SUMMARY
OBJECTIVE:
The aim of this study was to systematically review the colic and sleep outcomes of nonpharmacological intervention in infants with infantile colic and perform a meta-analysis of the available evidence.
METHODS:
The literature review for this systematic review was conducted between December 2022 and January 2023 using five electronic databases, namely PubMed, CINAHL, Scopus, Web of Science, and ULAKBİM. Published articles were scanned using MeSH-based keywords. Only randomized controlled trials conducted in the past 5 years were included. The data were analyzed using the Review Manager computer program.
RESULTS:
This meta-analysis included three studies involving a total of 386 infantile colic infants. After nonpharmacological treatment, it was found that infants with infantile colic reduced crying time (standardized mean difference: 0.61; 95%CI 0.29–0.92; Z=3.79; p=0.00002), improved sleep duration (standardized mean difference: 0.22; 95%CI −0.04 to 0.48; Z=1.64; p=0.10), and decreased crying intensity (mean difference: −17.24; 95%CI −20.11 to 14.37; Z=11.77; p<0.000001).
CONCLUSION:
According to the meta-analysis findings, it was determined that the risk of bias was low in the studies included and that nonpharmacological chiropractic, craniosacral, and acupuncture treatments applied to infantile colic infants in the three included studies reduced crying time and intensity and increased sleep duration.
KEYWORDS: Crying, Chiropractic, Acupuncture therapy
INTRODUCTION
Infantile colic (IC) is characterized by excessive crying and restlessness in babies who develop normally from all other directions 1–3 . IC is a common condition that occurs in 25% of infants 4 . Wessel et al. 5 were the first to describe the situation with his “rule of three,” that is, the condition in which the infant cries at least 3 times a day for at least 3 days in the previous 3 weeks.
IC adversely affects the comfort and health of both the infants and the parents, and on the contrary, studies are carried out with different therapeutic perspectives because the exact etiology is unknown. In these studies, drug applications and probiotics 6–8 evaluated the efficacy of interventions involving parental behavior and counseling 9 . In addition, complementary medicine practices, which are rapidly gaining popularity, are also being studied. In these studies, acupuncture 10 , reflexology 11 , physiotherapy, and visceral osteopathy have been studied to treat IC such as vertebral manipulation 12 . In the literature, the evidence evaluating the effect of nonpharmacological applications on sleep in infants with IC is limited. For this reason, the aim of this study was to systematically review the colic and sleep outcomes of nonpharmacological intervention in infants with IC and to perform a meta-analysis of the available evidence.
METHODS
In this study, Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement 13 was compiled in the preparation of the systematic review and meta-analysis.
Eligibility criteria
The following criteria (PICOS) were taken into account in the selection of the studies to be included in the study: participant (P): infants with IC. The infants included in the study had the following criteria for inclusion 1 : infants who have cried for at least 3 days for 3 h a day in the past week and 2 who have no health problems. Intervention (I): nonpharmacological methods. Nonpharmacological methods include the following 1 : chiropractic 2 , craniosacral therapy 3 , acupuncture 4 , yoga 5 , massage 6 , swaddling, and 7 shaking. Comparison (C) 1 : placebo and 2 routine care. Results (O): sleep duration, crying intensity, and duration. Study design (S): randomized controlled trials and controlled groups were included. Articles that were not IC, but only had gas complaints, pharmacological and pre-probiotic interventions, and evaluated the effect of the interventions other than sleep and IC intensity were excluded from traditional and systematic reviews.
Search strategy
The literature review for this systematic review was conducted between December 2022 and January 2023 using five electronic databases (PubMed, CINAHL, Scopus, Web of Science, and ULAKBİM). The studies in which the efficacy of nonpharmacological interventions in infants with infants with IC were examined by selecting keywords. The keywords were “baby” OR “newborn” OR “infant” AND “therapy” OR “nonpharmacological” OR “alternative therapy” AND “infantile colic” OR “crying” AND “sleep” AND “crying intensity.” The search strategy was changed according to the characteristics of each database. In addition, reviews on articles included in systematic reference lists and other previous systematic reviews were checked to reach further studies.
The data analysis
Meta-analysis was performed using Review Manager 5.4 (The Nordic Cochrane Center, Copenhagen, Denmark). The heterogeneity between the studies was evaluated using Cochran's Q test and Higgins’ I², and it was accepted that I² greater than 50% showed significant heterogeneity. Accordingly, random effect results were taken into account when I² was greater than 50%, and fixed effect results were taken into account if it was less than the value. Odds ratio for categorical variables, mean difference (MD), and standardized mean difference (SMD) for continuous variables were calculated. MD or SMD, along with the corresponding 95% confidence interval (CI), is appropriately pooled for continuous variables based on whether the results are measured on the same scales. All tests were calculated from two-pronged tests, and a p-value of less than 0.05 was considered statistically significant. The quality of the articles in randomized controlled trials and the Version 2 of the Cochrane Risk-of-Bias (RoB-2) tool were used for randomized trials.
RESULTS
Literature review
The PRISMA flowchart is summarized for literature review and selection. A total of 15 studies were reached through electronic database search and manual search. All 15 articles whose full texts could be accessed were examined. Titles and abstracts were read to identify relevant articles; two articles were excluded because of review articles, protocols, replicates, different populations, and not meeting the inclusion criteria. The remaining 13 full texts were evaluated for suitability. Three randomized controlled trial (RCT) articles were included in the quantitative synthesis as they met the required criteria (Table 1). The three RCT articles included outline the study.
Table 1. General features of the included studies.
| Author (reference)\Country | Study design | Population | The inclusion and exclusions criteria | Protocol | Comparisons | Drop out | Outcomes | Results |
|---|---|---|---|---|---|---|---|---|
| Holm et al. (2021)14, Denmark | RCT | 185 infant with IC (Interventions group n=96; control group n=89) |
|
|
Control group: Placebo | Interventions group (n=7), Control group (n=7) | Infant Crying, Sleep and Defecation Diary | Duration of crying in the treatment group was reduced by 1.5 h compared with 1 h in the control group, but when adjusted for baseline hours of crying, age, and chiropractic clinic, the difference was not significant. The proportion obtaining a clinically important reduction of 1 h of crying was 63% in the treatment group and 47% in the control group. |
| Castejón-Castejón et al. (2022)15, Spain | RCT | 54 Infant with IC (Interventions group n=29; control group n=25) |
|
|
Control group: IC coping training | Interventions group (n=0), Control group (n=4) | Sleep Diary, Infant Colic Severity Questionnaire | Significant statistical differences were observed in favor of experimental group compared to the control group on day 24 in crying hours’ primary outcome, and also in hours of sleep and colic severity secondary outcomes. Also, the differences between the groups of ≤2 CST sessions, three CST sessions and control were statistically significant on day 24 of the treatment for crying, sleep, and colic severity outcomes. |
| Landgren et al. (2020)10, Sweden | RCT | 147 Infant with IC (Minimal acupuncture n=48, Individual acupuncture n=49, control group n=48) |
|
|
Control group: Placebo | Minimal acupuncture n=2, Individual acupuncture n=0, control group n=1 | Infant Crying and Sleep Diary | There were no differences between groups for stooling, feeding, or sleeping at any time point according to data from the diaries. At the follow-up phone call, more parents in minimal acupuncture and individual acupuncture, control group perceived that feeding and sleep had changed and that the symptoms of colic had improved. |
IC: infantile colic.
Study characteristics
This systematic review and meta-analysis included three studies involving a total of 386 IC infants to assess the impact of nonpharmacological interventions on IC intensity and sleep duration outcomes 10,14,15 . In the interventions for IC described in the articles included in the study, Holm et al. 14 applied chiropractic, Castejón et al. 15 applied craniosacral therapy, and Landgren et al. 10 applied acupuncture. While the intervention period of the studies in the review lasted 2 weeks, Castejón et al. 15 evaluated the first day and the first week of the intervention and ended the intervention if the symptoms regressed. In two of the articles, due to the placebo effect, infants in the control group were called to the clinic and stayed with the specialist for 5 min without their parents 10,14 . In the study by Castejón et al. 15 , the control group was instructed to cope with IC. Nonpharmacological interventions to IC infants in the intervention group, Holm et al. 14 performed chiropractic twice a week for 2 weeks on IC infants in the intervention group. Castejón et al. 15 administered 1–3 sessions of craniosacral therapy to infants in the intervention group depending on the reduction of their symptoms. Landgren et al. 10 performed standard acupuncture at LI4 to a group twice a week for 2 weeks, while one group received traditional acupuncture points at LI4, ST36, or Sifeng, depending on the baby's symptoms, according to the diary. A crying diary and a sleep diary were used in all of the studies, and Castejón et al. 15 measured IC intensity with the Infant Colic Intensity Questionnaire.
Outcomes
The results of the meta-analysis were presented as Forest Pilot. In the included studies, IC was examined with improvement in crying duration, sleep duration, and crying intensity. The results of the research by Landgren et al. 10 were sleep duration and crying after the first and second interventions in the beginning. The Infant Pubic Intensity Per Day Questionnaire assessed sleep duration, crying time, sleep time, and being happy while awake before and after all interventions.
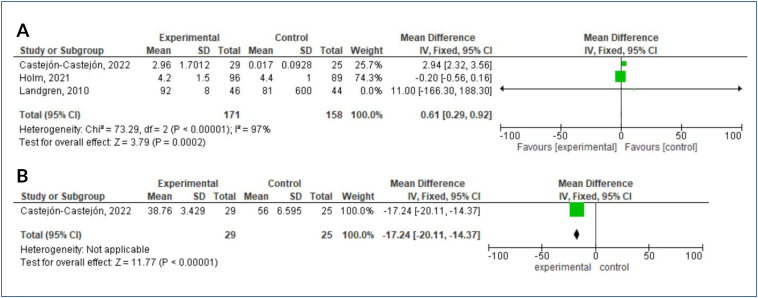
In three studies reviewed, the authors reported results on crying duration in the pre- and post-treatment periods. While the mean combined results of the studies did not differ in the post-treatment groups (SMD: 0.61, 95%CI 0.29–0.92, Z=3.79, p=0.00002), the effect of nonpharmacological treatment on crying time showed a significant difference between the groups (Figure 1A). In one study reviewed, the authors reported results on crying intensity in the pre- and post-treatment periods. The combined results of the studies showed that after treatment (MD: −17.24, 95%CI: −20.11 to 14.37, Z=11.77, p<0.000001), the effect of nonpharmacological treatment on crying intensity was significantly different between the groups and its intensity decreased (Figure 1B).
Figure 1. The results of the meta-analysis of the effect of nonpharmacological therapy on infantile colic crying time: (A) post-treatment and crying duration, and (B) post-treatment and crying intensity.
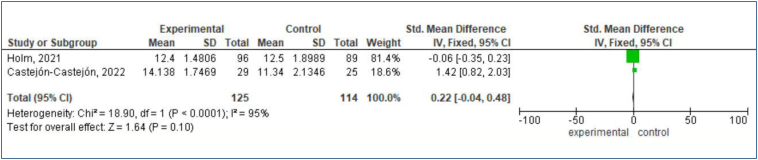
In the two studies examined, the authors reported results regarding sleep duration in the pre- and post-treatment periods. The combined results of the studies showed that while they did not differ in the post-treatment groups (SMD: 0.22, 95%CI: −0.04 to 0.48, Z=1.64, p=0.10), there was a significant difference in the effect of nonpharmacological treatment on sleep duration between the groups (Figure 2).
Figure 2. Results of the meta-analysis of the effect of nonpharmacological treatment on infantile colic sleep duration: post-treatment and sleep duration.
Risk of bias assessment
All the research has identified an adequate method for the random assignment of participants to treatment groups 10,14,15 . Therefore, there is a low risk of nepotism error. All studies reported adequate distribution secrecy using sequentially numbered and sealed opaque envelopes and rated them with a low risk of favoritism error 10,14,15 . In the two studies included in the meta-analysis, participants and researchers could not go blind to the study, so the two studies assessed participants and staff at risk of nepotism by blinding them, and this was taken into account when interpreting the findings 14,15 . Three studies assessed data at low risk as a result of blinding 10,14,15 . In three studies 10,14,15 , the effect has been so small that it has been balanced or not affected by the intervention and control groups to stop working. For this reason, we concluded that the risk of attrition is low. Because they discussed the significant results reported in all study methods, including negative results, and matched those reported in their records, all studies included in the meta-analysis were considered to have a low risk of reporting bias. For each study included, we described important concerns regarding other possible sources of bias that were not previously addressed in the above categories 10,14,15 .
DISCUSSION
This study aimed to systematically review the colic and sleep outcomes of nonpharmacological intervention in infants with IC and make a meta-analysis of the available evidence. According to the meta-analysis findings, the studies included in the analysis were found to have a low risk of bias, and in all three included studies, nonpharmacological chiropractic, craniosacral, and acupuncture treatments applied to IC infants reduced crying time and intensity and increased sleep duration.
Infants with IC begin to cry at the same time every day, and these cries cannot be stopped 1,2 . In a meta-analysis study, prebiotic supplementation was reported to be strong in crying intensity of IC infants, while manual therapies were reported to have weak evidence 16 . In the three studies included in the analysis, crying time was assessed in infants with IC 10,14,15 and also evaluated the intensity of crying in a study 15 . In IC, in addition to the important crying time in infants, the intensity is also important. In this respect, it is thought that there is a weakness in measuring the effectiveness of interventions in two other studies that did not evaluate crying intensity. In addition, in the research, the sleep and crying times of the infants were evaluated by their parents, and they were asked to keep a diary. Parents of infants with IC often have increased levels of anxiety and burnout, and their perception of signs of crying and sleep may be altered 17 . Research suggests that this evaluation cannot be objective. In addition, two studies included the placebo effect in infants in the control group who were called to the clinic and stayed with the specialist for 5 min without their parents 10,14 . This suggests that it reduces bias in the evaluation process between groups.
In infants with IC, crying and attacks usually begin in the evening or at midnight and last for at least 3 h. This situation adversely affects the level and quality of sleep for both the baby and the parents 1,2 . It was found that the nonpharmacological methods used in the studies included in the analysis increased sleep duration. A study reported that IC is reduced in the infants of mothers who massage their infants 2 . In the three studies included in the analysis, IC asked parents to keep a sleep diary to assess sleep duration 10,14,15 . Keeping a stopwatch for the sleep duration of infants is considered quantitative and objective data and can be considered reliable. However, in the studies evaluating sleep in term infants, devices that record the sleep-wake status and duration are used 18 . A study reported that the majority of mothers used medical and complementary therapies together in the treatment of IC and that the rate of mothers benefiting from complementary therapies was higher than medical treatment 2 . In line with these findings, nonpharmacological treatments are preferred by the parents of IC infants, and it is seen that there is weak evidence in line with the results of this meta-analysis. In addition, studies examining the effect of interventions on sleep in infants with IC are very limited.
CONCLUSION
In three studies included in this analysis, chiropractic, craniosacral, and acupuncture treatments for IC infants were found to increase sleep duration while reducing crying duration and intensity. Although there are effective and available methods in IC, the levels of evidence obtained are weak. Randomized, placebo, and double-blind controlled trials with objective assessments such as measurement with more actigraphy to improve sleep in IC infants, which have an important place for infant development, may be recommended.
Footnotes
Funding: none.
REFERENCES
- 1.Karaahmet A, Dolgun G, Özhan M. The effect of probiotics added to maternal nutrition on infantile colic: a systematic review and meta-analysis. J. Pediatr. 2021;30(2):105–116. doi: 10.5336/pediatr.2020-78942. [DOI] [Google Scholar]
- 2.Öztornacı BÖ, Doğan P, Karakul A, Akgül EA, Doğan Z, Sarı HY, et al. Mothers’ experiences with infantile colic of their babies. J Tepecik Educ Res Hosp. 2022;32(3):405–413. [Google Scholar]
- 3.Waikar Y. Infantile colic: an overview. J Neonatal Pediatr. 2018;4(1):1–3. doi: 10.4172/2572-4983.1000153. [DOI] [Google Scholar]
- 4.Wolke D, Bilgin A, Samara M. Systematic review and meta-analysis: fussing and crying durations and prevalence of colic in infants. J Pediatr. 2017;185:55.e4–61.e4. doi: 10.1016/j.jpeds.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 5.Wessel MA, Cobb JC, Jackson EB, Harris GS, Detwiler AC. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics. 1954;14(5):421–435. [PubMed] [Google Scholar]
- 6.Sarasu JM, Narang M, Shah D. Infantile colic: an update. Indian Pediatr. 2018;55(11):979–987. [PubMed] [Google Scholar]
- 7.Zeevenhooven J, Browne PD, L'Hoir MP, Weerth C, Benninga MA. Infant colic: mechanisms and management. Nat Rev Gastroenterol Hepatol. 2018;15(8):479–496. doi: 10.1038/s41575-018-0008-7. [DOI] [PubMed] [Google Scholar]
- 8.Savino F, Quartieri A, Marco A, Garro M, Amaretti A, Raimondi S, et al. Comparison of formula-fed infants with and without colic revealed significant differences in total bacteria, Enterobacteriaceae and faecal ammonia. Acta Paediatr. 2017;106(4):573–578. doi: 10.1111/apa.13642. [DOI] [PubMed] [Google Scholar]
- 9.Wurmser H, Rieger M, Domogalla C, Kahnt A, Buchwald J, Kowatsch M, et al. Association between life stress during pregnancy and infant crying in the first six months postpartum: a prospective longitudinal study. Early Hum Dev. 2006;82(5):341–349. doi: 10.1016/j.earlhumdev.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 10.Landgren K, Hallström I, Tiberg I. The effect of two types of minimal acupuncture on stooling, sleeping and feeding in infants with colic: secondary analysis of a multicentre RCT in Sweden (ACU-COL) Acupunct Med. 2021;39(2):106–115. doi: 10.1177/0964528420920308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al Qahtani AM, Ahmed HM. The effect of educational program for new mothers about infant abdominal massage and foot reflexology for decreasing colic at Najran City. Compr Child Adolesc Nurs. 2021;44(1):63–78. doi: 10.1080/24694193.2020.1740827. [DOI] [PubMed] [Google Scholar]
- 12.Hjern A, Lindblom K, Reuter A, Silfverdal SA. A systematic review of prevention and treatment of infantile colic. Acta Paediatr. 2020;109(9):1733–1744. doi: 10.1111/apa.15247. [DOI] [PubMed] [Google Scholar]
- 13.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1–1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holm LV, Jarbøl DE, Christensen HW, Søndergaard J, Hestbæk L. The effect of chiropractic care on infantile colic: results from a single-blind randomised controlled trial. Chiropr Man Therap. 2021;29(1):15–15. doi: 10.1186/s12998-021-00371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castejón-Castejón M, Murcia-González MA, Todri J, Lena O, Chillón-Martínez R. Treatment of infant colic with craniosacral therapy. a randomized controlled trial. Complement Ther Med. 2022;71:102885–102885. doi: 10.1016/j.ctim.2022.102885. [DOI] [PubMed] [Google Scholar]
- 16.Ellwood J, Draper-Rodi J, Carnes D. Comparison of common interventions for the treatment of infantile colic: a systematic review of reviews and guidelines. BMJ Open. 2020;10(2):e035405. doi: 10.1136/bmjopen-2019-035405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taştekin A. Why do babies cry? J Clin Med Pediatr. 2018;10(4):25–29. [Google Scholar]
- 18.Hysing M, Strand TA, Chandyo RK, Ulak M, Ranjitkar S, Schwinger C, et al. The effect of vitamin B12-supplementation on actigraphy measured sleep pattern; a randomized control trial. Clin Nutr. 2022;41(2):307–312. doi: 10.1016/j.clnu.2021.11.040. [DOI] [PubMed] [Google Scholar]