Highlights
-
•
Fewer healthcare personnel frequently received influenza vaccines from 2011─2018.
-
•
Frequently vaccinated healthcare personnel had some influenza vaccine knowledge.
-
•
Healthcare personnel who reported barriers were less frequently vaccinated.
-
•
Campaigns could strengthen influenza vaccine knowledge and accessibility.
Keywords: Knowledge, Attitudes, Practices, Influenza vaccination, Healthcare personnel
Abstract
Introduction
Despite a government-subsidized vaccination program, healthcare personnel (HCP) influenza vaccination uptake remains low in Peru. Using three years of cross-sectional surveys and an additional five years of prior vaccination history of HCP in Peru, we explored HCP knowledge, attitudes, and practices (KAP) of influenza illness and its impact on vaccination frequency.
Methods
In 2016, the Estudio Vacuna de Influenza Peru (VIP) cohort was initiated in Lima, Peru, which collected information about HCP KAP and influenza vaccination history from 2011─2018. HCP were classified by their 8-year influenza vaccination history as never (0 years), infrequently (1─4 years), or frequently (5─8 years) vaccinated. Logistic regression models were used to describe KAP associated with frequent compared to infrequent influenza vaccination, adjusted for each HCP’s healthcare workplace, age, sex, preexisting medical conditions, occupation, and length of time providing direct patient care.
Results
From 2016─2018, 5131 HCP were recruited and 3120 fully enrolled in VIP; 2782 consistently reported influenza vaccination status and became our analytic sample. From 2011─2018, 14.3% of HCP never, 61.4% infrequently, and 24.4% frequently received influenza vaccines. Compared to HCP who were infrequently vaccinated, frequently vaccinated HCP were more likely to believe they were susceptible to influenza (adjusted odds ratio [aOR]:1.49, 95% confidence interval [CI]:1.22─1.82), perceived vaccination to be effective (aOR:1.92, 95%CI:1.59─2.32), were knowledgeable about influenza and vaccination (aOR:1.37, 95%CI:1.06─1.77), and believed vaccination had emotional benefits like reduced regret or anger if they became ill with influenza (aOR:1.96, 95%CI:1.60─2.42). HCP who reported vaccination barriers like not having time or a convenient place to receive vaccines had reduced odds of frequent vaccination (aOR:0.74, 95%CI:0.61─0.89) compared to those without reported barriers.
Conclusion
Few HCP frequently received influenza vaccines during an eight-year period. To increase HCP influenza vaccination in middle-income settings like Peru, campaigns could strengthen influenza risk perception, vaccine knowledge, and accessibility.
Introduction
Influenza causes substantive economic and disease burden in Peru that results in high rates of hospitalizations and deaths [1], [2], [3], [4]. To mitigate this burden, each year Peru’s government purchases one trivalent inactivated influenza vaccine product though the Pan American Health Organization and provides doses free of charge for target groups identified by the World Health Organization (WHO) Strategic Advisory Group of Experts (SAGE) [5]; these target groups include young children, pregnant women, older adults, individuals with comorbidities, and healthcare personnel (HCP). Despite a national program for HCP influenza vaccination, knowledge, attitudes, and practices (KAP) of these SAGE target groups suggest that HCP insufficiently receive and recommend influenza vaccination in Peru [6], [7], [8], possibly because of ambivalence about individuals’ risk of influenza illness or the value of influenza vaccination [9]. Understanding the reasons why HCP are infrequently vaccinated could help health authorities improve risk communication, optimize influenza vaccine access, and address infrequent vaccine use and hesitancy.
Using three years of cross-sectional surveys and an additional five years of prior vaccination history among HCP in Peru, we aimed to assess influenza vaccination uptake among HCP as well as behavioral factors that influenced their likelihood of receiving influenza vaccines. Specifically, we (i) described who was most likely to be frequently compared to infrequently vaccinated against influenza, and (ii) identified factors associated with infrequent vaccination to determine priority areas for improving annual vaccination in this population.
Materials and methods
Study design
In 2016, the Estudio Vacuna de Influenza Peru (VIP) cohort was initiated to learn more about influenza vaccination acceptance and effectiveness among HCP. Details concerning VIP study recruitment and design have been previously published [10]. Briefly, participants were recruited into VIP using a stratified sampling strategy, where participants at one of five participating hospitals (Dos de Mayo National Hospital, Cayetano Heredia National Hospital, Daniel Alcides Carrion National Hospital, National Institute of Child Health (Del Niño), and Archbishop Loayza Hospital) in Lima, Peru were categorized into 18 strata by sex, age, and occupation; enrollment did not begin at National Institute of Child Health (Del Niño) and Archbishop Loayza Hospital until 2017. Once recruited, participants completed a survey at enrollment, at the start of each influenza season, and at the end of the season. This analysis focused on responses to the enrollment and start of season surveys. These surveys collected information about HCP demographics, occupational roles, workplaces, personal health status, and influenza illness and vaccination knowledge, attitudes, and practices (KAP). Prior influenza vaccination history from 2011 to 2015 was also collected by self-report at enrollment and verified by the HCP’s hospital vaccination registry. From 2016 to 2018, follow-up was conducted each July through August, during Peru’s annual influenza season which occurs from May to October [1], [11].
Among those who enrolled from 2016 to 2018, HCP were included in the analysis population if they were: (i) ≥ 18-years-old; (ii) worked ≥ 30 h a week; (iii) employed by the hospital for at least one year; (iv) provided direct patient care; (v) fully enrolled in the study for at least one year; and (vi) reported influenza vaccination status during at least one year of prospective follow-up from 2016 to 2018. Direct patient care was defined as regular hands-on contact with patients during a typical work shift. A participant was considered fully enrolled if they gave consent to participate in the study, attended study orientation, and provided a pre-season blood draw. If a person received the current season’s influenza vaccine prior to enrollment, they were not enrolled in VIP.
Demographic and occupational factors and influenza vaccination uptake
To learn more about HCP influenza vaccination practices over time, we restricted analyses to only HCP who had influenza vaccination status reported all 8 years and classified each person as never, infrequently, or frequently vaccinated against influenza from 2011 to 2018. Similar to previous work [12], HCP classified as never vaccinated self-reported receiving 0 influenza vaccinations during that period; people infrequently vaccinated reported receiving 1─4 influenza vaccinations, and those frequently vaccinated received 5─8 influenza vaccinations.
Excluding those who never received influenza vaccines, we assessed HCP characteristics associated with the likelihood of frequent versus infrequent vaccination against influenza. Demographic and occupational factors assessed included: (i) hospital of employment; (ii) age (18─34 years, 35─49 years, 50─70 years); (iii) sex; (iv) education level (high school or less, some university, graduated university, master’s degree, advanced graduate degree); (v) occupation (i.e., physicians; nurses, technicians, & therapists; and medical assistants & support personnel); (vi) medical care setting (i.e., outpatient, critical care, emergency department, hospital, and other); (vii) practicing patient care for > 10 years; (viii) perceived health status (excellent, very good, or good; fair or poor); (ix) smoking status; and (x) presence of a preexisting medical condition. Having a preexisting medical condition was defined as currently receiving medical care for at least one of the following conditions: asthma, cancer, lung condition, diabetes, heart condition, high blood pressure, immunosuppressive condition, kidney disease, neurologic problem, or other medical condition. The other medical condition category included tuberculosis, psoriasis, pancreatitis, migraines, gastritis, rheumatoid arthritis, and more.
Knowledge, attitudes, and practices and influenza vaccination uptake
Next, we investigated how KAP influenced influenza vaccination consistency over multiple years. To do so, we assessed how (i) perceived susceptibility to influenza illness; (ii) perceived vaccine effectiveness; (iii) influenza and vaccination knowledge; (iv) concerns about vaccination safety or pain from vaccination; (v) emotional benefits of vaccination like reduced regret or anger if HCP became ill with influenza; (vi) barriers to vaccination like inconvenient times or places for vaccination; (vii) supervisor recommendation of vaccination; (viii) and perceived vaccination protection for self and (ix) for patients was associated with how often HCP received influenza vaccines (Table 1). Composite coding choices for specific KAP are described in detail in Table 1 and were drawn from the Health Belief Model and the Theory of Planned Behavior with items based on prior literature [13]. For our analyses, only questions asked during each survey year were chosen to signify KAP perceptions, with the exception of perceived vaccination protection for self and patients, which was only collected at enrollment. To model the likelihood of frequent versus infrequent vaccination for eight years, we ran univariable and multivariable logistic regression models comparing each KAP category collected at enrollment. Models were adjusted for each HCP’s hospital workplace, age, sex, presence of at least one preexisting medical condition, occupation, and length of time practicing patient care, as determined by directed acyclic graph analysis (Supplemental Fig. 1). To examine how results differed across hospitals, we also ran adjusted logistic regressions stratified by each HCP’s hospital of employment. For KAP categories with composite coding choices, univariable and multivariable logistic regression models were re-rerun to compare odds of frequent vaccination across each specific KAP question that was in the composite variables.
Table 1.
Classification of knowledge, attitudes, and practices surrounding influenza vaccination.
| KAP criterion | Survey question | Response | Composite coding |
|---|---|---|---|
| Perceived influenza susceptibility | If you are unable to or don’t get an influenza vaccination, what do you think your chance of getting the flu this season will be? |
Not susceptible: Almost zero, very small, small, or moderate chance Susceptible: Large, very large, or almost certain chance |
Not done |
| Perceived vaccine effectiveness | How effective do you think the influenza vaccine is in preventing you from getting sick with influenza? |
Not effective: Not at all, not too, or somewhat effective Effective: Extremely or very effective |
Not done |
| Knowledge of influenza and vaccine | Agree or disagree with the following statement: People with influenza can transmit the virus only after their symptoms appear. |
0: Strongly agree, mildly agree, or neutral 1: Mildly or strongly disagree |
No knowledge: Sum of three variables equals 0 Some knowledge: Sum of three variables ≥ 1 |
| Agree or disagree with the following statement: The influenza vaccine could give me influenza. |
0: Strongly agree, mildly agree, or neutral 1: Mildly or strongly disagree |
||
| Agree or disagree with the following statement: People can spread influenza virus even when they are feeling well. |
0: Strongly disagree, mildly disagree, or neutral 1: Mildly or strongly agree |
||
| Concerns about vaccination safety or pain from vaccination | Agree or disagree with the following statement: Influenza vaccination is safe. |
0: Strongly agree, mildly agree, or neutral 1: Mildly or strongly disagree |
No concerns: Sum of two variables equals 0 Some concerns: Sum of two variables ≥ 1 |
| Agree or disagree with the following statement: The influenza shot is painful. |
0: Strongly disagree, mildly disagree, or neutral 1: Mildly or strongly agree |
||
| Emotional benefits of vaccination | Agree or disagree with the following statement: If I don’t get an influenza vaccination and end up getting sick with influenza, I’d be mad at myself for not getting the vaccine. |
0: Strongly disagree, mildly disagree, or neutral 1: Mildly or strongly agree |
No emotional benefits: Sum of two variables equals 0 Some emotional benefits: Sum of two variables ≥ 1 |
| Agree or disagree with the following statement: If I don’t get an influenza vaccination, I will regret it. |
0: Strongly disagree, mildly disagree, or neutral 1: Mildly or strongly agree |
||
| Barriers to vaccination like inconvenient times or places for vaccination | Agree or disagree with the following statement: I usually do not have time to get vaccinated with the influenza vaccine. |
0: Strongly disagree, mildly disagree, or neutral 1: Mildly or strongly agree |
No barriers: Sum of two variables equals 0 Some barrier: Sum of two variables ≥ 1 |
| Agree or disagree with the following statement: There is not a convenient place for me to get vaccinated with the influenza vaccine. |
0: Strongly disagree, mildly disagree, or neutral 1: Mildly or strongly agree |
||
| Supervisor recommendation of vaccination | Agree or disagree with the following statement: A supervisor or other leader at my workplace has recommended that I get an annual influenza vaccination. |
No: Strongly disagree, mildly disagree, or neutral Yes: Mildly or strongly agree |
Not done |
| Perceived vaccination protection for self | Agree or disagree with following statement: Influenza vaccination can protect me from getting sick with influenza. |
No protection: Strongly disagree, mildly disagree, or neutral Some protection: Mildly or strongly agree |
Not done |
| Perceived vaccination protection for patient | Agree or disagree with following statement: If I get an influenza vaccination, patients at my health facility will be better protected from influenza. |
No protection: Strongly disagree, mildly disagree, or neutral Some protection: Mildly or strongly agree |
Not done |
Abbreviations: KAP, knowledge, attitudes, and practices.
A sensitivity analysis was conducted to assess whether categorization choices of vaccine consistency influenced results; this was done by (i) re-running the initial univariable and multivariable logistic regression models using alternative cut points to define vaccine consistency (never: 0 vaccinations, inconsistent: 1─7 vaccinations, consistent: 8 vaccinations from 2011 to 2018) as well as (ii) running univariable and multivariable Poisson regression models with a continuous coding of cumulative number of years vaccinated. Models used for these sensitivity analyses adjusted for the same covariates as the main analysis. An additional sensitivity analysis restricted the dataset to only participants practicing healthcare since 2011 or earlier and likely able to receive influenza vaccines through hospital employment; this analysis re-ran the initial univariable and multivariable logistic regression models to compare people with frequent versus infrequent influenza vaccination over time.
We did a sub-analysis of participants who were surveyed during all three survey years (2016 to 2018) and were classified as being infrequently vaccinated from 2011 to 2018 to account for possible changes in KAP perceptions among those who were infrequently vaccinated. The sub-analysis focused on HCP who were infrequently vaccinated because this group had a history of receiving at least one influenza vaccine and potential to increase vaccination uptake. Among this subset, we ran univariable and multivariable generalized estimating equation (GEE) logistic regressions to model odds of annual influenza vaccination (yes, no) across each survey year’s KAP responses collected in the start of season survey. GEE models accounted for participant-level clustering. Perceived vaccination protection for self and patients was excluded from this analysis because it was only collected at enrollment. For KAP variables with composite coding, GEE models were repeated for the specific KAP questions.
We also estimated the odds that someone would get vaccinated based on the vaccine product offered that year. To do so, we ran univariable GEE logistic regressions comparing vaccine brands and people’s odds of switching their status to vaccinated among HCP who reported receiving vaccines and were surveyed from 2016 to 2018. All analyses were conducted using the R packages ‘tidyverse‘ and ‘geepack‘ in R version 4.0.4 [14], [15], [16].
Ethical review
The VIP study was approved by seven institutional review boards (IRBs) of collaborating facilities: (i) Naval Medical Research Unit 6; (ii) Abt Associates; (iii) Dos de Mayo National Hospital; (iv) Cayetano Heredia National Hospital; (v) Daniel Alcides Carrion National Hospital; (vi) National Institute of Child Health (Del Niño); (vii) and Archbishop Loayza Hospital. All participants provided written informed consent to participate in the study. IRBs at these organizations reviewed and approved the study protocols and procedures (Abt Associates Protocol: 0840; NAMRU6 Protocol: NAMRU6.2015.0001) in compliance with all applicable federal regulations governing the protection of human subjects.
Results
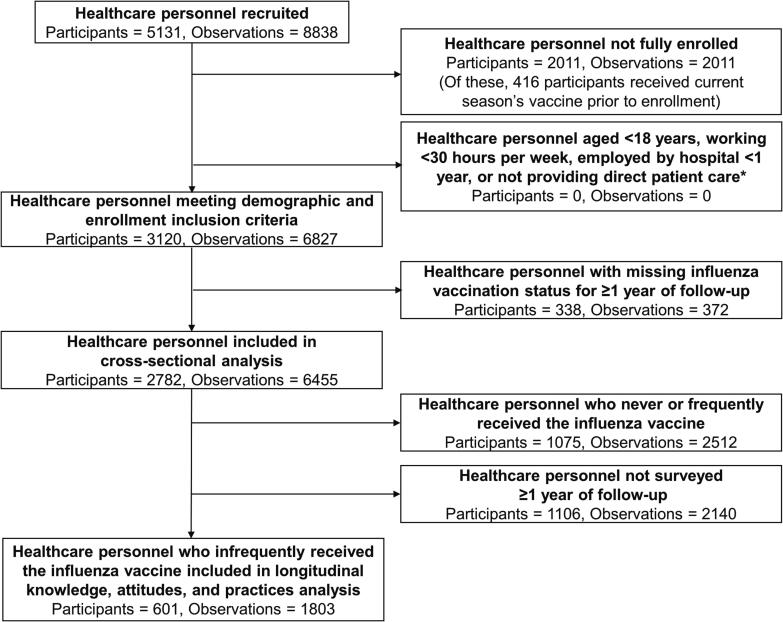
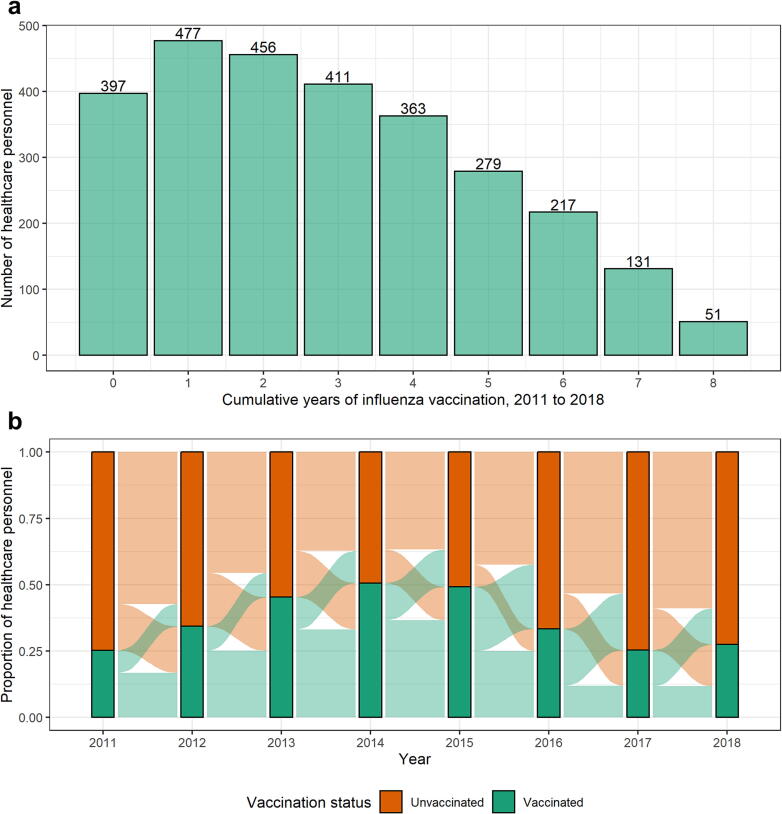
From 2016 to 2018, a total of 5131 HCP were recruited and 3120 fully enrolled in VIP with influenza vaccination history recorded from 2011 to 2018 (Fig. 1, Supplemental Table 1). After excluding 338 HCP without influenza vaccination status for at least one year of follow-up from 2011 to 2018, 2782 people remained in the analysis set. Of those excluded, influenza vaccine uptake was low with 73.9% of HCP never receiving an influenza vaccine over the eight-year period (Supplemental Table 2). In the analysis set, most HCP were aged 35─49 years (40.7%), female (72.1%), and worked as medical assistants or support personnel (53.7%) (Table 1). From 2011 to 2018, the number of years people received influenza vaccines varied, with HCP receiving the vaccine for a median of 3 (IQR: 3) out of 8 years’ influenza seasons and only 1.8% (n = 51) of HCP receiving the vaccine all 8 years (Fig. 2a). HCP had inconsistent influenza vaccination patterns with approximately 25% of people switching their vaccination status from year-to-year (Fig. 2b). HCP who received the Vaxigrip vaccine compared to the GC FLU vaccine had higher odds of switching their vaccination status to being vaccinated (crude odds ratio [cOR]: 2.71, 95% confidence interval [CI]: 1.97─3.73, Supplemental Table 3) and vaccination uptake differed across years and occupation depending on the vaccine brands offered (Supplemental Fig. 2). From 2011 to 2018, 14.3% (n = 397) of HCP never (0 years), 61.4% (n = 1707) infrequently (1─4 years), and 24.4% (n = 678) frequently (5─8 years) received seasonal influenza vaccines (Table 2).
Fig. 1.
Number of healthcare personnel recruited, enrolled, and included in the analysis in Peru. Healthcare personnel that were fully enrolled in the study met all additional demographic inclusion criteria: (i) ≥ 18 years old, (ii) working at ≥ 30 h a week, (iii), employed by the hospital for ≥ 1 year, (iv) and providing direct patient care. Personnel classified as never vaccinated self-reported receiving 0 influenza vaccinations from 2011 to 2018. People infrequently vaccinated self-reported receiving 1─4 influenza vaccinations and those frequently vaccinated received 5─8 influenza vaccinations during the same time.
Fig. 2.
Influenza vaccination status over time for healthcare personnel. 2a. The distribution of the cumulative years that healthcare personnel received influenza vaccines from 2011 to 2018 is displayed. Participants that did not report vaccination history for all 8 years are excluded. 2b. The proportion of healthcare personnel that received (green bars) or did not receive (orange bars) the influenza vaccine within each year is shown. The ribbons connecting each bar represent movement of healthcare personnel between vaccination status categories each year. Participants who did not report vaccination history for all 8 years are excluded. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Table 2.
Demographic and occupational characteristics associated with frequency of healthcare personnel influenza vaccination receipt.
| Characteristics* |
Total HCP^ n (%) |
Influenza vaccination history# |
Odds of frequent vs. infrequent vaccination |
||
|---|---|---|---|---|---|
|
Never n (%) |
Infrequently n (%) |
Frequently n (%) |
cOR (95% CI) |
||
| All | 2782 | 397 | 1707 | 678 | – |
| Hospital | |||||
| Dos de Mayo National Hospital | 672 (24.2) | 65 (16.4) | 386 (22.6) | 221 (32.6) | Ref |
| Cayetano Heredia National Hospital | 696 (25.0) | 73 (18.4) | 471 (27.6) | 152 (22.4) | 0.56 (0.44, 0.72) |
| Daniel Alcides Carrion National Hospital | 271 (9.7) | 37 (9.3) | 166 (9.7) | 68 (10.0) | 0.72 (0.51, 0.99) |
| National Institute of Child Health (Del Niño) | 547 (19.7) | 46 (11.6) | 325 (19.0) | 176 (26.0) | 0.95 (0.74, 1.21) |
| Archbishop Loayza Hospital | 596 (21.4) | 176 (44.3) | 359 (21.0) | 61 (9.0) | 0.30 (0.21, 0.41) |
| Age | |||||
| 18–34 years | 840 (30.2) | 115 (29.0) | 539 (31.6) | 186 (27.4) | Ref |
| 35–49 years | 1133 (40.7) | 154 (38.8) | 709 (41.5) | 270 (39.8) | 1.10 (0.89, 1.37) |
| 50–70 years | 809 (29.1) | 128 (32.2) | 459 (26.9) | 222 (32.7) | 1.40 (1.11, 1.77) |
| Sex | |||||
| Male | 777 (27.9) | 119 (30.0) | 490 (28.7) | 168 (24.8) | Ref |
| Female | 2005 (72.1) | 278 (70.0) | 1217 (71.3) | 510 (75.2) | 1.22 (1.00, 1.50) |
| Education level | |||||
| High school or less | 224 (8.1) | 38 (9.6) | 142 (8.3) | 44 (6.5) | Ref |
| Some university | 1088 (39.1) | 163 (41.1) | 674 (39.5) | 251 (37.0) | 1.20 (0.84, 1.75) |
| Graduated university | 950 (34.1) | 122 (30.7) | 580 (34.0) | 248 (36.6) | 1.38 (0.96, 2.01) |
| Master’s degree | 367 (13.2) | 55 (13.9) | 209 (12.2) | 103 (15.2) | 1.59 (1.06, 2.42) |
| Advanced graduate degree | 152 (5.5) | 18 (4.5) | 102 (6.0) | 32 (4.7) | 1.01 (0.60, 1.70) |
| Unknown | 1 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | – |
| Occupation | |||||
| Physicians | 379 (13.6) | 66 (16.6) | 240 (14.1) | 73 (10.8) | Ref |
| Nurses, technicians, & therapists | 910 (32.7) | 94 (23.7) | 539 (31.6) | 277 (40.9) | 1.69 (1.26, 2.29) |
| Medical assistants & support personnel | 1493 (53.7) | 237 (59.7) | 928 (54.4) | 328 (48.4) | 1.16 (0.87, 1.56) |
| Medical care setting | |||||
| Outpatient | 310 (11.1) | 49 (12.3) | 195 (11.4) | 66 (9.7) | Ref |
| Critical care | 217 (7.8) | 11 (2.8) | 126 (7.4) | 80 (11.8) | 1.88 (1.26, 2.79) |
| Emergency department | 298 (10.7) | 34 (8.6) | 172 (10.1) | 92 (13.6) | 1.58 (1.09, 2.31) |
| Hospital | 645 (23.2) | 91 (22.9) | 397 (23.3) | 157 (23.2) | 1.17 (0.84, 1.64) |
| Other** | 1102 (39.6) | 175 (44.1) | 681 (39.9) | 246 (36.3) | 1.07 (0.78, 1.47) |
| Unknown | 210 (7.5) | 37 (9.3) | 136 (8.0) | 37 (5.5) | – |
| Patient care for >10 years | |||||
| No | 1293 (46.5) | 169 (42.6) | 832 (48.7) | 292 (43.1) | Ref |
| Yes | 1487 (53.5) | 227 (57.2) | 874 (51.2) | 386 (56.9) | 1.26 (1.05, 1.51) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – |
| Perceived health status | |||||
| Excellent, very good, or good | 2240 (80.5) | 320 (80.6) | 1360 (79.7) | 560 (82.6) | Ref |
| Fair or poor | 540 (19.4) | 76 (19.1) | 346 (20.3) | 118 (17.4) | 0.83 (0.66, 1.04) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – |
| Smoker | |||||
| No | 2539 (91.3) | 356 (89.7) | 1567 (91.8) | 616 (90.9) | Ref |
| Yes | 241 (8.7) | 40 (10.1) | 139 (8.1) | 62 (9.1) | 1.13 (0.82, 1.55) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – |
| Preexisting medical condition*** | |||||
| No | 2198 (79.0) | 311 (78.3) | 1372 (80.4) | 515 (76.0) | Ref |
| Yes | 584 (21.0) | 86 (21.7) | 335 (19.6) | 163 (24.0) | 1.30 (1.05, 1.60) |
Abbreviations: CI, confidence interval; cOR, crude odds ratio; HCP, healthcare personnel.
* Collected at enrollment.
** The “other” medical care setting included internal medicine, pediatrics, surgery, gynecology and obstetrics, dentistry, pharmacy, laboratory, nutrition, and social assistance departments.
*** Included those currently receiving medical care for at least one of the following conditions: asthma, cancer, lung condition, diabetes, heart condition, high blood pressure, immunosuppressive condition, kidney disease, neurologic problem, or other medical condition.
Only people who had influenza vaccination status reported all 8 years (2011 to 2018) were in included in this analysis.
People classified as never vaccinated self-reported receiving 0 influenza vaccinations from 2011 to 2018. People infrequently vaccinated self-reported receiving 1─4 influenza vaccinations and those frequently vaccinated received 5─8 influenza vaccinations during the same time.
We identified groups of HCP who consistently received influenza vaccines (Table 2). Compared to HCP aged 18─34 years, those aged 50─70 years had higher odds of frequent vaccination (cOR: 1.40, 95% CI: 1.11─1.77). Increasing education level was associated with increased odds of frequent vaccination (Master’s degree vs. high school or less, cOR: 1.59, 95% CI: 1.06─2.42) except for those who had an advanced graduate degree (compared to high school or less, cOR: 1.01, 95% CI: 0.60─1.70); this trend was supported by HCP occupation with nurses, technicians, and therapists having a higher likelihood of frequent vaccination than physicians (cOR: 1.69, 95% CI: 1.26─2.29). Those that worked in a critical care (cOR: 1.88, 95% CI: 1.26─2.79) or emergency department (cOR: 1.58, 95% CI: 1.09─2.31) setting were more frequently vaccinated than those that worked in an outpatient setting. Practicing patient care for > 10 years (cOR: 1.26, 95% CI: 1.05─1.51) and having a preexisting medical condition (cOR: 1.30, 95% CI: 1.05─1.60) were also associated with increased odds of frequent influenza vaccination. Although, after adjusting for age, there was no longer an association between having a preexisting medical condition and odds of frequent vaccination (adjusted odds ratio [aOR]: 1.20, 95% CI: 0.96─1.50).
Next, we investigated how HCP’s knowledge, attitudes, and practices collected at enrollment were associated with how often HCP received influenza vaccines (Table 3). HCP who believed they were susceptible to influenza illness if they didn’t receive vaccines (aOR: 1.49, 95% CI: 1.22─1.82) or perceived vaccines to be effective (aOR: 1.92, 95% CI: 1.59─2.32) received seasonal influenza vaccines more often than those who did not. HCP with some knowledge of influenza and vaccines (aOR: 1.37, 95% CI: 1.06─1.77), especially of influenza vaccination (aOR: 1.26, 95% CI: 1.06─1.50, Supplemental Table 4), or who thought vaccination had emotional benefits like preventing anger or regret (aOR: 1.96, 95% CI: 1.60─2.42) also had higher odds of frequent compared to infrequent vaccination (Table 3, Supplemental Table 4). HCP who recalled supervisor recommendation of vaccination had 1.72 (95% CI: 1.43─2.08) times the odds of frequent vaccination compared to those who did not. HCP who perceived vaccination protected them (aOR: 2.70, 95% CI: 1.82─4.15) or their patients (aOR: 2.14, 95% CI: 1.52─3.07) were more likely to be frequently vaccinated; although, results were limited by a high amount of missingness (50.4% for perceived vaccination protection for self or patients).
Table 3.
Knowledge, attitudes, and practices associated with frequency of healthcare personnel influenza vaccination receipt.
| Characteristics* |
Total HCP^ n (%) |
Influenza vaccination history# |
Odds of frequent vs. infrequent vaccination |
|||
|---|---|---|---|---|---|---|
|
Never n (%) |
Infrequently n (%) |
Frequently n (%) |
cOR (95% CI) |
aOR## (95% CI) |
||
| All | 2782 | 397 | 1707 | 678 | – | – |
| Perceived influenza susceptibility | ||||||
| Not susceptible | 2073 (74.5) | 334 (84.1) | 1285 (75.3) | 454 (67.0) | Ref | Ref |
| Susceptible | 707 (25.4) | 62 (15.6) | 421 (24.7) | 224 (33.0) | 1.51 (1.24, 1.83) | 1.49 (1.22, 1.82) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – | – |
| Perceived vaccine effectiveness | ||||||
| Not effective | 1447 (52.0) | 275 (69.3) | 911 (53.4) | 261 (38.5) | Ref | Ref |
| Effective | 1333 (47.9) | 121 (30.5) | 795 (46.6) | 417 (61.5) | 1.83 (1.53, 2.20) | 1.92 (1.59, 2.32) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – | – |
| Knowledge of influenza and vaccine | ||||||
| No knowledge | 504 (18.1) | 97 (24.4) | 310 (18.2) | 97 (14.3) | Ref | Ref |
| Some knowledge | 2276 (81.8) | 299 (75.3) | 1396 (81.8) | 581 (85.7) | 1.33 (1.04, 1.71) | 1.37 (1.06, 1.77) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – | – |
| Concerns about vaccination safety or pain from vaccination | ||||||
| No concerns | 1574 (56.6) | 253 (63.7) | 955 (55.9) | 366 (54.0) | Ref | Ref |
| Some concerns | 1206 (43.4) | 143 (36.0) | 751 (44.0) | 312 (46.0) | 1.08 (0.91, 1.30) | 0.99 (0.83, 1.20) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – | – |
| Emotional benefits of vaccination | ||||||
| No emotional benefits | 1027 (36.9) | 195 (49.1) | 666 (39.0) | 166 (24.5) | Ref | Ref |
| Some emotional benefits | 1753 (63.0) | 201 (50.6) | 1040 (60.9) | 512 (75.5) | 1.98 (1.62, 2.42) | 1.96 (1.60, 2.42) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – | – |
| Barriers to vaccination like inconvenient times or places for vaccination | ||||||
| No barriers | 1753 (63.0) | 235 (59.2) | 1053 (61.7) | 465 (68.6) | Ref | Ref |
| Some barriers | 1027 (36.9) | 161 (40.6) | 653 (38.3) | 213 (31.4) | 0.74 (0.61, 0.89) | 0.74 (0.61, 0.89) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – | – |
| Supervisor vaccination recommendation | ||||||
| No | 1342 (48.2) | 239 (60.2) | 854 (50.0) | 249 (36.7) | Ref | Ref |
| Yes | 1438 (51.7) | 157 (39.5) | 852 (49.9) | 429 (63.3) | 1.73 (1.44, 2.07) | 1.72 (1.43, 2.08) |
| Unknown | 2 (0.1) | 1 (0.3) | 1 (0.1) | 0 (0.0) | – | – |
| Perceived vaccination protection for self | ||||||
| No protection | 302 (10.9) | 73 (18.4) | 198 (11.6) | 31 (4.6) | Ref | Ref |
| Some protection | 1077 (38.7) | 126 (31.7) | 668 (39.1) | 283 (41.7) | 2.71 (1.83, 4.12) | 2.70 (1.82, 4.15) |
| Unknown | 1403 (50.4) | 198 (49.9) | 841 (49.3) | 364 (53.7) | – | – |
| Perceived vaccination protection for patient | ||||||
| No protection | 360 (12.9) | 82 (20.7) | 230 (13.5) | 48 (7.1) | Ref | Ref |
| Some protection | 1019 (36.6) | 117 (29.5) | 636 (37.3) | 266 (39.2) | 2.00 (1.43, 2.85) | 2.14 (1.52, 3.07) |
| Unknown | 1403 (50.4) | 198 (49.9) | 841 (49.3) | 364 (53.7) | – | – |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; cOR, crude odds ratio; HCP, healthcare personnel.
* Collected at enrollment.
Perceived influenza susceptibility: If you are unable to or don’t get an influenza vaccination, what do you think your chance of getting the flu this season will be?
Perceived vaccine effectiveness: How effective do you think the influenza vaccine is in preventing you from getting sick with influenza?
Knowledge of influenza and vaccine was a composite of three questions: (i) Agree or disagree with the following statement: People with influenza can transmit the virus only after their symptoms appear; (ii) Agree or disagree with the following statement: The influenza vaccine could give me influenza; and (iii) Agree or disagree with the following statement: People can spread influenza virus even when they are feeling well.
Concerns about vaccination was a composite of two questions: (i) Agree or disagree with the following statement: Influenza vaccination is safe; and (ii) Agree or disagree with the following statement: The influenza shot is painful.
Emotional benefits of vaccination were a composite of two questions: (i) Agree or disagree with the following statement: If I don’t get an influenza vaccination and end up getting sick with influenza, I’d be mad at myself for not getting the vaccine; and (ii) Agree or disagree with the following statement: If I don’t get an influenza vaccination, I will regret it.
Barriers to vaccination was a composite of two questions: (i) Agree or disagree with the following statement: I usually do not have time to get vaccinated with the influenza vaccine; and (ii) Agree or disagree with the following statement: There is not a convenient place for me to get vaccinated with the influenza vaccine.
Supervisor recommendation vaccination: Agree or disagree with the following statement: A supervisor or other leader at my workplace has recommended that I get an annual influenza vaccination.
Perceived vaccination protection for self: Agree or disagree with following statement: Influenza vaccination can protect me from getting sick with influenza.
Perceived vaccination protection for patient: Agree or disagree with following statement: If I get an influenza vaccination, patients at my health facility will be better protected from influenza.
Only people who had influenza vaccination status reported all 8 years (2011 to 2018) were in included in this analysis.
People classified as never vaccinated self-reported receiving 0 influenza vaccinations from 2011 to 2018. People infrequently vaccinated received 1─4 influenza vaccinations and those frequently vaccinated received 5─8 influenza vaccinations during the same time.
Adjusted for HCP hospital of employment, age, sex, preexisting medical condition, occupation, and providing patient care for > 10 years.
Some HCP reported barriers to vaccination, such as not having time or a convenient place to receive vaccines, which was associated with reduced odds of frequent vaccination (aOR: 0.74, 95% CI: 0.61─0.89) compared to those who did not report barriers (Table 3); not having time to get vaccinated was a driver for this relationship (aOR: 0.58, 95% CI: 0.46─0.73, Supplemental Table 4). HCP generally concerned about vaccination were vaccinated as frequently as those without such concerns (aOR: 0.99, 95% CI: 0.83─1.20); however, assessing specific concerns illustrated that HCP concerned about vaccine safety were less likely to be frequently vaccinated (aOR: 0.52, 95% CI: 0.32─0.81, Supplemental Table 4). Similar patterns between KAP perceptions and frequency of influenza vaccination receipt were seen when results were stratified by each HCP’s hospital of employment (Supplemental Table 5); although not all perceptions were associated with vaccination frequency. Results remained constant across KAP categories when alternative coding choices were used to define vaccination consistency (Supplemental Tables 6 and 7) as well as when restricting analyses to people practicing patient care since 2011 or earlier (Supplemental Table 8).
To better capture how these KAP perceptions changed during survey years, we restricted the analysis to only people who were surveyed for all years of follow-up from 2016 to 2018 (i.e., 601 HCP). Among these 601 HCP, we investigated how each year’s KAP perceptions were associated with their odds of influenza vaccination that year (Table 4). Similar to the cross-sectional analysis of KAP perceptions at enrollment, perceived influenza susceptibility (aOR: 1.61, 95% CI: 1.25─2.07), influenza vaccine effectiveness (aOR: 1.62, 95% CI: 1.29─2.05), and emotional benefits of influenza vaccination like reduced regret or anger if they became ill with influenza (aOR: 1.68, 95% CI: 1.31─2.17) all remained significantly associated with higher odds of influenza vaccination. Influenza and vaccine knowledge (aOR: 1.11, 95% CI: 0.79─1.56) and having a supervisor recommend vaccination (aOR: 1.11, 95% CI: 0.89─1.39) were no longer associated with vaccination frequency among those surveyed for all years. The association between barriers to influenza vaccination (aOR: 0.93, 95% CI: 0.74─1.18) and vaccination frequency was attenuated but having general concerns about vaccination (aOR: 0.77, 95% CI: 0.61─0.98) and specifically vaccine safety (aOR: 0.31, 95% CI: 0.16─0.60) were associated with reduced odds of influenza vaccination (Table 4, Supplemental Table 9).
Table 4.
Association between knowledge, attitudes, and practices and odds of influenza vaccination among those infrequently vaccinated over time, 2016─2018.
| Characteristics* |
Total observations^ n (%) |
Influenza vaccination status, 2016─2018 |
Odds of being vaccinated vs. unvaccinated |
||
|---|---|---|---|---|---|
|
Unvaccinated n (row %) |
Vaccinated n (row %) |
cOR (95% CI) | aOR (95% CI)# | ||
| All | 1803 | 1411 (78.3) | 392 (21.7) | – | – |
| Perceived influenza susceptibility | |||||
| Not susceptible | 1339 (74.3) | 1067 (79.7) | 272 (20.3) | Ref | Ref |
| Susceptible | 423 (23.5) | 303 (71.6) | 120 (28.4) | 1.54 (1.20, 1.98) | 1.61 (1.25, 2.07) |
| Unknown | 41 (2.3) | 41 (100.0) | 0 (0.0) | – | – |
| Perceived vaccine effectiveness | |||||
| Not effective | 917 (50.9) | 749 (81.7) | 168 (18.3) | Ref | Ref |
| Effective | 845 (46.9) | 621 (73.5) | 224 (26.5) | 1.58 (1.25, 1.98) | 1.62 (1.29, 2.05) |
| Unknown | 41 (2.3) | 41 (100.0) | 0 (0.0) | – | – |
| Knowledge of influenza and vaccine | |||||
| No knowledge | 266 (14.8) | 210 (78.9) | 56 (21.1) | Ref | Ref |
| Some knowledge | 1493 (82.8) | 1157 (77.5) | 336 (22.5) | 1.09 (0.78, 1.53) | 1.11 (0.79, 1.56) |
| Unknown | 44 (2.4) | 44 (100.0) | 0 (0.0) | – | – |
| Concerns about vaccination safety or pain from vaccination | |||||
| No concerns | 1033 (57.3) | 786 (76.1) | 247 (23.9) | Ref | Ref |
| Some concerns | 726 (40.3) | 581 (80.0) | 145 (20.0) | 0.80 (0.64, 1.01) | 0.77 (0.61, 0.98) |
| Unknown | 44 (2.4) | 44 (100.0) | 0 (0.0) | – | – |
| Emotional benefits of vaccination | |||||
| No emotional benefits | 716 (39.7) | 593 (82.8) | 123 (17.2) | Ref | Ref |
| Some emotional benefits | 1045 (58.0) | 776 (74.3) | 269 (25.7) | 1.65 (1.29, 2.12) | 1.68 (1.31, 2.17) |
| Unknown | 42 (2.3) | 42 (100.0) | 0 (0.0) | – | – |
| Barriers to vaccination like inconvenient times or places for vaccination | |||||
| No barriers | 1143 (63.4) | 885 (77.4) | 258 (22.6) | Ref | Ref |
| Some barriers | 616 (34.2) | 483 (78.4) | 133 (21.6) | 0.95 (0.75, 1.19) | 0.93 (0.74, 1.18) |
| Unknown | 44 (2.4) | 43 (97.7) | 1 (2.3) | – | – |
| Supervisor recommendation vaccination | |||||
| No | 969 (53.7) | 761 (78.5) | 208 (21.5) | Ref | Ref |
| Yes | 793 (44.0) | 609 (76.8) | 184 (23.2) | 1.10 (0.88, 1.37) | 1.11 (0.89, 1.39) |
| Unknown | 41 (2.3) | 41 (100.0) | 0 (0.0) | – | – |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; cOR, crude odds ratio; HCP, healthcare personnel.
Perceived influenza susceptibility: If you are unable to or don’t get an influenza vaccination, what do you think your chance of getting the flu this season will be?
Perceived vaccine effectiveness: How effective do you think the influenza vaccine is in preventing you from getting sick with influenza?
Knowledge of influenza and vaccine was a composite of three questions: (i) Agree or disagree with the following statement: People with influenza can transmit the virus only after their symptoms appear; (ii) Agree or disagree with the following statement: The influenza vaccine could give me influenza; and (iii) Agree or disagree with the following statement: People can spread influenza virus even when they are feeling well.
Concerns about vaccination was a composite of two questions: (i) Agree or disagree with the following statement: Influenza vaccination is safe; and (ii) Agree or disagree with the following statement: The influenza shot is painful.
Emotional benefits of vaccination were a composite of two questions: (i) Agree or disagree with the following statement: If I don’t get an influenza vaccination and end up getting sick with influenza, I’d be mad at myself for not getting the vaccine; and (ii) Agree or disagree with the following statement: If I don’t get an influenza vaccination, I will regret it.
Barriers to vaccination was a composite of two questions: (i) Agree or disagree with the following statement: I usually do not have time to get vaccinated with the influenza vaccine; and (ii) Agree or disagree with the following statement: There is not a convenient place for me to get vaccinated with the influenza vaccine.
Supervisor recommendation vaccination: Agree or disagree with the following statement: A supervisor or other leader at my workplace has recommended that I get an annual influenza vaccination.
* Collected each survey year in the start of season survey. Perceived vaccination protection for self and patient were excluded because they were only captured at enrollment.
Only people classified as infrequently vaccinated (vaccinated self-reported receiving 1─4 influenza vaccinations from 2011 to 2018) and surveyed all three years from 2016 to 2018 (with multiple observations per person, n = 601 people) are included in this analysis.
Adjusted for HCP hospital of employment, age, sex, preexisting medical condition, occupation, and providing patient care for > 10 years.
Discussion
Despite vaccines being offered for free to HCP in the workplace, few HCP in Peru frequently received influenza vaccines during the eight study years. HCP received influenza vaccines more often if they believed the vaccine was effective, had knowledge of influenza vaccines, believed vaccination had emotional benefits like reduced anger and regret, recalled supervisor recommendation of vaccination, or perceived that the vaccine protected them or their patients from illness. Conversely, HCP who reported insufficient time to get vaccinated or vaccine safety concerns had reduced odds of frequent vaccination. To increase HCP influenza vaccination in middle-income settings like Peru, it may be helpful to enhance vaccination education, communication, and campaigns in the workplace.
Overall, about 60% of HCP infrequently received influenza vaccines over an eight-year period; this population with low influenza vaccine uptake was primarily physicians and HCP who worked in an outpatient setting. Similar trends in low influenza vaccination coverage have been seen among HCP in KAP studies in Honduras [17], Costa Rica [18], Egypt [19], and parts of the Middle East [20]. This low coverage was also seen in the general HCP population recruited into this study but excluded from analysis. HCP groups who infrequently receive influenza vaccines could be targeted for campaigns to increase national HCP vaccination uptake.
Low vaccination coverage among HCP could be due to HCP having low risk perception of the disease and of the vaccine protecting them and their patients from influenza infection; we found HCP who perceived vaccination protected against infection had higher odds of frequent vaccination, as has been previously observed in the U.S. and literature reviews [21], [22], [23]. Additionally, similar to findings in a previous study, those who believed vaccination had emotional benefits like reduced anger or regret if they contracted influenza were more likely to be frequently vaccinated [13]. To illustrate how influenza vaccination could reduce anxiety at a time when there is heightened concern about acquiring respiratory illness in hospitals, healthcare-focused vaccine advertising could highlight the perceived emotional benefits and protection of vaccination.
Improvement in influenza vaccination perceptions could also occur by increasing vaccine education and supervisor recommendation in the workplace. We found that 18% of HCP surveyed reported lacking some basic knowledge of influenza and its vaccine, 75% did not believe they were susceptible to influenza, 43% had concerns about vaccination, and 48% did not recall their supervisor recommending influenza vaccination to them. These gaps in influenza vaccine knowledge and trust among healthcare personnel have also been reported in Peru and other countries [19], [24], [25], [26], [27]. Healthcare facilities could improve influenza vaccine education by providing continuing medical education credits for courses focused on influenza prevention and treatment. These courses could reduce misconceptions of influenza and vaccination and increase knowledge about its safety and benefits. Supervisors could further increase uptake by indicating their support of the educational campaigns and vaccination.
About a quarter of HCP switched their influenza vaccination status each year, which seemed associated with differences in vaccine brands offered and perceptions of product-specific effectiveness. We found that people were 2.7 times as likely to get vaccinated when the Vaxigrip vaccine was offered compared to when the GC FLU vaccine was offered. This trend was consistent across occupations with all occupational groups increasing vaccine uptake compared to the previous year when the Vaxigrip vaccine was offered in 2018. Vaxigrip is produced by Sanofi, whereas GC Flu is produced by GC Biopharma Corporation. An association between vaccine brand preference and acceptance has also been observed in the context of Coronavirus Disease 2019 (COVID-19) vaccination [28], but to our knowledge, this association has only been documented for influenza vaccine type [29], not brand. Distributing informational materials that create trust across brands at vaccination clinics could increase acceptance of the influenza vaccine available each year to HCP in Peru.
To increase vaccination uptake, hospitals could decrease barriers to vaccination by increasing availability of convenient times or places to receive vaccines. Lack of time to receive a vaccine was repeatedly reported as a barrier to vaccination in prior KAP studies in similar settings [17], [18], [20] and was found to be the main driver for infrequent vaccination among people reporting barriers to vaccination. Currently in Peru, influenza vaccination for HCP is not mandated by employers and campaigns vary by location; some hospitals coordinate cars to bring vaccines to HCP locations, while others offer drop-in vaccination at hospitals. Some locations also prioritize groups they deem high priority for exposure in the hospital, such as HCP working in intensive care units, emergency departments, and pediatrics. Strategies that could be employed to improve these campaigns include offering more frequent vaccination clinics and mobile vaccination carts at personnel’s places of employment as well as having vaccinations available during work hours, evenings, and weekends. Vaccination uptake could also be improved by offering workplace incentives for receiving vaccines, such as financial rewards or competitions [30]. Alternatively, annual vaccination could be mandated by employers and disincentives adopted for those that remain unvaccinated, such as requiring declination forms and mask use in clinics [31], [32]; requiring vaccination has increased coverage in the U.S., with employers that require influenza vaccination reporting up to 95% vaccine uptake in HCP [30].
This study had limitations. Demographic and occupational factors were only reported for participants at enrollment and may have changed during annual surveys. KAP responses could have been subject to social desirability bias. Vaccination status was sometimes self-reported, which could be unreliable; however, self-reporting was not the sole source of vaccination status and typically aligned with medical records [33]. People who received the current season’s influenza vaccine prior to enrollment were not enrolled in VIP, which may have biased the study population to include people who were less likely to receive influenza vaccines; however, we believe this bias was minimal since vaccination coverage among the total number of participants recruited for the study was overall low (Supplemental Table 2). The study only included HCP who provided direct patient care, excluding non-clinical healthcare personnel.
Conclusions
In summary, we found that influenza vaccination among HCP in Peru was low and inconsistent during eight years with less than two percent of HCP getting vaccinated every year despite free access to vaccines in the workplace. This low vaccine uptake could be due to insufficient education about the benefits, effectiveness, and safety of influenza vaccination and insufficient supervisor recommendation for vaccination. These findings add to the limited literature on HCP influenza vaccination practices in middle-income countries. To increase HCP influenza coverage, campaigns could enhance vaccination education and accessibility.
Funding
This work was funded by the U.S. Centers for Disease Control and Prevention (CDC) through contract HHSD2002013M53890B (Achieving Public Health Impact through Research; task 200–2014-F-60406: “The Epidemiology and Prevention of Influenza Virus Infections in Low- and Middle-Income Countries”) to Abt Associates. The study was also funded through CDC Interagency Agreements 16FED1612328, 17FED1712076, 18FED1812054IPD and 19FED1916949IPD to Naval Medical Research Unit 6 (NAMRU6).
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the U.S. Centers for Disease Control and Prevention (CDC), the Department of the Navy, Department of Defense, nor the U.S. Government and the Pan American Health Organization (PAHO). Some authors are federal employees of the United States government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that copyright protection under this title is not available for any work of the United States Government.' Title 17 U.S.C. 101 defines a U.S. Government work as work prepared by a military service member or employee of the U.S. Government as part of that person's official duties.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Abt Associates reports financial support was provided by CDC contract HHSD2002013M53890B. Naval Medical Research Unit 6 (NAMRU6) reports financial support was provided by CDC Interagency Agreements 16FED1612328, 17FED1712076, 18FED1812054IPD and 19FED1916949IPD.
Acknowledgment
We would like to acknowledge the study participants and field teams at participating hospitals in Lima, Peru. We thank our collaborators Gabriella Newes-Adeyi, Angela Cheung, and Rachel Phadnis at Abt Associates for their contributions to the study. We appreciate Dr. Ticona for their work with study implementation at the Dos de Mayo National Hospital, the immunization programs from the participant hospitals, and Miriam Gonzales for supporting field activities. We also thank our CDC clearance reviewers Alicia Fry and Mike Jhung and Nia Mimms at CDC for managing the interagency agreement with the U.S. Navy.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jvacx.2023.100314.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- 1.Tinoco Y.O., Azziz-Baumgartner E., Uyeki T.M., Razuri H.R., Kasper M.R., Romero C., et al. Burden of Influenza in 4 Ecologically Distinct Regions of Peru: Household Active Surveillance of a Community Cohort, 2009–2015. Clin Infect Dis. 2017;65:1532–1541. doi: 10.1093/cid/cix565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheng P.Y., Palekar R., Azziz-Baumgartner E., Iuliano D., Alencar A.P., Bresee J., et al. Burden of influenza-associated deaths in the Americas, 2002–2008. Influenza Other Respir Viruses. 2015;9(Suppl 1):13–21. doi: 10.1111/irv.12317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palekar R.S., Rolfes M.A., Arriola C.S., Acosta B.O., Guidos P.A., Vargas X.B., et al. Burden of influenza-associated respiratory hospitalizations in the Americas, 2010–2015. PLoS One. 2019;14:e0221479. doi: 10.1371/journal.pone.0221479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tinoco Y.O., Azziz-Baumgartner E., Razuri H., Kasper M.R., Romero C., Ortiz E., et al. A population-based estimate of the economic burden of influenza in Peru, 2009–2010. Influenza Other Respir Viruses. 2016;10:301–309. doi: 10.1111/irv.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ropero Alvarez A.M., Jane Kurtis H., Vulanovic L., Hasan H., Ruiz C., Thrush E. The evolution of Vaccination Week in the Americas. Rev Panam Salud Publica. 2017;41:e150. doi: 10.26633/RPSP.2017.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reinders S., Romero C., Carcamo C., Tinoco Y., Valderrama M., La Rosa S., et al. A community-based survey on influenza and vaccination knowledge, perceptions and practices in Peru. Vaccine. 2020;38:1194–1201. doi: 10.1016/j.vaccine.2019.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Arriola CS, Vasconez N, Bresee J, Ministry of Civic Power for Health of N, Ropero AM. Knowledge, attitudes and practices about influenza vaccination among pregnant women and healthcare providers serving pregnant women in Managua, Nicaragua. Vaccine 2018; 36: 3686–93. [DOI] [PMC free article] [PubMed]
- 8.Thompson M.G., Soto G., Peretz A., Newes-Adeyi G., Yoo Y.M., Hirsch A., et al. Influenza vaccine effectiveness within prospective cohorts of healthcare personnel in Israel and Peru 2016–2019. Vaccine. 2021;39:6956–6967. doi: 10.1016/j.vaccine.2021.07.077. [DOI] [PubMed] [Google Scholar]
- 9.Cherian T, Morales KF, Mantel C, Lambach P, Independent Expert Advisory Group for Health Worker Influenza V. Factors and considerations for establishing and improving seasonal influenza vaccination of health workers: Report from a WHO meeting, January 16-17, Berlin, Germany. Vaccine 2019; 37: 6255–61. [DOI] [PMC free article] [PubMed]
- 10.Wesley M.G., Soto G., Arriola C.S., Gonzales M., Newes-Adeyi G., Romero C., et al. Prospective cohort study of influenza vaccine effectiveness among healthcare personnel in Lima, Peru: Estudio Vacuna de Influenza Peru, 2016–2018. Influenza Other Respir Viruses. 2020;14:391–402. doi: 10.1111/irv.12737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Durand L.O., Cheng P.Y., Palekar R., Clara W., Jara J., Cerpa M., et al. Timing of influenza epidemics and vaccines in the American tropics, 2002–2008, 2011–2014. Influenza Other Respir Viruses. 2016;10:170–175. doi: 10.1111/irv.12371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McLean H.Q., Thompson M.G., Sundaram M.E., Meece J.K., McClure D.L., Friedrich T.C., et al. Impact of repeated vaccination on vaccine effectiveness against influenza A(H3N2) and B during 8 seasons. Clin Infect Dis. 2014;59:1375–1385. doi: 10.1093/cid/ciu680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson M.G., Gaglani M.J., Naleway A., Ball S., Henkle E.M., Sokolow L.Z., et al. The expected emotional benefits of influenza vaccination strongly affect pre-season intentions and subsequent vaccination among healthcare personnel. Vaccine. 2012;30:3557–3565. doi: 10.1016/j.vaccine.2012.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.R Development Core Team . 4.0.4 ed. R Foundation for Statistical Computing; Vienna, Austria: 2021. R: A language and environment for statistical computing. [Google Scholar]
- 15.Wickham H., Averick M., Bryan J., Chang W., McGowan L., François R., et al. Welcome to the Tidyverse. J Open Source Software. 2019:4. [Google Scholar]
- 16.Højsgaard S., Halekoh U., Yan J. The R Package geepack for Generalized Estimating Equations. J Stat Softw. 2006;15:11. [Google Scholar]
- 17.Madewell Z.J., Chacon-Fuentes R., Jara J., Mejia-Santos H., Molina I.B., Alvis-Estrada J.P., et al. Knowledge, attitudes, and practices of seasonal influenza vaccination in healthcare workers. Honduras PLoS One. 2021;16:e0246379. doi: 10.1371/journal.pone.0246379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madewell Z., Chacon-Fuentes R., Badilla-Vargas X., Ramirez C., Ortiz M.R., Alvis-Estrada J.P., et al. Knowledge, attitudes, and practices for the use of seasonal influenza vaccination, healthcare workers. Costa Rica J Infect Dev Ctries. 2021;15:1004–1013. doi: 10.3855/jidc.14381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hakim S.A., Amin W., Allam M.F., Fathy A.M., Mohsen A. Attitudes, beliefs and practice of Egyptian healthcare workers towards seasonal influenza vaccination. Influenza Other Respir Viruses. 2021;15:778–788. doi: 10.1111/irv.12868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abu-Gharbieh E., Fahmy S., Rasool B.A., Khan S. Influenza vaccination: Healthcare workers attitude in three middle east countries. Int J Med Sci. 2010;7:319–325. doi: 10.7150/ijms.7.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naleway A.L., Henkle E.M., Ball S., Bozeman S., Gaglani M.J., Kennedy E.D., et al. Barriers and facilitators to influenza vaccination and vaccine coverage in a cohort of health care personnel. Am J Infect Control. 2014;42:371–375. doi: 10.1016/j.ajic.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Hofmann F., Ferracin C., Marsh G., Dumas R. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection. 2006;34:142–147. doi: 10.1007/s15010-006-5109-5. [DOI] [PubMed] [Google Scholar]
- 23.Hollmeyer H.G., Hayden F., Poland G., Buchholz U. Influenza vaccination of health care workers in hospitals–a review of studies on attitudes and predictors. Vaccine. 2009;27:3935–3944. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 24.Berg T.T., Wicker S. Knowledge, attitude and behavior towards vaccinations among nursing- and health care students in Hesse. An observational study. GMS J Med Educ. 2021:38. doi: 10.3205/zma001511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vora A., Shaikh A. Awareness, Attitude, and Current Practices Toward Influenza Vaccination Among Physicians in India: A Multicenter. Cross-Sectional Study Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.642636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andayi F., Emukule G.O., Osoro E., Ndegwa L.K., Otiato F., Muturi P., et al. Knowledge and attitude of Kenyan healthcare workers towards pandemic influenza disease and vaccination: 9 years after the last influenza pandemic. Vaccine. 2021;39:3991–3996. doi: 10.1016/j.vaccine.2021.05.057. [DOI] [PubMed] [Google Scholar]
- 27.Garcia P.J., George P.E., Romero C., Soto G., Carcamo C., Bayer A.M. “The flu... is a little more complicated than a cold”: Knowledge, beliefs, and practices related to influenza and influenza vaccination among at-risk populations and health professionals in Peru. Vaccine. 2020;38:7688–7695. doi: 10.1016/j.vaccine.2020.09.065. [DOI] [PubMed] [Google Scholar]
- 28.Wang K., Wong E.L., Cheung A.W., Yau P.S., Chung V.C., Wong C.H., et al. Influence of Vaccination Characteristics on COVID-19 Vaccine Acceptance Among Working-Age People in Hong Kong, China: A Discrete Choice Experiment. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.793533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nowalk M.P., Lin C.J., Toback S.L., Rousculp M.D., Eby C., Raymund M., et al. Improving influenza vaccination rates in the workplace: a randomized trial. Am J Prev Med. 2010;38:237–246. doi: 10.1016/j.amepre.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 30.Black C., Yue X., Ball S.W., Fink R.V., de Perio M.A., Laney A.S., et al. Influenza vaccination coverage among health care personnel - United States, 2017–18 influenza season. Morb Mortal Wkly Rep. 2018;67:1050–1054. doi: 10.15585/mmwr.mm6738a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haviari S., Benet T., Saadatian-Elahi M., Andre P., Loulergue P., Vanhems P. Vaccination of healthcare workers: A review. Hum Vaccin Immunother. 2015;11:2522–2537. doi: 10.1080/21645515.2015.1082014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hollmeyer H., Hayden F., Mounts A., Buchholz U. Review: interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir Viruses. 2013;7:604–621. doi: 10.1111/irv.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Regan A.K., Wesley M.G., Gaglani M., Kim S.S., Edwards L.J., Murthy K., et al. Consistency of self-reported and documented historical influenza vaccination status of US healthcare workers. Influenza Other Respir Viruses. 2022 doi: 10.1111/irv.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.