Abstract
INTRODUCTION:
Severe traumatic injury with shock can lead to direct and indirect organ injury, however, tissue-specific biomarkers are limited in clinical panels. We utilized proteomic and metabolomic databases to identify organ injury patterns after severe injury in humans.
METHODS:
Plasma samples (times 0-, 24-, and 72-hours [h] after arrival to trauma center) from injured patients enrolled in two randomized prehospital trials were subjected to multiplexed proteomics (SomaLogic Inc.). Patients were categorized by outcome: Non-resolvers (died >72h or required ≥7 days of critical care), Resolvers (survived to 30-days and required <7 days of critical care), and low injury severity score (ISS) controls. Established tissue-specific biomarkers were identified through a literature review and cross-referenced with tissue-specificity from the Human Protein Atlas. Untargeted plasma metabolomics (Metabolon Inc.), inflammatory mediators, and endothelial damage markers were correlated with injury biomarkers. Kruskal-Wallis/Mann-Whitney-U tests with false discovery rate correction assessed differences in biomarker expression across outcome groups (significance; P-value <0.1).
RESULTS:
Of 142 patients, 78 were Non-resolvers (median ISS=30), 34 Resolvers (median ISS=22), and 30 low ISS controls (median ISS=1). A broad release of tissue-specific damage markers was observed at admission; this was greater in Non-resolvers. By 72h, 9 cardiac, 3 liver, 8 neurologic, and 3 pulmonary proteins remained significantly elevated in Non-resolvers compared to Resolvers. Cardiac damage biomarkers showed the greatest elevations at 72h in Non-resolvers and had significant positive correlations with pro-inflammatory mediators and endothelial damage markers. Non-resolvers had lower concentrations of fatty acid metabolites compared to Resolvers, particularly acyl carnitines and cholines.
CONCLUSIONS:
We identified an immediate release of tissue-specific biomarkers with sustained elevation in the liver, pulmonary, neurologic, and especially cardiac injury biomarkers in patients with complex clinical courses after severe injury. The persistent myocardial injury in Non-resolvers may be due to a combination of factors including metabolic stress, inflammation, and endotheliopathy.
STUDY TYPE:
Level III, Prognostic/Epidemiological
Keywords: biomarkers, trauma, organ injury
INTRODUCTION
Traumatic injury is a leading cause of death and is associated with significant morbidity.(1, 2) With the advancement of optimal resuscitation strategies, more severely injured patients survive the initial insult of injury but are often prone to organ failure and hospitalizations requiring prolonged critical care. A recent multi-omic analysis demonstrated an early “Systemic Storm” pattern of broad increases in circulating proteins, metabolites, and endothelial damage markers following severe trauma that varied by patient outcome.(3) These findings also corroborated previously described early activation of the coagulation and complement cascades, neuroendocrine stress responses, and evidence of endotheliopathy in severely injured humans.(4–8) Based on these studies it is now accepted that the host response to injury can be associated with divergent outcomes, even in similarly injured humans.(3, 9–11)
Severe injury with shock can lead to both direct and indirect organ injury and dysfunction. Recent reports indicate that ongoing cardiac injury is an underappreciated feature in patients who remain critically ill after injury.(12–15), However, the longitudinal assessment of tissue-specific damage biomarkers in severely injured humans has been limited to the evaluation of a small number of molecules.(16) Multi-omics applied to longitudinal blood samples from trauma patients offers the opportunity to characterize tissue-specific injury biomarker patterns more broadly and assess the association of these patterns with patient outcomes.
The present study utilized high-dimensional proteomic and metabolomic datasets derived from blood samples of severely injured humans to identify organ injury patterns. We provide a hierarchy of organ injury markers that change over time and correlate these changes with outcomes and markers of cellular metabolism.
METHODS
The primary analysis was performed on representative plasma samples from patients enrolled in the Prehospital Air Medical Plasma (PAMPer) trial with key findings externally validated in the Study of Tranexamic Acid During Air and Ground Medical Prehospital Transport (STAAMP) trial. Both trials were prospective, multicenter, double-blind randomized control trials examining the effect of prehospital thawed plasma (PAMPer) or tranexamic acid (STAAMP) compared to standard-of-care in patients at risk for hemorrhage after injury (at least one episode of hypotension [SBP<90 mmHg] and tachycardia [HR>108 beats per min] or any episode of severe hypotension [SBP<70 mmHg; PAMPer]; at least one episode of hypotension [SBP ≤ 90 mmHg] or tachycardia [HR ≥ 110 beats per min; STAAMP]). Detailed study protocols are publicly available.(17, 18) The primary trials were approved by the US Food and Drug Administration, Human Research Protection Offices of the US Department of Defense, and the institutional review boards of the participating sites.(17, 18) The current analysis is a secondary analysis of these published datasets with de-identified patient information.
Citrated and EDTA plasma samples for patients enrolled in both trials were collected at the time of arrival to definitive trauma care (timepoint 0-hours [h]), and at 24h and 72h after admission and stored in a −80 °C freezer. Representative citrated samples with at least 30 samples per subgroup (PAMPer, N=112, all timepoints; STAAMP, N=188, 0- and 24h) were subjected to multiplexed proteomic analysis using the SomaScan assay (SomaLogic Inc, Colorado, USA) to achieve a statistical power of at least 0.8.(19) This proteomic platform technology and performance characteristics have previously been described, but briefly utilizes DNA-based binding reagents (aptamers) to quantify relative circulating binding epitopes availability for over 7000 proteins. In the case of duplicate proteins inherent in the assay due to multiple SOMAmer reagent targets, both protein targets were examined and labeled “protein name_1 or 2” to differentiate the targets.(3, 20, 21)
Details for the measurement of untargeted metabolomics have previously been reported.(21) Briefly, a representative subset of EDTA plasma samples from the PAMPer trial (N=145) were subjected to an untargeted metabolomics assay for 898 metabolites (liquid chromatography mass spectrometry; Metabolon Inc. Durham, NC, US). Raw data was peak-identified and underwent quality control processing using Metabolon’s internal software and library of available purified standard compounds to provide information on the relative levels of measured metabolites.
Lastly, we examined the endothelial damage markers syndecan-1, thrombomodulin, and sVEGFR1 from a representative subset of the PAMPer trial (N=112, Timepoint 0h; N=103, Timepoint 24h). Commercially available immunoassays were used to quantify endothelial damage marker measurements as previously described.(7, 22)
The patients were categorized into outcome groups using clinical data from the primary trials. Patients that died within 72h of injury were excluded from this analysis. The remaining patients were classified as Non-resolvers (died >72h or required ≥7 days of critical care) or Resolvers (survived to 30-days and required <7 days of critical care). For proteomic comparisons, admission (timepoint 0h) plasma samples from a minimally injured cohort (median ISS average of 1; N=30) in the standard care arm of the STAAMP trial were utilized as a control group. Age and sex-matched non-fasting healthy volunteers (N=17) were analyzed with metabolomic samples and served as a control group for metabolomic comparisons.(23)
Established tissue damage biomarkers for the cardiac, renal, neurologic, hepatic, and pulmonary systems were identified through a literature review and were cross-referenced with tissue-specific proteomes and transcriptomes from the Human Protein Atlas. Proteins with tissue-specific enrichment (≥4X expression compared to any other tissue) or elevation (≥4X expression compared to the average of all other tissues) in respective organs were analyzed.(24)
Raw proteomic data underwent quality analysis and normalization using multiple hybridization and calibration scale factors. Raw peak intensity data from the untargeted metabolomics layer was normalized based on the run-day blocks for each metabolite by a median normalization to equal 1. The normalized data in each layer were log2 transformed to approximate a normal distribution. For heatmap visualization, transformed values were auto-scaled as a z-score across each sample.
Non-parametric Kruskal-Wallis and Mann-Whitney-U tests with false discovery rate correction assessed differences in protein expression across outcome groups (corrected level of significance; P-value <0.1). Correlations between biomarkers were evaluated using Spearman’s Rank-Order correlation. Heatmaps and line/box plots of proteins and metabolites of interest were used for data visualization. For pre-processing of metabolomic features, volcano plots of log-fold changes between outcome groups and adjusted p-values at 24 and 72h were used to select the most discriminatory metabolomic features between outcome groups. The log-2-fold change in concentration of metabolites between 24 and 72h was also assessed to identify metabolites with diverging trajectories between outcome groups (Supplemental Figure 1). Statistical analysis was performed using R Version 4.1.2.(25) A Spearman’s correlation network that included 0h values of cardiac and endothelial injury markers as well as fatty acid metabolite levels was generated using scipy and networkx libraries of Python programming language v3.10.(26) This study utilized and followed the STARD guideline to ensure proper reporting (Supplemental Digital Content).
RESULTS
The primary analysis was performed on a representative cohort of the PAMPer trial and key findings were externally validated using a representative cohort from the STAAMP trial. Both cohorts were comprised of mostly blunt injury (87% [PAMPer], 81% [STAAMP], P 0.22), however PAMPer patients were more severely injured than STAAMP patients with higher median injury severity scores (ISS; 27 vs. 14, P<0.01), shock index (1.5 vs. 1.1, P<0.01), rates of traumatic brain injury (TBI; 57% vs. 25%, P<0.01), ICU length of stay (9 vs. 3, P<0.01), and 30-day mortality (21% vs. 3%, P<0.01).
Patient and injury characteristics stratified by outcome group are summarized in Table 1. In the PAMPer cohort, Non-resolvers were more frequently Black (12% vs. 0%, P=0.04), Non-Hispanic (96% vs. 82%, P=0.04), injured by blunt mechanism (91% vs. 76%, P=0.04), and were more severely injured (ISS; 30 vs. 22, P<0.01) with higher rates of TBI (65% vs. 38%, P<0.01) compared to Resolvers. Non-resolvers also had worse outcomes compared to Resolvers in the PAMPer trial (31% vs. 0% 30-day mortality, P<0.01; ICU length of stay 13 vs. 3 days, P<0.01). Injury and outcome characteristics between Non-resolvers and Resolvers in the STAAMP cohort mirrored those of the PAMPer cohort with higher rates of blunt injury mechanism (89% vs. 76%, P=0.02), TBI (51% vs. 14%, P<0.01), higher ISS (27 vs. 10, P<0.01), 30-day mortality (3% vs. 0%, P=0.06), and ICU length of stay (11 vs. 2 days, P<0.01) in the Non-resolvers.
Table 1.
Patient and Injury Characteristics of Representative Samples from PAMPer and STAAMP Cohorts Subjected to Proteomic Analysis Stratified by Outcome Group
| PAMPer | STAAMP | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Characteristic | Non-resolving (N=78) | Resolving (N=34) | P * | Low Injury Severity Score Controls (N=30) |
Non-resolving (N=37) | Resolving (N=121) | P * |
| Age, median (IQR) | 42 (26, 66) | 48 (28, 63) | 0.79 | 32 (25, 47) | 48 (31, 59) | 33 (23, 49) | 0.002 |
| Male sex, N (%) | 58 (74) | 25 (74) | 0.93 | 21 (70) | 31 (834) | 92 (76) | 0.32 |
| Race, N (%) | 0.005 | 0.25 | |||||
| White | 68 (87) | 29 (85) | 26 (87) | 33 (89) | 89 (74) | ||
| Black | 9 (12) | 0 (0) | 2 (7) | 2 (5) | 14 (12) | ||
| Other | 0 (0) | 3 (9) | 0 (0) | 0 (0) | 2 (2) | ||
| Unknown | 1 (1) | 2 (6) | 2 (7) | 2 (5) | 16 (13) | ||
| Ethnicity, N (%) | 0.04 | 0.14 | |||||
| Hispanic | 1 (1) | 1 (3) | 1 (3) | 4 (11) | 6 (5) | ||
| Non-Hispanic | 75 (96) | 28 (82) | 26 (87) | 31 (84) | 96 (79) | ||
| Unknown | 2 (3) | 5 (15) | 3 (10) | 2 (5) | 19 (16) | ||
| Injury Mechanism, N (%) | 0.04 | 0.02 | |||||
| Blunt | 71 (91) | 26 (76) | 27 (90) | 33 (89) | 92 (76) | ||
| Penetrating | 7 (9) | 8 (24) | 3 (10) | 2 (5) | 28 (23) | ||
| Both blunt and penetrating | 0 (0) | 0 (0) | 2 (5) | 1 (1) | |||
| Initial Glasgow Coma Scale, median (IQR) | 3 (3, 12) | 14 (8, 15) | <0.001 | 15 (12, 15) | 9 (3, 15) | 15 (11, 15) | <0.001 |
| Initial Glasgow Coma Scale <8, N (%) | <0.001 | <0.001 | |||||
| Yes | 51 (65) | 9 (26) | 7 (23) | 17 (46) | 23 (19) | ||
| No | 27 (35) | 25 (74) | 23 (77) | 20 (54) | 98 (81) | ||
| Traumatic Brain Injury, N (%) | 0.007 | ||||||
| Yes | 51 (65) | 13 (38) | 2 (7) | 19 (51) | 17 (14) | <0.001 | |
| No | 27 (35) | 21 (62) | 28 (93) | 16 (43) | 104 (86) | ||
| Missing | 0 (0) | 0 (0) | 0 (0) | 2 (5) | 0 (0.0) | ||
| Prehospital Systolic Blood Pressure, median (IQR), mmHg | 72 (65, 81) | 79 (64, 84) | 0.37 | 144.5 (125, 156) | 76 (70, 85) | 114 (90, 130) | <0.001 |
| Prehospital Heart Rate, median (IQR) | 121 (109, 128) | 117 (109.5, 125.5) | 0.42 | 117 (112, 121) | 119 (105, 145) | 120 (112, 130) | 0.88 |
| Prehospital Intubation, N (%) | 0.001 | <0.001 | |||||
| Yes | 51 (65) | 11 (32) | 6 (20) | 21 (57) | 20 (17) | ||
| No | 27 (35) | 23 (68) | 24 (80) | 16 (43) | 101 (84) | ||
| Prehospital CPR, N (%) | 0.35 | 0.07 | |||||
| Yes | 2 (3) | 0 (0) | 1 (3) | 1 (3) | 0 (0) | 0.07 | |
| No | 76 (97) | 34 (100) | 29 (97) | 36 (97) | 121 (100) | ||
| Prehospital packed red blood cell transfusion, N (%) | 0.66 | 0.4 | |||||
| Yes | 22 (28) | 11 (32) | 0 (0) | 3 (8) | 16 (13) | ||
| No | 56 (72) | 23 (68) | 30 (100) | 34 (92) | 105 (87) | ||
| Prehospital crystalloid volume, median (IQR), mL | 800 (0, 1400) | 775 (0, 1500) | 0.62 | 275 (0, 500) | 1000 (300, 1600) | 400 (150, 1000) | 0.004 |
| Prehospital Thawed Plasma, N (%) | 0.04 | NA | |||||
| Yes | 42 (54) | 11 (32) | NA | NA | NA | ||
| No | 36 (46) | 23 (68) | NA | NA | NA | ||
| Prehospital Tranexamic Acid (TXA), N (%) | NA | 0.5 | |||||
| TXA | NA | NA | 0 (0) | 17 (46) | 48 (40) | ||
| No TXA | NA | NA | 30 (100) | 20 (54) | 73 (60) | ||
| Tranexamic Acid (TXA) Dose, N (%) | NA | 0.01 | |||||
| Placebo | NA | NA | 30 (100) | 20 (54) | 73 (60) | ||
| 1 gram | NA | NA | 0 (0) | 6 (16) | 12 (10) | ||
| 2 grams | NA | NA | 0 (0) | 11 (30) | 17 (14) | ||
| 3 grams | NA | NA | 0 (0) | 0 (0) | 19 (16) | ||
| Injury Severity Score, median (IQR) | 30 (22, 41) | 22 (14, 24) | <0.001 | 1 (0, 1) | 27 (18, 38) | 10 (1, 17) | <0.001 |
| Head AIS Score, median (IQR) | 3 (2, 4) | 0 (0, 3) | <0.001 | 0 (0, 0) | 3 (0, 5) | 0 (0, 0) | <0.001 |
| Abdomen AIS Score, median (IQR) | 2 (0, 3) | 2 (0, 2) | 0.29 | 0 (0, 0) | 0 (0, 3) | 0 (0, 0) | <0.001 |
| Chest AIS Score, median (IQR) | 3 (2, 3) | 3 (0, 3) | 0.19 | 0 (0, 0) | 3 (2, 3) | 0 (0, 3) | <0.001 |
| External AIS Score, median (IQR) | 1 (0, 1) | 1 (0, 1) | 0.77 | 0 (0, 1) | 1 (0, 1) | 1 (0, 1) | 0.65 |
| Extremity AIS Score, median (IQR) | 2 (0, 3) | 2 (0, 3) | 0.17 | 0 (0, 0) | 2 (0, 3) | 1 (0, 3) | 0.005 |
| Face AIS Score, median (IQR) | 0 (0, 2) | 0 (0, 1) | 0.1 | 0 (0, 0) | 0 (0, 1) | 0 (0, 1) | 0.09 |
| 24-hour Mortality, N (%) | 1 | 1 | |||||
| No | 78 (100) | 34 (100) | 30 (100) | 37 (100) | 121 (100) | ||
| 30-day Mortality, N (%) | <0.001 | 0.06 | |||||
| Yes | 24 (31) | 0 (0) | 1 (3) | 1 (3) | 0 (0) | ||
| No | 54 (69) | 34 (100) | 29 (97) | 34 (92) | 121 (100) | ||
| Missing | 0 (0) | 0 (0) | 0 (0) | 2 (5) | 0 (0) | ||
| ICU Length of Stay, median (IQR), days | 13 (9, 18) | 3 (2, 5) | <0.001 | 0 (0,0) | 11 (9, 16) | 2 (0, 3) | <0.001 |
P-values comparing Non-resolvers to resolvers
Literature review and cross reference with The Human Protein Atlas (24) identified 41 tissue-specific damage biomarkers (8 cardiac, 6 renal, 16 neurologic, 7 hepatic, 4 pulmonary) represented in the SomaScan 7K proteomic platform. The analyzed biomarkers are listed according to tissue-specificity, organ system, and protein function in Supplemental Table 1.
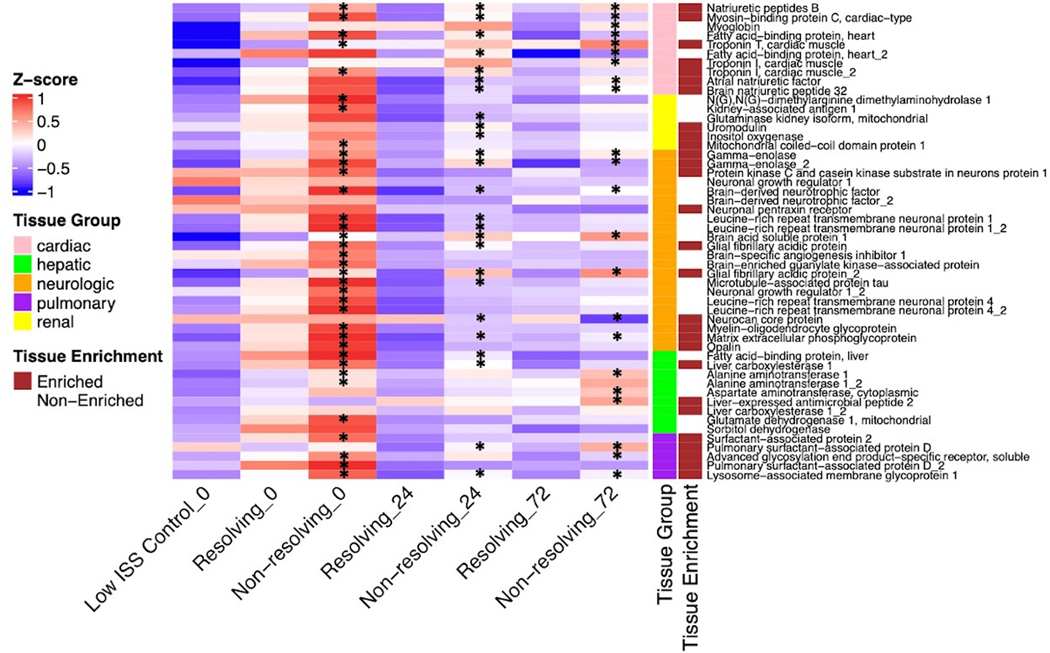
We first visualized the relative plasma levels of the 41 biomarkers across outcome groups and time in a heatmap of normalized Z-scores (Figure 1). We also examined these biomarkers across injury severity groups (Mild [ISS≤15], Moderate [ISS 16–24], Severe [ISS>25]). This identified an early (timepoint 0h) outcome and injury severity-based near-indiscriminate release of the analyzed biomarkers. Interestingly, the release of these circulating biomarkers was largely reversed in all outcome and injury severity-based groups by 24h. However, at the 72h timepoint, Non-resolvers demonstrated a sustained relatively higher level of these biomarkers across all organs except the renal system. Importantly, the sustained relative elevations of these biomarkers across outcome groups at 72h were not significantly associated with injury severity (Figure 1, Supplemental Figure 2). Further, these biomarker patterns were independent of the treatment arm in the PAMPer trial as there were no significant differences in biomarker concentrations between standard care and plasma arms except heart fatty acid binding protein_2 at 24h. Examination of these biomarkers in the STAAMP cohort confirmed the broad elevation at timepoint 0h among Resolvers and Non-resolvers. Similar to the PAMPer cohort, Resolvers demonstrated near complete resolution of the elevation of these biomarkers whereas Non-resolvers had ongoing increases in all organ group biomarkers except the renal system at timepoint 24h.
Figure 1.
Heatmap of Tissue-Specific Biomarkers Stratified by Timepoint and Outcome in PAMPer Cohort
Number of subjects in each group: 30 Low injury severity score (ISS) controls, 34 (Resolving 0h), 78 (Non-resolving 0h), 32 (Resolving 24h), 72 (Non-resolving 24h), 32 (Resolving 72h), 71 (Non-resolving 72h).
* Represents significant elevation with adjusted p-value <0.1 across outcome groups
Given the significant differences in demographics and injury mechanisms between outcome groups, we explored differences in biomarker concentrations across sex, race, prehospital shock, TBI, and injury mechanism. Interestingly, there were no significant differences in biomarker concentrations across sex (N=83 [Male], N=29 [Female]) and shock (any SBP<70 mmHg prior to arrival to trauma center; N=73 [shock], N=39 [no shock]) at all timepoints. When we compared patients with TBI (N=64) to patients without TBI (N=48), there were significant differences in 18 neurologic, 9 cardiac, 7 hepatic, 5 pulmonary, and 5 renal biomarker concentrations at timepoint 0h. However, by 72h there were only significant differences in concentrations of 5 neurologic, 1 cardiac, and 1 pulmonary protein. Similarly, patients who suffered blunt (N=97) compared to penetrating (N=15) injury mechanism demonstrated significant differences in 22 neurologic, 8 cardiac, 7 hepatic, 4 pulmonary, and 6 renal protein concentrations at timepoint 0. Again, by 72h, there were only significant differences in 4 neurologic, 2 cardiac, 1 renal, and 1 pulmonary protein concentrations across injury mechanism.
While biomarkers for all tissue groups (except renal) exhibited sustained elevation among Non-resolvers compared to Resolvers at 72h, this effect was most pronounced for the cardiac biomarkers. We therefore investigated the time-dependent trends in cardiac biomarkers across outcome groups. The relative concentrations of 4 representative cardiac damage biomarkers across time are depicted in Figure 2. While the trajectory of these cardiac biomarkers over time was similar between outcome groups, the relative concentrations of these proteins were highest in Non-resolvers compared to Resolvers at all timepoints (Figure 2A). Many of the cardiac damage markers returned to within the baseline range observed in Low ISS Controls in Resolvers by 72h. In contrast, Non-resolvers demonstrated sustained elevation (above the baseline range of the Low ISS Control group) in all cardiac damage biomarkers except myosin binding protein C (cardiac type) and fatty-acid binding protein_2 at 72h (Figure 2B,C). Lastly, among the analyzed cardiac damage biomarkers, the time-dependent trend in troponin T uniquely revealed a linear increase in relative concentration over time with significant differences between outcome groups occurring only at the 72h timepoint (Figure 2D).
Figure 2.
Time-dependent Relative Concentrations of Analyzed Cardiac Damage Biomarkers Stratified by Patient Outcome
Dot and error bars represent mean and standard deviation of respective outcome groups. Black line and gray bars represent mean and standard deviation of relative protein concentration in low injury severity control group at timepoint 0-hours.
* Signifies significant difference in relative concentration between resolving and non-resolving after false discovery rate correction. Number of subjects the same as Figure 1.
To assess the effect of direct chest injury on cardiac injury biomarkers, we compared cardiac damage biomarkers in patients with at least moderate chest injury (chest abbreviated injury score [AIS] > 2) to those with mild to no chest injury (chest ≤ AIS 2). This demonstrated relative elevation in plasma concentrations of myoglobin (cardiac), heart fatty acid-binding protein (cardiac), pulmonary surfactant-associated protein D (pulmonary), and advanced glycosylation end product-specific soluble receptor (pulmonary) at 0h among patients with a direct chest injury. By 24h, only pulmonary surfactant-associated protein D (pulmonary) was significantly elevated among those with chest injury, and there were no significant differences in relative concentrations of these biomarkers between chest injury groups at 72h.
Lastly, to clinically correlate our outcome group findings, we examined trends in tissue-specific damage biomarkers across vasopressor use as a proxy of cardiac dysfunction. We extrapolated vasopressor use within the first 3 days of admission from Denver multiple organ scores collected in the primary PAMPer trial.(27) This demonstrated an almost exclusive elevation in cardiac damage biomarkers at 24h and elevation of all examined cardiac damage biomarkers at 72h among those on vasopressors compared to those not requiring vasopressors.
The heart typically utilizes fatty acids as an energy substrate and fatty acids are transported into the mitochondria of myocytes as acyl carnitines.(28, 29) Cardiac metabolism can shift to burn ketones and glucose in stress states.(30, 31) We evaluated the longitudinal changes in circulating metabolites known to be involved in cardiac metabolism (fatty acid [N=159], ketone [N=2], and glucose [N=6] pathway metabolites).(30) Pre-processing of these metabolomic features through volcano plots identified acyl cholines and acyl carnitines conjugated to monosaturated, polyunsaturated, and long chain saturated fatty acids as the most discriminatory features between outcome groups at 24 and 72h (Supplementary Figure 1). Visualization of these metabolites in a heatmap depicts an overall early (time 0h) loss of fatty acid metabolites among Resolvers and Non-resolvers compared to healthy controls (Figure 3). This was followed by selective increases in multiple long-chain acyl cholines and a subset of saturated long chain-, polyunsaturated-, and monounsaturated-conjugated acyl carnitines among Resolvers compared to Non-resolvers by 72h (Figure 3).
Figure 3.
Heatmap of Plasma Acyl Carnitine and Acyl Choline Fatty Acid Metabolites Stratified by Timepoint and Patient Outcome
Number of subjects in each group: 17 Healthy Controls, 43 Resolving 0h, 102 Non-resolving 0h, 42 Resolving 24h, 100 Non-resolving 24h, 43 Resolving 72h, 99 Non-resolving 72h.
The time-dependent trajectories of a representative acyl carnitine, acyl choline, and medium-chain fatty acid, as well as pyruvate are shown in Figure 4, respectively. Dihomo-linoleoylcarnitine (C20:2) demonstrated a relative decrease from 0- to 24-hours among both Resolvers and Non-resolvers, with a subsequent relative increase compared to baseline concentrations at 72h only among Resolvers (Figure 4A). In contrast, palmitoylcholine was lower compared to healthy controls at time 0h which was more pronounced in Non-resolvers compared to Resolvers (Figure 4B). The relative concentration increased in both Non-resolvers and Resolvers over time, approaching levels in healthy controls in both outcome groups by 72h. Interestingly, caprylate (8:0), a medium-chain fatty acid associated with myocardial oxidative stress (32), was much lower compared to healthy controls in both outcome groups at 0- and 24h, and increased in concentration in only Non-resolvers at 72h. (Figure 4C). Pyruvate, a systemic marker of anaerobic glucose metabolism, was elevated compared to healthy controls in both Resolvers and Non-resolvers at 0h and remained elevated at 24h in Non-resolvers (Figure 4D). Taken together, these observations show that circulating levels of cardiac energy substrates inversely correlate with ongoing cardiac myocyte injury, while markers of metabolic stress associate with cardiac injury biomarkers.
Figure 4.
Representative Time-dependent Trajectories of Acyl Carnitines, Acyl Cholines, Medium Chain Fatty Acids, and Lactate Across Outcome Groups.
Depicted trajectories are representative of metabolites in acyl carnitine (Panel A), acyl choline (Panel B), medium chain fatty acids (Panel C), and pyruvate (Panel D). Number of subjects the same as Figure 3.
We next examined the correlation between cardiac damage biomarkers and the pro-inflammatory cytokines interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha), which have been shown to modulate cardiac stress.(15, 33–35) This revealed positive correlations between both pro-inflammatory cytokines and all measured cardiac damage biomarkers across the three timepoints. Overall, cardiac damage biomarkers had stronger correlations with TNF-alpha compared to IL-6. These correlations were the most prominent at the 0h timepoint with brain natriuretic peptide 32 (Rho 0.95–0.98) and atrial natriuretic factor (Rho 0.94–0.95) demonstrating the highest correlations with TNF-alpha. Similar significant positive correlations were observed at 24h between brain natriuretic peptide 32 (Rho 0.79–0.85) and atrial natriuretic factor (Rho 0.71–0.72) with TNF-alpha. At 72h, brain natriuretic peptide 32 (Rho 0.85–0.86) remained most strongly correlated to TNF-alpha.
We also investigated the association of the endothelial damage marker syndecan-1 and cardiac damage biomarkers which demonstrated significant positive correlations for all analyzed cardiac damage biomarkers. Atrial natriuretic factor (Rho 0.58) and Brain natriuretic peptide 32 (Rho 0.57) had the strongest overall correlations with syndecan-1 at all timepoints. Lastly, we generated a Spearman’s correlation network to visualize the relationships among cardiac damage markers, fatty acid metabolites, and markers of endotheliopathy at 0h (Figure 5). Besides high correlation levels between the cardiac markers, the network highlights positive associations between several cardiac damage markers and endothelial injury (syndecan-1, thrombomodulin, and sVEGFR1). In addition to positive correlations between 3-glycerophosphatate and ANP, BNP, and cardiac fatty acid binding protein, the latter shows moderate positive correlations with several acyl carnitines.
Figure 5.
Network of highly correlated (Spearman’s coefficient >0.5) cardiac metabolites (SomaLogic), fatty acid metabolites (Metabolon) and markers of endothelipathy (ELISA) in PAMPer patients at 0h
DISCUSSION
Through a comprehensive, high-throughput plasma proteomic analysis we identified evidence of sustained elevation of tissue-specific damage biomarkers among patients with complicated clinical courses following injury. Most prominent were elevations in cardiac-specific biomarkers. These findings were externally validated in plasma samples from an additional cohort of traumatically injured patients. Further, while the release of circulating tissue-specific damage biomarkers was associated with injury severity, mechanism, and TBI at admission, by 72h after admission, elevation of cardiac-specific biomarkers was not associated with injury severity or pattern. These findings add to a body of evidence that indicates that the host response to injury significantly contributes to prognosis and outcomes following trauma.(3, 9–11)
Evidence of cardiac stress independent of direct chest injury after traumatic injury has been previously characterized as trauma-induced secondary cardiac injury (TISCI).(12–15) This phenomenon was described in a cohort of trauma patients without direct thoracic injury that experienced adverse cardiac events during initial hospitalization. Patients with TISCI demonstrated increased risk of poor outcomes including mortality. TISCI is known to be associated with increases in circulating levels of brain natriuretic peptide, heart-type fatty acid binding protein, and troponin I at 24 and 72h after admission.(12) We expand this list to include 10 cardiac biomarkers and confirm the unique pattern of troponin I as a biomarker that shows a progressive increase over time as opposed to sustained elevations for most of the other biomarkers.(12) By including injury biomarkers representative of several major organ systems, we can conclude that ongoing myocardial injury stands out in comparison to secondary injury of other organs. Our analysis indicates that cardiac stress at 72h after injury may prognosticate a complicated clinical course lasting beyond 7 days and identify patients that could benefit from cardioprotective therapy.
Given the evidence of prolonged cardiac stress in Non-resolvers, we explored potential mechanistic underpinnings including an investigation of circulating metabolites involved in cardiac metabolism. We identified an early loss of acyl carnitines conjugated to monosaturated, polysaturated and long-chain saturated fatty acids in both outcome groups with resolution to baseline healthy control concentrations among Resolvers only. Acyl carnitines assist in the transport of fatty acids into the mitochondria of myocytes for subsequent β-oxidation and derivation of cardiac energy substrates.(29, 36) The sustained loss of acyl carnitines observed in Non-resolvers in our study suggests a potential metabolic-driven mechanism to the cardiac stress identified in this outcome group. Current knowledge about cardiac metabolism after trauma is limited, but extrapolations from other cardiac stressed states such as heart failure demonstrate decreased fatty oxidation rates and reduced expression of fatty acid transporters and oxidation enzymes.(30, 31, 37, 38) Shifts in cardiac metabolism after polytrauma has been investigated in a porcine model, which showed an early shift in cardiomyocyte substrate utilization from fatty acid oxidation to glucose metabolism with subsequent increase in fatty acid transporters such as heart fatty acid binding protein at later timepoints (72h).(39) Our findings on the loss of circulating acyl cholines and acyl carnitines raise the possibility that loss of fatty acid substrates could contribute to cardiac stress after injury and create an energy crisis in the heart.
Further, the loss of several acyl cholines after injury followed by a more rapid return in Resolvers is intriguing. The biological role of these molecules is uncertain, however previous investigation supports an effect on blood pressure based on the chain length of the acyl choline molecules. (40, 41) Additionally, recent in vitro studies suggest that a subset with fatty acids ranging from 18–22 carbons in length may regulate acetylcholine signaling and hence, could regulate cardiovascular function.(42)
While we did not identify significant differences in systemic markers of glucose metabolism between outcome groups, our findings support the previous large animal work by demonstrating an increase in circulating pyruvate, a carbohydrate metabolite at timepoint 0h.(39) Lastly, our exploration of medium-chain fatty acids showed overall depletion in both outcome groups with a selective increase at later time points only among Non-resolvers. Previous investigation suggests that increased concentrations of medium-chain fatty acids correlate to myocardial oxidative stress and atrophy.(32) Taken together, the differential time-dependent trends in cardiac metabolism substrates between Resolvers and Non-resolvers suggest, at least in part, a metabolic driven mechanism for the prolonged cardiac stress observed in patients with complicated clinical courses following injury.
In addition to cardiac metabolite substrates, we investigated correlations between cardiac damage biomarkers, pro-inflammatory mediators, and markers of endotheliopathy. The association of pro-inflammatory cytokines, particularly TNF-alpha, with cardiac injury markers is consistent with the prior literature demonstrating an association of admission TNF-alpha concentrations with adverse cardiac events after trauma.(13) Additionally, TNF-alpha has been shown to initiate a signaling pathway contributing to posttraumatic myocardial apoptosis.(35) Syndecan-1 also significantly positively correlated with all cardiac damage biomarkers in our cohort, suggesting the association of endotheliopathy with cardiac stress. Endotheliopathy can be initiated early after trauma and contribute to inflammation-associated organ injury, therefore the association of syndecan-1 with cardiac injury implicates cardiac myocyte endothelium damage.(7, 43) These findings point to a correlative relationship between endotheliopathy, inflammation, and cardiac stress which in concert with our metabolomic findings suggests multi-factorial mechanisms for cardiac stress following traumatic injury.
While our study utilized high integrity multi-omic platforms from clinical trials with excellent randomization, several limitations exist. First, we identified tissue-specific damage biomarkers using a combination of literature review and cross-reference with The Human Protein Atlas. Thus, other tissue-specific damage biomarkers that were not identified in our literature review may warrant investigation and our definition of tissue-specificity is subject to the limitations of The Human Protein Atlas. Second, external validation in the STAAMP cohort was only performed at 0 and 24h for the proteomic platform and therefore proteomic findings at 72h in addition to metabolomic, inflammatory, and endothelial damage findings were not externally validated. Third, limitations in the clinical data collected in the primary randomized trials did not include adverse cardiac events or clinical tests such as Troponin-I. Fourth, there were significant differences in demographics and injury patterns between outcome groups. While we examined biomarker concentrations across these differences, further investigation with adjustment for these variables is needed to verify that are findings are independent of these baseline characteristics. Finally, our exploratory analysis only examined circulating biomarkers in plasma. Further mechanistic studies including organ tissue samples are needed to prove causality and further delineate our findings.
In conclusion, using comprehensive plasma proteomics, we identified an immediate release of biomarkers specific to multiple organs that are associated with patient outcomes following traumatic injury. Biomarkers for liver, pulmonary, neurologic, and particularly cardiac injury remained elevated in patients with complex clinical courses after severe injury. We propose that changes in circulating lipids that are associated with severe injury could contribute to ongoing cardiac stress. While further mechanistic and causal studies are needed, our findings also suggest potential prognostication with early assessment of tissue-specific damage biomarkers and support the exploration of cardio-protective therapeutic targets to improve outcomes in traumatically injured patients.
Supplementary Material
Supplemental Table 1. Analyzed Tissue-specific Biomarkers with Corresponding Tissue Specificity and Function
Supplemental Digital Content. STROBE Checklist
Supplemental Figure 2. Heatmap of Tissue-Specific Biomarkers Stratified by Timepoint and Injury Severity in PAMPer Cohort
Supplemental Figure 1. Volcano Plot Comparing Log-2-fold Change in Concentration of Cardiac Metabolites Between Resolvers and Non-Resolvers for Metabolomic Analysis Pre-processing
Acknowledgments
The University of Pittsburgh holds a Physician-Scientist Institutional Award from the Burroughs Wellcome Fund (SL, JB). We would like to acknowledge the contribution of collaborators involved in the PAMPer and STAAMP studies for clinical data collection.
Role of funders/sponsors
There was no role in the conduct, design, data collection/management and analysis, or interpretation of findings in this manuscript by funding sources. Further, there was no influence of funding sources in the preparation, review, approval and submission of this manuscript for publication.
Sources of Funding:
This work was supported by US Army Medical Research and Material Command (W81XWG-12-2-0023 to JLS), T32HL098036 from the National Heart, Lung, and Blood Institute (SL), and the National Institutes of General Medical Sciences grant R35-GM-127027 to TRB.
Footnotes
Conflict of Interest: No conflicts of interest were declared by the authors.
References
- 1.Rhee P, Joseph B, Pandit V, Aziz H, Vercruysse G, Kulvatunyou N, et al. Increasing trauma deaths in the United States. Ann Surg. 2014;260(1):13–21. [DOI] [PubMed] [Google Scholar]
- 2.Alberdi F, Garcia I, Atutxa L, Zabarte M, Trauma, Neurointensive Care Work Group of the S. Epidemiology of severe trauma. Med Intensiva. 2014;38(9):580–8. [DOI] [PubMed] [Google Scholar]
- 3.Wu J, Vodovotz Y, Abdelhamid S, Guyette FX, Yaffe MB, Gruen DS, et al. Multi-omic analysis in injured humans: Patterns align with outcomes and treatment responses. Cell Rep Med. 2021;2(12):100478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maier RV. Scudder Oration on Trauma. A century of evolution in trauma resuscitation. J Am Coll Surg. 2014;219(3):335–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dimopoulou I, Tsagarakis S, Theodorakopoulou M, Douka E, Zervou M, Kouyialis AT, et al. Endocrine abnormalities in critical care patients with moderate-to-severe head trauma: incidence, pattern and predisposing factors. Intensive Care Med. 2004;30(6):1051–7. [DOI] [PubMed] [Google Scholar]
- 6.Johansson PI, Stensballe J, Ostrowski SR . Shock induced endotheliopathy (SHINE) in acute critical illness - a unifying pathophysiologic mechanism. Crit Care. 2017;21(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johansson PI, Henriksen HH, Stensballe J, Gybel-Brask M, Cardenas JC, Baer LA, et al. Traumatic Endotheliopathy: A Prospective Observational Study of 424 Severely Injured Patients. Ann Surg. 2017;265(3):597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cabrera CP, Manson J, Shepherd JM, Torrance HD, Watson D, Longhi MP, et al. Signatures of inflammation and impending multiple organ dysfunction in the hyperacute phase of trauma: A prospective cohort study. PLoS Med. 2017;14(7):e1002352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cuenca AG, Gentile LF, Lopez MC, Ungaro R, Liu H, Xiao W, et al. Development of a genomic metric that can be rapidly used to predict clinical outcome in severely injured trauma patients. Crit Care Med. 2013;41(5):1175–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tompkins RG. Genomics of injury: The Glue Grant experience. J Trauma Acute Care Surg. 2015;78(4):671–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abdelhamid SS, Scioscia J, Vodovotz Y, Wu J, Rosengart A, Sung E, et al. Multi-Omic Admission-Based Prognostic Biomarkers Identified by Machine Learning Algorithms Predict Patient Recovery and 30-Day Survival in Trauma Patients. Metabolites. 2022;12(9):774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De’Ath HD, Rourke C, Davenport R, Manson J, Renfrew I, Uppal R, et al. Clinical and biomarker profile of trauma-induced secondary cardiac injury. Br J Surg. 2012;99(6):789–97. [DOI] [PubMed] [Google Scholar]
- 13.De’Ath HD, Manson J, Davenport R, Glasgow S, Renfrew I, Davies LC, et al. Trauma-induced secondary cardiac injury is associated with hyperacute elevations in inflammatory cytokines. Shock. 2013;39(5):415–20. [DOI] [PubMed] [Google Scholar]
- 14.Naganathar S, De’Ath HD, Wall J, Brohi K. Admission biomarkers of trauma-induced secondary cardiac injury predict adverse cardiac events and are associated with plasma catecholamine levels. J Trauma Acute Care Surg. 2015;79(1):71–7. [DOI] [PubMed] [Google Scholar]
- 15.Wilson NM, Wall J, Naganathar V, Brohi K, De’Ath HD. Mechanisms Involved in Secondary Cardiac Dysfunction in Animal Models of Trauma and Hemorrhagic Shock. Shock. 2017;48(4):401–10. [DOI] [PubMed] [Google Scholar]
- 16.Bonaroti J, Li S, Abdelhamid S, Billiar T. Prognostic Biomarkers to Predict Outcomes in Trauma. In: Rajendram R, Preedy VR, Patel VB, editors. Biomarkers in Trauma, Injury and Critical Care. Cham: Springer International Publishing; 2022. p. 1–25. [Google Scholar]
- 17.Sperry JL, Guyette FX, Brown JB, Yazer MH, Triulzi DJ, Early-Young BJ, et al. Prehospital Plasma during Air Medical Transport in Trauma Patients at Risk for Hemorrhagic Shock. N Engl J Med. 2018;379(4):315–26. [DOI] [PubMed] [Google Scholar]
- 18.Guyette FX, Brown JB, Zenati MS, Early-Young BJ, Adams PW, Eastridge BJ, et al. Tranexamic Acid During Prehospital Transport in Patients at Risk for Hemorrhage After Injury: A Double-blind, Placebo-Controlled, Randomized Clinical Trial. JAMA Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tarazona S, Balzano-Nogueira L, Gomez-Cabrero D, Schmidt A, Imhof A, Hankemeier T, et al. Harmonization of quality metrics and power calculation in multi-omic studies. Nat Commun. 2020;11(1):3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gold L, Ayers D, Bertino J, Bock C, Bock A, Brody EN, et al. Aptamer-based multiplexed proteomic technology for biomarker discovery. PLoS One. 2010;5(12):e15004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu J, Moheimani H, Li S, Kar UK, Bonaroti J, Miller RS, et al. High Dimensional Multi-omics Reveals Unique Characteristics of Early Plasma Administration in Polytrauma Patients with TBI. Ann Surg. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gruen DS, Brown JB, Guyette FX, Vodovotz Y, Johansson PI, Stensballe J, et al. Prehospital plasma is associated with distinct biomarker expression following injury. JCI Insight. 2020;5(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cyr A, Zhong Y, Reis SE, Namas RA, Amoscato A, Zuckerbraun B, et al. Analysis of the Plasma Metabolome after Trauma, Novel Circulating Sphingolipid Signatures, and In-Hospital Outcomes. J Am Coll Surg. 2021;232(3):276–87 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uhlen M, Fagerberg L, Hallstrom BM, Lindskog C, Oksvold P, Mardinoglu A, et al. Proteomics. Tissue-based map of the human proteome. Science. 2015;347(6220):1260419. [DOI] [PubMed] [Google Scholar]
- 25.(2021) RCT. R: A language and environment for statistical computing Vienna, Austria. Accessed November 1, 2021. https://www.R-project.org/ [Google Scholar]
- 26.Virtanen P, Gommers R, Oliphant TE, Haberland M, Reddy T, Cournapeau D, et al. Author Correction: SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat Methods. 2020;17(3):352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sauaia A, Moore EE, Johnson JL, Ciesla DJ, Biffl WL, Banerjee A. Validation of postinjury multiple organ failure scores. Shock. 2009;31(5):438–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kolwicz SC Jr. Purohit S, Tian R.Cardiac metabolism and its interactions with contraction, growth, and survival of cardiomyocytes. Circ Res. 2013;113(5):603–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Longo N, Frigeni M, Pasquali M. Carnitine transport and fatty acid oxidation. Biochim Biophys Acta. 2016;1863(10):2422–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doenst T, Nguyen TD, Abel ED. Cardiac metabolism in heart failure: implications beyond ATP production. Circ Res. 2013;113(6):709–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kato T, Niizuma S, Inuzuka Y, Kawashima T, Okuda J, Tamaki Y, et al. Analysis of metabolic remodeling in compensated left ventricular hypertrophy and heart failure. Circ Heart Fail. 2010;3(3):420–30. [DOI] [PubMed] [Google Scholar]
- 32.Miyagawa Y, Mori T, Goto K, Kawahara I, Fujiwara-Tani R, Kishi S, et al. Intake of medium-chain fatty acids induces myocardial oxidative stress and atrophy. Lipids Health Dis. 2018;17(1):258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murphy SP, Kakkar R, McCarthy CP, Januzzi JL Jr. Inflammation in Heart Failure: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75(11):1324–40. [DOI] [PubMed] [Google Scholar]
- 34.Mann DL. Inflammatory mediators and the failing heart: past, present, and the foreseeable future. Circ Res. 2002;91(11):988–98. [DOI] [PubMed] [Google Scholar]
- 35.Li S, Jiao X, Tao L, Liu H, Cao Y, Lopez BL, et al. Tumor necrosis factor-alpha in mechanic trauma plasma mediates cardiomyocyte apoptosis. Am J Physiol Heart Circ Physiol. 2007;293(3):H1847–52. [DOI] [PubMed] [Google Scholar]
- 36.Smith E, Fernandez C, Melander O, Ottosson F. Altered Acylcarnitine Metabolism Is Associated With an Increased Risk of Atrial Fibrillation. J Am Heart Assoc. 2020;9(21):e016737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Doenst T, Pytel G, Schrepper A, Amorim P, Farber G, Shingu Y, et al. Decreased rates of substrate oxidation ex vivo predict the onset of heart failure and contractile dysfunction in rats with pressure overload. Cardiovasc Res. 2010;86(3):461–70. [DOI] [PubMed] [Google Scholar]
- 38.Heather LC, Cole MA, Lygate CA, Evans RD, Stuckey DJ, Murray AJ, et al. Fatty acid transporter levels and palmitate oxidation rate correlate with ejection fraction in the infarcted rat heart. Cardiovasc Res. 2006;72(3):430–7. [DOI] [PubMed] [Google Scholar]
- 39.Lackner I, Weber B, Knecht D, Horst K, Relja B, Gebhard F, et al. Cardiac Glucose and Fatty Acid Transport After Experimental Mono- and Polytrauma. Shock. 2020;53(5):620–9. [DOI] [PubMed] [Google Scholar]
- 40.Hunt R, de M. Taveau R.The Effects of a Number of Derivatives of Choline and Analogous Compounds on the Blood-pressure: U.S. Government Printing Office; 1911. [Google Scholar]
- 41.Schneider R, Timms AR. Some aspects of the pharmacology of an homologous series of choline esters of fatty acids. Br J Pharmacol Chemother. 1957;12(1):30–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akimov MG, Kudryavtsev DS, Kryukova EV, Fomina-Ageeva EV, Zakharov SS, Gretskaya NM, et al. Arachidonoylcholine and Other Unsaturated Long-Chain Acylcholines Are Endogenous Modulators of the Acetylcholine Signaling System. Biomolecules. 2020;10(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Naumann DN, Hazeldine J, Davies DJ, Bishop J, Midwinter MJ, Belli A, et al. Endotheliopathy of Trauma is an on-Scene Phenomenon, and is Associated with Multiple Organ Dysfunction Syndrome: A Prospective Observational Study. Shock (Augusta, Ga). 2018;49(4):420–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Analyzed Tissue-specific Biomarkers with Corresponding Tissue Specificity and Function
Supplemental Digital Content. STROBE Checklist
Supplemental Figure 2. Heatmap of Tissue-Specific Biomarkers Stratified by Timepoint and Injury Severity in PAMPer Cohort
Supplemental Figure 1. Volcano Plot Comparing Log-2-fold Change in Concentration of Cardiac Metabolites Between Resolvers and Non-Resolvers for Metabolomic Analysis Pre-processing