Abstract
Ebola virus contains a single glycoprotein (GP) that is responsible for receptor binding and membrane fusion and is proteolytically cleaved into disulfide-linked GP1 and GP2 subunits. The GP2 subunit possesses a coiled-coil motif, which plays an important role in the oligomerization and fusion activity of other viral GPs. To determine the functional significance of the coiled-coil motif of GP2, we examined the effects of peptides corresponding to the coiled-coil motif of GP2 on the infectivity of a mutant vesicular stomatitis virus (lacking the receptor-binding/fusion protein) pseudotyped with the Ebola virus GP. A peptide corresponding to the C-terminal helix reduced the infectivity of the pseudotyped virus. We next introduced alanine substitutions into hydrophobic residues in the coiled-coil motif to identify residues important for GP function. None of the substitutions affected GP oligomerization, but some mutations, two in the N-terminal helix and all in the C-terminal helix, reduced the ability of GP to confer infectivity to the mutant vesicular stomatitis virus without affecting the transport of GP to the cell surface, its incorporation into virions, and the production of virus particles. These results indicate that the coiled-coil motif of GP2 plays an important role in facilitating the entry of Ebola virus into host cells and that peptides corresponding to this region could act as efficient antiviral agents.
Ebola and Marburg viruses—filamentous, enveloped, nonsegmented negative-strand RNA viruses—belong to the family Filoviridae and cause hemorrhagic fever in primates with high mortality rates (16, 34). The Ebola virus consists of four subtypes (Zaire, Sudan, Ivory Coast, and Reston) (16, 34) and possesses at least seven structural proteins (39). The surface glycoprotein (GP), expressed from the fourth structural protein gene (39), is a type I GP containing both N- and O-linked carbohydrates (15, 17). It is the only transmembrane protein protruding as a trimeric spike from the virion surface and is responsible for receptor binding and membrane fusion, leading to virus penetration (44, 53). The Ebola virus GP is proteolytically cleaved into disulfide-linked GP1 and GP2 subunits (41, 47), much like other viral membrane fusion proteins, including the hemagglutinin (HA1 and HA2) subunits of influenza virus, envelope protein (SU and TM, or gp120 and gp41) subunits of retroviruses, and fusion protein (F1 and F2) subunits of paramyxoviruses.
We (44) and others (53, 54) have developed complementation systems using either a mutant vesicular stomatitis virus (VSV) or retrovirus for studying the functions of the Ebola virus GP during the early steps of infection, without the constraints of BL-4 containment. Our system relies on a recombinant form of VSV (VSVΔG*) that contains the green fluorescent protein (GFP) gene instead of the VSV G gene and thus is not infectious unless the receptor binding and membrane fusion protein is provided in trans (44). The Ebola virus GP confers infectivity to the mutant VSV and the complemented virus infects primate cells more efficiently than avian, insect, and other mammalian cells, corresponding to the host range tropism of Ebola virus (44).
Gallaher (18) proposed that the C-terminal 180 amino acids of the Ebola virus GP (GP2) are structurally similar to the retroviral transmembrane (TM) domain. The N terminus of GP2 contains the fusion peptide, as demonstrated by peptide and mutational analyses (20, 38). Next to the fusion peptide are a long amphipathic helix, a disulfide-bonded loop region homologous to the conserved immunosuppressive motif (46), and the C-terminal helix (Fig. 1A and B). Recently, GP2 ectodomain without the fusion peptide was crystallized, and its X-ray crystal structure was determined (31, 49). These analyses showed that the core structure of GP2 forms a trimeric coiled-coil derived from the N-terminal helices and buttressed by three surrounding helices from the C-terminal region aligned in an antiparallel orientation (31, 49). This helical structure is remarkably similar to that of the TM subunit of influenza virus, retroviruses, and paramyxoviruses (1, 3, 4, 6, 7, 13, 14, 23, 25, 30, 45, 48).
FIG. 1.
(A) Schematic representation of the Ebola virus GP. The GP is cleaved at position 501 into GP1 and GP2 subunits. The signal peptide, the fusion peptide, and the TM anchor are shown as shaded boxes, while the two helices are depicted as open boxes. The amino acid sequence between positions 554 and 630 is presented beneath the structure in single-letter code, and the residues in which mutations were introduced are indicated with italic letters. (B) Three-dimensional structure of the Ebola GP2 monomer. The residues containing a mutation are indicated by cyan coloring in the N-terminal helix and by violet in the C-terminal helix. (C) Helical wheel representation of the N- and C-terminal helices. N and C represent the N- and C-terminal helices, respectively. The a through g lettering represents the heptad repeats. Residues in which a mutation was introduced are indicated by boldface italic letters, with their respective positions given underneath the letters. (D) Expression of the wild-type Ebola virus GP and its mutants. 293T cells were transfected with a plasmid expressing Ebola virus GP or its mutants and lysed in a sample buffer. Proteins in the lysates were separated by SDS–10% PAGE, transferred to a PVDF membrane, and detected by anti-Ebola virus GP-SGP rabbit serum. Molecular masses of the marker proteins are shown on the left.
To understand the molecular events in the early steps of Ebola virus infection, we sought to determine the functional roles of different regions of the GP in these processes. Several studies on the coiled-coil of viral glycoproteins (e.g., the gp41 of human immunodeficiency virus type 1 [HIV-1], the F1 subunit of paramyxoviruses, and the S protein of coronavirus) have indicated the importance of the coiled-coil of these proteins for oligomerization and a subsequent membrane fusion event (2, 5, 10–12, 28, 35, 37, 50). Similarities among the core structures of the GP2 of Ebola virus, the gp41 of HIV-1, and the F1 subunit of paramyxoviruses suggest that the GP2 coiled-coil plays important roles in GP oligomerization and fusion activity between the viral envelope and the cellular membrane. We therefore assessed the inhibitory activity of peptides corresponding to the GP2 coiled-coil on GP function and determined the effects of amino acid substitutions in the N- and C-terminal helices of GP2 on the oligomerization and infectivity of VSVΔG∗ complemented with GP or one of its mutants.
MATERIALS AND METHODS
Plasmids.
A full-length cDNA encoding the Ebola virus (Zaire subtype) GP (40) was cloned into the expression vector pCAGGS/MCS (32, 33). The resulting construct was designated pCEboZGP.
Cells and viruses.
Vero cells were grown in Eagle minimal essential medium supplemented with 10% fetal calf serum (FCS), l-glutamine, vitamin and amino acid solutions, and antibiotics. Human embryonic kidney 293T cells were cultured in high-glucose Dulbecco modified Eagle medium containing 10% FCS, l-glutamine, and antibiotics.
The recombinant VSV, which possesses the GFP gene instead of the G protein gene, complemented with VSV G protein (VSVΔG∗-G) or the Ebola virus GP (VSVΔG∗-EbolaGP), was prepared as described previously (44). Briefly, 293T cells were transfected with pCEboZGP. At 36 h after transfection, cells were infected with VSVΔG∗-G at a multiplicity of infection of 1. Then, 24 h after infection, the supernatant was harvested for virus stock.
Site-directed mutagenesis.
Site-directed mutagenesis was carried out with the GeneEditor in vitro site-directed mutagenesis system (Promega), as described by the manufacturer. The presence of the desired mutations and the absence of unwanted mutations in the genes were confirmed by DNA sequencing (42). The mutant Ebola virus GPs were designated according to their respective amino acid substitutions (e.g., L554A denotes a mutant GP containing amino acid substitution Leu-to-Ala at position 554).
Western blotting.
Proteins were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and electrotransferred to a polyvinylidene difluoride (PVDF) membrane. The PVDF membrane was blocked overnight at 4°C with 5% skim milk in phosphate-buffered saline (PBS) and then incubated with anti-VSV M protein monoclonal antibody (MAb) and anti-Ebola virus GP-secreted GP (SGP) rabbit serum for 2 h at room temperature. The membrane was washed five times with PBS containing 0.05% Tween 20. Bound antibodies were detected with a Vectastain ABC kit (Vector) and the Western immunoblot ECL system (Amersham). Signal intensities were quantified with an Alpha Imager 2000 (Alpha Innotech Corp.).
Infectivity of the recombinant VSVs.
To decrease background infectivity contributed by VSVΔG∗-G during preparation of VSVΔG∗-EbolaGP or its mutants, we incubated viruses with anti-VSV G MAb for 1 h at room temperature. Vero cells were then incubated with recombinant VSVs for 12 to 14 h at 37°C, fixed with 3% formalin in PBS, and then directly examined for GFP expression in 10 randomly selected microscopic fields.
Inhibition of recombinant VSV infectivity by peptide.
The peptides EbolaGP555 (ICGLRQLANETTQALQLFLRATTELRTFSILNRKA) and EbolaGP610 (IEPHDWTKNITDKIDQIIHDFVDK), corresponding to GP amino acids at positions 555 to 589 and 610 to 633, respectively, were synthesized by a standard FMOC (9-fluorenylmethoxy carbonyl) method on an Applied Biosystems 433A peptide synthesizer (Perkin-Elmer) and purified by high-performance liquid chromatography on a C18 column with an acetonitrile gradient containing 0.1% trifluoroacetic acid. Recombinant VSVs were mixed with either peptide at 0, 0.2, 1, or 5 mg/ml and incubated for 1 h at room temperature. Vero cells were then incubated with a virus-peptide mixture for 12 to 14 h at 37°C, fixed with 3% formalin in PBS, and then directly examined for GFP expression in 10 randomly selected microscopic fields.
Flow cytometric analysis.
293T cells expressing wild-type or mutant Ebola virus GPs were detached by EDTA treatment and incubated with anti-Ebola virus GP-SGP rabbit serum for 1 h on ice. Cells were washed with PBS containing 1% fetal bovine serum and then were incubated with fluorescein isothiocyanate (FITC)-conjugated anti-rabbit immunoglobulin for 30 min on ice. After the cells were washed, they were resuspended in 3% formalin in PBS and analyzed by flow cytometry.
Chemical cross-linking.
293T cells expressing wild-type or mutant Ebola virus GPs were detached by EDTA treatment and incubated with dithiobis(succinimidyl-propionate) (DSP; final concentration, 1 mg/ml; Pierce Chemical Co.) for 2 h at room temperature. Reactions were stopped by adding Tris (final concentration, 100 mM). Cells were washed with PBS and lysed in 20 mM Tris-HCl (pH 7.5), 2 mM EDTA, 150 mM NaCl, 0.1% deoxycholic acid, and 1% Nonidet P-40. The cross-linked samples were analyzed by Western blotting using anti-Ebola virus GP-SGP rabbit serum.
GP cell-binding assay.
We constructed plasmids encoding the wild-type or mutant GPs with a six-histidine tag inserted between positions 38 and 39 by site-directed mutagenesis. At 24 h after transfection, cells were labeled with 50 μCi of Tran35S-label (ICN) per ml for 12 h. Cells were then washed with PBS and treated with lysis buffer (20 mM Tris-HCl [pH 7.5], 150 mM NaCl, and 40 mM n-octylglucoside). Lysed cells were centrifuged to remove cell debris, and the supernatant was mixed with Ni-nitrilotriacetic acid agarose (Qiagen), followed by purification of the GPs in a batch procedure. The GPs were eluted with elution buffer (20 mM Tris-HCl [pH 7.5], 150 mM NaCl, 250 mM imidazole, and 40 mM n-octylglucoside) and dialyzed against PBS.
For binding assays, radiolabeled GPs (ca. 18,000 cpm) were incubated with normal rabbit serum, anti-influenza A virus (A/WSN/33) rabbit serum, or anti-Ebola virus GP-SGP rabbit serum for 2 h at room temperature and then added to Vero cells for 2 h at 4°C. Cells were then washed five times with PBS to remove the unbound GPs and lysed in PBS containing 1% Nonidet P-40. Cell lysates were counted in a scintillation counter. The GP cell binding was determined by the following formula: (counts per minute [cpm] of lysate of GP-bound cells in the presence of normal rabbit serum) − (cpm of lysate of GP-bound cells in the presence of anti-Ebola virus GP-SGP rabbit serum).
RESULTS
Effect of the peptide corresponding to the C-terminal helix sequence of Ebola virus GP2 on the infectivity of VSVΔG∗-EbolaGP.
The peptides corresponding to the coiled-coil regions of viral fusion proteins possess antiviral activity (8, 22, 27, 36, 51, 52, 55). To test whether peptides corresponding to the GP2 N- and C-terminal helix regions inhibit virus infection, we synthesized two peptides, one corresponding to the N-terminal helix (residues 555 to 589) and the other corresponding to the C-terminal helix (residues 610 to 633). The first, EbolaGP555, was soluble only in organic solutions and was precipitated in a tissue culture medium, prompting us to test the ability of the C-terminal helix peptide, Ebola GP610, on the infectivity of VSVΔG∗-EbolaGP (Fig. 2). This peptide reduced the infectivity of VSVΔG∗-EbolaGP but not VSVΔG∗-G in a dose-dependent manner, indicating that at least the C-terminal helix of Ebola virus GP2 participates in the initiation of virus infection.
FIG. 2.
Effect of a peptide corresponding to the GP2 C-terminal helix at positions 610 to 633 on the infectivity of recombinant VSV complemented with Ebola virus GP. Recombinant VSVs complemented with either Ebola virus GP or VSV G were incubated with or without the peptide for 1 h at room temperature, prior to incubation with Vero cells. The infectivity of recombinant viruses was determined by calculating the number of GFP-positive cells in 10 random microscopic fields in the presence of various concentrations of the peptide. Experiments were performed three times, and a representative result is shown.
Expression of the mutant Ebola virus GPs.
The coiled-coil motif contains hydrophobic residues with a heptad periodicity, generating a hydrophobic face. Heptad positions are usually denoted “a” through “g.” Residues in positions a and d in one helix hydrophobically interact with those in others to stabilize the coiled-coil motif. To assess the importance of the coiled-coil motif of Ebola virus GP2 in GP functions, we introduced alanine substitutions into hydrophobic residues in positions a and d of the N- and C-terminal coiled-coil motifs of GP2 (Fig. 1C). We first analyzed the expression of the mutants in 293T cells by Western blotting using anti-Ebola virus GP-SGP antibody (Fig. 1D). With one exception (L569A), all of the mutant Ebola virus GPs were expressed in 293T cells in amounts and with gel migratory properties similar to those of the wild-type GP. The Leu-to-Ala substitution at position 569 resulted in a lower expression level of a slower-migrating GP than was seen with the wild-type GP.
Surface expression of the mutant Ebola virus GPs.
To verify that the mutant GPs were transported to the cell surface, we analyzed the GP-expressing 293T cells by flow cytometry. As shown in Table 1, all of the mutant Ebola virus GPs were expressed at the cell surface at levels comparable to that of the wild-type protein, indicating that mutations introduced in the coiled-coil motif of Ebola virus GP2 did not appreciably affect the transport of the resulting molecules.
TABLE 1.
Cell surface expression of the wild-type GP and its mutantsa
| GP | % Cells expressing GP | Mean fluorescence intensity |
|---|---|---|
| Wild type | 36.2 | 61.3 |
| L554A | 48.5 | 51.6 |
| L558A | 53.3 | 51.5 |
| L561A | 38.2 | 59.0 |
| L569A | 55.2 | 62.8 |
| F572A | 36.9 | 55.6 |
| L579A | 43.4 | 60.6 |
| L585A | 44.2 | 63.2 |
| F592A | 35.3 | 64.6 |
| L593A | 38.3 | 58.2 |
| I619A | 34.0 | 58.3 |
| I623A | 37.7 | 56.5 |
| I626A | 36.1 | 50.1 |
| F630A | 40.8 | 57.1 |
293T cells were transfected with plasmid DNA encoding the wild-type or mutant GP and incubated for 36 h. Cell surface expression of the GP was determined by flow cytometry with anti-Ebola virus GP-SGP rabbit serum followed by an FITC-conjugated secondary antibody.
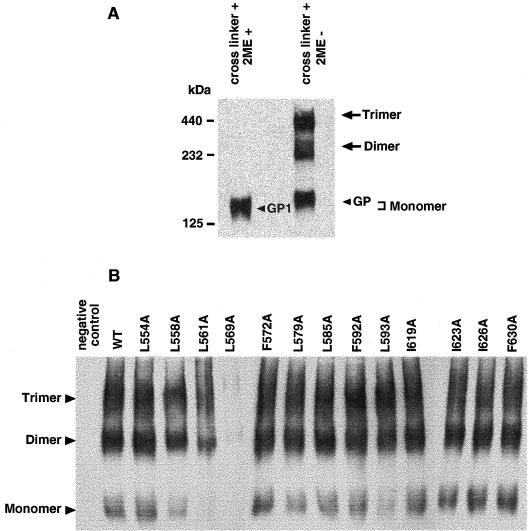
Oligomerization of the mutant Ebola virus GPs.
To determine whether amino acid substitutions affect oligomerization of the mutant Ebola virus GPs, we cross-linked the proteins expressed at the cell surface using a cross-linker, DSP, sensitive to reducing agents (e.g., 2-mercaptoethanol). When incubated with the cross-linker, the wild-type Ebola virus GP was detected in monomeric, dimeric, and trimeric forms (Fig. 3A) as observed by others (41). Only the monomer was detected with 2-mercaptoethanol treatment. Since all of the mutants formed oligomers to approximately the same extent as the wild-type protein when incubated with the cross-linker (Fig. 3B), we concluded that the mutations introduced into the coiled-coil motif of the GP2 did not affect GP oligomerization. However, for unknown reasons, the monomeric form of L561A was detected in reduced amounts, and the monomer and multimers of L569A were poorly detected, although cell surface amounts of these mutants, as detected by flow cytometry were similar to those for the wild-type protein (Table 1).
FIG. 3.
Oligomer formation of wild-type Ebola virus GP and its mutants. 293T cells were transfected with a plasmid expressing Ebola virus GP or its mutants, incubated with a cross-linker (DSP), and lysed in a lysis buffer. (A) The cross-linked wild-type GP that was treated or not treated with 2-mercaptoethanol (2ME) was separated by SDS–6% PAGE. The molecular masses of marker proteins are shown on the left. (B) The cross-linked samples in lysates were separated by SDS–3.5% PAGE. Western blotting was performed as described in Fig. 1.
Incorporation of the mutant Ebola virus GPs into recombinant VSV particles.
In order for the Ebola virus GP to confer infectivity to VSVΔG∗ virus, it must be incorporated into a VSV virion. To verify the efficiency of incorporation of the mutant Ebola virus GPs into VSV particles, we partially purified the recombinant VSVs from the supernatants of GP-expressing cells that were infected with VSVΔG∗-G (Fig. 4A). The levels of GP incorporation into VSV virions were then compared by Western blot analysis after standardization based on the intensity of VSV M protein. With a few exceptions, the mutant Ebola virus GPs were incorporated into VSV particles as well as or more efficiently than the wild-type protein, indicating that amino acid substitutions in the coiled-coil region of the Ebola virus GP did not negatively affect incorporation of the Ebola virus GPs into VSV particles. However, some of the GPs (especially L561A and L569A) with a mutation in the N-terminal helix were incorporated into VSV particles less efficiently than was the wild-type protein.
FIG. 4.
(A) Incorporation of wild-type Ebola virus GP and its mutants into VSV particles. VSVΔG∗ complemented with Ebola virus GP or its mutants was partially purified by centrifugation through 25% sucrose and lysed in a sample buffer. Viral proteins were separated by SDS–10% PAGE, and Western blotting was performed as described in Fig. 1. The relative levels of mutant GP incorporation into VSV compared to those with the wild-type GP are shown as the means of two independent experiments by comparing the GP intensity of purified viruses using VSV M protein for standardization. (B) Infectivity in Vero cells of recombinant VSV complemented with wild-type Ebola virus GP or its mutants. The infectivity of recombinant viruses is shown as infectious units, calculated from the number of GFP-positive cells in 10 random microscopic fields. The mean and standard error of two independent experiments are shown. (C) Relative binding activity of the wild-type and mutant GPs to Vero cells. GP cell-binding was determined as described in Materials and Methods. The binding activity of mutant GPs was shown as a percentage relative to that of the wild-type. The mean and standard error of two independent experiments are shown.
Effect of amino acid substitutions on the infectivity of VSVΔG∗-EbolaGP.
To test the effects of amino acid substitutions in the coiled-coil motif of the Ebola virus GP2 on the ability of the GP to initiate virus infection, we examined the infectivity of VSVΔG∗ complemented with either the wild-type or a mutant Ebola virus GP in Vero cells (Fig. 4B). Recombinant VSV pseudotyped with the wild-type GP had an infectivity titer of 106.9 infectious units/ml, as judged by the number of GFP-expressing cells. Among mutant GPs with an alteration in the N-terminal helix and with similar levels of incorporation into virions, F592A and L593A appreciably reduced the ability of the GP to confer infectivity to VSVΔG∗. Although the L561A and L569A mutations also negatively affected this ability, they were associated with decreased GP incorporation into VSV particles (Fig. 4). Other mutations in the N-terminal helix did not impair GP function, although VSVΔG∗ complemented with L554A or F572A mutant GPs showed slightly reduced infectivity. In contrast, all of the mutations introduced into the C-terminal helix reduced the ability of the GP to confer infectivity to VSVΔG∗ without affecting GP virion incorporation.
To determine whether the amino acid substitutions in the coiled-coil motif of the Ebola virus GP2 affect GP binding activity to the target cells, we produced the wild-type or mutant GPs and examined their cell-binding activity (Fig. 4C). The binding activity of any GPs was not inhibited by anti-influenza A virus (A/WSN/33) rabbit serum (negative control; data not shown). Although L569A and F572A mutant GPs bound to cells at a reduced level, other mutants bound as well as or more efficiently than the wild-type, suggesting that the mutations that reduced the ability of the GP to confer infectivity did not affect their cell binding. These results indicate that the coiled-coil motif of the Ebola virus GP2 is crucial for the initiation of virus infection by the GP and that alterations in the C-terminal helix have a more profound effect on GP function than do those in the N-terminal helix.
DISCUSSION
We have demonstrated that the N- and C-terminal helical regions of Ebola virus GP are important for the ability of this protein to support viral entry into host cells. Our findings are consistent with the fact that two comparable coiled-coil regions in the TM subunit of other viral glycoproteins (e.g., HA2 of influenza virus, F1 of paramyxoviruses, and TM or gp41 of retroviruses) are also critical for their functions (2, 5, 10–12, 35, 37, 50).
The crystal structures of many viral TM subunits are thought to be the fusion-active state and to represent the final, most-stable form of the protein after a conformational change, since these structures are thermostable and the N-terminal end (the fusion peptide) and the C-terminal end (adjacent to the TM domain) lie on the same side of the molecule (reviewed in reference 9). For viral fusion proteins, a conformational change to the fusion-active state is an essential step in the fusion of the viral envelope with target membranes. When the native state of the influenza virus HA is exposed to low pH, a long loop of the N terminus of HA2 forms a three-stranded coiled-coil by the spring-loaded mechanism, and the C-terminal end of HA2 refolds to form a loop and to pack against the N-terminal helix in an antiparallel orientation (fusion-active state) (3, 6). Although the native conformation of gp120-gp41 has not been identified for HIV-1, when the virus binds to cellular receptors, the conformation of gp120-gp41 complex changes to the fusion-active state (reviewed in references 9 and 43). Because of its remarkable similarity to the crystal structures of influenza virus HA2 and of HIV gp41, the crystal structure of the Ebola virus GP2 is thought to be the fusion-active state. Previous studies by us and others have shown that the Ebola virus GP requires exposure to low pH for its ability to initiate infection (44, 53). Although the native conformation of the Ebola virus GP has not been determined, a low-pH environment may trigger a conformational change in this protein (as shown for the influenza virus HA), resulting in the fusion of the viral envelope with cellular membranes (Fig. 5A).
FIG. 5.
Model for Ebola virus GP2-mediated membrane fusion. A conformational change would lead to the insertion of the fusion peptide into the host cell membrane (left panel). (A) Upon insertion of the fusion peptide into the host cell membrane, GP2 induces fusion of viral envelope with the host cell membrane. (B and C) Amino acid substitutions (shown in red) (B) or a peptide (shown in red) corresponding to the coiled-coil structure of GP2 (C) may inhibit a conformational change of the molecule, resulting in the lack of fusion between viral envelope and the host cell membrane.
Among 13 mutants we generated, six mutants (two in the N-terminal helix [F592A and L593A] and four in the C-terminal helix [I619A, I623A, I626A, and F630A]) either lost or showed a reduced ability (<10% of that of the wild-type GP) to confer infectivity to VSV lacking its receptor-binding and fusion protein. Because these mutant GPs formed a trimer and were incorporated into VSV particles as well as the wild-type GP, these substitutions did not appear to broadly affect the native conformation of the molecule but instead affected the process of the conformational change or the fusion-active conformation after a conformational change (Fig. 5B).
Amino acids at positions 592 and 593 are located at the end of the N-terminal helix adjacent to a disulfide bonded-loop in the crystal structure (Fig. 1B). This loop seems to serve as a hinge that can alter the direction of the downstream C-terminal helix upon a conformational change (31, 49). Thus, these substitutions might hinder a proper conformational change or affect the molecule of the fusion-active state after a conformational change. A substitution at position 561 in the N-terminal helix also inhibited GP function, although incorporation of the mutant into virions was reduced, indicating that this residue (L561) may also be important for GP conformation.
Amino acids at positions 619, 623, 626, and 630 are located in the C-terminal helix (Fig. 1B), which forms an outer helix that packs in an antiparallel manner into grooves formed by the N-terminal helix. After a conformational change, the C-terminal (outer) helix must interact with the N-terminal (inner) helix to form a stable, fusion-active conformation. Since amino acids at positions 619, 623, 626, and 630 interact with residues composing the N-terminal helix in the crystal structure (31, 49), substitutions may impede proper packing of the N- and C-terminal helices to form a fusion-active oligomer.
Studies of a point mutation in the N-terminal helix of the HIV-1 gp41 molecule revealed that substitutions of residues at position a or d in a heptad repeat can affect fusion activity (10, 12, 35). In our study, the majority of amino acid substitutions in the N-terminal helix (L554, L558, L569, F572, L579, and L585) did not appreciably inhibit GP function, whereas those in the C-terminal helix did, suggesting that with regard to the fusion process, the C-terminal helix may be important for stabilizing conformation of the GP molecule for the Ebola virus.
Amino acid changes in viral GPs can inhibit protein folding and oligomerization. In this study, we introduced alanine substitutions into the coiled-coil regions of the Ebola virus GP2 to minimize the effect of mutations on the overall structure. Alanine has a strong α-helix-forming propensity (19, 29). In fact, to inhibit oligomerization of HIV glycoprotein by alanine substitution, 9 of the 10 hydrophobic repeat residues in the N-terminal helix of HIV-1 gp41 must be changed (35). These findings are consistent with ours showing that alanine substitutions in the coiled-coil regions of the Ebola virus GP2 do not negatively affect oligomerization.
A peptide corresponding to the C-terminal helix inhibited infection of recombinant VSVs complemented with Ebola virus GP, although the peptide concentrations required to inhibit infection were higher than those used in other studies (8, 22, 27, 36, 51, 52, 55). This discrepancy may reflect differences in the assay systems. The studies of peptides for HIV-1 and paramyxoviruses were performed with multiple cycles of viral replication, whereas in our study only a single cycle of replication was used, raising the possibility that a lower amount of peptide was needed to inhibit multiple, as opposed to single, cycles of replication. Alternatively, the explanation may lie in differences between the fusion processes of Ebola virus and those of HIV-1 or paramyxoviruses. The former appears to fuse in the endosome (44, 53), while the latter fuses with the surface of cellular membrane (9, 26). If inhibitory peptides interact with the coiled-coil upon a conformational change of the fusion proteins, the amount of peptides available at the cell surface may be higher than in the endosome.
A peptide corresponding to the C-terminal helix of HIV-1 gp41 inhibited viral replication in vitro and in vivo (8, 22, 24, 52). The mechanism for this effect is thought to be due to inhibition of fusion of the viral envelope with cell membranes through binding of the peptide to the N-terminal helix region of HIV gp41 during a conformational change (reviewed in references 9 and 43). The inhibitory activity attributed to an Ebola virus peptide in our study may stem from the same mechanism (Fig. 5C). Attempts to elicit protective immune responses against Ebola virus by traditional active and passive immunization approaches have not been successful (21, 34). Thus, peptides corresponding to the C-terminal helix may prove useful as an antiviral agent against Ebola virus infection, depending on studies to define optimal peptide length and composition.
Results of the present study indicate the importance of the coiled-coil region of Ebola virus GP2 in GP function, as well as the potential of corresponding peptides as antiviral agents. Use of conformation-specific antibodies to probe GP conformational change may provide insight into the contributions of the GP2 coiled-coil region to the Ebola virus life cycle.
ACKNOWLEDGMENTS
We thank Krisna Wells, Martha McGregor, and Nicole Miller for excellent technical assistance; Yuko Kawaoka for illustration; and John Gilbert for editing the manuscript. We also thank Anthony Sanchez for providing anti-Ebola virus GP/SGP rabbit serum and Michael Whitt for providing the VSVΔG∗-G. Automated sequencing was performed at the University of Wisconsin-Madison Biotechnology Center. Peptide synthesis and purification were performed at the St. Jude Children's Research Hospital Hartwell Center for Bioinformatics and Biotechnology.
Support for this work was provided by NIAID Public Health Service research grants. S.W. is the recipient of the Japan Society for Promotion of Science Postdoctoral Fellowship for Research Abroad. T.W. is the recipient of a research fellowship of the Japan Society for the Promotion of Science for Young Scientists.
REFERENCES
- 1.Baker K A, Dutch R E, Lamb R A, Jardetzky T S. Structural basis for paramyxovirus-mediated membrane fusion. Mol Cell. 1999;3:309–319. doi: 10.1016/s1097-2765(00)80458-x. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein H B, Tucker S P, Kar S R, McPherson S A, McPherson D T, Dubay J W, Lebowitz J, Compans R W, Hunter E. Oligomerization of the hydrophobic heptad repeat of gp41. J Virol. 1995;69:2745–2750. doi: 10.1128/jvi.69.5.2745-2750.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bullough P A, Hughson F M, Skehel J J, Wiley D C. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature. 1994;371:37–43. doi: 10.1038/371037a0. [DOI] [PubMed] [Google Scholar]
- 4.Caffrey M, Cai M, Kaufman J, Stahl S J, Wingfield P T, Covell D G, Gronenborn A M, Clore G M. Three-dimensional solution structure of the 44 kDa ectodomain of SIV gp41. EMBO J. 1998;17:4572–4584. doi: 10.1093/emboj/17.16.4572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cao J, Bergeron L, Helseth E, Thali M, Repke H, Sodroski J. Effects of amino acid changes in the extracellular domain of the human immunodeficiency virus type 1 gp41 envelope glycoprotein. J Virol. 1993;67:2747–2755. doi: 10.1128/jvi.67.5.2747-2755.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carr C M, Kim P S. A spring-loaded mechanism for the conformational change of influenza hemagglutinin. Cell. 1993;73:823–832. doi: 10.1016/0092-8674(93)90260-w. [DOI] [PubMed] [Google Scholar]
- 7.Chan D C, Fass D, Berger J M, Kim P S. Core structure of gp41 from the HIV envelope glycoprotein. Cell. 1997;89:263–273. doi: 10.1016/s0092-8674(00)80205-6. [DOI] [PubMed] [Google Scholar]
- 8.Chan D C, Chutkowski C T, Kim P S. Evidence that a prominent cavity in the coiled coil of HIV type 1 gp41 is an attractive drug target. Proc Natl Acad Sci USA. 1998;95:15613–15617. doi: 10.1073/pnas.95.26.15613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan D C, Kim P S. HIV entry and its inhibition. Cell. 1998;93:681–684. doi: 10.1016/s0092-8674(00)81430-0. [DOI] [PubMed] [Google Scholar]
- 10.Chen S S-L, Lee C-N, Lee W-R, McIntosh K, Lee T-H. Mutational analysis of the leucine zipper-like motif of the human immunodeficiency virus type 1 envelope transmembrane glycoprotein. J Virol. 1993;67:3615–3619. doi: 10.1128/jvi.67.6.3615-3619.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen S S-L. Functional role of the zipper motif region of human immunodeficiency virus type 1 transmembrane protein gp41. J Virol. 1994;68:2002–2010. doi: 10.1128/jvi.68.3.2002-2010.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dubay J W, Roberts S J, Brody B, Hunter E. Mutations in the leucine zipper of the human immunodeficiency virus type 1 transmembrane glycoprotein affect fusion and infectivity. J Virol. 1992;66:4748–4756. doi: 10.1128/jvi.66.8.4748-4756.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dutch R E, Leser G P, Lamb R A. Paramyxovirus fusion protein: characterization of the core trimer, a rod-shaped complex with helices in anti-parallel orientation. Virology. 1999;254:147–159. doi: 10.1006/viro.1998.9532. [DOI] [PubMed] [Google Scholar]
- 14.Fass D, Harrison S C, Kim P S. Retrovirus envelope domain at 1.7 Å resolution. Nat Struct Biol. 1996;3:465–469. doi: 10.1038/nsb0596-465. [DOI] [PubMed] [Google Scholar]
- 15.Feldmann H, Will C, Schikore M, Slenczka W, Klenk H-D. Glycosylation and oligomerization of the spike protein of Marburg virus. Virology. 1991;182:353–356. doi: 10.1016/0042-6822(91)90680-A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldmann H, Klenk H-D, Sanchez A. Molecular biology and evolution of filoviruses. Arch Virol Suppl. 1993;7:81–100. doi: 10.1007/978-3-7091-9300-6_8. [DOI] [PubMed] [Google Scholar]
- 17.Feldmann H, Nichol S T, Klenk H-D, Peters C J, Sanchez A. Characterization of filoviruses based on differences in structure and antigenicity of the virion glycoprotein. Virology. 1994;199:469–473. doi: 10.1006/viro.1994.1147. [DOI] [PubMed] [Google Scholar]
- 18.Gallaher W R. Similar structural models of the transmembrane proteins of Ebola and avian sarcoma viruses. Cell. 1996;85:477–488. doi: 10.1016/s0092-8674(00)81248-9. [DOI] [PubMed] [Google Scholar]
- 19.Heinz D W, Baase W A, Matthews B W. Folding and function of a T4 lysozyme containing 10 consecutive alanines illustrate the redundancy of information in an amino acid sequence. Proc Natl Acad Sci USA. 1992;89:3751–3755. doi: 10.1073/pnas.89.9.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ito H, Watanabe S, Sanchez A, Whitt M A, Kawaoka Y. Mutational analysis of the putative fusion domain of Ebola virus glycoprotein. J Virol. 1999;73:8907–8912. doi: 10.1128/jvi.73.10.8907-8912.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jahrling P B, Geisbert J, Swearengen J R, Jaax G P, Lewis T, Huggins J W, Schmitdt J J, LeDuc J W, Peters C J. Passive immunization of Ebola virus-infected cynomolgus monkeys with immunoglobulin from hyperimmune horses. Arch Virol Suppl. 1996;11:135–140. doi: 10.1007/978-3-7091-7482-1_12. [DOI] [PubMed] [Google Scholar]
- 22.Jiang S, Lin K, Strick N, Neurath A R. HIV-1 inhibition by a peptide. Nature. 1993;365:113. doi: 10.1038/365113a0. [DOI] [PubMed] [Google Scholar]
- 23.Joshi S B, Dutch R E, Lamb R A. A core trimer of the paramyxovirus fusion protein: parallels to influenza virus hemagglutinin and HIV-1 gp41. Virology. 1998;248:20–34. doi: 10.1006/viro.1998.9242. [DOI] [PubMed] [Google Scholar]
- 24.Kilby J M, Hopkins S, Venetta T M, DiMassimo B, Cloud G A, Lee J Y, Alldredge L, Hunter E, Lambert D, Bolognesi D, Matthews T, Johnson M R, Nowak M A, Shaw G M, Saag M S. Potent suppression of HIV-1 replication in humans by T-20, a peptide inhibitor of gp41-mediated virus entry. Nat Med. 1998;4:1302–1307. doi: 10.1038/3293. [DOI] [PubMed] [Google Scholar]
- 25.Kobe B, Center R J, Kemp B E, Poumbourios P. Crystal structure of human T cell leukemia virus type 1 gp21 ectodomain crystallized as a maltose-binding protein chimera reveals structural evolution of retroviral transmembrane proteins. Proc Natl Acad Sci USA. 1999;96:4319–4324. doi: 10.1073/pnas.96.8.4319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lamb R A. Paramyxovirus fusion: a hypothesis for changes. Virology. 1993;197:1–11. doi: 10.1006/viro.1993.1561. [DOI] [PubMed] [Google Scholar]
- 27.Lambert D M, Barney S, Lambert A L, Guthrie K, Medinas R, Davis D E, Bucy T, Erickson J, Merutka G, Petteway S R., Jr Peptides from conserved regions paramyxovirus fusion (F) proteins are potent inhibitors of viral fusion. Proc Natl Acad Sci USA. 1996;93:2186–2191. doi: 10.1073/pnas.93.5.2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luo Z, Matthews A M, Weiss S R. Amino acid substitutions within the leucine zipper domain of the murine coronavirus spike protein cause defects in oligomerization and the ability to induce cell-to-cell. J Virol. 1999;73:8152–8159. doi: 10.1128/jvi.73.10.8152-8159.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lyu P C, Liff M I, Marky L A, Kallenbach N R. Side chain contributions to the stability of alpha-helical structure in peptides. Science. 1990;250:669–673. doi: 10.1126/science.2237416. [DOI] [PubMed] [Google Scholar]
- 30.Malashkevich V N, Chan D C, Chutkowski C T, Kim P S. Crystal structure of the simian immunodeficiency virus (SIV) gp41 core: conserved helical interactions underlie the broad inhibitory activity of gp41 peptides. Proc Natl Acad Sci USA. 1998;95:9134–9139. doi: 10.1073/pnas.95.16.9134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malashkevich V N, Schneider B J, McNally M L, Milhollen M A, Pang J X, Kim P S. Core structure of the envelope glycoprotein GP2 from Ebola virus at 1.9-Å resolution. Proc Natl Acad Sci USA. 1999;96:2662–2667. doi: 10.1073/pnas.96.6.2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Niwa H, Yamamura K, Miyazaki J. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene. 1991;108:193–199. doi: 10.1016/0378-1119(91)90434-d. [DOI] [PubMed] [Google Scholar]
- 33.Park E K, Castrucci M R, Portner A, Kawaoka Y. The M2 ectodomain is important for its incorporation into influenza A virions. J Virol. 1998;72:2449–2455. doi: 10.1128/jvi.72.3.2449-2455.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peters C J, Sanchez A, Rollin P E, Ksiazek T G, Murphy F A. Filoviridae: Marburg and Ebola viruses. In: Fields B N, Knipe D M, Howley P M, editors. Fields virology. 3rd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 1161–1176. [Google Scholar]
- 35.Poumbourios P, Wilson K A, Center R J, Ahmer W E, Kemp B E. Human immunodeficiency virus type 1 envelope glycoprotein oligomerization requires the gp41 amphipathic α-helical/leucine zipper-like sequence. J Virol. 1997;71:2041–2049. doi: 10.1128/jvi.71.3.2041-2049.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rapaport D, Ovadia M, Shai Y. A synthetic peptide corresponding to a conserved heptad repeat domain is a potent inhibitor of Sendai virus-cell fusion: an emerging similarity with functional domains of other viruses. EMBO J. 1995;14:5524–5531. doi: 10.1002/j.1460-2075.1995.tb00239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reitter J N, Sergel T, Morrison T G. Mutational analysis of the leucine zipper motif in the Newcastle disease virus fusion protein. J Virol. 1995;69:5995–6004. doi: 10.1128/jvi.69.10.5995-6004.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ruiz-Arguello M B, Goni F M, Pereira F B, Nieva J L. Phosphatidylinositol-dependent membrane fusion induced by a putative fusogenic sequence of Ebola virus. J Virol. 1998;72:1775–1781. doi: 10.1128/jvi.72.3.1775-1781.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanchez A, Kiley M P, Holloway B P, Auperin D D. Sequence analysis of the Ebola virus genome: organization, genetic elements, and comparison with the genome of Marburg virus. Virus Res. 1993;29:215–240. doi: 10.1016/0168-1702(93)90063-s. [DOI] [PubMed] [Google Scholar]
- 40.Sanchez A, Trappier S G, Mahy B W, Peters C J, Nichol S T. The virion glycoproteins Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc Natl Acad Sci USA. 1996;93:3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanchez A, Yang Z-Y, Xu L, Nabel G J, Crews T, Peters C J. Biochemical analysis of the secreted and virion glycoproteins of Ebola virus. J Virol. 1998;72:6442–6447. doi: 10.1128/jvi.72.8.6442-6447.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanger F, Nicklen S, Coulson A R. DNA sequencing with chain-terminating inhibitors. Proc Natl Acad Sci USA. 1977;74:5463–5467. doi: 10.1073/pnas.74.12.5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sodroski J G. HIV-1 entry inhibitors in the side pocket. Cell. 1999;99:243–246. doi: 10.1016/s0092-8674(00)81655-4. [DOI] [PubMed] [Google Scholar]
- 44.Takada A, Robison C, Goto H, Sanchez A, Murti K G, Whitt M A, Kawaoka Y. A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci USA. 1997;94:14764–14769. doi: 10.1073/pnas.94.26.14764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tan K, Liu J-H, Wang J-H, Shen S, Lu M. Atomic structure of a thermostable subdomain of HIV-1 gp41. Proc Natl Acad Sci USA. 1997;94:12303–12308. doi: 10.1073/pnas.94.23.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Volchkov V E, Blinov V M, Netesov S V. The envelope glycoprotein of Ebola virus contains an immunosuppressive-like domain similar to oncogenic retroviruses. FEBS Lett. 1992;305:181–184. doi: 10.1016/0014-5793(92)80662-z. [DOI] [PubMed] [Google Scholar]
- 47.Volchkov V E, Feldmann H, Volchkova V A, Klenk H-D. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci USA. 1998;95:5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weissenhorn W, Dessen A, Harrison S C, Skehel J J, Wiley D C. Atomic structure of the ectodomain from HIV-1 gp41. Nature. 1997;387:426–430. doi: 10.1038/387426a0. [DOI] [PubMed] [Google Scholar]
- 49.Weissenhorn W, Carfi A, Lee K-H, Skehel J J, Wiley D C. Crystal structure of the Ebola virus membrane fusion subunit, GP2, from the envelope glycoprotein ectodomain. Mol Cell. 1998;2:605–616. doi: 10.1016/s1097-2765(00)80159-8. [DOI] [PubMed] [Google Scholar]
- 50.Weng Y, Weiss C D. Mutational analysis of residues in the coiled-coil domain of human immunodeficiency virus type 1 transmembrane protein gp41. J Virol. 1998;72:9676–9682. doi: 10.1128/jvi.72.12.9676-9682.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wild C, Oas T, McDanal C, Bolognesi D, Matthews T. A synthetic peptide inhibitor of human immunodeficiency virus replication: correlation between solution structure and viral inhibition. Proc Natl Acad Sci USA. 1992;89:10537–10541. doi: 10.1073/pnas.89.21.10537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wild C T, Shugars D C, Greenwell T K, McDanal C B, Matthews T J. Peptides corresponding to a predictive (α-helical domain of human immunodeficiency virus type 1 gp41 are potent inhibitors of virus infection. Proc Natl Acad Sci USA. 1994;91:9770–9774. doi: 10.1073/pnas.91.21.9770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wool-Lewis R J, Bates P. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol. 1998;72:3155–3160. doi: 10.1128/jvi.72.4.3155-3160.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang Z, Delgado R, Xu L, Todd R F, Nabel E G, Sanchez A, Nabel G J. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science. 1998;279:1034–1037. doi: 10.1126/science.279.5353.1034. [DOI] [PubMed] [Google Scholar]
- 55.Yao Q, Compans R W. Peptides corresponding to the heptad repeat sequence of human parainfluenza virus fusion protein are potent inhibitors of virus infection. Virology. 1996;223:103–112. doi: 10.1006/viro.1996.0459. [DOI] [PubMed] [Google Scholar]