Abstract
Background
Discrimination has been posited as a contributor of sleep disparities for Latinxs. The strategy used to cope with discrimination may reduce or exacerbate its effects on sleep. This study examined whether different types of discrimination (everyday and major lifetime discrimination) were associated with sleep indices (quality, disturbances, efficiency) and whether coping strategy used moderated associations.
Method
Data of Latinx adults (N = 602; 51% women, 65% Dominican, Mage = 46.72 years) come from the Latino Health and Well-being Project, a community-based, cross-sectional study of Latinxs in Lawrence, MA. Multiple linear regressions were estimated separately for each sleep outcome.
Results
Everyday discrimination was significantly associated with poorer sleep quality and greater disturbances; major lifetime discrimination was significantly associated with worse sleep across the three sleep indices. Coping strategy moderated associations between discrimination and sleep. Compared with Latinxs who used passive coping, those who used passive–active coping strategies had poorer sleep quality the more they experienced everyday discrimination. Latinxs who used any active coping strategy, compared with passive coping, had greater sleep disturbances the more frequently they experienced major lifetime discrimination.
Conclusions
Findings show that everyday discrimination and major lifetime discrimination are associated with different dimensions of sleep and suggest that coping with discrimination may require the use of different strategies depending on the type of discrimination experienced.
Keywords: Latinxs, everyday discrimination, major lifetime discrimination, coping, sleep health, psychosocial stressors
Among Latinx adults, experiencing everyday and major lifetime discrimination was associated with poor sleep quality and sleep disturbances. Employing a combination of passive and active coping strategies to cope with frequent everyday discrimination was associated with worse sleep quality, while employing active coping strategies in response to frequent experiences of major lifetime discrimination was associated with more sleep disturbances.
Introduction
Sleep disparities have been reported, with Latinx individuals reporting worse sleep quality and suboptimal sleep durations compared with Whites [1, 2]. This is particularly concerning given that sleep plays a role in important functions including glucose regulation, hormone release, cardiovascular activity, immune responses, cognitive and emotional processes, and overall health [3, 4]. Poor sleep quality and inadequate sleep duration are associated with an increased risk of poor health and chronic conditions, such as obesity and diabetes [5]—two areas where Latinxs also evidence health inequities.
Although several factors contribute to sleep disparities, mounting evidence suggests that disproportionate exposure to discrimination (i.e., actual or perceived differential treatment) plays a significant role [6]. Eighty percent of Latinx adults in the United States report experiencing discrimination such as being rejected, stigmatized, or threatened in public settings, work, and school at least once in their lifetime [7]. In qualitative studies with Latinx adults, participants have disclosed instances of discrimination reflecting different manifestations, including differential access to resources and information, lack of respect, devaluation, suspicion, and dehumanization [8–11]. These studies point to the need to examine how discrimination experiences affect Latinxs’ sleep health.
Discrimination and Sleep
The Biopsychosocial Model of Racism [12] can help to explain the association between discriminatory experiences and sleep health. First, this model posits that perceived discrimination—as a psychosocial stressor—results in psychological and physiological stress responses [12] that may affect sleep. Discrimination can disrupt cognitive and emotional regulation and increase feelings of threat, rumination, loneliness, and distress [13]. Discrimination may also result in physiological changes [12]. Review studies have documented the important roles the hypothalamic–pituitary–adrenal axis plays in maintaining alertness and modulating sleep [14]. In times of stress, alterations of the hypothalamic–pituitary–adrenal axis at any level (e.g., glucocorticoid receptor) can cause cortisol dysregulation, which can negatively affect sleep health [14, 15]. Together, stress responses evoked by experiences of discrimination may constitute important mechanisms through which sleep is disrupted [16].
Experiences of discrimination are associated with poor sleep quality and efficiency, and sleep disturbances [17, 18]. A systematic review of 17 quantitative studies that examined the association between discrimination and sleep outcomes found strong evidence of a negative association with sleep quality (i.e., how well a person sleeps) and efficiency (i.e., percentage of time spent sleeping while in bed), and positive associations with sleep disturbances (e.g., nighttime awakenings)—whether sleep outcomes were measured objectively or subjectively [19]. These three sleep dimensions are relevant to the health of Latinxs, given their association with health outcomes in which Latinxs experience health inequities such as cardiometabolic conditions [20]. Across several multi-ethnic samples (inclusive of Latinxs), findings show that everyday and major lifetime discrimination are associated with these sleep dimensions [18, 21–24]. Overall, burgeoning research shows that discrimination can have deleterious effects on various aspects of sleep health [6].
Second, the Biopsychosocial Model of Racism [12] model emphasizes the importance of distinguishing between chronic and acute forms of discrimination. These events differ in magnitude (e.g., major life events versus daily occurrences) and frequency [25], which may result in them having differential associations with sleep indices. Everyday discrimination, which captures the breadth of exposure to day-to-day experiences of discrimination (e.g., being followed around in a store), is persistent and more pervasive [6]. Major lifetime discrimination captures cumulative exposure to major events of discrimination across life domains (e.g., being unfairly denied a promotion). Previous research finds that both everyday discrimination [17, 18] and major lifetime discrimination [18, 24] are associated with indicators of poor sleep, although studies with nationally representative samples indicate everyday discrimination is more consistently and robustly associated with health indicators [26, 27], including correlates of poor sleep. Examining whether these two forms of discrimination are associated with sleep indices above and beyond the other in a single study with a sample of Latinx adults remains an empirical question worthy of investigation.
Discrimination and Coping
The Biopsychosocial Model of Racism [12] also suggests that coping—defined as “cognitive and behavioral efforts to manage specific external and/or internal demands appraised as taxing or exceeding the resources of the individual” [28]—is a relevant moderator in the association between discrimination and health outcomes. Clark et al. [12] theorize that maladaptive and adaptive coping, such as passive and active coping, respectively, may independently affect health. Additionally, these strategies can exacerbate or protect against the adverse health effects of discrimination. Passive coping involves efforts to adapt to or avoid stress when faced with uncontrollable and unchangeable situations [29]. Perez et al. [30] found that Latinx immigrant adults who reported higher stress levels were more likely to report having experienced discrimination and having engaged in passive coping (i.e., denial) as their coping strategy in the face of these stressors. In other research studies, passive coping strategies (e.g., avoidance) were associated with mechanisms posited to impact sleep negatively [31], including negative emotions and venting [32], depressive symptoms [32, 33], higher blood pressure levels [34–36], and increased alcohol and drug use [32].
Conversely, active coping efforts (e.g., seeking support) aim to influence the situation by trying to modify the stressor and are associated with favorable outcomes [29]. Receipt of social support (emotional and instrumental) protects against discrimination’s harmful effects on sleep [37, 38]. Active coping strategies in response to discrimination are associated with lower sympathetic activation (i.e., lower blood pressure) [34], which may be beneficial for sleep. Less is known about whether joint use of passive and active coping strategies in response to discrimination is associated with better or worse outcomes when compared to individuals who use only one type of coping strategy. One study [39] found that relative to individuals who used only active coping or a combination of passive and active coping in response to interpersonal discrimination, those who only used passive coping reported higher levels of dissociative symptoms, which are directly associated with worse sleep (e.g., sleep disturbances) [40, 41] and indirectly associated with poor sleep quality via chronic worry [42]. Altogether, findings suggest that, relative to employing only passive coping strategies, using active or a combination of active and passive coping strategies may be more beneficial to sleep when faced with stressful experiences, such as discrimination.
Clark et al. [12] further suggest that the extent to which discrimination may affect health can vary based on both the coping strategy used and nature of discriminatory experience (acute versus chronic). For example, passive coping strategies may exacerbate negative sleep effects in the context of both types of discrimination. However, associations may be less consistent under acute stress such as major lifetime discrimination. Constantly employing passive strategies (e.g., keeping the experience to oneself) to cope with persistent, day-to-day unfair treatment can become maladaptive and detrimental to sleep health. Though not focused on discrimination, a study found that frequent use of passive coping strategies resulted in severe sleep-related disturbance among cancer patients [43]. Other studies find that chronic exposure to stressful conditions (e.g., work overload) and frequent use of passive coping predict emotional exhaustion [44], which is associated with sleep disturbances and worse sleep quality [45, 46]. Furthermore, under conditions of high chronic stress, passive coping is associated with dissociative symptoms [44], a correlate of poor sleep health [40, 41]. Against this backdrop, it is theoretically plausible that the exacerbating effects of passive coping would be more consistently detrimental to different aspects of sleep under conditions of chronic stress, such as in the context of everyday discrimination.
Present Study
The current study addresses several gaps in the literature: (a) examining whether everyday discrimination and major lifetime discrimination are cross-sectionally associated with sleep health (i.e., quality, daily disturbances, and efficiency) and (b) identifying if and how coping strategies (i.e., passive, active, and passive–active coping) moderate the association between each discrimination type and sleep indices. It is hypothesized that greater frequency of everyday and major lifetime discrimination will be associated with worse sleep health across indices [23, 24, 47]. Based on theory [12] and previous research [26, 27], we expect more consistent associations between everyday discrimination and sleep indices than with lifetime discrimination. Due to the limited research on the effects of coping strategies in the context of different forms of discrimination, no concrete hypotheses regarding moderation effects by type of discrimination were formulated. However, based on prior research [33–36], it is hypothesized that passive–active and active coping will be protective, whereas passive coping will exacerbate the effects of both types of discrimination on all three sleep outcomes.
Method
Participants and Procedures
This study is based on a secondary analysis of cross-sectional data from the Latino Health and Well-being (LHWB) Project cohort. Data were collected between September 2011 and May 2013. Participants were recruited from the Lawrence Family Health Center in Lawrence, MA. Proportional sampling within age (i.e., 21–34, 35–54, and 55–85 years) and gender strata from electronic patient records was used to randomly identify potential participants who met inclusion criteria (i.e., self-identifying as Latino/Hispanic, Spanish, or English speakers, aged 21–85, no plans to move from the area within 1 year, and able to verbally answer surveys). Out of 2,783 potentially eligible individuals identified, 1,236 (44.4%) could be contacted by study staff, and 602 (21.6%) ultimately agreed to participate. Informed consent was obtained and surveys were verbally administered in English or Spanish by trained bilingual/bicultural research assistants at a centralized community location. Participants received $50 as compensation. The University of Massachusetts Medical School Institutional Review Board (IRB) approved the main study (#H-14144). Exempt status for secondary analysis of the main study from the University of California Irvine IRB was obtained.
Measures
Major lifetime discrimination.
The Experiences of Discrimination Scale [48], a nine-item self-report measure, assessed experiences of major lifetime discrimination in several domains (e.g., “Have you ever experienced discrimination, or been made to feel inferior, while getting housing because of your race, nationality, ethnicity, or skin color?”). Responses to items followed a yes (coded as 1) or no (coded as 0) format. The sum of all affirmative responses was used, with higher numbers reflecting greater counts of discrimination (possible scores range: 0–9). This measure has been used with Latinx samples [49, 50]. In the present study, the scale demonstrated acceptable reliability (α = .74).
Everyday discrimination.
The Everyday Discrimination Scale [51] was used to assess routine discriminatory events in participants’ daily life. A six-point scale (1= never, 6 = almost every day) was used to determine the frequency of experiences of discrimination across nine scenarios (e.g., “You received poorer service than other people at restaurants or stores”). The sum of all items was used, with higher scores indicating a greater frequency of everyday discrimination (possible score range: 9–54). The measure demonstrated good reliability in a nationally representative sample of Latinx adults [52]. The scale showed good internal consistency (α = .87) in the current sample.
Sleep.
The Pittsburgh Sleep Quality Index (PSQI) [53] includes 18 items, which encompass seven dimensions of sleep measured retrospectively within the past month: duration, disturbance, latency, daytime dysfunction, efficiency, quality, and sleeping medication use. The PSQI included open-ended items such as “During the past month, what time have you usually gone to bed at night?” and items with Likert-scale response options such as “How would you rate your sleep quality, overall, during the past month?” (1 = very good, 4 = very bad). First, we followed the procedure by Buysse et al. [53] to obtain the scores for all seven components. Each component has a minimum score of zero and a maximum score of three points. To obtain scores for the three dimensions of interest (i.e., quality, efficiency, and disturbances), we followed Cole et al.’s [54] scoring method, which found support for a three-factor model solution from the seven PSQI components (Factor 1: Sleep Quality [quality, latency, use of sleep medications]; Factor 2: Sleep Efficiency [duration, efficiency], Factor 3: Daily Disturbances [disturbances, daytime dysfunction]). The three factors were calculated by averaging across the appropriate components (range of scores: 0–3), with higher scores reflecting worse sleep quality, less efficient sleep, and more disturbances. The PSQI three-factor structure showed a good fit to data of English- and Spanish-speaking Mexican adults [55]. In our sample, the three PSQI dimensions showed good internal consistency: Quality (α = .71), efficiency (α = .75), and disturbances (α = .69).
Coping strategy.
Two items from the Experiences of Discrimination scale were used to assess coping strategies, these items have shown fair test-retest reliability [48]. Participants responded to the two items by indicating how they generally respond to unfair treatment: Item 1: “accept it as a fact of life [accept]” (coded as 1) or “try to do something about it [do something]” (coded as 0) and Item 2: “talk to other people about it [talk]” (coded as 1) or “keep it to yourself [keep to self]” (coded as 0). Responses were classified as passive coping if “accept” and “keep to self” were used; active coping if “talk” and “do something” were used, and passive–active coping if any combination of passive and active strategies were used. This three-level categorization has been employed in previous research [34, 39, 56, 57].
Sociodemographic characteristics.
Age (in years), gender (women, men), education level (1 = Less than high school to 6= college graduate), Latinx ethnicity (Dominican, Puerto Rican, Other Latinx), nativity status (U.S. born vs. foreign born), perceived income (whether the respondent has enough money to meet their needs), and employment status (unemployed vs. employed) were included as covariates in statistical models.
Analytic Strategy
Preliminary analyses.
We conducted bivariate analysis between all covariates and outcome variables (i.e., sleep indices). Associations with p-values of <.25 were considered in a fully adjusted model of covariates to arrive at a more parsimonious model of potential confounders; covariates significant at this stage were included in the estimated models [58]. Missing values on our variables represented less than 1%, fewer than the recommended 5% for imputation, which allowed listwise deletion in all analyses [59].
Main analyses consisted of estimating multiple linear regression models. Sleep outcomes were modeled by building three models for each sleep measure. In Model 1 (main effects model), both everyday and major lifetime discrimination variables along with covariates were included. In Model 2 (main effects model), the categorical coping strategy variable was added. The final model (Model 3) further added the 2-way interaction terms for everyday discrimination × coping strategy and for major lifetime discrimination × coping strategy to test the effect modification of coping in the associations between discrimination type and sleep outcomes. Continuous variables included in interaction terms (i.e., discrimination measures) were mean centered to reduce multicollinearity [60]. To aid in interpreting and illustrating any significant interactions, coefficients from the final models were used to calculate predicted marginal means of sleep outcomes. Follow-up contrasts of estimated marginal means examined the interaction term at different levels of each discrimination measure. Analyses were conducted using Stata Version 15.
Results
Descriptive Statistics and Correlations
The mean age of participants was 46.7 years (SD = 15.4), with women and men representing 51% and 49%, respectively, of the total analytic sample. Participants were primarily foreign born (92% vs. U.S. born [8%]). Nearly two-thirds (65%) of the sample identified as Dominican, 16% as Puerto Rican, and 18% as “Other Latinxs” (i.e., Cuban, Central American, Mexican, and South American). More than half of the sample had less than a high school degree (51%), 11% had a high school degree, 25% had some post-high school degree education, and 11% had a college degree or higher. Fifty-one percent of our sample was employed and 49% were unemployed, laid off, or retired. More than half of the sample (52%) reported having just enough or more than enough income to support their needs, whereas the remaining 48% reported not having enough income.
Table 1 reports descriptive statistics for and bivariate correlations among the main study variables. Participants reported relatively low levels of everyday discrimination and major lifetime discrimination, with the average person reporting about one discriminatory event per year and one occurrence of major lifetime discrimination. The most reported coping strategy used was passive–active (69%), followed by active strategies only 26%, and passive strategies only (5%); these rates are similar to those reported in another study [34]. Both discrimination measures were significantly and positively associated with the three sleep indices.
Table 1.
Descriptive Statistics and Correlations Among Main Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Everyday discrimination (ED) | — | |||||||
| 2. Major lifetime discrimination (MLD) | .43*** | — | ||||||
| Sleep dimensions | ||||||||
| 3. PSQI perceived quality factor | .19*** | .13** | — | |||||
| 4. PSQI sleep efficiency factor | .10* | .13** | .55*** | — | ||||
| 5. PSQI daily disturbances factor | .24*** | .26*** | .51*** | .33*** | — | |||
| Coping strategies | ||||||||
| 6. Passive only | .06 | .05 | .03 | .01 | .09* | — | ||
| 7. Active and passive | −.01 | −.01 | −.10* | −.02 | −.12* | — | — | |
| 8. Active only | −.02 | −.02 | .09* | .02 | .08* | — | — | — |
| M (SD) | 14.96 (7.21) | 0.94 (1.54) | 1.03 (0.87) | 1.01 (1.04) | 0.69 (0.66) | — | — | — |
| % (SE) | — | — | — | — | — | 5% (0.01) | 69% (0.02) | 26% (0.02) |
Higher scores in PSQI measures indicate worse sleep quality, efficiency, and disturbances, respectively. Data were missing on ED for one participant (n = 601) and on coping for five participants (n = 597). Range of actual scores on continuous measures was ED = 9–46, MLD = 0–8, PSQI measures = 0–3.
*p < .05, **p <. 01, ***p < .001.
Multivariable Linear Regression Models
Sleep quality.
In Model 1 (see Supplementary Table 1), results showed that everyday discrimination (β = 0.16, p < .001) and major lifetime discrimination (β = 0.09, p = .04) were significantly associated with worse sleep quality. In Model 2 (see Supplementary Table 1), results indicated that coping strategy used is not associated with sleep quality. Both discrimination measures remained significantly associated with worse sleep quality. In the final model (Model 3, Table 2), results showed that coping strategy moderated the effects of everyday discrimination on sleep quality, but not of major lifetime discrimination. Specifically, the slopes of the regression lines between everyday discrimination and sleep quality were significantly different (β = 0.28, p = .033) for those using passive coping strategies compared to those using passive–active strategies.
Table 2.
Multiple Linear Regression Models Predicting Sleep Outcomes
| PSQI perceived quality | PSQI daily disturbances | PSQI sleep efficiency | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Models | B (SE) | 95% CI | β | B (SE) | 95% CI | β | B (SE) | 95% CI | β |
| Main effects | |||||||||
| Discrimination type | |||||||||
| ED | −0.02 (0.02) | −0.054, 0.018 | −0.15 | 0.04 (0.01)** | 0.013, 0.066 | 0.43 | −0.01 (0.02) | −0.052, 0.038 | −.05 |
| MLD | 0.10 (0.13) | −0.148, 0.345 | 0.17 | −0.10 (0.09) | −0.286, 0.081 | −0.24 | 0.01 (0.15) | −0.295, 0.312 | .01 |
| Main effects | |||||||||
| Coping strategy | |||||||||
| Passive only | REF | REF | REF | ||||||
| Passive-Active | −0.14 (0.17) | −0.477, 0.196 | −0.07 | −0.21 (0.13)† | −0.464, 0.037 | −0.15 | −0.08 (0.21) | −0.499, 0.331 | −.04 |
| Active only | 0.05 (0.18) | −0.304, 0.400 | 0.02 | −0.06 (0.13) | −0.324, 0.200 | −0.04 | −0.05 (0.22) | −0.487, 0.381 | −.02 |
| Interactions | |||||||||
| Discrimination × Coping Strategy | |||||||||
| ED × Passive Only | REF | REF | REF | ||||||
| ED × Passive-Active | 0.04 (0.02)* | 0.003, 0.079 | 0.28 | −0.03 (0.01)† | −0.054, 0.002 | −0.24 | 0.02 (0.02) | −0.022, 0.071 | .14 |
| ED × Active Only | 0.02 (0.02) | −0.020, 0.064 | 0.08 | −0.03 (0.02)† | −0.059, 0.003 | −0.14 | −0.01 (0.03) | −0.057, 0.047 | −.02 |
| MLD × Passive Only | REF | REF | REF | ||||||
| MLD × Passive-Active | −0.05 (0.13) | −0.306, 0.197 | −0.08 | 0.18 (0.10)† | −0.006, 0.368 | 0.37 | 0.06 (0.16) | −0.255, 0.365 | .07 |
| MLD × Active Only | −0.02 (0.14) | −0.288, 0.253 | −0.01 | 0.26 (0.10)* | 0.059, 0.462 | 0.27 | 0.14 (0.17) | −0.189, 0.479 | .09 |
| N | 590 | 590 | 585 | ||||||
| F-test statistic | F(16, 573) = 6.19*** | F(16, 573) = 6.94*** | F(16, 568) = 2.95*** | ||||||
| Adj. R2 | 12% | 14% | 5% | ||||||
CI confidence interval; ED everyday discrimination; MLD major lifetime discrimination; PSQI Pittsburgh Sleep Quality Index; REF reference group. All models adjusted for covariates.
*p < .05, **p < .01, ***p < .001, †p < .10.
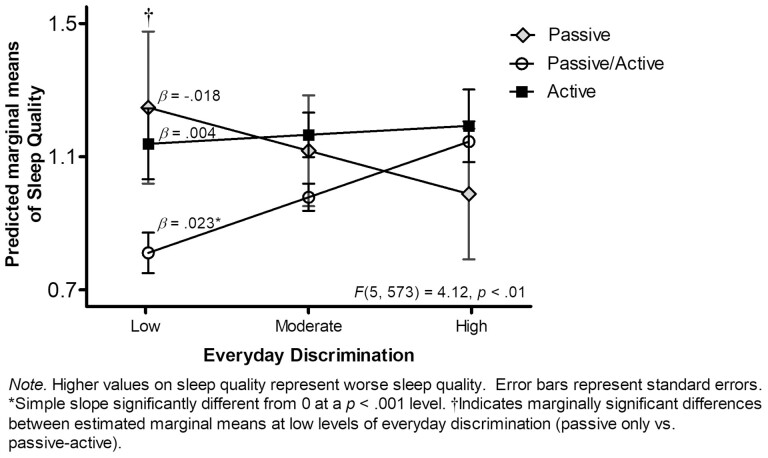
Follow-up contrasts showed that, at low levels of everyday discrimination, Latinxs who used only passive coping strategies were predicted to have marginally worse sleep quality compared with those who used passive–active coping strategies (Mdiff = −0.44, SE = 0.24, p = .065). There were no significant differences in sleep quality at moderate or high levels of everyday discrimination between coping groups. Post hoc simple slopes analyses showed that among Latinxs who used either only passive coping (β = −0.018, SE = 0.018, p = .33) or only active coping (β = 0.004, SE = 0.012, p = .75), increasing levels of everyday discrimination did not affect sleep quality. However, among Latinxs who used passive–active coping, increasing levels of everyday discrimination were associated with poorer sleep quality (β = 0.023, SE = 0.006, p < .001). Figure 1 shows the plotted simple slopes and predicted marginal means of sleep quality as a function of everyday discrimination and coping strategy.
Fig. 1.
Sleep quality as a function of everyday discrimination and coping strategy.
Sleep disturbances.
In Model 1 (see Supplementary Table 2), results showed that everyday discrimination (β = 0.17, p < .001) and major lifetime discrimination (β = 0.21, p < .001) were significantly associated with more sleep disturbances. In Model 2 (see Supplementary Table 2), results indicated that coping strategy used was not associated with sleep disturbances. Both discrimination measures remained significantly associated with more sleep disturbances. In Model 3 (see Table 2), results revealed that coping strategy moderated the effects of major lifetime discrimination on sleep disturbances, but not for everyday discrimination. Specifically, the slopes of the regression lines between major lifetime discrimination and sleep disturbances were significantly different between those employing only passive strategies compared with those employing only active coping strategies (β = 0.27, p = .011).
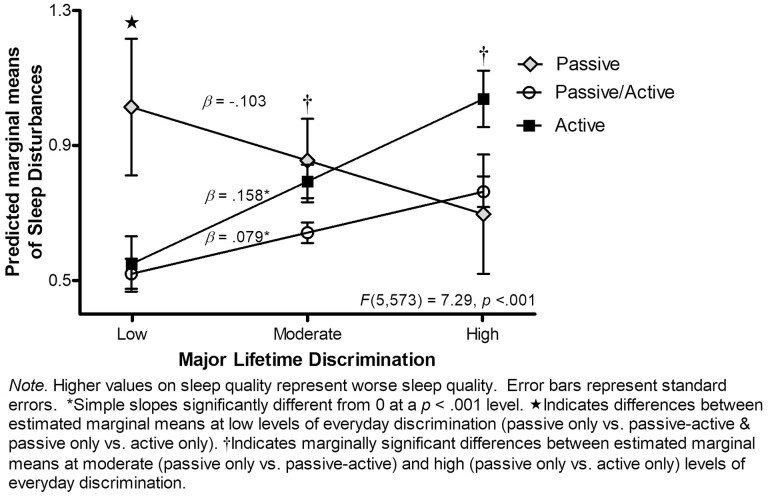
Findings from follow-up contrasts revealed significant differences in sleep disturbances by coping strategy used only at low levels of major lifetime discrimination. That is, at low levels of major lifetime discrimination, Latinxs who employed passive coping strategies in response to discrimination were predicted to have significantly more sleep disturbances compared to those who employed passive–active coping (Mdiff = −0.49, SE = 0.21, p = .017) or active only coping (Mdiff = −0.46, SE = 0.22, p = .033). Post hoc simple slopes analyses revealed that among Latinxs who employed passive only coping strategies (β = −0.103, SE = 0.093, p = .27), increasing levels of major lifetime discrimination were not associated with sleep disturbances. However, among Latinxs who employed passive–active (β = 0.079, SE =.021, p < .001) or active only coping strategies (β = 0.158, SE = 0.043, p < .001), increasing levels of major lifetime discrimination were associated with more sleep disturbances. Figure 2 shows the plotted simple slopes and predicted marginal means of sleep disturbances as a function of major lifetime discrimination and coping strategy.
Fig. 2.
Sleep disturbances as a function of major lifetime discrimination and coping strategy.
Sleep efficiency.
In Models 1 and 2, results showed major lifetime discrimination was significantly associated with efficiency, whereas everyday discrimination was only significantly associated with efficiency in Model 1 (see Supplementary Table 3). There was no main effect of coping in Model 2. In Model 3 (Table 2), coping did not moderate associations between discrimination measures and efficiency. Furthermore, the main effect for major lifetime discrimination on efficiency was not significant in this final model.
Discussion
The current study examined: (a) how everyday discrimination and major lifetime discrimination related to different sleep indices and (b) if and how coping strategies moderated these associations among a community sample of predominantly immigrant, Caribbean Latinxs. Consistent with hypothesized main effects and prior research [24, 47, 61–63], findings revealed that everyday discrimination and major lifetime discrimination were associated with worse sleep quality, more sleep disturbances, and worse sleep efficiency. However, everyday discrimination was no longer significantly associated with efficiency once the coping variable was added to the model; this finding corroborates results from previous studies using everyday discrimination [21] or racial/ethnic discrimination [64] scales with Latinx adults. Overall, findings align with the Biopsychosocial Model of Racism [12], which conceptualizes chronic and acute types of discrimination as stressors that can impact health-related outcomes Results from moderation analyses provide additional insight into the discrimination–sleep relationship.
Everyday Discrimination, Coping, and Sleep
Results showed that employing a passive–active coping strategy (vs. passive) was associated with worse sleep quality. When the interaction was probed, results showed that among those employing passive–active coping, higher levels of everyday discrimination were associated with worse sleep quality. Though contrary to what was hypothesized, follow-up contrasts revealed that at low levels of everyday discrimination, those who employed passive–active coping reported marginally better sleep quality than those who employed only passive coping. Albeit marginal, the pattern is in line with the prediction that passive–active coping would have a buffering effect, though it appears to depend on the frequency of everyday discrimination.
Consistent with socio-cognitive models of racism [13], employing passive–active coping strategies when exposed to everyday discrimination may mean having to negotiate when and how to respond to repeated discriminatory occurrences, which could deplete cognitive resources [65] and negatively affect sleep quality. The ambiguity that results from experiences such as being treated with less courtesy than others may make it difficult for individuals to determine whether they were treated unfairly [66] and what to do about it, which can be stressful above and beyond the event [67]. In addition to taxing cognitive resources, this ambiguity can also prolong the stress response, which could compromise sleep quality [68]. Furthermore, the confronting prejudiced responses model [69] argues that targets of discrimination may be reluctant to do something about discriminatory incidents to avoid interpersonal conflict and social costs [70]. Yet, not responding could have intrapersonal costs, such as feeling powerless [70], which may contribute to rumination [61] and vigilance [64]—mechanisms via which discrimination relates to worse sleep quality.
There are several potential reasons for why everyday discrimination may not have impacted the sleep quality among Latinxs who engaged in only passive or only active coping. As posited by the “shift-and-persist” perspective [71], perhaps individuals who used only passive coping have accepted the pervasive nature of unfair treatment as a part of life and may have developed ways to persist through these experiences. Latinxs who only used active coping strategies could have accrued and benefited from health-promoting psychosocial reserves such as increased sense of autonomy [72], control [73], and emotional support [74]. Evidence suggests active coping behaviors (e.g., problem-solving) have buffering effects [75], whereas active coping dispositions such as high-effort control exacerbate the harmful effects of discrimination. Synergistic effects between everyday discrimination and coping strategy were not observed for sleep efficiency or disturbances. This could be because other factors, such as negative mood and pain [76, 77], may be more predictive of sleep efficiency and disturbances than experiences of everyday discrimination and coping.
Major Lifetime Discrimination, Coping, and Sleep
Results showed that in the context of major lifetime discrimination, employing an active (vs. passive) coping strategy was associated with more sleep disturbances. Follow-up contrasts showed that Latinxs who used passive–active and active coping strategies reported less sleep disturbances than those who used only passive coping—consistent with the hypothesized buffering effect—but only at low levels of major lifetime discrimination. Simple slopes analyses showed that more sleep disturbances were associated with increasing levels of major lifetime discrimination among those using passive–active or active coping strategies.
One reason for these findings could be the consequential effects of major lifetime discrimination [6]. That is, although experiences of major lifetime discrimination tend to occur less often, when they do occur, they can have significant consequences that limit access to health-promoting resources [67]. For example, being denied a bank loan may indirectly result in sleep disturbances through limiting Latinxs’ ability to buy or rent a home in a safe neighborhood that facilitates sleep [6]. Likewise, being unfairly denied a promotion might force an individual to work long hours, which could result in irregular sleep schedules [78]. Because instances of major lifetime discrimination are less ambiguous and have greater costs, individuals may be more inclined to use active coping strategies in response to them. However, the initial protective effect observed for active coping (at low levels of major lifetime discrimination) may result in psychosocial costs the more these strategies are used. Latinxs in our study relied mostly on talking to others as a coping strategy in response to discrimination. This strategy could be detrimental to sleep if overused because repeatedly disclosing one’s discriminatory experiences may result in seeing oneself as a victim [67] or developing negative schemas about oneself [13]. It could also be that the active coping options in our study were not specific enough. “Try to do something about it” may include strategies that can result in interpersonal conflict [11], which is related to sleep disturbances via increased negative affect [79]. Meta-analytic findings also show that active coping is not always associated with better health outcomes [80]—providing support for our seemingly counterintuitive results. Our results suggest the protective effects of active coping depend on the type of discrimination and frequency with which it occurs.
Strengths, Limitations, and Future Directions
Our study has several strengths. First, it focuses on a segment of the Latinx population (i.e., Caribbean Latinxs) underrepresented in this area of research, who may be at increased risk of poor sleep outcomes [81] and greater exposure to discrimination [82]. Second, we included multiple measures of discrimination and sleep indicators, which had not been previously done in a single study. Several key limitations are acknowledged. First, we included only self-report measures, which are subject to participant recall and social desirability. Future studies should include both self-report and objective sleep measures, including dimensions not evaluated in this study (e.g., sleep architecture) and history of sleep disorders (e.g., insomnia) to evaluate whether the observed associations remain, above and beyond any preexisting sleep problems. Although the study’s cross-sectional design does not allow for claims of causality or temporality to be made, prospective studies show that exposure to discrimination disrupts sleep in the short and long term [83]. Additionally, studies with Latinxs and other ethnic groups [39, 48] have used the same coping items and a similar categorization approach as ours. However, these items and approach limit our ability to capture the range of coping strategies individuals may use in response to discrimination, including those found salient to Latinxs (e.g., religious coping) [70].
Last, our findings may not generalize to other Latinx groups and those living in different contexts. Participants in this study were mostly foreign born and resided in an ethnic enclave where they may have encountered fewer instances of discrimination [84]. Studies that have included Latinx or immigrant adults also report relatively low levels of both types of discrimination [18, 48, 85, 86]. Our findings are compelling, given that we identified associations despite low levels of everyday and major lifetime discrimination in our sample, which may bias our results toward the null hypothesis. Still, future work should aim to investigate how Latinxs residing in neighborhoods with different ethnoracial compositions may experience and be impacted by discrimination.
Implications
Overall, our findings provide new insight to how chronic and acute forms of discrimination relate to different sleep indicators among Latinx adults. Notably, our findings point to the importance of considering synergistic effects of type of discrimination exposure and coping approach employed when confronted with such experiences. As Joseph and Kuo [70] point out, coping strategies may be more beneficial in some contexts compared to others, suggestive of the need for different interventions. Emerging evidence shows that mindfulness-based interventions may be able to reduce stress due to discrimination [87] and can improve sleep health by reducing symptoms of stress-related disorders [88, 89]. Other interventions that may promote optimal sleep health include those that empower Latinxs to harness supportive social relationships to cope with discrimination, given that social support is associated with better sleep quality [90]. Since major lifetime discrimination may occur in institutional settings (e.g., workplaces), it is critical to consider approaches that may both reduce discrimination and improve sleep. Results from a workplace intervention study found that training supervisors about interactional injustice resulted in insomnia symptom improvement among their subordinates at the conclusion of the training and up to 6 months after [91]. These findings suggest that intervening at institutional levels may, over time, improve sleep health among subordinate groups over time via reduced exposure to discrimination from subordinates.
Conclusion
Latinxs are at an increased risk of experiencing discrimination [7] and poor sleep [21], increasing their risk of adverse outcomes such as mental health disorders, chronic health diseases, and disability across the life course. Substantial economic costs can be incurred by nations due to the burden of disease associated with exposure to discrimination [92] and sleep disorders [93]. Notably, Latinxs will represent one in five (21.2%) workers in the U.S. labor force in 2030 [94]. Thus, the burden of disease experienced by Latinxs could reduce their labor force participation and have a negative economic impact on their families, communities, and the country. As such, the health of Latinxs is intricately tied to the overall health of the nation and its economic viability. Efforts aimed at eradicating discrimination at multiple levels to reduce and ultimately eliminate sleep inequities experienced by Latinxs would benefit this community and our broader society.
Supplementary Material
Contributor Information
Angelina Majeno, Department of Psychological Science, University of California–Irvine, Irvine, CA, USA.
Kristine M Molina, Department of Psychological Science, University of California–Irvine, Irvine, CA, USA.
Christine F Frisard, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, MA, USA.
Stephenie C Lemon, Population and Quantitative Health Sciences, University of Massachusetts Medical School, Worcester, MA, USA.
Milagros C Rosal, Population and Quantitative Health Sciences, University of Massachusetts Medical School, Worcester, MA, USA.
Funding
This research was supported through a grant from the National Institute of Mental Health (R01 MH085653), PI: Milagros Rosal.
Compliance with Ethical Standards
Conflict of Interest: The authors report no conflicts of interest.
Authors’ Contributions A.M. served as lead for conceptualization, investigation, writing-original draft, and formal analysis. K.M. served as lead for resources and supervision of investigation and formal analysis and contributed to conceptualization and writing-original draft. A.M. and K.M. contributed equally to writing-review and editing. C.F. served in a supporting role for funding acquisition, methodology, project administration, data curation, and writing-review and editing. S.L. and M.R. served as lead for funding acquisition, methodology, and project administration equally, and served in a supporting role for writing-review and editing.
Ethical approval: The institutional review board of the University of Massachusetts Medical School approved all recruitment, consent, and interviewing procedures. Secondary data analysis of LWHB data was IRB exempt by the University of California, Irvine. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration of 1975, as revised in 2000 or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Transparency Statements: (a) Study registration: This study was not formally registered. (b) Analytic plan pre-registration: The analysis plan was not formally pre-registered. (c) Data availability: De-identified data from this study are not available in a public archive. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author and per approval of the original study principal investigators. (d) Analytic code availability: Analytic code used to conduct the analyses presented in this study are not available in a public archive. They may be available by emailing the corresponding author. (e) Materials availability: Materials used to conduct the study are not publicly available.
References
- 1. Bixler E. Sleep and society: An epidemiological perspective. Sleep Med. 2009; 10:S3–S6. [DOI] [PubMed] [Google Scholar]
- 2. Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N.. “Sleep disparity” in the population: Poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010; 10(1):475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Irwin MR. Why sleep is important for health: A psychoneuroimmunology perspective. Annu Rev Psychol. 2015; 66(1):143–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Orzeł-Gryglewska J. Consequences of sleep deprivation. Int J Occup Med Environ Health. 2010; 23(1):95–114. doi: 10.2478/v10001-010-0004-9 [DOI] [PubMed] [Google Scholar]
- 5. Knutson KL, Van Cauter E, Van Cauter E.. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008; 1129(1):287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Williams DR, Mohammed SA, Mohammed SA.. Discrimination and racial disparities in health: Evidence and needed research. J Behav Med. 2009; 32(1):20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arellano-Morales L, Roesch SC, Gallo LC, et al. Prevalence and correlates of perceived ethnic discrimination in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. J Lat Psychol. 2015; 3(3):160–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones CP. Levels of racism: A theoretic framework and a gardener’s tale. Am J Public Health. 2000; 90(8):1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ashing-Giwa KT, Padilla G, Tejero J, et al. Understanding the breast cancer experience of women: A qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psychooncology. 2004; 13(6):408–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Goodkind JR, Gonzales M, Malcoe LH, Espinosa J.. The Hispanic Women’s Social Stressor Scale: Understanding the multiple social stressors of U.S.- and Mexico-born Hispanic women. Hisp J Behav Sci. 2008; 30(2):200–229. [Google Scholar]
- 11. Sharaievska I, Stodolska M, Shinew KJ, Kim J.. Perceived discrimination in leisure settings in Latino urban communities. Leisure/Loisir. 2010; 34(3):295–326. [Google Scholar]
- 12. Clark R, Anderson NB, Clark VR, Williams DR.. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol. 1999; 54(10):805–816. [DOI] [PubMed] [Google Scholar]
- 13. Brondolo E, Blair IV, Kaur A.. Biopsychosocial mechanisms linking discrimination to health: A focus on social cognition. In: Major B, Dovidio JF, Link BG, eds. The Oxford Handbook of Stigma, Discrimination, and Health. New York, NY: Oxford University Press; 2017:219–240. [Google Scholar]
- 14. Buckley TM, Schatzberg AF.. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: Normal HPA axis activity and circadian rhythm, exemplary sleep disorders. Int J Clin Endocrinol Metab. 2005; 90(5):3106–3114. [DOI] [PubMed] [Google Scholar]
- 15. van Dalfsen JH, Markus CR.. The serotonin transporter polymorphism (5-HTTLPR) and cortisol stress responsiveness: Preliminary evidence for a modulating role for sleep quality. Stress. 2018; 21(6):503–510. [DOI] [PubMed] [Google Scholar]
- 16. Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR.. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race Soc Probl. 2013; 5(2):100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM.. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012; 10(4):235–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Slopen N, Williams DR.. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep. 2014; 37(1):147–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Slopen N, Lewis TT, Williams DR.. Discrimination and sleep: A systematic review. Sleep Med. 2016; 18:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Abbott SM, Weng J, Reid KJ, et al. Sleep timing, stability, and BP in the Sueño Ancillary Study of the Hispanic Community Health Study/Study of Latinos. Chest. 2019; 155(1):60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Alcántara C, Patel SR, Carnethon M, et al. Stress and sleep: Results from the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. SSM - Popul Health. 2017; 3:713–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gaston SA, Feinstein L, Slopen N, Sandler DP, Williams DR, Jackson CL.. Everyday and major experiences of racial/ethnic discrimination and sleep health in a multiethnic population of U.S. women: Findings from the Sister Study. Sleep Med. 2020; 71:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Johnson DA, Lewis TT, Guo N, et al. Associations between everyday discrimination and sleep quality and duration among African-Americans over time in the Jackson Heart Study. Sleep. 2021; 44(12):zsab162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ong AD, Williams DR.. Lifetime discrimination, global sleep quality, and inflammation burden in a multiethnic sample of middle-aged adults. Cultur Divers Ethnic Minor Psychol. 2019; 25(1):82–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ayalon L, Gum AM.. The relationships between major lifetime discrimination, everyday discrimination, and mental health in three racial and ethnic groups of older adults. Aging Ment Health. 2011; 15(5):587–594. [DOI] [PubMed] [Google Scholar]
- 26. Kessler RC, Mickelson KD, Williams DR.. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999; 40(3):208–230. [PubMed] [Google Scholar]
- 27. Liu SY, Kawachi I.. Discrimination and telomere length among older adults in the United States. Public Health Rep. 2017; 132(2):220–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lazarus RS, Folkman S.. Stress, Appraisal, and Coping. New York, NY: Springer; 1984. [Google Scholar]
- 29. Carver CS, Scheier MF.. Situational coping and coping dispositions in a stressful transaction. J Pers Soc Psychol. 1994; 66(1):184–195. [DOI] [PubMed] [Google Scholar]
- 30. Perez SM, Gavin JK, Diaz VA.. Stressors and coping mechanisms associated with perceived stress in Latinos. Ethn Dis. 2015; 25(1):78–82. [PubMed] [Google Scholar]
- 31. Brondolo E, Brady ver Halen N, Pencille M, Beatty D, Contrada RJ.. Coping with racism: A selective review of the literature and a theoretical and methodological critique. J Behav Med. 2009; 32(1):64–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nakamura YM, Orth U.. Acceptance as a coping reaction: Adaptive or not? Swiss J Psychol. 2005; 64(4):281–292. [Google Scholar]
- 33. Noh S, Kaspar V.. Perceived discrimination and depression: Moderating effects of coping, acculturation, and ethnic support. Am J Public Health.. 2003;93(2):232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Krieger N, Sidney S.. Racial discrimination and blood pressure: the CARDIA Study of young Black and White adults. Am J Public Health.. 1996;86(10):1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Moody-Ayers SY, Stewart AL, Covinsky KE, Inouye SK.. Prevalence and correlates of perceived societal racism in older African-American adults with type 2 diabetes mellitus. J Am Geriatr Soc. 2005; 53(12):2202–2208. [DOI] [PubMed] [Google Scholar]
- 36. Singleton GJ, Robertson J, Robinson JC, Austin C, Edochie V.. Perceived racism and coping: Joint predictors of blood pressure in Black Americans. Negro Educ Rev. 2008; 59(1/2):125–126. [Google Scholar]
- 37. Ayres MM, Leaper C.. Adolescent girls’ experiences of discrimination: An examination of coping strategies, social support, and self-esteem. J Adolesc Res. 2013; 28(4):479–508. [Google Scholar]
- 38. Lee S, Waters SF.. Asians and Asian Americans’ experiences of racial discrimination during the COVID-19 pandemic: Impacts on health outcomes and the buffering role of social support. Stigma Health. 2021; 6(1):70–78. [Google Scholar]
- 39. Polanco-Roman L, Danies A, Anglin DM.. Racial discrimination as race-based trauma, coping strategies, and dissociative symptoms among emerging adults. Psychol Trauma. 2016; 8(5):609–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Giesbrecht T, Merckelbach H.. Subjective sleep experiences are related to dissociation. Pers Individ Dif. 2004; 37(7):1341–1345. [Google Scholar]
- 41. Van Der Kloet D, Giesbrecht T, Franck E, et al. Dissociative symptoms and sleep parameters—An all-night polysomnography study in patients with insomnia. Compr Psychiatry. 2013; 54(6):658–664. [DOI] [PubMed] [Google Scholar]
- 42. Yıldırım A, Boysan M, Yılmaz O.. The mediating role of pathological worry in associations between dissociative experiences and sleep quality among health staff. Sleep Hypn. 2018; 20(3):190–209. doi: 10.5350/Sleep.Hypn.2017.19.0152 [DOI] [Google Scholar]
- 43. Hoyt MA, Thomas KS, Epstein DR, Dirksen SR.. Coping style and sleep quality in men with cancer. Ann Behav Med. 2009; 37(1):88–93. [DOI] [PubMed] [Google Scholar]
- 44. Riolli L, Savicki V.. Optimism and coping as moderators of the relationship between chronic stress and burnout. Psychol Rep. 2003;92(3_suppl):1215–1226. [DOI] [PubMed] [Google Scholar]
- 45. Melamed S, Ugarten U, Shirom A, Kahana L, Lerman Y, Froom P.. Chronic burnout, somatic arousal and elevated salivary cortisol levels. J Psychosom Res. 1999; 46(6):591–598. [DOI] [PubMed] [Google Scholar]
- 46. Metlaine A, Sauvet F, Gomez-Merino D, et al. Sleep and biological parameters in professional burnout: A psychophysiological characterization. Veauthier C, ed. PLoS One. 2018; 13(1):e0190607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Majeno A, Tsai KM, Huynh VW, McCreath H, Fuligni AJ.. Discrimination and sleep difficulties during adolescence: The mediating roles of loneliness and perceived stress. J Youth Adolesc. 2018; 47(1):135–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM.. Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005; 61(7):1576–1596. [DOI] [PubMed] [Google Scholar]
- 49. Busse D, Yim IS, Campos B.. Social context matters: Ethnicity, discrimination and stress reactivity. Psychoneuroendocrinology. 2017; 83:187–193. [DOI] [PubMed] [Google Scholar]
- 50. Otiniano Verissimo AD, Grella CE, Amaro H, Gee GC.. Discrimination and substance use disorders among Latinos: The role of gender, nativity, and ethnicity. Am J Public Health. 2014; 104(8):1421–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Williams DR, Yan Y, Jackson JS, Anderson NB.. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J Health Psychol. 1997; 2(3):335–351. [DOI] [PubMed] [Google Scholar]
- 52. Molina KM, Estrella ML, Rivera-Olmedo N, Frisard C, Lemon S, Rosal MC.. It weigh(t)s on you: Everyday discrimination and adiposity among Latinos. Obesity (Silver Spring). 2018; 26(9):1474–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ.. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 54. Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, Irwin MR.. Validation of a 3-factor scoring model for the Pittsburgh Sleep Quality Index in older adults. Sleep. 2006; 29(1):112–116. [DOI] [PubMed] [Google Scholar]
- 55. Tomfohr LM, Schweizer CA, Dimsdale JE, Loredo JS.. Psychometric characteristics of the Pittsburgh Sleep Quality Index in English speaking non-Hispanic Whites and English and Spanish speaking Hispanics of Mexican descent. J Clin Sleep Med. 2013; 09(01):61–66. doi: 10.5664/jcsm.2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Dyke ML, Cuffee YL, Halanych JH, McManus RH, Curtin CA, llison JJ.. The relationship between coping styles in response to unfair treatment and understanding of diabetes self-care. Diabetes Educ. 2013; 39(6):848–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Krieger N. Racial and gender discrimination: Risk factors for high blood pressure? Soc Sci Med. 1990; 30(12):1273–1281. [DOI] [PubMed] [Google Scholar]
- 58. Heeringa S, West BT, Berglund PA.. Applied Survey Data Analysis. Boca Raton, FL: CRC Press, Taylor & Francis Group; 2017. [Google Scholar]
- 59. Tabachnick, BG, Fidell, LS.. Using Multivariate Statistics. Boston, MA: Allyn & Bacon/Pearson Education; 2007. [Google Scholar]
- 60. Aiken, LS, & West, SG.. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks, CA: Sage Publications, Inc; 1991. [Google Scholar]
- 61. Hoggard LS, Hill LK.. Examining how racial discrimination impacts sleep quality in African Americans: Is perseveration the answer? Behav Sleep Med. 2018; 16(5):471–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Vaghela P, Sutin AR.. Discrimination and sleep quality among older U.S. adults: the mediating role of psychological distress. Sleep Health. 2016; 2(2):100–108. [DOI] [PubMed] [Google Scholar]
- 63. Steffen PR, Bowden M.. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethn Dis. 2006; 16(1):16–21. [PubMed] [Google Scholar]
- 64. Pichardo CM, Molina KM, Rosas CE, Uriostegui M, Sanchez-Johnsen L.. Racial discrimination and depressive symptoms among Latina/o College students: The role of racism-related vigilance and sleep. Race Soc Probl. 2021; 13:86–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ozier EM, Taylor VJ, Murphy MC.. The cognitive effects of experiencing and observing subtle racial discrimination. J Soc Issues. 2019; 75(4):1087–1115. [Google Scholar]
- 66. Major B, Quinton WJ, McCoy SK.. Antecedents and consequences of attributions to discrimination: Theoretical and empirical advances. Adv Exp Soc Psychol. 2002; 34:251–330. [Google Scholar]
- 67. Harrell SP. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthopsychiatry. 2000; 70(1):42–57. [DOI] [PubMed] [Google Scholar]
- 68. Smyth J, Zawadzki M, Gerin W.. Stress and disease: A structural and functional analysis. Soc Personal Psychol Compass. 2013; 7(4):217–227. [Google Scholar]
- 69. Ashburn-Nardo L, Abdul Karim MF.. The CPR Model. In: Confronting Prejudice and Discrimination. San Diego, CA: Elsevier; 2019:29–47. [Google Scholar]
- 70. Joseph J, Kuo BCH.. Black Canadians’ coping responses to racial discrimination. J Black Psychol. 2009; 35(1):78–101. doi: 10.1177/0095798408323384. [DOI] [Google Scholar]
- 71. Chen E, Miller GE.. “Shift-and-Persist” Strategies: Why low socioeconomic status isn’t always bad for health. Perspect Psychol Sci. 2012; 7(2):135–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Sanchez DT, Himmelstein MS, Young DM, Albuja AF, Garcia JA.. Confronting as autonomy promotion: Speaking up against discrimination and psychological well-being in racial minorities. J Health Psychol. 2016; 21(9):1999–2007. [DOI] [PubMed] [Google Scholar]
- 73. Jang Y, Chiriboga DA, Small BJ.. Perceived discrimination and psychological well-being: The mediating and moderating role of sense of control. Int J Aging Hum Dev. 2008; 66(3):213–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Garcini LM, Chen MA, Brown R, et al. “Abrazame que ayuda” (Hug me, it helps): Social support and the effect of perceived discrimination on depression among U.S.- and foreign-born Latinxs in the USA. J Racial Ethn Health Disparities. 2020; 7(3):481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Michaels EK, Reeves AN, Thomas MD, et al. Everyday racial discrimination and hypertension among midlife African American women: Disentangling the role of active coping dispositions versus active coping behaviors. Int J Environ Res Public Health. 2019;16(23):4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Desjardins S, Lapierre S, Hudon C, Desgagné A.. Factors involved in sleep efficiency: A population-based study of community-dwelling elderly persons. Sleep. 2019; 42(5):zsz038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Yip T, Cheon YM.. Sleep, psychopathology and cultural diversity. Curr Opin Psychol. 2020; 34:123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: The Whitehall II Prospective Cohort Study. Sleep. 2009; 32(6):737–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Brissette I, Cohen S.. The contribution of individual differences in hostility to the associations between daily interpersonal conflict, affect, and sleep. Pers Soc Psychol Bull. 2002;28(9):1265–1274. [Google Scholar]
- 80. Clarke AT. Coping with interpersonal stress and psychosocial health among children and adolescents: A meta-analysis. . J Youth Adolescence. 2006; 35(1):10–23. [Google Scholar]
- 81. Dudley KA, Weng J, Sotres-Alvarez D, et al. Actigraphic sleep patterns of U.S. Hispanics: The Hispanic Community Health Study/Study of Latinos. Sleep. 2017; 40(2):zsw049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Araujo-Dawson B. Understanding the complexities of skin color, perceptions of race, and discrimination among Cubans, Dominicans, and Puerto Ricans. Hisp J Behav Sci. 2015; 37(2):243–256. [Google Scholar]
- 83. Gordon AM, Prather AA, Dover T, Espino-Pérez K, Small P, Major B.. Anticipated and experienced ethnic/racial discrimination and sleep: A longitudinal study. Pers Soc Psychol Bull. 2020; 46(12):1724–1735. [DOI] [PubMed] [Google Scholar]
- 84. Viruell-Fuentes EA. Beyond acculturation: Immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med. 2007; 65(7):1524–1535. [DOI] [PubMed] [Google Scholar]
- 85. Lewis TT, Yang FM, Jacobs EA, Fitchett G.. Racial/ethnic differences in responses to the Everyday Discrimination Scale: A differential item functioning analysis. Am J Epidemiol. 2012; 175(5):391–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Pérez DJ, Fortuna L, Alegría M.. Prevalence and correlates of everyday discrimination among U.S. Latinos. J Community Psychol. 2008; 36(4):421–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Martinez JH, Suyemoto KL, Abdullah T, Burnett-Zeigler I, Roemer L.. Mindfulness and valued living in the face of racism-related stress. Mindfulness. 2022; 13(5):1112–1125. doi: 10.1007/s12671-022-01826-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Crowe M, Jordan J, Burrell B, Jones V, Gillon D, Harris S.. Mindfulness-based stress reduction for long-term physical conditions: A systematic review. Aust N Z J Psychiatry. 2016; 50(1):21–32. [DOI] [PubMed] [Google Scholar]
- 89. Greeson JM, Zarrin H, Smoski MJ, et al. Mindfulness meditation targets transdiagnostic symptoms implicated in stress-related disorders: Understanding relationships between changes in mindfulness, sleep quality, and physical symptoms. Evid Based Complement Alternat Med. 2018; 2018:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Krause N, Rainville G.. Exploring the relationship between social support and sleep. Health Educ Behav. 2020; 47(1):153–161. [DOI] [PubMed] [Google Scholar]
- 91. Greenberg J. Losing sleep over organizational injustice: Attenuating insomniac reactions to underpayment inequity with supervisory training in interactional justice. J Appl Psychol. 2006; 91(1):58–69. [DOI] [PubMed] [Google Scholar]
- 92. Elias A, Paradies Y.. Estimating the mental health costs of racial discrimination. BMC Public Health. 2016; 16(1):1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Hafner M, Troxel W.. Americans Don’t Sleep Enough, and It’s Costing Us $411 billion. The RAND Blog; Published November 30, 2016. https://www.rand.org/blog/2016/11/americans-dont-sleep-enough-and-its-costing-us.html. Accessibility verified June 3, 2022. [Google Scholar]
- 94. Dubina K. Hispanics in the Labor Force: 5 Facts. U.S. Department of Labor Blog. Published September 15, 2021. https://blog.dol.gov/2021/09/15/hispanics-in-the-labor-force-5-facts#:~:text=The%20Hispanic%20proportion%20of%20the,labor%20force%2C%20at%2021.2%25. Accessibility verified June 3, 2022. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.