Abstract
Background
People who inject drugs (PWID) have low rates of COVID-19 testing yet are vulnerable to severe disease. In partnership with a mobile syringe service program (SSP) in San Diego County, CA, we developed the evidence-, community-, and Social Cognitive Theory-informed “LinkUP” intervention (tailored education, motivational interviewing, problem-solving, and planning) to increase COVID-19 testing uptake among PWID.
Purpose
To assess preliminary efficacy of LinkUP in increasing PWID COVID-19 testing in a pilot randomized controlled trial (RCT).
Methods
We referred participants (PWID, ≥18 years old, San Diego County residents who had not recently undergone voluntary COVID-19 testing) to mobile SSP sites that had been randomized (by week) to offer the active LinkUP intervention or didactic attention-control conditions delivered by trained peer counselors. Following either condition, counselors offered on-site rapid COVID-19 antigen testing. Analyses estimated preliminary intervention efficacy and explored potential moderation.
Results
Among 150 participants, median age was 40.5 years, 33.3% identified as Hispanic/Latinx, 64.7% were male, 73.3% were experiencing homelessness, and 44.7% had prior mandatory COVID-19 testing. The LinkUP intervention was significantly associated with higher COVID-19 testing uptake (p < .0001). Homelessness moderated intervention effects; LinkUP increased COVID-19 testing uptake more among participants experiencing homelessness (adjusted risk ratio [aRR]: 1.80; 95% CI: 1.56–2.09; p < .0001) than those not experiencing homelessness (aRR: 1.20; 95% CI: 1.01–1.43; p = .04).
Conclusions
Findings from this pilot RCT support the preliminary efficacy of the “LinkUP” intervention to increase COVID-19 testing among PWID and underscore the importance of academic-community partnerships and prevention service delivery through SSPs and other community-based organizations serving vulnerable populations.
Keywords: Substance use, Intravenous, SARS-CoV-2, COVID-19 testing, Vulnerable populations, Harm reduction, Motivational interviewing
People who inject drugs randomized to receive a brief motivational intervention at a syringe service program were more likely to accept point-of-care COVID-19 testing than those receiving an attention-control educational intervention. Findings from this pilot randomized trial support the efficacy of this intervention to increase COVID-19 testing among PWID and underscore the importance of academic-community partnerships and prevention service delivery
Introduction
Amidst the ongoing opioid and polysubstance use epidemics, people who inject drugs (PWID) represent a sizeable and growing proportion of the U.S. population [1]. A national U.S. study identified nearly nine times the risk of COVID-19 diagnosis among patients with substance use disorders (SUD) compared to those without SUD [2]. Among people who inject drugs (PWID), multilevel factors elevate the risk of SARS-CoV-2 infection, hospitalization, and death, including chronic and infectious disease comorbidities [2, 3], stigma, and other structural factors (e.g., homelessness, poverty, limited transportation, and health insurance) that reduce utilization of preventive screening and healthcare services [4, 5].
Related to these well-documented barriers to healthcare utilization, PWID has suboptimal rates of COVID-19 testing [6], which may be compounded by limited COVID-19 knowledge and perceived risk [7] and institutional distrust [8]. Our research in the San Diego, California, and Tijuana, Mexico border region found that SARS-CoV-2 prevalence was higher among PWID than the general population while levels of COVID-19 testing were lower [9]. As of September 2021, two-thirds had never been tested for COVID-19, despite over half having recently been in contact with at least one service setting in which COVID-19 testing could have been offered [9]. We also found that many COVID-19 symptoms are similar to those of opioid withdrawal, possibly leading to PWID being less aware of SARS-CoV-2 infection [10], underscoring the need for increased COVID-19 testing in this population.
In addition to the multilevel barriers to healthcare utilization among PWID [4, 5], emerging research has identified distrust of the public health pandemic response and mandatory nature of COVID-19 testing often encountered by people experiencing homelessness and incarceration (e.g., required testing in shelters and correctional facilities) as factors that limit COVID-19 testing and vaccination motivation and uptake [6–9, 11]. Based on this literature and consultations with community-based organizations serving PWID in San Diego County, we developed the theory-, evidence-, and community-informed “LinkUP” intervention to increase COVID-19 testing uptake (primary outcome) and vaccination uptake (secondary outcome) among PWID [10]. To test the preliminary efficacy of LinkUP, we received funding from the NIH Rapid Acceleration of Diagnostics Underserved Populations (RADxUP) initiative which aims to reduce COVID-19 transmission in disproportionately impacted populations [12].
LinkUP was informed by Social Cognitive Theory [13], which posits that health-promoting behaviors are determined by interconnected outcome expectations (i.e., beliefs about the consequences of one’s behavioral choices), behavioral capability (i.e., ability to engage in desired behaviors), self-efficacy (i.e., belief in one’s ability to engage in desired behaviors), observational learning (i.e., from seeing role models perform desired behaviors), and the environmental context surrounding individuals’ behaviors. Our manualized intervention involved tailored education, motivational interviewing, problem-solving, and planning strategies to increase COVID-19 knowledge, perceived risk, and testing motivation, self-efficacy, and behavioral skills [14, 15]. Furthermore, it was delivered by trained peer counselors at a mobile syringe service program (SSP) with strong ties to the local PWID community to facilitate observational learning (i.e., from trusted role models) and support individuals in overcoming environmental barriers to COVID-19 testing. Peer counselors were outreach workers of the SSP, identified by the SSP and compensated by our study, who had lived experience with substance use and were highly familiar with—and trusted by—the local PWID community. SSPs have a long history of successfully engaging PWID in preventive screening and healthcare services [16, 17] including SUD treatment and infectious disease screening, treatment, and vaccination [18–26]. Furthermore, SSPs are routinely viewed by their clients as trustworthy sources of health information and referrals [4,27–30], making them ideal settings for interventions addressing COVID-19 testing. In this pilot randomized controlled trial (RCT; ClinicalTrials.gov identifier NCT05181657), we hypothesized that the LinkUP intervention would significantly increase COVID-19 testing relative to a didactic attention-matched control condition. This manuscript focuses only on the primary outcome (COVID-19 testing uptake), as follow-up to ascertain vaccination uptake following referrals to community-based clinics is still ongoing.
Methods
Study Design and Setting
The LinkUP pilot RCT was conducted from March to June, 2022. As previously described [10], the trial design was conceptualized and implemented in partnership with our Community Scientific Advisory Board and OnPoint, San Diego County’s only mobile, needs-based SSP. LinkUP leveraged the infrastructure of “La Frontera,” an ongoing binational cohort study of HIV, HCV, and overdose risk among PWID in the San Diego-Tijuana border region to investigate SARS-CoV2 epidemiology [9] and barriers to COVID-19 testing [6]. Participants in La Frontera were recruited via street outreach in locations where the OnPoint mobile SSP routinely operated, and other areas where PWID was known to live or congregate. Participants were eligible if they were ≥18 years old, reported past-month injection drug use, and resided in San Diego County or Tijuana, Mexico. As RADxUP funding was restricted to U.S. projects, we reviewed La Frontera data from San Diego residents who had agreed to be recontacted for future research to assess potential LinkUP eligibility, which included (1) reporting not having ever been voluntarily tested for COVID-19 outside of La Frontera or reporting having had mandatory COVID-19 testing (i.e., required testing in shelters and correctional facilities) over two months ago; and (2) either meeting the study’s “symptomatic” or “unvaccinated” definitions (i.e., being fully vaccinated according to guidelines from the U.S. Centers for Disease Control and Prevention was an exclusion criterion) [10]. To assess LinkUP eligibility, trained, bilingual study staff then recontacted potentially eligible La Frontera participants, depending on their preferences and resources, via phone calls, texts, social media, and street outreach in areas where PWID was known to live or congregate. Study staff then explained the study in English or Spanish using a consent form, answered any questions, and obtained written informed consent for the LinkUP pilot RCT, which included consent to share de-identified data with the RADxUP Data Coordinating Center at Duke University. The University of California, San Diego IRB reviewed and approved all study procedures.
Baseline Assessments
Interviewer-administered, computer-assisted assessments collected data on socio-demographics, substance use behaviors, and health and COVID-19-related factors (Table 1). Participants also provided blood specimens for HIV and HCV testing at baseline. We conducted all data collection outdoors with physical distancing and facemasks for participants and research staff [9]. As previously described [11], to reduce participant burden, one-week following baseline, we used contact methods described above to locate participants and administer a supplemental COVID-19 survey assessing COVID-19 knowledge (including misinformation and disinformation), exposures, protective behaviors, and additional RADx-UP Tier 1 Common Data Elements [31]. We assessed COVID-19 misinformation through endorsement of six items that were dichotomized (i.e., “True” and “Unsure” vs. “False”); however, due to poor psychometric properties, it was not possible to develop a scale and we thus examined misinformation items individually [11]. For disinformation, assessed through endorsement of six dichotomized conspiracy-theory items, Chronbach’s alpha was 0.72. However, due to the small number of items that we had available for the disinformation scale, we also calculated the average inter-item correlation as a measure of internal consistency which is invariant to the number of items. The mean inter-item correlation is 0.31, which indicates good internal consistency since the ideal range is considered to be between 0.15 and 0.50. [32, 33] We summed disinformation items to calculate a total score (range: 0–6).
Table 1.
Characteristics of PWID in San Diego County Participating in the LinkUP Intervention by Intervention Arm (n = 150).
| Characteristics | Active intervention (n = 75) |
Didactic intervention (n = 75) |
Overall (n = 150) |
p |
|---|---|---|---|---|
| Intervention factors | ||||
| Median length of counseling duration (in minutes; interquartile range [IQR]) | 25.0 (20.0,30.0) | 25.0 (20.0,30.0) | 25.0 (20.0,30.0) | .35 |
| Got tested for COVID-19 post intervention | 69 (92.0%) | 47 (62.7%) | 116 (77.3%) | <.001 |
| Socio-demographic factors | ||||
| Male sex at birth | 51 (68.0%) | 46 (61.3%) | 97 (64.7%) | .39 |
| Median age (IQR) | 38.0 (33.0,50.0) | 45.0 (36.0,54.0) | 40.5 (34.0,51.0) | .01 |
| Hispanic/Latinx/Mexican | 24 (32.0%) | 26 (34.7%) | 50 (33.3%) | .73 |
| Speaks English | 75 (100%) | 73 (97.3%) | 148 (98.7%) | .50 |
| Median # of years of education completed (IQR) | 11.0 (10.0,12.0) | 12.0 (10.0,13.0) | 12.0 (10.0,12.0) | .43 |
| Monthly income < $500 USD | 35 (46.7%) | 34 (45.3%) | 69 (46.0%) | .87 |
| Homeless* | 61 (81.3%) | 49 (65.3%) | 110 (73.3%) | .03 |
| Slept in shelter or welfare residence* | 8 (10.7%) | 6 (8.0%) | 14 (9.3%) | .78 |
| Incarcerated* | 13 (17.6%) | 7 (9.3%) | 20 (13.4%) | .14 |
| Engaged in sex work* | 4 (5.3%) | 2 (2.7%) | 6 (4.0%) | .68 |
| Substance use behaviors | ||||
| Injected meth* | 53 (70.7%) | 47 (62.7%) | 100 (66.7%) | .30 |
| Injected cocaine* | 8 (10.7%) | 4 (5.3%) | 12 (8.0%) | .37 |
| Injected either heroin or fentanyl* | 54 (72.0%) | 56 (74.7%) | 110 (73.3%) | .71 |
| Health-related factors | ||||
| Lacks health insurance | 8 (10.7%) | 12 (16.0%) | 20 (13.3%) | .34 |
| Ever had a flu vaccine a | 35 (47.9%) | 33 (45.2%) | 68 (46.6%) | .87 |
| Tested HIV+ b | 3 (4.4%) | 5 (7.1%) | 8 (5.8%) | .72 |
| Tested HCV+ c | 33 (49.3%) | 34 (48.6%) | 67 (48.9%) | .94 |
| Attended a syringe exchange program* | 61 (81.3%) | 56 (74.7%) | 117 (78.0%) | .32 |
| Had any COVID-19 symptoms (past week) | 38 (50.7%) | 38 (50.7%) | 76 (50.7%) | 1.00 |
| COVID-19 related factors | ||||
| Median # for: on a scale of 1–10, how worried are you about getting COVID-19 (or getting it again; IQR) | 5.0 (1.0, 7.0) | 3.0 (1.0, 6.0) | 4.0 (1.0, 7.0) | .60 |
| Thinks they had COVID-19 | 18 (24.0%) | 18 (24.0%) | 36 (24.0%) | 1.00 |
| Knowingly was exposed to somebody with a positive COVID-19 test result d | 3 (4.1%) | 7 (9.5%) | 10 (6.8%) | .19 |
| Had prior mandatory COVID-19 testing | 33 (44.0%) | 34 (45.3%) | 67 (44.7%) | .87 |
| Partially vaccinated for COVID-19 | 16 (21.6%) | 17 (22.7%) | 33 (22.1%) | 1.00 |
| Income worse since COVID-19 began | 55 (73.3%) | 49 (65.3%) | 104 (69.3%) | .29 |
| Low/very low food security since COVID-19 began | 54 (72.0%) | 43 (57.3%) | 97 (64.7%) | .06 |
| Most important sources of COVID-19 information | ||||
| Friends e | 42 (60.0%) | 31 (47.0%) | 73 (53.7%) | .13 |
| Doctors/health professionals e | 3 (4.3%) | 5 (7.6%) | 8 (5.9%) | .42 |
| Social media e | 13 (18.6%) | 14 (21.2%) | 27 (19.9%) | .70 |
| COVID-19 misinformation | ||||
| Does NOT think that the virus that causes COVID-19 can be easily spread from one person to another | 18 (24.0%) | 13 (17.6%) | 31 (20.8%) | .33 |
| Does NOT think that many thousands of people have died from COVID-19 | 18 (24.0%) | 15 (20.3%) | 33 (22.1%) | .58 |
| Thinks that most people already have immunity to COVID-19 | 49 (65.3%) | 52 (70.3%) | 101 (67.8%) | .52 |
| Thinks that you can tell someone has COVID-19 by looking at them | 13 (17.3%) | 7 (9.5%) | 20 (13.4%) | .16 |
| Thinks that there are effective treatments for COVID-19 that can cure most people | 64 (85.3%) | 50 (67.6%) | 114 (76.5%) | .01 |
| Thinks that having COVID-19 is about as dangerous as having the flu | 29 (38.7%) | 27 (36.5%) | 56 (37.6%) | .78 |
| COVID-19 disinformation | ||||
| Median # of disinformation items that they believe (out of 6; IQR) | 2.0 (1.0, 4.0) | 3.0 (1.0, 4.0) | 2.0 (1.0, 4.0) | .29 |
Note: All the n (%) represent the affirmative response to the binary variables.
*Past six months.
Missing values: an = 4; bn = 12; cn = 13; dn = 2; en = 14.
Participants received $20 and $10 compensation for completing baseline and supplemental surveys, respectively, and a laminated study ID card and were then referred to nearby OnPoint SSP sites allocated to receive either the active intervention or didactic condition (described below), for which they received an additional $10 compensation regardless of their COVID-19 testing uptake.
Randomization and Intake
To reduce contamination between conditions, we randomized weeks of study implementation to involve either the active LinkUP intervention or didactic attention-control condition (i.e., the OnPoint SSP and study team collaborated to administer whichever condition was allocated to that particular week). We co-located OnPoint and research operations so LinkUP participants could immediately connect with OnPoint peer counselors for provision of harm reduction supplies and referrals to other services. Peer counselors also confirmed participants’ identity via study ID cards and briefly re-assessed COVID-19 testing, vaccination history, and health and harm reduction needs. Counselors then delivered the condition randomly allocated to that week. Counselors received formal training in human subjects’ research ethics, motivational interviewing, and COVID-19 biology, testing, vaccination referrals, and common misinformation and disinformation from the PhD-level Project Director on our research team, who was experienced in motivational interviewing and knowledgeable about COVID-19 biology and public health recommendations. The Project Director also supervised intervention delivery and met one-on-one with counselors to provide refresher training and feedback to ensure fidelity to the intervention manuals [10].
Active LinkUP Intervention Condition
Peer counselors delivered the half-hour, single-session, manualized LinkUP intervention that was based on relevant literature, Social Cognitive Theory [13], formative research [6, 8, 9], and input from our Community and Scientific Advisory Board. The intervention began with a series of brief educational videos on COVID-19 epidemiology, testing, and vaccination (~5 minutes total; in English or Spanish). The rest of the session (~25 minutes on average) was interactive and flexible, involving tailored education focused on individuals’ unique beliefs and concerns, motivational interviewing to attempt to tip participants’ decisional balance, and problem-solving and planning strategies for future vaccination (as a secondary outcome for which follow-up data collection is still ongoing) [14, 15]. At the end of the session, counselors offered onsite COVID-19 testing and referrals to community vaccination services (described below).
Didactic Attention-Control Condition
Peer counselors also delivered the manualized didactic condition, which began with the same brief educational videos (~5 minutes total) and then involved another educational video on cardiopulmonary resuscitation (CPR; ~25 minutes), selected for relevance to the study population and appropriate length (i.e., so the didactic condition would last approximately the same amount of time as the active intervention condition. Peer counselors did not engage in motivational interviewing during the didactic session but could answer questions (if asked) using standard scripts and offered onsite COVID-19 testing and vaccination referrals (described below).
Onsite COVID-19 Testing and Vaccination Referrals
Immediately following either condition, peer counselors offered rapid COVID-19 antigen testing (Abbott BinaxNow) with pre- and post-test counseling and instructions on self-collecting nasal swabs. Counselors read and shared results with participants within 15 minutes. Participants testing positive were asked to provide an additional nasal swab for PCR confirmation and advised to practice physical distancing and wear facemasks. Participants testing positive or exhibiting COVID-19 symptoms were also referred to nearby clinics and provided with information on other community services using a list of local resources. Counselors also referred participants to nearby clinics and pharmacies offering FDA-approved or -authorized COVID-19 vaccines.
Post-Intervention Outcome Assessment
Peer counselors documented intervention receipt and duration (in minutes), whether participants agreed to rapid COVID-19 testing, and if so, their test results.
Data Analysis
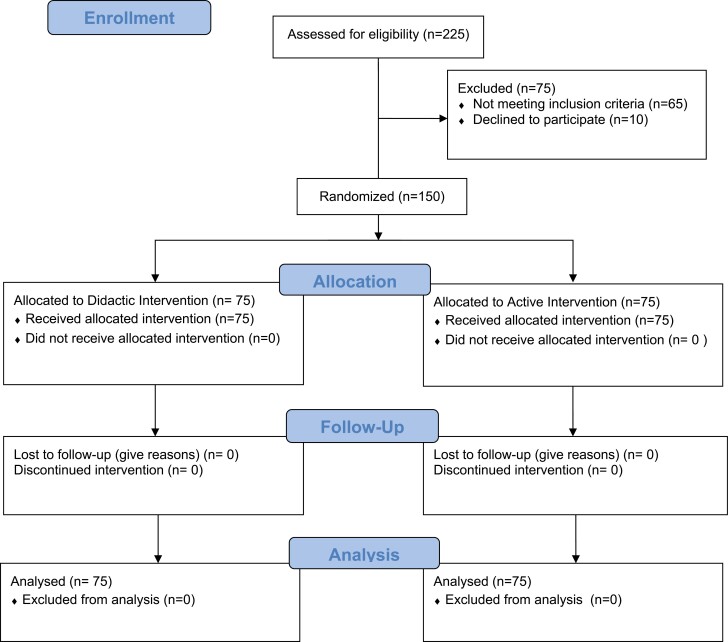
Following CONSORT guidelines [34], we conducted an intent-to-treat (i.e., per-randomization) analysis in which all enrolled participants were included in data analyses (Fig. 1). We first compared participant characteristics between the two study conditions (Table 1) and between those who did and did not get tested for COVID-19 post-intervention (Table 2) using frequencies, percentages, and Chi-square or Fisher’s Exact tests for binary variables and medians, interquartile ranges, and Mann–Whitney U tests for continuous variables.
Fig. 1.
CONSORT flow diagram.
Table 2.
Univariate Associations Between PWID Who Did and Did Not Accept COVID-19 Testing following the LinkUP Intervention (n = 150)
| Characteristics | Tested (n = 116; 77.3%) |
Not tested (n = 34; 22.7%) | Total (n = 150; 100%) |
Univariate RR (95% CI) |
p-Value |
|---|---|---|---|---|---|
| Intervention factors | |||||
| Active LinkUP intervention group | 69 (59.5%) | 6 (17.6%) | 75 (50.0%) | 1.45 (1.18,1.78) | <.001 |
| Median length of counseling duration (in minutes; interquartile range [IQR]) | 25.0 (20.0, 30.0) | 20.0 (20.0, 30.0) | 25.0 (20.0, 30.0) | 1.00 (0.99,1.01) | .73 |
| Socio-demographic factors | |||||
| Male sex at birth | 74 (63.8%) | 23 (67.6%) | 97 (64.7%) | 0.96 (0.79,1.17) | .69 |
| Median age (IQR) | 41.5 (35.0, 52.0) | 38.0 (32.0, 48.0) | 40.5 (34.0, 51.0) | 1.01 (1.00,1.01) | .27 |
| Hispanic/Latinx/Mexican | 35 (30.2%) | 15 (44.1%) | 50 (33.3%) | 0.86 (0.63,1.18) | .36 |
| Speaks English | 115 (99.1%) | 33 (97.1%) | 148 (98.7%) | 1.05 (1.03,1.08) | <.001c |
| Median # of years of education completed (IQR) | 12.0 (10.0, 13.0) | 11.5 (10.0, 12.0) | 12.0 (10.0, 12.0) | 1.01 (0.97,1.05) | .61 |
| Monthly income < $500 USD | 51 (44.0%) | 18 (52.9%) | 69 (46.0%) | 0.91 (0.77,1.08) | .28 |
| Homeless* | 83 (71.6%) | 27 (79.4%) | 110 (73.3%) | 0.93 (0.82,1.07) | .31 |
| Slept in shelter or welfare residence* | 12 (10.3%) | 2 (5.9%) | 14 (9.3%) | 1.10 (0.79,1.54) | .58 |
| Incarcerated* | 18 (15.7%) | 2 (5.9%) | 20 (13.4%) | 1.13 (1.00,1.28) | .06 |
| Engaged in sex work* | 4 (3.4%) | 2 (5.9%) | 6 (4.0%) | 0.85 (0.55,1.31) | .46 |
| Substance use behaviors | |||||
| Injected meth* | 80 (69.0%) | 20 (58.8%) | 100 (66.7%) | 1.11 (0.90,1.36) | .35 |
| Injected cocaine* | 12 (10.3%) | 0 (0.0%) | 12 (8.0%) | 1.34 (1.04,1.72) | .02 |
| Injected either heroin or fentanyl* | 83 (71.6%) | 27 (79.4%) | 110 (73.3%) | 0.96 (0.84,1.10) | .53 |
| Health-related factors | |||||
| Lacks health insurance | 17 (14.7%) | 3 (8.8%) | 20 (13.3%) | 1.11 (0.97,1.27) | .12 |
| Ever had a flu vaccine a | 53 (47.3%) | 15 (44.1%) | 68 (46.6%) | 1.05 (0.89,1.23) | .57 |
| Tested HIV+ b | 7 (6.6%) | 1 (3.1%) | 8 (5.8%) | 1.18 (0.85,1.63) | .32 |
| Tested HCV+ c | 49 (46.7%) | 18 (56.3%) | 67 (48.9%) | 0.93 (0.78,1.11) | .42 |
| Attended a syringe exchange program* | 89 (76.7%) | 28 (82.4%) | 117 (78.0%) | 0.93 (0.79,1.10) | .42 |
| Had any COVID-19 symptoms (past week) | 58 (50.0%) | 18 (52.9%) | 76 (50.7%) | 0.99 (0.81,1.23) | .96 |
| COVID-19 related factors | |||||
| Median # for: on a scale of 1–10, how worried are you about getting COVID-19 (or getting it again; IQR) | 4.0 (1.0, 7.0) | 4.0 (1.0, 7.0) | 4.0 (1.0, 7.0) | 1.00 (0.97,1.03) | .97 |
| Thinks they had COVID-19 | 26 (22.4%) | 10 (29.4%) | 36 (24.0%) | 0.92 (0.73,1.15) | .45 |
| Knowingly was exposed to somebody with a positive COVID-19 test result d | 9 (7.9%) | 1 (2.9%) | 10 (6.8%) | 1.22 (0.95,1.57) | .13 |
| Had prior mandatory COVID-19 testing | 56 (48.3%) | 11 (32.4%) | 67 (44.7%) | 1.15 (1.03,1.29) | .01 |
| Partially vaccinated for COVID-19 (vs. non-vaccinated) | 25 (21.7%) | 8 (23.5%) | 33 (22.1%) | 1.00 (0.86,1.15) | .97 |
| Income worse since COVID-19 began | 83 (71.6%) | 21 (61.8%) | 104 (69.3%) | 1.06 (0.90,1.25) | .49 |
| Low/very low food security since COVID-19 began | 76 (65.5%) | 21 (61.8%) | 97 (64.7%) | 1.04 (0.89,1.21) | .66 |
| Most important sources of COVID-19 information | |||||
| Friends e | 56 (53.3%) | 17 (54.8%) | 73 (53.7%) | 0.97 (0.76,1.24) | .80 |
| Doctors/health professionals e | 6 (5.7%) | 2 (6.5%) | 8 (5.9%) | 0.97 (0.66,1.43) | .89 |
| Social media e | 19 (18.1%) | 8 (25.8%) | 27 (19.9%) | 0.98 (0.81,1.17) | .81 |
| COVID-19 misinformation | |||||
| Does NOT think that the virus that causes COVID-19 can be easily spread from one person to another | 27 (23.5%) | 4 (11.8%) | 31 (20.8%) | 1.12 (0.87,1.43) | .39 |
| Does NOT think that many thousands of people have died from COVID-19 | 27 (23.5%) | 6 (17.6%) | 33 (22.1%) | 1.03 (0.83,1.27) | .79 |
| Thinks that most people already have immunity to COVID-19 | 78 (67.8%) | 23 (67.6%) | 101 (67.8%) | 0.98 (0.88,1.10) | .73 |
| Thinks that you can tell someone has COVID-19 by looking at them | 16 (13.9%) | 4 (11.8%) | 20 (13.4%) | 0.96 (0.77,1.20) | .74 |
| Thinks that there are effective treatments for COVID-19 that can cure most people | 87 (75.7%) | 27 (79.4%) | 114 (76.5%) | 0.85 (0.72,1.00) | .05 |
| Thinks that having COVID-19 is about as dangerous as having the flu | 41 (35.7%) | 15 (44.1%) | 56 (37.6%) | 0.93 (0.76,1.14) | .48 |
| COVID-19 disinformation | |||||
| Median # of disinformation items that they believe (out of 6; IQR) | 2.0 (1.0, 4.0) | 3.0 (1.0, 4.0) | 2.0 (1.0, 4.0) | 0.98 (0.93,1.04) | .54 |
Note: All the n (%) represent the affirmative response to the binary variables in each group (i.e., among tested, not tested, and total).
Missing values: an = 4; bn = 12; cn = 13; dn = 2; en = 14.
*Past 6 months; pp-values for the Wald Chi-Square tests from univariate modified Poisson regressions; cp-value to be interpreted with caution due to sparse data (i.e., only two participants reported not speaking English).
To assess whether the active LinkUP intervention was more successful than the didactic condition at increasing COVID-19 testing uptake (primary outcome), we used a multivariable modified Poisson regression model [35–37], via Generalized Estimating Equations (GEE), with intervention group as the primary variable of interest and potential confounders included as covariates. We also accounted for potential clustering by specifying an exchangeable correlation structure for participants who were recruited during the same week. To determine the covariates to control for, we used the modified disjunctive cause criterion set forth by VanderWeele (2019) who suggests controlling for covariates that may cause the exposure, the outcome, or both and exclude any instrumental variable that predicts the exposure but conditional on the exposure does not predict the outcome [38]. We first selected a set of variables (e.g., age, gender, homelessness, income) based on previous research findings [6] and regressed each individual variable on the outcome (Table 2) as well as on the exposure (data not shown) using modified Poisson regressions with robust standard error estimations via GEE, accounting for clustering by recruitment week. Variables that yielded p-values ≤ .10 in univariate regressions were further considered as candidates for covariates in multivariable models and retained in the final multivariable model if the p-value remained ≤ .10. Additionally, interactions between the intervention group and covariates were evaluated to determine if any covariates moderated the effect of the intervention on the outcome. For interactions, we used a conservative, accepted alpha level of 0.15 [39]. Only one interaction was found to be significant, and consequently, we calculated and tested simple main effects to determine the intervention effect at different levels of the factor involved in the interaction. Finally, we assessed the multivariable model for multi-collinearity by examining the largest condition index and variance inflation factors. We conducted all analyses using SAS (v9.4).
Results
Sample Characteristics
Among the 150 participants, median age was 40.5 years (interquartile range [IQR]: 34.0-51.0), one-third identified as Hispanic/Latinx/Mexican, and the majority reported male sex at birth (64.7%) and past 6-month experiences of homelessness (73.3%; Table 1). The most prevalent drugs injected in the past 6 months were heroin or fentanyl (73.3%), methamphetamine (66.7%), and cocaine (8.0%). Most participants had health insurance (86.7%) and had attended a SSP in the past 6 months (78.0%). Over half had never had a flu vaccine (53.3%).
On a scale from 1 to 10, the median level of concern about getting COVID-19 was 4.0 (IQR: 1.0–7.0). Overall, 44.7% reported having mandatory COVID-19 testing prior to joining the study, including 60% of those who were incarcerated and 71% of those who slept in shelter/welfare residence in the past 6 months (compared to 42% who were not incarcerated and 42% of those and did not sleep in shelter/welfare residence in the past 6 months). Overall, 22.1% had been partially vaccinated against COVID-19 prior to the study. Participants’ “most important” sources of COVID-19-related information included friends (53.7%), followed by social media (19.9%) and doctors/health professionals (5.9%).
LinkUP Intervention Participation
By design, half of participants (n = 75; 50.0%) received the active LinkUP intervention and half (n = 75; 50.0%) received the didactic attention-control condition of approximately the same duration. Following the intervention, overall, 116 (77.3%) received onsite COVID-19 testing; we only detected one SARS-CoV-2 case. However, significantly more participants in the active LinkUP intervention group received onsite COVID-19 testing than in the didactic group (92.0% vs. 62.7%; p < .001; Table 1). Of note, 56 (48.3%) of the 116 who agreed to receive onsite COVID testing and 11 (32.4%) of the 34 who did not agree to onsite COVID testing had already received prior mandatory (i.e., required) testing (Table 2).
When comparing participant characteristics and behaviors by condition, we found that the groups were unbalanced with respect to age, past 6-months homelessness, food insecurity, and beliefs in curative treatments for COVID-19; however, none of these variables were significantly associated with the COVID-19 testing outcome (Table 2), so we only investigated them as potential moderators of the intervention effect.
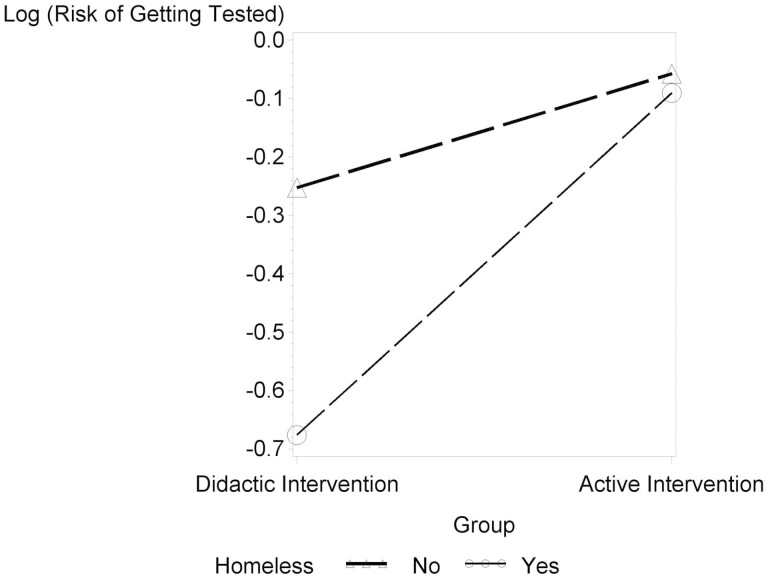
LinkUP Intervention Effect on COVID-19 Testing
When assessing univariate associations between the intervention and our primary outcome, we found it to be statistically significant (RR: 1.45; 95% CI: 1.18–1.78; p < .001; Table 2). Furthermore, when assessing associations between participant characteristics and the outcome, we found that speaking English, recent incarceration, having injected cocaine in the past 6 months, having had prior mandatory COVID-19 testing, and endorsing the COVID-19 misinformation item that “there are effective treatments that can cure most people is just as dangerous as the flu” were significant at an alpha level of .10 (Table 2). At the multivariable level (Table 3), prior mandatory COVID-19 testing was positively associated with COVID-19 testing uptake (aRR: 1.13; 95% CI: 0.98–1.30; p = .09). Homelessness significantly moderated the intervention effect (p < .0001), with the intervention having a greater impact among participants experiencing homelessness (aRR: 1.80; 95% CI: 1.56–2.09; p < .0001) than among those who were not (aRR: 1.20; 95% CI: 1.01–1.43; p = .04; see Fig. 2). Univariate regressions stratified by homelessness provided the following estimates of the intervention effect of the among non-homeless and homeless, respectively: RR: 1.23 (95% CI: 1.08–1.40; p = .002) and RR: 1.85 (95% CI: 1.77–1.94; p < .001; data not shown).
Table 3.
Effect of the LinkUP Intervention on COVID-19 Testing Among PWID in San Diego County (n = 150).
| Baseline characteristics | Adjusted RR (95% CI) | p-Valuep |
|---|---|---|
| Intervention vs. didactic condition | 1.20 (1.01,1.43) | .041 |
| Homelessness, past 6 months (yes vs. no) | 0.66 (0.57,0.76) | <.0001 |
| Had mandatory COVID-19 testing prior to joining the study (yes vs. no) | 1.13 (0.98,1.30) | .099 |
| Intervention * Homelessness | 1.50 (1.23,1.83) | <.0001 |
| Intervention (yes vs. no) among participants experiencing homelessness | 1.80 (1.56,2.09) | <.0001 |
| Intervention (yes vs. no) among participants not experiencing homelessness | 1.20 (1.01,1.43) | .041 |
p p-Values for the Wald Chi-Square tests from multivariable modified Poisson regression model.
Fig. 2.
Intervention effect by homelessness status.
Discussion
This pilot RCT provides preliminary evidence that the theory-, evidence-, and community-informed LinkUP intervention increased COVID-19 testing uptake among PWID attending mobile SSP sites in San Diego County compared to an attention-control condition, particularly for participants experiencing homelessness. Although this pilot trial was not powered to fully investigate the mechanisms through which LinkUP promoted COVID-19 testing, based on our community consultations and formative research identifying multilevel barriers to COVID-19 testing in this vulnerable population, we believe that LinkUP’s theoretical grounding and multicomponent nature supported its success. In particular, we had learned that PWID in San Diego County had low levels of COVID-19 knowledge, perceived risk, and motivation for prevention behaviors and service engagement, which could have made structural barriers to COVID-19 testing and vaccination access seem unsurmountable [6, 8, 9, 11]. We drew from Social Cognitive Theory to identify tailored education, motivational interviewing, and problem-solving and planning [14, 15] as key intervention strategies for helping participants overcome these key barriers to cognitive and behavioral change [13]. Furthermore, the implementation of LinkUP within a mobile SSP staffed by trusted peer counselors may have additionally promoted preliminary intervention efficacy, along with the direct provision of services and referrals onsite that increased the accessibility of COVID-19 testing far beyond what it would have been within other clinical and community venues. Further research, including prospective assessments of COVID-19 misinformation and disinformation among those who do and do not access SSPs, could help assess hypothesized mechanisms through which LinkUP operates and explore potential moderators of intervention effects.
For example, we found that homelessness moderated LinkUP effects, with the intervention appearing to have a greater impact on COVID-19 testing uptake among participants experiencing homelessness than those who were not. While we previously found homelessness to be associated with prior COVID-19 testing in the overall binational La Frontera cohort study [6], it is possible that testing within that earlier time period was mandatory in many settings frequently encountered by this population (e.g., emergency departments, shelters, jails, and prisons that required COVID-19 testing). As our qualitative research revealed, such mandatory testing may have bolstered individuals’ distrust of the pandemic response, reducing their motivation to seek out future testing services on their own [8]. As the prevalence of COVID-19 testing in the general population declined between the end of data collection for our previous study (in September, 2021) and the start of this pilot RCT (in March, 2022), it is possible that experiences of mandatory COVID-19 testing also declined for our participants as well. We thus posit that LinkUP may have restored trust and increased motivation to undergo voluntary COVID-19 testing. Indeed, the association between prior mandatory COVID-19 testing and voluntary testing uptake following LinkUP observed here suggests that peer counselors’ motivational interviewing, possibly combined with onsite testing access at the SSP, also addressed similar mechanisms of action.
Ultimately, we also believe that the preliminary success of LinkUP hinged on our strong community–academic partnership with a mobile SSP, OnPoint, that had cultivated trust within the local PWID community. While the accessibility of mobile SSPs within vulnerable PWID communities may be greater than “brick and mortar” (i.e., fixed) locations [40], more research is needed to understand specific advantages and disadvantages of leveraging these essential public health services within the broader context of this prolonged public health emergency [41]. Research has shown that, at the individual level, the COVID-19 pandemic may have altered PWID access to harm reduction services in diverse ways [42]. At the organizational level, as the pandemic response pressured some organizations to shift away from the provision of harm reduction services (and into the provision of COVID-19 testing, for example), some staff may have felt over-exertion and burnout [43]. Efforts to scale-up LinkUP or similar SSP-based interventions should thus consider the various implementation needs of these organizations, which require adequate funding and occupational support for the harm reduction workforce.
It is also important to consider our findings in light of other promising intervention strategies that could be complimentary to or synergistic with those used in LinkUP. For example, a growing body of research supports the role of financial incentives in promoting COVID-19 testing and vaccination [44]. In particular, contingency management, or the provision of financial incentives to reinforce recommended behaviors, can support adherence to infectious disease testing and vaccination recommendations among individuals with SUD including PWID [45–50]. Another RADxUP-funded project using a pre-post evaluation design recently suggested that contingency management involving $10 incentives could also improve COVID-19 testing uptake among SSP participants [51]. However, additional research is needed to understand the short- and longer-term impacts of contingency management efforts within such programs, including how resulting behavior changes can be sustained over time for vulnerable populations. Furthermore, as the COVID-19 pandemic limited SSP access in many settings [42, 52, 53], it may be worthwhile to explore alternative approaches such as the distribution of COVID-19 self-test kits through vending machines or peer networks. However, while self-testing for other infectious diseases (e.g., HIV) holds promise for PWID [54, 55], concerns regarding poor adherence to quarantine guidelines following COVID-19 self-testing in the U.S. general population [56] underscore the need for more research on these models [56].
Our pilot RCT had several limitations. First, our non-random sampling of PWID who were largely recruited via street outreach in an era characterized by increasing “street sweeps” of homeless encampments means that our findings may not be generalizable to the entire population of PWID in San Diego County, or PWID in other parts of the country. At the same time, similar initiatives to dismantle homeless encampments and forcibly displace persons experiencing homelessness are increasingly common across the U.S. [57, 58], despite growing evidence that they disconnect vulnerable individuals from essential prevention, healthcare, and substance use treatment services [59, 60]. Second, we relied on recall and self-report of sensitive and socially stigmatized behaviors, and some of our COVID-19-specific measures, while demonstrating high internal consistency [11], have not been formally validated. Third, our control condition provided brief educational videos on COVID-19; thus, differences between the two study arms may have been attenuated, and additional research (e.g., in the context of a fully powered RCT) is needed to confirm intervention efficacy and further explore the mechanisms of potential mediators and moderators of intervention effects. Finally, additional longitudinal research is needed to determine if LinkUP’s referrals to community vaccination services resulted in actual vaccination uptake, our secondary outcome, which may be supported by similar theory-derived strategies (e.g., planning strategies for following through on SSP-delivered referrals to offsite vaccination services) [61].
Conclusions
In summary, our pilot RCT supports the preliminary efficacy of the LinkUP intervention in increasing COVID-19 testing among PWID, particularly those experiencing homelessness. While further research is needed to confirm hypothesized mechanisms of action and identify key moderators of intervention effects, our findings suggest that uptake of COVID-19 testing among PWID may remain modest unless testing is paired with education, motivational interviewing, and problem-solving to address knowledge and attitude-related barriers. Implementation research is also needed to understand how LinkUP could be optimized for and sustained within other SSPs across the United States, as SSPs are diverse in terms of their size, scope, geographic locations, service delivery models, and other organizational and external factors. Nevertheless, this pilot trial underscores the importance of partnering with trusted community-based organizations in efforts to deliver essential prevention services and supplies to vulnerable populations disproportionately impacted by substance use, COVID-19, and other infectious diseases.
Acknowledgments
The authors gratefully acknowledge the La Frontera study team, DSMB and CSAB members, participants in San Diego County and Sharon Trillo-Park for assistance with manuscript preparation.
Contributor Information
Angela R Bazzi, Herbert Wertheim School of Public Health, University of California, San Diego, La Jolla, CA, USA; Department of Community Health Sciences, Boston University School of Public Health, Boston, MA, USA.
Daniela Abramovitz, Department of Medicine, School of Medicine, University of California, San Diego; La Jolla, CA, USA.
Alicia Harvey-Vera, Department of Medicine, School of Medicine, University of California, San Diego; La Jolla, CA, USA; Universidad Xochicalco, Facultad de Medicina, Tijuana, BC, Mexico; United States-Mexico Border Health Commission, Tijuana, BC, Mexico.
Tara Stamos-Buesig, OnPoint, Harm Reduction Coalition of San Diego, San Diego, CA, USA.
Carlos F Vera, Department of Medicine, School of Medicine, University of California, San Diego; La Jolla, CA, USA.
Irina Artamonova, Department of Medicine, School of Medicine, University of California, San Diego; La Jolla, CA, USA.
Jenna Logan, OnPoint, Harm Reduction Coalition of San Diego, San Diego, CA, USA.
Thomas L Patterson, Department of Psychiatry, University of California San Diego, CA, USA.
Steffanie A Strathdee, Department of Medicine, School of Medicine, University of California, San Diego; La Jolla, CA, USA.
Funding
This research was supported by funding from the National Institute on Drug Abuse (NIDA) through grants K01DA043412 (to ARB) and R01DA049644-S1 and R01DA049644-02S2 (to SAS), and the San Diego Center for AIDS Research (through National Institute of Allergy and Infectious Diseases grant P30AI036214, pilot grant to ARB and SAS). The funding sources played no role in writing or influencing the decision to publish the manuscript.
Compliance with Ethical Standards
Conflict of Interest Bazzi, Abramovitz, Harvey-Vera, Stamos-Buesig, Vera, Artamonova, Logan, Patterson, and Strathdee declare that they have no conflict of interest.
Authors’ Contributions Angela R. Bazzi: conceptualization, methodology, investigation, supervision, funding acquisition, writing—original draft, writing—review and editing. Daniela Abramovitz: methodology, formal analysis, data curation, writing—review and editing. Alicia Y. Harvey-Vera: investigation, writing—review and editing. Tara Stamos-Buesig: methodology, resources, writing—review and editing. Carlos F. Vera: investigation, writing—review and editing. Irina Artamonova: data curation, writing—review and editing. Jenna Logan: methodology, supervision, writing—review and editing. Thomas L. Patterson: methodology, writing—review and editing. Steffanie A. Strathdee: conceptualization, methodology, supervision, project administration, funding acquisition, writing—review and editing.
Ethical approval This study has been approved by the Office of IRB Administration at the University of California San Diego in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Transparency Statement
Study Registration: This trial was registered prospectively at ClinicalTrials.gov (identifier NCT05181657).
Analytic Plan Registration: The analytic plan was registered at ClinicalTrials.gov under the same identifier (identifier NCT05181657). Additionally, we have published the protocol paper in Addiction Science & Clinical Practice (Bazzi et al. 2022).
Availability of Data: De-identified data used in this analysis is available upon request. Interested parties should contact Daniela Abramovitz at dabramovitz@health.ucsd.edu for more information on how to submit a data request.
Availability of Analytic Code: Analytic code is available upon request. Interested parties should contact Daniela Abramovitz at dabramovitz@health.ucsd.edu for more information on how to submit a data request.
Availability of Materials: N/A
References
- 1. Bradley H, Hall E, Asher A, et al. Estimated number of people who inject drugs in the United States. Clin Infect Dis. 2022; 76(1):96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang QQ, Kaelber DC, Xu R, Volkow ND.. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry. 2021; 26(1):30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lim J, Pavalagantharajah S, Verschoor CP, et al. Infectious diseases, comorbidities and outcomes in hospitalized people who inject drugs (PWID). PLoS One. 2022; 17(4):e0266663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Biancarelli DL, Biello KB, Childs E, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019; 198:80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Motavalli D, Taylor JL, Childs E, et al. “Health Is on the Back Burner”: Multilevel Barriers and Facilitators to Primary Care Among People Who Inject Drugs. J Gen Intern Med. 2021; 36(1):129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yeager S, Abramovitz D, Harvey-Vera AY, et al. A cross-sectional study of factors associated with COVID-19 testing among people who inject drugs: missed opportunities for reaching those most at risk. BMC Public Health. 2022; 22(1):842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cioffi CC, Kosty D, Nachbar S, Capron CG, Mauricio AM, Tavalire HF.. COVID-19 vaccine deliberation among people who inject drugs. Drug Alcohol Depend Rep. 2022; 3(3):100046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Valasek CJ, Pines H, Streuli SA, et al. : COVID-19 vaccination acceptability and experiences among people who inject drugs in San Diego County. Preventive Medicine Reports. 2022; 30:101989. doi:10.1016/j.pmedr.2022.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Strathdee SA, Abramovitz D, Harvey-Vera A, et al. Prevalence and correlates of SARS-CoV-2 seropositivity among people who inject drugs in the San Diego-Tijuana border region. PLoS One. 2021; 16(11):e0260286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bazzi AR, Harvey-Vera A, Buesig-Stamos T, et al. Study protocol for a pilot randomized controlled trial to increase COVID-19 testing and vaccination among people who inject drugs in San Diego County. Addict Sci Clin Pract. 2022; 17(1):48. doi: 10.1186/s13722-022-00328-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Strathdee SA, Abramovitz D, Harvey-Vera A, et al. Correlates of coronavirus disease 2019 (COVID-19) vaccine hesitancy among people who inject drugs in the San Diego-Tijuana border region. Clin Infect Dis. 2022; 75(1):e726–e733. doi: 10.1093/cid/ciab975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tromberg BJ, Schwetz TA, Pérez-Stable EJ, et al. Rapid scaling up of Covid-19 diagnostic testing in the United States — The NIH RADx Initiative. N Engl J Med. 2020; 383(11):1071–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bandura A. Social Foundations of Thought and Action. Englewood Cliffs, NJ; 1986. [Google Scholar]
- 14. Miller WR, Rollnick S.. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY: Guilford Press; 2013. [Google Scholar]
- 15. Rollnick S, Miller WR, Butler C.. Motivational Interviewing in Health Care: Helping Patients Change Behavior. 2nd. ed. New York, NY: The Guilford Press; 2022. [Google Scholar]
- 16. Jones CM. Syringe services programs: an examination of legal, policy, and funding barriers in the midst of the evolving opioid crisis in the U.S. Int J Drug Policy. 2019; 70:22–32. [DOI] [PubMed] [Google Scholar]
- 17. Heinzerling KG, Kral AH, Flynn NM, et al. Unmet need for recommended preventive health services among clients of California syringe exchange programs: implications for quality improvement. Drug Alcohol Depend. 2006; 81(2):167–178. [DOI] [PubMed] [Google Scholar]
- 18. Smith DM, Werb D, Abramovitz D, et al. ; for Proyecto El Cuete. Predictors of needle exchange program utilization during its implementation and expansion in Tijuana, Mexico. Am J Addict. 2016; 25(2):118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wood E, Lloyd-Smith E, Li K, et al. Frequent needle exchange use and HIV incidence in Vancouver, Canada. Am J Med. 2007; 120(2):172–179. [DOI] [PubMed] [Google Scholar]
- 20. Brahmbhatt H, Bigg D, Strathdee SA.. Characteristics and utilization patterns of needle-exchange attendees in Chicago: 1994–1998. J Urban Health. 2000; 77(3):346–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schechter MT, Strathdee SA, Cornelisse PG, et al. Do needle exchange programmes increase the spread of HIV among injection drug users? An investigation of the Vancouver outbreak. AIDS. 1999; 13(6):F45–F51. [DOI] [PubMed] [Google Scholar]
- 22. Glick SN, Prohaska SM, LaKosky PA, Juarez AM, Corcorran MA, Des Jarlais DC.. The Impact of COVID-19 on Syringe Services Programs in the United States. AIDS Behav. 2020; 24(9):2466–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Belackova V, Salmon AM, Schatz E, Jauncey M.. Drug consumption rooms (DCRs) as a setting to address hepatitis C–findings from an international online survey. Hepato, Med Policy. 2018; 3:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Eckhardt BJ, Scherer M, Winkelstein E, Marks K, Edlin BR.. Hepatitis C treatment outcomes for people who inject drugs treated in an accessible care program located at a syringe service program. Open Forum Infectious Dis. 2018; 5(4):ofy048. doi: 10.1093/ofid/ofy048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Miller K, Sheaves F, Maher L, Page J, Bridges-Webb I, Treloar C.. ‘C’the potential: needle and syringe programs as hepatitis C treatment sites. Drugs: Educ, Prevent Policy. 2019; 27(1):1–3. [Google Scholar]
- 26. Sivakumar A, Madden L, DiDomizio E, Eller A, Villanueva M, Altice FL.. Treatment of Hepatitis C virus among people who inject drugs at a syringe service program during the COVID-19 response: the potential role of telehealth, medications for opioid use disorder and minimal demands on patients. Int J Drug Policy. 2022; 101:103570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Paquette CE, Syvertsen JL, Pollini RA.. Stigma at every turn: health services experiences among people who inject drugs. Int J Drug Policy. 2018; 57:104–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Biello K, Bazzi A, Mimiaga M, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduction J. 2018; 15:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Roth AM, Tran NK, Felsher M, et al. Integrating HIV preexposure prophylaxis with community-based syringe services for women who inject drugs: results from the Project SHE Demonstration Study. J Acquir Immune Defic Syndr. 2021; 86:e61–e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Roth AM, Goldshear JL, Martinez-Donate AP, Welles S, Chavis M, Van Der Pol B. Reducing missed opportunities: pairing sexually transmitted infection screening with syringe exchange services. Sex Transm Dis. 2016; 43:706–708. [DOI] [PubMed] [Google Scholar]
- 31. National Institutes of Health (NIH): NIH RADx-UP Common Data Elements. Available at https://radx-up.org/research/cdes/ Accessibility verified May 20, 2022.
- 32. Briggs SR, Cheek JM.. The role of factor analysis in the development and evaluation of personality scales. J Pers. 1986; 54:106–148. [Google Scholar]
- 33. Clark LA, Watson D: Constructing validity: basic issues in objective scale development; 2016.
- 34. Consort Transparent Reporting of Trials: The CONSORT Statement. Available at http://www.consort-statement.org/ Accessibility verified December 19, 2022.
- 35. Barros AJ, Hirakata VN: Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med. Res. Method. 2003; 3:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004; 159:702–706. [DOI] [PubMed] [Google Scholar]
- 37. Chen W, Qian L, Shi J, Franklin M.. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol. 2018; 18:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019; 34:211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Thiese MS, Ronna B, Ott U.. P value interpretations and considerations. J Thorac Dis. 2016; 8:E928–E931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Riley ED, Safaeian M, Strathdee SA, et al. Comparing new participants of a mobile versus a pharmacy-based needle exchange program. J Acquir Immune Defic Syndr. 2000; 24:57–61. [DOI] [PubMed] [Google Scholar]
- 41. NASTAD: COVID-19 Vaccine: Guidance for Syringe Sharing Services Programs, Health Departments, and People Who Use Drugs. Available at https://www.nastad.org/resource/covid-19-vaccine-guidance-syringe-services-programs-health-departments-and-people-who-use-0 Accessibility verified May 12, 2021.
- 42. Aponte-Melendez Y, Mateu-Gelabert P, Fong C, Eckhardt B, Kapadia S, Marks K.. The impact of COVID-19 on people who inject drugs in New York City: increased risk and decreased access to services. Harm Reduct J. 2021; 18:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wang A, Jawa R, Mackin S, et al. “We were building the plane as we were flying it, and we somehow made it to the other end”: syringe service program staff experiences and well-being during the COVID-19 pandemic. Harm Reduct J. 2022; 19:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Warren N, Kisely S, Siskind D.. Maximizing the uptake of a COVID-19 vaccine in people with severe mental illness: a public health priority. JAMA Psychiatry. 2021; 78:589–590. [DOI] [PubMed] [Google Scholar]
- 45. Higgins ST, Klemperer EM, Coleman SRM.. Looking to the empirical literature on the potential for financial incentives to enhance adherence with COVID-19 vaccination. Prev Med. 2021; 145:106421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Iversen J, Peacock A, Price O, Byrne J, Dunlop A, Maher L.. COVID-19 vaccination among people who inject drugs: leaving no one behind. Drug Alcohol Rev. 2021; 40:517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Herrmann ES, Matusiewicz AK, Stitzer ML, Higgins ST, Sigmon SC, Heil SH.. Contingency management interventions for HIV, tuberculosis, and hepatitis control among individuals with substance use disorders: a systematized review. J Subst Abuse Treat. 2017; 72:117–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ward KM, Falade-Nwulia O, Moon J, et al. A randomized controlled trial of cash incentives or peer support to increase HCV treatment for persons with HIV who use drugs: the CHAMPS study. Open Forum Infect Dis. 2019; 6:ofz166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tressler S, Bhandari R.. Interventions to increase completion of hepatitis B vaccination in people who inject drugs: a systematic review and meta-analysis. Open Forum Infect Dis. 2019; 6:ofz521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Norton BL, Bachhuber MA, Singh R, et al. Evaluation of contingency management as a strategy to improve HCV linkage to care and treatment in persons attending needle and syringe programs: a pilot study. Int J Drug Policy. 2019; 69:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cioffi CC, Kosty D, Capron CG, Tavalire HF, Barnes RC, Mauricio AM.. Contingency management and SARS-CoV-2 testing among people who inject drugs. Public Health Rep. 2022; 137:573–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Efunnuga H, Higgs P, Walker S, O’Keefe D.. Health service utilisation and access for people who inject drugs during COVID-19. Drug Alcohol Rev. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kesten JM, Holland A, Linton MJ, et al. Living Under Coronavirus and Injecting Drugs in Bristol (LUCID-B): a qualitative study of experiences of COVID-19 among people who inject drugs. Int J Drug Policy. 2021; 98:103391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ballard AM, Haardöerfer R, Prood N, Mbagwu C, Cooper HLF, Young AM.. Willingness to participate in at-home HIV testing among young adults who use opioids in rural appalachia. AIDS Behav. 2021; 25:699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Peiper NC, Shamblen S, Gilbertson A, et al. Acceptability of a HIV self-testing program among people who use illicit drugs. Int J Drug Policy. 2022; 103:103613. [DOI] [PubMed] [Google Scholar]
- 56. Woloshin S, Dewitt B, Krishnamurti T, Fischhoff B.. Assessing how consumers interpret and act on results from at-home COVID-19 self-test kits: a randomized clinical trial. JAMA Intern Med. 2022; 182:332–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Amster R. Patterns of exclusion: sanitizing space, criminalizing homelessness. Social Justice. 2003; 30:195–221. [Google Scholar]
- 58. Robinson T. No right to rest: police enforcement patterns and quality of life consequences of the criminalization of homelessness. Urban Affairs Rev.. 2017; 55:41–73. [Google Scholar]
- 59. Qi D, Abri K, Mukherjee MR, et al. Health Impact of street sweeps from the perspective of healthcare providers. J Gen Intern Med. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Weisenthal K, Kimmel SD, Kehoe J, Larochelle MR, Walley AY, Taylor JL.. Effect of police action on low-barrier substance use disorder service utilization. Harm Reduct J. 2022; 19:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Iversen J, Wand H, Kemp R, et al. Uptake of COVID-19 vaccination among people who inject drugs. Harm Reduct J. 2022; 19:59. [DOI] [PMC free article] [PubMed] [Google Scholar]