Abstract
Background
Patients prefer medical communication including both hopefulness and realism, though health-care professional (HCPs) struggle to balance these. Providers could thus benefit from a detailed personal understanding of hope, allowing them to model and convey it to patients. Additionally, given that hope is associated with lower levels of burnout, HCPs may benefit from tools designed to enhance their own personal hopefulness. Several investigators have proposed offering HCPs interventions to augment hope. We developed an online workshop for this purpose.
Methods
Feasibility and acceptability of the workshop were assessed in members of the SWOG Cancer Research Network. Three measures were used: the Was-It-Worth-It scale, a survey based on the Kirkpatrick Training Evaluation Model, and a single item prompting participants to rate the degree to which they believe concepts from the workshop should be integrated into SWOG studies.
Results
Twenty-nine individuals signed up for the intervention, which consisted of a single 2-hour session, and 23 completed measures. Results from Was-It-Worth-It items indicate that nearly all participants found the intervention relevant, engaging, and helpful. Mean ratings for Kirkpatrick Training Evaluation Model items were high, ranging from 6.91 to 7.70 on 8-point scales. Finally, participants provided a mean rating of 4.44 on a 5-point scale to the item “To what degree do you believe it may be useful to integrate concepts from this workshop into SWOG trials/studies?”
Conclusions
An online workshop to enhance hopefulness is feasible and acceptable to oncology HCPs. The tool will be integrated into SWOG studies evaluating provider and patient well-being.
Hope, as operationalized by Snyder et al. (1), is a cognitive construct predicated on goal orientation accompanied by pathways thinking and personal agency. This model is easily measured with validated scales, which have been shown to predict positive outcomes ranging from lower depression and anxiety to higher levels of health-promoting behaviors in a variety of populations, including in situations throughout the cancer care continuum (2,3). For instance, hope is important in the contexts of advanced cancer and palliative care (4,5). A secondary analysis of data from project ENABLE (Educate, Nurture, Advise, Before Life Ends) (6), an early palliative care intervention for individuals with advanced malignancy, showed that patients with higher levels of hope demonstrated longer overall survival time than those with lower hope.
Patients often prefer medical communication that includes both hope and realism (7,8). In a survey of 412 individuals with cancer, patients rated their preferences for 13 prognostic phrases differing in explicitness and certainty (9). Overall, participants preferred disclosures containing “hope for the best, plan for the worst” statements such as “We will do our best to make sure that you have a better-than-average outcome, but in case you progress faster than average, I think it is a good idea to prepare yourself for the unexpected” (p. e945). However, clinicians often struggle to balance the two. This may be because health-care professionals (HCPs) themselves lack a detailed understanding of hope, often confusing it with optimism or positive thinking (1,2). In their review of the literature, Clayton et al. (10) found that providers have differing and sometimes conflicting notions of hope. It may be important for HCPs to more fully understand and embody hope to model and convey it to patients. Thus, training in hope for HCPs may be helpful.
Moreover, higher personal hope among HCPs appears associated with less job burnout and greater overall life satisfaction (11). Accordingly, in addition to offering providers training in the nature of hope itself, there also may be potential personal value in hope enhancement interventions (12,13).
Feldman and Dreher (14) developed a single-session hope workshop as an in-person intervention that requires approximately 2 hours to complete. Although this and similar interventions have been applied to populations ranging from students to incarcerated individuals (15,16), it has been offered to HCPs in only limited circumstances and exclusively in an in-person format (13).
Given the disruption occasioned by COVID-19, we adapted the workshop for online delivery accompanied by a smartphone application. Thus, the need arose to evaluate the intervention in this new format (17). The present research constitutes a brief study of the feasibility and acceptability of an online iteration of this single-session intervention for oncology professionals. Additionally, we query HCPs participating in this study regarding the degree to which they believe similar hope enhancement techniques should be offered to patients with cancer in the context of clinical trials.
Methods
The present research consisted of a single-arm feasibility and acceptability study. Invitations were emailed to 141 members of the SWOG Cancer Research Network (formerly the Southwestern Oncology Group), which is a member of the National Clinical Trials Network of the National Cancer Institute. Emails were sent to a cross-section of professions within the organization. Enrollment was limited to 1 of 4 available time slots. A total of 29 individuals signed up and attended the intervention, which consisted of a single 2-hour session followed by self-report measures. To optimize fidelity, the same facilitators (B.W.C., D.B.F.) conducted each session and were credentialed with a manualized course. Six to 8 individuals participated in each session, which was delivered live via the Zoom video platform.
The workshop was derived from an in-person experience (14) consisting of 3 components. First, a brief didactic presentation on hope was offered. This was oriented around Snyder’s “Hope Theory” (1), which posits that hope consists of 3 components, known within the workshop as the “three conditions for hope to thrive”: goals (desired ends), pathways (perceived plans or strategies for reaching goals), and agency (motivation or energy to pursue goals). According to 3 decades of research, when these conditions are met, individuals experience a variety of positive psychosocial and physical outcomes (2,3).
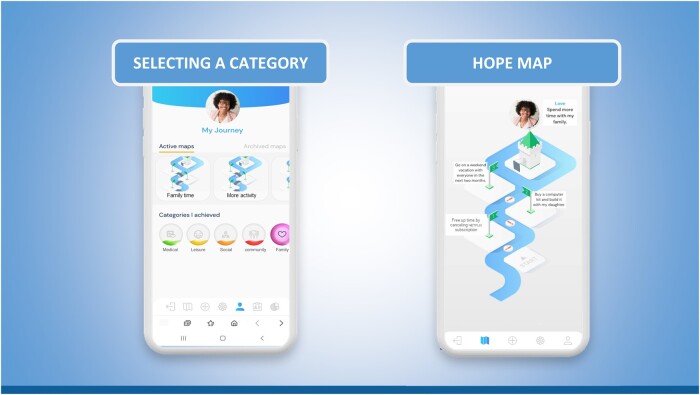
The workshop includes 2 activities to integrate these conditions into participants’ lives: hope mapping and hope-related mental rehearsal. Hope mapping, previously a paper-and-pencil exercise, is now conducted via a smartphone app known as Hopetimize (Life’s Door, Jerusalem, Israel). Users are guided to identify a meaningful goal and a pathway toward that goal (see Figure 1). They also identify obstacles that may hamper pursuing that goal along with potential ways to circumvent those obstacles. The mental rehearsal exercise is derived from research showing that such techniques increase performance of skill-related behaviors in various domains, including sports (18) and music (19). In this 15-minute exercise, participants are guided to close their eyes and imagine executing the pathway from their hope map, encountering each obstacle listed, and motivating themselves to circumnavigate those obstacles.
Figure 1.
Representative display of the mapping process for the Hopetimize smartphone app.
Immediately post workshop, 3 measures were used. First, we administered the Was-It-Worth-It (WIWI) scale (20), which was developed to assess the degree to which participants in research studies find the experience worthwhile. It consists of 5 questions, 3 answered yes or no and 2 answered on Likert scales. Second, we administered a survey based on the Kirkpatrick Training Evaluation Model (TEM) (21), one of the widest-used approaches for assessing training experiences like the Hope Workshop. Accordingly, training experiences are assessed on 4 dimensions: general reaction, learning, anticipated behavior change, and outcome. These dimensions are operationalized through individual items rated on Likert-scales. Most items from these measures, along with means and SDs, are found in Tables 1 and 2. Consistent with past research using these tools, summary scores were not used because items were treated as distinct measures. Finally, a single item prompted participants to rate the degree to which they believed hope concepts from the workshop should be integrated into future SWOG studies involving patients. The study was approved by the institutional review board of Shaare Zedek Medical Center (Jerusalem, Israel).
Table 1.
Ratings on the 4 elements of Kirkpatrick’s Training Evaluation Model (TEM)a
| Item | Mean (SD) |
|---|---|
| “I found the workshop relevant and engaging.” (reaction) | 7.70 (.70) |
| “I learned something (eg, knowledge or skills) in the workshop.” (learning) | 7.65 (.94) |
| “I will change how I do or approach something in my personal or professional life as a result of the workshop.” (behavior) | 7.22 (1.28) |
| “I feel more hopeful as a result of the workshop.” (result) | 6.91 (1.31) |
All items rated on 8-point scales ranging from “definitely false” to “definitely true.”
Table 2.
Ratings on “Was-it-Worth-it” (WIWI) items
| Item | Yes | No | Undecided | Missing response |
|---|---|---|---|---|
| “Was it worthwhile for you to participate in the Hope Workshop?” | 23 | 0 | 0 | 0 |
| “If you had it to do over, would you participate in the Hope Workshop again?” | 22 | 1 | 0 | 0 |
| “Would you recommend participating in the Hope Workshop to others?” | 22 | 0 | 1 | 0 |
Results
Twenty-nine SWOG investigators participated in the workshop, and 23 (79%) completed measures. Table 3 displays sample characteristics. The most common professions were physicians and nursing specialties. Although there was a wide age distribution, the sample was heavily skewed toward female (74%) and White (78%) participants. Because no data were obtained from participants who did not complete measures, it is not known whether they differed on any characteristics.
Table 3.
Sample characteristics
| No. | % | |
|---|---|---|
| Gender | ||
| Female | 17 | 74 |
| Male | 6 | 26 |
| Ethnicity | ||
| Asian/Asian American | 3 | 13 |
| White | 18 | 78 |
| No response | 2 | 9 |
| Profession | ||
| Physician | 8 | 35 |
| Registered nurse | 4 | 17 |
| Nurse practitioner | 2 | 9 |
| Researcher (PhD, etc) | 5 | 22 |
| Patient advocate | 3 | 13 |
| Other staff | 1 | 4 |
| Age, y | ||
| 30-39 | 4 | 17 |
| 40-49 | 3 | 13 |
| 50-59 | 6 | 26 |
| 60-69 | 3 | 13 |
| 70-79 | 5 | 22 |
| No response | 2 | 9 |
Within the Kirkpatrick TEM instrument, items are rated on 8-point scales, with responses ranging from “definitely false” to “definitely true.” Table 1 shows that ratings were high, ranging from 6.91 to 7.70.
Results on the WIWI were similarly positive (please see Table 2). In particular, nearly all participants answered “yes” to items, including “Was it worthwhile to participate in the Hope Workshop?”, “If you had to do it over, would you participate in the Hope Workshop again?”, and “Would you recommend participating in the Hope Workshop to others?” Two additional WIWI items were reported on 3-point scales, where 1 indicated “it got worse,” 2 indicated “it stayed the same,” and 3 indicated “it improved.” These items were “Overall, how was your experience of participating in the Hope Workshop?” and, “Overall, do you believe your quality of life has increased by participating in the Hope Workshop?”, with means of 2.70 (SD = .64) and 2.52 (SD = .51), respectively.
Finally, a single item asked, “To what degree do you think it may be useful to integrate concepts from this workshop into SWOG trials/studies?” On average, this was rated 4.44 (SD = .59) on a scale ranging from 1 (“not at all useful”) to 5 (“extremely useful”).
Discussion
According to the results of this pilot study, a single-session online hope intervention augmented by a smartphone app appears both feasible and acceptable in a sample of oncology HCPs. Responses to the WIWI and Kirkpatrick TEM items indicate that they not only saw value in this intervention for themselves and fellow HCPs but also potentially for patients in future trials.
The SWOG Cancer Research Network has a long-standing commitment to harnessing innovative nonmedical technologies in influencing traditional oncologic endpoints. For instance, Hershman and colleagues (22) rigorously evaluated text messaging to optimize adherence to endocrine therapy among postmenopausal women with breast cancer. In that trial, however, the authors did not find that nonpersonalized text messaging was effective. The hope enhancement intervention described herein is, by definition, a personalized approach and, for this reason, National Clinical Trials Network leadership has expressed interest in studying this approach (Mark O’Rourke, personal communication).
Recently, an online questionnaire documented that nearly 25% of Society of Gynecologic Oncology members suffered from burnout (8). Moreover, those with higher levels of hope were less likely than those with lower hope to meet the criteria for burnout. This relationship is understandable given that burnout can be conceptualized as hopelessness that one’s efforts matter in the work context. This compels us to ask whether professionals can become more hopeful and therefore be less likely to suffer from burnout. Feldman et al. (23) found that hope and social support—both mainstays of the workshop described herein—may mitigate the effects of burnout on general life satisfaction. Moreover, Bareket-Bojmel et al. (24) tested a mediation model among 1200 individuals from 3 countries during the COVID-19 pandemic, concluding that perceived social support facilitates hope during dire times. It is not surprising, therefore, that the professionals in the present sample deemed our brief hope intervention valuable.
The COVID-19 pandemic necessitated broad adoption of digital medical options. Virtual platforms allow participation and honing of skills in a context that is not dependent on geographic proximity. Furthermore, the virtual nature of the hope intervention reported here provides for easy scalability, enabling diffusion to a wide audience. Finally, overhead costs are relatively low compared with other interventions, and results appear to be noted relatively quickly.
There are limitations of this study. First, the population studied was highly educated. Although we believe the app is intuitive, if it is to be used by patients in addition to HCPs, it is crucial to demonstrate ease of use regardless of level of formal education. Second, there was limited diversity in the present sample, particularly in terms of race and ethnicity. This highlights the necessity of future research using broader samples of individuals who might benefit from hope enhancement interventions (25). Finally, invitations to participate were accepted at a relatively low rate (20%). Busy clinicians are hard pressed to access training sessions at fixed times. Work is now ongoing to determine if it is feasible to offer a more flexible “self-guided” online training module more adapted to the lives of busy clinicians.
The tool described in this report is inexpensive and easily adopted. In an inherently fragile “cancer ecosystem,” which includes patients, caregivers, and HCPs, we dare not forfeit the opportunity enhance hope, reduce burnout, and directly or indirectly optimize oncologic endpoints (3,6). We believe that the virtual experience we have developed makes hope—as a pragmatic construct—readily accessible to disparate stakeholders who could benefit from its forward-looking orientation.
Supplementary Material
Acknowledgements
The authors wish to thank the Pamm Gross Kahane Research Institute of the non-profit organization Life’s Door for funding the development of the app used in this research.
The funders played no role in the publication of this article.
This study was presented as a poster (Abstract #348157) at the 2021 ASCO Quality Care Symposium.
Contributor Information
Benjamin W Corn, Shaare Zedek Cancer Center, Jerusalem, Israel.
David B Feldman, Department of Counseling Psychology, Santa Clara University, Santa Clara, CA, USA.
Ishwaria M Subbiah, Department of Palliative, Rehabilitation and Integrative Medicine, MD Anderson Cancer Center of the University of Texas, Houston, TX, USA.
Phyllis D Corn, Life’s Door, Jerusalem, Israel.
Marie A Bakitas, School of Nursing, University of Alabama at Birmingham, Birmingham, AL, USA.
Robert S Krouse, Department of Surgery, University of Pennsylvania School of Medicine, Philadelphia, PA, USA.
Matthew F Hudson, Department of Medicine, Prisma Heath Cancer Institute, Greenville, SC, USA.
Lauren A Fowler, Department of Physiology and Pharmacology, Wake Forest University School of Medicine, Winston-Salem, NC, USA.
Valerie Fraser, Division of Patient Advocacy, SWOG Cancer Research Network, San Antonio, TX, USA.
Carole Siegal, Division of Patient Advocacy, SWOG Cancer Research Network, San Antonio, TX, USA.
Rajiv Agarwal, Division of Hematology/Oncology, Department of Medicine, Vanderbilt University Medical Center, Nashville, TN, USA.
Jacqueline L Ge, Department of Counseling Psychology, Santa Clara University, Santa Clara, CA, USA.
Jyotsana Parajuli, School of Nursing, University of North Carolina, Charlotte, NC, USA.
Jamie S Myers, School of Nursing, University of Kansas Medical Center, Kansas City, KS, USA.
Mark A O’Rourke, Department of Medicine, Prisma Heath Cancer Institute, Greenville, SC, USA.
Data availability
All data are incorporated into the article and its online supplementary material.
Author contributions
Ben Corn, MD (Conceptualization; Data curation; Formal analysis; Investigation; Supervision; Writing – original draft; Writing – review & editing); David B. Feldman, PhD (Conceptualization; Data curation; Formal analysis; Investigation; Supervision; Writing – original draft; Writing – review & editing); Ishwaria M. Subbiah, MD (Investigation; Project administration); Phyllis D. Corn, MSc (Investigation; Project administration); Marie A. Bakitas, PhD (Investigation; Project administration); Robert A. Krouse, MD (Investigation; Project administration); Matthew F. Hudson, PhD (Investigation; Project administration); Lauren A. Fowler, PhD (Investigation; Project administration); Valerie Fraser, MS (Investigation; Project administration); Carole Siegal, MS (Investigation; Project administration); Rajiv Agarwal, MD (Investigation; Project administration); Jacqueline L. GE, MS (Investigation; Project administration); Jyotsana Parajuli, PhD (Investigation; Project administration); Jamie S. Myers, PhD (Investigation; Project administration); Mark A. O’Rourke, MD, MS (Investigation; Project administration).
Funding
Pamm Gross Kahane Research Institute of Life’s Door, Jerusalem, Israel.
Conflicts of interest
BWC is co-founder and Chairman, and PDC is co-founder and President of the non-profit organization Life’s Door. RA is supported by NIH/NCI K12CA090625. IMS is supported by the American Cancer Society (ACS) Clinician Scientist Development Grant and the Andrew Sabin Family Foundation. MAO is Co-chair of the SWOG Cancer Research Network’s Palliative and End-of-Life Care Committee. All other authors have no conflicts of interest to disclose.
References
- 1. Snyder CR. Hope theory: rainbows in the mind. Psychol Inq. 2002;13(4):249-275. [Google Scholar]
- 2. Feldman DB, Bach J.. Hope. In: Friedman H, ed. Encyclopedia of Mental Health. 2nd ed. Elsevier; 2015:332-336. [Google Scholar]
- 3. Corn BW, Feldman DB, Wexler ID.. The science of hope. Lancet Oncol. 2020;21(9):e452-e459. [DOI] [PubMed] [Google Scholar]
- 4. Sullivan MD. Hope and hopelessness at the end of life. Am J Geriatr Psychiatry. 2003;11(4):393-405. [PubMed] [Google Scholar]
- 5. Feldman DB, Kasl-Godley J, Khouzam A, Pisca NE, Cabrera AP, Donboli M.. From cure to quality of life: the shifting meaning of hope at the end of life. In: Bauman W, ed. Hope: Global Interdisciplinary Perspectives. Inter-Disciplinary Press; 2008:133-146. [Google Scholar]
- 6. Corn BW, Feldman DB, Hull JG, O’Rourke MA, Bakitas MA.. Dispositional hope as a potential outcome parameter among patients with advanced malignancy: an analysis of the ENABLE database. Cancer. 2022;128(2):401-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Oosterveld-Vlug MG, Francke AL, Pasman HR, Onwuteaka-Philipsen BD.. How should realism and hope be combined in physician–patient communication at the end of life? An online focus-group study among participants with and without a Muslim background. Palliat Support Care. 2017;15(3):359-368. [DOI] [PubMed] [Google Scholar]
- 8. Hagerty RG, Butow PN, Ellis PM, et al. Communicating with realism and hope: incurable cancer patients' views on the disclosure of prognosis. J Clin Oncol. 2005;23(6):1278-1288. [DOI] [PubMed] [Google Scholar]
- 9. Mori M, Fujimori M, Ishiki H, et al. Adding a wider range and “hope for the best, and prepare for the worst” statement: preferences of patients with cancer for prognostic communication. Oncologist. 2019;24(9):e943-e952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clayton JM, Hancock K, Parker S, et al. Sustaining hope when communicating with terminally ill patients and their families: a systematic review. Psychooncology. 2008;17(7):641-659. [DOI] [PubMed] [Google Scholar]
- 11. Busireddy KR, Miller JA, Ellison K, et al. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9(3):294-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vetter MH, Vetter MK, Fowler J.. Resilience, hope and flourishing are inversely associated with burnout among members of the Society of Gynecologic Oncology. Gynecol Oncol Rep. 2018;25:52-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shah M, Ferguson A, Corn PD, et al. Developing workshops to enhance hope among patients with metastatic breast cancer and oncologists: a pilot study. J Clin Oncol Oncol Pract. 2021;17(6):e785-e793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Feldman DB, Dreher DE.. Can hope be changed in 90 minutes? Testing the efficacy of a single-session goal-pursuit intervention for college students. J Happiness Stud. 2012;13(4):745-759. [Google Scholar]
- 15. Li Z, Mao X, He Z, Zhang B, Yin X.. Measure invariance of Snyder’s dispositional hope scale in American and Chinese college students. Asian J Soc Psychol. 2018;21(4):263-270. [Google Scholar]
- 16. Read M, Noonan I.. What does hope mean when working with suicidal prisoners? Br J Mental Health Nurs. 2018;7(1):24-31. [Google Scholar]
- 17. Pandit D, Agrawal S.. Exploring challenges of online education during COVID times. FIIB Business Rev. 2022;11(3):263-270. [Google Scholar]
- 18. Peynircioğlu ZF, Thompson JL, Tanielian TB.. Improvement strategies in free-throw shooting and grip-strength tasks. J Gen Psychol. 2000;127(2):145-156. [DOI] [PubMed] [Google Scholar]
- 19. Lim S, Lippman LG.. Mental practice and memorization of piano music. J Gen Psychol. 1991;118(1):21-30. [DOI] [PubMed] [Google Scholar]
- 20. Sloan JA, Mahoney MR, Sargent DJ, et al. Was it worth it (WIWI)? Patient satisfaction with clinical trial participation: results from North Central Cancer Treatment Group (NCCTG) phase III trial N0147. J Clin Oncol. 2011;29(suppl 15):6122-6123. [Google Scholar]
- 21. Heydari MR, Taghva F, Amini M, Delavari S.. Using Kirkpatrick's model to measure the effect of a new teaching and learning methods workshop for health care staff. BMC Res Notes. 2019;12(1):388. doi: 10.1186/s13104-019-4421-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hershman DL, Unger JM, Hillyer GC, et al. Randomized trial of text messaging to reduce early discontinuation of adjuvant aromatase inhibitor therapy in women with early-stage breast cancer. J Clin Oncol. 2020;38(19):2122-2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Feldman DB, O'Rourke MA, Bakitas MA, et al. Hope, burnout and life satisfaction: an intriguing trinity among investigators of the SWOG Cancer Research Network. J Clin Oncol Oncol Pract. 2021;17(7):e908-e916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bareket-Bojmel L, Shahar G, Abu-Kaf S, Margalit M.. Perceived social support, loneliness, and hope during the COVID-19 pandemic: testing a mediating model in the UK, USA and Israel. Br J Clin Psychol. 2021;60(2):133-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chang EC, Banks KH.. The color and texture of hope: some preliminary findings and implications for hope theory and counseling among diverse racial/ethnic groups. Cult Divers Ethn Minor Psychol. 2007;13(2):94-103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are incorporated into the article and its online supplementary material.