Abstract
In this article, we provide a brief overview of some of the outstanding sessions that were (co)organised by the Allied Respiratory Professionals Assembly during the 2022 European Respiratory Society International Congress, which was held in a hybrid format. Early Career Members from Assembly 9 summarised the content of the sessions, with the support of the Officers from the four Assembly groups: Respiratory Function Technologists and Scientists (Group 9.01); Physiotherapists (Group 9.02); Nurses (Group 9.03); and Psychologists and Behavioural Scientists (Group 9.04). The sessions covered the following topics: recent advances in cardiopulmonary exercise and challenge testing; the role and new trends in physiotherapy, exercise and physical activity promotion interventions in chronic respiratory diseases; development of the international curriculum for respiratory nurses and nursing aspects in disease management; and treatment adherence, e-health interventions and post-coronavirus disease 2019 challenges. This Highlights article targets delegates who attended the Congress sessions, as well as those who were unable to attend, and provides valuable insight into the latest scientific data and emerging areas affecting the clinical practice of Allied Respiratory Professionals.
Short abstract
This article provides a brief overview of some of the outstanding sessions that were (co)organised by @ERS_Assembly9 (Allied Respiratory Professionals) during #ERSCongress 2022 https://bit.ly/3TBBvK6
Introduction
The European Respiratory Society (ERS) International Congress is an annual event that brings together thousands of experts from around the world to present and discuss the latest scientific and clinical advances in the respiratory field. In 2022, the ERS Congress took place in a hybrid format (Barcelona, Spain and online) and provided the Allied Respiratory Professionals with a wide range of outstanding sessions (co)organised by Assembly 9.
In this article, the four groups from the Assembly highlight some of the sessions presented at the ERS Congress 2022. Early Career Members (including respiratory function technologists and scientists, physiotherapists, nurses, and psychologists and behavioural scientists) summarise the latest scientific and clinical insights presented in five oral presentation and two thematic poster sessions: one session on recent advances in cardiopulmonary exercise and challenge testing; two sessions on new trends in physiotherapy, exercise and physical activity (PA) promotion interventions in chronic respiratory diseases; one session on the development of the international curriculum for respiratory nurses; two sessions on nursing aspects in disease management; and one session on the best abstracts from psychologists and behavioural scientists. Summaries of the sessions with important take-home messages are provided.
Group 9.01: respiratory function technologists and scientists
Cardiopulmonary exercise and challenge testing: utilisation and safety implications
This session included seven oral presentations that covered recent advances and current perspectives concerning the clinical application of cardiopulmonary exercise testing (CPET) and direct bronchial provocation via histamine and methacholine.
Clinical application of exercise testing
CPET is an important clinical tool with an established role in the diagnosis and management of chronic lung disease [1]. Mcarthur et al. [2] presented findings concerning the safety and accuracy of a recently established physiologist-led CPET service. In total, 579 CPETs were conducted in 1 year, with almost one third (n=188) performed by physiologists. Of these, none of the tests required medical attention. Importantly, following training, physiologists felt competent at conducting the CPET autonomously, and adopting this approach saved approximately 282 h of annual consultant time.
Blibech and colleagues evaluated the predictive value of CPET on surgical outcomes in patients undergoing lung resection surgery in Tunisia [3]. In this study, post-operative complications were associated with higher age, smoking history and minute ventilation/carbon dioxide production (V′E/V′CO2) slope, and lower forced expiratory volume in 1 s (FEV1), maximum oxygen consumption (V′O2max) and oxygen pulse. The authors concluded that V′O2max and V′E/V′CO2 are important CPET parameters that should be included as part of functional evaluation risk stratification algorithms to guide lung resection surgery referral pathways.
Rath et al. [4] assessed the effects of expiratory flow limitation during tidal breathing (EFLT) on lung function, exercise limitation and symptom perception in 86 patients with stable COPD (male n=83; age 64±9 years; body mass index (BMI) 22.4±4.2 kg·m−2). Respiratory impedance was measured via forced oscillometry, and small airway dysfunction was defined as either whole-breath reactance at 5 Hz (X5) less than the lower limit of normal, and/or difference in resistance at 5 and 19 Hz (R5−19) more than the upper limit of normal. The sample was stratified into two subgroups: 1) COPD with EFLT and 2) COPD without EFLT. The authors observed no difference between groups for modified Medical Research Council score, COPD Assessment Test (CAT) score or 6-min walk test (6MWT) distance (p>0.05). However, the fall in oxygen saturation measured by pulse oximetry (SpO2) and increase in Borg dyspnoea scores during the 6MWT were higher in COPD with EFLT (p<0.05).
Ong-Salvador et al. [5] explored whether transcutaneous carbon dioxide (PtcCO2) is a reliable alternative to partial pressure of carbon dioxide in arterial blood (PaCO2) and whether PtcCO2 can distinguish between hypercapnia and hypocapnia during exercise. CPETs with arterial blood gases (ABG) (n=124 patients; male 44%; age 56±68 years) were divided into three subgroups: ABG at rest (n=65), ABG at peak exercise (n=112), and ABG at rest and peak exercise (n=53). The authors observed no significant differences and reported a strong linear correlation between PtcCO2 and PaCO2 at rest and peak exercise; however, the PtcCO2 in isolation failed to discern between hypercapnia and hypocapnia during CPET.
Vesteng et al. [6] presented data from a retrospective study comparing the agreement between oxygen saturation measured via SpO2 during 6MWT versus arterial oxygen saturation (SaO2) during a CPET. In total, 70 patients with chronic lung disease (male n=40; age 61±13 years) were included. No difference was observed at rest between SpO2 and SaO2 (p=0.133); however, the saturation was significantly lower for SpO2 when comparing nadir values (i.e. the lowest measure of saturation obtained throughout the tests) (p=0.042). The authors concluded that an indirect measure of SpO2 during a 6MWT may overestimate desaturation when compared to direct measures of SaO2, although SpO2 appears to capture clinically relevant desaturation.
Challenge tests: direct bronchial provocation via histamine and methacholine
de Vreede [7] conducted a retrospective analysis of histamine provocation tests to determine factors impacting post-challenge recovery. The study population (569 patients with a post-challenge 10% decline in FEV1) were randomly matched and divided into two subgroups: 1) insufficient recovery following the administration of 400 μg salbutamol (n=94) (defined as >10% change in FEV1 from baseline), and 2) sufficient recovery (n=94) (defined as <10% change in FEV1 from baseline). In those classified as insufficient recovery, 79 had a high BMI. Logistic regression indicated an explanatory power of 27.9% of insufficient recovery based on gender and BMI, and the probability of insufficient recovery increased by 11.8% in those with a BMI ≥25 kg·m−2 (p<0.01). Based on these findings, the authors suggested that gender and BMI should be considered when interpreting the recovery response to histamine provocation tests.
The study from Steenbruggen and De Laat [8] evaluated the safety of the quadruple 1-min protocol using the tidal volume methacholine challenge [9]. Methacholine challenge tests were conducted and “extreme falls” in FEV1 were defined as >20% fall in FEV1 following the initial dose or >30% fall in FEV1 after any subsequent dose. In total, 339 tests were conducted, and of these, only four (1.2%) patients had a >20% fall in FEV1. Specifically, three patients fully recovered 15 min post 400 μg salbutamol, with one patient within 10% of baseline. Full recovery was also observed in the two patients (0.6%) experiencing >30% fall in FEV1. Despite the low number of cases, the findings from this study support the concept that the quadruple 1-min protocol using the tidal volume methacholine challenge is a feasible and safe procedure for adults when conducted by experienced physiologists.
Take-home messages
CPET is safe and well-tolerated by people with chronic lung disease. Parameters such as V′O2max and V′E/V′CO2 may be useful to assess the functional status of patients considered for lung resection surgery.
Expiratory flow limitation is related to reduced pulmonary function, increased dyspnoea scores and a significant fall in SpO2 during exercise.
PtcCO2 in isolation does not appear to discern between hypercapnia and hypocapnia during CPET.
SpO2 captures clinically relevant desaturation, although it may overestimate desaturation when compared to direct measures of SpO2.
Gender and BMI should be considered when interpreting the recovery response to histamine provocation tests.
The quadruple 1-min protocol using the tidal volume methacholine challenge is safe and feasible when conducted by experienced physiologists.
Group 9.02: physiotherapists
New trends in exercise, physical activity and behavioural changes in COPD, interstitial lung disease and asthma
Discovering new ways to improve pulmonary rehabilitation (PR) and PA access and outcomes is a research priority [10–12]. This oral presentation session provided new insights into current interventions and measures used in respiratory diseases.
To improve PR access [10], new intervention models have been emerging. Oliveira et al. [13] conducted a Delphi study to achieve consensus on the essential outcomes of rapid access rehabilitation for acute exacerbations of COPD (AE-COPD) [13]. The key components identified, i.e. eligibility and timeline, treatment priorities, programme design, outcomes and measures and referral and uptake, provide the foundation for developing interventions to optimise access to PR in AE-COPD. Wuyts et al. [14] compared the effects of a hybrid PR programme with a conventional programme in stable COPD. After PR, significant improvements were observed in both groups in exercise capacity, muscle strength and dyspnoea (p<0.05). The authors concluded that this hybrid PR programme seems to be effective by increasing patients’ accessibility [10, 15–19].
Physical inactivity is associated with poor health outcomes in chronic respiratory diseases [20–25]. Therefore, increasing PA in these populations is imperative. Marklund et al. [26] explored individuals’ perceptions when using an e-health tool to promote PA in COPD. For participants, the tool provided individual support and feeling of control, which highlights its relevance to maintain/increase PA levels. Breuls et al. [27] compared the effects of a 12-week telecoaching intervention for PA promotion with usual care in interstitial lung disease (ILD). After 12 weeks, no significant differences were observed between groups in PA. Therefore, the authors recommended PA promotion interventions with direct supervision or social support to increase PA in ILD. Paixão et al. [28] explored the feasibility of a home-based PA programme (iLiFE) in ILD. iLiFE showed to be feasible and safe, presenting high adherence and potential to improve many health domains, such as PA. In asthma, Carvalho-Pinto and colleagues found that an 8-week behaviour change intervention aimed to increase PA in daily life significantly improved patients’ PA levels, sleep quality and asthma-related and anxiety symptoms when compared to usual care [29].
The emerging evidence to develop new PR models [10] highlights the need for simple, interpretable and meaningful measures. Rodrigues et al. [30] used clustering to identify COPD subgroups according to their performance on several functional status measures (6MWT, 1-min sit-to-stand (1-minSTS), handgrip, and quadriceps muscle strength). The four clusters that were found according to the achievement of 70% of predicted in these measures were 1) non-achievers, 2) partial achievers, 3) achievers and 4) overachievers. These clusters may guide tailored interventions to improve patients’ functional status [31]. Finally, Quadflieg et al. [32] explored the applicability of the 1-minSTS to predict post-operative complications in lung cancer and showed that a cut-off of 22 repetitions and 59% predicted in the 1-minSTS could discriminate between patients with and without post-operative complications.
Take-home messages
New models of PR, such as rapid access rehabilitation and hybrid delivery, have been shown to increase patients’ access and accessibility to PR in acute and stable COPD.
e-Health tools, PA promotion and behaviour change interventions (with direct supervision) might be a good solution to improve PA levels in chronic respiratory diseases.
Functional status measures, including 6MWT and 1-minSTS, can help cluster individuals with COPD and discriminate post-operative complications in lung cancer.
Challenges in respiratory physiotherapy assessment and management
This oral presentation session provided a round-up on challenges regarding physiotherapy assessment and management of patients with chronic respiratory disorders, post-coronavirus disease 2019 (post-COVID-19) and under mechanical ventilation in the acute or home settings.
The study of Souto-Miranda et al. [33] showed that sex-related differences exist in treatable traits among patients with COPD. Most traits were more prevalent in women than men in patients referred to secondary and tertiary care, with differences being more extensive in tertiary care.
Tanguay et al. [34] presented their newly developed reference equations for quadriceps strength, endurance and power that explained 50% to 70% of the total variance in quadriceps functions in healthy individuals. Percentage of predicted values for quadriceps muscle function based on these reference equations correlated weakly to moderately with the 6MWT and 1-minSTS performance in patients with COPD, which supports the construct validity of the equations in this population.
COVID-19 has also an impact on exercise capacity, PA and respiratory muscle function. Diciolla et al. [35] showed that fatigue was clinically relevant and could be an explaining factor of a lower performance in exercise capacity (measured by 6MWT and 1-minSTS) in post-COVID-19 patients at 12 months after discharge. Arents et al. [36] objectively measured PA in 49 post-COVID-19 patients at 12 months after hospital discharge. From these, 67% were low active (i.e. <7500 steps per day) and their PA levels were positively associated with 6-min walking distance. Post-COVID-19 patients might need to be coached to a more active lifestyle to meet the guidelines [37]. Lima Souza Saldanha et al. [38] found that, in a cohort of 269 post-COVID-19 patients with persistent symptoms of dyspnoea and fatigue, 32% had inspiratory muscle weakness which was also associated with a lower handgrip strength.
Managing patients on invasive and non-invasive home mechanical ventilation (HMV) is challenging, in terms of the availability of healthcare professionals at home and cost of care. Telemonitoring of HMV may be a solution, as it allows a clinical coordinator specialised in mechanical ventilation to remotely follow the HMV data and reach out to the clinical staff who are assisting patients at home for case discussions, corrective actions and follow-up. A study presented in this session showed that telemonitoring of HMV led to better quality of the service provided by homecare providers and was associated with clinical improvement and 45% reduction in the cost to manage patients on HMV [39].
Take-home messages
Healthcare providers should be aware of sex-related differences in treatable traits among patients with COPD.
New reference equations for quadriceps strength, endurance and power that explain 50% to 70% of the total variance in quadriceps function in healthy subjects are available, and these measures seem valid in patients with COPD.
COVID-19 has long-term impact on PA, exercise capacity and respiratory muscle function.
Telemonitoring of HMV may lead to clinical benefits and cost reduction.
Group 9.03: nurses
Development of the international curriculum for respiratory nurses: perspectives and needs
This oral presentation session highlighted the perceived need for the development and implementation of the international core curriculum for respiratory nurses (ICCRN) on a global scale. Leading nurses, on behalf their national associations, stated their support for the undergoing International Coalition for Respiratory Nursing (ICRN) project.
Examples of good practice
The introduction of the clinical nurse specialists and advanced nurse practitioner's role is one of the most significant changes in nursing practice in Ireland in recent years. The study from Murray [40] suggested that specific education in the respiratory field enhances nursing professionalisation. Stridsman et al. [41] presented the nursing education plan in the respiratory field in Sweden and highlighted that specialised nurses are the bridge between healthcare and the society. The courses are designed with a person-centred approach with focus on self-management, interprofessional collaboration and evaluation of treatment adherence. Dos Santos Castro Padilha et al. [42] highlighted that rehabilitation nursing in Portugal underpins the development of specialised nursing skills to support respiratory patients to enhance self-care and self-management behaviours, to maintain activity tolerance and integration into society. The authors believe that the ICRN project will underpin the definition and harmonisation of educational standards towards recognising nurses' certification worldwide, with the support from Portuguese Order of Nurses and the Portuguese Association of Rehabilitation Nurses. On behalf of the Association of Respiratory Nurse Specialists (ARNS), Heslop-Marshall et al. [43] announced that the ARNS joined the ICRN, with the aim of advocating for respiratory nursing, promoting excellence in practice and influencing respiratory nursing health policies.
Obstacles in nursing education in respiratory care
Roberts et al. [44] showed a significant variation in the provision of respiratory education in UK pre-registration nursing programmes. They reported low levels of final year nursing student confidence in key respiratory knowledge and skills, and recommended these to be embedded in the curricula. Examples of limitations in areas of nursing training in Croatia were presented by Sajnic and colleagues [45, 46]. Pressing problems in nursing are the lack of nurses, underpayment, uneven key contents in the curricula of graduate studies, non-recognition of higher education, and nursing as an independent profession in the society [47]. A similar situation was reported by Çevik Akyıl et al. [48] in Turkey. The authors referred to the lack of specific educational programmes in respiratory nursing and rising numbers of nurses quitting their jobs due to working conditions and highlighted that the only way to improve respiratory patient outcomes and nurse job satisfaction is having worldwide standardised education and recognised certification programmes through the development of an ICCRN [48].
New steps towards harmonised nursing education in respiratory care
Narsavage et al. [49] presented a cross-sectional survey that was designed to identify the current curricula in European Union (EU) and non-EU countries and the need for an ICCRN. Survey results confirmed a wide variation in nursing education and respiratory nursing education across the world, with many countries lacking formal educational programmes in this field and 97% reporting a need for an ICCRN. To advance this significant work, the ICRN group led by A. Šajnić and supervised by G. Narsavage plans to conduct a Delphi study to identify core curriculum requirements for respiratory nursing education at pre-registration and advanced educational levels to meet each country's specific educational requirements for recognition of respiratory nursing speciality practice [50]. Following HERMES methodology guidelines [51], Sajnic et al. [52] presented the steps of the ICRN project: in 2020 experts were identified, the ICRN working group registered the Scoping Review Protocol [53], and the items obtained from this protocol will be included in the first online Delphi survey. Acting on findings, a consensus document for the core curriculum will be published.
Take-home messages
The development of an international curriculum for respiratory nursing will provide more effective and safer delivery of care to respiratory patients around the globe.
Under the leadership of the ERS nurses' group Chair, an ICRN was formed after the ERS International Congress 2020 for the development of a harmonised syllabus and curriculum for respiratory nurses, thereby responding to the need for harmonised respiratory nursing education on a global scale.
Nursing aspects in asthma and COPD: self-management and pulmonary rehabilitation
This oral presentation session included eight presentations that highlighted the importance and effectiveness of nursing-led non-pharmacological interventions in PR programmes for patients with asthma and/or COPD. It also addressed the negative effects of the lockdown on patients’ quality of life and the benefits from led telenursing consultations during the COVID-19 pandemic. Below we present their main results.
Rezelj et al. [54] concluded that the results of the Asthma Control Test (ACT) and the Severe Asthma Questionnaire (SAQ) in severe asthma patients after bronchodilators (n=80) were significantly correlated (p<0.0001). Miranda Valladares et al. [55] showed a significant improvement of quality of life in a retrospective study with COPD patients who received nursing non-pharmacological interventions: 1) 8-week PR (including cardiorespiratory and muscular training), 2) PA promotion (with implementation of exercise routines) and 3) therapeutic education (focused on the pathophysiology of the disease and the foundations of the therapeutic regimen).
Refsgaard Iversen et al. [56] investigated the effect of affiliation with a cross-sectorial lung team (CLT), consisting of respiratory nurses and community nurses. On average, patients affiliated with the CLT had fewer hospitalisations and shorter length of hospital stay compared to usual care [56].
Bech et al. [57] assessed the benefits on oxygen therapy management through an SpO2-based automatic oxygen administration device in patients with COPD. Although there was a feeling of safety in the use of the devices, patients expressed that machines cannot replace healthcare workers in complex healthcare management.
Granados Santiago et al. [58] showed that COPD patients’ overall perceived health status in the COVID-19 lockdown was significantly lower than before the pandemic (p<0.05), showing enhanced psychological vulnerability. Still on pandemic impact, Miranda Valladares et al. [59] showed that lockdown had a significant negative effect on several clinical variables (i.e. FEV1% predicted, dyspnoea, distance walked in the 6MWT and BODE (BMI, airflow obstruction, dyspnoea, and exercise capacity) index) on functional capacity and physiological parameters of patients with COPD.
Silva et al. [60] performed a systematic review and meta-analysis on the optimal structure of PR maintenance programmes (PRMP), revealing that 1) PRMP with alternate supervision showed better results concerning the 6MWT and FEV1% values than unsupervised programmes, and 2) home-based and supervised PRMP led to better functional capacity improvements than community-based and unsupervised programmes. Alves Vaz et al. [61] presented the preliminary results of the efficacy and safety of an 8-week pulmonary telerehabilitation programme, showing a tendency to an improvement in all clinical variables (e.g. dyspnoea, functional capacity, anxiety and depression), with no reported adverse effects.
Take-home messages
Non-pharmacological interventions (PR, PA promotion and therapeutic education) can increase quality of life in patients with COPD.
A cross-sectorial lung team consisting of respiratory nurses and community nurses is a feasible way to guarantee patients’ accessibility to the right care at the right time.
Home-based and supervised maintenance programmes may have a more significant impact on patients’ functional capacity than community-based and unsupervised programmes.
Nursing interventions in various respiratory areas
This thematic poster session highlighted several nursing practice aspects in the respiratory field. To summarise them, we divided the posters into nursing interventions, review of nurses’ clinical practice, and health policies.
Nursing interventions
Martín Núñez et al. [62] found that patients with long COVID syndrome had significant cognitive impairment, increased anxiety levels, depression and difficulties in concentration, and decreased memory even 1 year after COVID infection. Carrera Cueva et al. [63] demonstrated that a telenursing consultation decreased anxiety and depression and increased adherence to treatment among post-COVID-19 patients. In asthma management, Silva and Rodrigues [64] presented a quasi-experimental study of a social media-based intervention and showed that it enhanced asthma control, in a statistically and clinically significant way, indicating better control of the disease. Miranda Valladares et al. [65] reinforced that depression and anxiety determine the effects of PR on the quality of life of patients with COPD.
Review of nurses’ clinical practice
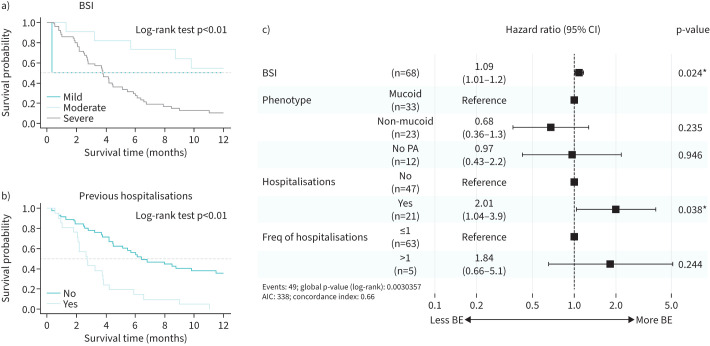
In reviewing low molecular weight heparin injection complications in a retrospective study with COVID-19 pneumonia, Keramida et al. [66] found that abdominal haematomas, although uncommon, have relevant clinical significance and suggested re-training and monitoring of subcutaneous heparin injection technique. Based on a cohort study, Bueno Freire et al. [67] concluded that the severity of bronchiectasis and previous hospitalisations were associated with a higher risk of exacerbations in patients colonised by Pseudomonas aeruginosa (figure 1). Regarding aerosol inhalation therapy, Yu et al. [68] showed the superior efficacy of modified viral and bacterial filters used in aerosol inhalation therapy compared with the usual viral and bacterial filters, preventing particles from spreading to the patient environment without increasing respiratory work. Bettany [69] showed the benefits of completing nebulised challenges in respiratory patients in primary care settings to alleviate pressures in secondary care, as it appears to be a safe intervention. The Torralba García et al. [70] study disclosed a desaturation-distance relation that showed prognostic value for survival in pre-transplant patients with haematopoietic stem cells. Hussain et al. [71] demonstrated a relationship between the automation process in blood monitoring of people with ILD under antifibrotic therapy and a high degree of engagement and satisfaction. Concerning breathlessness, Morris et al. [72] found that fan therapy may relieve breathlessness in fibrotic ILD. Finally, Gray-ffrench et al. [73] reviewed the literature on the outcomes of indoor and outdoor aeroallergen exposure in type 2-high childhood asthma and treatment strategies to address them. Portela Ferreño et al. [74] studied sleep length and level of knowledge on sleep disorders. Participants reported a low sleep duration (5.6±1.9 h) and 45% were not acquainted with sleep disorders. The authors reflected on the educational role of nursing staff specialised in sleep.
FIGURE 1.
Survival curves, log-rank test and multivariate Cox proportional hazards model. Survival curves with the log-rank test according to a) the bronchiectasis severity index (BSI) and b) previous hospitalisations. c) Cox proportional hazards model. PA: Pseudomonas aeruginosa; AIC: Akaike information criterion; BE: bronchiectasis exacerbation. *: p<0.05. Reproduced and modified from [67] with permission.
Health policies
John et al. [75] found a significant inconsistency in clean air policies of schools across district councils in England and claimed that improving this is a priority for childhood respiratory health. Bagnasco et al. [76] studied workplace violence in nurses working in hospital pneumology settings, concluding that public health companies should invest in resources to manage and prevent it. Related to this finding, Kovačević et al. [77] showed that work stressors are undoubtedly related to the development of burnout syndrome and can lead to changing the workplace and occupation. Therefore, the priority of healthcare institutions should be actions directed at recognising and reducing job stressors.
To optimise respiratory patient care and safety, Loua Henriksen et al. [78] aimed to develop a core competency-based curriculum to meet the educational needs of respiratory nurses that will optimise respiratory patient care and safety in Denmark.
Take-home messages
Nursing-specific interventions are shown to be effective in managing respiratory diseases.
Research, education and monitoring are crucial to improve nursing skills regarding patients’ treatment.
The development of an international curriculum in respiratory nursing is of utmost importance so that every patient can have access to the best possible care.
Group 9.04: psychologists and behavioural scientists
Best abstracts from psychologists and behavioural scientists
People who are confronted with a chronic respiratory disease often find it difficult to manage the functional and instrumental limitations, as well as to change behavioural lifestyles. Over the past few years, COVID-19 has confronted them with additional emotional triggers that lead to psychological distress, anxiety and/or depression. This thematic poster session included the highest-scored abstracts submitted to Group 9.04, organised in three main topics: bridge between neural processing of respiratory sensations, development of new tools and treatment adherence; e-health interventions; and post-COVID-19 challenges.
Bridge between neural processing of respiratory sensations, development of new tools and treatment adherence
COPD symptoms like dyspnoea can be influenced by fear, anxiety, and depression [79]. Vanden Bossche et al. [80] showed how high dyspnoea-specific fear is associated with the perception and the neural processing of respiratory sensations, while Denutte et al. [81] found a common neural mechanism for different qualities of dyspnoea.
These aspects can significantly impact on the types of psychological assistance requests, often related to depressive disorders, poor coping strategies, and non-adherence to therapy [82]. To improve management of respiratory diseases like COPD, a proactive, patient-centred approach should be taken, involving co-development of a standard of care and increasing patient awareness and understanding of their condition to empower them to lead a high-quality life [83], in a multidisciplinary environment [84].
In doing so, it is first of all important to develop a thorough medical history, considering risk factors such as smoking addiction. Farver-Vestergaard et al. [85] found that smoking addiction is not investigated in 23.6% of cases and not examined in depth by professionals in 42.5% of cases, despite its possible consequences. In addition, Frølund et al. [86] suggested measuring patient participation in consultations, by drawing The Activity Barometer. Similarly, Pagnini et al. [87] developed a new instrument to detect implicit and explicit illness expectations in individuals with asthma, the Illness Expectations Test [88], finding that these expectations can influence asthma progression and adherence. Finally, d'Ancona et al. [89] emphasised that to effectively support patients’ transition to inhalers with a lower global warming potential, physicians must recognise patients’ individual choices and concerns about the effectiveness of the new inhaler on their asthma control.
e-Health interventions
Verkleij et al. [90] developed the first therapist-guided internet-delivered cognitive behavioural therapy intervention for depression/anxiety in adults with cystic fibrosis. Their study demonstrated the feasibility, acceptability, and efficacy of the training, with 90% improvement in both anxiety and depression scores. In their systematic review, Vaseur et al. [91] identified risk, benefit, self-efficacy and patient understanding as important shared decision-making tools and clinical decision support systems [92], which are crucial for shaping the roles of patients and healthcare professionals in decision-making.
Post-COVID-19 challenges
Boros et al. [93], in line with O'Donnell et al. [94] and Ledesma et al. [95], reported gender differences in the experience of psychological distress following COVID-19, with women being more affected than men [96]. Other studies found a high prevalence of post-traumatic stress disorder (PTSD), anxiety, and depression even 3 months after discharge from hospital [97], with the need for long-term monitoring [98].
Baltazar et al. [99] found that individuals with low anxiety exhibited effective psychophysiological adaptation. Rosas Trujillo et al. [100] reported that patients who were conscious during hospitalisation and did not undergo invasive mechanical ventilation (IMV) were more at risk of developing PTSD than those with IMV who were sedated [101]. Moreover, Casarin López et al. [102] and Rosas Trujillo et al. [103] found a high prevalence of probable mild cognitive impairment in patients as early as 9 months after discharge, in contrast to those with IMV who had a recovery time of 3–6 months and presented difficulties in the executive and memory domains [104]. As possible treatments, Peláez-Hernádez et al. [105] implemented an eight-session virtual mindfulness-based cognitive therapy to reduce emotional distress and IL-6 levels [106].
Take-home messages
Psychological distress, anxiety, and adherence to proposed treatments are among the main components of the psychological needs of people with respiratory diseases.
The development of e-health interventions and recent measurement tools suggests a focus on patient involvement, adherence, expectations and environment.
COVID-19 further emphasises the need to monitor patients’ psychological well-being, with attention to certain symptoms, such as those of PTSD, as well as the development of cognitive impairment even several months after discharge.
Final remarks
This Highlights article provides valuable insight into the latest scientific data and clinical insights gained from several sessions presented at the 2022 ERS Congress, hoping to inspire readers to keep up to date in their areas of interest. We look forward to seeing you in Milan in 2023 for another successful ERS Congress!
Footnotes
Provenance: Commissioned article, peer reviewed.
Conflict of interest: E. Volpato received the ERS Young Scientist Sponsorship for her abstract entitled “Asthma expectations predict symptoms over time: a longitudinal cohort study” at the ERS International Congress 2022, outside the submitted work; and is an Affiliate Member Representative for the Clinical and Dynamic Psychology Section of the Italian Psychology Association (2020–2022) (unpaid), outside the submitted work.
Conflict of interest: A. Nyberg reports grants or contracts from the Swedish Heart and Lung Foundation, and Strategic Grant – Umeå University, outside the submitted work.
Conflict of interest: A. Šajnić reports grants or contracts from the Association of Respiratory Nurse Specialists (ARNS), outside the submitted work; payment or honoraria from Roche, outside the submitted work; and participation on an advisory board for AstraZeneca, outside the submitted work; and is a Professional Advisory Committee Member at the European Lung Foundation and Chair of the International Coalition of Respiratory Nurses.
Conflict of interest: J. Cruz is an associate editor of this journal.
Conflict of interest: The remaining authors have nothing to disclose.
Support statement: C. Paixão's work is supported by Fundação para a Ciência e a Tecnologia (PhD grant SFRH/BD/148741/2019), Programa Operacional de Competitividade e Internacionalização through Fundo Europeu de Desenvolvimento Regional (POCI-01-0145-FEDER-007628) and under the project UIDB/04501/2020. J. Cruz acknowledges the support of the Center for Innovative Care and Health Technology, funded by Portuguese national funds provided by Fundação para a Ciência e Tecnologia (UIDB/05704/2020).
References
- 1.Radtke T, Crook S, Kaltsakas G, et al. ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur Respir Rev 2019; 28: 180101. doi: 10.1183/16000617.0101-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mcarthur S, Macleod J, Baxter S, et al. Transition to a physiologist led cardiopulmonary exercise testing (CPET) service and evaluation of one year outcomes. Eur Respir J 2022; 60: Suppl. 66, 710. [Google Scholar]
- 3.Ben Salah N, Mrassi H, Blibech H, et al. Cardiopulmonary exercise test and risk assessment in lung resection surgery: a Tunisian experience. Eur Respir J 2022; 60: Suppl. 66, 3560. [Google Scholar]
- 4.Rath AK, Kumar V, Sahu D, et al. Effects of tidal expiratory flow limitation on lung functions, exercise limitation and symptoms severity in stable COPD. Eur Respir J 2022; 60: Suppl. 66, 1134. [Google Scholar]
- 5.Ong-Salvador R, Jak P, Bekkema R, et al. The role of transcutaneous carbon dioxide measurement during exercise. Eur Respir J 2022; 60: Suppl. 66, 2294. [Google Scholar]
- 6.Vesteng LK, Karlsen CG, Grongstad A. Comparing peripheral capillary oxygen saturation during a six-minute walk test with arterial saturation during a cardiopulmonary exercise test. Eur Respir J 2022; 60: Suppl. 66, 1825. [Google Scholar]
- 7.de Vreede CC. Recovery after histamine provocation: predictive power of gender and body mass index. Eur Respir J 2022; 60: Suppl. 66, 980. [Google Scholar]
- 8.Steenbruggen I, De Laat P. Methacholine challenge: safety of the quadrupling protocol. Eur Respir J 2022; 60: Suppl. 66, 1063. [Google Scholar]
- 9.Coates AL, Wanger J, Cockcroft DW, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J 2017; 49: 1601526. doi: 10.1183/13993003.01526-2016 [DOI] [PubMed] [Google Scholar]
- 10.Holland AE, Cox NS, Houchen-Wolloff L, et al. Defining modern pulmonary rehabilitation. An official American Thoracic Society workshop report. Ann Am Thorac Soc 2021; 18: e12–e29. doi: 10.1513/AnnalsATS.202102-146ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Souto-Miranda S, Vaes AW, Gloeckl R, et al. International perspectives on outcome measurement in pulmonary rehabilitation of people with COPD: a qualitative study. Respir Med 2022; 201: 106936. doi: 10.1016/j.rmed.2022.106936 [DOI] [PubMed] [Google Scholar]
- 12.Demeyer H, Louvaris Z, Frei A, et al. Physical activity is increased by a 12-week semiautomated telecoaching programme in patients with COPD: a multicentre randomised controlled trial. Thorax 2017; 72: 415–423. doi: 10.1136/thoraxjnl-2016-209026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oliveira A, Quach S, Alsubheen S, et al. Rapid access rehabilitation after exacerbations of COPD – a qualitative study. Respir Med 2021; 186: 106532. doi: 10.1016/j.rmed.2021.106532 [DOI] [PubMed] [Google Scholar]
- 14.Wuyts M, Blondeel A, Breuls S, et al. Hybrid pulmonary rehabilitation versus conventional outpatient pulmonary rehabilitation: a propensity-matched analysis. Eur Respir J 2022; 60: Suppl. 66, 2860. [Google Scholar]
- 15.Alison JA, McKeough ZJ, Johnston K, et al. Australian and New Zealand Pulmonary Rehabilitation Guidelines. Respirology 2017; 22: 800–819. doi: 10.1111/resp.13025 [DOI] [PubMed] [Google Scholar]
- 16.Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013; 68: Suppl. 2, ii1–ii30. doi: 10.1136/thoraxjnl-2013-203808 [DOI] [PubMed] [Google Scholar]
- 17.Marciniuk DD, Brooks D, Butcher S, et al. Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease – practical issues: a Canadian Thoracic Society Clinical Practice Guideline. Can Respir J 2010; 17: 159–168. doi: 10.1155/2010/425975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013; 188: e13–e64. doi: 10.1164/rccm.201309-1634ST [DOI] [PubMed] [Google Scholar]
- 19.Bishop J, Spencer L, Dwyer T, et al. Does an 8-week pulmonary rehabilitation (PR) program have equivalent outcomes to a 12-week program in COPD? A randomised controlled trial. Eur Respir J 2022; 60: Suppl. 66, 2787. [Google Scholar]
- 20.Watz H, Pitta F, Rochester CL, et al. An official European Respiratory Society statement on physical activity in COPD. Eur Respir J 2014; 44: 1521–1537. doi: 10.1183/09031936.00046814 [DOI] [PubMed] [Google Scholar]
- 21.Gimeno-Santos E, Frei A, Steurer-Stey C, et al. Determinants and outcomes of physical activity in patients with COPD: a systematic review. Thorax 2014; 69: 731–739. doi: 10.1136/thoraxjnl-2013-204763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax 2006; 61: 772–778. doi: 10.1136/thx.2006.060145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yohannes AM, Baldwin RC, Connolly M. Mortality predictors in disabling chronic obstructive pulmonary disease in old age. Age Ageing 2002; 31: 137–140. doi: 10.1093/ageing/31.2.137 [DOI] [PubMed] [Google Scholar]
- 24.Nishiyama O, Yamazaki R, Sano H, et al. Physical activity in daily life in patients with idiopathic pulmonary fibrosis. Respir Investig 2018; 56: 57–63. doi: 10.1016/j.resinv.2017.09.004 [DOI] [PubMed] [Google Scholar]
- 25.Cordova-Rivera L, Gibson PG, Gardiner PA, et al. A systematic review of associations of physical activity and sedentary time with asthma outcomes. J Allergy Clin Immunol Pract 2018; 6: 1968–1981.e2. doi: 10.1016/j.jaip.2018.02.027 [DOI] [PubMed] [Google Scholar]
- 26.Marklund S, Sörlin A, Stenlund T, et al. The importance of feeling in control – people with COPD's experiences regarding maintaining or increasing physical activity when using an eHealth tool. A grounded theory analysis. Eur Respir J 2022; 60: Suppl. 66, 3029. [Google Scholar]
- 27.Breuls S, Blondeel A, Wuyts M, et al. Physical activity coaching in patients with ILD: a pilot study. Eur Respir J 2022; 60: Suppl. 66, 2447. [Google Scholar]
- 28.Paixão C, Ferreira P, Mendes MA, et al. iLiFE-Lifestyle Integrated Functional Exercise for people with interstitial lung disease: a feasibility study. Eur Respir J 2022; 60: Suppl. 66, 1640. [DOI] [PubMed] [Google Scholar]
- 29.Freitas P, Passos NF, Cukier A, et al. Behavior change to increase physical activity reduces sleep disturbances in asthma: a randomized controlled trial. Eur Respir J 2022; 60: Suppl. 66, 4207. [DOI] [PubMed] [Google Scholar]
- 30.Rodrigues G, Afreixo V, Souto-Miranda S, et al. Clusters of functional status in COPD: an exploratory analysis. Eur Respir J 2022; 60: Suppl. 66, 3182. [Google Scholar]
- 31.Samuel Santos E, Rodrigues G, Souto-Miranda S, et al. Anxiety and depression symptoms after pulmonary rehabilitation in people with interstitial lung disease: responders and non-responders. Eur Respir J 2022; 60: Suppl. 66, 3523. [Google Scholar]
- 32.Quadflieg K, Higgins R, Criel M, et al. Prognostic value of the 1-minute sit-to-stand test on postoperative complications in people with lung cancer elected for lung surgery. Eur Respir J 2022; 60: Suppl. 66, 4585. [Google Scholar]
- 33.Souto-Miranda S, van 't Hul AJ, Vaes AW, et al. Differences in pulmonary and extra-pulmonary traits between women and men with chronic obstructive pulmonary disease. J Clin Med 2022; 11: 3680. doi: 10.3390/jcm11133680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tanguay S, Saey D, Nyberg A, et al. Reference equations for quadriceps function in COPD: a multicenter study. Eur Respir J 2022; 60: Suppl. 66, 1204. [Google Scholar]
- 35.Diciolla NS, García-Pascual Abad D, Ampuero López A, et al. Fatigue and functional capacity post COVID-19. Eur Respir J 2022; 60: Suppl. 66, 2340. [Google Scholar]
- 36.Arents E, Hermans F, Salhi B, et al. The impact of Covid-19 on physical activity one year after hospital discharge. Eur Respir J 2022; 60: Suppl. 66, 3550. [Google Scholar]
- 37.Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020; 54: 1451–1462. doi: 10.1136/bjsports-2020-102955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lima Souza Saldanha MF, Costa Souza V, Lafetá Lima M, et al. Respiratory muscle strength in patients post infection by COVID-19. Eur Respir J 2022; 60: Suppl. 66, 3045. [Google Scholar]
- 39.Silveira J, Hayashi M, Pires R, et al. Telemonitoring of home mechanical ventilation in Brazil: clinical and economical outcomes in a private Brazilian home care. Eur Respir J 2022; 60: Suppl. 66, 4591. [Google Scholar]
- 40.Murray B. An exploration of the experiences of respiratory clinical nurse specialists (CNS) and advance nurse practitioners (ANP) in Irish healthcare settings. Eur Respir J 2022; 60: Suppl. 66, 1797. [Google Scholar]
- 41.Stridsman C, Zakrisson A, Sterner T. Nurses specialized through higher education in asthma, allergy and COPD. Experiences from a Swedish perspective – a winning concept for the clinic. Eur Respir J 2022; 60: Suppl. 66, 153. [Google Scholar]
- 42.Dos Santos Castro Padilha JM, Silva RP, Macedo F, et al. International curriculum for nurses working with respiratory patients – why do we need it? A Portuguese perspective. Eur Respir J 2022; 60: Suppl. 66, 2038. [Google Scholar]
- 43.Heslop-Marshall K, King J, Wheatley I, et al. The International Coalition of Respiratory Nurses (IRCN): development of a curriculum towards advanced nursing education and improvements in care. Eur Respir J 2022; 60: Suppl. 66, 606. [Google Scholar]
- 44.Roberts NJ, Renwick M, Welch L, et al. How confident are nursing students about their respiratory knowledge and assessment skills? Eur Respir J 2022; 60: Suppl. 66, 119. doi: 10.1183/13993003.01686-2022 [DOI] [Google Scholar]
- 45.Sajnic A, Narsavage G, Karabatic S, et al. An International Curriculum for Respiratory Nurses (ICRN): supporting standardized respiratory nursing education in Croatia. Eur Respir J 2022; 60: Suppl. 66, 682. [Google Scholar]
- 46.Sajnic A, Cukljek S, Rezic S, et al. Respiratory nursing training in Croatia. Breathe 2018; 14: 246–247. doi: 10.1183/20734735.019418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Proglas Sestrinstva Republike Hrvatske 2020 [Proclamation of nursing of the Republic of Croatia 2020]. www.hkms.hr/wp-content/uploads/2020/02/Proglas-hrvatskog-sestrinstva-2020.pdf
- 48.Çevik Akyıl R, Oğuz G, Kıymaç Sarı M, et al. Developing an International Curriculum for respiratory nurses and the need for a curriculum in Turkey. Eur Respir J 2022; 60: Suppl. 66, 2521. [Google Scholar]
- 49.Narsavage G, Šajnić A, Kelly C, et al. Development of an international curriculum for respiratory nurses (ICRN): a global needs survey. Eur Respir J 2022; 60: Suppl. 66, 204. [Google Scholar]
- 50.Šajnić A, Kelly C, Smith S, et al. Need and baseline for harmonising nursing education in respiratory care: preliminary results of a global survey. Breathe 2022; 18: 210172. doi: 10.1183/20734735.0172-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Loddenkemper R, Séverin T, Eiselé J-L, et al. HERMES: a European Core Syllabus in Respiratory Medicine. Breathe 2006; 3: 59–69. doi: 10.1183/18106838.0301.59 [DOI] [Google Scholar]
- 52.Sajnic A, Narsavage G, Kelly C, et al. Steps in the development of an international curriculum for respiratory nurses (ICRN): a Delphi Process plan to standardise levels of respiratory nursing education. Eur Respir J 2022; 60: Suppl. 66, 515. [Google Scholar]
- 53.Murray B, Smith S, Roberts N, et al. Existing respiratory nursing curriculum, frameworks, and other documentation relevant to respiratory nursing education: A Scoping Review Protocol. OSF Registries, 2022. 10.17605/OSF.IO/6DRFG [DOI]
- 54.Rezelj M, Tršan J, Počvavšek I, et al. Comparing results of the Asthma Control Test and Severe Asthma Quality of life Questionnaire in patients with severe asthma on biologics. Eur Respir J 2022; 60: Suppl. 66, 2234. [Google Scholar]
- 55.Miranda Valladares S, Gonzalez Sanchez B, Entrambasaguas Martin M, et al. Impact on the quality of life of patients with COPD after three non-pharmacological interventions. Eur Respir J 2022; 60: Suppl. 66, 562. [Google Scholar]
- 56.Refsgaard Iversen B, Rodkjaer L, Bregnballe V, et al. The impact on number of hospitalizations and length of hospital stay for patients with advanced COPD affiliated with a cross-sectorial lung team. Eur Respir J 2022; 60: Suppl. 66, 880. [Google Scholar]
- 57.Bech CS, Poulsen I, Nørholm V, et al. Patients’ experience of automated oxygen administration during hospitalization with acute exacerbation in COPD – a qualitative study. Eur Respir J 2022; 60: Suppl. 66, 1574. [DOI] [PubMed] [Google Scholar]
- 58.Granados Santiago M, González Dueñas J, Calvache Mateo A, et al. Pain perception in COPD patients across the COVID-19 pandemic. Eur Respir J 2022; 60: Suppl. 66, 3575. [Google Scholar]
- 59.Miranda Valladares S, Entrambasaguas Martin M, Gonzalez Sanchez B, et al. Lockdown impact in patients with severe and very severe COPD. Eur Respir J 2022; 60: Suppl. 66, 627. [Google Scholar]
- 60.Silva L, Maricoto T, Costa P, et al. Pulmonary rehabilitation maintenance programmes: what makes the difference? Eur Respir J 2022; 60: Suppl. 66, 226. [Google Scholar]
- 61.Alves Vaz SF, Loureiro AI, Rodrigues RQ, et al. Pulmonary telerehabilitation in the COVID era – pilot program. Eur Respir J 2022; 60: Suppl. 66, 2645. [Google Scholar]
- 62.Martín Núñez J, Navas Otero A, López López P, et al. Cognitive impairment in long COVID syndrome patients one year after infection. Eur Respir J 2022; 60: Suppl. 66, 3967. [Google Scholar]
- 63.Carrera Cueva C, Domínguez Blasco M, Ruiz Serrano De La Espada MR, et al. Respiratory nursing post-COVID consultation. Eur Respir J 2022; 60: Suppl. 66, 1653. [Google Scholar]
- 64.Silva L, Rodrigues L. Effectiveness of the “AsmaSemCrise” programme in asthma control. Eur Respir J 2022; 60: Suppl. 66, 227. [Google Scholar]
- 65.Miranda Valladares S, Perez Redondo M, Entrambasaguas Martin M, et al. The effect of the respiratory rehabilitation depends on the level of anxiety and depression. Eur Respir J 2022; 60: Suppl. 66, 577. [Google Scholar]
- 66.Keramida E, Bellou E, Bracka I, et al. Abdominal haematomas following subcutaneous heparin injections in COVID19 patients; food for thought in daily practice. Eur Respir J 2022; 60: Suppl. 66, 4314. [Google Scholar]
- 67.Bueno Freire L, Alcaraz Serrano V, Vázquez Burgos N, et al. Exacerbation risk factors in bronchiectasis colonized by Pseudomonas aeruginosa. Eur Respir J 2022; 60: Suppl. 66, 2205. [Google Scholar]
- 68.Yu T, Lin H, Qin Z, et al. Performance of the modified viral and bacterial filter during aerosol inhalation therapy. Eur Respir J 2022; 60: Suppl. 66, 743. [Google Scholar]
- 69.Bettany M. Nebulised medications in secondary care: rising to the challenge. Eur Respir J 2022; 60: Suppl. 66, 3610. [Google Scholar]
- 70.Torralba García Y, Alsina Restoy X, Torres Castro R, et al. Prognostic value of the distance walked in the 6-minute walk test and the desaturation-distance ratio (DDR) in patients who will receive hematopoietic stem-based transplantation (HSCT). Eur Respir J 2022; 60: Suppl. 66, 3662. [Google Scholar]
- 71.Hussain S, Ruggiero C, Parsons K, et al. Patient perspective on antifibrotic monitoring – impact on management at a single UK prescribing centre. Eur Respir J 2022; 60: Suppl. 66, 2877. [Google Scholar]
- 72.Morris H, Zakis K, Swale J, et al. Effectiveness of fan therapy in breathlessness management in fibrotic interstitial lung disease. Eur Respir J 2022; 60: Suppl. 66, 164. [Google Scholar]
- 73.Gray-ffrench M, Sinha I, Abrams E, et al. A literature review of allergen management in children with type 2-high asthma. Eur Respir J 2022; 60: Suppl. 66, 4300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Portela Ferreño MI, Piñeiro Lopez A, Pastor Campo A, et al. How much do we sleep and how much do we know about sleep? Eur Respir J 2022; 60: Suppl. 66, 661. [Google Scholar]
- 75.John C, Lawrence B, Sinha I, et al. Audit of council-level clean air policies for schools in England. Eur Respir J 2022; 60: Suppl. 66, 4268. [Google Scholar]
- 76.Bagnasco A, Catania G, Pagnucci N, et al. Nurses with workplace violence in pneumology settings during Covid-19. Eur Respir J 2022; 60: Suppl. 66, 3538. [Google Scholar]
- 77.Kovačević T, Zaric B, Mikov I, et al. Managing patients with respiratory diseases: burnout among HCP. Eur Respir J 2022; 60: Suppl. 66, 3527. [Google Scholar]
- 78.Loua Henriksen S, Albrectsen Paine M, Sandau Bech C, et al. Development of a core competency-based curriculum in respiratory nursing – a nationwide Delphi study. Eur Respir J 2022; 60: Suppl. 66, 1040. [Google Scholar]
- 79.Miravitlles M, Ribera A. Understanding the impact of symptoms on the burden of COPD. Respir Res 2017; 18: 67. doi: 10.1186/s12931-017-0548-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vanden Bossche L, Denutte Y, Reijnders T, et al. Neural processing of respiratory sensations during resistive load-induced dyspnea in patients with COPD. Eur Respir J 2022; 60: Suppl. 66, 2172. [Google Scholar]
- 81.Denutte Y, Holk T, Janssens W, et al. Comparable neural gating of respiratory sensations during increasing dyspnea across different qualities of dyspnea. Eur Respir J 2022; 60: Suppl. 66, 3665. [Google Scholar]
- 82.Hussein H, Fellows J, Marsh J, et al. Patterns of psychological conditions presenting to a severe asthma psychology service. Eur Respir J 2022; 60: Suppl. 66, 2763. [Google Scholar]
- 83.Hurst JR, Winders T, Worth H, et al. A patient charter for chronic obstructive pulmonary disease. Adv Ther 2021; 38: 11–23. doi: 10.1007/s12325-020-01577-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Koff PB, Min SJ, Freitag TJ, et al. Impact of proactive integrated care on chronic obstructive pulmonary disease. Chronic Obstr Pulm Dis 2021; 8: 100–116. doi: 10.15326/jcopdf.2020.0139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Farver-Vestergaard I, Hjorth P, Løkke A. Smoking cessation support in a hospital-based healthcare setting: the provider perspective. Eur Respir J 2022; 60: Suppl. 66, 1943. [Google Scholar]
- 86.Frølund J, Farver-Vestergaard I, Poulsen H, et al. Using The Activity Barometer (TAB) to assess patient participation in diagnostic consultations. Eur Respir J 2022; 60: Suppl. 66, 879. [Google Scholar]
- 87.Pagnini F, Volpato E, Poletti V, et al. Asthma expectations predict symptoms over time: a longitudinal cohort study. Eur Respir J 2022; 60: Suppl. 66, 1616. [Google Scholar]
- 88.Pagnini F, Volpato E, Dell'Orto S, et al. Illness expectations assessment in people with asthma: a tool for explicit and implicit beliefs. J Asthma Allergy 2021; 14: 449–455. doi: 10.2147/JAA.S307763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.d'Ancona G, Sethi K, Holman N, et al. What do people with asthma think about switching to a more environmentally friendly inhaler? Eur Respir J 2022; 60: Suppl. 66, 3143. [Google Scholar]
- 90.Verkleij M, Georgiopoulos A, Barendrecht H, et al. Pilot of a therapist-guided internet-delivered cognitive behavioral therapy intervention for anxiety and depression (eHealth CF-CBT) in Dutch adults with cystic fibrosis. Eur Respir J 2022; 60: Suppl. 66, 729. [Google Scholar]
- 91.Vaseur R, Te Braake E, Beinema T, et al. Technology-supported shared decision-making in chronic conditions: preliminary results of a systematic review. Eur Respir J 2022; 60: Suppl. 66, 2987. [DOI] [PubMed] [Google Scholar]
- 92.Shneiderman B. A taxonomy and rule base for the selection of interaction styles. In: Baecker RM, Grudin J, Buxton WAS, et al., eds. Readings in Human–Computer Interaction: Toward the Year 2000. 2nd Edn. San Francisco, Morgan Kaufmann Publishers, 1995; pp. 401–410. [Google Scholar]
- 93.Boros A, Martusewicz-Boros M, Boros P, et al. Relationship between COVID-19 consequences and subjective distress 6 months after hospitalization. Eur Respir J 2022; 60: Suppl. 66, 2626. [Google Scholar]
- 94.O'Donnell SE, Croce G, Mandurino Mirizzi F, et al. Pain, fatigue and psychological sequelae in patients surviving COVID-19: results from a prospective observational controlled study. Eur Respir J 2022; 60: Suppl. 66, 4227. [Google Scholar]
- 95.Ledesma C, Peláez-Hernández V, Luna-Rodríguez L, et al. Sleep disturbances in post-Covid patients as a function of sex. Eur Respir J 2022; 60: Suppl. 66, 3385. [Google Scholar]
- 96.Zhang W, Walkover M, Wu YY. The challenge of COVID-19 for adult men and women in the United States: disparities of psychological distress by gender and age. Public Health 2021; 198: 218–222. doi: 10.1016/j.puhe.2021.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Luna Rodríguez GL, Peláez-Hernández V, Orea-Tejeda A, et al. Posttraumatic-stress disorder, and others psychological impairment in COVID-19 surviving patients. Eur Respir J 2022; 60: Suppl. 66, 3325. [Google Scholar]
- 98.Tu Y, Zhang Y, Li Y, et al. Post-traumatic stress symptoms in COVID-19 survivors: a self-report and brain imaging follow-up study. Mol Psychiatry 2021; 26: 7475–7480. doi: 10.1038/s41380-021-01223-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Baltazar V, Peláez-Hernández V, Casarín-López F, et al. Heart rate variability in post-COVID-19 patients with different anxiety levels. Eur Respir J 2022; 60: Suppl. 66, 3354. [Google Scholar]
- 100.Rosas Trujillo A, Baltazar Chávez V, Peláez Hernández V, et al. Psychological affectation in surviving patients of COVID-19, consideration of the use of invasive mechanical ventilation. Eur Respir J 2022; 60: Suppl. 66, 4234. [Google Scholar]
- 101.Tarsitani L, Vassalini P, Koukopoulos A, et al. Post-traumatic stress disorder among COVID-19 survivors at 3-month follow-up after hospital discharge. J Gen Intern Med 2021; 36: 1702–1707. doi: 10.1007/s11606-021-06731-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Casarin López F, Pelaéz Hernandez V, Luna Rodriguez GL, et al. Cognitive alterations in COVID-19 survivors with and without invasive mechanical ventilation during hospital stay. Eur Respir J 2022; 60: Suppl. 66, 3897. [Google Scholar]
- 103.Rosas Trujillo A, Casarín López F, Baltazar Chávez V, et al. Cognitive impairment as a sequel to SARS-CoV-2 infection. Eur Respir J 2022; 60: Suppl. 66, 4245. [Google Scholar]
- 104.Hampshire A, Trender W, Chamberlain SR, et al. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine 2021; 39: 101044. doi: 10.1016/j.eclinm.2021.101044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Peláez-Hernádez V, Luna Rodríguez GL, Domínguez-Trejo B, et al. Effects of a brief behavioural cognitive e-therapy for emotional alterations, and inflammation in COVID-19 survivors. Eur Respir J 2022; 60: Suppl. 66, 3330. [Google Scholar]
- 106.Wahlund T, Mataix-Cols D, Olofsdotter Lauri K, et al. Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 pandemic: a randomised controlled trial. Psychother Psychosom 2021; 90: 191–199. doi: 10.1159/000512843 [DOI] [PMC free article] [PubMed] [Google Scholar]