Abstract
Cannabinoids are compounds isolated from cannabis and are also widely present in both nervous and immune systems of animals. In recent years, with in-depth research on cannabinoids, their clinical medicinal value has been evaluated, and many exciting achievements have been continuously accumulating, especially in the field of neurodegenerative disease. Alzheimer's disease is the most common type of neurodegenerative disease that causes dementia and has become a global health problem that seriously impacts human health today. In this review, we discuss the therapeutic potential of cannabinoids for the treatment of Alzheimer’s disease. How cannabinoids act on different endocannabinoid receptor subtypes to regulate Alzheimer’s disease and the roles of the endocannabinoid system in Alzheimer’s disease are outlined, and the underlying mechanisms are discussed. Finally, we summarize the most relevant opportunities of cannabinoid pharmacology related to Alzheimer’s disease and discuss the potential usefulness of cannabinoids in the clinical treatment of Alzheimer’s disease.
Keywords: Cannabinoids, CB1 receptor, CB2 receptor, endocannabinoid, neurodegenerative diseases, Alzheimer's disease
1. INTRODUCTION
Neurodegenerative diseases are a group of heterogeneous diseases characterized by the progressive and selective loss of anatomically- or physiologically-related neuronal systems [1]. Alzheimer’s disease (AD) is a highly complicated neurodegenerative disease that seriously affects human health. It was first described by German neuroscientist Alois Alzheimer in a 51-year-old patient Auguste Deter, who suffered from severe memory loss. During the autopsy of this patient, plaques and tangles in the cerebral cortex were found [2]. Subsequent studies have revealed that the histopathological features of AD involve the accumulation of β-amyloid (Aβ), intracellular aggregation of neurofibrillary tangles (NFTs), loss of a specific subset of neurons, and neuroinflammation resulting from glial activation [3-5]. Aβ and NFT are considered the main causes of disease progression; therefore, amyloid and phosphorylated microtubule-related tau proteins have become important targets for AD research. The production of amyloid begins with the cleavage of amyloid precursor protein (APP) on the plasma membrane by β-secretase (BACE1) and γ-secretase to produce insoluble Aβ fibrils. Then insoluble Aβ fibrils form oligomers, diffuse into the synaptic cleft, and interfere with synaptic signaling [6-8]. In AD patients, Aβ plaques are initially found in the basal, temporal lobe, and orbitofrontal neocortex areas of the brain and later spread throughout the entire neocortex, hippocampus, amygdala, diencephalon, and basal ganglia [9, 10]. In severe cases, Aβ is also found in the midbrain, lower brainstem, and cerebellar cortex, indicating that the accumulation of Aβ plaques is positively correlated with the course of AD [9, 10]. High concentrations of Aβ cause kinases to hyper-phosphorylate and activate microtubule-associated tau proteins, causing tau proteins to aggregate into insoluble NFTs. After plaques and tangles accumulate, microglia gather around the plaques. This promotes the activation of microglia and local inflammation and aggravates neurotoxicity, eventually leading to cognitive decline [11]. Importantly, AD is associated with an early loss of synaptic proteins, and the levels and distributions of some synaptic proteins have been found to be associated with dementia severity [12].
It has long been hypothesized that Aβ exerts toxicity in brain neurons [13, 14]. Although existing evidence reveals the harmful effects of Aβ on cellular Ca2+ homeostasis, neurotransmission, neuronal signaling, and receptor/ion channel function [15], the precise mechanisms of Aβ toxicity are still unclear. Particularly, which targets specifically mediate Aβ toxicity are still elusive. At present, the true causes of AD are still unclear, and even though decades of research have been conducted, there is still no drug that can effectively slow down the progression and improve the learning and memory deficits in Alzheimer's disease [16, 17]. Aβ accumulation and aggregation in neuritic or senile plaques and severe, selective cholinergic neuronal deficits are characteristic hallmarks of AD [13]. The extent of learning and memory deficits in AD is proportional to the degree of forebrain cholinergic neuronal degeneration, and the extent of Aβ deposition is used to characterize disease severity [13]. Processes, such as impairment of neurotrophic support and disorders of glucose metabolism, have been implicated in cholinergic neuronal loss and AD [18]. However, neurotoxic effects of Aβ across a range of in vivo or in vitro models suggested that Aβ plays a role in cholinergic neuronal degeneration and consequent learning and memory deficits [13, 19]; however, their mechanisms are still unclear. Therefore, understanding of such mechanisms is significant to help improve AD diagnosis and treatment.
Emerging lines of evidence indicate that a high level of Aβ induces neuronal or neurocircuit hyperexcitation. For example, chronic exposure to high levels of Aβ sensitizes some neuronal networks to hyperexcitation [20]. In animals that over-express Aβ, the high levels of Aβ peptide cause epileptiform activity within the entorhinal-hippocampal circuitry [21]. Westmark et al. compared seizure threshold (test response to pentylenetetrazol, PTZ) between AD model animals (Tg2576) and wild-type mice, and found a reduction in seizure threshold in AD model animals [22]. These shreds of evidence suggest that Aβ induces neuronal hyperexcitation, and reduction of this hyperexcitation may play a role in preventing/improving the pathogenesis of AD and could also open new therapeutic avenues. The cannabinoid system may perfectly fix this problem.
Thus far, there are 2 types of US FDA-approved drugs for the treatment of AD based on acetylcholinesterase inhibitors (donepezil, galantamine, and rivastigmine) [23] and NMDA receptor antagonists (memantine) [24]. All of these drugs are only symptomatic treatments, and none can prevent or delay the progression of AD, let alone cure AD [25], and unfortunately, promising preclinical results have repeatedly failed to be translated into clinical applications [26]. Although Aduhelm (aducanumab) has been approved recently by the FDA, its efficacy is still questionable [27].
Cannabis, as a controversial drug, has become increasingly prominent in the AD research field [28-30]. In the late 20th century, the first cannabis-derived compound was approved for clinical use, and subsequently, it was approved for treating neurological disorders [31-34]. For example, the approvals of nabiximols, a mixture of THC and the non-psychotropic cannabinoid, cannabidiol, for the treatment of spasticity and neuropathic pain in multiple sclerosis, and purified botanical cannabidiol for the treatment of otherwise untreatable forms of pediatric epilepsy have suggested a potential for clinical use of cannabinoids and endocannabinoids in neurological diseases [33]. Low concentrations of Δ9-tetrahydrocannabinol (THC) can reduce the Aβ level of N2a-variant amyloid-β protein precursor (APP) cells and inhibit Aβ aggregation by directly interacting with Aβ peptide [35]. THC attenuates Aβ accumulation in the human CNS cell line (MC65 cells) in a model whereby an inducible Aβ protein exerts toxicity through an inflammatory response [36]. In addition, THC can competitively inhibit enzyme acetylcholinesterase (AChE) by binding to its peripheral anion sites, thereby increasing ACh levels and reducing Aβ-peptide aggregation induced by AChE [37]. Furthermore, it was found that pretreatment with cannabidiol (CBD) can inhibit the expression of proteins involved in tau phosphorylation and Aβ production in gingival mesenchymal stem cells [38]. Therefore, it is suggested that cannabis can be used as a novel potential drug for the treatment of AD. In this review, we summarize recent discoveries and developments of cannabinoids and analyze the data of cannabinoids that regulate AD through the activation of cannabinoid receptor type 1 (CB1) receptors, cannabinoid receptor type 2 (CB2) receptors, and the endocannabinoid system.
2. CANNABIS, CB1, AND CB2 RECEPTORS
The earliest use of cannabis as a drug can be traced back to around 2350 BC [39]. Cannabis contains a variety of compounds. The main components of cannabinoids are cannabidiol (CBD) and THC, both of which are lipophilic metabolites of resorcinol [40]. CBD was isolated in the late 1930s, but it was not until 1963 that the structure was defined [41] and identified as the active substance in hashish [42].
With in-depth studies on THC, the cannabinoid type 1 receptor (CB1R) was discovered in 1988 [43], and then the endogenous cannabinoid N-arachidonoyl-ethanolamine (AEA) was discovered in 1992 [44]. Later, a second endocannabinoid 2-arachidonic acid glyceride (2-AG) was identified [45]. These two endocannabinoids are derivatives of arachidonic acid, and they have different syntheses and metabolisms by different pathways.
Howlett was the first to report that cannabinoids may inhibit the formation of cAMP through receptors, and the efficacy of the cannabinoids examined is parallel to the level of their pharmacological effects [46]. Subsequently, the CB1R was cloned in 1990 [47]. Later, the cannabinoid type 2 receptor (CB2R) was found in the spleen in 1993 [48].
CB1R belongs to the superfamily of G protein-coupled receptors (GPCRs). The expressions of CB1Rs are distributed throughout the body in mammals, with CB1R expression highest in the basal ganglia in the central nervous system (CNS), including the substantia nigra (SNr), globus pallidus, hippocampal dentate gyrus, and the molecular layer of the cerebellum [49, 50], while the density of CB1Rs observed in the main sensory and motor areas is much lower [51, 52], suggesting that CB1Rs are involved in motivation (marginal) and cognitive (associative) information processing. Table 1 summarizes the CB1R distribution.
Table 1.
The expression trend of CB1Rs in various neurological diseases.
| Brain Regions | Tendency | Species | Neurological Disorders | References |
|---|---|---|---|---|
| Prefrontal cortex, hippocampus, and caudate putamen |
Decrease | Humans | AD | [53-55] |
| Dorsal hippocampus (DH), basolateral amygdala complex (BLA) | Decrease | Mice(model) | 12-month-old AD | [56] |
| Cerebellum, dentate nucleus | Decrease | Mice(model) | Cerebellar ataxia | [57, 58] |
| Striatum | Decrease | Mice(model) | Huntington's disease | [59, 60] |
| Prefrontal and midcingulate cortex | Decrease | Humans, rat (model) |
Parkinson's disease | [61-63] |
Cannabinoid receptor type 2 (CB2) is a plasma membrane G-protein-coupled receptor cloned in 1993 [64]. Since then, the expression and function of CB2Rs in the brain have been debated. Previous studies suggested that CB2Rs were absent in the brain since CB2 mRNA transcripts were not detected in rat brain using in situ hybridization (ISH) [48]. Consistent with this finding, Northern blot analysis also failed to detect CB2 mRNA in rat, mouse, and human brains [65-67]. Real-time polymerase chain reaction (RT-PCR) assays demonstrated abundant CB2 mRNA among immune tissues, such as the spleen and on macrophages, but barely detectable levels in rat and mouse brains [65, 66, 68, 69]. Based on these findings, CB2Rs have been classically considered ‘peripheral cannabinoid receptors’ [48, 70, 71]. Recently, this concept has been challenged by the identification of CB2Rs throughout the central nervous system (CNS) [72-74], particularly in microglial cells [75, 76], though they are expressed at lower densities than CB1Rs. When compared to CB1Rs, central CB2Rs exhibit the following unique features: (1) Lower expression levels, suggesting that these receptors may not mediate the effect of cannabis under normal physiological conditions, (2) Highly inducible, meaning that under certain pathological conditions (e.g., addiction, inflammation, stroke, schizophrenia, stress, anxiety, etc.), CB2R expression is enhanced in the brain [77], suggesting a close relationship between the alteration of CB2R expression/function and various psychiatric and neurological diseases, and (3) Exhibit special distribution, given that CB2Rs are chiefly expressed in neuronal somatodendritic areas [74] (postsynaptic) but CB1Rs are predominantly expressed on neuronal terminals, especially on GABAergic terminals (presynaptic), which leads to some opposing effects after activation by these two receptor subtypes [78]. Considering these characteristic features, the CB2R appears to be an important substrate for neuroprotection [79], and targeting CB2Rs will likely offer a novel therapeutic strategy for treating neuropsychiatric and neurological diseases without typical CB1R-mediated side-effects. Given these positive implications, an urgent need to understand the functional effects of CB2Rs in the brain, especially in the mesocorticolimbic system, has emerged within the scientific community.
Emerging evidence shows that significant CB2 mRNA has been detected by ISH in cultured granule cells among the granule layer and Purkinje cell layer of the mouse cerebellum [80], in mouse retina [81], and the globus pallidus of non-human primates [82]. RT-PCR analysis has also been used to detect CB2 mRNA expression in various brain regions, including the retina [81], cortex [82-85], striatum [66, 85], hippocampus [82], amygdala [84, 85], brainstem [72], and cerebellum [86]. Furthermore, two CB2 mRNA transcripts (CB2A and CB2B) have been identified in the rodent and human brain [83], along with a new CB2 transcript that has been found in mouse and human B lymphocytes [87]. Moreover, immunoblot and IHC assays have detected significant CB2-like bands or immunostaining in various brain regions [72, 73, 88-90]. This suggests a possibility that CB2R expression not only exists in peripheral tissues but also in the brain. As mentioned previously, CB2Rs mediate a variety of important modulations in DA-associated behaviors [91], including food intake, body weight [92-95], depression [96], anxiety [84, 97], and schizophrenia-like behavior [85, 98]. Recent reports emerging from several labs, including ours, have shown that brain CB2Rs play a pivotal role in the elimination of cocaine, alcohol, and nicotine addiction [99-101]. Collectively, these lines of evidence strongly suggest an important impact of CB2Rs on the mesocorticolimbic system as well as critical roles in various brain functions, including psychiatric, cognitive, and neurobiological activity. Table 2 summarizes CB2R distribution.
Table 2.
The expression trend of CB2Rs in various neurological diseases.
| Brain Regions | Tendency | Species | Neurological Disorders | References |
|---|---|---|---|---|
| Hippocampus and entorhinal and parahippocampal cortices |
Increase | Humans and mice (model) | AD | [34, 55, 102] |
| Granular layer, Purkinje cells | Increase | Humans | Spinocerebellar ataxias | [103, 104] |
| Striatal microglia | Increase | Humans and mice (model) | Huntington's disease | [105, 106] |
| Substantia nigra microglial cells, striatal | Increase | Humans, rat (model) and mice (model) | Parkinson's disease | [107-109] |
| Spinal cord microglia | Increase | Mice (model) | Amyotrophic lateral sclerosis | [110] |
It has been shown that CB2Rs play an important role in neural precursor cell proliferation, axonal guidance, and synaptic transmission [111, 112]. As a G protein-coupled receptor, signal transduction initiated by the CB2R is mediated by Gi/o [113], increasing intracellular calcium levels by activating the phospholipase C (PLC) and inositol 1,4,5-trisphosphate (IP3) signaling pathways [114]. CB2Rs inhibit cAMP, thereby reducing intracellular cAMP levels [115]. In addition, CB2R activation can also be combined with other cellular pathways, including PKA, ERK1/2, and P38 [116, 117]. In contrast to CB1Rs, CB2R expression in the brain is relatively low, but it is highly inducible under pathological conditions, suggesting that CB2Rs are related to many neurological diseases [77, 118], and CB2Rs are mainly expressed in the postsynaptic soma dendritic region, so the activation of CB2Rs has an important protective effect on neurons [118, 119].
3. EFFECTS OF CB1RS ON AD PATHOGENESIS AND THERAPEUTICS
Cognitive deficits are a significant feature in AD patients, and the brain areas related to learning and cognition are rich in CB1Rs [51, 52]. Analysis of brain tissue samples from AD patients showed that the density of CB1Rs in the brains of AD patients is reduced, especially in the frontal cortex [54, 55]. Correlation analysis of neuropathological studies showed that the CB1R level of cortical brain tissue after death in AD patients is found to be lower than that of the age-matched controls [55]. In experimental animal models, reduction of CB1R expression lowers the PSD-95 protein level and aggravates learning and memory dysfunction in APP/PS1 transgenic mice, indicating that CB1Rs protect against AD-related pathological events and play a key role in AD progression [120]. In the triple transgenic mouse model of AD (3xTg-AD), CB1R activity is up-regulated in the anterior part of the thalamus at 4 months of age, while its activity in the basal nucleus of Meynert decreases at 15 months of age [121]. This is consistent with the different degrees of nitrification of CBRs in the late course of AD [54].
It has been reported that treatment with Δ9-THC significantly reduces Aβ plaques in APP transgenic mice, which may be due to the activation of the neutrophil (an Aβ-degrading enzyme) [30]. It has been found that WIN-55,212-2 (CB1R agonist) can rescue AD-like pathological features and learning deficits caused by intracerebroventricular injection of Aβ25–35 in rats [54]. In addition, another study reported that the endocannabinoid receptor system (ECBS) activates peroxisome proliferator-activated γ receptor (PPAR-γ) by activating CB1Rs, which, in turn, stimulate the expression of lipoprotein receptor protein 1 (LRP1) that has been shown to play an important role in the brain-blood transport of Aβ [122] to increase the clearance of Aβ across the blood-brain barrier [123]. It has also been reported that CB1R deficiency can aggravate AD-related cognitive deficits in AD animal models; CB1R-deficient mice showed a decrease in the number of APP plaques and its fragments [124]. However, compared to APP23 mice with intact CB1Rs, APP23/CB1(-/-) mice exhibited learning and memory impairment.
Bilateral injection of Aβ in the prefrontal cortex will cause a significant change in the activity-dependent electrophysiological response of hippocampal CA1 pyramidal neurons. It was reported that the combination therapy with ACEA (a selective CB1R agonist) almost completely prevented the effects of Aβ treatment alone [125]. Whole-cell patch-clamp recordings showed that in the absence of synaptic input, the intrinsic action potential (AP) frequency was reduced, and the discharge irregularity increased in the Aβ treatment group. Aβ treatment also induced significant changes in spontaneous and evoked neuronal responses. However, co-treatment with ACEA enabled almost complete retention of the normal intrinsic electrophysiological properties of pyramidal cells [125]. ACEA was also found to reduce the cytotoxic effects of Aβ42 oligomers in primary cultures of cortical neurons and reverse the Aβ-induced glycogen synthase kinase-3β (GSK3β) dephosphorylation in vitro and in vivo [126]. Moreover, compared with age-matched vehicle-treated APP transgenic mice, ACEA-treated mice showed a reduced astrocytic response near Aβ plaques and decreased expression of the proinflammatory cytokine interferon-γ in astrocytes. ACEA is present in both the neurons, which mediate at least in part by GSK3β inhibition, and the glia, resulting in decreased reactive astrocytes and reduced interferon-γ expression [126, 127]. Therefore, with the progression of AD, the expression of CB1R gradually decreases, and early CB1R activation can reduce the deposition of Aβ plaques, decrease neurotoxicity, and rescue learning and memory deficits. This suggests that targeted activation of CB1Rs might provide a novel approach to treat AD.
4. EFFECTS OF CB2RS ON AD PATHOGENESIS AND THERAPEUTICS
Changes in the expression of ECB receptors during the pathogenesis of AD may be time-dependent. In this regard, CB1 and CB2 have different expression patterns. CB1Rs in the hippocampus and frontal lobe show higher levels of activity in the early stages of AD, but their activity decreases as the disease progresses [104, 128]. In contrast, in the late stage of AD, the expression of CB2Rs is found to be higher when neuroinflammation is more pronounced, and microglia and astrocytes are activated [128].
The upregulation of CB2R and its preferential distribution near Aβ plaques have been reported in several AD animal models and postmortem studies, suggesting that CB2R expression is induced in the course of AD [54, 55, 102]. Activation of these receptors stimulates the removal of amyloid by macrophages [129]. It has been reported that activation of CB2R up-regulates PPARγ signaling and attenuates Aβ-induced neuroinflammation, neurodegeneration, and spatial memory impairment in animals [130]. It was found that CB2R agonist JWH-133 reduced Thr181 tau phosphorylation, as well as the expression of GSK3β, p38, and the active form of SAPK/JNK in APP/PS1 mice [131], and also reduced the levels of superoxide dismutase (SOD) 1 and 2 in APP/PS1 mice [132]. Treating AD mice with 1-phenylisatin (a selective modulator of CB2R) can prevent streptozotocin and aluminum trichloride + d-galactose-induced learning and memory impairment and brain damage [133]. Long-term oral administration of two different cannabinoid agonists (WIN 55,212-2 and JWH-133) was found to rescue neuroinflammation, reduce Aβ levels, and improve the cognitive ability of Tg APP 2576 mice [134]. Activating CB2Rs with a lower dose of JWH-015 could remove natural Aβ from human tissue sections and stimulate the human THP-1 macrophage cell line, but not U373MG astrocytoma cells, to endocytose synthetic pathogenic Aβ peptides bound to a culture dish, and this effect was reversed by the selective CB2R antagonist SR144528 [129]. In addition, lack of CB2Rs failed to change tau phosphorylation in mice [135]. In J20APP mice, the lack of CB2Rs reduced total tau without exerting any effects on tau phosphorylation [136]. These results suggested that activation of CB2Rs can reduce tau phosphorylation and help the clearance of Aβ plaques.
In addition, studies have shown that the enhanced coupling of cannabinoid receptor/effector levels in the hippocampus and frontal cortex of mice decreases significantly with age [137], which may be related to the nitrosylation of receptors, which may cause damage to the connection between the receptor and its effectors during the course of AD [54]. This is consistent with a study that found that the availability of CB2Rs in AD patients is reduced compared to healthy individuals [138].
In the APP/PS1 AD mouse model, loss of CB2Rs reduces the activation of microglia and the infiltration of macrophages. In addition, these mice express low levels of pro-inflammatory chemokines and cytokines in the brain, as well as reduced concentrations of soluble Aβ 40/42 [139]. It has been reported that CB2R activation converts microglia from the M1 to M2 phenotype [140] and facilitates phagocytosis [141]. In addition, a new type of CB2R agonist (MDA7) provides protection against Aβ fibril-induced activation of microglia and astrocytes, normalizes CB2R expression, promotes Aβ clearance, weakens synaptic plasticity defects, and impairs learning and memory [142]. In an in vitro experiment, selective CB2 agonists prevented the Aβ-induced release of pro-inflammatory cytokines by reducing intracellular calcium concentration and enhancing microglia phagocytosis [143]. The activation of CB2Rs by JWH-015 increases Aβ-induced astrocyte proliferation in cell culture [144]. It has been shown that administration of the CB2R agonist JWH-133 prevented the activation of microglia and the release of pro-inflammatory cytokines near Aβ deposits in APP transgenic mice [132]. In addition, Aβ-induced CD40-mediated phagocytosis of microglia was found to be inhibited by the CB2R agonist JWH-015 [145]. A specific role for CB2Rs in the modulation of tau is suggested by the potentiation of autophagy and improvement in the redox state. Recently, we have shown that in a hippocampal culture cell model, JWH-133 significantly prevented chronic Aβ-induced neuronal toxicity [146], supporting the idea that CB2Rs possess a neuroprotective effect against chronic Aβ-induced neuronal degeneration.
5. EFFECTS OF ENDOCANNABINOIDS ON AD PATHOGENESIS AND THERAPEUTICS
Two primary endocannabinoids in brain tissue (anandamide and 2-arachidonylglycerol) have been identified as CB1R and CB2R agonists [44, 147, 148]. The neuroprotective effects of endocannabinoids may be due to interference with several cellular and molecular mechanisms, including apoptosis and inflammation [149, 150]. The progression of AD is related to the changes in the endocannabinoid system [151, 152]. Both cannabinoid receptor agonists and endocannabinoids, such as AEA, can reduce the neurotoxicity caused by Aβ-peptide in a mitogen-activated protein kinase (MAPK) pathway in a dependent manner by activating CB1Rs to protect human NTERA-2/cl-D1 teratocarcinoma cells [153].
Studies have reported that 8-month-old Aβ APPswe/ PS1ΔE9 mice have lower 2-AG levels than wild-type mice in the striatum [137]. 2-AG treatment can prevent Aβ-induced hemichannel activity and inflammatory characteristics in astrocytes and neuronal damage caused by excitotoxic glutamate release in hippocampal slices treated with Aβ [154]. Furthermore, early administration of 2-AG reuptake inhibitor (VDM11) can prevent hippocampal damage and memory loss in rats [155]. Increasing 2-AG by inhibiting MAGL can prevent APP/PS1 prostaglandin (PGE2) production in mice, as well as neuroinflammation-related Aβ42 accumulation and neurodegeneration [156]. Inhibition of MAGL can also reduce the expression of the β-amyloid precursor protein lyase 1 (BACE1) in AD mouse models, inhibit the production and accumulation of Aβ, maintain the integrity of hippocampal synaptic structure and function, and improve long-term synaptic plasticity, spatial learning, and memory, as well as inhibit the activation of microglia and astrocytes to prevent neuroinflammation and reduce neurodegeneration [157].
AEA has been reported to up-regulate Notch-1 signaling in cultured neurons. Regulating Notch signaling has recently emerged as a possible approach for altered neurogenesis [158]. Exposing cultured neurons to Aβ (1-42) will increase the endogenous Notch-1 inhibitor numb (Nb) expression, leading to impaired Notch-1 signaling. Adding AEA can prevent Nb expression and enhance Notch-1 signaling [159]. The stimulating effect of AEA on Notch-1 signaling persists in the presence of Aβ (1-42). Through Notch-1 signaling, AEA may be able to help restore neurogenesis and cognition in AD [159].
6. EFFECTS OF THC AND CBD ON AD PATHOGENESIS AND THERAPEUTICS
Current treatments of AD mainly target symptoms, and there are no therapeutics available in clinical practice to prevent the neurodegenerative progress or induce neuronal repair. The increased lines of evidence demonstrate that the delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) cannabinoids of the plant Cannabis sativa have shown neuroprotection in AD animal models [160, 161].
In general, cannabis smoking is a reversible disruption of short-term memory induced by THC, the primary psychoactive component of cannabis. However, a recent report showed that THC is also able to improve neurological function in old animals when chronically administered at low concentrations [162]. For example, a recent study reported that an N2a-variant of amyloid β precursor (APP) cells treated with low doses of THC showed a neuroprotective effect on the cells. The possible targets for THC include decreased Aβ levels in tested cells. THC directly interacts with the Aβ peptide, thereby inhibiting aggregation. Moreover, it inhibits the enzyme acetylcholinesterase, enhances the mitochondria function, and reduces glycogen synthase kinase-3β (GSK-3β) and related signaling pathways [35]. These data sets strongly suggest that THC could be a potential therapeutic option for AD through multiple functions and pathways. Furthermore, recent studies have demonstrated that THC paradoxically promotes hippocampal neurogenesis, prevents neurodegenerative processes occurring in animal models of Alzheimer's disease, protects from inflammation-induced cognitive damage, and restores memory and cognitive function in old mice [163-165]. However, in the study, the THC was administered only twice for 48 h; thus, this may not be sufficient to establish a conclusion. Further studies are needed to determine the dose-dependency and time-dependency of potential treatment of cannabinoids to exert a continuous neuroprotective effect and understand the subsequent ceasing of neurodegeneration and neuronal repair [161].
Cannabidiol (CBD) is one of the most well-known phytocannabinoid used in the treatment of AD. In general, it presents low toxicity and poor systemic absorption via oral administration of capsules or aqueous emulsions by humans and animals [163]. The studies have demonstrated the ability of CBD to reduce reactive gliosis and neuroinflammatory responses [166] as well as promote neurogenesis [167]. Importantly, CBD was also found to reverse and prevent the development of cognitive deficits in AD rodent models [168]. Although the pharmacological mechanisms of CBD-induced neuroprotection are still not well known, it has been suggested that CBD exhibits antioxidant, anti-inflammatory properties, and moderate brain region-specific reductions in insoluble Aβ40 levels [169]. Furthermore, CBD was shown to protect against Aβ-mediated neurotoxicity and microglial-activated neurotoxicity [170] to reduce Aβ production by inducing APP ubiquitination [170] and improve cell viability [171]. These features suggest that CBD is perfectly used to prevent and treat pathogenic processes typically found in AD.
7. LIMITATION OF BRAIN ECBS AS A THERAPEUTIC TARGET
The main challenges in the use of cannabinoids in the treatment of AD come from the following aspects. First, there are no obvious molecular markers in the diagnosis of AD disease, and timely treatment cannot be carried out [172, 173]. Secondly, the distribution of the ECBS in terms of time and space is difficult to control, which increases treatment difficulty [174]. For example, CB2Rs have great potential for treating AD, but the expression of CB2Rs in the central nervous system is relatively low; however, its expression is high in the periphery, and it is highly inducible [118]. Therefore, when and how to specifically target CB2Rs becomes a major challenge. Finally, endocannabinoids are naturally present in mammals, but so far, there is no specific agonist/antagonist regimen to avoid unwanted health outcomes to treat AD [175].
CONCLUSION
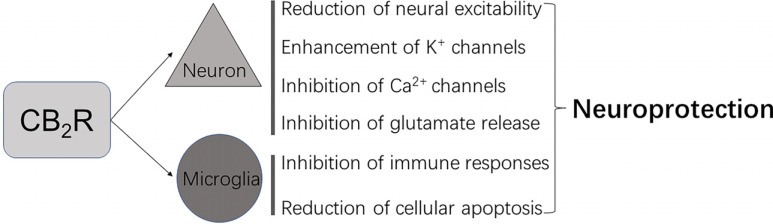
The ECBS, as a potential therapeutic target for AD, mainly involves the regulation of excitability mediated through CB1R and CB2Rs and is based on cannabinoids targeting several important processes involved in the pathogenesis of AD, such as beta-amyloid protein deposition and tau protein phosphorylation, inflammation, mitochondrial dysfunction, and excitatory neurotoxicity (Fig. 1).
Fig. (1).
CB2R-mediated neuroprotection.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Stanley Lin for reviewing this manuscript.
LIST OF ABBREVIATIONS
- AD
Alzheimer’s Disease
- APP
Amyloid Precursor Protein
- CNS
Central Nervous System
- ECBS
Endocannabinoid Receptor System
- LRP1
Lipoprotein Receptor Protein 1
- NFTs
Neurofibrillary Tangles
- SOD
Superoxide Dismutase
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
This work was supported by the Key Area Research and Development Program of Guangdong Province (2018B030334001), the 2020 Li Ka Shing Foundation Cross-Disciplinary Research Grant (2020LKSFG01A), and CNSF (81771437).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Lin M.T., Beal M.F. Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature. 2006;443(7113):787–795. doi: 10.1038/nature05292. [DOI] [PubMed] [Google Scholar]
- 2.Selkoe D.J. Cell biology of protein misfolding: the examples of Alzheimer’s and Parkinson’s diseases. Nat. Cell Biol. 2004;6(11):1054–1061. doi: 10.1038/ncb1104-1054. [DOI] [PubMed] [Google Scholar]
- 3.Hardy J., Selkoe D.J. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 4.Hardy J. New insights into the genetics of Alzheimer’s disease. Ann. Med. 1996;28(3):255–258. doi: 10.3109/07853899609033127. [DOI] [PubMed] [Google Scholar]
- 5.Campion D., Dumanchin C., Hannequin D., Dubois B., Belliard S., Puel M., Thomas-Anterion C., Michon A., Martin C., Charbonnier F., Raux G., Camuzat A., Penet C., Mesnage V., Martinez M., Clerget-Darpoux F., Brice A., Frebourg T. Early-onset autosomal dominant Alzheimer disease: prevalence, genetic heterogeneity, and mutation spectrum. Am. J. Hum. Genet. 1999;65(3):664–670. doi: 10.1086/302553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen J.X., Yan S.S. Role of mitochondrial amyloid-beta in Alzheimer’s disease. J. Alzheimers Dis. 2010;20(s2) Suppl. 2:S569–S578. doi: 10.3233/JAD-2010-100357. [DOI] [PubMed] [Google Scholar]
- 7.Crews L., Masliah E. Molecular mechanisms of neurodegeneration in Alzheimer’s disease. Hum. Mol. Genet. 2010;19(R1):R12–R20. doi: 10.1093/hmg/ddq160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McConlogue L., Buttini M., Anderson J.P., Brigham E.F., Chen K.S., Freedman S.B., Games D., Johnson-Wood K., Lee M., Zeller M., Liu W., Motter R., Sinha S. Partial reduction of BACE1 has dramatic effects on Alzheimer plaque and synaptic pathology in APP Transgenic Mice. J. Biol. Chem. 2007;282(36):26326–26334. doi: 10.1074/jbc.M611687200. [DOI] [PubMed] [Google Scholar]
- 9.Goedert M. NEURODEGENERATION. Alzheimer’s and Parkinson’s diseases: The prion concept in relation to assembled Aβ tau, and α-synuclein. Science. 2015;349(6248):1255555. doi: 10.1126/science.1255555. [DOI] [PubMed] [Google Scholar]
- 10.Tiwari S., Atluri V., Kaushik A., Yndart A., Nair M. Alzheimer’s disease: Pathogenesis, diagnostics, and therapeutics. Int. J. Nanomedicine. 2019;14:5541–5554. doi: 10.2147/IJN.S200490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Streit W.J. Microglia and Alzheimer’s disease pathogenesis. J. Neurosci. Res. 2004;77(1):1–8. doi: 10.1002/jnr.20093. [DOI] [PubMed] [Google Scholar]
- 12.Beeri M.S., Haroutunian V., Schmeidler J., Sano M., Fam P., Kavanaugh A., Barr A.M., Honer W.G., Katsel P. Synaptic protein deficits are associated with dementia irrespective of extreme old age. Neurobiol. Aging. 33(6):e1–e8. doi: 10.1016/j.neurobiolaging.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Selkoe D.J. Translating cell biology into therapeutic advances in Alzheimer’s disease. Nature. 1999;399(6738) Suppl.:A23–A31. doi: 10.1038/399a023. [DOI] [PubMed] [Google Scholar]
- 14.Kása P., Rakonczay Z., Gulya K. The cholinergic system in Alzheimer’s disease. Prog. Neurobiol. 1997;52(6):511–535. doi: 10.1016/S0301-0082(97)00028-2. [DOI] [PubMed] [Google Scholar]
- 15.Fraser S.P., Suh Y.H., Djamgoz M.B. Ionic effects of the Alzheimer’s disease beta-amyloid precursor protein and its metabolic fragments. Trends Neurosci. 1997;20(2):67–72. doi: 10.1016/S0166-2236(96)10079-5. [DOI] [PubMed] [Google Scholar]
- 16.Lane C.A., Hardy J., Schott J.M. Alzheimer’s disease. Eur. J. Neurol. 2018;25(1):59–70. doi: 10.1111/ene.13439. [DOI] [PubMed] [Google Scholar]
- 17.Thomas K.R., Bangen K.J., Weigand A.J., Edmonds E.C., Wong C.G., Cooper S., Delano-Wood L., Bondi M.W. Objective subtle cognitive difficulties predict future amyloid accumulation and neurodegeneration. Neurology. 2020;94(4):e397–e406. doi: 10.1212/WNL.0000000000008838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dolezal V., Kasparová J. Beta-amyloid and cholinergic neurons. Neurochem. Res. 2003;28(3-4):499–506. doi: 10.1023/A:1022865121743. [DOI] [PubMed] [Google Scholar]
- 19.Walsh D.M., Selkoe D.J. Deciphering the molecular basis of memory failure in Alzheimer’s disease. Neuron. 2004;44(1):181–193. doi: 10.1016/j.neuron.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez G.A., Barrett G.M., Duff K.E., Hussaini S.A. Chemogenetic attenuation of neuronal activity in the entorhinal cortex reduces Aβ and tau pathology in the hippocampus. PLoS Biol. 2020;18(8):e3000851. doi: 10.1371/journal.pbio.3000851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Palop J.J., Chin J., Roberson E.D., Wang J., Thwin M.T., Bien-Ly N., Yoo J., Ho K.O., Yu G.Q., Kreitzer A., Finkbeiner S., Noebels J.L., Mucke L. Aberrant excitatory neuronal activity and compensatory remodeling of inhibitory hippocampal circuits in mouse models of Alzheimer’s disease. Neuron. 2007;55(5):697–711. doi: 10.1016/j.neuron.2007.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Westmark C.J., Westmark P.R., Beard A.M., Hildebrandt S.M., Malter J.S. Seizure susceptibility and mortality in mice that over-express amyloid precursor protein. Int. J. Clin. Exp. Pathol. 2008;1(2):157–168. [PMC free article] [PubMed] [Google Scholar]
- 23.Perry E., Walker M., Grace J., Perry R. Acetylcholine in mind: A neurotransmitter correlate of consciousness? Trends Neurosci. 1999;22(6):273–280. doi: 10.1016/S0166-2236(98)01361-7. [DOI] [PubMed] [Google Scholar]
- 24.Cacabelos R., Takeda M., Winblad B. The glutamatergic system and neurodegeneration in dementia: Preventive strategies in Alzheimer’s disease. Int. J. Geriatr. Psychiatry. 1999;14(1):3–47. doi: 10.1002/(SICI)1099-1166(199901)14:1<3:AID-GPS897>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 25.Reeve E., Farrell B., Thompson W., Herrmann N., Sketris I., Magin P.J., Chenoweth L., Gorman M., Quirke L., Bethune G., Hilmer S.N. Deprescribing cholinesterase inhibitors and memantine in dementia: Guideline summary. Med. J. Aust. 2019;210(4):174–179. doi: 10.5694/mja2.50015. [DOI] [PubMed] [Google Scholar]
- 26.Hodson R. Alzheimer’s disease. Nature. 2018;559(7715):S1. doi: 10.1038/d41586-018-05717-6. [DOI] [PubMed] [Google Scholar]
- 27.Knopman D.S., Jones D.T., Greicius M.D. Failure to demonstrate efficacy of aducanumab: An analysis of the EMERGE and ENGAGE trials as reported by Biogen, December 2019. Alzheimers Dement. 2021;17(4):696–701. doi: 10.1002/alz.12213. [DOI] [PubMed] [Google Scholar]
- 28.Aso E., Ferrer I. Cannabinoids for treatment of Alzheimer’s disease: Moving toward the clinic. Front. Pharmacol. 2014;5:37. doi: 10.3389/fphar.2014.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weier M., Hall W. The Use of Cannabinoids in Treating Dementia. Curr. Neurol. Neurosci. Rep. 2017;17(8):56. doi: 10.1007/s11910-017-0766-6. [DOI] [PubMed] [Google Scholar]
- 30.Chen R., Zhang J., Fan N., Teng Z.Q., Wu Y., Yang H., Tang Y.P., Sun H., Song Y., Chen C. Δ9-THC-caused synaptic and memory impairments are mediated through COX-2 signaling. Cell. 2013;155(5):1154–1165. doi: 10.1016/j.cell.2013.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keating G.M. Delta-9-Tetrahydrocannabinol/Cannabidiol Oromucosal Spray (Sativex®): A Review in Multiple Sclerosis-Related Spasticity. Drugs. 2017;77(5):563–574. doi: 10.1007/s40265-017-0720-6. [DOI] [PubMed] [Google Scholar]
- 32.Novotna A., Mares J., Ratcliffe S., Novakova I., Vachova M., Zapletalova O., Gasperini C., Pozzilli C., Cefaro L., Comi G., Rossi P., Ambler Z., Stelmasiak Z., Erdmann A., Montalban X., Klimek A., Davies P. Sativex Spasticity Study, G., A randomized, double-blind, placebo-controlled, parallel-group, enriched-design study of nabiximols* (Sativex((R))), as add-on therapy, in subjects with refractory spasticity caused by multiple sclerosis. Eur. J. Neurol. 2011;18(9):1122–1131. doi: 10.1111/j.1468-1331.2010.03328.x. [DOI] [PubMed] [Google Scholar]
- 33.Cristino L., Bisogno T., Di Marzo V. Cannabinoids and the expanded endocannabinoid system in neurological disorders. Nat. Rev. Neurol. 2020;16(1):9–29. doi: 10.1038/s41582-019-0284-z. [DOI] [PubMed] [Google Scholar]
- 34.Talarico G., Trebbastoni A., Bruno G., de Lena C. Modulation of the cannabinoid system: A new perspective for the treatment of the Alzheimer’s disease. Curr. Neuropharmacol. 2019;17(2):176–183. doi: 10.2174/1570159X16666180702144644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cao C., Li Y., Liu H., Bai G., Mayl J., Lin X., Sutherland K., Nabar N., Cai J. The potential therapeutic effects of THC on Alzheimer’s disease. J. Alzheimers Dis. 2014;42(3):973–984. doi: 10.3233/JAD-140093. [DOI] [PubMed] [Google Scholar]
- 36.Currais A., Quehenberger O.M., Armando A., Daugherty D., Maher P., Schubert D. Amyloid proteotoxicity initiates an inflammatory response blocked by cannabinoids. NPJ Aging Mech. Dis. 2016;2(1):16012. doi: 10.1038/npjamd.2016.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eubanks L.M., Rogers C.J., Beuscher A.E., IV, Koob G.F., Olson A.J., Dickerson T.J., Janda K.D. A molecular link between the active component of marijuana and Alzheimer’s disease pathology. Mol. Pharm. 2006;3(6):773–777. doi: 10.1021/mp060066m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Libro R., Giacoppo S., Soundara Rajan T., Bramanti P., Mazzon E. Natural phytochemicals in the treatment and prevention of dementia: An overview. Molecules. 2016;21(4):518. doi: 10.3390/molecules21040518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ligresti A., De Petrocellis L., Di Marzo V. From Phytocannabinoids to cannabinoid receptors and endocannabinoids: Pleiotropic physiological and pathological roles through complex pharmacology. Physiol. Rev. 2016;96(4):1593–1659. doi: 10.1152/physrev.00002.2016. [DOI] [PubMed] [Google Scholar]
- 40.Pertwee R.G., Howlett A.C., Abood M.E., Alexander S.P., Di Marzo V., Elphick M.R., Greasley P.J., Hansen H.S., Kunos G., Mackie K., Mechoulam R., Ross R.A. International union of basic and clinical pharmacology. LXXIX. Cannabinoid receptors and their ligands: Beyond CB1 and CB2. Pharmacol. Rev. 2010;62(4):588–631. doi: 10.1124/pr.110.003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mechoulam R., Shvo Y., Hashish I., Hashish I. The structure of cannabidiol. Tetrahedron. 1963;19(12):2073–2078. doi: 10.1016/0040-4020(63)85022-X. [DOI] [PubMed] [Google Scholar]
- 42.Gaoni Y., Mechoulam R. Isolation, structure, and partial synthesis of an active constituent of hashish. J. Am. Chem. Soc. 1964;86(8):1646–1647. doi: 10.1021/ja01062a046. [DOI] [Google Scholar]
- 43.Devane W.A., Dysarz F.A., III, Johnson M.R., Melvin L.S., Howlett A.C. Determination and characterization of a cannabinoid receptor in rat brain. Mol. Pharmacol. 1988;34(5):605–613. [PubMed] [Google Scholar]
- 44.Devane W.A., Hanus L., Breuer A., Pertwee R.G., Stevenson L.A., Griffin G., Gibson D., Mandelbaum A., Etinger A., Mechoulam R. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258(5090):1946–1949. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 45.Sugiura T., Kishimoto S., Oka S., Gokoh M. Biochemistry, pharmacology and physiology of 2-arachidonoylglycerol, an endogenous cannabinoid receptor ligand. Prog. Lipid Res. 2006;45(5):405–446. doi: 10.1016/j.plipres.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 46.Howlett A.C., Qualy J.M., Khachatrian L.L. Involvement of Gi in the inhibition of adenylate cyclase by cannabimimetic drugs. Mol. Pharmacol. 1986;29(3):307–313. [PubMed] [Google Scholar]
- 47.Matsuda L.A., Lolait S.J., Brownstein M.J., Young A.C., Bonner T.I. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346(6284):561–564. doi: 10.1038/346561a0. [DOI] [PubMed] [Google Scholar]
- 48.Munro S., Thomas K.L., Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365(6441):61–65. doi: 10.1038/365061a0. [DOI] [PubMed] [Google Scholar]
- 49.Maccarrone M., Bari M., Battista N., Di Rienzo M., Finazzi-Agrò A. Endogenous cannabinoids in neuronal and immune cells: Toxic effects, levels and degradation. Funct. Neurol. 2001;16(4) Suppl.:53–60. [PubMed] [Google Scholar]
- 50.Howlett A.C. The cannabinoid receptors. Prostaglandins Other Lipid Mediat. 2002;68-69:619–631. doi: 10.1016/S0090-6980(02)00060-6. [DOI] [PubMed] [Google Scholar]
- 51.Biegon A., Kerman I.A. Autoradiographic study of pre- and postnatal distribution of cannabinoid receptors in human brain. Neuroimage. 2001;14(6):1463–1468. doi: 10.1006/nimg.2001.0939. [DOI] [PubMed] [Google Scholar]
- 52.Glass M., Dragunow M., Faull R.L. Cannabinoid receptors in the human brain: A detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77(2):299–318. doi: 10.1016/S0306-4522(96)00428-9. [DOI] [PubMed] [Google Scholar]
- 53.Westlake T.M., Howlett A.C., Bonner T.I., Matsuda L.A., Herkenham M. Cannabinoid receptor binding and messenger RNA expression in human brain: An in vitro receptor autoradiography and in situ hybridization histochemistry study of normal aged and Alzheimer’s brains. Neuroscience. 1994;63(3):637–652. doi: 10.1016/0306-4522(94)90511-8. [DOI] [PubMed] [Google Scholar]
- 54.Ramírez B.G., Blázquez C., Gómez del Pulgar T., Guzmán M., de Ceballos M.L. Prevention of Alzheimer’s disease pathology by cannabinoids: Neuroprotection mediated by blockade of microglial activation. J. Neurosci. 2005;25(8):1904–1913. doi: 10.1523/JNEUROSCI.4540-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Solas M., Francis P.T., Franco R., Ramirez M.J. CB2 receptor and amyloid pathology in frontal cortex of Alzheimer’s disease patients. Neurobiol. Aging. 2013;34(3):805–808. doi: 10.1016/j.neurobiolaging.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 56.Bedse G., Romano A., Cianci S., Lavecchia A.M., Lorenzo P., Elphick M.R., Laferla F.M., Vendemiale G., Grillo C., Altieri F., Cassano T., Gaetani S. Altered expression of the CB1 cannabinoid receptor in the triple transgenic mouse model of Alzheimer’s disease. J. Alzheimers Dis. 2014;40(3):701–712. doi: 10.3233/JAD-131910. [DOI] [PubMed] [Google Scholar]
- 57.Stephens G.J. Does modulation of the endocannabinoid system have potential therapeutic utility in cerebellar ataxia? J. Physiol. 2016;594(16):4631–4641. doi: 10.1113/JP271106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rodríguez-Cueto C., Hernández-Gálvez M., Hillard C.J., Maciel P., García-García L., Valdeolivas S., Pozo M.A., Ramos J.A., Gómez-Ruiz M., Fernández-Ruiz J. Dysregulation of the endocannabinoid signaling system in the cerebellum and brainstem in a transgenic mouse model of spinocerebellar ataxia type-3. Neuroscience. 2016;339:191–209. doi: 10.1016/j.neuroscience.2016.09.046. [DOI] [PubMed] [Google Scholar]
- 59.Laprairie R.B., Bagher A.M., Rourke J.L., Zrein A., Cairns E.A., Kelly M.E.M., Sinal C.J., Kulkarni P.M., Thakur G.A., Denovan-Wright E.M. Positive allosteric modulation of the type 1 cannabinoid receptor reduces the signs and symptoms of Huntington’s disease in the R6/2 mouse model. Neuropharmacology. 2019;151:1–12. doi: 10.1016/j.neuropharm.2019.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sepers M.D., Smith-Dijak A., LeDue J., Kolodziejczyk K., Mackie K., Raymond L.A. Endocannabinoid-specific impairment in synaptic plasticity in striatum of Huntington’s disease mouse model. J. Neurosci. 2018;38(3):544–554. doi: 10.1523/JNEUROSCI.1739-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Navarrete F., García-Gutiérrez M.S., Aracil-Fernández A., Lanciego J.L., Manzanares J. Cannabinoid CB1 and CB2 receptors, and monoacylglycerol lipase gene expression alterations in the basal ganglia of patients with Parkinson’s disease. Neurotherapeutics. 2018;15(2):459–469. doi: 10.1007/s13311-018-0603-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leija-Salazar M., Bermúdez de León M., González-Horta A., González-Hernández B. Arachidonyl-2′-chloroethylamide (ACEA), a synthetic agonist of cannabinoid receptor, increases CB1R gene expression and reduces dyskinesias in a rat model of Parkinson’s disease. Pharmacol. Biochem. Behav. 2020;194:172950. doi: 10.1016/j.pbb.2020.172950. [DOI] [PubMed] [Google Scholar]
- 63.Ceccarini J., Casteels C., Ahmad R., Crabbé M., Van de Vliet L., Vanhaute H., Vandenbulcke M., Vandenberghe W., Van Laere K. Regional changes in the type 1 cannabinoid receptor are associated with cognitive dysfunction in Parkinson’s disease. Eur. J. Nucl. Med. Mol. Imaging. 2019;46(11):2348–2357. doi: 10.1007/s00259-019-04445-x. [DOI] [PubMed] [Google Scholar]
- 64.Felder C.C., Briley E.M., Axelrod J., Simpson J.T., Mackie K., Devane W.A. Anandamide, an endogenous cannabimimetic eicosanoid, binds to the cloned human cannabinoid receptor and stimulates receptor-mediated signal transduction. Proc. Natl. Acad. Sci. USA. 1993;90(16):7656–7660. doi: 10.1073/pnas.90.16.7656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schatz A.R., Lee M., Condie R.B., Pulaski J.T., Kaminski N.E. Cannabinoid receptors CB1 and CB2: A characterization of expression and adenylate cyclase modulation within the immune system. Toxicol. Appl. Pharmacol. 1997;142(2):278–287. doi: 10.1006/taap.1996.8034. [DOI] [PubMed] [Google Scholar]
- 66.Galiègue S., Mary S., Marchand J., Dussossoy D., Carrière D., Carayon P., Bouaboula M., Shire D., Le Fur G., Casellas P. Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur. J. Biochem. 1995;232(1):54–61. doi: 10.1111/j.1432-1033.1995.tb20780.x. [DOI] [PubMed] [Google Scholar]
- 67.Griffin G., Wray E.J., Tao Q., McAllister S.D., Rorrer W.K., Aung M.M., Martin B.R., Abood M.E. Evaluation of the cannabinoid CB2 receptor-selective antagonist, SR144528: Further evidence for cannabinoid CB2 receptor absence in the rat central nervous system. Eur. J. Pharmacol. 1999;377(1):117–125. doi: 10.1016/S0014-2999(99)00402-1. [DOI] [PubMed] [Google Scholar]
- 68.McCoy K.L., Matveyeva M., Carlisle S.J., Cabral G.A. Cannabinoid inhibition of the processing of intact lysozyme by macrophages: Evidence for CB2 receptor participation. J. Pharmacol. Exp. Ther. 1999;289(3):1620–1625. [PubMed] [Google Scholar]
- 69.Burdyga G., Lal S., Varro A., Dimaline R., Thompson D.G., Dockray G.J. Expression of cannabinoid CB1 receptors by vagal afferent neurons is inhibited by cholecystokinin. J. Neurosci. 2004;24(11):2708–2715. doi: 10.1523/JNEUROSCI.5404-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Buckley N.E., McCoy K.L., Mezey E., Bonner T., Zimmer A., Felder C.C., Glass M., Zimmer A. Immunomodulation by cannabinoids is absent in mice deficient for the cannabinoid CB(2) receptor. Eur. J. Pharmacol. 2000;396(2-3):141–149. doi: 10.1016/S0014-2999(00)00211-9. [DOI] [PubMed] [Google Scholar]
- 71.Buckley N.E. The peripheral cannabinoid receptor knockout mice: An update. Br. J. Pharmacol. 2008;153(2):309–318. doi: 10.1038/sj.bjp.0707527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Van Sickle M.D., Duncan M., Kingsley P.J., Mouihate A., Urbani P., Mackie K., Stella N., Makriyannis A., Piomelli D., Davison J.S., Marnett L.J., Di Marzo V., Pittman Q.J., Patel K.D., Sharkey K.A. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310(5746):329–332. doi: 10.1126/science.1115740. [DOI] [PubMed] [Google Scholar]
- 73.Ashton J.C., Friberg D., Darlington C.L., Smith P.F. Expression of the cannabinoid CB2 receptor in the rat cerebellum: An immunohistochemical study. Neurosci. Lett. 2006;396(2):113–116. doi: 10.1016/j.neulet.2005.11.038. [DOI] [PubMed] [Google Scholar]
- 74.Onaivi E.S., Ishiguro H., Gong J.P., Patel S., Meozzi P.A., Myers L., Perchuk A., Mora Z., Tagliaferro P.A., Gardner E., Brusco A., Akinshola B.E., Liu Q.R., Chirwa S.S., Hope B., Lujilde J., Inada T., Iwasaki S., Macharia D., Teasenfitz L., Arinami T., Uhl G.R. Functional expression of brain neuronal CB2 cannabinoid receptors are involved in the effects of drugs of abuse and in depression. Ann. N. Y. Acad. Sci. 2008;1139(1):434–449. doi: 10.1196/annals.1432.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Núñez E., Benito C., Pazos M.R., Barbachano A., Fajardo O., González S., Tolón R.M., Romero J. Cannabinoid CB2 receptors are expressed by perivascular microglial cells in the human brain: An immunohistochemical study. Synapse. 2004;53(4):208–213. doi: 10.1002/syn.20050. [DOI] [PubMed] [Google Scholar]
- 76.Witting A., Walter L., Wacker J., Möller T., Stella N. P2X7 receptors control 2-arachidonoylglycerol production by microglial cells. Proc. Natl. Acad. Sci. USA. 2004;101(9):3214–3219. doi: 10.1073/pnas.0306707101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Miller L.K., Devi L.A. The highs and lows of cannabinoid receptor expression in disease: Mechanisms and their therapeutic implications. Pharmacol. Rev. 2011;63(3):461–470. doi: 10.1124/pr.110.003491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Onaivi E.S., Ishiguro H., Gu S., Liu Q.R. CNS effects of CB2 cannabinoid receptors: Beyond neuro-immuno-cannabinoid activity. J. Psychopharmacol. 2012;26(1):92–103. doi: 10.1177/0269881111400652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pacher P., Mechoulam R. Is lipid signaling through cannabinoid 2 receptors part of a protective system? Prog. Lipid Res. 2011;50(2):193–211. doi: 10.1016/j.plipres.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Skaper S.D., Buriani A., Dal Toso R., Petrelli L., Romanello S., Facci L., Leon A. The ALIAmide palmitoylethanolamide and cannabinoids, but not anandamide, are protective in a delayed postglutamate paradigm of excitotoxic death in cerebellar granule neurons. Proc. Natl. Acad. Sci. USA. 1996;93(9):3984–3989. doi: 10.1073/pnas.93.9.3984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lu Q., Straiker A., Lu Q., Maguire G. Expression of CB2 cannabinoid receptor mRNA in adult rat retina. Vis. Neurosci. 2000;17(1):91–95. doi: 10.1017/S0952523800171093. [DOI] [PubMed] [Google Scholar]
- 82.Lanciego J.L., Barroso-Chinea P., Rico A.J., Conte-Perales L., Callén L., Roda E., Gómez-Bautista V., López I.P., Lluis C., Labandeira-García J.L., Franco R. Expression of the mRNA coding the cannabinoid receptor 2 in the pallidal complex of Macaca fascicularis. J. Psychopharmacol. 2011;25(1):97–104. doi: 10.1177/0269881110367732. [DOI] [PubMed] [Google Scholar]
- 83.Liu Q.R., Pan C.H., Hishimoto A., Li C.Y., Xi Z.X., Llorente-Berzal A., Viveros M.P., Ishiguro H., Arinami T., Onaivi E.S., Uhl G.R. Species differences in cannabinoid receptor 2 (CNR2 gene): Identification of novel human and rodent CB2 isoforms, differential tissue expression and regulation by cannabinoid receptor ligands. Genes Brain Behav. 2009;8(5):519–530. doi: 10.1111/j.1601-183X.2009.00498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garcia-Gutierrez M.S., Garcia-Bueno B., Zoppi S., Leza J.C., Manzanares J. Chronic blockade of cannabinoid CB(2) receptors induces anxiolytic-like actions associated to alterations in GABA(A) receptors. Br. J. Pharmacol. 2011 doi: 10.1111/j.1476-5381.2011.01625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Navarrete F., Pérez-Ortiz J.M., Manzanares J. Cannabinoid CB2 receptor-mediated regulation of impulsive-like behaviour in DBA/2 mice. Br. J. Pharmacol. 2012;165(1):260–273. doi: 10.1111/j.1476-5381.2011.01542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Viscomi M.T., Oddi S., Latini L., Pasquariello N., Florenzano F., Bernardi G., Molinari M., Maccarrone M. Selective CB2 receptor agonism protects central neurons from remote axotomy-induced apoptosis through the PI3K/Akt pathway. J. Neurosci. 2009;29(14):4564–4570. doi: 10.1523/JNEUROSCI.0786-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sherwood T.A., Nong L., Agudelo M., Newton C., Widen R., Klein T.W. Identification of transcription start sites and preferential expression of select CB2 transcripts in mouse and human B lymphocytes. J. Neuroimmune Pharmacol. 2009;4(4):476–488. doi: 10.1007/s11481-009-9169-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Baek J.H., Zheng Y., Darlington C.L., Smith P.F. Cannabinoid CB2 receptor expression in the rat brainstem cochlear and vestibular nuclei. Acta Otolaryngol. 2008;128(9):961–967. doi: 10.1080/00016480701796944. [DOI] [PubMed] [Google Scholar]
- 89.Brusco A., Tagliaferro P., Saez T., Onaivi E.S. Postsynaptic localization of CB2 cannabinoid receptors in the rat hippocampus. Synapse. 2008;62(12):944–949. doi: 10.1002/syn.20569. [DOI] [PubMed] [Google Scholar]
- 90.Gong J.P., Onaivi E.S., Ishiguro H., Liu Q.R., Tagliaferro P.A., Brusco A., Uhl G.R. Cannabinoid CB2 receptors: Immunohistochemical localization in rat brain. Brain Res. 2006;1071(1):10–23. doi: 10.1016/j.brainres.2005.11.035. [DOI] [PubMed] [Google Scholar]
- 91.Vlachou S., Panagis G. Regulation of brain reward by the endocannabinoid system: A critical review of behavioral studies in animals. Curr. Pharm. Des. 2014;20(13):2072–2088. doi: 10.2174/13816128113199990433. [DOI] [PubMed] [Google Scholar]
- 92.Agudo J., Martin M., Roca C., Molas M., Bura A.S., Zimmer A., Bosch F., Maldonado R. Deficiency of CB2 cannabinoid receptor in mice improves insulin sensitivity but increases food intake and obesity with age. Diabetologia. 2010;53(12):2629–2640. doi: 10.1007/s00125-010-1894-6. [DOI] [PubMed] [Google Scholar]
- 93.Ignatowska-Jankowska B., Jankowski M.M., Swiergiel A.H. Cannabidiol decreases body weight gain in rats: Involvement of CB2 receptors. Neurosci. Lett. 2011;490(1):82–84. doi: 10.1016/j.neulet.2010.12.031. [DOI] [PubMed] [Google Scholar]
- 94.Emadi L., Jonaidi H., Hosseini Amir Abad E. The role of central CB2 cannabinoid receptors on food intake in neonatal chicks. J. Comp. Physiol. A Neuroethol. Sens. Neural Behav. Physiol. 2011;197(12):1143–1147. doi: 10.1007/s00359-011-0676-z. [DOI] [PubMed] [Google Scholar]
- 95.Flake N.M., Zweifel L.S. Behavioral effects of pulp exposure in mice lacking cannabinoid receptor 2. J. Endod. 2012;38(1):86–90. doi: 10.1016/j.joen.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 96.García-Gutiérrez M.S., Pérez-Ortiz J.M., Gutiérrez-Adán A., Manzanares J. Depression-resistant endophenotype in mice overexpressing cannabinoid CB(2) receptors. Br. J. Pharmacol. 2010;160(7):1773–1784. doi: 10.1111/j.1476-5381.2010.00819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.García-Gutiérrez M.S., Manzanares J. Overexpression of CB2 cannabinoid receptors decreased vulnerability to anxiety and impaired anxiolytic action of alprazolam in mice. J. Psychopharmacol. 2011;25(1):111–120. doi: 10.1177/0269881110379507. [DOI] [PubMed] [Google Scholar]
- 98.Ortega-Alvaro A., Aracil-Fernández A., García-Gutiérrez M.S., Navarrete F., Manzanares J. Deletion of CB2 cannabinoid receptor induces schizophrenia-related behaviors in mice. Neuropsychopharmacology. 2011;36(7):1489–1504. doi: 10.1038/npp.2011.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Xi Z.X., Peng X.Q., Li X., Song R., Zhang H.Y., Liu Q.R., Yang H.J., Bi G.H., Li J., Gardner E.L. Brain cannabinoid CB2 receptors modulate cocaine’s actions in mice. Nat. Neurosci. 2011;14(9):1160–1166. doi: 10.1038/nn.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Navarrete F., Rodríguez-Arias M., Martín-García E., Navarro D., García-Gutiérrez M.S., Aguilar M.A., Aracil-Fernández A., Berbel P., Miñarro J., Maldonado R., Manzanares J. Role of CB2 cannabinoid receptors in the rewarding, reinforcing, and physical effects of nicotine. Neuropsychopharmacology. 2013;38(12):2515–2524. doi: 10.1038/npp.2013.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ortega-Alvaro A., Ternianov A., Aracil-Fernandez A., Navarrete F., Garcia-Gutierrez M.S., Manzanares J. Role of cannabinoid CB receptor in the reinforcing actions of ethanol. Addict. Biol. 2013 doi: 10.1111/adb.12076. [DOI] [PubMed] [Google Scholar]
- 102.Benito C., Núñez E., Tolón R.M., Carrier E.J., Rábano A., Hillard C.J., Romero J. Cannabinoid CB2 receptors and fatty acid amide hydrolase are selectively overexpressed in neuritic plaque-associated glia in Alzheimer’s disease brains. J. Neurosci. 2003;23(35):11136–11141. doi: 10.1523/JNEUROSCI.23-35-11136.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Navarro G., Morales P., Rodríguez-Cueto C., Fernández-Ruiz J., Jagerovic N., Franco R. Targeting cannabinoid CB2 receptors in the central nervous system. medicinal chemistry approaches with focus on neurodegenerative disorders. Front. Neurosci. 2016;10:406. doi: 10.3389/fnins.2016.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rodríguez-Cueto C., Benito C., Fernández-Ruiz J., Romero J., Hernández-Gálvez M., Gómez-Ruiz M. Changes in CB(1) and CB(2) receptors in the post-mortem cerebellum of humans affected by spinocerebellar ataxias. Br. J. Pharmacol. 2014;171(6):1472–1489. doi: 10.1111/bph.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dowie M.J., Grimsey N.L., Hoffman T., Faull R.L., Glass M. Cannabinoid receptor CB2 is expressed on vascular cells, but not astroglial cells in the post-mortem human Huntington’s disease brain. J. Chem. Neuroanat. 2014;59-60:62–71. doi: 10.1016/j.jchemneu.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 106.Palazuelos J., Aguado T., Pazos M.R., Julien B., Carrasco C., Resel E., Sagredo O., Benito C., Romero J., Azcoitia I., Fernández-Ruiz J., Guzmán M., Galve-Roperh I. Microglial CB2 cannabinoid receptors are neuroprotective in Huntington’s disease excitotoxicity. Brain. 2009;132(Pt 11):3152–3164. doi: 10.1093/brain/awp239. [DOI] [PubMed] [Google Scholar]
- 107.Gómez-Gálvez Y., Palomo-Garo C., Fernández-Ruiz J., García C. Potential of the cannabinoid CB(2) receptor as a pharmacological target against inflammation in Parkinson’s disease. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2016;64:200–208. doi: 10.1016/j.pnpbp.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 108.Concannon R.M., Okine B.N., Finn D.P., Dowd E. Upregulation of the cannabinoid CB2 receptor in environmental and viral inflammation-driven rat models of Parkinson's disease. Exp Neurol. 2016;283(Pt A):204-212. doi: 10.1016/j.expneurol.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 109.Concannon R.M., Okine B.N., Finn D.P., Dowd E. Differential upregulation of the cannabinoid CB2 receptor in neurotoxic and inflammation-driven rat models of Parkinson’s disease. Exp. Neurol. 2015;269:133–141. doi: 10.1016/j.expneurol.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 110.Espejo-Porras F., García-Toscano L., Rodríguez-Cueto C., Santos-García I., de Lago E., Fernandez-Ruiz J. Targeting glial cannabinoid CB2 receptors to delay the progression of the pathological phenotype in TDP-43 (A315T) transgenic mice, a model of amyotrophic lateral sclerosis. Br. J. Pharmacol. 2019;176(10):1585–1600. doi: 10.1111/bph.14216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Palazuelos J., Ortega Z., Díaz-Alonso J., Guzmán M., Galve-Roperh I. CB2 cannabinoid receptors promote neural progenitor cell proliferation via mTORC1 signaling. J. Biol. Chem. 2012;287(2):1198–1209. doi: 10.1074/jbc.M111.291294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li Y., Kim J. Deletion of CB2 cannabinoid receptors reduces synaptic transmission and long-term potentiation in the mouse hippocampus. Hippocampus. 2016;26(3):275–281. doi: 10.1002/hipo.22558. [DOI] [PubMed] [Google Scholar]
- 113.Ma Z., Gao F., Larsen B., Gao M., Luo Z., Chen D., Ma X., Qiu S., Zhou Y., Xie J., Xi Z.X., Wu J. Mechanisms of cannabinoid CB2 receptor-mediated reduction of dopamine neuronal excitability in mouse ventral tegmental area. EBioMedicine. 2019;42:225–237. doi: 10.1016/j.ebiom.2019.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Stella N. Endocannabinoid signaling in microglial cells. Neuropharmacology. 2009;56(Suppl. 1):244–253. doi: 10.1016/j.neuropharm.2008.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mensching L., Rading S., Nikolaev V., Karsak M. Monitoring cannabinoid CB2 -receptor mediated cAMP dynamics by FRET-based live cell imaging. Int. J. Mol. Sci. 2020;21(21):E7880. doi: 10.3390/ijms21217880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Howlett A.C. Cannabinoid receptor signaling. Handb. Exp. Pharmacol. 2005;168:53–79. doi: 10.1007/3-540-26573-2_2. [DOI] [PubMed] [Google Scholar]
- 117.Lu H.C., Mackie K. An Introduction to the Endogenous Cannabinoid System. Biol. Psychiatry. 2016;79(7):516–525. doi: 10.1016/j.biopsych.2015.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chen D.J., Gao M., Gao F.F., Su Q.X., Wu J. Brain cannabinoid receptor 2: Expression, function and modulation. Acta Pharmacol. Sin. 2017;38(3):312–316. doi: 10.1038/aps.2016.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhang H.Y., Gao M., Liu Q.R., Bi G.H., Li X., Yang H.J., Gardner E.L., Wu J., Xi Z.X. Cannabinoid CB2 receptors modulate midbrain dopamine neuronal activity and dopamine-related behavior in mice. Proc. Natl. Acad. Sci. USA. 2014;111(46):E5007–E5015. doi: 10.1073/pnas.1413210111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Aso E., Andrés-Benito P., Ferrer I. Genetic deletion of CB1 cannabinoid receptors exacerbates the Alzheimer-like symptoms in a transgenic animal model. Biochem. Pharmacol. 2018;157:210–216. doi: 10.1016/j.bcp.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 121.Manuel I., Lombardero L., LaFerla F.M., Giménez-Llort L., Rodríguez-Puertas R. Activity of muscarinic, galanin and cannabinoid receptors in the prodromal and advanced stages in the triple transgenic mice model of Alzheimer’s disease. Neuroscience. 2016;329:284–293. doi: 10.1016/j.neuroscience.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 122.Shibata M., Yamada S., Kumar S.R., Calero M., Bading J., Frangione B., Holtzman D.M., Miller C.A., Strickland D.K., Ghiso J., Zlokovic B.V. Clearance of Alzheimer’s amyloid-ss(1-40) peptide from brain by LDL receptor-related protein-1 at the blood-brain barrier. J. Clin. Invest. 2000;106(12):1489–1499. doi: 10.1172/JCI10498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bachmeier C., Beaulieu-Abdelahad D., Mullan M., Paris D. Role of the cannabinoid system in the transit of beta-amyloid across the blood-brain barrier. Mol. Cell. Neurosci. 2013;56:255–262. doi: 10.1016/j.mcn.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 124.Stumm C., Hiebel C., Hanstein R., Purrio M., Nagel H., Conrad A., Lutz B., Behl C., Clement A.B. Cannabinoid receptor 1 deficiency in a mouse model of Alzheimer’s disease leads to enhanced cognitive impairment despite of a reduction in amyloid deposition. Neurobiol. Aging. 2013;34(11):2574–2584. doi: 10.1016/j.neurobiolaging.2013.05.027. [DOI] [PubMed] [Google Scholar]
- 125.Haghani M., Janahmadi M., Shabani M. Protective effect of cannabinoid CB1 receptor activation against altered intrinsic repetitive firing properties induced by Aβ neurotoxicity. Neurosci. Lett. 2012;507(1):33–37. doi: 10.1016/j.neulet.2011.11.044. [DOI] [PubMed] [Google Scholar]
- 126.Aso E., Palomer E., Juvés S., Maldonado R., Muñoz F.J., Ferrer I. CB1 agonist ACEA protects neurons and reduces the cognitive impairment of AβPP/PS1 mice. J. Alzheimers Dis. 2012;30(2):439–459. doi: 10.3233/JAD-2012-111862. [DOI] [PubMed] [Google Scholar]
- 127.Patricio-Martínez A., Sánchez-Zavaleta R., Angulo-Cruz I., Gutierrez-Praxedis L., Ramírez E., Martínez-García I., Limón I.D. The acute activation of the CB1 receptor in the hippocampus decreases neurotoxicity and prevents spatial memory impairment in rats lesioned with β-amyloid 25-35. Neuroscience. 2019;416:239–254. doi: 10.1016/j.neuroscience.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 128.Di Marzo V., Stella N., Zimmer A. Endocannabinoid signalling and the deteriorating brain. Nat. Rev. Neurosci. 2015;16(1):30–42. doi: 10.1038/nrn3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tolón R.M., Núñez E., Pazos M.R., Benito C., Castillo A.I., Martínez-Orgado J.A., Romero J. The activation of cannabinoid CB2 receptors stimulates in situ and in vitro beta-amyloid removal by human macrophages. Brain Res. 2009;1283:148–154. doi: 10.1016/j.brainres.2009.05.098. [DOI] [PubMed] [Google Scholar]
- 130.Fakhfouri G., Ahmadiani A., Rahimian R., Grolla A.A., Moradi F., Haeri A. WIN55212-2 attenuates amyloid-beta-induced neuroinflammation in rats through activation of cannabinoid receptors and PPAR-γ pathway. Neuropharmacology. 2012;63(4):653–666. doi: 10.1016/j.neuropharm.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 131.Casarejos M.J., Perucho J., Gomez A., Muñoz M.P., Fernandez-Estevez M., Sagredo O., Fernandez Ruiz J., Guzman M., de Yebenes J.G., Mena M.A. Natural cannabinoids improve dopamine neurotransmission and tau and amyloid pathology in a mouse model of tauopathy. J. Alzheimers Dis. 2013;35(3):525–539. doi: 10.3233/JAD-130050. [DOI] [PubMed] [Google Scholar]
- 132.Aso E., Juvés S., Maldonado R., Ferrer I. CB2 cannabinoid receptor agonist ameliorates Alzheimer-like phenotype in AβPP/PS1 mice. J. Alzheimers Dis. 2013;35(4):847–858. doi: 10.3233/JAD-130137. [DOI] [PubMed] [Google Scholar]
- 133.Jayant S., Sharma B.M., Bansal R., Sharma B. Pharmacological benefits of selective modulation of cannabinoid receptor type 2 (CB2) in experimental Alzheimer’s disease. Pharmacol. Biochem. Behav. 2016;140:39–50. doi: 10.1016/j.pbb.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 134.Martín-Moreno A.M., Brera B., Spuch C., Carro E., García-García L., Delgado M., Pozo M.A., Innamorato N.G., Cuadrado A., de Ceballos M.L. Prolonged oral cannabinoid administration prevents neuroinflammation, lowers β-amyloid levels and improves cognitive performance in Tg APP 2576 mice. J. Neuroinflammation. 2012;9(1):8. doi: 10.1186/1742-2094-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Aso E., Andrés-Benito P., Carmona M., Maldonado R., Ferrer I. Cannabinoid Receptor 2 Participates in Amyloid-β Processing in a Mouse Model of Alzheimer’s Disease but Plays a Minor Role in the Therapeutic Properties of a Cannabis-Based Medicine. J. Alzheimers Dis. 2016;51(2):489–500. doi: 10.3233/JAD-150913. [DOI] [PubMed] [Google Scholar]
- 136.Koppel J., Vingtdeux V., Marambaud P., d’Abramo C., Jimenez H., Stauber M., Friedman R., Davies P. CB2 receptor deficiency increases amyloid pathology and alters tau processing in a transgenic mouse model of Alzheimer’s disease. Mol. Med. 2014;20(1):29–36. doi: 10.2119/molmed.2013.00140.revised. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Maroof N., Ravipati S., Pardon M.C., Barrett D.A., Kendall D.A. Reductions in endocannabinoid levels and enhanced coupling of cannabinoid receptors in the striatum are accompanied by cognitive impairments in the AβPPswe/PS1ΔE9 mouse model of Alzheimer’s disease. J. Alzheimers Dis. 2014;42(1):227–245. doi: 10.3233/JAD-131961. [DOI] [PubMed] [Google Scholar]
- 138.Ahmad R., Postnov A., Bormans G., Versijpt J., Vandenbulcke M., Van Laere K. Decreased in vivo availability of the cannabinoid type 2 receptor in Alzheimer’s disease. Eur. J. Nucl. Med. Mol. Imaging. 2016;43(12):2219–2227. doi: 10.1007/s00259-016-3457-7. [DOI] [PubMed] [Google Scholar]
- 139.Schmöle A.C., Lundt R., Ternes S., Albayram Ö., Ulas T., Schultze J.L., Bano D., Nicotera P., Alferink J., Zimmer A. Cannabinoid receptor 2 deficiency results in reduced neuroinflammation in an Alzheimer’s disease mouse model. Neurobiol. Aging. 2015;36(2):710–719. doi: 10.1016/j.neurobiolaging.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 140.Orihuela R., McPherson C.A., Harry G.J. Microglial M1/M2 polarization and metabolic states. Br. J. Pharmacol. 2016;173(4):649–665. doi: 10.1111/bph.13139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mecha M., Feliú A., Carrillo-Salinas F.J., Rueda-Zubiaurre A., Ortega-Gutiérrez S., de Sola R.G., Guaza C. Endocannabinoids drive the acquisition of an alternative phenotype in microglia. Brain Behav. Immun. 2015;49:233–245. doi: 10.1016/j.bbi.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 142.Wu J., Bie B., Yang H., Xu J.J., Brown D.L., Naguib M. Activation of the CB2 receptor system reverses amyloid-induced memory deficiency. Neurobiol. Aging. 2013;34(3):791–804. doi: 10.1016/j.neurobiolaging.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 143.Martín-Moreno A.M., Reigada D., Ramírez B.G., Mechoulam R., Innamorato N., Cuadrado A., de Ceballos M.L. Cannabidiol and other cannabinoids reduce microglial activation in vitro and in vivo: Relevance to Alzheimer’s disease. Mol. Pharmacol. 2011;79(6):964–973. doi: 10.1124/mol.111.071290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Esposito G., Iuvone T., Savani C., Scuderi C., De Filippis D., Papa M., Di Marzo V., Steardo L. Opposing control of cannabinoid receptor stimulation on amyloid-beta-induced reactive gliosis: In vitro and in vivo evidence. J. Pharmacol. Exp. Ther. 2007;322(3):1144–1152. doi: 10.1124/jpet.107.121566. [DOI] [PubMed] [Google Scholar]
- 145.Ehrhart J., Obregon D., Mori T., Hou H., Sun N., Bai Y., Klein T., Fernandez F., Tan J., Shytle R.D. Stimulation of cannabinoid receptor 2 (CB2) suppresses microglial activation. J. Neuroinflammation. 2005;2(1):29. doi: 10.1186/1742-2094-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhao J., Wang M., Liu W., Ma Z., Wu J. Activation of cannabinoid receptor 2 protects rat hippocampal neurons against Aβ-induced neuronal toxicity. Neurosci. Lett. 2020;735:135207. doi: 10.1016/j.neulet.2020.135207. [DOI] [PubMed] [Google Scholar]
- 147.Sugiura T., Kondo S., Sukagawa A., Nakane S., Shinoda A., Itoh K., Yamashita A., Waku K. 2-Arachidonoylglycerol: A possible endogenous cannabinoid receptor ligand in brain. Biochem. Biophys. Res. Commun. 1995;215(1):89–97. doi: 10.1006/bbrc.1995.2437. [DOI] [PubMed] [Google Scholar]
- 148.Wilson R.I., Nicoll R.A. Endocannabinoid signaling in the brain. Science. 2002;296(5568):678–682. doi: 10.1126/science.1063545. [DOI] [PubMed] [Google Scholar]
- 149.Walter L., Stella N. Cannabinoids and neuroinflammation. Br. J. Pharmacol. 2004;141(5):775–785. doi: 10.1038/sj.bjp.0705667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Guzman M. Neurons on cannabinoids: Dead or alive? Br. J. Pharmacol. 2003;140(3):439–440. doi: 10.1038/sj.bjp.0705465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Medina-Vera D., Rosell-Valle C., López-Gambero A.J., Navarro J.A., Zambrana-Infantes E.N., Rivera P., Santín L.J., Suarez J., Rodríguez de Fonseca F. Imbalance of Endocannabinoid/Lysophosphatidylinositol Receptors Marks the Severity of Alzheimer’s Disease in a Preclinical Model: A Therapeutic Opportunity. Biology (Basel) 2020;9(11):E377. doi: 10.3390/biology9110377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Berry A.J., Zubko O., Reeves S.J., Howard R.J. Endocannabinoid system alterations in Alzheimer’s disease: A systematic review of human studies. Brain Res. 2020;1749:147135. doi: 10.1016/j.brainres.2020.147135. [DOI] [PubMed] [Google Scholar]
- 153.Milton N.G. Anandamide and noladin ether prevent neurotoxicity of the human amyloid-beta peptide. Neurosci. Lett. 2002;332(2):127–130. doi: 10.1016/S0304-3940(02)00936-9. [DOI] [PubMed] [Google Scholar]
- 154.Gajardo-Gómez R., Labra V.C., Maturana C.J., Shoji K.F., Santibañez C.A., Sáez J.C., Giaume C., Orellana J.A. Cannabinoids prevent the amyloid β-induced activation of astroglial hemichannels: A neuroprotective mechanism. Glia. 2017;65(1):122–137. doi: 10.1002/glia.23080. [DOI] [PubMed] [Google Scholar]
- 155.van der Stelt M., Mazzola C., Esposito G., Matias I., Petrosino S., De Filippis D., Micale V., Steardo L., Drago F., Iuvone T., Di Marzo V. Endocannabinoids and beta-amyloid-induced neurotoxicity in vivo: Effect of pharmacological elevation of endocannabinoid levels. Cell. Mol. Life Sci. 2006;63(12):1410–1424. doi: 10.1007/s00018-006-6037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Yan W., Yun Y., Ku T., Li G., Sang N. NO2 inhalation promotes Alzheimer’s disease-like progression: Cyclooxygenase-2-derived prostaglandin E2 modulation and monoacylglycerol lipase inhibition-targeted medication. Sci. Rep. 2016;6(1):22429. doi: 10.1038/srep22429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chen R., Zhang J., Wu Y., Wang D., Feng G., Tang Y.P., Teng Z., Chen C. Monoacylglycerol lipase is a therapeutic target for Alzheimer’s disease. Cell Rep. 2012;2(5):1329–1339. doi: 10.1016/j.celrep.2012.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Schweisguth F. Regulation of notch signaling activity. Curr. Biol. 2004;14(3):R129–R138. doi: 10.1016/j.cub.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 159.Tanveer R., Gowran A., Noonan J., Keating S.E., Bowie A.G., Campbell V.A. The endocannabinoid, anandamide, augments Notch-1 signaling in cultured cortical neurons exposed to amyloid-β and in the cortex of aged rats. J. Biol. Chem. 2012;287(41):34709–34721. doi: 10.1074/jbc.M112.350678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Cassano T., Villani R., Pace L., Carbone A., Bukke V.N., Orkisz S., Avolio C., Serviddio G. From Cannabis sativa to Cannabidiol: Promising therapeutic candidate for the treatment of Neurodegenerative diseases. Front. Pharmacol. 2020;11:124. doi: 10.3389/fphar.2020.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Cooray R., Gupta V., Suphioglu C. Current aspects of the endocannabinoid system and targeted THC and CBD phytocannabinoids as potential therapeutics for Parkinson’s and Alzheimer’s diseases: A review. Mol. Neurobiol. 2020;57(11):4878–4890. doi: 10.1007/s12035-020-02054-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Calabrese E.J., Rubio-Casillas A. Biphasic effects of THC in memory and cognition. Eur. J. Clin. Invest. 2018;48(5):e12920. doi: 10.1111/eci.12920. [DOI] [PubMed] [Google Scholar]
- 163.Monteiro K.L.C., Dos Santos Alcântara M.G., de Aquino T.M., da Silva-Júnior E.F. Cannabinoid pharmacology and its therapeutic uses in Alzheimer’s disease. Neural Regen. Res. 2021;16(5):990–991. doi: 10.4103/1673-5374.294336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Herrmann N., Ruthirakuhan M., Gallagher D., Verhoeff N.P.L.G., Kiss A., Black S.E., Lanctôt K.L. Randomized Placebo-Controlled Trial of Nabilone for Agitation in Alzheimer’s Disease. Am. J. Geriatr. Psychiatry. 2019;27(11):1161–1173. doi: 10.1016/j.jagp.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 165.Russo E.B. Cannabis Therapeutics and the Future of Neurology. Front. Integr. Nuerosci. 2018;12:51. doi: 10.3389/fnint.2018.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Mukhopadhyay P., Rajesh M., Horváth B., Bátkai S., Park O., Tanchian G., Gao R.Y., Patel V., Wink D.A., Liaudet L., Haskó G., Mechoulam R., Pacher P. Cannabidiol protects against hepatic ischemia/reperfusion injury by attenuating inflammatory signaling and response, oxidative/nitrative stress, and cell death. Free Radic. Biol. Med. 2011;50(10):1368–1381. doi: 10.1016/j.freeradbiomed.2011.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hamelink C., Hampson A., Wink D.A., Eiden L.E., Eskay R.L. Comparison of cannabidiol, antioxidants, and diuretics in reversing binge ethanol-induced neurotoxicity. J. Pharmacol. Exp. Ther. 2005;314(2):780–788. doi: 10.1124/jpet.105.085779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Watt G., Karl T. In vivo Evidence for Therapeutic Properties of Cannabidiol (CBD) for Alzheimer’s Disease. Front. Pharmacol. 2017;8:20. doi: 10.3389/fphar.2017.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Watt G., Shang K., Zieba J., Olaya J., Li H., Garner B., Karl T. Chronic treatment with 50mg/kg cannabidiol improves cognition and moderately reduces Aβ40 levels in 12-month-old male AβPPswe/PS1ΔE9 transgenic mice. J. Alzheimers Dis. 2020;74(3):937–950. doi: 10.3233/JAD-191242. [DOI] [PubMed] [Google Scholar]
- 170.Janefjord E., Mååg J.L., Harvey B.S., Smid S.D. Cannabinoid effects on β amyloid fibril and aggregate formation, neuronal and microglial-activated neurotoxicity in vitro. Cell. Mol. Neurobiol. 2014;34(1):31–42. doi: 10.1007/s10571-013-9984-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Harvey B.S., Ohlsson K.S., Mååg J.L., Musgrave I.F., Smid S.D. Contrasting protective effects of cannabinoids against oxidative stress and amyloid-β evoked neurotoxicity in vitro. Neurotoxicology. 2012;33(1):138–146. doi: 10.1016/j.neuro.2011.12.015. [DOI] [PubMed] [Google Scholar]
- 172.Karikari T.K., Benedet A.L., Ashton N.J., Lantero Rodriguez J., Snellman A., Suárez-Calvet M., Saha-Chaudhuri P., Lussier F., Kvartsberg H., Rial A.M., Pascoal T.A., Andreasson U., Schöll M., Weiner M.W., Rosa-Neto P., Trojanowski J.Q., Shaw L.M., Blennow K., Zetterberg H. Diagnostic performance and prediction of clinical progression of plasma phospho-tau181 in the Alzheimer’s Disease Neuroimaging Initiative. Mol. Psychiatry. 2021;26(2):429–442. doi: 10.1038/s41380-020-00923-z. [DOI] [PubMed] [Google Scholar]
- 173.Karikari T.K., Emeršič A., Vrillon A., Lantero-Rodriguez J., Ashton N.J., Kramberger M.G., Dumurgier J., Hourregue C., Čučnik S., Brinkmalm G., Rot U., Zetterberg H., Paquet C., Blennow K. Head-to-head comparison of clinical performance of CSF phospho-tau T181 and T217 biomarkers for Alzheimer’s disease diagnosis. Alzheimers Dement. 2021;17(5):755–767. doi: 10.1002/alz.12236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sharma D.S., Paddibhatla I., Raghuwanshi S., Malleswarapu M., Sangeeth A., Kovuru N., Dahariya S., Gautam D.K., Pallepati A., Gutti R.K. Endocannabinoid system: Role in blood cell development, neuroimmune interactions and associated disorders. J. Neuroimmunol. 2021;353:577501. doi: 10.1016/j.jneuroim.2021.577501. [DOI] [PubMed] [Google Scholar]
- 175.Reddy V., Grogan D., Ahluwalia M., Salles É.L., Ahluwalia P., Khodadadi H., Alverson K., Nguyen A., Raju S.P., Gaur P., Braun M., Vale F.L., Costigliola V., Dhandapani K., Baban B., Vaibhav K. Targeting the endocannabinoid system: A predictive, preventive, and personalized medicine-directed approach to the management of brain pathologies. EPMA J. 2020;11(2):217–250. doi: 10.1007/s13167-020-00203-4. [DOI] [PMC free article] [PubMed] [Google Scholar]