Abstract
Suicide prevention efforts generally target acute precipitants of suicide, though accumulating evidence suggests that vulnerability to suicide is partly established early in life before acute precipitants can be identified. The aim of this systematic review was to synthesize evidence on early life vulnerability to suicide beginning in the prenatal period and extending through age 12. We searched PubMed, Embase, PsycNet, Web of Science, Scopus, Social Services Abstracts, and Sociological Abstracts for prospective studies published through January 2021 that investigated early life risk factors for suicide mortality. The search yielded 13,237 studies; 54 of these studies met our inclusion criteria. Evidence consistently supported the link between sociodemographic (e.g., young maternal age at birth, low parental education, higher birth order), obstetric (e.g., low birth weight), parental (e.g., exposure to parental death by external causes), and child developmental factors (e.g., exposure to emotional adversity) and higher risk of suicide death. Among studies that also examined suicide attempt, there was a similar profile of risk factors. We discuss a range of potential pathways implicated in these associations and suggest that additional research be conducted to better understand how early life factors could interact with acute precipitants and increase vulnerability to suicide.
Keywords: suicide, prenatal, childhood, longitudinal, cohort
Introduction
Nearly 900,000 people die by suicide every year worldwide [67], reinforcing the urgency for more effective prevention strategies [16, 51, 61]. A challenge to improving suicide prevention strategies is the difficulty in identifying effective targets for early intervention in the general population [7, 32]. A greater understanding of the many unfolding developmental factors that contribute to the etiology of suicide, possibly decades before high-risk groups can currently be identified, would contribute to this effort [15, 40, 99].
To date, most work has focused on the prevention of suicide among high-risk groups (e.g., psychiatric patients) through addressing acute precipitants of suicide risk [21]. However, at the population level, most suicides do not occur among high-risk groups; for example, psychiatric disorders account for less than half of the attributable risk for suicide [59, 98]. Therefore, etiologic research on suicide would benefit from better understanding of how vulnerability to suicide is established prior to acute precipitants in high-risk groups.
Similar to psychiatric conditions [36, 62, 72, 77, 89] such as depression [13, 96], psychosis [26], and disruptive behavior disorders [57, 90], suicidality is a life course problem [22]. Vulnerability to suicide is partly established very early in development and may amplify the effects of acute risk factors for suicide during adolescence or adulthood. Yet, early life vulnerability to suicide is not adequately understood. Recently, Orri et al. [73] conducted a meta-analysis of prospective studies on in utero and perinatal risk factors for suicide and found that fetal growth (e.g., low birthweight, small for gestational age) and sociodemographic factors at birth (e.g., older birth order, young mother age, single marital status, low parental education) were associated with suicide mortality. Their meta-analysis demonstrates the importance of early life vulnerability during the prenatal and perinatal periods. As this vulnerability likely extends into early childhood, we conducted a systematic review of the literature on early life vulnerability to suicide encompassing exposures from the prenatal period through 12 years of age. This age precedes the emergence of suicidal thoughts and behaviors taking place during adolescence and young adulthood [12, 53]. Most studies examining childhood risk factors for suicide tend to include ages up to 18 years [e.g., 4], though there is likely significant heterogeneity between childhood and adolescent risk factors. By examining risk factors through 12 years of age, we aim to better understand how vulnerability to suicide that is established in childhood contributes to the risk of suicide mortality starting in adolescence and extending into adulthood. While our main focus is on suicide mortality, we also describe findings from studies that analyzed childhood risk factors for both suicide mortality and suicide attempt in order to evaluate the comparative effects of risk factors between suicide attempt and suicide death.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [75] was used to develop a protocol a priori (available in the Online Resource) and for reporting this systematic review.
Inclusion and exclusion criteria
We sought to identify longitudinal studies that examined early life risk factors for suicide mortality satisfying the following inclusion criteria: (1) prospective design or assessment of hypothesized risk factors prior to suicide; (2) suicide death was identified through medical registry or death certificate; (3) hypothesized risk factors occurred between the prenatal period and childhood (up to 12 years of age); (4) published in a peer-reviewed journal; and (5) written in English. We excluded studies that: (1) collected information on childhood exposures after the suicide death occurred (e.g., retrospective or psychological autopsy studies); (2) examined exposures that occurred after 12 years of age only; (3) did not differentiate suicide death from suicide ideation, plan, or attempt; (4) was not an original empirical investigation; and (5) was written in a language other than English.
Search strategy
We searched PubMed (US National Library of Medicine), Embase (Elsevier), PsycNet (PsycINFO and PsycArticles [American Psychological Association]), Web of Science: Core Collection (Clarivate Analytics), Scopus (Elsevier), Social Services Abstracts (ProQuest), and Sociological Abstracts (ProQuest) in November 2019 and January 2021 and limited to only the English language. The search strategies were developed in consultation with the study authors and run by a biomedical librarian (AAL) in the databases selected. A combination of controlled vocabulary terms (e.g., MeSH, EMTREE, APA Thesaurus of Psychological Index Terms) and text words related to suicide, risk factors, early life, and prospective designs were used (see Online Resource). The search results were exported to EndNote X9 (Clarivate Analytics) and duplicate citations identified and removed. We also scanned the reference lists of included studies, relevant reviews, and meta-analyses identified through the search.
Study selection process
First, each article title and abstract were screened independently by two investigators (PVR, TG, JY, RG, MG, RP, KM, DLH, SEG) using the established eligibility criteria in Covidence (Veritas Health Innovation) for possible inclusion in full text screening. In cases of disagreement, a third investigator reviewed the record (SEG, DLH) and a consensus on inclusion was reached by discussion among the three reviewers. Next, after obtaining the full text of all selected articles, two investigators (PVR, TG, JY, RG, MG, RP, KM, DLH, SEG) screened each full text against the inclusion and exclusion criteria. Reasons for excluding a study were recorded. Disagreements were resolved through discussion with a third reviewer (SEG, DLH) prior to making the final decision.
Data extraction
Data extraction was conducted manually by two investigators (PVR, TG). For each study we extracted, if available, the study characteristics (including the study design, number of suicide deaths, age range of follow-up period, and certification method of suicide death) and exposure information. We also extracted the relevant effect sizes for prenatal and childhood exposures and information on adjustment variables.
Risk of bias assessment
Risk of bias for individual studies was conducted using the Newcastle-Ottawa Assessment Scale for observational studies [102]. For cohort studies we rated selection of participants and exposures, comparability of exposed and non-exposed, and outcome assessment and length/adequacy of follow-up period. For case-control studies, we rated selection of cases and controls, comparability of cases and controls, and characteristics related to exposure. The maximum score that could be awarded was 9, with higher scores indicating lower risk of bias. Quality scores were independently generated by two researchers (PVR and TG). Conflicts were resolved through a third investigator (SEG).
Results
Study selection
Figure 1 displays the flow of information for this systematic review. The database searches returned 26,944 records and an additional 8 records were retrieved through reviewing the reference lists. After 13,715 duplicates were removed, the titles and abstracts of 13,237 articles were screened for relevance of which 12,970 articles were excluded, and 267 articles were retained for full text review. Of the 267, 4 full texts were not available; thus only 263 full texts were screened. After examining the full text, 208 further articles were excluded (see Figure 1 for specific reasons), and 54 studies from 26 independent samples were included in the review [1, 2, 8–10, 17–20, 23–25, 29, 30, 34, 39, 44–47, 50, 54–56, 58, 63–66, 68–71, 74, 78–88, 91, 93, 95, 97, 100, 101, 103–105].
Fig 1.
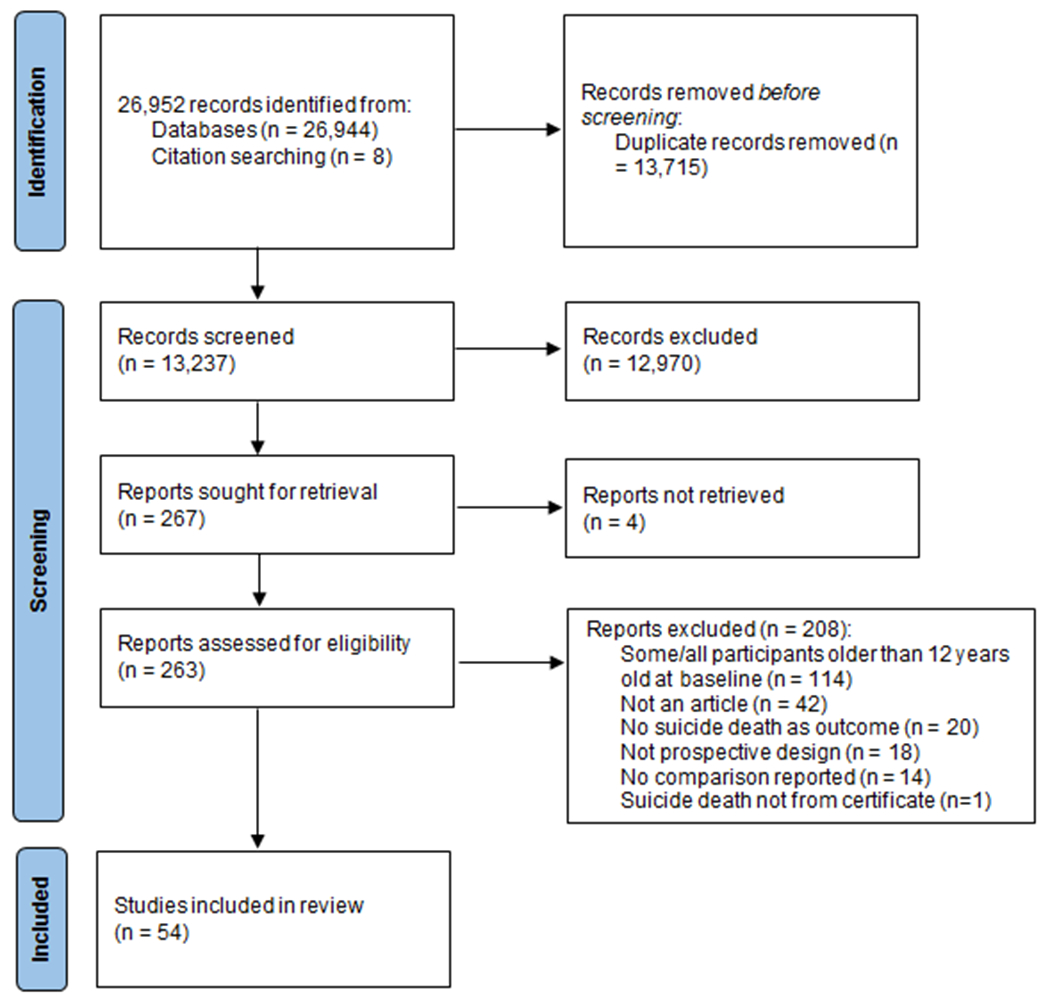
PRISMA flow diagram
Study characteristics
The characteristics of these studies, including the list of risk factors examined and a summary of main findings for each factor examined, can be found in Table 1. Exposure information was divided in four broad domains: 1) sociodemographic factors, 2) pregnancy or delivery factors, 3) parental factors (including factors related to health and stress exposure) and 4) child factors ([including factors related to health, neurodevelopment, and emotional adversity in offspring). Fifty studies used a cohort design, whereas 4 studies used a case-control design. The factors most frequently examined were sociodemographic (n=36, 67%), and pregnancy and delivery factors (n=22, 41%); very few studies looked at parental (n=7) or child factors (n=6) occurring between birth and 12 years of age. Findings by domain are described in the next sections. Fifteen of the 54 studies (28%) also examined associations with suicide attempt as a separate outcome, which we describe separately below.
Table 1.
Characteristics of studies included in the review.
| Study | Cohort name/design, study sample (n) | ICD codes of causes of death counted as suicides; Number of suicide deaths (n) | Age range at follow-up, years | Exposures | Summary of Findings |
|---|---|---|---|---|---|
| Alaraisanen, et al. [2] | Northern Finland Birth Cohort 1966, covering all live births in Finland in 1966 (n=10,742) | Intentional self-harm (ICD-8/9: E950-E959; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0) (n=69) |
16 to 39 | SOCIODEMOGRAPHIC: Maternal age, single marital status, paternal SES, birth order. PREGNANCY/DELIVERY: Unwanted pregnancy, smoking during pregnancy, maternal antenatal depressed mood. | SOCIODEMOGRAPHIC: Maternal age at birth under 20 (vs. 20-34) associated with higher suicide risk (OR=2.20 [1.02-4.73]) in male offspring but not in female offspring. PREGNANCY/DELIVERY: No associations found. |
| Al-Haddad, et al. [1] | Birth cohort of all individuals born in Sweden between 1973-2014 (n=1,791,520) | Intentional self-harm (ICD-8: E950, E950.9, E952.9, E953.9, E954.9, E955.9, E956.9, E957.9, E958.9, E959.9; ICD 9: E950-E959; ICD 10: X60-X84) (n=not provided) | Birth to 41 | PREGNANCY/DELIVERY: Hospitalization during pregnancy with any maternal infection, severe maternal infection, urinary tract infection. | PREGNANCY/DELIVERY: Exposure to infection during fetal life associated with higher suicide risk (data not shown). |
| Bjorkenstam, et al. [8] | Birth cohort of individuals born in Sweden between 1987-1991 (n=548,721) | Intentional self-harm (ICD-10: X60-X84); Injury of undetermined intent (ICD-10: Y10-Y34) (n=431) |
15 to 24 | SOCIODEMOGRAPHIC: Parental education c, foreign-born parent. | SOCIODEMOGRAPHIC: No associations found. |
| Bjorksten and Bjerregaard [9] | Birth cohort of individuals in Greenland who died by suicide and were born in Traditional Lifestyle period (1903-1950), Transition period (1951-1960), and Modern Lifestyle period (1961-1980) (n=118,648) |
Intentional self-harm (ICD-8: E950.3-950.9, E951.1, E953.0, E954.0, E955.0, E956.0, E957.0, E958.0, E959.0; ICD-10: X60-65, X70-74, X78, X80, X83.0) (n=274 Traditional; n=317 Modern; n=317 Transition) |
17 to 84 (Traditional); 14 to 53 (Transition); 11 to 46 (Modern) a | PREGNANCY/DELIVERY: Month of birth. | PREGNANCY/DELIVERY: Season of birth in suicide victims born in three different life periods not associated with suicide risk in the Transition and Modern Lifestyle period. Spring born in the Traditional Lifestyle period (vs. other months) associated with higher suicide risk (N=274; r=0.17; Z=8.11; p<0.001). |
| Bjorngaard, et al. [10] | Birth cohort, with sibling comparison, of individuals born in Norway between 1967-1996. (n=1,690,306) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-84) (n=5,388) |
12 to 41 | SOCIODEMOGRAPHIC: Maternal age, single marital status, maternal education, paternal education, birth order. | SOCIODEMOGRAPHIC: Maternal age under 20 (vs. 20-24) associated with higher suicide risk in offspring population sample (OR=1.35 [1.19-1.54]). Also vs. 25-29, 30-34, and >34. Maternal age under 20 (vs. 25-29) associated with higher suicide risk in offspring siblings’ subsample (OR=1.39 [1.01-1.92]). Also vs. 30-34, and 34. Maternal marital status other than married or cohabiting at birth associated with higher suicide risk in offspring (HR=1.50 [1.34-1.68]). Parental primary/lower secondary education (vs secondary/college) at the time of birth associated with higher suicide risk (maternal education, HR=1.10 [1.10-1.20]; paternal education, from HR=1.13 [1.05, 1.25] to HR=1.33 [1.18, 1.49]). Second, third and ≥4th birth order (vs. first) associated with higher suicide risk (from HR=1.50 [1.37-1.65] to HR=2.11 [1.81-2.47]). |
| Burrell, et al. [17] | Nested case-control study in a birth cohort of individuals in Norway who experienced parental death due to external causes with suicides occurring between 1992 and 2012. (n=7,875) |
Intentional self-harm (ICD-8/9: E95; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0) (n=375) |
12 to 65 | SOCIODEMOGRAPHIC: Foreign-born. PARENTAL FACTORS: Child’s age at parental death. |
SOCIODEMOGRAPHIC: Foreign-born child (vs. native Norwegian) associated with higher suicide risk (OR=1.55 [1.06-2.26]). PARENTAL FACTORS: Exposure to parental death by external causes between ages 0-12 (vs. age 45-65) associated with higher suicide risk (OR=1.82 [1.05-3.13]). |
| Burrell, et al. [18] | Nested case-control study in a birth cohort of individuals in Norway with suicides occurring between 1969 and 2012 (n=351,061) |
Intentional self-harm (ICD-8/9: E95; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0) (n=19,015) |
11 to 64 | PARENTAL FACTORS: Child’s age at parental death. | PARENTAL FACTORS: Exposure to parental death by external causes between ages 0-9 (OR=2.31 [1.74-3.05]), 10-17 (OR=3.06 [2.53-3.72]), 18-24 (OR=2.13 [1.74-2.61]), 25-44 (OR=1.86 [1.58-2.18]), but not between ages 45-64 associated with higher suicide risk. |
| Calvin, et al. [19] | Birth cohort of individuals born in Scotland in 1936 and who were participants in the Scottish Mental Survey in 1947 (n=65,765) |
Intentional self-harm (ICD-6/7: E970-E979; ICD-8/9: E950-E959; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87); Injury of undetermined intent (ICD-8/9: E980-E989; ICD-10: Y10-Y34); Sequelae of events of undetermined intent (ICD-10: Y87.2); Sequelae of unspecified external cause (ICD-10: Y89.9) (n=144 for suicide; n=220 for suicide including undetermined intent) b |
11 to 79 | CHILD FACTORS: Intelligence at age 11. | CHILD FACTORS: General intelligence examined at age 10-11 not associated with suicide risk in the entire sample or women, but higher intelligence scores associated with lower suicide risk in men (HR=0.80 [0.66-0.96]). |
| Chen, et al. [20] | Nested-case control study in a birth cohort of live births in Taiwan registered between 1978-1993 with suicides occurring between 1993-2008 (n=5,654,833) |
Intentional self-harm (ICD-9: E950-E959); Injury of undetermined intent (ICD-9: E980-E989); Accidental poisoning by pesticide (ICD-9: E863); Accidental suffocation (ICD-9: E913) (n=3,984) |
15 to 30 a | SOCIODEMOGRAPHIC: Maternal age, single marital status, parental education, birth order, sibship size. | SOCIODEMOGRAPHIC: Maternal age at birth under 20 and 20-24 (vs. 25-29) associated with higher suicide risk (<20, OR=1.65 [1.44-1.89], 20-24, OR=1.20 [1.11-1.30]). Single maternal marital status at birth associated with higher suicide risk in offspring (OR=1.76[1.31-2.35]). Paternal education ≤6 years and between 7-9 years (vs >12) associated with higher suicide risk for male (≤6, OR=1.22 [1.06-1.40]; 7-9, OR=1.21 [1.05-1.39] but not female offspring. Maternal education not associated with suicide risk. Second, third and ≥4th birth order (vs. first) associated with higher suicide risk (from HR=1.23 [1.13-1.33] to HR=1.45 [1.28-1.65]). |
| Class, et al. [23] | Birth cohort of singleton offspring born in Sweden between 1973-1997 (n=2,155,221) |
Intentional self-harm (ICD-8/9: E950-959; ICD-10: X60-84); Injury of undetermined intent (ICD-8/9: E980-989; ICD-10: Y10-34); Sequelae of intentional self-harm, assault (ICD-10: Y87.0); Sequelae of injury of undetermined intent (ICD-10: Y87.2) (n=1,751) |
12 to 35 | PREGNANCY/DELIVERY: Prenatal stress exposure. PARENTAL FACTORS: Preconception maternal stress exposure, postnatal maternal stress exposure. | PREGNANCY/DELIVERY: No associations found. PARENTAL FACTORS: Death of mother’s first degree relative during first year, but not during first two years and second year, associated with higher suicide risk (HR=1.52 [1.09-2.12]). |
| Cnattingius, et al. [24] | Pregnancy cohort, with sibling comparison, of Swedish offspring born between 1983-1996 (n=1,449,333) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34) (n=374) |
10 to 24 | SOCIODEMOGRAPHIC: Maternal age, paternal age, single marital status, maternal education, birth order, foreign-born mother. PREGNANCY/DELIVERY: Maternal smoking, hypertensive disease, placental abruption, mode of delivery, gestational age, birth weight-for-gestational age, birth length, head circumference. | SOCIODEMOGRAPHIC: Maternal age at birth under 20 (vs. 25-29) associated with higher suicide risk (HR=2.47 [1.65-3.69]). Maternal age between 30 and 34 (vs. 25-29) associated with lower suicide risk (HR=0.73 [0.54-0.98]). Paternal age at birth <19 and between 20-24 years (vs. 25-29) associated with higher suicide risk (<19, HR=4.02 [1.77-9.17]; 20-24, HR=1.44 [1.02-2.04]). Not living with father-to-be associated with higher suicide risk in offspring (HR=1.54 [1.05-2.25]). Maternal education between 13-24 years (vs. 10-12) associated with lower suicide risk (HR=0.61 (0.43-0.87]) in offspring. Having a mother born in another Nordic country other than Sweden associated with higher suicide risk (HR=1.65 [1.14-2.37]). PREGNANCY/DELIVERY: Maternal smoking of 1-9 cigarettes and ≥ 10 cigarettes (vs. none) as assessed at the first visit to antenatal care associated with higher suicide risk (1-9 cigarettes, HR=1.81 [1.40-2.35]); ≥ 10 cigarettes, HR=1.78 [1.31-2.42]). |
| Danziger, et al. [25] | Uppsala Birth Cohort Study, all births that occurred at the Uppsala University Hospital in Sweden between 1915 and 1929. (n=11,650) |
Intentional self-harm (ICD-7: E970-979; ICD-8/9: E950-959; ICD-10: X60-84); Injury of undetermined intent (ICD-8/9: E980-989; ICD-10: Y10-34) (n=161) |
31 to 87 | SOCIODEMOGRAPHIC: Maternal age, single marital status, SES, birth order. PREGNANCY/DELIVERY: Birth weight-for-gestational age, birth length, gestational age. | SOCIODEMOGRAPHIC: No associations found. PREGNANCY/DELIVERY: No associations found. |
| Ekblad, et al. [29] | Birth cohort of all singletons born in Finland between 1987-1989 with information on prenatal smoking exposure (n=175,869) |
Intentional self-harm (ICD-10: X60-X84) (n=64) |
Birth to 20 | PREGNANCY/DELIVERY: Maternal smoking. | PREGNANCY/DELIVERY: No associations found. |
| Ekeus, et al. [30] | Birth cohort of Swedish singletons born to primiparas women between 1973-1979 (n=292,129) |
Intentional self-harm (ICD-10: X60-X84); Injury of undetermined intent (ICD-10: Y10-Y34); Accidental poisonings (ICD-9: E850-E859); Accidental falls (ICD-9: E880-E889) (n=333) |
8 to 29 | SOCIODEMOGRAPHIC: Maternal age. |
SOCIODEMOGRAPHIC: Maternal age at birth between 12 and 19, 20-24, 30-34, and ≥35 (vs. 25-29) associated with higher suicide risk (12-19, RR=2.4 [1.7-3.3]; 20-24, RR=1.5 [1.1-1.9]; 30-34, RR=1.7 [1.1-2.6]; ≥35, RR=2.0 [1.0-3.8]) |
| Geoffroy, et al. [34] | 1958 Birth Cohort, comprising births in England, Scotland, and Wales during 1 week in March 1958 (n=16,470) |
Intentional self-harm (ICD-9: E950-959; ICD-10: X60-84); Injury of undetermined intent (ICD-9: E980-989; ICD-10: Y10-34) (n=51) |
Birth to 50 | SOCIODEMOGRAPHIC: Maternal age, single marital status, paternal SES, birth order, absence of basic amenities, domestic tension, institutional care, contact with social services. PREGNANCY/DELIVERY: Birth weight, maternal smoking. PARENTAL FACTORS: Parental death. CHILD FACTORS: Childhood behavior (internalizing/externalizing), neglect appearance, peer bullying, number of emotional adverse experiences, arithmetic skills, reading skills, bladder control. | SOCIODEMOGRAPHIC: Maternal age over 29 years (vs. 20-29) associated with lower suicide risk (HR=0.44 [0.21-0.92]). Residing in institutional care by age 7 associated with higher suicide risk (HR=4.22 [1.51-11.76]). Contact with social services by the age of 7 reported by health visitors associated with increased suicide risk (HR=1.80 (1.17-2.76]). PREGNANCY/DELIVERY: Birth weight under 2500g (vs. ≥2500g) associated with higher suicide risk (HR=2.47 [1.05-5.81]). PARENTAL FACTORS: Exposure to parental death of any cause by age 7 associated with higher suicide risk (HR=4.52 [1.40-14.59]). CHILD FACTORS: Mother report whether their child had been bullied by peers at 7 years associated with higher suicide risk (HR=2.84 [1.16-6.96]). More than 3 emotional adverse experiences, including reports at 7 years of parental death, neglected appearance, domestic tension, institutional care, contact with social services, parental divorce or separation, and frequent bullying, is associated with higher suicide risk (HR=3.12 [1.01-9.62]). |
| Gravseth, et al. [38] | Birth cohort of Norwegians born between 1967-1976 who were alive and had not emigrated by January 1st of the year of their 19th birthday (n=610,359) | Intentional self-harm (ICD-9: 950-959; ICD-10: X60-X84) (n=1,406) |
19 to 37 | SOCIODEMOGRAPHIC: Parental education, birth order. | SOCIODEMOGRAPHIC: Primary or lower secondary parental education (vs. post/graduate) in the highest educated parent associated with higher suicide risk (HR=1.58 [1.20-2.08]) in offspring. Being second, third and ≥5th born (vs. first) associated with higher suicide risk (from HR=1.20 [1.04-1.38] to HR=1.57 [1.21-2.04]). |
| Hjern and Allebeck [43] | Birth cohort of children born between 1968-1979 and living in family households in 1985 census (youth group) and their parents born between 1929-1965 (parent group) All had to be living in Sweden for at least 5 years. (n=1,250,000 youth group; n= 1,470,000 parent group) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34) (n=1,159 youth group; n= 2381 parent group) |
11 to 30 (youth group) 25 to 69 (parent group) |
SOCIODEMOGRAPHIC: Foreign-born parents, parents of intercountry adoptees, intercountry, foreign-born children, second generation immigrants. | SOCIODEMOGRAPHIC: Compared to Swedish-born with two Swedish-born parents, higher suicide risk was associated with being an intercountry adoptee (OR=4.5 [3.2-6.4]), and a second-generation immigrant from Finland (OR=2.0 [1.5-2.6]), Western Europe (OR=2.2 [1.2-3.4]) or Western Europe/Sweden (OR=1.5 (1.1-2.1]). |
| Hjern, et al. [44] | Birth cohort of individuals born between 1970-1979 who were still alive and residents of Sweden in 1985. (n=871,088) | Intentional self-harm (ICD-9: 950-959); Injury of undetermined intent (ICD-9: 980-989) (n=465) |
7 to 25 | SOCIODEMOGRAPHIC: Foreign-born. | SOCIODEMOGRAPHIC: First-generation immigrants from Finland and Southern Europe (vs. Swedish-born) associated with higher suicide risk (Finland, OR=1.6 [1.3-1.9]; Southern Europe, OR=1.3 [1.0-1.6]). |
| Hjern, et al. [46] | Birth cohort of Swedish residents born between 1973-1982 who had settled in Sweden before 7 years of age and were living in family households in 1990 census. (n=989,871) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34) (n=788) |
13 to 27 | SOCIODEMOGRAPHIC: Foreign-born, long term foster care (in foster care for at least 2 years before 13th birthday), other child welfare recipients (at least one child before they were 13). | SOCIODEMOGRAPHIC: Compared to general population, higher suicide risk was associated with being an intercountry adoptee before age 7 (OR=3.5 [2.3-5.0]) and in long term foster care (> 2 years before 13th birthday) (OR=4.3 [2.8-6.6]) Child welfare recipients before their 13th birthday, including temporary placements in foster or residential care for less than two years to regular support by an adult outside of the family, associated with higher suicide risk (OR=2.7 [1.9-3.9]). |
| Hjern, et al. [45] | Birth cohort of individuals born between 1972-1986 who were alive and residents in Sweden on their 18th birthday. (n=1,466,707) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34) (n=4,523) |
18 to 44 | SOCIODEMOGRAPHIC: Foreign-born, age at adoption. | SOCIODEMOGRAPHIC: International adoptees adopted before their 9th birthday (vs. Swedish-born) associated with higher suicide risk (from RR = 1.48 [1.15-1.81[ to RR = 2.33 [1.92-2.75]). |
| Jacobson and Bygdeman [48] | Case-control study with sibling comparison of adults who died by suicide by violent means between 1978-1995, and who were born in one of seven hospitals in Stockholm, Sweden between 1945-1980. | ICD codes not specified (n=242) |
Birth to 50 | PREGNANCY/DELIVERY: Complication score, presentation other than vertex, stained meconium-stained amniotic fluid and membranes, instrumental delivery or internal version, emergency caesarean section, resuscitation, other complication, number of times opiates were given within 24 hours before birth recorded. | PREGNANCY/DELIVERY: Birth-related trauma events, both single and multiple (vs. none) associated with higher suicide risk in males (Single, OR=2.2 [1.3-3.6]; Multiple, OR=4.9 [1.8-13]) but not females. Presentation other than vertex associated with higher suicide risk (offspring to sibling ratio=2.7, p=0.02). Resuscitation associated with higher suicide risk (offspring to sibling ratio=2.2, p=0.04). Other birth complications associated with higher suicide risk (offspring to sibling ratio=3.1, p=0.002). Mothers given, on average, fewer doses of opiates (50-100 mg pethidinehydrochloride or 15-20 mg morphine) within 24 hours before birth associated with higher suicide risk (data not shown). |
| Korhonen, et al. [53] | Case-control study of patients with cancer who were diagnosed in Denmark, Finland and Sweden before age 20 between 1971-2009 and matched comparison subjects from the Socioeconomic Consequences in Adult Life after Childhood Cancer in Scandinavia (SALiCCS) research program. (n=175,567) |
Intentional self-harm (ICD 8/9: E950-E959; ICD 10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0) (n=390) |
Birth to 59.1 (cancer Patients) Birth to 58.8 (population-based sample) |
CHILD FACTORS: Patient age at diagnosis of cancer. | CHILD FACTORS: Age at cancer diagnosis between 15-19, but not between ages 0-4, 5-9, and 10-14, associated with suicide risk (RR=1.61 [1.09-2.39]). |
| Lahti, et al. [54] | Helsinki Birth Cohort Study, a birth cohort of singleton live births in Finland at 2 public maternity hospitals in Helsinki, Finland between 1934-1944 . (n=12,597) |
Intentional self-harm (ICD-8/9: E95; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0); Other symptoms and signs involving emotional state (ICD-10: R45.8) (n=126) |
29 to 70.5 | PREGNANCY/DELIVERY: Gestational age, birthweight-for-gestational-age. | PREGNANCY/DELIVERY: Gestational age was calculated by subtracting the date of birth from mothers’ self-reported date of last menstrual period. Gestational age between 34-36 weeks (vs. 37-41 weeks) associated with higher suicide risk in males but not females (HR=2.01 [1.03-3.90]). |
| Lahti, et al. [55] | Helsinki Birth Cohort Study, a birth cohort of singleton live births in Finland at 2 public maternity hospitals in Helsinki, Finland between 1934-1944 . (n=13,243) |
Intentional self-harm (ICD-8/9: E95; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0); Other symptoms and signs involving emotional state (ICD-10: R45.8) (n=135) |
29 to 70.5 | SOCIODEMOGRAPHIC: Birth order, maternal age. PREGNANCY/DELIVERY: Birth weight. |
SOCIODEMOGRAPHIC: No associations found. PREGNANCY/DELIVERY: No associations found |
| Li, et al. [57] | Case-control study in a birth cohort of singleton births from 1968-1996 in Washington state, USA, and who died at 1-19 years of age (n=37,321) |
Intentional self-harm (ICD-9: E950-E959) (n=303) |
1 to 19 | PREGNANCY/DELIVERY: Birth weight. | PREGNANCY/DELIVERY: No associations found. |
| Miller, et al. [63] | Northern Finland Birth Cohort 1966 (n=10,965) |
ICD codes not specified (n=63) |
Birth to 39 | SOCIODEMOGRAPHIC: Maternal age, paternal age, parents’ age difference. | SOCIODEMOGRAPHIC: Paternal age at birth not associated with suicide risk in the whole sample. Paternal age at birth between 35-39 and 40-44 (vs. 25-29) associated with higher suicide risk (35-39, RR =7.73 [1.37-43.69]; 40-44, RR =8.61 [2.40-144.45]) in female offspring but not in male offspring. Parental age difference, defined as paternal age minus maternal age, between 15-20 years (vs. 0-5) associated with higher suicide risk in offspring (HR=5.21 [1.24-21.87]). |
| Miller, et al. [64] | Birth cohort of individuals with nonaffective psychosis born in Helsinki, Finland, between 1951 and 1960 (n=529) |
ICD codes not specified (n=39) |
Birth to 55 | SOCIODEMOGRAPHIC: Maternal age, paternal age. | SOCIODEMOGRAPHIC: No associations found. |
| Mittendorfer-Rutz, et al. [65] | Birth cohort of individuals born in Sweden between 1973 and 1980 (n=713,370) |
Intentional self-harm (ICD-8/9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-8/9: E980-E989; ICD-10: Y10-Y34) (n=563) |
10 to 26 | SOCIODEMOGRAPHIC: Maternal age, maternal education, birth order. PREGNANCY/DELIVERY: Birth weight, birth length, prenatal hypertensive diseases, caesarean section. | SOCIODEMOGRAPHIC: Maternal age at birth under 20 years (vs. 20-29) associated with higher suicide risk (HR=2.30 [1.64-3.22]). Maternal education between 10 and 12 years (vs. ≥13) associated with higher suicide risk (HR=1.26 [1.02-1.57]) in offspring. PREGNANCY/DELIVERY: Birth weight between 800-2499 grams (vs. 3250-3749g) associated with higher suicide risk (HR=2.23 [1.43-3.46]). Birth length between 39-47 centimeters (vs. 50-51 cm) associated with higher suicide risk (HR=1.36 [1.01-1.84]). |
| Mok, et al. [66] | Birth cohort of individuals born in Denmark between 1966-1996 (n=1,793,681) |
Intentional self-harm (ICD-8: E950- E959; ICD-10: X60-X84) (n=2,108) |
15-40 | SOCIODEMOGRAPHIC: Maternal age, paternal age. | SOCIODEMOGRAPHIC: Maternal age at birth between 12-19 and 20-24 years (vs. 25-29) associated with higher suicide risk (12-19, IRR=1.46 [1.19-1.79]; 20-24, IRR=1.30 [1.16-1.47]). Paternal age at birth over 29 associated with higher suicide risk (range 30-34, IRR=1.15 [1.01-1.31] to ≥45, IRR=1.81 [1.33-2.43]). |
| Neeleman, et al. [68] | MRC National Survey of Health and Development (Birth cohort in the United Kingdom) (n=3,591) |
17 Psychiatrist rating based on vignettes of unnatural deaths (n=11) |
16-50 | SOCIODEMOGRAPHIC: SES. PARENTAL FACTORS: Parental disability. CHILD FACTORS: Early hospital admissions, age at first speech, cognitive alertness, motor development, physical development, enuresis. | SOCIODEMOGRAPHIC: No associations found. PARENTAL FACTORS: No associations found. CHILD FACTORS: Nocturnal enuresis at age 4 associated with higher suicide risk (OR=1.5 [1.1-2.1]). Global impression of physical development rated by medical examiners around ages 2 (OR=1.4 [1.0-2.0]) and 11 (OR=1.7 [1.2-2.6]) associated with higher suicide risk. |
| Neugebauer and Reuss [69] | Case-control; Individuals born in New York City and committing suicide in New York City between 1985 and 1991 (n=567) |
Computerized death certificate data (n=189) |
15-22 | SOCIODEMOGRAPHIC: Maternal age, single marital status, type of hospital service (public vs private), foreign born, parity. PREGNANCY/DELIVERY: Complication score time at 1st prenatal care, Apgar score at 1min, and Apgar score at 5min, birth order, maternal chronic illness. | SOCIODEMOGRAPHIC: Use of general (vs. private) hospital service during birth associated with higher suicide risk (Suicides cases, n [%]: Private, 67 [36]; General, 119 [64]). PREGNANCY/DELIVERY: No associations found. |
| Niederkrotenthaler, et al. [70] | Case-control study in a birth cohort of singletons born in Sweden between 1973-1983 who died by suicide with information on both biological parents. (n=14,490) |
Intentional self-harm (ICD-8/9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-8/9: E980-E989; ICD-10: Y10-Y34) (n=1,407) |
10 to 31 | PARENTAL FACTORS: Parental attempted suicide, parental suicide death, parental disability pension due to psychiatric diagnosis, parental disability pension due to somatic diagnosis, parental psychiatric inpatient care, parental death other than suicide. | PARENTAL FACTORS: Exposure to parental suicide attempt before the age of 3 years OR=2.88 [2.02-4.11]), between 3 and 10 (OR=2.60 [1.86-3.65]) and over the age of 10 (OR=2.46 (1.83-3.32]) associated with higher suicide risk. Exposure to parental death by suicide before (OR=2.93 [1.67-5.15]) and after the age of 10 (OR=2.36 [1.46-3.80]) years associated with higher suicide risk. Exposure to parental death other than suicide after age 10 (OR=1.47 [1.15-1.88]), but not before, associated with suicide risk. Parental disability due to psychiatric illness before the age of 3 (OR=3.06 [1.61-5.81]), between ages 3-10 (OR=2.59 [1.69-3.98]), and after age 10 (OR=2.15 [1.71-2.70]) associated with higher suicide risk. Parental disability due to somatic illness before the age of 3 (OR=1.88 [1.04-3.41]) and after age 10 (OR=1.31 [1.12-1.54]), but not between ages 3-10, associated with higher suicide risk. Parental psychiatric inpatient care before age of 3 (OR=2.49 [2.02-3.08]), between ages 3-10 (OR=1.90 [1.49-2.41]), and after age 10 (OR=2.14 [1.76-2.60]) associated with higher suicide risk. |
| Niederkrotenthaler, et al. [71] | Case-control study in a birth cohort of singletons born in Sweden between 1973-1983 who died by suicide with information on both biological parents. (n=14,490) |
Intentional self-harm (ICD-8/9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-8/9: E980-E989; ICD-10: Y10-Y34) (n=1,407) |
10 to 31 | SOCIODEMOGRAPHIC: Maternal age, paternal age, birth order. PREGNANCY/DELIVERY: Birth weight, birth length, small for gestational age (SGA), gestational age (GA). | SOCIODEMOGRAPHIC: Maternal age at birth under 20 years (vs. 20-29) associated with higher suicide risk (OR=1.57 [1.17-2.06]). Paternal age at birth under 25 years (vs. 25-29) associated with higher suicide risk (OR=1.20 [1.03-1.41]). PREGNANCY/DELIVERY: Birth weight between 800-2499 grams (vs. 3250-3749g) associated with higher suicide risk (OR=1.78 [1.26-2.51]). Birth length between 39 and 47 centimeters (vs. 50-51 cm) associated with higher suicide risk (OR=1.31 [1.04-1.64]). Birth length between 54 and 60 cm (vs. 50-51 cm) associated with lower suicide risk (OR=0.78 [0.62-0.98]). |
| Osler, et al. [74] | Birth cohort of men born in Copenhagen, Denmark, in 1953 (n=9,359) |
Intentional self-harm (ICD-8: E950- E959; ICD-10: X60-X64, X-66-X84) (n=92) |
18-49 | SOCIODEMOGRAPHIC: Single marital status, paternal SES. PREGNANCY/DELIVERY: Birth weight. | SOCIODEMOGRAPHIC: No associations found. PREGNANCY/DELIVERY: No associations found. |
| Richard, et al. [79] | Cohort of children aged 0-17 identified from the Quebec population-based physician reimbursement database in 1987 (n=135,629) |
Coroner database, coded with ICD-9 and ICD-10 (n=482) |
Birth to 38 | CHILD FACTORS: Age at traumatic brain injury (TBI), age at probable TBI, age at musculoskeletal injury. | CHILD FACTORS: Age at TBI under 12 (HR=1.49 [1.04-2.14]), between ages 12-17 (HR=1.57 [1.09-2.26]), and after 17 (HR=2.53 [1.79-3.59]) associated with higher suicide risk. Age at probable TBI after 17 (HR=1.64 [1.25-2.15]), but not between ages 0-12, and between ages 12-17, associated with lower suicide risk. Age at musculoskeletal injury after 17 (HR=1.77 [1.38-2.27]), but not between ages 0-12, and between ages 12-17, associated with lower suicide risk. |
| Richard-Devantoy, et al. [78] | 1958 Birth Cohort, comprising births in England, Scotland, and Wales during 1 week in March 1958 (n=14,505) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84) Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34) (n=55) |
Birth to 54 | CHILD FACTORS: Reading and math skills at age 7 and 11, and intelligence at 11. | CHILD FACTORS: No associations found. |
| Riordan, et al. [80] | Scottish Morbidity Record, birth cohort of individuals born between 1975-1988 (n=897,685) |
Death records which recorded the cause of death as suicide. (n=1,087) |
13 to 31 | SOCIODEMOGRAPHIC: Maternal age, birth order, family size, SES. PREGNANCY/DELIVERY: Birth weight, gestational age. | SOCIODEMOGRAPHIC: Maternal age at birth between 15-19 and 20-24 years (vs. 25-29) associated with higher suicide risk (15-19, HR=2.33 [1.87-2.89]; 20-24, HR=1.57 [1.33-1.84]). Quintile 4 and 5 of deprivation (vs. quintile 1) at birth associated with higher suicide risk in offspring (4, HR=1.61 [1.28-2.04]; 5, HR=1.57 [1.25-1.97]). Second, third, and ≥4th birth order (vs. first) associated with higher suicide risk (from HR=1.53 [1.31-1.78] to HR=2.69 [2.10-3.44]). Family size not associated with suicide. PREGNANCY/DELIVERY: No associations found. |
| Riordan, et al. [81] | Scottish Morbidity Record, birth cohort of individuals born between 1969-1986 (n=1,061,830) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34); Sequelae of intentional self-harm (ICD-10: Y87.0); Sequelae of injury of undetermined intent (ICD-10: Y87.2) (n=1,464) |
13 to 34 | SOCIODEMOGRAPHIC: Maternal age, parental SES, birth order. PREGNANCY/DELIVERY: Birth weight, gestational age. | SOCIODEMOGRAPHIC: Maternal age at birth between 15-19 and 20-24 years (vs. 25-29) associated with higher suicide risk (15-19, HR=2.00 [1.66-2.41]; 20-24, HR=1.40 [1.23-1.60]). Skilled and unskilled parental occupation at birth (vs. professional) associated with higher suicide risk in offspring (skilled, HR=1.35 [1.15-1.58]; unskilled, HR=1.69 [1.42-2.03]). Second, third, and ≥4th birth order (vs. first) associated with higher suicide risk (from HR=1.61 [1.41-1.84] to HR=2.76 [2.29-3.31]). PREGNANCY/DELIVERY: Birth weight under 2500 grams (vs. 3250-3749g) associated with higher suicide risk (HR=1.35 [1.05-1.72]). |
| Risnes, et al. [82] | Birth cohort with sibling comparison of Norwegian individuals born between 1967- 1997 (n=1,562,647) | Intentional self-harm (ICD-8: E950-E959; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0) (n=3,274) |
15 to 45 | PREGNANCY/DELIVERY: Gestational age. | PREGNANCY/DELIVERY: Post-term gestational age of ≥ 42-44 weeks (vs. 37-41 weeks + 6 days) associated with higher suicide risk in the population-level analysis (HR=1.14 [1.04-1.26]) but not in the sibling-level analysis. |
| Rojas and Stenberg [83] | Stockholm birth cohort of men born in 1953 (Stockholm Birth Cohort study panel) (n=5,293) |
Intentional self-harm (ICD-8: E950-E959); Injury of undetermined intent (ICD-8: E980-E989) (n=33) |
17 to 30 | SOCIODEMOGRAPHIC: Single marital status, family size, SES. | SOCIODEMOGRAPHIC: No associations found. |
| Rostila, et al. [84] | Swedish Work and Mortality Data. Birth cohort of groups of 2 or more siblings born between 1932-1980 in which at least 1 died by suicide (n=34,413) |
Intentional self-harm (ICD-8: E950- E959; ICD-10: X60-X64, X-66-X84) (n=10,656) |
Birth to 70 | SOCIODEMOGRAPHIC: Birth order. | SOCIODEMOGRAPHIC: Second, third, and ≥4th birth order (vs. first) associated with higher suicide risk (from HR=1.25 [1.17-1.34] to HR=1.79 [1.54-2.08]). |
| Saarela, et al. [85] | Birth cohort of individuals born in Finland between 1922-1987 (n=254,059) |
ICD codes not specified (n=1,377) |
Birth to 89 | SOCIODEMOGRAPHIC: Birth order. | SOCIODEMOGRAPHIC: Second, third, and ≥4th birth order (vs. first) associated with higher suicide risk (from HR=1.27 [1.09-1.47] to HR=1.72 [1.22-2.44]). |
| Salib and Cortina-Borja [87] | Birth cohort of individuals born in England and Wales between 1955-1966 (n=11,035,365) |
Intentional self-harm (ICD-9: E950-E959); Injury of undetermined intent (ICD-9: E980-E989) (n=26,915) |
16 to 46 | PREGNANCY/DELIVERY: Month of birth. | PREGNANCY/DELIVERY: Birth months in spring to early summer (vs. autumn-early winter) associated with higher suicide risk (17.9% [13.0-21.8]). This risk is higher in females (29.6% [8.0-50.7]) than males (13.7% [5.2-22.2]). |
| Salib and Cortina-Borja [86] | Birth cohort of individuals born in England and Wales between 1941-1966 (n=22,423,117) |
Intentional self-harm (ICD-9: E950-E959); Injury of undetermined intent (ICD-9: E980-E989) (n=52,358) |
16 to 45 | PREGNANCY/DELIVERY: Month of birth. | PREGNANCY/DELIVERY: Birth months in spring associated with higher suicide risk (17.9% [13%−33%]). Females born in those spring months (vs. males born during those months; 15% [5%- 22%]) associated with higher suicide risk (27% [8%−47%]). |
| Salk, et al. [88] | Case-control study of adolescents who died by suicide between 1975- 1983 in Rhode Island, USA and whose birth records were available (n=156) |
Death deemed by suicide by the Office of the State Medical Examiner, Department of Health, Rhode Island (n=52) |
12 to 20 | PREGNANCY/DELIVERY: Number of maternal, prenatal, birth and neonatal risk factors, complication score (0-45). Also, separately, previous premature births, bleeding during pregnancy, maternal chronic disease, duration labor, fetal HR during labor, no antenatal care before 20 weeks, respiratory distress of neonate, infant infection, placenta previa or abruption. | PREGNANCY/DELIVERY: Number of maternal, prenatal, birth and neonatal risk factors (of a maximum of 46) associated with higher suicide risk (Mean [SD]; Suicide cases: 4.62[4.96]; Control group 1: 3.52 [3.72]; Control group 2: 3.67 [3.71]; Cases v control 1: p<0.01; Cases v control 2: p<0.05; Cases v control 1 and 2 combined: p<0.01). Overall pregnancy, birth, and neonatal risk score associated with higher suicide risk (Mean [SD] [range 0-10]; Suicides: 1.44 [1.27]; Control 1: 0.35 [0.76]; Control 2: 0.48 [0.84]; p<0.005 between the suicide group and each of the control groups). Placental previa/abruption associated with higher suicide risk (n: Suicides=4, Control 1= 1, Control 2=0, p<0.005 between suicide and control groups). No antenatal care before 20 weeks associated with higher suicide risk (n: Suicides=16, Control 1=2, Control 2=6, p<0.005 between suicide and control groups). Infant infection associated with higher suicide risk (n: Suicides=7, Control 1=3, Control 2=1, p<0.005 between suicide and control group). Previous premature births associated with higher suicide risk (n: Suicides=6, Control 1=1, Control 2=2, p<0.005 between suicide and control groups). Bleeding during pregnancy associated with higher suicide risk (n: Suicides=4, Control 1=1, Control 2=0, p<0.005 between suicide and control groups). Maternal chronic disease associated with higher suicide risk (n: Suicides=11, Control 1=0, Control 2=3, p<0.005 between suicide and control groups). Abnormal duration, either too short or too long, of 1st stage (<3 hours or >20 hours) or 2nd stage labor (<10 minutes or > 2hours) associated with higher suicide risk. (n: 1st stage labor, suicides=8, control 1=0, and control 2=4, difference p<0.005; 2nd stage labor, suicides=8, control 1=3, and control 2=0, difference p<0.005). Respiratory distress of neonate > 1 hour at birth associated with higher suicide risk (n: Suicides=10, Control 1=4, Control 2=2, p<0.005 between suicide and control groups) |
| Sorensen, et al. [91] | Copenhagen Perinatal Cohort, birth cohort of individuals born between 1959-1961 and their parents (n=7,177) |
ICD codes not specified (n=48) |
10 to 46 | SOCIODEMOGRAPHIC: SES at 1 year of age. | SOCIODEMOGRAPHIC: Lower parental social status (linear) at age 1 associated with higher suicide risk in offspring (HR=1.23 [1.03-1.49]). |
| Steck, et al. [93] | Swiss National Cohort (SNC). Adolescents aged 10-18 who were registered in the 1990 or 2000 census. (n=2,395,677) |
Intentional self-harm (ICD-8: E950-E958; ICD-10: X60-X75, X77-X78, X80-X84) (n=592) |
10 to 18 | SOCIODEMOGRAPHIC: Maternal age, paternal age, parental education, birth order, foreign-born child. | SOCIODEMOGRAPHIC: Being only child and middle-born children (vs. first born) associated with higher suicide risk (only child, HR=1.3 [1.02-1.7]; Middle born, HR=1.4 [1.05-1.8]). Being a Swiss child associated with higher suicide risk compared to foreign children (HR=1.52 [1.20-1.92]) |
| Strand and Kunst [95] | Birth cohort of Norwegians born between 1955-1965 (n=613,807) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84); Sequelae of intentional self-harm (ICD-10: Y87.0) (n=1,013) |
25 to 46 | SOCIODEMOGRAPHIC: Maternal education, paternal education, paternal SES. | SOCIODEMOGRAPHIC: Higher levels of parental education associated with higher suicide risk in female (Father education, RR=2.50 [1.59-4.00], Mother education, RR=2.13 [1.32-3.45]) but not male offspring. Higher household income associated with higher suicide risk in female (RR=2.22 [1.39-3.45]) but not male offspring. |
| Suvisaari, et al. [97] | Helsinki High-Risk Study, birth cohort of offspring of mothers with psychosis born between 1940-1977 in Finland (n=337) |
ICD codes not specified (n=7) |
16 to 65 | SOCIODEMOGRAPHIC: SES at birth. | SOCIODEMOGRAPHIC: No associations found. |
| von Borczyskowski, et al. [100] | Birth cohort of individuals born in Sweden between 1946-1968 (n=2,471,496) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34) (n=8,815) |
19 to 55 | SOCIODEMOGRAPHIC: Maternal age. | SOCIODEMOGRAPHIC: Maternal age at birth under 25 years and over 34 (vs. 25-34) associated with higher suicide risk in men (<25, HR=1.22 [1.15-1.29]; >34, HR=1.15 [1.07-1.23]) and women (<25, HR=1.22 [1.11-1.34]; >34, HR=1.14 [1.01-1.28]) offspring. |
| von Borczyskowski, et al. [101] | Birth cohort of individuals born in Sweden between 1946-1968 (n=2,471,496) |
Intentional self-harm (ICD-9: E950-E959; ICD-10: X60-X84)); Injury of undetermined intent (ICD-9: E980-E989; ICD-10: Y10-Y34) (n=8,815) |
19 to 55 | SOCIODEMOGRAPHIC: Maternal age, adoption between 6-12 months. | SOCIODEMOGRAPHIC: Maternal age at birth under 25 years and over 34 (vs. 25-34) associated with higher suicide risk in non-adopted (<25, HR=1.16 [1.11-1.21]; >34, HR=1.11 [1.05-1.17]) and adopted (<25, HR=1.56 [1.05-2.30]; >34, HR=1.10 [0.80-1.49]) offspring. Being adopted between 6-12 months associated with higher suicide risk (Suicides, %: Non-adopted, 0.4% [5.2/1000 men, 2.0/1000 women]; Adopted, 0.7% [8.5/1000 men, 3.9/1000 women], p<0.001). |
| Wilcox, et al. [103] | Birth cohort of individuals born between 1946-1968 and residents in Sweden on December 31. 1986 (n=3,591,096) |
Intentional self-harm (ICD-8: E950-E959; ICD-10: X60-X84) (n=1362) |
Birth to 25 | PARENTAL FACTORS: Parental death by suicide, accident, and other causes. | PARENTAL FACTORS: Exposure to parental death by suicide at age 0-12 (IRR=3.0 [1.7-5.3]), 13-17 (IRR=3.1 [2.1-4.6], but not at 18-25, associated with higher suicide risk. Exposure to parental death by accident at age 0-12 years (IRR=2.0 [1.1-3.8]) but not later up to 25 years, associated with higher suicide risk. Exposure to parental death by other causes other than suicide/accident at any age between 0-25 not associated with suicide risk. |
| Zambon, et al. [104] | Birth cohort of individuals born in Sweden between 1977-1991 (n=1,616,342) |
Intentional self-harm (ICD-10: X60-X84); Injury of undetermined intent (ICD-10: Y10-Y34) (n=652) |
7 to 26 | SOCIODEMOGRAPHIC: Maternal age, parental education, foreign-born parent. | SOCIODEMOGRAPHIC: Maternal age at birth under 20 years (vs. ≥20) associated with higher suicide risk (RR=1.82 [1.32-2.52]). Having a mother born in another Nordic country other than Sweden associated with higher suicide risk (RR=2.29 [1.64-3.21]). |
| Zammit, et al. [105] | Birth cohort of individuals born in Sweden between 1972-1977 (n=204,323) |
Intentional self-harm (ICD-8/9: E950-E959; ICD-10: X60-X84); Injury of undetermined intent (ICD-8/9: E980-E989; ICD-10: Y10-Y34) (n=314) |
26 to 31 | SOCIODEMOGRAPHIC: Parental education, single marital status at age 8, SES at age 8, foreign-born parents. | SOCIODEMOGRAPHIC: Single-parent household at age 8 associated with higher suicide risk (OR= 1.54 [1.11-2.13]). Having 1 or 2 foreign-born parent associated with higher suicide risk (1, OR=1.60 [1.12-2.29]; 2, OR=2.49 [1.73-3.59]). |
Age range of suicides given only
ICD, International Classification of Diseases; SES, socioeconomic status (includes parental occupation, social class, income or poverty indicators)
Risk of bias
The two investigators conducting the risk of bias had 97% agreement (kappa=0.88). Overall, risk of bias was low (Supplementary Table S1). Of the 54 studies, 38 (70.4%) scored the highest score, 9; 15 studies (27.8%) scored 8, and one study scored 7. The reasons studies scored less than 9 were 1) comparability between exposed/cases and non/exposed/controls, in which none or just one relevant covariate was considered or 2) there was unexplained attrition at follow-up.
Sociodemographic factors
Common sociodemographic factors examined by the studies included in our review were parental age at birth, marital status, income (including receipt of income from welfare), occupation, education, and birth order of the child (See Supplementary Table S2 for a comprehensive report).
Offspring of younger mothers, particularly those less than 20 years of age, had up to a 2.5-fold higher risk of suicide than offspring of mothers in their late 20’s [10, 20, 24, 30, 63, 65, 66, 71, 80, 81, 100, 101, 104]. This risk was independent of other demographic factors such as sex, parental education, or socioeconomic status (SES), as well as gestational age and birth weight. However, a small number of studies did not find an association of younger maternal age with offspring suicide risk [25, 56, 69, 93] or found it only in males [2, 64]. Whether or not suicide risk increased with advanced maternal age was less clear. A U-shaped association between maternal age and offspring suicide appeared in several studies [30, 100, 101], but in other studies the suicide risk among offspring of mothers >29 years of age was even lower than among offspring of mothers in their 20’s [24, 34].
Evidence was inconsistent for paternal age (examined in 6 studies). Offspring of younger fathers (<20 in one study and <24 in another) and offspring of relatively older fathers (>30) had a higher risk of suicide than offspring of fathers in their late 20’s [24, 66, 71], but three other studies found no association between father’s age and suicide risk [63, 64, 93].
In most of the 10 studies that examined parents’ marital status, offspring of single parents had a 1.5 to 2-fold higher suicide risk than offspring of married or cohabiting parents; however, the results were only statistically significant in the studies with larger samples [10, 20, 24, 105].
Offspring of parents with lower education had 50% higher suicide risks adjusting for other demographic factors [10, 24, 39, 65], though parental education was associated with suicide risk only among men in one study [20] and only among women in another [95]. Most studies examining parental occupation and income did not find associations with suicide risk [2, 25, 34, 68, 74, 83, 97], except for one large cohort, in which lower parental occupation was associated with higher suicide risk [81]. Studies using a composite measure of SES, including parental occupation, education, income, and housing conditions, found lower SES to be associated with suicide risk [80, 91].
Later-born children – particularly children with 4 or more older siblings – had a higher risk of suicide in some [10, 20, 39, 80, 81, 84, 85] but not all studies [2, 24, 25, 34, 56, 65, 69, 71]
Finally, immigrant status (either first or second generation) was associated with higher suicide risk [24, 44, 104, 105]. This was also the case for international and national adoptees, children who resided in institutional care, or children who had contact with social services or received child welfare [34, 45–47, 101]. However, most of these studies were conducted in a single country, Sweden.
Pregnancy and delivery factors
Long-term vulnerability to suicide appears to be established as early as the prenatal period, as is a wide range of mental and physical health conditions [13, 26, 38] (See Supplementary Table S3 for a comprehensive report). Perturbations in fetal development may be the source of this vulnerability, which is most often captured in population samples through measures of fetal growth and birth weight. Neonatal anthropometrics - including birth weight, birth length, and head circumference - were analyzed in nine studies. Four of the 8 studies examining the association between birth weight and suicide found that low birth weight (<2500 grams) compared to normal birth weight was associated with a 1.5 to 2.5-fold higher risk of suicide in offspring, [34, 65, 71, 81] adjusting for sociodemographic factors and gestational age. Two of the 4 studies examining birth length found an association between shorter length (i.e., 39-47 cm) and higher suicide risk compared to normal birth length at term [65, 71]. In contrast, none of the studies examining being born small for gestational (SGA) or large for gestational age (LGA) found an association with suicide in offspring [24, 25, 55, 71]. Similar to studies examining SGA and LGA, most studies examining only gestational age (n=5 of 7) found no association with suicide in offspring [24, 25, 71, 80, 81]. Relatedly, though maternal smoking during pregnancy can impact fetal growth [5], only one large study [24] out of 4 found an association between maternal smoking during pregnancy and suicide risk in offspring, with approximately a 2-fold higher risk compared to offspring not exposed to maternal smoking; this was independent of socioeconomic factors, gestational age, and birth weight.
Pregnancy and delivery complications have been studied frequently in relation to offspring psychopathology, though less so with respect to suicide. Jacobson and Bygdeman [50] found birth-related traumas to be associated with a 2-4-fold higher suicide risk among males. Salk and colleagues [88] found higher pregnancy complication scores in suicide cases than controls. However, these two studies did not adjust for sociodemographic factors. After adjusting for type of hospital service, which was itself associated with suicide risk, Neugebauer and Reuss [69] did not find an association between pregnancy complications and offspring suicide risk. Mode of delivery - including instrumental, vaginal, and caesarean delivery – was not associated with suicide risk [24, 50, 65].
Finally, studies of seasonality effects generally show higher suicide risks for people born in the Spring [9, 86, 87] .
Parental factors
Children and adolescents who experience the death of a parent, especially if that death is by external causes such as suicide or accidents, carry with them into adulthood an elevated risk of suicide, up to a 4-fold higher risk in some studies [17, 18, 34, 70, 103]. Most studies show that this risk is higher when parental death occurs when the child is younger, in contrast to in older adolescence and adulthood. In contrast to these results, parental death by causes other than suicide or accidents has been either associated with higher suicide risk in offspring only when exposure occurred at ages over than 10 [70] or not associated at all with suicide risk [103]. One study, though, found an association between parental death by any cause before the child was 7 years old, and higher suicide risk (HR = 4.52) [34], yet the authors did not compare distinct ages of exposures or distinct causes of death.
Parental stressful conditions also contribute to suicide risk in offspring [23, 68, 70]. Postnatal maternal stress was associated with a 1.5-fold higher suicide risk among offspring (Class et al., 2014); parental disability from both somatic and psychiatric conditions was also associated with higher offspring suicide risk [70]. Supplementary Table S4 provides a comprehensive report of all findings.
Child factors
There are long-term mental health consequences of childhood medical conditions, and several studies in our review found that these consequences include suicide (See Supplementary Table S4 for a comprehensive report of findings). Korhonen et al. (2019) found that cancer, probable traumatic brain injury (TBI), and musculoskeletal injuries in late childhood or adolescence, but not in early childhood, are associated with higher suicide risk. Richard et al. (2015) found that verified TBI at any age was associated with higher risk of suicide. Nocturnal enuresis at ages 4-5 was associated with higher risk in one study [68], but not in another study that adjusted for perinatal, sociodemographic, and behavioral/emotional factors [34]. Other studies did not detect associations between childhood conditions or measures of child development and later suicide: early hospital admission, intelligence at ages 10-11, arithmetic and reading skills at ages 7 and 11, internalizing symptoms at age 7, diurnal enuresis at age 3, age at first speech, cognitive alertness at age 7, and motor development at age 2 were not associated with suicide risk [19, 34, 68, 78]. Similarly, externalizing symptoms at age 7 were initially associated with higher risk but not when adjusted for perinatal, sociodemographic, and behavioral/emotional factors [34]. Finally, neglected appearance by itself was not associated with suicide risk but exposure to more than three adverse emotional experiences by age 7 (e.g., including parental death, neglected appearance, domestic tension, institutional care, peer bullying, and poor physical development) was associated with up to 3-fold higher risk of suicide [34].
Risk factors for suicide attempt compared to suicide death
Fifteen of the 54 studies in our review examined associations between early life factors and both suicide death and suicide attempt. When comparing associations across both outcomes within studies, results did not differ substantially: early life factors associated with suicide death were also associated with suicide attempt (see Supplementary Table S5), with few exceptions in which some exposures, like younger maternal age in two studies [2, 24, 65, 71, 103], were associated with suicide death but not attempt. However, there were more exposures associated with suicide attempt than with suicide death. This likely reflects a lack of power to detect associations with mortality, since the number of people who died by suicide in most studies was substantially lower than the number of people with suicide attempts. Overall, though, the profile of early risk factors associated with suicide attempt is similar to the profile of risk factors for suicide death, which includes socioeconomic factors, factors associated with fetal growth, and the loss of a parent but not birth and other obstetric factors.
Discussion
Our review synthesized the literature on the prospective associations between early life factors, spanning from pregnancy to 12 years of age, and suicide mortality. Evidence supports associations between several socioeconomic and obstetric factors and higher risk of suicide death in offspring including young maternal age at birth, low parental education, higher birth order, and low birth weight. Evidence from larger samples suggests that smoking during pregnancy, parental SES, and single marital status could also be related to higher suicide risk in offspring, but replication in other large studies is needed. Among the few studies that examined early childhood neurodevelopment and adverse exposures, childhood exposures to parental death by external causes and emotional adversity, but not neurodevelopmental characteristics, were associated with suicide risk. Our review uncovered several questions that remain to be answered.
First, is the association between early life exposures and suicide mortality causal? All the studies in our review were observational studies, from which causality cannot be established. In addition, for each exposure studied, the variables adjusted for differed across studies. The associations could be due to a wide range of environmental and genetic risks for suicide. Family aggregation of suicidal behaviors exists, and parental psychopathology and family history of self-harm are associated with suicide behaviors in offspring [14, 70, 103]. However, among those studies that employed sibling comparison designs or studies controlling for parental psychopathology [10, 24, 82], associations between early life factors and suicide death remained, suggesting that these associations are not entirely due to confounding by genetic and other shared family factors. In the absence of strong causal evidence, knowledge of early life risk factors for suicide is still important as this information may aid in more precisely identifying high-risk individuals at increased risk of suicide who may benefit from preventive interventions (e.g., people with depression with one or more early life risk factors for suicide).
Second, how might early life factors increase vulnerability to suicide death that occurs several decades later? The prenatal period, infancy and early childhood are sensitive developmental periods with heightened plasticity, periods during which adverse experiences may have enduring consequences. For example, in the context of heightened plasticity, psychological and physiological responses to adversity may prove adaptive (protective) in the short-term but ultimately be pathologic later in adulthood [37]. Reponses to altered fetal growth and early socioeconomic and emotional adversity could include changes in immune, neuroendocrine, epigenetic, and neural systems that impact neurodevelopment [15, 27, 36, 72, 77, 99]. From a life-history perspective, early life exposures may have an enduring impact on suicide risk because they may alter the pace of major life transitions, increase risk taking, and reduce future orientation, all of which may be implicated in the etiology of suicidal behaviors [106]. In addition to changes in biological systems, early socioeconomic and emotional adversity, such as maternal young age or the loss of a parent, will influence the immediate context in which the child is raised thus increase the likelihood of being exposed to further social and psychological factors associated with vulnerability to suicide such as physical or sexual abuse, lower educational attainment, less social support, harmful parenting practices, or family conflict. All together, these biological, social and psychological changes resulting from early adversity would increase the risk of psychiatric disorders, altered decision making, and development of specific personality traits that make individuals more vulnerable to stressors and increase suicide risk [99]. Whereas our review highlights that a wide range of early childhood factors is associated with long-term suicide risk, the attributable risk for any individual factor is likely small. Considered in the aggregate, suicide risk could be substantially influenced by accumulated exposures starting early in development spanning multiple domains such as social, familial, personality, and psychiatric. It is still unclear, though, whether early life factors interact with proximal factors to eventually increase the risk of (or protect against) suicide mortality. Early life factors could directly confer risk for many of the proximal antecedents of suicide. For example, a study using the 1958 British Cohort found that early life factors previously linked to suicide death [34] such as younger maternal age, higher birth order, and childhood adversities were also linked to higher risk of suicidal ideation, internalizing disorders, and alcohol use disorder through middle adulthood [33] – all proximal risk factors of suicide death. In that study, externalizing behaviors in childhood and low birth weight were not linked to these proximal risk factors for suicide, suggesting other paths to suicide are involved. It is also possible that early life risks for suicide magnify the influences of proximal factors, essentially creating a suicide-related diathesis that is activated by the presence of psychopathology or stressful environments. For example, low birth weight or early childhood adversity could be associated with alterations of the HPA axis, thus reducing the threshold for stress reactivity under stressful conditions or in the presence of proximal factors [15, 35, 62, 99]. For instance, among people with depression, those exposed to early life adversity are at higher risk of suicide than those not exposed to early life adversity [28]. We speculate that early life factors confer risk for suicide mortality through both pathways: by leading to and interacting with proximal factors. Figure 2 provides a conceptual model outlining the developmental pathways linking early risk factors, proximal factors, and suicide mortality. Future research is needed to determine how much of the influence of early life risk factors on suicide is explained by proximal factors, and how the effects of proximal factors (i.e., acute precipitants to suicide) are modified by early life factors.
Fig 2. Schematic representation of the effect of early life factors on increased vulnerability to suicide mortality.
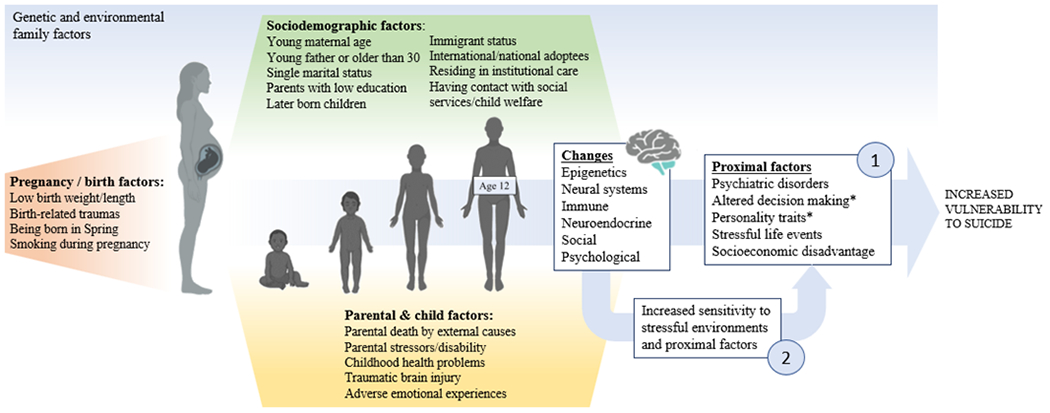
Pregnancy-related factors, sociodemographic factors, and parental and child factors during first years of childhood are thought to influence epigenetic, neural, immune, neuroendocrine, social, and psychological changes with two potential long-term effects: 1) Increased likelihood to exposure to more proximal and precipitant factors, which in turn increase vulnerability to suicide, and 2) Increased sensitivity to stressful environments and effects of proximal factors if these occur. Genetic and environmental family factors might affect some of these effects. * Altered decision making and personality traits are listed here under proximal factors given that this review focuses on early life factors; however, they are sometimes conceptualized as distal factors in the literature.
Third, apart from socioeconomic adversity and the loss of a parent, very few studies included in this review examined other early childhood exposures associated with suicide death such as childhood abuse, neurodevelopment or behavioral factors. This may be because most studies relied on administrative registries where such information is often not available. Nevertheless, childhood abuse and psychopathology have been linked to suicidal ideation and attempts in adolescence and adulthood [4, 31]. In our review, children who suffered peer bullying and males with externalizing behaviors had a higher risk of suicide death for [34]. Future prospective studies on suicide risk should ideally collect comprehensive information on the family environment, children’s behavior, and neuropsychological development to gain a fuller understanding of how early life factors influence the immediate environments of children and how those eventually increase or decrease their vulnerability to suicide.
Fourth, future studies should examine exposures in children and adolescents separately. Most studies examining ‘childhood exposures’ combine children and adolescents (i.e., over 12 years of age) or define ‘childhood exposure’ as any event occurring before the 18th birthday [4]. However, if our aim is identifying childhood vulnerability for suicide, combining children with adolescents, or even young adults, is problematic for several reasons. First, adolescence is a developmental period in which over half of mental health problems have their onset [52] including suicidal behaviors [53]. Adolescence is also characterized by more impulsive behaviors and altered decision-making [43]. Therefore, vulnerability might be already established by that time. Second, previous studies suggest that the timing of exposure matters. For example, this review shows that early childhood neurocognitive factors are not associated with a higher risk of suicide death. However, the same factors in adolescence and young adulthood have been associated with a higher risk of suicidal behaviors in longitudinal studies [3, 41, 42]. In contrast, this review shows that the opposite pattern is seen for loss of a parent or parental suicide attempt [17, 18, 70, 103], in which earlier exposures are associated with a higher risk of suicidal behaviors than later exposures. These findings underscore the importance of studying suicide vulnerability using a developmental approach to capture nuances in the timing of exposures.
Finally, early life risk factors for suicide mortality were similar to those for suicide attempt in studies that examined both outcomes. Evidence from retrospective studies suggests that suicide attempters and completers primarily differ in the lethality of methods (e.g., poisoning in attempters vs. firearm or hanging in completers), and sex distribution (attempters are more likely to be female while completers are more likely to be male) [60, 92]. Some studies have also found differences in age, race distribution, drug/alcohol use, and health comorbidities [49, 76]. The findings of our review are consistent with a study that found no differences between distal factors for violent and non-violent methods of suicide attempt, and completed suicide linked to violent methods, suggesting that early life factors might confer vulnerability to suicide attempts in general [94]. The lethality of the attempt would then be dependent on other factors occurring during development such as substance use behaviors, health problems, or accessibility to lethal means, among others. More studies are needed that directly compare risk factors between suicide attempt and suicide mortality, possibly comparing both outcomes directly rather than to healthy controls; this has the potential to inform both universal and targeted interventions as well as interventions to mitigate risk for the escalation of suicide behaviors. A caveat to this conclusion is that we did not conduct a systematic review of childhood risk factors for suicide attempt, but rather only considered risk factors for attempt in studies that also examined risk factors for suicide death. Therefore, these results do not represent the overall profile of risk factors for suicide attempt.
The major contributions of this review are the focus on childhood risk factors predating onset of most suicide behaviors and broad coverage of high-quality prospective studies of suicide mortality. However, the review and the studies included in it also have limitations. First, the restriction to published studies introduces the possibility of publication bias; unfortunately, it is not possible to assess the extent of unpublished findings of observational studies as would be possible for registered trials. The finding that many of the studies in our review reported no association between childhood risk factors and suicide potentially mitigates this concern. Second, the studies were conducted in the context of high-income western countries (HIC), and mostly Nordic Europe and Great Britain. Therefore, findings cannot be generalized to other HIC, and low- and middle-income countries (LMIC). The latter is especially important since many of the early life factors identified for suicide may be particularly relevant in LMIC given the higher prevalence of low weight births [11], younger mothers at birth [48], and poverty-related suicide [6] in these countries. Additionally, there was variability in whether studies controlled for potential confounders and, when they did, whether they controlled for the same confounders, which limits the interpretability of results across studies.
Conclusion
Vulnerability to suicide mortality is partly established early in life, with sociodemographic factors, prenatal factors, especially low birth weight, and early exposure to the loss of a parent by external causes, having particularly notable contributions. Our review underscores that vulnerability to suicide begins to be formed long before current approaches to identifying individuals at heightened risk for suicide can detect. In theory, the implication is that suicide prevention efforts should be initiated much earlier in the life course than they currently are. The challenges in causal inferences described above stand in the way of developing interventions for suicide based on the studies included in our review; on the other hand, many of the risk factors identified increase risk not only for suicide but for common mental disorders. Thus, broad based efforts early in the life course to improve mental health would be expected to benefit suicide as well.
Our proposed conceptual model in Figure 2 highlights two sets of potential pathways linking early childhood risk factors to suicide. The goal of pursuing research examining these two pathways would be to generate a better understanding of developmental pathways that lead to suicide and thereby identify opportunities to mitigate the adverse consequences of the risk factors identified by our review as well as the timing of when such opportunities may exist.
Supplementary Material
Acknowledgments:
We want to thank Risë Goldstein, Mahad Gudal, Jacob S. Jeffers, Jeremy Luk, Katherine Maultsby, and Reeya Patel for their help and contributions in this project.
Funding:
This work was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Project 1ZIAHD008976).
Footnotes
Conflicts of interest: All authors declare no conflicts of interest.
Code availability: Not applicable
Ethics approval: Not applicable
Informed consent: Not applicable
Consent for publication: All authors have approved the current version of the manuscript for publication.
Contributor Information
Pablo Vidal-Ribas, Social and Behavioral Sciences Branch, Division of Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland, USA
Theemeshni Govender, Social and Behavioral Sciences Branch, Division of Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland, USA
Jing Yu, Social and Behavioral Sciences Branch, Division of Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland, USA
Alicia A. Livinski, National Institutes of Health Library, Office of Research Services, OD, NIH, Bethesda, Maryland, USA.
Denise L. Haynie, Social and Behavioral Sciences Branch, Division of Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland, USA.
Stephen E. Gilman, Social and Behavioral Sciences Branch, Division of Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland, USA; Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA
Availability of data and material:
Protocol of systematic review and search strategy is included in the Online Resource
References
- 1.Al-Haddad BJS et al. (2019) Long-term Risk of Neuropsychiatric Disease After Exposure to Infection In Utero. JAMA Psychiatry. 76(6):594–602. 10.1001/jamapsychiatry.2019.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alaraisanen A et al. (2012) Ante- and perinatal circumstances and risk of attempted suicides and suicides in offspring: the Northern Finland birth cohort 1966 study. Soc Psychiatry Psychiatr Epidemiol. 47(11):1783–94. 10.1007/s00127-012-0479-8 [DOI] [PubMed] [Google Scholar]
- 3.Andersson L et al. (2008) Association of IQ scores and school achievement with suicide in a 40-year follow-up of a Swedish cohort. Acta Psychiatr Scand. 118(2):99–105. 10.1111/j.1600-0447.2008.01171.x [DOI] [PubMed] [Google Scholar]
- 4.Angelakis I, Austin JL, and Gooding P (2020) Association of Childhood Maltreatment With Suicide Behaviors Among Young People: A Systematic Review and Meta-analysis. JAMA Netw Open. 3(8):e2012563. 10.1001/jamanetworkopen.2020.12563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banderali G et al. (2015) Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review. Journal of Translational Medicine. 13(1):327. 10.1186/s12967-015-0690-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bantjes J et al. (2016) Poverty and suicide research in low- and middle-income countries: systematic mapping of literature published in English and a proposed research agenda. Glob Ment Health (Camb). 3:e32. 10.1017/gmh.2016.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belsher BE et al. (2019) Prediction Models for Suicide Attempts and Deaths: A Systematic Review and Simulation. JAMA Psychiatry. 76(6):642–651. 10.1001/jamapsychiatry.2019.0174 [DOI] [PubMed] [Google Scholar]
- 8.Bjorkenstam C, Kosidou K, and Bjorkenstam E (2017) Childhood adversity and risk of suicide: cohort study of 548 721 adolescents and young adults in Sweden. Bmj. 357:j1334. 10.1136/bmj.j1334 [DOI] [PubMed] [Google Scholar]
- 9.Bjorksten KS and Bjerregaard P (2015) Season of birth is different in Inuit suicide victims born into Traditional than into Modern Lifestyle: a register study from Greenland. BMC Psychiatry. 15:147. 10.1186/s12888-015-0506-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bjorngaard JH et al. (2013) Maternal age at child birth, birth order, and suicide at a young age: a sibling comparison. Am J Epidemiol. 177(7):638–44. 10.1093/aje/kwt014 [DOI] [PubMed] [Google Scholar]
- 11.Blencowe H et al. (2019) National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. The Lancet Global Health. 7(7):e849–e860. 10.1016/S2214-109X(18)30565-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bolger N et al. (1989) The onset of suicidal ideation in childhood and adolescence. J Youth Adolesc. 18(2):175–90. 10.1007/bf02138799 [DOI] [PubMed] [Google Scholar]
- 13.Braithwaite EC, Murphy SE, and Ramchandani PG (2014) Prenatal risk factors for depression: a critical review of the evidence and potential mechanisms. J Dev Orig Health Dis. 5(5):339–50. 10.1017/S2040174414000324 [DOI] [PubMed] [Google Scholar]
- 14.Brent DA and Mann JJ (2005) Family genetic studies, suicide, and suicidal behavior. Am J Med Genet C Semin Med Genet. 133c(1):13–24. 10.1002/ajmg.c.30042 [DOI] [PubMed] [Google Scholar]
- 15.Brodsky BS (2016) Early Childhood Environment and Genetic Interactions: the Diathesis for Suicidal Behavior. Curr Psychiatry Rep. 18(9):86. 10.1007/s11920-016-0716-z [DOI] [PubMed] [Google Scholar]
- 16.Brown GK and Jager-Hyman S (2014) Evidence-based psychotherapies for suicide prevention: future directions. Am J Prev Med. 47(3 Suppl 2):S186–94. 10.1016/j.amepre.2014.06.008 [DOI] [PubMed] [Google Scholar]
- 17.Burrell LV, Mehlum L, and Qin P (2017) Risk factors for suicide in offspring bereaved by sudden parental death from external causes. J Affect Disord. 222:71–78. 10.1016/j.jad.2017.06.064 [DOI] [PubMed] [Google Scholar]
- 18.Burrell LV, Mehlum L, and Qin P (2018) Sudden parental death from external causes and risk of suicide in the bereaved offspring: A national study. J Psychiatr Res. 96:49–56. 10.1016/j.jpsychires.2017.09.023 [DOI] [PubMed] [Google Scholar]
- 19.Calvin CM et al. (2017) Childhood intelligence in relation to major causes of death in 68 year follow-up: prospective population study. Bmj. 357:j2708. 10.1136/bmj.j2708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen YY et al. (2013) Perinatal risk factors for suicide in young adults in Taiwan. Int J Epidemiol. 42(5):1381–9. 10.1093/ije/dyt129 [DOI] [PubMed] [Google Scholar]
- 21.Chesney E, Goodwin GM, and Fazel S (2014) Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 13(2):153–60. 10.1002/wps.20128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chew KS and McCleary R (1994) A life course theory of suicide risk. Suicide Life Threat Behav. 24(3):234–44 [PubMed] [Google Scholar]
- 23.Class QA et al. (2014) Offspring psychopathology following preconception, prenatal and postnatal maternal bereavement stress. Psychol Med. 44(1):71–84. 10.1017/S0033291713000780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cnattingius S et al. (2011) Maternal smoking during pregnancy and risks of suicidal acts in young offspring. Eur J Epidemiol. 26(6):485–92. 10.1007/s10654-011-9556-7 [DOI] [PubMed] [Google Scholar]
- 25.Danziger PD, Silverwood R, and Koupil I (2011) Fetal growth, early life circumstances, and risk of suicide in late adulthood. Eur J Epidemiol. 26(7):571–81. 10.1007/s10654-011-9592-3 [DOI] [PubMed] [Google Scholar]
- 26.Davies C et al. (2020) Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 7(5):399–410. 10.1016/s2215-0366(20)30057-2 [DOI] [PubMed] [Google Scholar]
- 27.De Asis-Cruz J, Andescavage N, and Limperopoulos C (2021) Adverse Prenatal Exposures and Fetal Brain Development: Insights from Advanced Fetal MRI. Biol Psychiatry Cogn Neurosci Neuroimaging. 10.1016/j.bpsc.2021.11.009 [DOI] [PubMed] [Google Scholar]
- 28.Dias de Mattos Souza L et al. (2016) History of childhood trauma as risk factors to suicide risk in major depression. Psychiatry Res. 246:612–616. 10.1016/j.psychres.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 29.Ekblad M et al. (2010) Prenatal smoking exposure and the risk of psychiatric morbidity into young adulthood. Arch Gen Psychiatry. 67(8):841–9. 10.1001/archgenpsychiatry.2010.92 [DOI] [PubMed] [Google Scholar]
- 30.Ekeus C, Olausson PO, and Hjern A (2006) Psychiatric morbidity is related to parental age: a national cohort study. Psychol Med. 36(2):269–76. 10.1017/s0033291705006549 [DOI] [PubMed] [Google Scholar]
- 31.Fergusson DM, Woodward LJ, and Horwood LJ (2000) Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med. 30(1):23–39. 10.1017/s003329179900135x [DOI] [PubMed] [Google Scholar]
- 32.Franklin JC et al. (2017) Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 143(2):187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- 33.Geoffroy MC et al. (2018) Are early-life antecedents of suicide mortality associated with psychiatric disorders and suicidal ideation in midlife? Acta Psychiatr Scand. 137(2):116–124. 10.1111/acps.12844 [DOI] [PubMed] [Google Scholar]
- 34.Geoffroy MC, Gunnell D, and Power C (2014) Prenatal and childhood antecedents of suicide: 50-year follow-up of the 1958 British Birth Cohort study. Psychol Med. 44(6):1245–56. 10.1017/s003329171300189x [DOI] [PubMed] [Google Scholar]
- 35.Gilman SE et al. (2015) Contributions of the social environment to first-onset and recurrent mania. Mol Psychiatry. 20(3):329–36. 10.1038/mp.2014.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glover V (2011) Annual Research Review: Prenatal stress and the origins of psychopathology: an evolutionary perspective. J Child Psychol Psychiatry. 52(4):356–67. 10.1111/j.1469-7610.2011.02371.x [DOI] [PubMed] [Google Scholar]
- 37.Gluckman PD et al. (2009) Towards a new developmental synthesis: adaptive developmental plasticity and human disease. The Lancet. 373(9675):1654–1657. 10.1016/S0140-6736(09)60234-8 [DOI] [PubMed] [Google Scholar]
- 38.Gluckman PD et al. (2008) Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 359(1):61–73. 10.1056/NEJMra0708473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gravseth HM et al. (2010) Suicide in young Norwegians in a life course perspective: population-based cohort study. J Epidemiol Community Health. 64(5):407–12. 10.1136/jech.2008.083485 [DOI] [PubMed] [Google Scholar]
- 40.Gunnell D and Lewis G (2005) Studying suicide from the life course perspective: implications for prevention. Br J Psychiatry. 187:206–8. 10.1192/bjp.187.3.206 [DOI] [PubMed] [Google Scholar]
- 41.Gunnell D et al. (2011) School performance and risk of suicide in early adulthood: follow-up of two national cohorts of Swedish schoolchildren. J Affect Disord. 131(1–3):104–12. 10.1016/j.jad.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 42.Hansson Bittár N, Falkstedt D, and Sörberg Wallin A (2020) How intelligence and emotional control are related to suicidal behavior across the life course - A register-based study with 38-year follow-up. Psychol Med. 50(13):2265–2271. 10.1017/s0033291719002423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hartley CA and Somerville LH (2015) The neuroscience of adolescent decision-making. Curr Opin Behav Sci. 5:108–115. 10.1016/j.cobeha.2015.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hjern A and Allebeck P (2002) Suicide in first- and second-generation immigrants in Sweden: a comparative study. Soc Psychiatry Psychiatr Epidemiol. 37(9):423–9. 10.1007/s00127-002-0564-5 [DOI] [PubMed] [Google Scholar]
- 45.Hjern A, Lindblad F, and Vinnerljung B (2002) Suicide, psychiatric illness, and social maladjustment in intercountry adoptees in Sweden: a cohort study. The Lancet. 360(9331):443–448. 10.1016/s0140-6736(02)09674-5 [DOI] [PubMed] [Google Scholar]
- 46.Hjern A et al. (2020) Increased risk of suicidal behaviour in non-European international adoptees decreases with age - A Swedish national cohort study. EClinicalMedicine. 29-30:100643. 10.1016/j.eclinm.2020.100643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hjern A, Vinnerljung B, and Lindblad F (2004) Avoidable mortality among child welfare recipients and intercountry adoptees: a national cohort study. J Epidemiol Community Health. 58(5):412–7. 10.1136/jech.2003.014282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huda MM et al. (2021) Time trends and sociodemographic inequalities in the prevalence of adolescent motherhood in 74 low-income and middle-income countries: a population-based study. The Lancet Child & Adolescent Health. 5(1):26–36. 10.1016/S2352-4642(20)30311-4 [DOI] [PubMed] [Google Scholar]
- 49.Iribarren C et al. (2000) Hospitalization for suicide attempt and completed suicide: epidemiological features in a managed care population. Soc Psychiatry Psychiatr Epidemiol. 35(7):288–96. 10.1007/s001270050241 [DOI] [PubMed] [Google Scholar]
- 50.Jacobson B and Bygdeman M (1998) Obstetric care and proneness of offspring to suicide as adults: case-control study. Bmj. 317(7169):1346–9. 10.1136/bmj.317.7169.1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Katz C et al. (2013) A SYSTEMATIC REVIEW OF SCHOOL-BASED SUICIDE PREVENTION PROGRAMS. Depression and Anxiety. 30(10):1030–1045. 10.1002/da.22114 [DOI] [PubMed] [Google Scholar]
- 52.Kessler RC et al. (2007) Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 20(4):359–64. 10.1097/YCO.0b013e32816ebc8c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kessler RC, Borges G, and Walters EE (1999) Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 56(7):617–26. 10.1001/archpsyc.56.7.617 [DOI] [PubMed] [Google Scholar]
- 54.Korhonen LM et al. (2019) Suicides and deaths linked to risky health behavior in childhood cancer patients: A Nordic population-based register study. Cancer. 125(20):3631–3638. 10.1002/cncr.32373 [DOI] [PubMed] [Google Scholar]
- 55.Lahti M et al. (2015) Late preterm birth, post-term birth, and abnormal fetal growth as risk factors for severe mental disorders from early to late adulthood. Psychol Med. 45(5):985–99. 10.1017/S0033291714001998 [DOI] [PubMed] [Google Scholar]
- 56.Lahti M et al. (2014) Maternal Grand Multiparity and the Risk of Severe Mental Disorders in Adult Offspring. PLoS One. 9(12):e114679. 10.1371/journal.pone.0114679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Latimer K et al. (2012) Disruptive behaviour disorders: a systematic review of environmental antenatal and early years risk factors. Child Care Health Dev. 38(5):611–28. 10.1111/j.1365-2214.2012.01366.x [DOI] [PubMed] [Google Scholar]
- 58.Li CI, Daling JR, and Emanuel I (2003) Birthweight and risk of overall and cause-specific childhood mortality. Paediatr Perinat Epidemiol. 17(2):164–70. 10.1046/j.1365-3016.2003.00487.x [DOI] [PubMed] [Google Scholar]
- 59.Li Z et al. (2011) Attributable risk of psychiatric and socio-economic factors for suicide from individual-level, population-based studies: A systematic review. Social Science & Medicine. 72(4):608–616. 10.1016/j.socscimed.2010.11.008 [DOI] [PubMed] [Google Scholar]
- 60.Lim M, Lee SU, and Park JI (2014) Difference in suicide methods used between suicide attempters and suicide completers. Int J Ment Health Syst. 8(1):54. 10.1186/1752-4458-8-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Matsubayashi T and Ueda M (2011) The effect of national suicide prevention programs on suicide rates in 21 OECD nations. Soc Sci Med. 73(9):1395–400. 10.1016/j.socscimed.2011.08.022 [DOI] [PubMed] [Google Scholar]
- 62.McLaughlin KA et al. (2010) Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 40(10):1647–58. 10.1017/s0033291709992121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miller B et al. (2010) Advanced paternal age, mortality, and suicide in the general population. J Nerv Ment Dis. 198(6):404–11. 10.1097/NMD.0b013e3181e07d79 [DOI] [PubMed] [Google Scholar]
- 64.Miller B et al. (2010) Paternal age and mortality in nonaffective psychosis. Schizophr Res. 121(1–3):218–26. 10.1016/j.schres.2010.01.020 [DOI] [PubMed] [Google Scholar]
- 65.Mittendorfer-Rutz E, Rasmussen F, and Wasserman D (2004) Restricted fetal growth and adverse maternal psychosocial and socioeconomic conditions as risk factors for suicidal behaviour of offspring: a cohort study. Lancet. 364(9440):1135–40. 10.1016/s0140-6736(04)17099-2 [DOI] [PubMed] [Google Scholar]
- 66.Mok PLH et al. (2017) Younger or older parental age and risk of suicidality, premature death, psychiatric illness, and criminality in offspring. J Affect Disord. 208:130–138. 10.1016/j.jad.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Naghavi M (2019) Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. BMJ. 364:l94. 10.1136/bmj.l94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Neeleman J, Wessely S, and Wadsworth M (1998) Predictors of suicide, accidental death, and premature natural death in a general-population birth cohort. Lancet. 351(9096):93–7. 10.1016/s0140-6736(97)06364-2 [DOI] [PubMed] [Google Scholar]
- 69.Neugebauer R and Reuss ML (1998) Association of maternal, antenatal and perinatal complications with suicide in adolescence and young adulthood. Acta Psychiatr Scand. 97(6):412–8. 10.1111/j.1600-0447.1998.tb10024.x [DOI] [PubMed] [Google Scholar]
- 70.Niederkrotenthaler T et al. (2012) Exposure to parental mortality and markers of morbidity, and the risks of attempted and completed suicide in offspring: an analysis of sensitive life periods. J Epidemiol Community Health. 66(3):233–9. 10.1136/jech.2010.109595 [DOI] [PubMed] [Google Scholar]
- 71.Niederkrotenthaler T, Rasmussen F, and Mittendorfer-Rutz E (2012) Perinatal conditions and parental age at birth as risk markers for subsequent suicide attempt and suicide: a population based case-control study. Eur J Epidemiol. 27(9):729–38. 10.1007/s10654-012-9724-4 [DOI] [PubMed] [Google Scholar]
- 72.O’Donnell KJ and Meaney MJ (2017) Fetal Origins of Mental Health: The Developmental Origins of Health and Disease Hypothesis. Am J Psychiatry. 174(4):319–328. 10.1176/appi.ajp.2016.16020138 [DOI] [PubMed] [Google Scholar]
- 73.Orri M et al. (2019) In-utero and perinatal influences on suicide risk: a systematic review and meta-analysis. Lancet Psychiatry. 6(6):477–492. 10.1016/S2215-0366(19)30077-X [DOI] [PubMed] [Google Scholar]
- 74.Osler M, Nybo Andersen AM, and Nordentoft M (2008) Impaired childhood development and suicidal behaviour in a cohort of Danish men born in 1953. J Epidemiol Community Health. 62(1):23–8. 10.1136/jech.2006.053330 [DOI] [PubMed] [Google Scholar]
- 75.Page MJ et al. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Parra Uribe I et al. (2013) Attempted and completed suicide: not what we expected? J Affect Disord. 150(3):840–6. 10.1016/j.jad.2013.03.013 [DOI] [PubMed] [Google Scholar]
- 77.Raikkonen K and Pesonen AK (2009) Early life origins of psychological development and mental health. Scand J Psychol. 50(6):583–91. 10.1111/j.1467-9450.2009.00786.x [DOI] [PubMed] [Google Scholar]
- 78.Richard-Devantoy S et al. (2019) Childhood cognitive skill trajectories and suicide by mid-adulthood: an investigation of the 1958 British Birth Cohort. Psychol Med:1–8. 10.1017/S0033291719003143 [DOI] [PubMed] [Google Scholar]
- 79.Richard YF et al. (2015) The association between traumatic brain injury and suicide: are kids at risk? Am J Epidemiol. 182(2):177–84. 10.1093/aje/kwv014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Riordan DV et al. (2012) Family size and perinatal circumstances, as mental health risk factors in a Scottish birth cohort. Soc Psychiatry Psychiatr Epidemiol. 47(6):975–83. 10.1007/s00127-011-0405-5 [DOI] [PubMed] [Google Scholar]
- 81.Riordan DV et al. (2006) Perinatal circumstances and risk of offspring suicide. Birth cohort study. Br J Psychiatry. 189:502–7. 10.1192/bjp.bp.105.015974 [DOI] [PubMed] [Google Scholar]
- 82.Risnes KR et al. (2016) Premature Adult Death in Individuals Born Preterm: A Sibling Comparison in a Prospective Nationwide Follow-Up Study. PLoS One. 11(11):e0165051. 10.1371/journal.pone.0165051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rojas Y and Stenberg S-Å (2010) Early life circumstances and male suicide—A 30-year follow-up of a Stockholm cohort born in 1953. Social Science & Medicine. 70(3):420–427. 10.1016/j.socscimed.2009.10.026 [DOI] [PubMed] [Google Scholar]
- 84.Rostila M, Saarela J, and Kawachi I (2014) Birth order and suicide in adulthood: evidence from Swedish population data. Am J Epidemiol. 179(12):1450–7. 10.1093/aje/kwu090 [DOI] [PubMed] [Google Scholar]
- 85.Saarela J, Cederstrom A, and Rostila M (2016) Birth order and mortality in two ethno-linguistic groups: Register-based evidence from Finland. Soc Sci Med. 158:8–13. 10.1016/j.socscimed.2016.04.008 [DOI] [PubMed] [Google Scholar]
- 86.Salib E and Cortina-Borja M (2006) Effect of month of birth on the risk of suicide. Br J Psychiatry. 188:416–22. 10.1192/bjp.bp.105.009118 [DOI] [PubMed] [Google Scholar]
- 87.Salib E and Cortina-Borja M (2010) An association between month of birth and method of suicide. Int J Psychiatry Clin Pract. 14(1):8–17. 10.3109/13651500903261323 [DOI] [PubMed] [Google Scholar]
- 88.Salk L et al. (1985) RELATIONSHIP OF MATERNAL AND PERINATAL CONDITIONS TO EVENTUAL ADOLESCENT SUICIDE. The Lancet. 325(8429):624–627. 10.1016/S0140-6736(85)92156-7 [DOI] [PubMed] [Google Scholar]
- 89.Schlotz W and Phillips DI (2009) Fetal origins of mental health: evidence and mechanisms. Brain Behav Immun. 23(7):905–16. 10.1016/j.bbi.2009.02.001 [DOI] [PubMed] [Google Scholar]
- 90.Sciberras E et al. (2017) Prenatal Risk Factors and the Etiology of ADHD-Review of Existing Evidence. Curr Psychiatry Rep. 19(1):1. 10.1007/s11920-017-0753-2 [DOI] [PubMed] [Google Scholar]
- 91.Sorensen HJ et al. (2009) Suicide and mental illness in parents and risk of suicide in offspring: a birth cohort study. Soc Psychiatry Psychiatr Epidemiol. 44(9):748–51. 10.1007/s00127-009-0495-5 [DOI] [PubMed] [Google Scholar]
- 92.Spicer RS and Miller TR (2000) Suicide acts in 8 states: incidence and case fatality rates by demographics and method. Am J Public Health. 90(12):1885–91. 10.2105/ajph.90.12.1885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Steck N et al. (2018) Suicide in adolescents: findings from the Swiss National cohort. Eur Child Adolesc Psychiatry. 27(1):47–56. 10.1007/s00787-017-1019-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Stenbacka M and Jokinen J (2015) Violent and non-violent methods of attempted and completed suicide in Swedish young men: the role of early risk factors. BMC Psychiatry. 15:196. 10.1186/s12888-015-0570-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Strand BH and Kunst A (2007) Childhood socioeconomic position and cause-specific mortality in early adulthood. Am J Epidemiol. 165(1):85–93. 10.1093/aje/kwj352 [DOI] [PubMed] [Google Scholar]
- 96.Su Y, D’Arcy C, and Meng X (2020) Research Review: Developmental origins of depression - a systematic review and meta-analysis. J Child Psychol Psychiatry. 10.1111/jcpp.13358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Suvisaari J et al. (2008) Mortality in offspring of mothers with psychotic disorder. Psychol Med. 38(8):1203–10. 10.1017/s0033291707002383 [DOI] [PubMed] [Google Scholar]
- 98.Too LS et al. (2019) The association between mental disorders and suicide: A systematic review and meta-analysis of record linkage studies. Journal of Affective Disorders. 259:302–313. 10.1016/j.jad.2019.08.054 [DOI] [PubMed] [Google Scholar]
- 99.Turecki G et al. (2012) The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 35(1):14–23. 10.1016/j.tins.2011.11.008 [DOI] [PubMed] [Google Scholar]
- 100.von Borczyskowski A et al. (2010) Gender differences in risk factors for suicide: findings from a Swedish national cohort study. Can J Psychiatry. 55(2):108–11. 10.1177/070674371005500207 [DOI] [PubMed] [Google Scholar]
- 101.von Borczyskowski A et al. (2011) Familial factors and suicide: an adoption study in a Swedish National Cohort. Psychol Med. 41(4):749–58. 10.1017/s0033291710001315 [DOI] [PubMed] [Google Scholar]
- 102.Wells GA et al. , The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000, Oxford. [Google Scholar]
- 103.Wilcox HC et al. (2010) “Psychiatric morbidity, violent crime, and suicide among children and adolescents exposed to parental death”: Corrigendum. Journal of the American Academy of Child & Adolescent Psychiatry. 49(8):858–858. 10.1016/j.jaac.2010.06.014 [DOI] [PubMed] [Google Scholar]
- 104.Zambon F et al. (2011) Youth suicide: an insight into previous hospitalisation for injury and sociodemographic conditions from a nationwide cohort study. Inj Prev. 17(3):176–81. 10.1136/ip.2010.030080 [DOI] [PubMed] [Google Scholar]
- 105.Zammit S et al. (2014) Individual- and area-level influence on suicide risk: a multilevel longitudinal study of Swedish schoolchildren. Psychol Med. 44(2):267–77. 10.1017/s0033291713000743 [DOI] [PubMed] [Google Scholar]
- 106.Ziker JP and Snopkowski K (2020) Life-History Factors Influence Teenagers’ Suicidal Ideation: A Model Selection Analysis of the Canadian National Longitudinal Survey of Children and Youth. Evolutionary Psychology. 18(3):1474704920939521. 10.1177/1474704920939521 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Protocol of systematic review and search strategy is included in the Online Resource


