Abstract
Adverse childhood experiences (ACEs) are consistently found to be negatively associated with physical, psychological, and psychosocial well-being throughout the lifespan. While previous research has established risk factors and noxious outcomes arising post-ACEs, less attention has been given to factors such as resilience, perceived social support, and subjective well-being that may help explain the relationship between ACEs and psychopathology. Hence, the objectives of this study are to examine: (1) the relationships among ACEs and symptoms of anxiety, depression, and suicidality in adulthood, and (2) whether resilience, social support, and subjective well-being mediate the relationship between ACEs and psychopathological symptoms. Cross-sectional data on ACEs, psychological factors, potential mediating variables, and sociodemographic factors were collected from a community sample of adults aged 18–81 (N = 296) via an on-line survey. Endorsing ACEs was significantly and positively correlated with symptoms of anxiety, depression, and suicidality. Results of parallel mediation analyses showed that social support, negative affect, and life satisfaction statistically mediated the relationships between ACEs and psychopathological outcomes in adulthood. These results highlight the importance of identifying potential mediators of the ACEs-psychopathological symptoms relationship to aid in the development of screening and intervention practices that could bolster developmental outcomes following traumatic childhood experiences.
Keywords: ACEs, Anxiety, Depression, Suicidality, Resilience, Social Support, SWB
Introduction
Adverse childhood experiences (ACEs) are categories of events occurring before the age of eighteen years that potentially disrupt optimal developmental trajectories (Felitti et al., 1998). Conceptual definitions of ACEs vary in the literature, though commonly reported events include emotional, physical, and sexual abuse; emotional and physical neglect; parental divorce, mental illness, abandonment, or death; and household dysfunction (Felitti et al., 1998). ACEs represent a broader notion than child abuse and neglect, and often influence familial and social-environmental dynamics extending beyond the individual child (Kalmakis & Chandler, 2014).
The relationships between ACEs, psychopathology, and disrupted developmental pathways throughout the lifespan are well established (Felitti et al., 1998; Sachs-Ericsson et al., 2015; Wilson et al., 2011). While there is preliminary evidence to suggest that resilience, social support, and subjective well-being (SWB) could help explain the relationships between childhood adversity and negative outcomes (e.g., Busseri & Sadava, 2011; Raeye, 2020), research examining these variables as mediators of the relationship between ACEs and psychopathology remains scarce. The goal of the present study is to investigate the potential mediating effects of resilience, perceived social support, and SWB in the relationship between ACEs, symptoms of anxiety and depression, and suicidality, in adults.
A pioneering longitudinal study examining the long-term sequelae of ACEs followed nearly 10,000 participants in North America and found that 67% experienced at least one ACE, and 13% reported four or more (Felitti et al., 1998). The results depicted a dose–response relationship between number of ACEs and likelihood of developing physical, psychiatric, and psychosocial complications in adulthood (Felitti et al., 1998). Considering the deleterious consequences of childhood adversity, it is imperative to examine factors that may explain the link between ACEs and long-term pernicious outcomes, which may provide targets for ameliorating repercussions.
Biological and Cognitive Ramifications of Adversity
The association between ACEs, poor health, and subpar psychosocial outcomes in adulthood is well-documented, although the mechanisms of this relationship are less understood. One proposed mechanism entails the sustained biological and cognitive alterations arising from prolonged periods of stress responses (Evans & Kim, 2013; Teicher et al., 2003). In response to either perceived or objective threatening stimuli, the autonomic and sympathetic nervous systems evoke physiological responses, such as the ‘fight-flight-freeze’ reaction (McCrory et al., 2010). An important structure to this process is the hypothalamic-pituitary-adrenocortical (HPA) axis which releases stress hormones (e.g., cortisol, adrenaline, norepinephrine) into the bloodstream to aid a person in escaping a threatening situation (McEwen, 2005). Excessive production of stress hormones and persistent physiological responses (i.e., allostatic load) induce a wear and tear effect on the body (McEwen, 2000). Chronic stress is associated with chemical imbalances within the brain (Watters & Martin, 2021) and contributes to physical and psychological complexities (McEwen, 2000). Stress accumulation is associated with difficulties in self-regulatory processes, prospective planning and attentional control, and emotion regulation (Evans & Kim, 2013).
Children experiencing prolonged exposure to volatile environments display different neurobiological profiles than children in stable environments (Korotana et al., 2016). These distinct neurobiological profiles and physiological alterations persist into adulthood and promote emotional and behavioral consequences (Teicher et al., 2003). Alongside these biological and cognitive sequelae, there may be additional third variables that may explain the increased risk of developing psychopathology after childhood adversity.
ACEs and Psychopathology
The protracted stress response associated with experiencing adverse events interacts with genetic predispositions and environmental factors (e.g., unstable households, poverty, community violence, discrimination) to influence the development of psychiatric disorders that become especially pronounced in adolescence and adulthood (Sachs-Ericsson et al., 2015). Anxiety, depression, posttraumatic stress disorder, and self-injurious thoughts and behaviors (SITBs) are among the most frequently reported psychological problems following ACEs (Dube et al., 2001; Kendall-Tackett, 2002).
Anxiety
Anxiety disorders share commonalities of excessive fear, worry, uncertainty, and related disturbances in anticipation of potentially threatening events (American Psychiatric Association, 2013). Mersky et al. (2018) report that in a sample of adult survivors of childhood trauma, adversity scores were positively associated with anxiety symptoms, such that individuals with greater recollections of retrospective trauma memories had a lower tolerance for uncertainty and higher rates of clinically significant anxiety. Caravaca-Sanchez et al.’s (2019) results support this association and demonstrate that a higher level of ACEs is correlated with greater rates of anxiety and lower reports of social support.
Depression
Childhood adversity is robustly associated with depressive disorders, which are characterized by depressed mood, irritability, desolate feelings, hopelessness, and cognitive alterations (American Psychiatric Association, 2013). Depressive disorders affect nearly 300 million people worldwide and are leading causes of health and economic burdens, as well as strong predictors of SITBs (World Health Organization, 2017). Several explanations exist for the high frequency of depression among trauma-exposed populations. Surviving adversity is associated with the development of avoidant personality styles that impair relationship development, heightening the vulnerability for depressed affect (Kendall-Tackett, 2002). Trauma is further associated with emotional dysregulation, which predicts disruptions in multiple facets of life (Evans & Kim, 2013). These mechanisms engender biopsychosocial consequences that are risk factors for depression.
Self-Injurious Thoughts and Behaviors (SITBs)
SITBs comprise factors such as non-suicidal self-injury (NSSI; i.e., self-injurious behaviors in the absence of suicidal intent), suicidal ideation (i.e., thoughts about ending one’s life), suicide plans (i.e., formulated strategies for how to end one’s life), suicide attempts (i.e., non-fatal self-injurious behaviors with some intent to die), and completed suicide (i.e., death by suicide; Nock et al., 2008; Silverman, 2006). Estimates suggest that there are roughly twenty-five million non-fatal suicide attempts annually, and over 800,000 suicide deaths each year, corresponding to one person taking their life every forty seconds (World Health Organization, 2014).
Traumatic experiences and psychiatric disorders are salient risk factors for suicidal behaviors (Nock et al., 2008; Sugawara et al., 2012). ACEs, regardless of category, are significant risk factors for suicide attempts, increasing the probability of completion two- to five-fold when compared to the general population (Dube et al., 2001). The high prevalence of psychiatric disorders and SITBs among those with ACEs highlights the necessity to better understand the factors mediating this relationship to provide targets for interventions.
Potential Mediators of ACEs and Psychopathology
Resilience
One potential mediator of the ACEs-psychopathology relationship is resilience. Operational definitions of resilience are varied, but the construct is understood to capture one’s ability to maintain a state of adaptive psychological equilibrium (Bonanno, 2004) and tolerate negative affect (Lyons, 1991) in the face of adverse circumstances. There are consistent negative correlations between adverse childhood events and resilience (Daniel et al., 2020; Kelifa et al., 2020) and between resilience and symptoms of anxiety (Collazzoni et al., 2020) and depression (Min et al., 2012). Diminished resilience is also associated with greater suicide ideation (Cleverley & Kidd, 2011; Liu et al., 2014), greater perceived burdensomeness (Kleiman & Beaver, 2013), and more significant global psychological distress (Vieira et al., 2020). Hence, dampened resilience may partially explain the relationship between ACEs and psychopathology.
Social Support
Social support, defined as the subjective perception or objective reality that one is cared for and loved, esteemed, and is a constituent of a community of mutual obligation (Cobb, 1976), is a buffer against negative effects of adversity (Goswami, 2012). Individuals with high ACE scores may lack social capital, leading to restricted support networks in the form of compassionate family members, peers, mentors, and role models (Raeye, 2020). Limited social networks may arise as ACEs are associated with biological, psychiatric, and social repercussions that diminish one’s ability to effectively cope with internal and external demands, resulting in interpersonal deficits (Sachs-Ericsson et al., 2015). Additionally, trauma exposure is associated with risk-taking and antisocial behaviors which impairs the development and maintenance of supportive social relations (Shonkoff & Garner, 2012).
Subjective Well-Being (SWB)
One common conceptualization of SWB is a tripartite model encompassing life satisfaction, positive affect, and negative affect (Diener, 1984). Life satisfaction, the cognitive judgmental component of SWB, comprises a global cognitive evaluation of life, while the affective components of SWB (i.e., positive and negative affect) relate to one’s positive and negative emotional reactivity. In general, greater SWB is associated with less symptoms of mental illness, better functional and perceived health, and strong social relations and prosocial functioning (Diener et al., 1995; Pressman & Cohen, 2005).
Research suggests that ACEs are negatively correlated with SWB and positively associated with psychological distress (e.g., Corcoran & McNulty, 2018; Wang et al., 2021). For example, Brodski and Hutz (2012) found that adult participants who experienced emotional abuse in childhood were more likely to have lower positive affect, life satisfaction, and self-esteem and higher negative affect. Similarly, Mosley-Johnson et al. (2019) demonstrated that individuals who had greater earlylife adversity had a diminished sense of life satisfaction and social well-being in adulthood.
There is also evidence supporting the inverse relationship between SWB and commonly arising disorders following ACEs, suggesting that well-being diminishes in the presence of anxiety, depression, and SITBs. For example, Malone and Wachholtz (2018) report that in a sample of Mainland Chinese participants, levels of anxiety and depression were negatively related with measures of social, functional, and affective well-being. Depression is strongly linked to reduced ratings of SWB, potentially due to its impact on negative affect (Cavanagh et al., 2003) and resilience (Kelifa et al., 2020).
The Current Study
There are robust relationships between ACEs and negative health and psychosocial outcomes, but research to explain the mechanisms of these relationships is scarce. It is possible that there are third variables accounting for the association between ACEs and the development of anxiety and depressive symptoms, and SITBs. The current study aims to address this gap by examining the mediating effects of resilience, perceived social support, and SWB in the relationship between ACEs and symptoms of anxiety and depression, and components of SITBs in a community sample of adults. Based on previous research, we hypothesize that there will be a dose–response relationship between ACE scores and symptoms of anxiety, depression, and suicidality. Additionally, we predict that resilience, perceived social support, and SWB (i.e., life satisfaction, positive affect, negative affect) will statistically mediate the relationships between ACEs and symptoms of anxiety, depression, and suicidality.
Method
Participants
Participants (N = 296) between the ages of 18 and 81 years (Mage = 41.43, SD = 15.17) were recruited through ResearchMatch.org, which is “a national health volunteer registry that was created by several academic institutions and supported by the U.S. National Institutes of Health as part of the Clinical Translational Science Award (CTSA) program. ResearchMatch has a large population of volunteers who have consented to be contacted by researchers about health studies for which they may be eligible” (ResearchMatch, 2022). Inclusion criteria for the current study include being at least 18 years of age, a resident of the United States, and proficiency in the English language. Embedded within the survey were five items designed to confirm that participants were attentively responding to the questions (e.g., “For psychometric purposes, please select ‘Mildly Disagree’ for this item”). Thirty-three participants (10.0%) from the initial sample of 329 individuals were excluded from the dataset for answering two or more of these items incorrectly. The resulting sample (N = 296) comprised 222 (75.0%) females, 54 (18.2%) males, 13 (4.4%) gender variant/nonconforming individuals, and 2 (0.6%) who responded as “other” or “prefer not to answer.” The majority of the sample identified as White (84.8%). See Table 1 for participant characteristics.
Table 1.
Participant Characteristics (N = 296)
| Characteristic M (SD) N(%) | |||||||
|---|---|---|---|---|---|---|---|
| Age | 41.43 (15.17) | - | |||||
| 18–39 years | - | 150 (50.7) | |||||
| 40–64 years | - | 116 (39.2) | |||||
| 65–81 years | - | 23 (7.6) | |||||
| Missing | - | 7 (2.5) | |||||
| Gender | |||||||
| Male | - | 54 (18.2) | |||||
| Female | - | 222 (75.0) | |||||
| Gender variant/nonconforming | - | 13 (4.4) | |||||
| Other/prefer not to answer | - | 2 (0.6) | |||||
| Missing | - | 5 (1.7) | |||||
| Race/Ethnicity | |||||||
| White | - | 251 (84.8) | |||||
| White and Black/African American (non-Hispanic) | - | 1 (0.3) | |||||
| White and Hispanic/Latinx | - | 5 (1.7) | |||||
| White and American Indian/Alaskan Native | - | 5 (1.7) | |||||
| White and Asian/Asian American/Pacific Islander | - | 4 (1.4) | |||||
| White and Middle Eastern/North African | - | 3 (1.0) | |||||
| White and Jewish | - | 1 (0.3) | |||||
| Black/African American (non-Hispanic) | - | 7 (2.4) | |||||
| Hispanic/Latinx | - | 8 (2.7) | |||||
| Hispanic/Latinx and American Indian/Alaskan Native | - | 1 (0.3) | |||||
| Asian/Asian American/Pacific Islander | - | 3 (1.0) | |||||
| Middle Eastern/North African | - | 1 (0.3) | |||||
| Other/Prefer not to answer | - | 6 (2.0) | |||||
| Education (Years) | 16.02 (3.67) | - | |||||
| Current Psychiatric Diagnosis | |||||||
| Present | - | 243 (82.1) | |||||
| Not present | - | 46 (15.5) | |||||
| Missing | - | 7 (2.4) | |||||
Procedure
The procedures and measures of this on-line study were approved by Fordham University’s Institutional Review Board (IRB no. 1875). All study procedures were compliant with the ethical standards of the Helsinki Declaration of 1975, as revised in 2008. All participants were required to provide electronic consent twice indicating that they understand the sensitive nature of the study, and agree to participate in the study. After providing informed consent, participants completed a battery of self-report measures. The order of assessments was identical for all participants and was presented in the following sequence: Adverse Childhood Experience Questionnaire (ACE-Q; Felitti et al., 1998), Beck Anxiety Inventory (BAI; Beck et al., 1988), Beck Depression Inventory—Second Edition (BDI-II; Beck et al., 1996), Suicidal Behaviors Questionnaire—Revised (SBQ-R; Osman et al., 2001), Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al., 1988), Mentoring Relationship Characteristics (Harris et al., 2009; the data gathered from this scale were not included in the current analyses), Brief Resilience Scale (BRS; Smith et al., 2008), Satisfaction with Life Scale (SWLS; Diener et al., 1985), and the Positive and Negative Affect Schedule Scale (PANAS; Watson et al., 1988). Sociodemographic variables were collected at the end of the questionnaire. All participants were provided with a list of hotlines and text lines that are available 24 hours a day, 7 days a week, as well as a list of mental health resources following the completion of the SBQ-R (Osman et al., 2001), and again after submitting the survey. Upon completion of the study, participants had the opportunity to be entered in a raffle to win one of ten $50 electronic gift cards.
Measures
Each measure described below demonstrates adequate to good reliability (Cronbach’s alphas ranging from 0.74- 0.93). Reliabilities for the current data are presented in the diagonal of the correlation matrix (Table 2).
Table 2.
Descriptive Statistics and Correlations Among Participant Characteristics and Variables of Interest
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Adverse childhood experiences (ACEs) | 3.95 (2.49) | (.74) | ||||||||||||
| 2. Anxiety symptoms | 39.18 (12.00) | .44** | (.92) | |||||||||||
| 3. Depressive symptoms | 46.08 (15.16) | .43** | .67** | (.93) | ||||||||||
| 4. Suicidality | 10.17 (4.81) | .36** | .30** | .48** | (.79) | |||||||||
| 5. Social support | 4.54 (1.51) | -.25** | -.23** | -.46** | -.17** | (.93) | ||||||||
| 6. Resilience | 2.74 (0.98) | -.20** | -.36** | -.45** | -.34** | .22** | (.91) | |||||||
| 7. Life satisfaction | 19.04 (9.61) | -.29** | -.39** | -.63** | -.38** | .55** | .46** | (.89) | ||||||
| 8. Positive affect | 57.74 (17.10) | -.17** | -.28** | -.52** | -.26** | .39** | .48** | .56** | (.88) | |||||
| 9. Negative affect | 54.77 (19.23) | .37** | .64** | .72** | .39** | -.28** | -.48** | -.52** | -.31** | (.89) | ||||
| 10. Years of education | 16.02 (3.67) | -.13* | -.23** | -.23** | -.16** | .10 | .16** | .21** | .48** | -.17** | – | |||
| 11. Age | 41.43 (15.17) | .00 | -.22** | -.10 | -.16** | -.20** | .08 | .01 | .02 | -.18** | .16** | – | ||
| 12. Employment status | .14* | .12* | .10 | .07 | -.15* | -.01 | -.13* | -.12 | .04 | .06 | .42** | – | ||
| 13. Income | -.25** | -.25** | -.36** | -.23** | .20** | .23** | .42** | .26** | -.19** | .26** | .05 | -.23** | – | |
| 14. Psychiatric diagnosis (1 = present; 2 = absent) | -.14* | -.20** | -.19** | -.22** | -.08 | .28** | .08 | .16** | -.28** | .02 | .06 | -.03 | .09 |
Cronbach alphas for the current sample are reported in parentheses along the diagonal
* p < .05; ** p < .01
Adverse Childhood Experience Questionnaire (ACE-Q)
The Adverse Childhood Experience Questionnaire (ACE-Q; Felitti et al., 1998) is a 10-item measure intended to assess the most frequently reported types of childhood adversities (i.e., physical, emotional, and sexual abuse; neglect; parental divorce, mental illness, incarceration, or death; domestic violence; and household substance use) in the literature (Felitti et al., 1998; Wilson et al., 2011). Participants were asked to dichotomously (i.e., yes or no) indicate whether they experienced a category of events prior to turning eighteen years of age. The responses were summed to produce a cumulative ACE score, ranging from 0—10; higher scores are reflective of greater adverse experiences.
Beck Anxiety Inventory (BAI)
The Beck Anxiety Inventory (BAI; Beck et al., 1988) is a 21-item self-report instrument measuring the severity of anxiety symptoms. Participants were asked to indicate whether they have experienced distinct anxiety symptoms within the past month on a 4-point Likert scale, ranging from 0 = “Not at all” to 3 = “Severely—It bothered me a lot.” The total BAI score was calculated by summing responses across the items.
Beck Depression Inventory – Second Edition (BDI-II)
The Beck Depression Inventory—Second Edition (BDI-II; Beck et al., 1996) is a 21-item self-report inventory measuring the severity of depressive symptoms. Participants rated the relevance of a set of statements examining the cognitive, somatic, affective, and debilitating symptoms of depression, as they related to them in the past two weeks. Responses were scored on a 4-point scale for each item, ranging from 0—3. Each of the 21 items were summed to produce a single score for depressive symptomatology.
Suicidal Behaviors Questionnaire-Revised (SBQ-R)
The Suicidal Behaviors Questionnaire—Revised (SBQ-R; Osman et al., 2001) is a 4-item measure assessing four symptoms relating to suicidal ideation and behaviors. Item 1 refers to lifetime suicide ideation and attempt and is scored on a 4-point scale with 1 = “Non-suicidal subgroup” and 4 = “Suicide attempt subgroup.” Item 2 evaluates the frequency of suicidal ideation over the past twelve months. Responses to this item are scored on a 5-point scale with 1 = “Never” and 5 = “Very often (5 or more times).” Item 3 assesses the threat of a future attempt and is scored on a 3-point scale. Lastly, item 4 probes the self-reported likelihood of prospective suicidal behaviors. This item is scored on a 6-point scale, with 0 = “Never” and 6 = “Very likely.” The total SBQ-R score ranges from 3–18; higher scores indicate greater suicidality.
Multidimensional Scale of Perceived Social Support (MSPSS)
Perceived social support was measured with the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al., 1988), which is a 12-item self-report scale of the perceived adequacy of social support that one receives from family, friends, and significant others. Responses are indicated on a 7-point Likert scale ranging from 1 = “Strongly disagree” to 7 = “Strongly agree.” A cumulative social support score is derived from the sum of responses, divided by the number of items answered.
Brief Resilience Scale (BRS)
The Brief Resilience Scale (BRS; Smith et al., 2008) consists of six questions measuring one’s subjective judgments of their ability to bounce back following adversity. Three items are positively worded, and three are negatively worded and reverse scored. Responses range on a 5-point Likert scale with 1 = “Strongly disagree” and 5 = “Strongly agree.” A resilience score was calculated by adding individual responses, ranging from 6–30, and dividing it by the number of items answered. Higher values indicate higher levels of resilience.
Satisfaction with Life Scale (SWLS)
The Satisfaction with Life Scale (SWLS; Diener et al., 1985) is a 5-item scale assessing global cognitive judgments of perceived satisfaction with one’s life. Participants indicated on a 7-point Likert scale how much they agree with statements regarding their life conditions (e.g., “The conditions of my life are excellent”). Responses ranged from 1 = “Strongly disagree” to 7 = “Strongly agree.” The total score was determined by summing the scores of each item.
Positive and Negative Affect Schedule (PANAS) Scale
The Positive and Negative Affect Schedule (PANAS) Scale (Watson et al., 1988) contains 20 items with two subscales that assess positive and negative affect. These items include words that describe feelings and emotions (e.g., positive affect – interested, excited, proud; negative affect – distressed, guilty, irritable). The score for each subscale was calculated by summing the ten positive items, and the ten negative items. Higher values are indicative of higher levels of positive affect and negative affect for each respective subscale. The internal consistency for the PANAS has been shown to range between Cronbach’s α = 0.86—0.90 for the positive affect subscale, and α = 0.84—0.87 for the negative affect subscale (Watson et al., 1988).
Analyses Plan
Pearson bivariate correlations were used to examine the relationships between exposure to ACEs and anxiety, depression, and suicidality symptomatology. The primary analyses utilized parallel mediation, which allows for the examination of multiple mediators and covariates simultaneously. To examine whether resilience, social support, and SWB mediated the relationships between ACEs and symptoms of psychopathology, bootstrapping with the PROCESS macro (version 4.0; Hayes, 2017) in SPSS 25.0 was used. When zero is not included in the 95% confidence intervals for the indirect effect for the mediation analyses, it is interpreted as a significant indirect effect and provides evidence that the variable mediates the relationship.
For each mediation model, covariates were retained if they had zero order correlations with the outcome variable. When anxiety symptoms or suicidality were the outcomes, age, education in years, income, and presence of a psychiatric diagnosis (1 = present; 2 = absent) were included as covariates. When the depressive symptoms variable was the outcome, then education in years, income, and psychiatric diagnosis (1 = present; 2 = absent) were included as covariates.
Results
Of the 296 participants, 25 (8.4%) experienced no adverse childhood events, 34 (11.5%) experienced one ACE, 31 (10.5%) experienced two ACEs, and 206 (69.9%) reported three or more ACEs. One hundred and seventy (57.4%) participants reported suicidal ideation within the past 12 months, 89 (30.0%) disclosed at least one prior suicide attempt, and 33 (11.2%) reported it is likely they will one day attempt suicide.
Correlational Analyses
Results of Pearson bivariate correlational analyses displayed that ACEs were significantly positively associated with symptoms of anxiety (r = 0.44), depression (r = 0.43), suicidality (r = 0.36), and negative affect (r = 0.37) at the p < 0.01 level. ACEs were also significantly negatively correlated with resilience (r = -0.20), social support (r = -0.25), life satisfaction (r = -0.29), and positive affect (r = -0.17) at the p < 0.01 level. Social support and resilience were both negatively correlated with each measure of psychopathological symptoms. See correlation matrix in Table 2.
Mediation Analyses
To examine whether the relationship between ACEs and psychopathology was mediated by resilience, social support, and SWB (life satisfaction, positive affect, and negative affect), bootstrapping was used and the 95% confidence intervals for the unstandardized indirect effects were obtained with 5,000 bootstrap resamples. Parallel mediation analyses were run separately for each outcome (anxiety symptoms, depressive symptoms, and suicidality).
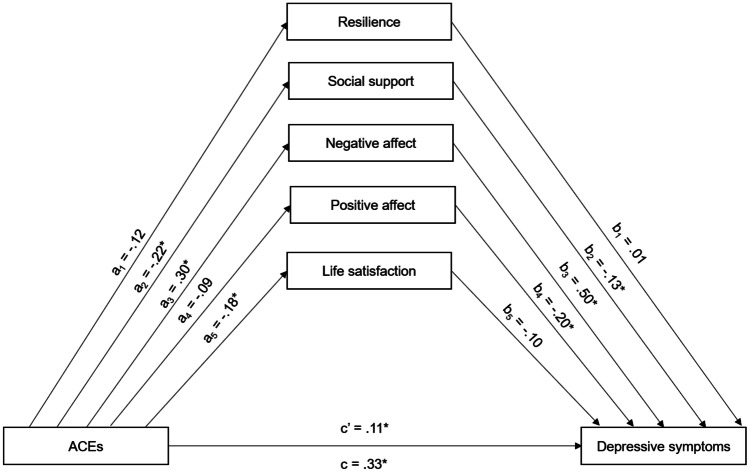
The results of the parallel mediation model predicting depressive symptoms shows that ACEs are indirectly related to depressive symptoms through its relationship with social support and negative affect (see Table 3). A model for the parallel mediation analyses is presented in Fig. 1. Standardized coefficients are provided in Fig. 1 as a heuristic to understanding the magnitude of the effects. Table 3 presents the unstandardized coefficients and the values that are presented throughout the results section are unstandardized unless noted otherwise.
Table 3.
Parallel Mediating Effects of Resilience, Social Support, Negative Affect, Positive Affect, and Life Satisfaction on the Relationship Between ACEs and Psychopathological Symptoms (Values Are Unstandardized Coefficients)
| Effect of ACEs on M | Effect of M on DV | Indirect effect | Total effect | Direct effect | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependent variable (DV) | Mediator (M) | a | SE | b | SE | (a x b) | SE | 95% CI | c | SE | c' | SE |
| aDepressive symptoms | 1.97* | 0.33 | 0.64* | 0.24 | ||||||||
| Resilience | -0.04 | 0.33 | 0.08 | 0.71 | 0.00 | -0.07 | -0.07, 0.07 | |||||
| Social support | -0.13* | 0.04 | -1.34* | 0.45 | 0.18 | 0.08 | 0.04, 0.37 | |||||
| Negative affect | 2.36* | 0.44 | 0.39* | 0.04 | 0.93 | 0.20 | 0.55, 1.34 | |||||
| Positive affect | -0.63 | 0.42 | -0.17* | 0.04 | 0.11 | 0.08 | -0.04, 0.29 | |||||
| Life satisfaction | -0.71* | 0.22 | -0.16 | 0.09 | 0.11 | 0.08 | -0.01, 0.28 | |||||
| bAnxiety | 1.73* | 0.26 | 0.94* | 0.24 | ||||||||
| Resilience | -0.05* | 0.35 | -0.42 | 0.69 | 0.02 | 0.04 | -0.05, 0.12 | |||||
| Social support | -0.13* | 0.04 | -0.39 | 0.45 | 0.05 | 0.06 | -0.06, 0.20 | |||||
| Negative affect | 2.44* | 0.44 | 0.31* | 0.04 | 0.74 | 0.17 | 0.44, 1.10 | |||||
| Positive affect | -0.63 | 0.28 | -0.01 | 0.04 | 0.01 | 0.03 | -0.05, 0.09 | |||||
| Life satisfaction | -0.71* | 0.22 | 0.05 | 0.08 | -0.04 | 0.06 | -0.18, 0.09 | |||||
| bSuicidality | 0.60* | 0.11 | 0.45* | 0.12 | ||||||||
| Resilience | -0.05* | 0.35 | -0.62 | 0.34 | 0.03 | 0.02 | -0.01, 0.09 | |||||
| Social support | -0.13* | 0.04 | 0.11 | 0.22 | -0.01 | 0.03 | -0.08, 0.05 | |||||
| Negative affect | 2.44* | 0.44 | 0.03 | 0.02 | 0.06 | 0.04 | -0.02, 0.15 | |||||
| Positive affect | -0.63 | 0.28 | -0.06 | 0.02 | 0.00 | 0.02 | -0.02, 0.04 | |||||
| Life satisfaction | -0.71* | 0.22 | -0.09* | 0.04 | 0.06 | 0.04 | 0.01, 0.14 | |||||
aYears of education, income, and presence of psychiatric diagnosis included as covariates
bAge, years of education, income, and presence of psychiatric diagnosis were included as covariates; Bolded confidence intervals do not include zero, indicating a significant indirect effect
* p < .05
Fig. 1.
Parallel Mediation Analysis Examining Mediators of the Relationship Between Adverse Childhood Experiences (ACEs) and Depressive Symptoms Note. an is the effect of ACEs on the mediator variable; bn is the effect of the mediator variable on depressive symptoms; c’ is the direct effect of ACEs on depressive symptoms; c is the total effect of ACEs on depressive symptoms. All presented effects are standardized. Years of education, income, and psychiatric diagnosis were included as covariates. *p < .05
The total effect of ACEs on depressive symptoms was significant such that higher levels of ACEs were associated with higher levels of depressive symptoms (cstandardized = 0.33, p < 0.05). Higher ACEs were significantly associated with lower levels of social support and life satisfaction, and higher levels of negative affect. As shown in Table 3, the 95% confidence intervals based on 5,000 bootstrap samples for the unstandardized indirect effects of social support (a*b = 0.18) and negative affect (a*b = 0.93) did not include zero (0.04—0.37 and 0.55—1.34, respectively). The indirect effects through resilience, positive affect, and life satisfaction were not significantly different from zero (see Table 3). After taking into account ACEs indirect effect through all the mediators, the ACEs variable was still a significant predictor of depressive symptoms (c’standardized = 0.11, p < 0.05).
The total effect of ACEs on anxiety symptoms was significant (cstandardized = 0.37, p < 0.05). In the parallel mediation model, only negative affect had a significant effect on anxiety symptoms (b = 0.31, p < 0.05; see Table 3). The 95% confidence interval based on 5,000 bootstrap samples for the unstandardized indirect effect for negative affect (a*b = 0.74) did not include zero (0.44—1.10). The indirect effects through resilience, social support, positive affect, and life satisfaction contained zero in their 95% confidence intervals. After taking into account ACEs indirect effect through all the mediators, the ACEs variable was still a significant predictor of anxiety symptoms (c’standardized= 0.20, p < 0.05).
ACEs were significantly positively associated with suicidality (cstandardized = 0.30, p < 0.05). Life satisfaction was significantly negatively associated with suicidality (b = -0.09, p < 0.05; see Table 3), and the 95% confidence interval based on 5,000 bootstrap samples for the unstandardized indirect effect for life satisfaction (a*b = 0.06) did not include zero (0.01—0.14). The ACEs variable continued to be a significant predictor of suicidality (c’standardized = 0.23, p < 0.01) after taking into account the indirect effect of ACEs through all of the mediators.
Discussion
Childhood adversity exerts a lasting influence on developmental trajectories and health outcomes in adulthood. Individuals with ACEs are predisposed to health-risk behaviors (Chartier et al., 2009), have physiological (Felitti et al., 1998), cognitive, and emotional alterations (e.g., Johnson et al., 2002; Kendall-Tackett, 2002), are at an increased risk of self-injurious thoughts and behaviors (Cleverley & Kidd, 2011; Kleiman & Beaver, 2013) and are more likely than those without ACEs to develop psychiatric disorders (Andersen & Teicher, 2008). The current study investigated the relationships between retrospective reports of ACEs and symptoms of anxiety, depression, and suicidality in adulthood, and examined mediators of the relationship between ACEs and psychopathological symptoms.
Consistent with our first hypothesis, ACEs were significantly positively associated with anxiety, depression, and suicidality symptom severity. These findings are consistent with previous research and suggest that there are factors associated with experiencing adversity that amplify the risk of developing psychopathology in adulthood (Korotana et al., 2016). Suicidality was particularly prominent in our sample as over half of participants reported experiencing suicidal ideation within a 12-month period, and nearly one-third endorsed a history of at least one suicide attempt. Considering that a history of suicide attempts is a robust predictor of recurrent attempts (Chu et al., 2015), and meta-analytic reviews display high rates of non-fatal suicide attempts among the ACEs population (Devries et al., 2014; Evans et al., 2005), there is a pressing need to better understand the pathways by which ACEs predispose people to self-injurious thoughts and behaviors in order to develop targeted suicide prevention strategies.
Partially supporting our second hypothesis, the relationships between ACEs and the outcome variables (anxiety and depressive symptoms, and suicidality) were statistically mediated by social support, negative affect, and life satisfaction. Via parallel mediation analyses, we found significant indirect effects of ACEs through social support and negative affect on depressive symptoms. ACEs significantly indirectly influenced anxiety symptoms through negative affect, and significantly indirectly influenced suicidality through life satisfaction.
Exposure to traumatic events alters one’s cognitive schemas related to the safety of the world (Briere & Elliot, 1994), and contributes to negative self-perceptions, unhelpful thought patterns (Cukor & McGinn, 2006), greater negative affect (Wright et al., 2009), and poor interpersonal relations (Johnson et al., 2002), all of which increase susceptibility to psychopathology (Kendall-Tackett, 2002). The results of the current study support that the relationship between ACEs and negative outcomes can be partially explained by social support, life satisfaction, and lower levels of negative affect, all of which have been conceptualized as protective factors (Larkin et al., 2014; Tabibnia & Radecki, 2018; Wang et al., 2021).
Negative affect has been implicated in numerous mood disorders, especially in depressive disorders (Varma, 2017). Contrarily, positive affect and life satisfaction are inversely related to psychopathology indicators (Etter et al., 2013). The current study is consistent with these previous findings as higher levels of ACEs were associated with lower positive affect and life satisfaction, and greater negative affect. Both life satisfaction and negative affect statistically mediated the ACEs-psychopathological symptoms relationship corroborating the notion that higher SWB may be a protective factor against psychological distress (Busseri & Sadava, 2011). ACEs may shape the development of negative internal working models which may be linked to feelings of worthlessness, helplessness, hopelessness, an impaired view of oneself, and negative cognitive biases (Briere & Elliot, 1994; Korotana et al., 2016). Hence, it may be possible that psychopathology results, at least in part, from the negative affect and subsequent diminished life satisfaction one may experience after adverse events.
Social support is associated with reduced engagement in health-risk behaviors, increases in positive coping and emotion regulation skills, and enhanced feelings of belongingness and community (Tabibnia & Radecki, 2018). ACEs have been shown to impact the development of positive social skills thereby weakening reciprocal relations, which could be a source of protective support (Korotana et al., 2016). Isolation and decreased social connectedness are interconnected with a myriad of negative outcomes, including poor mental health, increased suicidality (Areba et al., 2021), diminished well-being (Chu et al., 2010), and increased delinquent behavior (Turner et al., 2021). Thus, social support could promote adaptive coping mechanisms, less health-risk behaviors, greater help-seeking behaviors, and could be implicated in increasing treatment compliance.
Implications and Future Directions
The current findings augment previous research and highlight that childhood adversity is a public health crisis requiring increased attention and systemic identification and management approaches. Following the original ACE study (Felitti et al., 1998), the field has witnessed a growing urgency to develop feasible, scalable, and empirically supported interventions to surveil for ACEs and mitigate the associated long-term negative health outcomes. In the United States, this has been demonstrated by the increased state-level data collection on ACE prevalence rates and associated chronic disease indicators through the ACE Optional Module in Centers for Disease Control’s Behavioral Risk Factor Surveillance System (BRFSS; Centers for Disease Control & Prevention, 2003). Such surveillance is conducive to monitoring disease burden related to ACEs and has the potential to inform policy and welfare programs. However, despite the continued efforts to better understand the prevalence and impact of ACEs, there are notable gaps in translating knowledge gained from research into clinical practice and policy development and implementation.
The predominant biomedical healthcare model often discounts the role of social determinants, like childhood adversity, in predicting health outcomes (Tink et al., 2017). Primary care settings that track human development from infancy into adulthood are optimal contexts for providing preventative care and interventions for diverse populations. While it has been repeatedly emphasized that educating healthcare providers about the health and psychosocial impacts of ACEs is integral (Dube, 2018), the healthcare system has not widely enacted training curricula on the identification and management of ACEs, and generally has not adopted trauma-informed approaches. Results from the 2013 American Academy of Pediatrics Periodic Survey demonstrated that only 11% of primary care practitioners were strongly or somewhat familiar with the ACE study, and three-quarters of pediatricians had no familiarity with the ACE study and displayed limited knowledge of how ACEs impact health (Kerker et al., 2016).
Several barriers may explain the restricted application of ACEs identification and management practices in primary care. Provider concerns over integrating ACE assessment tools into health assessments include lack of training in ACEs-informed care and limited competency in addressing positive screens (Flanagan et al., 2018), apprehension of causing patients potential discomfort (Rariden et al., 2021), inadequate appointment durations, limited referral resources, and fear of triggering mental health crises (Gillespie & Folger, 2017). Contrary to these concerns, research supports the feasibility of implementing training sessions on ACEs, subsequent health outcomes, and trauma-informed care in healthcare settings. Such efforts have been associated with increased clinician knowledge, competency, confidence, and comfort in screening and addressing the consequences of childhood adversity in a sensitive manner (Rariden et al., 2021). Furthermore, a systematic review examining studies conducted across perinatal, pediatric, and adult primary care settings, as well as patient home and academic settings found that most patients were receptive to ACE screenings as a method of comprehensively assessing general health (Rariden et al., 2021).
As the field continues to evaluate the acceptability and feasibility of integrating ACE assessments into general physical and mental health evaluations, it is paramount to act cautiously and ethically. An important future direction for research is to refine available ACE informed screening instruments to broaden the scope of examined adversities in a culturally competent manner and include assessments of related physical and mental health symptoms. Finkelhor (2018) discusses this goal and recommends that researchers carefully consider how cultural differences impact the understanding of adversity and the motivations to address resultant outcomes. Consideration of what screenings should aim to assess should be taken seriously. The associations between ACEs and negative health outcomes are statistically robust, but there may be additional important mediating processes in these relationships that could serve as effective targets for screening and interventions. Future research should focus on identifying mediating mechanisms and identifying factors that promote well-being following trauma exposure. Such studies should be conducted with longitudinal designs, with more than two data collection timepoints. Most of the research to-date examining the outcomes of ACEs has been cross-sectional, potentially resulting in biased estimates of mediation effects (Cole & Maxwell, 2003). There is an ongoing debate about whether it is more effective to screen for the residues of childhood adversity, such as psychopathological symptoms, to identify and treat at-risk individuals (Finkelhor, 2018).
There also remain questions about the potential iatrogenic effects of ACE positive screens in light of the limited evidence-based interventions for those with clinically significant ACE scores and outcomes (Finkelhor, 2018). Dube (2018) highlights that ACE screenings should not be pursued for the purpose of diagnosis, but rather, should pave the way for positively impacting population level health through trauma-informed secondary and tertiary prevention approaches. Before implementing universal ACE screenings into clinical settings, protocols must be developed to ensure focused follow-up assessments and adequate referrals for those with positive screens. Clinicians are urged to screen patients throughout the lifespan for ACE histories contingent on established relationships with community behavioral health and psychiatry entities, and availability of ample resources to address the needs of trauma-impacted populations (Flanagan et al., 2018). On the basis of the results of the current study and recommendations of previous researchers (Flanagan et al., 2018), clinicians should pair ACE screenings with strengths-based screenings, such as those examining social support availability and life satisfaction, in order to capitalize on existing resources that may be at the disposal of people who screen positive for adversity. Understanding the protective factors available alongside risk factors could frame conversations about intervention plans.
It is cardinal for these comprehensive screenings to be employed only if collaborative community relationships are present among multidisciplinary teams of providers to support ethical post-screening interventions and to minimize potential iatrogenic screening effects. As recommended by Garner et al. (2012), screenings should be complemented with protocols for educating providers on the content being assessed, sharing information with families, ensuring joint action plans for interventions, locating accessible services, and conducting ongoing monitoring of outcomes. Thus, trauma-informed care denotes identifying vulnerability and protective factors, upholding a commitment to providing ongoing evaluation and monitoring of progress, and ensuring equitable access to services designed specifically to address the needs of communities with trauma histories.
Limitations
Several methodological factors of this study limit the inferences that could be drawn from the results. Although each of the measures utilized in this study demonstrated adequate to strong psychometric properties, the paradigm relied on self-report measures of childhood adversity, psychopathological symptoms, resilience, social support, and subjective well-being, which are susceptible to potential biases (e.g., social desirability bias) and recall inaccuracies (e.g., deficits in retrospective recall; limited self-awareness). The cross-sectional data limit our ability to infer causal interpretations and confer the mediational analyses to be statistical, rather than conceptual. Additionally, the recruitment materials for this study specified that early life adversity would be examined, which may have contributed to a self-selecting sample. Lastly, there may also be selection bias in recruitment since the study was conducted over the internet and required access to technology and the internet. Hence, results may not be generalizable to populations disproportionately impacted by ACEs, such as those who are incarcerated or unhoused (Cleverley & Kidd, 2011; Stensrud et al., 2019).
Conclusion
Despite these limitations, this study is one of the first to examine resilience, social support, and subjective well-being as mediators in the relationship between ACEs and psychopathological symptoms in adulthood. The current findings annex valuable evidence about the mechanisms underlying the development of poor psychological and psychosocial outcomes after ACEs, and indicate that perceived social support, negative affect, and life satisfaction statistically mediate the relationships between ACEs and symptoms of psychopathology. The results elucidate protective factors that could be integrated into ACE assessments and implemented into trauma-informed treatment protocols to address the growing concern of physical and mental health problems among populations exposed to ACEs.
Funding
Funding for this project was provided by a Fordham College Lincoln Center Dean’s Undergraduate Research grant to VK.
Data Availability
As per the study protocol approved by Fordham University's Institutional Review Board and the privacy and confidentiality regulations shared with participants in the informed consent form, data are only accessible by the study authors and their affiliated research team.
Declarations
Competing Interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). 10.1176/appi.books.9780890425596
- Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends in Neuroscience. 2008;31:183–191. doi: 10.1016/j.tins.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Areba, E. M., Taliaferro, L. A., Forster, M., McMorris, B. J., Mathiason, M. A., & Eisenberg, M. E. (2021). Adverse childhood experiences and suicidality: School connectedness as a protective factor for ethnic minority adolescents. Children and Youth Services Review, 120, [105637]. 10.1016/j.childyouth.2020.105637
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory-Second Edition Manual. The Psychological Corporation; 1996. [Google Scholar]
- Bonanno GA. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? The American Psychologist. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Briere J, Elliot D. Immediate and long-term impacts of child sexual abuse. The Future of Children. 1994;4(2):54–69. doi: 10.2307/1602523. [DOI] [PubMed] [Google Scholar]
- Brodski SK, Hutz CS. The repercussions of emotional abuse and parenting styles on self-esteem, subjective well-being: A retrospective study with university students in Brazil. Journal of Aggression, Maltreatment & Trauma. 2012;21(3):256–276. doi: 10.1080/10926771.2012.666335. [DOI] [Google Scholar]
- Busseri MA, Sadava SW. A review of the tripartite structure of subjective well-being: Implications for conceptualization, operationalization, analysis, and synthesis. Personality and Social Psychology Review. 2011;15(3):290–314. doi: 10.1177/1088868310391. [DOI] [PubMed] [Google Scholar]
- Caravaca-Sanchez F, Fearn NE, Vidovic KR, Vaughn MG. Female prisoners in Spain: Adverse childhood experiences, negative emotional states, and social support. Health & Social Work. 2019;44(3):157–166. doi: 10.1093/hsw/hlz013. [DOI] [PubMed] [Google Scholar]
- Cavanagh, J. T., Carson, A. J., Sharpe, M., & Lawrie, S. M. (2003). Psychological autopsy studies of suicide: A systematic review. Psychological Medicine, 33(3), 395–405. 10.1017/s0033291702006943 [DOI] [PubMed]
- Centers for Disease Control and Prevention Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the behavioral risk factor surveillance team. Morbidity and Mortality Weekly Report. Recommendations and Reports. 2003;52:1–12. [PubMed] [Google Scholar]
- Chartier MJ, Walker JR, Naimark B. Health risk behaviors and mental health problems as mediators of the relationship between childhood abuse and adult health. American Journal of Public Health. 2009;99(5):847–854. doi: 10.2105/AJPH.2007.122408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu PS, Saucier DA, Hafner E. Meta-analysis of the relationships between social support and well-being in children and adolescents. Journal of Social and Clinical Psychology. 2010;29(6):624–645. doi: 10.1521/jscp.2010.29.6.624. [DOI] [Google Scholar]
- Chu C, Klein KM, Buchman-Schmitt JM, Hom MA, Hagan CR, Joiner TE. Routinized assessment of suicide risk in clinical practice: An empirically informed update. Journal of Clinical Psychology. 2015;71(12):1186–1200. doi: 10.1002/jclp.22210. [DOI] [PubMed] [Google Scholar]
- Cleverley K, Kidd SA. Resilience and suicidality among homeless youth. Journal of Adolescence. 2011;34(5):1049–1054. doi: 10.1016/j.adolescence.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Cobb S. Social support as a moderator of life stress. Psychosomatic Medicine. 1976;38(5):300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Collazzoni A, Stratta P, Pacitti F, Rossi A, Santarelli V, Bustini M, Talevi D, Socci V, Rossi R. Resilience as a mediator between interpersonal risk factors and hopelessness in depression. Frontiers in Psychiatry. 2020;11:10. doi: 10.3389/fpsyt.2020.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran M, McNulty M. Examining the role of attachment in the relationship between childhood adversity, psychological distress and subjective well-being. Child Abuse & Neglect. 2018;76:297–309. doi: 10.1016/j.chiabu.2017.11.012. [DOI] [PubMed] [Google Scholar]
- Cukor D, McGinn LK. History of child abuse and severity of adult depression: The mediating role of cognitive schema. Journal of Child Sexual Abuse. 2006;15(3):19–34. doi: 10.1300/J070v15n03_02. [DOI] [PubMed] [Google Scholar]
- Daniel R, Ring K, Husbands T, Marshall H, Wang J, Shah A, Chan RY. Resilience in the setting of adverse childhood experiences: A cross-sectional study. Clinical Pediatrics. 2020;59(14):1296–1300. doi: 10.1177/0009922820941633. [DOI] [PubMed] [Google Scholar]
- Devries KM, Mak JY, Child JC, Falder G, Bacchus LJ, Astbury J, Watts CH. Childhood sexual abuse and suicidal behavior: A meta-analysis. Pediatrics. 2014;133(5):e1331–e1344. doi: 10.1542/peds.2013-2166. [DOI] [PubMed] [Google Scholar]
- Diener E. Subjective well-being. Psychological Bulletin. 1984;95(3):542–575. doi: 10.1037/0033-2909.95.3.542. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Diener E, Diener M, Diener C. Factors predicting the subjective well-being of nations. Journal of Personality and Social Psychology. 1995;69(5):851–864. doi: 10.1037/0022-3514.69.5.851. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DF, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the lifespan: Findings from the Adverse Childhood Experiences Study. Journal of the American Medical Association. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- Dube SR. Continuing conversations about adverse childhood experiences (ACEs) screening: A public health perspective. Child Abuse & Neglect. 2018;85:180–184. doi: 10.1016/j.chiabu.2018.03.007. [DOI] [PubMed] [Google Scholar]
- Etter DW, Gauthier JR, McDade-Montez E, Cloitre M, Carlson EB. Positive affect, childhood adversity, and psychopathology in psychiatric inpatients. European Journal of Psychotraumatology. 2013;4:1–9. doi: 10.3402/ejpt.v4i0.20771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Hawton K, Rodham K. Suicidal phenomena and abuse in adolescents: A review of epidemiological studies. Child Abuse & Neglect. 2005;29(1):45–58. doi: 10.1016/j.chiabu.2004.06.014. [DOI] [PubMed] [Google Scholar]
- Evans WG, Kim P. Childhood poverty, chronic stress, self-regulation, and coping. Child Development Perspectives. 2013;7(1):43–48. doi: 10.1111/cdep.12013. [DOI] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelhor D. Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse & Neglect. 2018;85:174–179. doi: 10.1016/j.chiabu.2017.07.016. [DOI] [PubMed] [Google Scholar]
- Flanagan T, Alabaster A, McCaw B, Stoller N, Watson C, Young-Wolff KC. Feasibility and acceptability of screening for adverse childhood experiences in prenatal care. Journal of Women's Health. 2018;27(7):903–911. doi: 10.1089/jwh.2017.6649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner AS, Shonkoff JP, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics Early childhood adversity, toxic stress, and the role of the pediatrician: Translating developmental science into lifelong health. Pediatrics. 2012;129(1):e224–e231. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- Gillespie RJ, Folger AT. Feasibility of assessing parental ACEs in pediatric primary care: Implications for practice-based implementation. Journal of Child & Adolescent Trauma. 2017;10(3):249–256. doi: 10.1007/s40653-017-0138-z. [DOI] [Google Scholar]
- Goswami H. Social relationships and children’s subjective well-being. Social Indicators Research. 2012;107:575–588. doi: 10.1007/s11205-011-9864-z. [DOI] [Google Scholar]
- Harris, K. M., Halpern, C. T., Whitsel, E., Hussey, J., Tabor, J., Entzel, P., & Udry, J. R. (2009). The National Longitudinal Study of Adolescent to Adult Health: Research Design. https://addhealth.cpc.unc.edu/documentation/study-design/
- Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). Guilford Publications.
- Johnson JG, Cohen P, Gould MS, Kasen S, Brown J, Brook JS. Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Archives of General Psychiatry. 2002;59(8):741–749. doi: 10.1001/archpsyc.59.8.741. [DOI] [PubMed] [Google Scholar]
- Kalmakis KA, Chandler GE. Adverse childhood experiences: Towards a clear conceptual meaning. Journal of Advanced Nursing. 2014;70(7):1489–1501. doi: 10.1111/jan.12329. [DOI] [PubMed] [Google Scholar]
- Kelifa MO, Yang Y, Carly H, Bo W, Wang P. How adverse childhood experiences relate to subjective well-being in college students: The role of resilience and depression. Journal of Happiness Studies: An Interdisciplinary Forum on Subjective Well-Being. 2020;22(5):2103–2123. doi: 10.1007/s10902-020-00308-7. [DOI] [Google Scholar]
- Kendall-Tackett K. The health effects of childhood abuse: Four pathways by which abuse can influence health. Child Abuse & Neglect. 2002;26(6–7):715–729. doi: 10.1016/s0145-2134(02)00343-5. [DOI] [PubMed] [Google Scholar]
- Kerker BD, Storfer-Isser A, Szilagyi M, Stein RE, Garner AS, O'Connor KG, Hoagwood KE, Horwitz SM. Do pediatricians ask about adverse childhood experiences in pediatric primary care? Academic Pediatrics. 2016;16(2):154–160. doi: 10.1016/j.acap.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, Beaver JK. A meaningful life is worth living: Meaning in life as a suicide resiliency factor. Psychiatry Research. 2013;210(3):934–939. doi: 10.1016/j.psychres.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Korotana LM, Dobson KS, Pusch D, Josephson T. A review of primary care interventions to improve health outcomes in adult survivors of adverse childhood experiences. Clinical Psychology Review. 2016;46:59–90. doi: 10.1016/j.cpr.2016.04.007. [DOI] [PubMed] [Google Scholar]
- Larkin H, Felitti VJ, Anda RF. Social work and adverse childhood experiences research: Implications for practice and health policy. Social Work in Public Health. 2014;29(1):1–16. doi: 10.1080/19371918.2011.619433. [DOI] [PubMed] [Google Scholar]
- Liu DW, Fairweather-Schmidt AK, Roberts RM, Burns R, Anstey KJ. Does resilience predict suicidality? A lifespan analysis. Archives of Suicide Research. 2014;18(4):453–464. doi: 10.1080/13811118.2013.833881. [DOI] [PubMed] [Google Scholar]
- Lyons JA. Strategies for assessing the potential for positive adjustment following trauma. Journal of Traumatic Stress. 1991;4(1):93–111. doi: 10.1002/jts.2490040108. [DOI] [Google Scholar]
- Malone C, Wachholtz A. The relationship of anxiety and depression to subjective well-being in a Mainland Chinese sample. Journal of Religion and Health. 2018;57(1):266–278. doi: 10.1007/s10943-017-0447-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrory E, De Brito SA, Viding E. Research review: The neurobiology and genetics of maltreatment and adversity. Journal of Child Psychology and Psychiatry. 2010;51(10):1079–1095. doi: 10.1111/j.1469-7610.2010.02271.x. [DOI] [PubMed] [Google Scholar]
- McEwen SB. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22:108–124. doi: 10.1016/S0893-133X(99)00129-3. [DOI] [PubMed] [Google Scholar]
- McEwen SB. Stressed or stressed out: What is the difference? Journal of Psychiatry & Neuroscience: JPN. 2005;30(5):315–318. [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, Janczewski CE, Nitkowski JC. Poor mental health among low-income women in the U.S.: The roles of adverse childhood and adult experiences. Social Science & Medicine. 2018;206:14–21. doi: 10.1016/j.socscimed.2018.03.043. [DOI] [PubMed] [Google Scholar]
- Min JA, Jung YE, Kim DJ, Yim HW, Kim JJ, Kim TS, Lee CU, Lee C, Chae, & J. H. Characteristics associated with low resilience in patients with depression and/or anxiety disorders. Quality of Life Research. 2012;22(2):231–241. doi: 10.1007/s11136-012-0153-3. [DOI] [PubMed] [Google Scholar]
- Mosley-Johnson E, Garacci E, Wagner N, Mendez C, Williams JS, Egede LE. Assessing the relationship between adverse childhood experiences and life satisfaction, psychological well-being, and social well-being: United States Longitudinal Cohort 1995–2014. Quality of Life Research. 2019;28(4):907–914. doi: 10.1007/s11136-018-2054-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30(1):133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman A, Baggem CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples. Assessment. 2001;8(4):443–454. doi: 10.1177/107319110100800409. [DOI] [PubMed] [Google Scholar]
- Pressman SD, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Raeye D. Resilience in the setting of adverse childhood experiences: A cross-sectional study. Clinical Pediatrics. 2020;59(14):1296–1300. doi: 10.1177/0009922820941633. [DOI] [PubMed] [Google Scholar]
- Rariden C, SmithBattle L, Yoo JH, Cibulka N, Loman D. Screening for adverse childhood experiences: Literature review and practice implications. The Journal for Nurse Practitioners. 2021;17(1):98–104. doi: 10.1016/j.nurpra.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ResearchMatch. (2022). Researchers Frequently Asked Questions.https://www.researchmatch.org/researchers/faq
- Sachs-Ericsson NJ, Rushing NC, Stanley IH, Sheffler J. In my end is my beginning: Developmental trajectories of adverse childhood experiences to late-life suicide. Aging & Mental Health. 2015;20(2):139–165. doi: 10.1080/13607863.2015.1063107. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):232–246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Silverman MM. The language of suicidology. Suicide and Life-Threatening Behavior. 2006;36(5):519–532. doi: 10.1521/suli.2006.36.5.519. [DOI] [PubMed] [Google Scholar]
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Stensrud RH, Gilbride DD, Bruinekool RM. The childhood to prison pipeline: Early childhood trauma as reported by a prison population. Rehabilitation Counseling Bulletin. 2019;62(4):195–208. doi: 10.1177/0034355218774844. [DOI] [Google Scholar]
- Sugawara N, Yasui-Furukori N, Sasaki G, Umeda T, Takahashi I, Danjo K, Matsuzaka M, Kaneko S, Nakaji S. Relationships between suicidal ideation and the dimensions of depressive symptoms among middle-aged population in Japan. Journal of Affective Disorders. 2012;136(3):819–823. doi: 10.1016/j.jad.2011.09.034. [DOI] [PubMed] [Google Scholar]
- Tabibnia G, Radecki D. Resilience training that can change the brain. Consulting Psychology Journal: Practice and Research. 2018;70(1):59–88. doi: 10.1037/cpb0000110. [DOI] [Google Scholar]
- Teicher MH, Andersen SL, Polcari A, Andersen CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neuroscience and Biobehavioral Reviews. 2003;27(1–2):33–44. doi: 10.1016/S0149-7634(03)00007-1. [DOI] [PubMed] [Google Scholar]
- Tink W, Tink JC, Turin TC, Kelly M. Adverse childhood experiences: Survey of resident practice, knowledge, and attitude. Family Medicine. 2017;49(1):7–13. [PubMed] [Google Scholar]
- Turner D, Wolf AJ, Barra S, Müller M, Gregório Hertz P, Huss M, Tüscher O, Retz W. The association between adverse childhood experiences and mental health problems in young offenders. European Child & Adolescent Psychiatry. 2021;30(8):1195–1207. doi: 10.1007/s00787-020-01608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varma, D. (2017). Relationship of positive and negative affect with depression in clinical and normal group. Psychological and Behavioral Science International Journal, 2(1). 10.19080/PBSIJ.2016.02.555579
- Vieira IS, Pedrotti Moreira F, Mondin TC, Cardoso TA, Branco JC, Kapczinski F, Jansen K, Souza L, da Silva RA. Resilience as a mediator factor in the relationship between childhood trauma and mood disorder: A community sample of young adults. Journal of Affective Disorders. 2020;274:48–53. doi: 10.1016/j.jad.2020.04.011. [DOI] [PubMed] [Google Scholar]
- Wang, P., Kelifa, M. O., Yu, B., & Yang, Y. (2021). Classes of childhood adversities and their associations to the mental health of college undergraduates: A nationwide cross-sectional study. Environmental Health and Preventative Medicine, 26(73). 10.1186/s12199-021-00993-7 [DOI] [PMC free article] [PubMed]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS Scale. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watters ER, Martin G. Health outcomes following childhood maltreatment: An examination of the biopsychosocial model. Journal of Aging and Health. 2021;33(7–8):596–606. doi: 10.1177/08982643211003783. [DOI] [PubMed] [Google Scholar]
- Wilson RK, Hansen JD, Li M. The traumatic stress response in child maltreatment and resultant neuropsychological effects. Aggression and Violent Behavior. 2011;16(2):87–97. doi: 10.1016/j.avb.2010.12.007. [DOI] [Google Scholar]
- World Health Organization . Preventing suicide: A global imperative. World Health Organization; 2014. [Google Scholar]
- World Health Organization. (2017). Depression and other common mental disorders: Global health estimates. Geneva, Switzerland: World Health Organization. License: CC BY-NC-SA3.0IGO.
- Wright MO, Crawford E, Del Castillo D. Childhood emotional maltreatment and later psychological distress among college students: The mediating role of maladaptive schemas. Child Abuse & Neglect. 2009;33(1):59–68. doi: 10.1016/j.chiabu.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Zimet DG, Dahlem WN, Zimet GS, Farley KG. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52(1):30–41. doi: 10.1207/s15327752jpa5201. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As per the study protocol approved by Fordham University's Institutional Review Board and the privacy and confidentiality regulations shared with participants in the informed consent form, data are only accessible by the study authors and their affiliated research team.