
| Familiarity with basic statistical methods (multivariate analysis) | |||
| No | 4 (9.8) | ||
| Yes | 7 (17.1) | ||
| Missing | 30 (73.2) | ||
| Do you have experience in grant management? | |||
| No | 39 (95.1) | ||
| Yes | 2 (4.9) | ||
| Do you know the importance of bio-banking in research? | |||
| No | 30 (73.2) | ||
| Yes | 11(26.8) | ||
| Having a research mentor in your hospital | Mentorship Category | ||
| No | 18 (43.9) | Participant has a mentor at their home institution | 28 (31.8) |
| Yes | 21 (51.2) | Participant has a mentor at another Nigerian institution | 22 (25.0) |
| Missing | 2 (4.9) | Participant has a mentor outside Nigeria | 11 (12.5) |
| Participant mentors others | 31 (35.2) | ||
| Most Common Barriers to Conducting Research | Most Common Barriers to Conducting Research | ||
| Lack of Mentorship | 31 (75.6) | Lack of financial support for conducting research | 58 (65.9) |
| Lack of financial support for conducting research | 22 (56.7) | Lack of Mentorship | 53 (60.2) |
| Lack of knowledge on research design, funding & grant management | 19 (46.3) | Lack of research infrastructure | 46 (52.3) |
| Lack of time | 11 (26.8) | Lack of knowledge on how to analyze research finding | 31 (35.2) |
| Lack of knowledge on appropriate study design | 30 (34.1) | ||
| Lack of time | 21 (23.9) | ||
| Lack of personal salary support for research | 16 (18.2) | ||
| Access to software/statistical packages for analysis | 15 (17.0) | ||
Many of the forty-five participants that completed the immediate post-symposium questionnaire (64.4%) found the topics taught in the symposium most useful/relevant for developing and progressing in their research careers. (see Fig.1)
Fig 1.
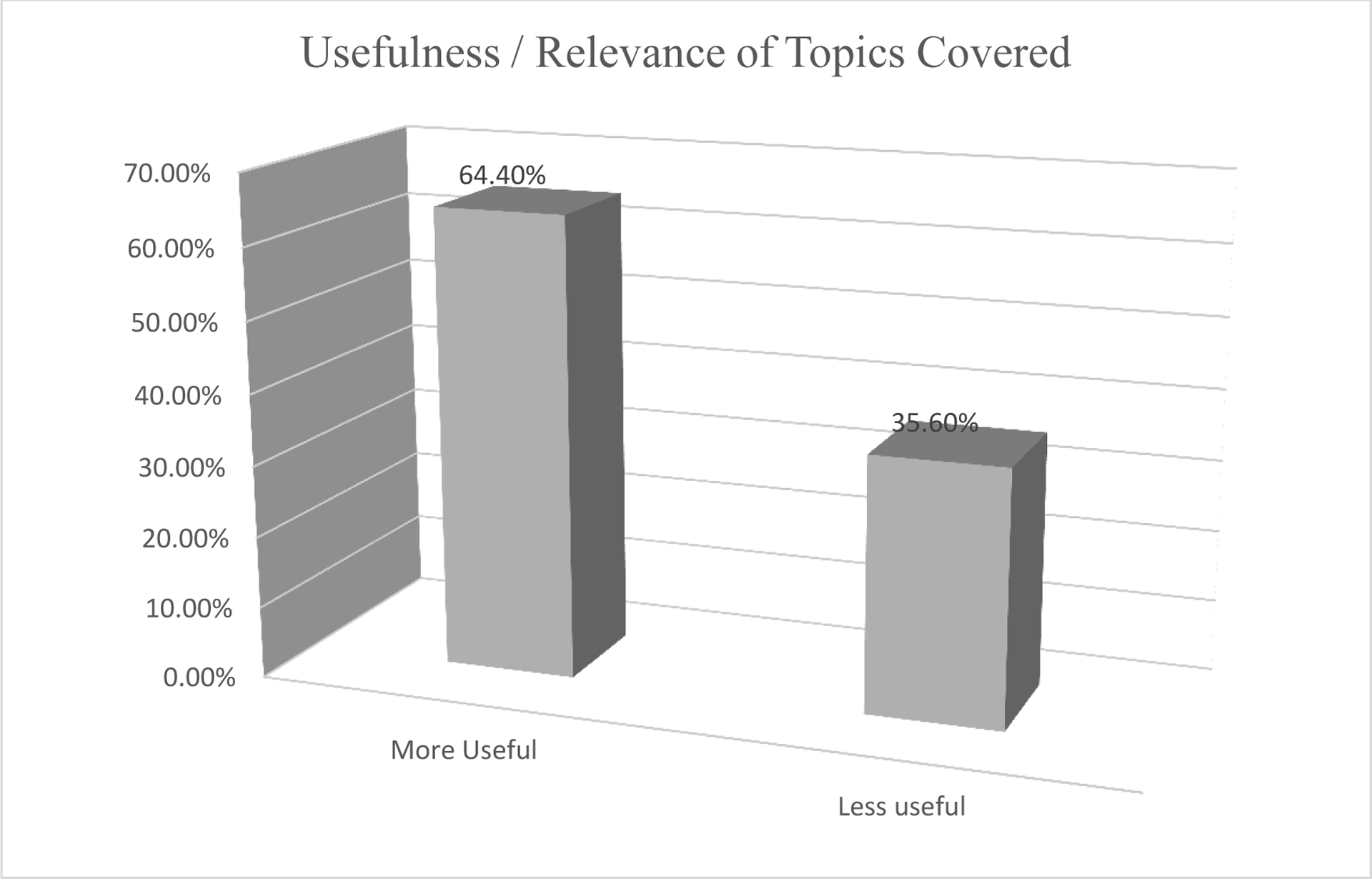
Usefulness / Relevance of Topics Covered in the Symposium to the Participants’ research career
Almost all participants came up with at least one research goal for the coming year including some participants whose goal centered on readiness to partner with ARGO in various cancer-related research initiatives. In general, there was a sustained improvement in the pass rate across the three stages of the assessment. Overall pass rate (i.e. the proportion of participants that scored 50% and above in the knowledge-based questions) increased significantly from 9.8% to 46.7% to 81.5% in the baseline, immediate post-symposium, and three-month post-symposium assessments respectively (p < 0.001). When the performance in the knowledge-based questions was disaggregated to the three main domains covered in the symposium – epidemiological design, biostatistics, and qualitative research domains, the proportion of participants that scored 50% and above also increased significantly (p < 0.001 for epidemiological design and qualitative research domains; and p = 0.002 for biostatistics domain). (see Table 3).
Table 3:
Performance in the 3 Stages Knowledge-Based Assessment
| Pre-test (n = 41) |
Post-test (n = 45) |
3 months Post-test (n = 27) |
||
|---|---|---|---|---|
| Category | Freq. (%) | Freq. (%) | Freq. (%) | Statistics |
| Overall performance | ||||
| Pass | 4 (9.8) | 21 (46.7) | 22 (81.5) | χ2 = 35.27 df =2 P < 0.001 |
| Fail | 37 (90.2) | 24 (53.3) | 5 (18.5) | |
| Epidemiological Design Domain | ||||
| Pass | 5 (12.2) | 20 (44.4) | 16 (59.3) | χ2 = 17.78 df =2 P < 0.001 |
| Fail | 36 (87.8) | 25 (55.6) | 11 (40.7) | |
| Bio-statistics Domain | ||||
| Pass | 24 (58.5) | 35 (77.8) | 27 (100.0) | χ2 = 12.72 df =2 P = 0.002 |
| Fail | 17 (41.5) | 10 (22.2) | 0 (0.0) | |
| Qualitative Research Domain | ||||
| Pass | 4 (9.8) | 30 (66.7) | 23 (85.2) | χ2 = 44.93 df =2 P < 0.001 |
| Fail | 37 (90.2) | 15 (33.3) | 4 (14.8) | |
Additionally, 66.7% of the participants who returned their questionnaire three months post-symposium had written at least one research proposal since after the symposium. Thirty-seven percent of these written proposals were cancer-related. While the cancer-related proposal writing process was completed for 11.1% of the participants only 5.6% of them had commenced data collection. (see Table 4)
Table 4:
Experience with Proposal Writing 3 months after the Symposium
| Variables | Freq. (%) |
|---|---|
| At least one proposal written (n = 27) | |
| Yes | 18 (66.7) |
| No | 9 (33.3) |
| The area where the proposal is written (n = 27) | |
| Cancer- Related | 4 (14.8) |
| Other Areas | 8 (29.6) |
| Both | 6 (22.2) |
| Not Applicable | 9 (33.3) |
| Stage of cancer proposal (n =18) | |
| Conceptualization | 8 (44.4) |
| Proposal completely written | 2 (11.1) |
| Study/data collection commenced | 1 (5.6) |
| Not applicable | 7 (38.9) |
| Stage of the proposal on other areas (n =18) | |
| Conceptualization | 4 (22.2) |
| Proposal completely written | 5 (27.8) |
| Study/data collection commenced | 5 (27.8) |
| Not applicable | 4 (22.2) |
Second symposium:
The mean age of the eighty-one participants that completed the pre-symposium questionnaire was 37.4 ± 7.2 years with majority still being males (77.3%). (see Table 1). While a higher proportion of participants (78.4%) were interested in clinical research only 13.6% of them had a formal research degree. Although, only 35.2% of participants in this second symposium participated in the first, the top three items identified by participants as obstacles to undertaking research came with different rankings namely lack of financial support for conducting research (65.9%), lack of mentorship (60.2%), and lack of research infrastructure (52.3%). Only 4.5% of the participants hold research grants or funding. However, participants have different categories of mentors—31.8% had mentors at their home institution, 12.5% at another Nigerian institutions and 35.2% had mentor outside Nigeria. (see table 2) Participants’ level of confidence in carrying out some research-related activities increased significantly after the symposium compared to what it was before the symposium. (p < 0.001) (see Table 5)
Table 5 –
Pre- & Post- symposium level of confidence in carrying out certain research related activities.
| Variable | Pre-symposium Median (IQR) | Post-symposium Median (IQR) | p- value |
|---|---|---|---|
| % level of confidence sum | 411.0 (447.5) | 886 (311.0) | < 0.001* |
Wilcoxon Signed Ranks Test
Discussion
Nigeria, like many other LMICs faces a high cancer burden associated with poor outcomes due to late presentation and low access to treatment. Efforts to improve cancer outcomes in the country should be informed by locally relevant evidence. However, there is an existing gap for cancer research capacity building.[4] Greater ability to develop and lead cancer research focused on Nigerian priorities and needs represents a major pathway to changing the cancer narrative in the country. ARGO is rising to the occasion filling the existing gaps in oncology research capacity in Nigeria through its training initiatives. Another example of African initiatives to increase research capacity in Nigeria is the Consortium for Advanced Research Training in Africa (CARTA) program. This initiative has focused on training health sciences researchers in Africa for the future and has ensured that the training of these young scientists would make them globally competitive. [4, 10] This consortium comprises institutions in Kenya, South Africa, Tanzania, Uganda, Malawi, Nigeria and Rwanda with key northern partners. The aim of CARTA is to build a vibrant African academy able to lead world-class multidisciplinary research that impacts positively on public and population health. [10, 11] Some PhD students in member institutions have benefitted from CARTA’s capacity building programs.
Our evaluation revealed a paucity of cancer-focused research knowledge and skills among the study population at baseline. This is reflective of what has been reported in many scientific journals that health research capacity in LMICs remains deficient. [12–17] Our study also identified that participants had poor knowledge of study design and statistical analysis at baseline. Studies have associated low authorship from LMICs with poor knowledge of study design and statistical analysis, among others; hence, increasing reliance on researchers from HICs. [16, 17] Lack of funding for research and lack of mentorship were also identified by participants as major barriers to conducting research. This is congruent with what is reported elsewhere in the literature, and associated with low research capacity in LMICs. [16, 17]
Our study demonstrated a significant improvement in knowledge pertaining to the fundamentals of research, which was sustained three months after the symposium. This was also reflected in the positive progressive impact of the capacity building initiative on the participants’ own research practice and significant improvement in the participants’ level of confidence in carrying out certain research-related activities. This is similar to the finding in an evaluation conducted on Tropical Disease Research’s (TDR) contribution to individuals and institutional research career capacity strengthening, between the initiation and the end of the training program in which participants demonstrated substantial improvements in their self-perceived efficacy for study conceptualization, study planning and the ethical conduct of research.[8] The difference between the two studies is that while our study was a stage-wise evaluation of serial symposium exposures, that conducted on TDR’s research capacity building initiative was on grant award to pursue higher degrees in institutions of learning. The sustained improvement in the knowledge of fundamentals of research observed three months after the first symposium in our study could be partly attributed to the mentoring provided to the participants that were successfully followed up via the social media platform. Similar improvement in knowledge was observed in the different cadre of health workers provided clinical mentorship required to render better quality healthcare services in a study conducted in Jigawa State, Northern Nigeria.[18] The study at Jigawa State focused on evaluation of capacity building for service delivery contrary to evaluation of research capacity building which was the main focus of this study
The two symposia evaluated in this study provided valuable lessons and guide points for future learning goals and strengthening of research capacity building in Nigeria. The onsite symposium allowed participants to engage in small participatory group work. It also provided an excellent opportunity for the facilitators to learn more about the individual participants and their respective interests in research. COVID-19 pandemic gathering restriction was also an eye-opener to the vast potential of research capacity building that can be explored online. We also learned through the review of the participants’ performances at the various stages of the assessment that while the lectures resonated well with participants and their knowledge base and level of confidence in carrying out specific research-related activities increased post symposia, they still highlighted the need for additional support. As such, there remains an opportunity and a need for in-depth training and ongoing mentorship around the fundamentals of clinical research and their application to clinically relevant questions, coupled with assistance in budget preparation and publication of research manuscripts. The symposia evaluated in this study allowed us to introduce and open a pathway for physician-researchers in Nigeria to pursue learning opportunities that would enable them to gain the knowledge and opportunities to further their scientific and professional careers in the global field of cancer research. This can gradually fill the existing gap for oncology researchers in Nigeria. Likewise, the model of small group work employed in the onsite symposium should be included in future training. Selecting a few of these participants to pursue additional degrees for research capacity building will also be explored in the near future.
Conclusion
There is a need for cancer research capacity building in Nigeria, similar to many LMICs. This study demonstrates that both in-person and online symposia focused on the fundamentals of cancer research in Nigeria can successfully increase baseline knowledge, skills, and experience, and encourage greater participation in research. This study also provided an opportunity for Nigerian physician-scientists to identify and reflect on the critical areas of need and the challenges faced in conducting clinical research related to cancer in the country. It provides invaluable guidance for strengthening and building research capacity in Nigeria, and for growing a network of individuals and institutions committed to undertaking rigorous research that is relevant to cancer needs in Nigeria. Through ARGO’s training infrastructure, its platform for mentorship, and the expanding cancer-related studies underway; it is committed to closing the knowledge gap and building a strong cadre of physician-scientists who will expand cancer research expertise across the African continent.
Key message:
The research capacity building efforts of ARGO is on the path of filling the existing gaps in research capacity among Nigerian physician-scientists.
References
- 1.Morounke SG, et al. , Epidemiology and incidence of common cancers in Nigeria. Population, 2017. 84(82,231,000): p. 166,629,000. [Google Scholar]
- 2.International Agency for Research on Cancer WHO, Latest Global Cancer Data: Cancer Burden rises to 18.1 million nw cases and 9.6 million cancer deaths in 2018. . CA: A cancer Journal for Clinicians, 2018. [Google Scholar]
- 3.Kingham TP, et al. , Treatment of cancer in sub-Saharan Africa. The Lancet Oncology, 2013. 14(4): p. e158–e167. [DOI] [PubMed] [Google Scholar]
- 4.Kramer B and Libhaber E, Closing the barrier between disease and health outcomes in Africa through research and capacity development. Global health action, 2018. 11(1): p. 1425597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fonn S African PhD research capacity in public health: raison d’etre and how to build it. in Global forum update on research for health. 2006. Global Forum for Health Research Geneva. [Google Scholar]
- 6.Cooke J, Gardois P, and Booth A, Uncovering the mechanisms of research capacity development in health and social care: a realist synthesis. Health research policy and systems, 2018. 16(1): p. 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.UNDP, Capacity assessment and development in a system and strategic management. . Bureau for Development Policy, UNDP, New York, Technical Advisory panel N0 3, 1998. [Google Scholar]
- 8.Minja H, et al. , Impact of health research capacity strengthening in low-and middle-income countries: the case of WHO/TDR programmes. PLoS Negl Trop Dis, 2011. 5(10): p. e1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Planning M, Evaluation Framework for Capacity Strengthening in Health Research. Geneva: ESSENCE on Health Research, 2011. [Google Scholar]
- 10.Ezeh AC, et al. , Building capacity for public and population health research in Africa: the consortium for advanced research training in Africa (CARTA) model. Global health action, 2010. 3(1): p. 5693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fonn S, et al. , Building the capacity to solve complex health challenges in sub-Saharan Africa: CARTA’s multidisciplinary PhD training. Canadian Journal of Public Health, 2016. 107(4–5): p. e381–e386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowsher G, et al. , A narrative review of health research capacity strengthening in low and middle-income countries: lessons for conflict-affected areas. Globalization and health, 2019. 15(1): p. 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Franzen SR, Chandler C, and Lang T, Health research capacity development in low and middle income countries: reality or rhetoric? A systematic meta-narrative review of the qualitative literature. BMJ open, 2017. 7(1): p. e012332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Käser M, et al. , Research capacity strengthening in low and middle income countries–an evaluation of the WHO/TDR career development fellowship programme. PLoS neglected tropical diseases, 2016. 10(5): p. e0004631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edwards N, Kaseje D, and Kahwa E, Building and evaluating research capacity in healthcare systems: Case studies and innovative models. 2016: Juta and Company (Pty) Ltd. [Google Scholar]
- 16.Mendis S, Research Is Essential for Attainment of NCD Targets and Sustainable Development Goals. Global Heart, 2016. 11(1): p. 139–140. [DOI] [PubMed] [Google Scholar]
- 17.Bloomfield GS, et al. , Training and capacity building in LMIC for research in heart and lung diseases: the NHLBI–UnitedHealth Global Health centers of excellence program. Global heart, 2016. 11(1): p. 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okereke E, et al. , Evaluating Health Workers’ Knowledge Following the Introduction of Clinical Mentoring in Jigawa State, Northern Nigeria. African journal of reproductive health, 2015. 19(3): p. 118–125. [PubMed] [Google Scholar]


