Abstract
Rinderpest virus (RPV) causes a severe disease of cattle resulting in serious economic losses in parts of the developing world. Effective control and elimination of this disease require a genetically marked rinderpest vaccine that allows serological differentiation between animals that have been vaccinated against rinderpest and those which have recovered from natural infection. We have constructed two modified cDNA clones of the vaccine strain RNA genome of the virus, with the coding sequence of either a receptor site mutant form of the influenza virus hemagglutinin (HA) gene or a membrane-anchored form of the green fluorescent protein (GFP) gene (ANC-GFP), inserted as a potential genetic marker. Infectious recombinant virus was rescued in cell culture from both constructs. The RPVINS-HA and RPVANC-GFP viruses were designed to express either the HA or ANC-GFP protein on the surface of virus-infected cells with the aim of stimulating a strong humoral antibody response to the marker protein. In vitro studies showed that the marker proteins were expressed on the surface of virus-infected cells, although to different extents, but neither was incorporated into the envelope of the virus particles. RPVINS-HA- or RPVANC-GFP-vaccinated cattle produced normal levels of humoral anti-RPV antibodies and significant levels of anti-HA or anti-GFP antibodies, respectively. Both viruses were effective in stimulating protective immunity against RPV and antibody responses to the marker protein in all animals when tested in a cattle vaccination trial.
Rinderpest virus (RPV) is a nonsegmented negative-strand RNA virus which is classified in the Morbillivirus genus of the family Paramyxoviridae. It is the causative agent of rinderpest, a severe and highly contagious disease of wild and domestic ruminants characterized by very high morbidity and mortality rates and thus of great economic importance in affected countries in Africa and Asia (6). Only a single serotype of RPV is known, although there is considerable variation in the virulence and pathogenicity of field isolates (26). RPV is genetically and antigenically very closely related to other viruses in the Morbillivirus genus such as measles virus (MV).
Global eradication of rinderpest is planned to be achieved by the year 2010 (21, 27). In the final stages of this campaign, countries will have to stop vaccination and show that in the absence of herd immunity, there is no hidden disease resulting from circulating mild strains of the virus. However, a rinderpest vaccine will still be required in the transition phase of local eradication campaigns and for emergency vaccination during isolated outbreaks of the disease. The most commonly used RPV vaccine is the Plowright attenuated RBOK strain, which was derived by multiple passage in cell culture of the virulent Kabete ‘O’ strain (18). The RBOK vaccine is safe and extremely effective, providing complete and lifelong protection from rinderpest with a single inoculation (17, 18). As there is only one serotype of RPV, including the vaccine, it is not possible to distinguish serologically between cattle which have recovered from a natural infection and those which have been vaccinated. A genetically marked rinderpest vaccine which could readily be distinguished from wild-type strains would be of great value during the final phases of the eradication campaign. It would then be possible to use vaccination without interfering with the ability to carry out serological surveys to detect the continued presence of disease.
In a previous paper we reported on the development of recombinant RPV vaccines RPVINS-GFP and RPVSIG-GFP, which expressed intracellular and secreted forms of green fluorescent protein (GFP), respectively, as potential genetic markers (30). The efficacy of these vaccines was tested in a standard cattle vaccination trial. Both viruses provided complete protection from rinderpest when animals were challenged with virulent virus. Intracellular expression of GFP failed to induce anti-GFP antibody in any of the vaccinated cattle; secretion of GFP gave rise to a significant anti-GFP antibody response, but in only half of the vaccinated cattle. This indicated that extracellular expression of the marker protein improved the antibody response, but simple secretion of the protein was still insufficient for the generation of a strong and uniform antimarker humoral antibody response in all vaccinated animals. Therefore, other expression strategies, or other marker genes, were needed to produce a more effective humoral antibody response in vaccinated cattle. Here we report the successful development of two genetically marked recombinant RPV vaccines expressing foreign membrane-anchored proteins. The recombinant viruses produced, RPVINS-HA and RPVANC-GFP, expressed in the first case a receptor site mutant form of the influenza virus hemagglutinin (HA) protein and in the second case a membrane-anchored form of GFP (ANC-GFP) as marker proteins. The expression of these recombinant marker proteins by virus-infected cells, their localization in a cell line and bovine cells in vitro, and the incorporation of marker protein into virus envelopes were examined. Finally, the efficacy of these viruses in providing complete immunity to rinderpest and eliciting a strong antibody response to the marker protein was demonstrated in a cattle vaccination trial.
MATERIALS AND METHODS
Cell culture and viruses.
Cell culture, virus growth, and determination of virus titers and growth rates were carried out as previously described (4, 5, 30). The cells used in this study were 293 (a human embryonal kidney cell line), B95a (an Epstein-Barr virus-transformed marmoset lymphoblastoid cell line), and Vero (an African green monkey kidney cell line). Influenza A/Aichi/2/68 (H3N2) virus X31 strain (allantoic fluid from virus grown in chicken eggs) was provided by John McCauley (Institute for Animal Health, Compton, United Kingdom), and titrations were carried out using MDCK (Madin-Darby canine kidney) cells.
Construction of pRPVINS-HA and pRPVANC-GFP.
The pRPVINS-HA genomic cDNA clone was constructed by inserting an influenza virus HA double mutation gene sequence into the pRPVINS genomic plasmid (5). This HA sequence was constructed by combining two receptor site mutations of the influenza A/Aichi/2/68 (H3N2) virus X31 strain HA gene derived from plasmids pRB21-HA-Y98F and pRB21-HA-L194A (provided by D. A. Steinhauer), which encode the amino acid changes tyrosine 98 to phenylalanine (Y98F) and leucine 194 to alanine (L194A), respectively (15). Plasmid pRB21-HA-Y98F was digested with XhoI and HincII, pRB21-HA-L194A was digested with HincII and PstI, and the two relevant fragments each containing a single mutation were ligated into pGEM7Zf(+). The double mutation HA-Y98F-L194A gene sequence (hereafter designated HA) was then amplified from this plasmid using Pfu polymerase (Stratagene) and the primers 5′ACTAAGCGCGCATTAATCATGAAGACCATCATT3′ and 5′TAATGCGCGCTAATACACTCAAATGCAAATGTT3′ (BssHII sites underlined). The PCR product of the mutant HA open reading frame (ORF) was digested with BssHII; as BssHII and AscI have compatible ends, the 1,722-bp fragment was then ligated into AscI-digested pRPVINS.
The pRPVANC-GFP genomic cDNA clone was constructed by fusing the EGFP (enhanced GFP) gene sequence (Clontech) to the influenza virus HA membrane anchor sequence and inserting this ANC-GFP gene sequence into the pRPVSIG genomic plasmid (30). The HA anchor sequence was amplified from plasmid pRB21-HA-L194A using Pfu polymerase (Stratagene) and the primers 5′ATATTATGTACAAGTCTGGATACAAAGACTGGA3′ (BsrGI site underlined) and 5′ATAATATAAGCTTTCATCAAATGCAAATGTTGCACCT3′ (HindIII site underlined). The PCR product was digested with BsrGI and HindIII and then ligated into BsrGI- and HindIII-digested pEGFP-C1 (Clontech) to make plasmid pEGFP-HA. The ANC-GFP fusion gene sequence was amplified from this plasmid using Pfu polymerase and the primers 5′CGTAGCGCGCAATGGTGAGCAAGGGCGAGGAGCTGT3′ (BssHII site underlined) and 5′ATAATGGCGCGCCGAAGCTTTCATCAAATGCAA3′ (AscI site underlined). The PCR product was digested with BssHII, and the 864-bp fragment was then ligated into AscI-digested pRPVSIG, placing the ANC-GFP ORF in frame with the signal sequence.
In each case one clone was selected, the identity of the HA or ANC-GFP ORF inserted into the pRPVINS or pRPVSIG AscI restriction site was confirmed by sequencing, and the DNA was then used for virus rescue. The genome length of each recombinant virus was an exact multiple of six (7).
Transfection and recovery of infectious recombinant viruses.
293 cells in six-well plates were transfected as previously described (30), with the following modifications. For each well, 2 μg of genome plasmid was used and the cells were transfected using Transfast reagent (Promega) at a ratio of 6 μl of Transfast per μg of DNA, according to the manufacturer's instruction, after the cells had been infected with recombinant virus MVA-T7. The cells were then incubated at 37°C for 1 h with the DNA-Transfast reagent mixture, and 1.4 ml of Dulbecco's modified Eagle's medium containing 10% fetal calf serum was added to each well. Cells were incubated at 37°C for 2 days. Virus was extracted and used to infect B95a cells and Vero cells as previously described. Reverse transcriptase-PCR (RT-PCR) for identification of recombinant RPVs was carried out as previously described (30).
Radioimmunoprecipitation analysis of HA and ANC-GFP proteins.
Radioimmunoprecipitations were carried out using virus-infected B95a cells as previously described (5), with the following modifications. Antibodies used were 0.5 μl of rabbit anti-HA polyclonal antibody (provided by D. A. Steinhauer), 0.5 μl of polyclonal rabbit anti-GFP antibody (Clontech), and 0.2 μl of mouse anti-RPV P (phosphoprotein) monoclonal antibody 2-1 (5) together with 0.5 μl of rabbit anti-mouse antibody (Dakopatts).
Confocal fluorescence microscopy.
B95a cells infected with virus rescued from an unaltered RPV genome copy (RPVII), from RPVINS-HA, or from RPVANC-GFP at a multiplicity of infection (MOI) of 0.1 were grown in flasks at 37°C. At 2 days postinfection, the cells were detached by shaking, the cell suspension was transferred to tubes, and the cells were pelleted by centrifugation at 400 × g for 5 min. The cells were fixed using 3% paraformaldehyde in phosphate-buffered saline (PBS) for 1 h and washed in PBS. The cells were then used for labeling of surface proteins. For labeling of internal proteins, the cells were first permeabilized with PBS–0.1% Triton X-100 (Sigma) for 10 min and then washed with PBS. Nonspecific binding to cells was blocked by incubating cells in PBS–0.5% bovine serum albumin (Sigma) (PBS-BSA) for 30 min. The cells were then washed with PBS. Proteins were labeled by incubating the cells with primary antibody diluted in PBS-BSA for 1 h. RPV H (hemagglutinin) protein was detected with mouse anti-RPV H monoclonal antibody RC19 (31) diluted 1:40. RPV P was detected with mouse anti-RPV P monoclonal antibody 2-1 diluted at 1:500. Influenza virus HA was detected with rabbit anti-HA polyclonal antibody diluted 1:500. GFP was detected both by GFP fluorescence and with rabbit anti-GFP polyclonal antibody diluted 1:500. The cells were then washed in PBS. Primary antibodies were detected by incubation of cells for 1 h with secondary antibodies diluted 1:500 in PBS-BSA, using Texas red-conjugated goat anti-mouse immunoglobulin G (IgG) (Molecular Probes), Texas red-conjugated goat anti-rabbit IgG (Molecular Probes), and marina blue-conjugated goat anti-mouse IgG (Molecular Probes). The cells were washed in PBS and resuspended in PBS. The cells were attached to coverslips by incubating the cell suspensions on poly-l-lysine (Sigma)-coated coverslips for 30 min; then the cells were washed in PBS, and the coverslips were mounted using Vectashield (Vector Laboratories).
Bovine peripheral blood leukocytes (PBL) were extracted from 10-ml samples of cattle blood as follows. Samples were centrifuged at 1,000 × g for 10 min. The buffy coat was removed and diluted in 10 ml of PBS, the mixture was underlaid with 10 ml of Histopaque 1083 (Sigma), and the samples were centrifuged at 800 × g for 25 min. The PBL were removed, washed with PBS, then pelleted by centrifugation at 200 × g, resuspended in RPMI 1640 medium, and aliquoted into a six-well plate. The PBL were stimulated to proliferate by adding 200 μl of phytohemagglutinin (100 μg/ml in RPMI 1640; Sigma) to each well. The cells were then infected with RPVII, RPVINS-HA, or RPVANC-GFP at an MOI of 0.1 and incubated for 2 days at 37°C. The cells and medium were removed, and the PBL were attached to coverslips by centrifugation at 200 × g for 5 min in a Cytospin 3 centrifuge (Shandon). PBL on the coverslips were washed three times with PBS, then fixed using 3% paraformaldehyde for 20 min, washed with PBS, incubated in 50 mM ammonium chloride in PBS for 10 min, and washed again. Cells were used directly or were permeabilized with 0.1% Triton X-100 as described above. Proteins were labeled by incubating the cells for 1 h with primary antibody diluted in PBS-BSA. The cells were then washed with PBS-BSA and PBS. Primary antibodies were detected by incubation of cells for 1 h with secondary antibodies diluted in PBS-BSA. Primary and secondary antibodies and concentrations used were the same as for B95a cell labeling. The cells were washed with PBS, and then the coverslips were mounted using Mowiol (Calbiochem). Transmitted light and fluorescence microscopy was carried out using a Leica confocal microscope.
Assay for protein incorporation into the virus envelope.
Antibody (a very large excess confirmed as sufficient to precipitate control virus) and 104 50% tissue culture infective doses (TCID50) of virus were combined in a total volume of 400 μl of PBS. Samples were incubated for 1 h on ice and mixed briefly at 10-min intervals; then 40 μl of protein A-Sepharose was added to each sample, and the samples were incubated for 1 h on ice with mixing as before. The samples were clarified by centrifugation at 12,000 × g at 4°C, and the supernatants were used for virus titration. Supernatants from the RPV samples were titrated using B95a cells, and the influenza A virus X31 samples were titrated using MDCK cells. The antibodies used in the assay were rabbit RPV hyperimmune antiserum (WRL, Pirbright, Surrey, United Kingdom), rabbit nonimmune antiserum, rabbit anti-HA polyclonal antibody, and rabbit anti-GFP polyclonal antibody.
Immunoelectron microscopy.
B95a cells infected with RPVII or RPVINS-HA at an MOI of 0.1 were grown in flasks at 37°C. At 2 days postinfection, the cells were detached by shaking, the cell suspension was transferred to tubes, and the cells were pelleted by centrifugation at 400 × g for 5 min. The cells were fixed using 2% paraformaldehyde in PBS for 20 min and then washed in PBS. Nonspecific binding to cells was blocked by incubating cells in PBS–0.5% BSA for 30 min. Cell surface proteins were labeled by incubating the cells with primary antibody diluted in PBS-BSA for 1 h. RPV H protein was detected with mouse anti-RPV H monoclonal antibody RC19 diluted 1:40; influenza virus HA was detected with rabbit anti-HA polyclonal antibody diluted 1:100. The cells were then washed in PBS. Primary antibodies were detected by incubation of cells for 1 h with secondary antibodies diluted 1:40 in PBS-BSA, using 5-nm-gold-conjugated goat anti-mouse IgG or 10-nm-gold-conjugated goat anti-rabbit IgG (A P Biotech). After being washed with PBS, the cells were fixed in phosphate-buffered 2% glutaraldehyde (Agar Scientific) for 2 h and then in phosphate-buffered 2% osmium tetroxide (Agar Scientific) overnight. The cells were dehydrated in ethanol and embedded via 1,2-epoxypropane (Agar Scientific) in epoxy resin (Agar Scientific). Ultrathin sections were cut with a diamond knife, then contrasted with uranyl acetate and lead citrate (Leica EM stain), and viewed in a Jeol 1200EX transmission electron microscope.
Assay for influenza virus HA receptor binding function.
Vero cells (106 per well in six-well plates) were infected with RPVINS-HA or RPVII at an MOI of 1 or given PBS (negative control). MDCK cells (106 per well in six-well plates) were infected with influenza A virus X31 at an MOI of 1 or given PBS (negative control). The cells were incubated for 2 days at 37°C. Chicken red blood cells (RBC) in Alsever's saline (75 mM sodium chloride, 100 mM glucose, 25 mM trisodium citrate dihydrate [pH 6.1]) were diluted 1:4 in PBS and centrifuged at 500 × g for 5 min for pelleting. The RBC were washed twice in PBS and then resuspended in 20 ml of PBS. Confluent virus-infected or control cells were washed with PBS; then 1 ml of RBC diluted in PBS was added to each well, and the cells were incubated for 40 min at 37°C. The cells were then washed extensively with PBS and scored for agglutination of RBC to the cell layer.
Vaccination and challenge experiments.
Twelve Friesian cattle between 6 and 12 months of age were used in the vaccination trial; four cattle were vaccinated with RPVINS-HA vaccine, four were vaccinated with RPVANC-GFP vaccine, and four were vaccinated with the rescued virus RPVII as controls. The cattle were challenged with the RPV Saudi 1/81 strain at 4 weeks postvaccination. Vaccines and challenge viruses were each administered diluted in PBS by subcutaneous injection using a dose of 104 TCID50 per animal. Blood and eye swabs were collected on specific days postvaccination. PBL were counted in a hemocytometer. Eye swabs were stored in 1 ml of Trizol (Gibco) at −20°C for RNA extraction. The presence of virus in lachrymal secretions was determined by RT-PCR as previously described (30), using RPV-specific PCR primers (RPV-F3 and RPV-F4) and bovine actin-specific PCR primers (BA1 and BA2) as an RNA positive control (9).
ELISA for the detection of RPV, influenza virus HA, and GFP antibodies.
Cattle serum samples for testing by enzyme-linked immunosorbent assay (ELISA) were prepared from coagulated blood. ELISAs were carried out for anti-RPV H antibodies using the RPV competitive ELISA (2) and for anti-GFP antibodies using an indirect ELISA as previously described (30). The anti-HA antibody response was detected using an indirect ELISA as previously described for anti-GFP antibodies with the following modifications. ELISA plates (Nunc Maxisorb) were coated with 50 μl of influenza A virus X31 (15) allantoic fluid (106 TCID50/ml) from chicken eggs (provided by J. McCauley), diluted 1:10 in PBS at pH 7.6. The plates were incubated on an orbital shaker at 37°C for 1 h and then washed with PBS, and the test sera were added at a dilution of 1:200 in blocking buffer (5% Marvel milk powder and 0.1% Tween 20 in PBS).
RESULTS
Rescue of recombinant viruses from cloned DNA.
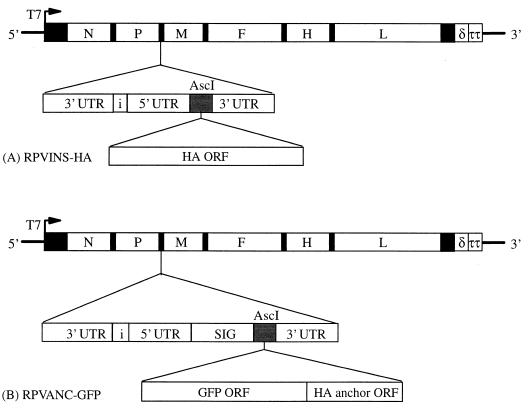
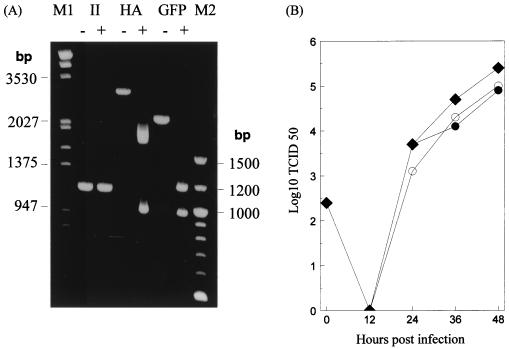
As potential markers for candidate marked RPV vaccines, we used a membrane-anchored GFP and a mutant influenza virus HA protein, which should effectively abolish sialic acid receptor binding function (15). Recombinants RPVINS-HA and RPVANC-GFP were rescued in cell culture from genomic cDNA clones, the construction of which is illustrated in Fig. 1, using established techniques (4, 30). Both recombinant viruses produced cytopathic effect in infected B95a and Vero cell cultures which appeared to be identical to that produced by the standard RBOK vaccine. To confirm that the rescued viruses were the expected recombinants, RT-PCR was carried out on viral RNA using primers (RPV-P6 and RPV-M2) which bracket the original AscI insertion site for the HA mutant and ANC-GFP sequences (30). In each case, the PCR product detected corresponded to the expected size of 1,155 bp for RPVII, 2,919 bp for RPVINS-HA, or 2,127 bp for RPVANC-GFP (Fig. 2A). RT-PCR of the same viral samples without using reverse transcriptase failed to produce any PCR product (data not shown), indicating that the RPVII, RPVINS-HA, and RPVANC-GFP PCR products originated from viral RNA and not from the transfected plasmids. The PCR products from the RPV-P6 and RPV-M2 primer reactions were digested with either AscI (RPVII and RPVANC-GFP) or BssHII (RPVINS-HA) to confirm the presence of the restriction site and to distinguish between the two recombinant viruses. As expected, the RPVII PCR product was not cleaved when digested with AscI due to the absence of the restriction site in the normal virus genome. Digestion of the RPVINS-HA PCR product with BssHII yielded the correct-size DNA products, corresponding to the expected sizes of 1,722, 964, and 233 bp (the smallest band was faint and is not shown in the figure). Digestion of the RPVANC-GFP PCR product with AscI yielded the correct-size DNA products, corresponding to the expected sizes of 1,163 and 964 bp. These data showed that the rescued viruses were the correct recombinant RPVs.
FIG. 1.
Diagrams representing the pRPVINS-HA and pRPVANC-GFP antigenome cDNA constructs, made as described in Materials and Methods. (A) The pRPVINS-HA construct was made by inserting the mutant HA ORF into the unique AscI cloning site in the gene expression cassette, located between the P and M genes of pRPVINS. (B) The pRPVANC-GFP construct was made by inserting the ANC-GFP ORF into the unique AscI cloning site in the gene expression cassette, which includes an N-terminal secretory signal sequence (SIG) located between the P and M genes of pRPVSIG. ORFs of RPV: N, nucleocapsid; P, phosphoprotein; M, matrix; F, fusion; H, hemagglutinin; L, large protein of RPV. UTR, untranslated region represented in black in the complete genome diagram; i, intergenic triplet; T7, T7 RNA polymerase promoter; δ, hepatitis delta ribozyme; ττ, T7 RNA polymerase terminators.
FIG. 2.
Analysis of rescued recombinant viruses. (A) RT-PCR and restriction enzyme digestion analysis of recombinant RPVs. RT-PCR was carried out on total RNA from cells infected with RPVII (II), RPVINS-HA (HA), or RPVANC-GFP (GFP). PCR products were analyzed with (+) or without (−) digestion with an appropriate restriction enzyme, AscI (II or GFP) or BssHII (HA). M1, λ DNA/HindIII and EcoRI DNA markers (Roche); M2, 100-bp DNA ladder markers (Gibco). (B) Growth of recombinant viruses in Vero cells. Cells were infected with RBOK (⧫), RPVINS-HA (○), or RPVANC-GFP (●), and the amount of virus in the cultures was measured at various times from 0 to 48 h postinfection. Each time point represents the mean of two separate experiments.
Comparison of virus growth kinetics.
To examine the effects of introduction of novel gene sequences into the RPV genome, the growth characteristics of the recombinants RPVINS-HA and RPVANC-GFP were compared with those of the standard RBOK vaccine. Growth curves for each of these viruses in Vero cells are shown for comparison in Fig. 2B. The growth rates of RPVINS-HA and RPVANC-GFP were slightly lower than that of RBOK, which produced a titer of 105.5 TCID50/ml by 48 h. The two marker viruses produced titers which were about 0.5 log lower than that of RBOK. The reduced growth rates of the two recombinant viruses were expected because they have larger genomes than the original RBOK strain and because the insertion of an extra gene between the P and M (matrix) genes leads to reduced levels of expression of the downstream M, F (fusion protein), H, and L (large protein) genes (3, 5, 33). Similar slightly reduced virus titers were also observed with previous recombinants RPVINS-3D (5), RPVINS-GFP (30), and RPVSIG-GFP (30). However, both RPVINS-HA and RPVANC-GFP could be grown to maximum titers (106 TCID50/ml) similar to those for the RBOK strain for vaccine production in Vero cell cultures (data not shown). These results showed that modification of the RBOK genome and incorporation of the gene expression cassette and foreign gene sequences did not significantly alter the virus growth characteristics in cell culture.
Analysis of HA and ANC-GFP expression in cell culture.
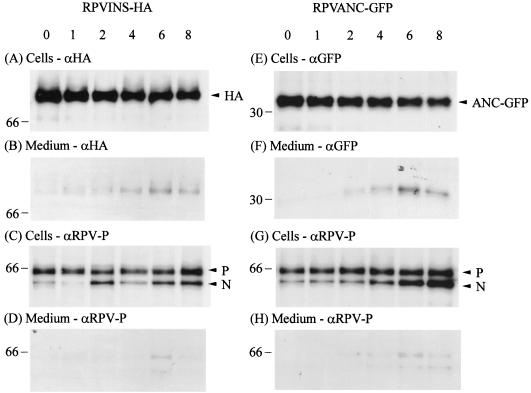
Since the RBOK vaccine is primarily lymphotropic in vivo, infecting and replicating in leukocytes (28), the expression of HA and ANC-GFP proteins in vitro was analyzed using the B95a lymphoblastoid cell line (11, 12). B95a cells were infected with RPVINS-HA or RPVANC-GFP. Cell proteins were radiolabeled and the turnover of labeled protein and release into the medium was followed for up to 8 h by determining the amount of HA, ANC-GFP, or a normal RPV protein, in this case P, in the cells and surrounding medium (Fig. 3). Expressed radiolabeled HA, ANC-GFP, and RPV P were immunoprecipitated with anti-HA, anti-GFP, and anti-RPV P antibodies, respectively, and the precipitated proteins were analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
FIG. 3.
Analysis of HA and ANC-GFP expression and secretion by RPVINS-HA- and RPVANC-GFP-infected B95a cells. Cells were labeled for 2 h and then the medium was replaced with normal medium containing unlabeled methionine and cysteine. Medium was collected after 0, 1, 2, 4, 6, and 8 h of chase and analyzed for the presence of labeled secreted proteins, whereas the corresponding cell sheet was lyzed and analyzed for the presence of labeled intracellular proteins. Proteins were immunoprecipitated with either anti-HA polyclonal antibody (αHA), anti-GFP polyclonal antibody (αGFP), or anti-RPV P monoclonal antibody (αRPV-P) as described in Materials and Methods. (A to D) RPVINS-HA-infected cells; (E to H) RPVANC-GFP-infected cells. Numbers above the gels represent the time in hours after protein labeling at which the samples were collected. Positions of the molecular mass markers in kilodaltons are indicated on the left. Positions of the RPV N and P proteins are indicated on the right.
In RPVINS-HA cell lysates, anti-HA antibodies detected a protein which migrated with an apparent molecular mass of approximately 80 kDa (Fig. 3A), consistent with the size of the glycosylated influenza virus HA protein in sodium dodecyl sulfate-gels. Anti-GFP antibodies detected a protein which migrated with an apparent molecular mass of approximately 32 kDa (Fig. 3E), consistent with the expected size of the ANC-GFP protein. A very small quantity of HA or ANC-GFP was detected in the culture medium of RPVINS-HA (Fig. 3B)- or RPVANC-GFP (Fig. 3F)-infected cells, respectively. This may be the result of low-level release of HA or ANC-GFP into the medium; alternatively, it may be the result of some infected B95a cells detaching into the medium, as these cells, which are normally only weakly adherent, detach very easily when infected with virus. The levels of both proteins decreased by about half during the 8-h time course of the chase period examined. In a similar experiment, intracellular expression of GFP in RPVINS-GFP-infected cells was previously shown to be completely stable over an 8-h time course (30).
When cells were infected with either recombinant virus, no reduction in the amount of RPV P protein precipitated from the cell lysates was observed during the 8-h time course (Fig. 3C and G). A very small quantity of RPV P, most likely from detached cells, was detected in the culture medium at some stages (Fig. 3D and H). A second protein band which migrated just below the RPV P band, and was probably coimmunoprecipitated with RPV P protein by anti-RPV P antibody, corresponded to the position where RPV N (nucleocapsid) protein would normally be expected (4, 8, 23). These observations are similar to those of a previous study (30). The results showed that RPVINS-HA and RPVANC-GFP efficiently expressed HA and ANC-GFP, respectively. Both proteins were expressed in equivalent quantities and appeared to be turned over at similar rates, as very similar levels of HA and ANC-GFP were observed in virus-infected cells throughout the time course observed.
Localization of HA and ANC-GFP in virus-infected cells.
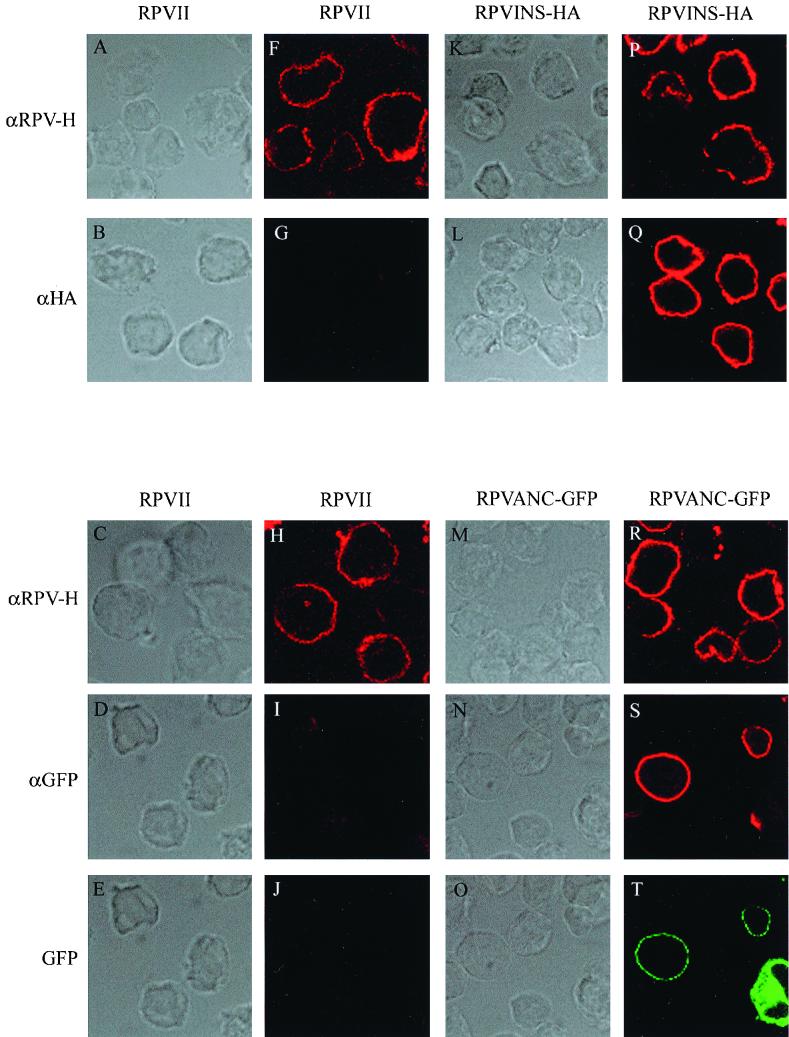
The expression and localization of RPV H, HA, and ANC-GFP were examined at 2 days postinfection in RPVII-, RPVINS-HA-, and RPVANC-GFP-infected B95a cells and bovine PBL. The HA and ANC-GFP genes in the viruses possess signal sequences which should direct the expressed proteins to the endoplasmic reticulum and thence to the surface of virus-infected cells. Protein localization on the surface of infected cells was determined by examining antibody-labeled nonpermeabilized and permeabilized cells using transmitted light and confocal fluorescence microscopy.
The localization of HA and ANC-GFP was compared to that of the RPV H protein, which is normally found on the surface of RPV-infected cells. Figure 4 shows the transmitted light and fluorescence images of nonpermeabilized virus-infected B95a cells. The RPV H protein was detected by indirect immunofluorescence at high levels on the surface of cells infected with RPVII (Fig. 4F and H), RPVINS-HA (Fig. 4P), or RPVANC-GFP (Fig. 4R). The distribution of this protein in the plasma membrane appeared to be in many distinct patches, in contrast to the uniform surface distribution of the HA protein (compare Fig. 4F and Q). Similarly, ANC-GFP appeared by immunofluorescence to be evenly distributed on the cell surface when it was expressed there (Fig. 4S). However, this protein was not efficiently transported to the surface of infected B95a cells. The majority of such cells infected with RPVANC-GFP showed high levels of internal GFP but little or no surface expression (Fig. 4S and T, bottom right corner). The more patchy distribution of GFP fluorescence compared to indirect immunofluorescence (compare Fig. 4S and T) may reflect a concentration dependence of the GFP fluorescence. In no case was significant labeling of internal structures detected in nonpermeabilized cells by antibodies to RPV H, HA, or GFP. Antibody labeling of permeabilized infected B95a cells gave rise to strong labeling of internal RPV H and HA proteins in RPVINS-HA-infected cells and strong labeling of internal RPV H protein and ANC-GFP in RPVANC-GFP-infected cells (data not shown); these patterns were quite distinct from the plasma membrane surface labeling detected in nonpermeabilized cells (Fig. 4). Using double antibody labeling, cells infected with RPVINS-HA or RPVANC-GFP always stained positive for both RPV H and either HA or ANC-GFP as appropriate, indicating that the marker protein was expressed in all virus-infected cells (data not shown). No significant fluorescence with anti-HA or anti-GFP antibodies or GFP fluorescence was observed in the RPVII-infected control cells (Fig. 4B, D, E, G, I, and J).
FIG. 4.
Cell surface expression and localization of HA, ANC-GFP, and RPV H in recombinant RPV-infected cells using GFP fluorescence and indirect immunofluorescence confocal microscopy. Shown are transmitted light (A to E) and immunofluorescence (F to J) images of RPVII-infected B95a cells, transmitted light (K and L) and immunofluorescence (P and Q) images of RPVINS-HA-infected B95a cells, and transmitted light (M to O), immunofluorescence (R and S), and GFP fluorescence (T) images of RPVANC-GFP-infected B95a cells. Virus-infected B95a cells were fixed at 2 days postinfection, and nonpermeabilized cells were used for surface protein labeling as described in Materials and Methods. The relevant virus is indicated at the top, and antibody specificity is indicated on the left. Anti-RPV-H (αRPV-H), anti-HA (αHA), and anti-GFP (αGFP) antibody immunofluorescence is red; GFP fluorescence (GFP) is green. Original magnification of photomicrographs was ×1,000.
The expression and localization of RPV H, HA, and ANC-GFP were also examined in nonpermeabilized and permeabilized virus-infected PBL (data not shown). The localization patterns of the RPV H and HA proteins were very similar in bovine PBL to those observed in B95a cells. However, ANC-GFP was detected by indirect immunofluorescence and GFP fluorescence at high levels on the surface of all RPVANC-GFP-infected PBL. We observed no infected PBL which had internal but no surface localization of ANC-GFP.
These results showed that the HA protein was efficiently expressed and localized at high levels on the surface of all PBL and B95a cells. ANC-GFP was efficiently expressed by both PBL and B95a cells and was localized to the surface of infected PBL, but it was not efficiently transported to the surface of most RPVANC-GFP-infected B95a cells. The distribution of HA and ANC-GFP was different from that of the RPV H protein. For all three viruses, the RPV H protein appeared to localize predominantly to patches on the surface of infected cells, whereas HA and ANC-GFP both appeared to be uniformly distributed over the surface of virus-infected cells where they were expressed in the plasma membrane.
The stability of the HA and ANC-GFP marker genes in RPVINS-HA and RPVANC-GFP were tested by repeated passage in Vero cells at low MOI. After eight passages they showed by immunofluorescence staining HA and GFP expression in infected cells similar to that reported above (data not shown). This showed that the genes were stably maintained and expressed during a large number of virus generations in cell culture.
Protein incorporation into virus particle envelopes.
We carried out an assay using virus immunoprecipitation to determine if either the HA protein or ANC-GFP was incorporated into the RPVINS-HA or RPVANC-GFP envelope, respectively. It was assumed that if the marker protein was incorporated into the virus envelope, it would be possible to immunoprecipitate it with a specific antibody. Therefore, if the influenza virus HA protein or ANC-GFP was present in the virus envelope, incubation with anti-HA or anti-GFP antibody, as appropriate, should immunoprecipitate the virus.
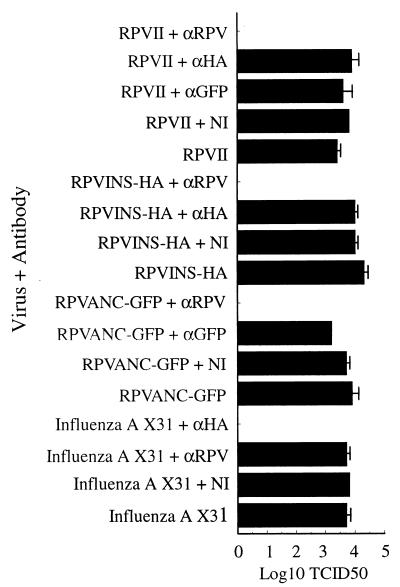
Four viruses were tested in this assay: RPVII, RPVINS-HA, RPVANC-GFP, and influenza A virus X31 (Fig. 5). As expected, the positive control experiments resulted in immunoprecipitation of all four viruses used in the assay: the three recombinant RPVs were all efficiently immunoprecipitated by anti-RPV antibody, and influenza A virus X31 was efficiently immunoprecipitated by anti-HA antibody. No positive control for GFP was possible because no other virus which expressed ANC-GFP in its envelope was available. However, the anti-GFP polyclonal antibody would be expected to immunoprecipitate RPV expressing ANC-GFP in the viral envelope, since it very efficiently immunoprecipitated ANC-GFP in the pulse-chase experiment (Fig. 3) and labeled this protein on the surface of infected cells (Fig. 4). Incubation of the viruses with anti-marker protein antibody (anti-HA or anti-GFP) or with nonimmune rabbit serum failed to show significant immunoprecipitation of any of the four viruses.
FIG. 5.
Assay for incorporation of HA and ANC-GFP into the envelopes of RPVINS-HA and RPVANC-GFP. In each case, 104 TCID50 of virus was mixed with antibody and protein A-Sepharose, and the titer of virus remaining in the supernatants was determined. The virus-antibody combinations used in the immunoprecipitations are shown on the y axis; supernatant virus titers are shown on the x axis. RPV hyperimmune antiserum is indicated by αRPV, nonimmune antiserum is indicated by NI, anti-HA polyclonal antibody is indicated by αHA, anti-GFP polyclonal antibody is indicated by αGFP. A no-antibody control was also included for each virus. Assay sensitivity was >20 TCID50 of virus/ml. The bar chart shows the mean of two separate experiments, with the individual results indicated by error bars.
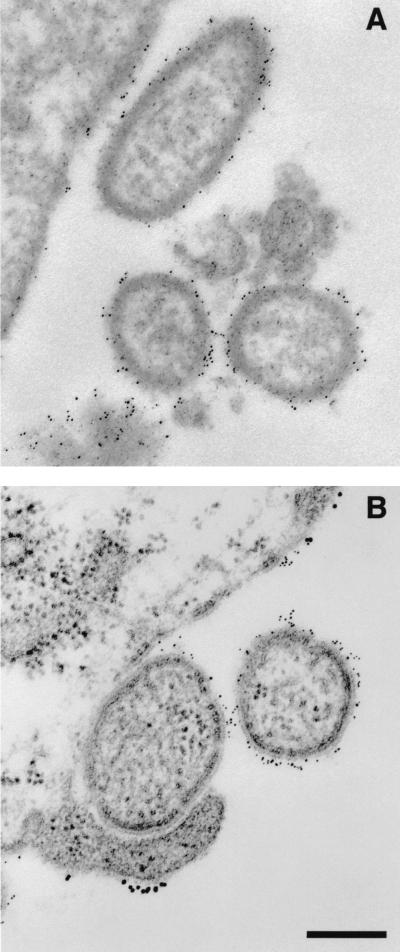
Immunoelectron microscopy of RPVII and RPVI-HA-infected cells.
The results of the precipitation assay described above suggested that neither HA nor ANC-GFP was incorporated into virus envelopes. To directly examine the localization of the RPV H and HA proteins in virus-infected cells and viruses, and to corroborate the immunoprecipitation assay data, we examined infected cells by immunoelectron microscopy.
RPVII- or RPVINS-HA-infected B95a cells were immunolabeled for surface proteins using anti-RPV H and anti-HA antibodies followed by 5-nm-gold-conjugated antibody to detect anti-RPV H antibody and 10-nm-gold-conjugated antibody to detect anti-HA antibody. Electron micrographs of thin sections of RPVII- and RPVI-HA-infected B95a cells are shown in Fig. 6. RPV H antigen was detected on the surface membrane of RPVII-infected cells and in the RPVII virus envelope, as shown by the presence of 5-nm gold particles on both structures (Fig. 6A). No 10-nm gold particles were observed either on the surface of RPVII-infected B95a cells or on virus envelopes. Both the RPV H and HA antigens were detected on the surface membrane of RPVINS-HA-infected B95a cells; however, only 5-nm gold particles were detected on the envelope of RPVINS-HA (Fig. 6B).
FIG. 6.
Immunoelectron microscopy of RPVII (A)- and RPVINS-HA (B)-infected B95a cells. Virus-infected cells were fixed at 2 days postinfection and labeled with both anti-RPV H (which was detected using a 5-nm-gold-conjugated secondary antibody) and anti-HA (which was detected using a 10-nm-gold-conjugated secondary antibody). Bar represents 200 nm.
The data from this experiment showed that the RPV H protein was localized to the surface of both RPVII- and RPVINS-HA-infected cells and was incorporated into the RPVII envelope. The HA protein was expressed on the surface of RPVINS-HA-infected cells but was not incorporated into the RPVINS-HA virus envelope. The absence of 10-nm gold particles either on the surface of RPVII-infected cells or on virus envelopes showed that neither the primary anti-HA nor secondary antibodies reacted with either B95a cells or parental virus proteins.
Analysis of receptor binding function of mutant HA protein.
RPVINS-HA was designed to express a receptor site double mutant HA protein, which should abolish binding of the HA protein to the sialic acid receptor expressed on the surface of virus-infected cells. The receptor binding function of the mutant HA protein was examined in an assay for attachment of RBC (which contain high levels of sialic acid on their surface) to HA protein on the cell surface. The RBC attached strongly to the surface of influenza virus X31-infected cells, which expressed wild-type HA protein, but did not attach to RPVINS-HA-infected cells, which expressed the mutant HA protein on their surface, or to RPVII-infected or negative control cells (data not shown). These results showed that in this assay the receptor binding function of the double mutant HA protein expressed by RPVINS-HA was effectively abolished, in agreement with a previous study of RBC binding by HA receptor site single mutants (15).
Immunogenicity, pathogenicity, and efficacy of marker vaccines in cattle.
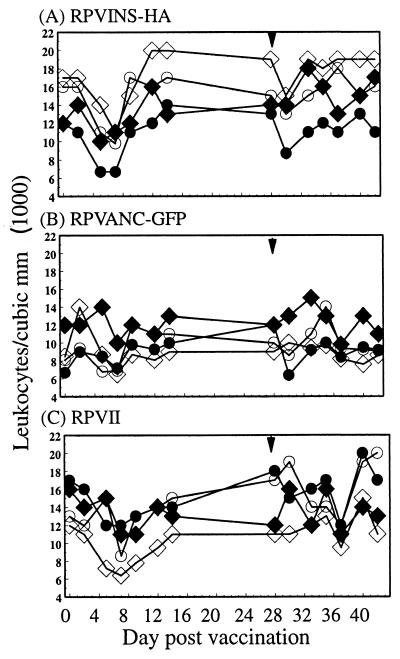
To determine the effectiveness of these viruses in generating protective immunity and stimulating antibody responses to the marker proteins in the natural host species, the viruses were tested in a standard cattle vaccination trial. A total of eight cattle were vaccinated: four (TV58, TV59, TV60, and TV61) with RPVINS-HA and four (TY28, TY29, TY30, and TY31) with RPVANC-GFP. Because it was not considered necessary to repeat control vaccine experiments when each novel RPV vaccine was tested, the RPVII vaccine control results shown here were those previously reported (30). In that experiment, four cattle (TR2, TR3, TR4, and TR5) were vaccinated with RPVII. However, the same batch of freeze-dried challenge virus was used in the experiments reported here as in the previous study. At 4 weeks postvaccination, all cattle were challenged with the highly virulent RPV Saudi 1/81 strain. No signs of clinical disease associated with rinderpest infection were observed in any of the eight RPVINS-HA- or RPVANC-GFP-vaccinated cattle following either vaccination or challenge. The rectal temperatures and leukocyte levels in the cattle were monitored as indicators of subclinical disease and viremia. The rectal temperatures of all cattle remained within the normal range during both vaccination and challenge stages (data not shown). A moderate leukopenia was observed in some of the cattle after vaccination whichever vaccine was used, but leukocyte counts returned to normal levels by 2 weeks postvaccination (Fig. 7). This mild leukopenia, which may be indicative of vaccine virus replication, is also commonly observed in cattle given the standard RBOK vaccine (30). Very little leukopenia was observed after challenge, suggesting that only minimal replication of challenge virus took place. A mild transient leukopenia was also observed with RPVII-, RPVINS-GFP-, and RPVSIG-GFP-vaccinated cattle as previously reported (30), although a much more dramatic and severe leukopenia occurs in cattle infected with virulent virus (1).
FIG. 7.
PBL counts for cattle vaccinated with RPVINS-HA (TV58 [○], TV59 [⧫], TV60 [◊], and TV61 [●]) (A), RPVANC-GFP (TY28 [○], TY29 [⧫], TY30 [◊], and TY31 [●]), (B), and RPVII (TR2 [○], TR3 [⧫], TR4 [◊], and TR5 [●]) (C). The cattle were vaccinated on day 0 and challenged on day 28 with virulent RPV Saudi 1/81. The day of challenge is indicated by an arrowhead.
The cattle were also monitored for the presence of viral RNA in samples of eye secretions. The vaccine strain has lost its ability to replicate in epithelial cells and is strictly lymphotrophic, and it has never been found to be shed by vaccinated animals (28). If genetic modification of the vaccine affected its attenuation, then it might potentially be found in secretions. The eye is an abundant source of virus in animals naturally infected with RPV; if no virus can be detected in the eyes of vaccinated cattle, then it is unlikely to be found elsewhere. RT-PCR was used to detect virus RNA since it is the most sensitive detection system for the analysis of clinical samples for RPV (9). It has been used in many similar vaccine trials and found to be very efficient for detecting virus RNA (16). No virus RNA was detected in the eye swabs from any of the RPVINS-HA- or RPVANC-GFP-vaccinated cattle following either vaccination or challenge. Similarly, no virus RNA was detected in eye swabs from any of the RPVII-vaccinated cattle (30). RPV RT-PCR positive and negative controls gave the expected results in these tests. Cellular actin mRNA was detected using RT-PCR with bovine actin-specific primers in most RNA preparations, showing that the isolated RNA was of good quality and would enable the detection of RPV-specific RNA present in sufficient quantity in the sample (data not shown). These results showed that RPVINS-HA and RPVANC-GFP were safe and effective RPV vaccines which provided complete protection from rinderpest when vaccinated cattle were challenged with the highly virulent RPV Saudi 1/81 strain. No increase in viremia or virus secretion was detected.
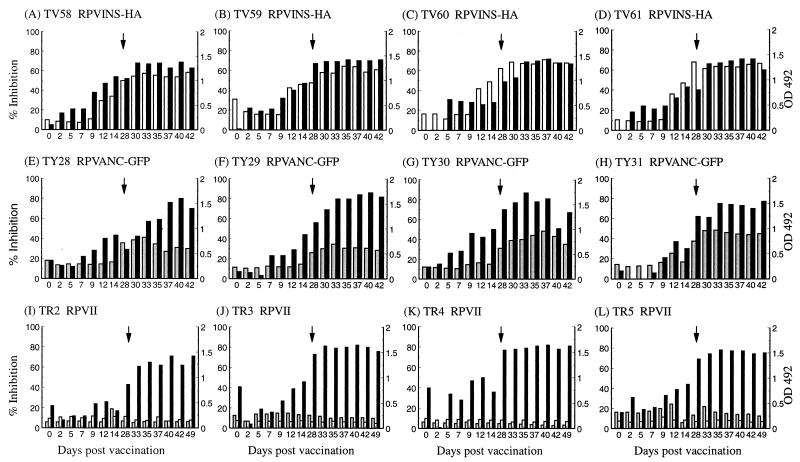
Antibody responses to RPV and marker proteins in vaccinated cattle.
The level of humoral antibodies to RPV and the marker proteins was measured by standard ELISAs. All eight vaccinated cattle developed high levels of anti-RPV H antibodies (Fig. 8) similar to those previously seen in control cattle (30) and comparable to those found in animals vaccinated with the standard cell culture-grown RBOK vaccine. Furthermore, no appreciable anamnestic response was observed upon challenge with RPV Saudi 1/81, suggesting that only minimal replication of the challenge virus took place.
FIG. 8.
ELISA detection of anti-RPV-H, anti-HA, and anti-GFP antibodies in sera from cattle vaccinated with recombinant RPV vaccines. ELISA results are shown for the four cattle (TV58, TV59, TV60, and TV61) vaccinated with RPVINS-HA (A to D), the four cattle (TY28, TY29, TY30, and TY31) vaccinated with RPVANC-GFP (E to H), and the four cattle (TR2, TR3, TR4, and TR5) vaccinated with RPVII (I to L). The cattle were vaccinated on day 0 and then challenged with RPV Saudi 1/81 on day 28 (indicated by an arrow). Anti-RPV-H (black bars) antibody responses represent percent inhibition (left-hand y axis); anti-HA (white bars) or anti-GFP (grey bars) antibody responses represent optical densities measured at 492 nm (OD 492; right-hand y axis). The results shown in panels I to L, with the exception of the anti-HA results, are taken from reference 30.
High levels of anti-HA antibody were detected in the sera of all four cattle vaccinated with RPVINS-HA (Fig. 8A to D). The levels of anti-HA antibodies persisted and remained high, with no significant reduction until 42 days postvaccination, which was the last day animals were tested for humoral antibody responses to the vaccines. Good levels of anti-GFP antibody were also detected in the sera of all four cattle given the RPVANC-GFP vaccine (Fig. 8E to H). The levels of anti-GFP antibodies showed an initial increase and then, after a slight reduction in antibody levels in three of the four animals at around day 33, remained constant until 42 days postvaccination, the last day of the experiment. Sera from the four cattle that received the RPVII control vaccine (30), as expected, showed no anti-HA or anti-GFP antibody serum reactivity (Fig. 8I to L) (sera from this previous experiment were tested for anti-HA antibodies). We have frequently observed high background ELISA readings in day 0 sera, possibly due to stress of the experimental animals, but the high ratio of positive to background readings observed means that this is not a significant problem. These data show that the RPVINS-HA and RPVANC-GFP vaccines possess the same characteristics as the RBOK vaccine and that all of the cattle vaccinated with the marker vaccines responded well to the appropriate marker protein.
DISCUSSION
We report here the successful development of two genetically marked recombinant rinderpest vaccines using either the influenza virus HA protein or ANC-GFP as a marker. A number of recombinant negative-strand RNA viruses have been constructed as vectors for the highly stable expression of foreign genes encoding membrane-anchored proteins to produce heterologous viruses and vaccines. These include the rhabdovirus vesicular stomatitis virus (VSV) expressing human CD4 (22), influenza virus HA or neuraminidase (13, 19, 20), and respiratory syncytial virus (RSV) G or F protein (10) and MV expressing the VSV G protein (24). Recombinant VSV and MV vaccines expressing membrane-anchored proteins as immunizing agents have been shown to give rise to good humoral antibody responses in vaccinated animals (19, 20, 24). We considered that an RPV vaccine expressing a gene encoding a membrane-anchored form of GFP as a marker antigen might be expected to stimulate a strong anti-marker protein humoral antibody response in vaccinated animals. Since GFP is not known or expected to bind to any cell surface receptors, incorporation of ANC-GFP into the virus envelope was not considered likely to modify the cellular tropism of the virus. The influenza virus HA protein was selected as an alternative potential genetic marker for the recombinant RBOK vaccine because it is known to be capable of eliciting high levels of anti-HA humoral antibody in vaccinated animals (32). The HA protein and ANC-GFP appeared to be good candidate marker antigens; because cattle would not normally be exposed to them in the environment, serological surveys should not give rise to false-positive results for unvaccinated animals. Although very unlikely to be a problem with a vaccine strain, it was possible that incorporation of a foreign receptor protein in the virus envelope might give rise to a virus with a novel tissue or host tropism and potentially generate a new pathogen. Therefore, to enable the HA protein to be more safely used as a genetic marker for the vaccine, a mutant HA gene sequence was generated which was designed to encode an HA protein with reduced or no ability to bind to its sialic acid cell surface receptor (15). The receptor binding function of the mutant HA protein was shown to be abolished using an assay for RBC attachment to the surface of virus-infected cells, which was as expected for the double mutant protein (15). This greatly reduced the possibility that the HA protein might modify the tissue tropism or host range of the recombinant virus. Another aspect in favor of their safety is the fact that there is no experimental evidence, either in vitro or in vivo, for recombination between nonsegmented negative-strand viruses.
The effectiveness of these vaccines in generating protective immunity and stimulating antibody responses to the marker proteins was tested in cattle, the natural host of RPV, using a standard vaccination trial. Both vaccines provided complete protection from a subsequent lethal challenge with a highly virulent strain of RPV, and all of the cattle produced normal levels of anti-RPV H humoral antibodies. RPVINS-HA and RPVANC-GFP exhibit all characteristics of the standard RBOK vaccine (17, 18) except for slightly slower growth in cell culture, which agrees with previous genetic manipulation studies of this virus (5, 30).
The HA protein and ANC-GFP were not incorporated into the envelope of RPVINS-HA and RPVANC-GFP, respectively. The immunoprecipitation assay showed that antibodies specific for HA or GFP failed to immunoprecipitate either RPVINS-HA or RPVANC-GFP. Furthermore, immunoelectron microscopy of RPVINS-HA-infected cells showed that the HA protein was found on the surface of infected cells but was not incorporated into the envelope of the virus. This confirmed that the absence of virus immunoprecipitation by specific antibodies indicated that the protein was not incorporated into virus envelopes. However, our experiments cannot completely exclude the possibility that either of the two proteins may be incorporated at low levels into the envelope of a small proportion of viruses, as this would be difficult to detect by either immunoprecipitation or immunoelectron microscopy.
These findings suggest that RPV is quite specific in the type of proteins which are incorporated into the virus envelope. In contrast, recombinant VSV expressing the influenza virus HA (13, 20) or the RSV G or F (10) glycoprotein and recombinant MV expressing the VSV G glycoprotein, although in the absence of the MV F and H envelope proteins (24), were found to express the foreign proteins on the surface of virus-infected cells and also efficiently incorporate the foreign proteins into virus envelopes. The incorporation of these foreign proteins into the envelope of the recombinant viruses did not appear to require an endogenous virus-specific signal (10, 13, 20, 22, 24). A number of possibilities might explain the exclusion of foreign proteins from the RPV envelope. It may be that incorporation into the envelope requires a very specific interaction with the normal virus proteins such as the RPV M, F, or H protein. Interestingly, our experiments showed that the RPV H protein formed patches on the surface of infected cells, unlike HA and ANC-GFP, which appeared to be localized all over the surface of infected cells. This suggests that the RPV H protein may interact with other RPV H or F molecules on the cell surface to form complexes, and possibly excluding nonviral cell surface proteins. Alternatively, the RPV H and F proteins or complexes may be recruited to specific locations on the cell surface by the M protein to form virus budding sites. These possibilities need to be addressed by examination of the localization of the RPV F and M proteins in normal RPV-infected cells and by examining the localization of these and foreign proteins in cells infected by recombinant RPV mutants which fail to express the RPV H, F, or M protein in single or multiple mutant combinations.
Previous studies with recombinant VSV and MV vaccines have not shown that incorporation of the protein into the viral envelope, as opposed to expression only on the surface of virus-infected cells, is required for the generation of the humoral immune response (19, 20, 24). The results reported here suggest that the incorporation of a foreign protein into the virus envelope is not required to generate a strong humoral response, at least in recombinant RPV-vaccinated animals. However, we do not know if this is generally applicable to other viruses or whether it is specific only to viruses such as RPV which infect and replicate in cells of the immune system. The most important aspect of the absence of marker protein incorporation into viruses is that it enhances the safety of these potential vaccines, since they are unlikely to possess novel tissue or host tropisms which might be determined by foreign envelope proteins.
Very good antibody responses were produced against the marker proteins in all of the vaccinated cattle. The RPVINS-HA-vaccinated cattle all produced high levels of anti-HA humoral antibodies, and the RPVANC-GFP-vaccinated cattle all produced reasonably high levels of anti-GFP humoral antibodies. The humoral antibody response to HA was more easily detectable by ELISA than the response to GFP in cattle. We do not know precisely why this form of marker antigen expression was so effective in generating humoral antibodies compared to the previous strategies using intracellularly expressed or secreted forms of GFP (30). It may be that membrane anchorage keeps the marker antigen concentrated and localized, thereby more effectively stimulating the immune system. It is also possible that HA and ANC-GFP are internalized from the cell surface and directed more efficiently into the class II major histocompatibility complex presentation pathway (14, 25, 29), allowing the marker proteins to activate B-lymphocyte antibody production.
In conclusion, RPVINS-HA and RPVANC-GFP were shown to be safe and effective marked RPV vaccines which should allow serological differentiation between vaccinated and naturally infected animals. Our studies suggest that membrane anchorage of a protein is very efficient for generating an antibody response to antigens expressed from RPV vaccines, and this may well apply to other morbilliviruses such MV. Long-term field trials are now required to establish the duration of antibody responses to the marker proteins and that the clinical efficacy of the vaccine has not been affected by the insertion of the extra gene.
ACKNOWLEDGMENTS
We thank Brian Taylor, Natasha Smith, Luke Fitzgerald, and Gemma Sefton for care of the experimental animals. Thanks are also due to Hannah Cook for excellent technical assistance and to Subash Das, Jude Heaney, and Tom Wileman for very helpful advice and discussions.
This work was funded by the Department for International Development (DFID), UK, grant R7048.
REFERENCES
- 1.Anderson J, Barrett T, Scott G R. FAO animal health manual. Manual on the diagnosis of rinderpest. 2nd ed. Rome, Italy: Food and Agriculture Organization of the United Nations; 1996. [Google Scholar]
- 2.Anderson J, McKay J A. The detection of antibodies against peste des petits ruminants virus in cattle, sheep and goats and the possible implications to rinderpest control programmes. Epidemiol Infect. 1994;112:225–234. doi: 10.1017/s0950268800057599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ball L A, Pringle C R, Flanagan B, Perepelitsa V P, Wertz G W. Phenotypic consequences of rearranging the P, M, and G genes of vesicular stomatitis virus. J Virol. 1999;73:4705–4712. doi: 10.1128/jvi.73.6.4705-4712.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baron M D, Barrett T. Rescue of rinderpest virus from cloned cDNA. J Virol. 1997;71:1265–1271. doi: 10.1128/jvi.71.2.1265-1271.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baron M D, Foster-Cuevas M, Baron J, Barrett T. Expression of epitopes of a heterologous virus using a recombinant rinderpest virus. J Gen Virol. 1999;80:2031–2039. doi: 10.1099/0022-1317-80-8-2031. [DOI] [PubMed] [Google Scholar]
- 6.Barrett T, Rossiter P B. Rinderpest: the disease and its impact on humans and animals. Adv Virus Res. 1999;53:89–110. doi: 10.1016/s0065-3527(08)60344-9. [DOI] [PubMed] [Google Scholar]
- 7.Calain P, Roux L. The rule of six, a basic feature for efficient replication of Sendai virus defective interfering RNA. J Virol. 1993;67:4822–4830. doi: 10.1128/jvi.67.8.4822-4830.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diallo A, Barrett T, Lefevre P C, Taylor W P. Comparison of proteins induced in cells infected with rinderpest and peste des petits ruminants viruses. J Gen Virol. 1987;68:2033–2038. doi: 10.1099/0022-1317-68-7-2033. [DOI] [PubMed] [Google Scholar]
- 9.Forsyth M, Barrett T. Evaluation of polymerase chain reaction for the detection and characterization of rinderpest and peste des petits ruminants viruses for epidemiological studies. Virus Res. 1995;39:151–163. doi: 10.1016/0168-1702(95)00076-3. [DOI] [PubMed] [Google Scholar]
- 10.Kahn J S, Schnell M J, Buoncore L, Rose J K. Recombinant vesicular stomatitis virus expressing respiratory syncytial virus (RSV) glycoproteins: RSV fusion protein can mediate infection and cell fusion. Virology. 1999;254:81–91. doi: 10.1006/viro.1998.9535. [DOI] [PubMed] [Google Scholar]
- 11.Kobune F, Sakata H, Sugiura A. Marmoset lymphoblastoid cells as a sensitive host for isolation of measles virus. J Virol. 1990;64:700–705. doi: 10.1128/jvi.64.2.700-705.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobune F, Sakata H, Sugiyama M, Sugiura A. B95a, a marmoset lymphoblastoid cell line, as a sensitive host for rinderpest virus. J Gen Virol. 1991;72:687–692. doi: 10.1099/0022-1317-72-3-687. [DOI] [PubMed] [Google Scholar]
- 13.Kretzschmar E, Buonocore L, Schnell M J, Rose J K. High-efficiency incorporation of functional influenza virus glycoproteins into recombinant vesicular stomatitis viruses. J Virol. 1997;71:5982–5989. doi: 10.1128/jvi.71.8.5982-5989.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marks M S, Roche P A, Van Donselaar E, Woodruff L, Peters P J, Bonifacino J S. A lysosomal targetting signal in the cytoplasmic tail of the β chain directs HLA-DM to MHC class II compartments. J Cell Biol. 1995;131:351–369. doi: 10.1083/jcb.131.2.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin J, Wharton S A, Lin Y P, Takemoto D K, Skehel J J, Wiley D C, Steinhauer D A. Studies of the binding properties of influenza hemagglutinin receptor-site mutants. Virology. 1998;241:101–111. doi: 10.1006/viro.1997.8958. [DOI] [PubMed] [Google Scholar]
- 16.Ohishi K, Inui K, Barrett T, Yamanouchi K. Long term protective immunity to rinderpest in cattle following a single vaccination with a recombinant vaccinia virus expressing the virus haemagglutinin protein. J Gen Virol. 2000;81:1439–1446. doi: 10.1099/0022-1317-81-6-1439. [DOI] [PubMed] [Google Scholar]
- 17.Plowright W. The duration of immunity in cattle following inoculation of rinderpest cell culture vaccine. J Hyg Camb. 1984;92:285–296. doi: 10.1017/s0022172400064524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plowright W, Ferris R D. Studies with rinderpest virus in tissue culture. The use of attenuated culture virus as a vaccine in cattle. Res Vet Sci. 1962;3:172–182. [Google Scholar]
- 19.Roberts A, Kretzschmar E, Perkins A S, Forman J, Price R, Buonocore L, Kawaoka Y, Rose J K. Vaccination with recombinant vesicular stomatitis viruses expressing an influenza virus hemagglutinin provides complete protection from influenza virus challenge. J Virol. 1998;72:4704–4711. doi: 10.1128/jvi.72.6.4704-4711.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roberts A, Buonocore L, Price R, Rose J K. Attenuated vesicular stomatitis viruses as vaccine vectors. J Virol. 1999;73:3723–3732. doi: 10.1128/jvi.73.5.3723-3732.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rweyemamu M M, Cheneau Y. Strategy for the global rinderpest eradication programme. Vet Microbiol. 1995;44:369–376. doi: 10.1016/0378-1135(95)00030-e. [DOI] [PubMed] [Google Scholar]
- 22.Schnell M J, Buonocore L, Kretzschmar E, Johnson E, Rose J K. Foreign glycoproteins expressed from recombinant vesicular stomatitis viruses are incorporated efficiently into virus particles. Proc Natl Acad Sci USA. 1996;93:11359–11396. doi: 10.1073/pnas.93.21.11359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaji D, Shaila M S. Domains of rinderpest virus phosphoprotein involved in interaction with itself and the nucleocapsid protein. Virology. 1999;258:415–424. doi: 10.1006/viro.1999.9740. [DOI] [PubMed] [Google Scholar]
- 24.Spielhofer P, Bachi T, Fehr T, Christiansen G, Cattaneo R, Kaelin K, Billeter M A, Naim H Y. Chimeric measles viruses with a foreign envelope. J Virol. 1998;72:2150–2159. doi: 10.1128/jvi.72.3.2150-2159.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tan M C A A, Mommaas A M, Drijfhout J W, Jordens R, Onderwater J J M, Verwoerd D, Mulder A A, van der Heiden A N, Scheidegger D, Oomen L C J M, Ottenhoff T H M, Tulp A, Neefjes J J, Koning F. Mannose receptor-mediated uptake of antigens strongly enhances HLA class II-restricted antigen presentation by cultured dendritic cells. Eur J Immunol. 1997;27:2426–2435. doi: 10.1002/eji.1830270942. [DOI] [PubMed] [Google Scholar]
- 26.Taylor W P. Epidemiology and control of rinderpest. Rev Sci Tech Off Int Epizoot. 1986;5:407–410. doi: 10.20506/rst.5.2.250. [DOI] [PubMed] [Google Scholar]
- 27.Taylor W P, Bhat P N, Nanda Y P. The principles and practice of rinderpest eradication. Vet Microbiol. 1995;44:359–367. doi: 10.1016/0378-1135(95)00029-a. [DOI] [PubMed] [Google Scholar]
- 28.Taylor W P, Plowright W. Studies on the pathogenesis of rinderpest in experimental cattle. III. Proliferation of an attenuated strain in various tissues following subcutaneous inoculation. J Hyg Camb. 1965;63:263–275. doi: 10.1017/s0022172400045149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thompson S A, Burrows S R, Misko I S, Moss D J, Coupar B E H, Khanna R. Targetting a polyepitope protein incorporating multiple class II-restricted viral epitopes to the secretory/endocytic pathway facilitates immune recognition by CD4+ cytotoxic T lymphocytes: a novel approach to vaccine design. J Virol. 1998;72:2246–2252. doi: 10.1128/jvi.72.3.2246-2252.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walsh E P, Baron M D, Anderson J, Barrett T. Development of a genetically marked recombinant rinderpest vaccine expressing green fluorescent protein. J Gen Virol. 2000;81:709–805. doi: 10.1099/0022-1317-81-3-709. [DOI] [PubMed] [Google Scholar]
- 31.Wamwayi H M, Fleming M, Barrett T. Characterization of African field isolates of rinderpest virus. Vet Microbiol. 1995;44:151–163. doi: 10.1016/0378-1135(95)00008-x. [DOI] [PubMed] [Google Scholar]
- 32.Webster R G. Influenza viruses. In: Webster R G, Granoff A, editors. Encyclopedia of virology. San Diego, Calif: Academic Press; 1996. [Google Scholar]
- 33.Wertz G W, Perepelitsa V P, Ball L A. Gene rearrangement attenuates expression and lethality of a nonsegmented negative strand RNA virus. Proc Natl Acad Sci USA. 1998;95:3501–3506. doi: 10.1073/pnas.95.7.3501. [DOI] [PMC free article] [PubMed] [Google Scholar]