Introduction and importance:
Necrotizing fasciitis (NF) represents a rapidly progressive, life-threatening infection involving the fascia and subcutaneous tissue. Early diagnosis and intervention are crucial to treat, especially in diabetic patients.
Case presentation:
This case report presents on a patient with diabetes mellitus rapidly developed a NF of the upper extremities following a minor trauma in the palmar of greater thenar. In the initial stages of her hospital admission, severe hand soft tissue infection, and systemic toxicity is the most prominent clinical manifestation. During her hospitalization, efficacious multidisciplinary treatment was carried out to avoid severe consequences.
Clinical discussion and conclusion:
The objective of this case report is to present a successful individual strategy in a complex case to standardize the treatment process. Accurate and standardized management can improve the prognosis of patients affected from upper extremities NF of diabetic avoiding and severe complications and saving lives.
Keywords: case report, diabetes mellitus, necrotizing fasciitis
Introduction
Highlights
Necrotizing fasciitis is a disease with high mortality and disability.
Early diagnosis of the necrotizing fasciitis may be lifesaving.
Promptly debridement is essential to improve the prognosis of the disease.
A multidisciplinary approach is recommended for successful treatments.
Necrotizing fasciitis (NF) is a rarely, devastating, and progressively fatal infection that will involve the subcutaneous fat and deep fascial layers1. NF was first named by Wilson in 1952, with describing the cardinal features of the disease2,3.
There is an increased incidence in Asian and African countries, recently4 seeing that the pathophysiological characteristics of diabetes mellitus (DM), DM is the most common comorbidity of NF and diabetic patients predispose to cause higher mortality rates5. Therefore, it is particularly important to standardize the diagnosis and treatment process of NF for diabetic patients.
Upper extremities of infection disease in diabetic are rare compared to foot complications occurring in a ratio of 1:206. But the mortality rates related to upper and lower limb involvement were similar7. In clinical, diabetic foot disease is ubiquitous and the cognition has been well improved. However, to the best of our knowledge, the upper extremities of diabetic NF have neither been widely reported nor gained satisfactorily treatment. Here, our manuscript aims to standardize and guide the treatment of patients with upper limb NF through this index case. This report was written following the Surgical CAse REport (SCARE) 2020 Criteria8,9.
Presentation of case
A 77-year-old woman was referred to our center with an infection of the upper extremities (right forearm). The basic information of the patient is shown in Table 1. Five days ago, the thenar of her right hand was slightly scratched by a branch. Swelling and purulent exudation occurred rapidly at the wound site. And erythema and swelling spread to the whole hand. Meanwhile, she developed fever, anorexia, and fatigue symptoms. The patient went to the local community clinic. She received intravenous antibiotics for 3 days and underwent the incision for drainage. However, pain and swelling spread to the whole forearm within the following 2 days. The clinical symptoms and signs of the patients kept worsening. Then, the patient was then transferred to our center.
Table 1.
Characteristics of the patient
| Age (years) | 77 |
|---|---|
| Sex | Female |
| Social background | Farmer |
| Duration of diabetes (years) | 10 |
| BMI (kg/m2) | 22.1 |
| Blood sugar management | Bad control |
| Comorbidities | Hypertension, Arrhythmias including intraventricular block, Coronary heart disease, Old myocardial ischemia |
After admission to our hospital, a physical examination revealed listless-looking woman with no febrile. The right hand and forearm were swollen, warm, numbness. There are a 15 cm long incision along the shape of the palmaris longus muscle to the proximal end filled with black necrosis in the palm and forearm, a large amount of pus flowed out of the wound, and local metacarpal fascia was exposed. The infection was up to the forearm, about 3 cm below the elbow (Fig. 1A, B). A blood test showed a relatively high index of inflammation status (LRINEC score, Table 2). Radiography showed that there was no abnormality in bone. The wound swab was taken for bacterial culture to guide the following use of antibiotics. Before the result of germiculture returns, the combination of cefotaxime sulbactam and ornidazole were utilized for almost 10 days. The broad-spectrum antibiotics was given priority to be considered. NF was considered as preliminary diagnosis. Aggressive surgical debridement was performed immediately, on the first day of admission. During the operation, the infection part was fully dissected for drainage, all the visible necrotic tissues and tendon was removed, and the important blood vessels and nerves were protected as much as possible.
Figure 1.

Clinical photographs of wound healing process of necrotizing fasciitis of upper extremities in diabetic patients. Initially presentation when the patient just entered our institution, were shown as (A, B); C showed the wound 8 days after emergency debridement; The wounds after the second debridement and the second round of VSD were as shown in D; E and F represented autologous intermediate-thickness skin grafting from the patient’s ipsilateral thigh and 2 weeks after operation, respectively. The follow-up assessment at 3 (G), 6 (H) months from the first surgery.
Table 2.
Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score
| Variable (units) | Value | LRINEC score |
|---|---|---|
| CRP (mg/l) | 151 | 4 |
| WBC (cell/mm3) | 15.4 | 1 |
| Hgb (g/dl) | 11.3 | 1 |
| Sodium (mmol/l) | 132 | 2 |
| Creatinine (mg/dl) | 0.37 | 0 |
| Glucose (mg/dl) | 277 | 1 |
CRP, C-Reactive Protein; WBC, White Blood Cell Count; Hgb, Hemoglobin; LRINEC, Laboratory Risk Indicator for Necrotizing Fasciitis.
Furthermore, effective systemic support treatments are applied during the perioperative period. The modalities included the empirical use of broad-spectrum antibiotics, maintaining the balance of water-electrolyte and acid-base equilibrium, rectification of hypoproteinemia, and tight glycemic control. The patient’s blood pressure and coagulation function were also monitored and properly adjusted. Strict internal medicine management to help patients improve surgical endurance.
Eight days later, after systemic medical treatment and dressing of the wound, the general condition and wound infection of the patient were significantly improved compared with those at admission (Fig. 1C). The second debridement was opted. In this operation, the residual necrotic tissue was further removed and the surviving palmaris longus tendon was retained as much as possible, so as to cover the median nerve. Finally, wounds were partly sutured and negative pressure drainage technic was used to promote wound growth and culture granulation tissue.
At the 15th day from the admission, the patient underwent the third surgery. After two debridement operations combined with negative pressure suction, the bed of the wound has been prepared well (Fig. 1D). According to the laboratory results, the culture of wound secretion taken during the second debridement showed no bacterial growth. Autologous intermediate-thickness skin grafting from the patient’s ipsilateral thigh was intermittently implanted into the defect area of the right palm and forearm (Fig. 1E). Two weeks after the operation, the grafted skin survived well and the wound healed completely (Fig. 1F). After being discharged from the hospital, the patient was instructed to perform functional exercise focusing on wrist flexion and extension.
At the follow-up at 3 months, the patient reported that the activity function of the fingers and wrists had almost recovered to a normal level (Fig. 1G). In December 2020, the last follow-up at 6 months, the two-point discrimination of each finger (two-point discrimination experiment) also returned to normal (Fig. 1H).
Discussion
This study is to report a successful therapy and functionally reconstruction case of NF of the upper extremities in a diabetic patient. We deemed that this process can be used as a treatment standard for the upper limb treatment of diabetic NF.
NF is a clinically challenging disease that doctors must be aware of, which requires a rapid diagnosis, early and extensive surgical debridement and treatment with appropriate antibiotics. The early diagnosis of the NF may be lifesaving because the lesions of NF progress rapidly, followed by a high possibility of sepsis, a high risk of amputation, and a high mortality rate5. In our case report, it took only 3 days for the infection zone of the patient to go from the palm over the wrist joint to the three fingers of the distal forearm, and during emergency surgery, it was observed that the infection zone had spread from the deep forearm to about three fingers below the elbow joint. These studies have validated the importance of an early diagnosis of the disease. However, its rarity and the paucity of early pathognomonic signs often make NF being misdiagnosis as a normal soft tissue infection, the initial misdiagnosis even was occurred in almost three-quarters of patients10. Our team was composed of experienced orthopedic surgeons, endocrinologists, as well as working closely with vascular surgeons and ICU physicians. Based on the patient’s medical history, physical examination, and auxiliary examinations, our team’s doctors quickly diagnosed suspected diabetes with NF (right forearm). After that, interdisciplinary treatment was given promptly and emergency exploratory surgery was given, and diabetes with NF (right forearm) was determined with the support of exploratory surgery. And the early diagnosis of NF lays a solid foundation for a satisfactory prognosis.
The patient in this case is an elderly female patient with DM, and with multiple basic diseases, such as hypertension. When diagnosed as suspected NF, the patient was treated with comprehensive multidisciplinary treatments, and an emergency debridement operation was prepared. In these comprehensive multidisciplinary treatments, empirical broad-spectrum antibiotics was firstly used for patient, many previous studies also showed that the timely use of antibiotics will be benefit for the restoration of NF. Moreover, DM was a risk factor for NF10 , and was assigned with a significant higher risk for amputation5. A patient with diabetic foot showed that no formal hypoglycemic therapy contributed to the development of NF Shang et al.11 also showed hyperglycemia may contribute to NF, and the perioperative glycemic control is of vital importance for this disease therapy. Glycemic of the patient in this case was regulated by insulin and the blood sugar was controlled at about 10 mmol/l. Besides, maintenance of water and electrolyte, acid-base and protein balance, antihypertensive, and anticoagulant treatments was also carried out for patient life support. Arterial blood gases should be monitored and kept in a normal range (PH value is 7.35–7.45, standard bicarbonate radical range is 22–26 mmol/l). These results showed comprehensive multidisciplinary treatments was another key factor for NF (right forearm) treatment, which is also a highlight in our treatment process.
The application of antibiotics is an obligatory tool that supports the surgical therapy and is intimately connected to the mortality. According to the microbiological findings of wound secretion, NF was divided into four types. In addition to the most frequent type I (polymicrobial infection), type III (Vibrio vulnificus) is the main monomicrobial infection and with high mortality of in the upper limbs of NF diabetes. Therefore, the early use of antibiotics in the treatment of NF in the upper limbs should be based on the principle of board-spectrum antibiotics, especially covering streptococci, staphylococci, gram-negative rods, and anaerobes. In this case, initially broad-spectrum antibiotics was chosen, and later the use of antibiotics was adjusted according to the results of bacterial culture.
The emergency incision and drainage and removal of necrotic tissue is important for the treatments. A previous study showed the delay of surgical intervention and inadequate initial debridement of NF would cause a significantly higher mortality rate, and a delay beyond 12 h can be fatal12. The survival rate of NF lies approximately around 93% if the time between the admission and the first debridement does not exceed the 24 h, decreasing dramatically to 75% at 48 h13. Moreover, survivors were also undergone repeated debridement operation for 2–4 times14. Multiple surgeries with different purposes are also operated in our plan. Previous studies have shown hand dysfunction and stiffness are common after hand treatment in hand infections patients. During and after surgery, more attention should be paid to the maintenance and recovery of hand function; in this case, we have strengthened the protection of important blood vessels, tendons, and nerves from the first emergency operation, and in next operations. Focusing on soft tissue reconstruction and assisting with continuous physical function exercises, the patient’s hand flexion function was finally recovered well. In conclusion, when DM is complicated with NF in the arm, it is not only necessary to perform emergency diagnosis and treatment according to NF, but also the special anatomical structure and functional requirements of the hand. Because of the anatomical characteristics, the NF of the upper limb needs to pay more attention to the protection of fine function than that of the lower limb. The treatment of NF in the lower limbs, especially in the foot, should focus on the decompression treatment of the foot to prevent the recurrence of ulcer.
In summary, this special flow chart of clinical diagnosis and treatment of diabetes complicated with arm NF (Fig. 2) was formulated according to the treatment process of this patient. It is very practical and effective and can be referred to by more medical workers.
Figure 2.
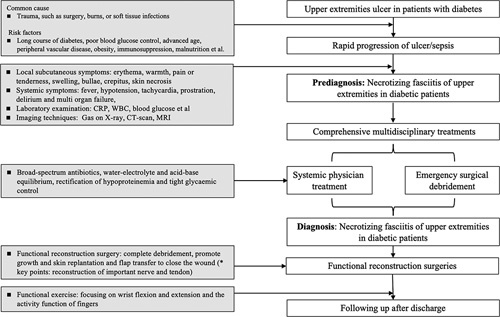
Management algorithm.
Conclusion
In view of the extremely dangerous condition of NF, and the lack of standard treatment in upper limb NF, this case emphasizes early diagnosis and rapidly receiving standardized therapy. It is essential to enhance medical workers’ consciousness to avoid delays in diagnosis and ensure practical and effective management.
Ethical approval
No ethical approval is needed for this type of publication in our institution. The patients provided written informed consent for all treatments and procedures, and for publication of this report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
This work was supported by National Natural Science Foundation of China (NO. 81770810) and research funded projects of Junxie hospital (NO. 21YY008).
Author contributions
W.T.Y. and J.D.: drafted the manuscript; W.W., C.Y.C., and J.-S.S.: collected and analyzed the data; W.A.P. and C.Y.D.: contributed to study conception and revised the manuscript; S.B.: undertook the follow-up work. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest disclosure
The authors declare that there is no conflict of interest.
Provenance and peer review
Not commissioned, externally peer reviewed.
Registration of research studies
Name of the registry: NA.
Unique Identifying number or registration ID: NA.
Hyperlink to your specific registration (must be publicly accessible and will be checked): NA.
Guarantor
Dr Ai-ping Wang, Endocrinologist.
E-mail: waphospital454@126.com
Contact Number: +86 132 7075 1818
Footnotes
Tian-yuan Wang and Dong Jiang contributed equally to this work and are co-first authors.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 11 April 2023
Contributor Information
Tian-yuan Wang, Email: wtyuan_123@163.com.
Dong Jiang, Email: 1186833396@qq.com.
Wei Wang, Email: 95409000@qq.com.
Yin-chen Chen, Email: gheatcyc@163.com.
Jin-shan Sun, Email: 1210245884@qq.com.
Bo Sun, Email: shsunbuo@163.com.
Yue-dong Chen, Email: chenyd727@163.com.
References
- 1. Baiu I, Staudenmayer K. Necrotizing soft tissue infections. JAMA 2019;321:1738. [DOI] [PubMed] [Google Scholar]
- 2. Wilson B. Necrotizing fasciitis. Am Surg 1952;18:416–431. [PubMed] [Google Scholar]
- 3. Carter PS, Banwell PE. Necrotising fasciitis: a new management algorithm based on clinical classification. Int Wound J 2004;1:189–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers C. for Disease, Prevention, Tropical diabetic hand syndrome–Dar es Salaam, Tanzania, 1998-2002. MMWR Morb Mortal Wkly Rep 2002;51:969–970. [PubMed] [Google Scholar]
- 5. Leiblein M, Marzi I, Sander AL, et al. Necrotizing fasciitis: treatment concepts and clinical results. Eur J Trauma Emerg Surg 2018;44:279–290. [DOI] [PubMed] [Google Scholar]
- 6. Yeika EV, Tchoumi Tantchou JC, Foryoung JB, et al. Tropical diabetic hand syndrome: a case report. BMC Res Notes 2017;10:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Espandar R, Sibdari SY, Rafiee E, et al. Necrotizing fasciitis of the extremities: a prospective study. Strategies Trauma Limb Reconstr 2011;6:121–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lukowiak TM, Aizman L, Perz A, et al. Association of age, sex, race, and geographic region with variation of the ratio of basal cell to cutaneous squamous cell carcinomas in the United States. JAMA Dermatol 2020;156:1192–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Agha RA, Franchi T, Sohrabi C, et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) Guidelines. Int J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 10. Goh T, Goh LG, Ang CH, et al. Early diagnosis of necrotizing fasciitis. Br J Surg 2014;101:e119–e125. [DOI] [PubMed] [Google Scholar]
- 11. Shang S, Zhang R, Hou Z. Necrotizing fasciitis-A catastrophic complication following routine tibia fracture surgery: a case report and literature review. Medicine (Baltimore) 2017;96:e6908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Misiakos EP, Bagias G, Papadopoulos I, et al. Early diagnosis and surgical treatment for necrotizing fasciitis: a multicenter study. Front Surg 2017;4:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wong CH, Chang HC, Pasupathy S, et al. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 2003;85:1454–1460. [PubMed] [Google Scholar]
- 14. Vayvada H, Demirdover C, Menderes A, et al. Necrotising fasciitis in the central part of the body: diagnosis, management and review of the literature. Int Wound J 2013;10:466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]


