ABSTRACT
The widespread use of Blockchain technology (BT) in nations that are developing remains in its early stages, necessitating a more comprehensive evaluation using efficient and adaptable approaches. The need for digitalization to boost operational effectiveness is growing in the healthcare sector. Despite BT's potential as a competitive option for the healthcare sector, insufficient research has prevented it being fully utilised. This study intends to identify the main sociological, economical, and infrastructure obstacles to BT adoption in developing nations' public health systems. To accomplish this goal, the study employs a multi-level analysis of blockchain hurdles using hybrid approach. The study's findings provide decision- makers with guidance on how to proceed, as well as insight into implementation challenges.
KEYWORDS: Blockchain technology, electronic health records (EHR), public healthcare, modelling, barrier, MCDM
1. Introduction
In developing nations, the expenditure on safeguarding public health is comparatively expensive and increases during catastrophes (Coupet et al., 2021). Public health spending is increasing in emerging nations like China and India to 5% of the GDP (Pérez, 2021). The majority of spending is heading towards digitisation and automation. Thus there are opportunities to enhance the healthcare systems and provide incentives. The Indian healthcare sector is expected to grow to a value of US 372 billion with the emergence of public and private parties (Rai et al.,2021).The technology and information management exhibits an essential role in public healthcare systems and influence health information technology functions and it results into improved public health. Recent research studies have emphasised on digitalisation of the public health systems have the potential to benefit beneficiaries. Among recent digital technologies, blockchain technology (BT) is gaining momentum into public services. The evolutionary technology has core properties across all its real-life applications including traceability, decentralisation, autonomy and immutability. BT build a well trusted digital network that maintains digital transactions across every user levels. With its evolving presence, no industry is exempted from the commercial and technical competency of BT. BT exhibits great potential and influence the industry and social order. Blockchain provides sequential, distributed records across the network. With its emergence, Blockchain is getting increasing attention from academic and industrial researchers. Healthcare Industry is focusing on key areas, which includes patient experience (satisfaction, loyalty, word of mouth, etc.), digitalisation, effective market segmentation, promotion, and sustainable marketing solutions. With the latest technology, this industry and its service portfolios can be optimised, and may become highly personalised, mobile, and ubiquitous, which brings an overall improvement such as minimising the travel cost, and service levels. In healthcare, BT can constantly improve interoperability standards on a regular basis. While maintaining the integrity and privacy of the electronic health records (EHR) (Garrido et al., 2021; Sharma & Joshi, 2021). In recent times, health information technology has emerged as a thrust research area where BT can be deployed and that may connect billions of connected devices to generate millions of data transactions (Hasselgren et al., 2020; Jeet & Kang, 2020). Due to advance technologies and infrastructure, the healthcare industry is undergoing a rephrasing stage. The new digital ecosystem is leveraging the value and giving a safe and effective customer experience to the patients. Healthcare Industry is focusing on key areas, which includes patient experience (satisfaction, loyalty, word of mouth, etc.), digitalisation, effective market segmentation, promotion, and sustainable marketing solutions (Malhotra et al., 2022). With the latest technology, this industry and its service portfolios can be optimised, and may become highly personalised, mobile, and ubiquitous, which brings an overall improvement such as minimising the travel cost, and service levels (Saxena & Verma, 2020). The potential of BT in the context of developing nations must be assessed and harnessed (Balasubramanian et al., 2021).
1.1. Research motivation
In some developed nations, the risk of adopting BT in public sectors is relatively low. e.g., countries like USA, UK, and Japan (Malhotra et al., 2021; Sanka et al., 2021). However, it is still in its infancy in emerging markets like India because of unclear BT regulations and guidelines and significant worries over data privacy and stakeholder reliability (Badhotiya et al., 2021; Farouk et al., 2020; Toufaily et al., 2021). In recent years, developing countries have begun digitisation their health care systems to address impending difficulties brought on by the epidemic. Consequently, public health system barriers in developing nations vary from those in developed countries; however, adopting BT can unite a wide range of industries to create societal issues (Amarakoon et al., 2021; Manish Katiyar & Singhal, 2021). BT’s participation in emerging and developing economies is thus crucial because these countries need more reliable digital resources and skills. Previous studies have evaluated the adoption of blockchain technology, value creation, and public-private partnership co-creation (Balasubramanian et al., 2021; L. Sharma et al., 2021; Toufaily et al., 2021). According to Schulz (2020), Blockchain technology may fuel a sustainable governance and policy strategy enabling a long-term public health system. In developed countries, research projects have been sparked by the deployment of BT, and those programmes are gaining momentum constantly. (Clohessy et al., 2019; Prakash et al., 2020; Sharma et al., 2021). However, developing countries like India need more research initiatives in BT adoption and related practices. Previous studies have explored BT barriers in developing countries (Schmidt & Sandner, 2017; Schuetz & Venkatesh, 2020). However, no quantitative models are available now that demonstrate how the barriers are connected and encourage BT adoption through sensible and efficient steps to remove the barriers in developing countries like India. Blockchain technology (BT) has been increasingly important in recent years for identifying interdependencies and integrating critical roles, resources, data, and capabilities in public healthcare systems (Puri et al., 2021; Tanwar et al., 2020).In developing nations with underdeveloped institutions and few options to address social problems connected to public health, BT may provide local government with more influence. It is necessary to investigate the potential of BT for public health in developing nations like India as well as the primary adoption hurdles, operational guidelines, and offering a strategic roadmap for the future of public health.
The aim of the study paper is to examine the research questions and seek to bridge the research gap that has been identified.
RQ1:
What are barriers to enabling the use of BT in the public healthcare systems of developing nations
RQ2:
How do BT adoption barriers in the healthcare sector relate to those in developing nations?
RQ3:
What is the strategy for reducing the hurdles to BT adoption in the healthcare sector?
The study on BT adoption barriers linked to public healthcare institutions’ ability to use digital infrastructure, like the UTAUT, to understand the dynamics of change management (Arfi et al., 2021; Joshi, 2013; Warkentin & Orgeron, 2019). The study aims to analyse key BT-related barriers in developing nations like India to respond to the study’s issues. The following goals were set to close this literature gap:
To examine into the implementation barriers for BT in the context of Indian public healthcare;
To recognise the linkage among the chosen barriers identified by the systematic literature study;
To offer tactical recommendations to remove the barriers to BT adoption in public health systems.
The paper is organised as follows: background details on blockchain technology, the public health system, and the theoretic foundations of the research article are elaborated in Section 2. The methodologies are discussed in Section 3, along with an explanation of how they were used for the study. The proposed research framework and a thorough discussion of the use of BT in public health are presented in the next section. The research study’s findings are discussed in Section 5. The plan roadmap to lessen the effect of impediments on public health systems is highlighted in Section 6. Section 7‘s conclusion, restrictions, and open research barriers are all incorporated for upcoming research.
2. Literature review
2.1. Public healthcare and digital technologies
Using Systematic Literature Review (SLR)(Gebayew et al., 2018) enlightened the upsurge practice of digital technologies in healthcare. Similarly, Sikandar et al., 2022). gives insights on the usages of digital technology to overcome public service delivery challenges. Similarly, Golinelli et al. (2020) conducted a thematic analysis on a variety aspects of technology adoption in public health systems (viz, Electronic Health Records (EHRs); Telemedicine; The use of mobile health (mHealth); Medical research, Supply Chain Management, health data analytics; risk of cybersecurity threats; raises of privacy and legal concerns). Osipov and Skryl (2021) discussed the role and digital technologies' effects in improving the delivery of healthcare services and support public health management. Although, there are several critical perspectives on digital health (Chaudhary et al., 2022); Zarour et al., 2021). Additionally, there is concern that digital health technologies may be designed and implemented in ways that disproportionately benefit specific groups while leaving others behind (Veinot et al., 2018). Finally, some critics argue that the emphasis on digital solutions may need to address the underlying social determinants of health (Hatef et al., 2019; Justvig et al., 2022). The literature supports the argument that digital technologies have the potential to greatly improve the delivery of healthcare services and support population health management in public healthcare. It’s important to consider the barriers and potential solutions to implement them effectively. Despite the importance of all emerging digital technologies, SLR indicates a significant need for study, particularly in the domains of blockchain technologies and public healthcare.
2.2. Systematic literature review
This section discussed the systematic literature review on the implementation barriers of blockchain technology in public healthcare. The SLR was carried out to explore the relevant published literature on healthcare industry and blockchain technology. The purpose of the SLR was to search and critically evaluate studies that have examined the difficulties and obstacles encountered when implementing blockchain technology in various aspects of public healthcare such as medical records management, supply chain management, and data sharing. In addition, The goal of the review was to identify patterns, gaps, and inconsistencies in the existing literature in order to inform future research and implementation decisions. In addition, Review has been performed by authors in accordance with Preferred Reporting Items for Systematic Reviews (PRISMA) standards (Cacciamani et al., 2023).Although, Common parameters that make systematic reviews reproducible and scientifically sound are frequently not understood in these studies (Pollock and Berge, 2018; Mitchell & Kan, 2019; Rethlefsen et al., 2021). PRISMA provides a standard peer-review process that uses a set of guidelines, and this paper adheres to it (Moher et al., 2015), to help ensure the effectiveness of the revision procedure and its reproducibility. A review methodology that outlines the criteria utilised to select publications, the search strategy, data extraction tools, and data analysis methodologies was developed for the current study. The details of review methodology is explained in the following steps:
2.2.1. Data sources and search strategies
We thoroughly examined two academic databases (Web of Science and Scopus) between 2015 and 2020. We identified peer-reviewed studies written in the English language. We conducted a broader search strategy to determine the eligible studies for review. Search terms were modified together with Boolean operators. The search string includes “Healthcare” AND “Blockchain technology”; “Public Health” AND “Blockchain technology”; “Blockchain” AND “Public Healthcare”; “Public Health” AND “barriers for blockchain adoption” as keywords for topics searched as article titles, and abstract, in Scopus and Web of Science. The qualifying papers that were included after the computerised search also had their reference lists manually searched.
2.2.2. Selection of studies
Using the aforementioned standards (Meade & Richardson, 1997; Meline, 2006). Authors independently assessed paper titles and abstracts to decide which papers qualified for inclusion in the research. For final inclusion, the complete text of papers that might be pertinent was examined. Every disagreement was settled by agreement with one of the researchers.
2.2.3. Data assessment
The authors independently extracted the information and evaluated the quality of the articles. Based on the previous researches (Joshi et al., 2022; Sharma et al., 2022); Unhelkar et al., 2022), each study’s data were collected and entered into an evidence table. The authors gathered information through original research. Any disagreements were resolved by the writers’ collective agreement.
2.2.4. Eligibility criteria
There were three rounds of choosing the papers to review. The authors participated in the screening of the title and abstract for the first round of analysis. Afterwards, they examined the articles in the second round. The results were arranged in a table, and the selection criteria were made in accordance with the study topic. Studies with no full text accessible, were deleted. To determine their inclusion in our study, articles from this round were recovered and given a thorough inspection. All papers that did not discuss research analysing the procedure and results of competence development in relation to graduate employability were disregarded in order to answer our specific research concerns. Using the Scopus and Web of Science databases, the relevant papers were extracted using the procedures outlined in Table 1.
Table 1.
The search criteria.
| Search terms | Initial search | First screening | Second screening | Third screening |
|---|---|---|---|---|
| ‘Healthcare AND ‘Blockchain technology’ | 15 | 10 | 8 | 5 |
| ‘Public health’ AND ‘blockchain technology’ | 104 | 43 | 32 | 12 |
| ‘blockchain’ AND ‘public healthcare’ | 65 | 23 | 12 | 8 |
| ‘public health’ and ‘digital technology’ | 48 | 12 | 8 | 6 |
| ‘public health’ AND ‘barriers for blockchain adoption’ | 18 | 9 | 3 | 2 |
| Total articles | 33 |
2.2.5. Constitution of the corpus of analysis
By primary author’s name and the year of publishing, the studies are listed in alphabetically. The texts were given a number to identify them. Based on methods and methodologies recommended by Vaismoradi et al. (2013), a thematic analysis of the articles’ content was conducted. The research solely used journal publications published between “2015–2020”. In the initial search, 250 items were discovered. 97 articles that were relevant to the study themes remained after the duplicates were eliminated. Working papers, and conference proceedings were also omitted.The listed studies were arranged chronologically by first author last name and by year of publication. A number was used to code the articles. Thematic content analysis of the articles was conducted utilising techniques and methods created by Archibald et al. (2015). There were found to be 63 papers that were relevant to the study’s questions. Cross-referencing was employed to complete the selection process, and 3 relevant articles are added in the pool of documents. Thus, 33 papers were ultimately picked. Figure 1 depicts the process of data synthesis. Due to the special nature of the subject, research from other industries was taken into account to determine the structures. The study’s systematic literature review (SLR), which is presented in Table 1, was completed. In order to address our specific research concerns, any articles that did not discuss research evaluating the process and results of competence development associated to graduate employability were eliminated from consideration.
Figure 1.

Systematic Review Process (Source: Rethelfsen et al., 2021).
2.2.6. Characteristics of included studies
Figure 2 shows that 2015 was indeed the year with the highest number of studies included in our search. Our results indicate that the volume of research published during the previous four years has significantly increased.
Figure 2.

Relevant published studies.
2.3. Blockchain technology and public healthcare
The healthcare sector is growing continuously, the need for the players to use new business strategies (Moreiraand Silva, 2016; Costa & Godinho Filho, 2016; Tuisku et al., 2019). About 60% of the healthcare sector as a whole still needs to prepare to adapt to a collaborative and integrated environment. Analytics cannot be implemented or used as a result. In contrast to other sectors, like retail and finance, this one lacks cutting-edge technology and the adoption of analytical tools/methods (Y. Wang & Hajli, 2017). The ecosystem in this sector is gradually evolving, with a focus on value chains’ improvisation (Blijleven et al., 2016). However, operational barriers have restricted the public health sector’s capacity for innovation (such as data privacy and cost-effective security, etc). (Pratt, et al., 2018). The ageing of the population in developing nations, where the average age of the population is increasing, is another emerging issue (Carson et al., 2020; Joshi & Sharma, 2022). Consequently, efficient and patient-centred public healthcare systems. The healthcare industry has been using BT to modernise public health systems (Arfi et al., 2021; Unhelkar et al., 2022). By 2024, the BT will grow by 20 billion USD in worth, in contrast to 315.9 million USD in 2015 (Tandon et al., 2020). BT is a sequential structured arrangement of blocks carrying records (Lee & Yoon, 2021; Wenzl, 2019). Both Figure 3(a) and (b) represents the sequence of block in a blockchain.
Figure 3.

(a) Block and its components. (b) Blockchain sequence.
Source: Authors.
EHRs are a part of the newly growing “digital health” industry, which aims to enhance public services by managing internet-enabled databases (Cheong et al., 2009; Dutot et al., 2018; Miller et al., 2007). E-health means improved public health possible locally, regionally, nationally, and internationally (Eysenbach, 2000; van Gemert-Pijnen et al., 2011). Redundancy and higher healthcare service costs are driven by the existence of various healthcare systems (Okpala et al., 2018). Initiated in Canada in 2001, the idea of Electronic Health Record System (EHRs) has since spread to all developed nations (Mohammad et al., 2018; Protti, 2015; Tahan et al., 2017; Tharmalingam et al., 2016). Although the utilisation of EHRs for transactions within and between hospitals and clinics is becoming more extremely common, their full potential has not yet been realised due to several adoption and usage barriers related to health networks, health information exchange (HIE), national health policy (NHP), and health IT standards (Demiris, 2004). The electronic health record (EHR) systems gather and store data that is then organised to perform various analyses for decision-making (Rasmi et al., 2020). EHR is a particular formal information system in terms of functionality that enables integration across various healthcare providers (Qiu et al., 2018). EHR offers several benefits, including the ability to control diseases and contributes to reducing drug mistakes (Alonso-Coello et al., 2016; Purushotham et al., 2018). Despite some disadvantages to EHR, such as lengthy wait times, security issues, and interoperability (Coorevits et al., 2013; Roehrs et al., 2017). In emerging countries like India, public health is constantly evolving (Gauttam et al., 2021; Luthra et al., 2022). Strategically incorporating BT can minimise medical errors that could otherwise threaten patients’ health and the entire viability of healthcare systems (Dwivedi et al., 2019). Implementing EMR with BT is becoming increasingly essential as one of the ICT goals (Joshi et al., 2022). Therefore, implementing BT in an e-health system may be a great method and source of learning for the cause of global healthcare sector.
2.4. Blockchain technology and public healthcare in developing countries
In developing countries, e-health services are progressively gaining popularity. Blockchain technology has the capacity to enhance public healthcare in underdeveloped nations by offering a transparent and secure approach to storing and exchanging patient data, as well as to facilitate transactions and payments. Some of the ways that blockchain technologies can be used in public healthcare in developing countries includes:
Electronic Medical Records (EMRs): Utilising blockchain technology, a decentralised, secure system for patient data inventory can be developed, which can improve the quality and efficiency of healthcare delivery.
Supply Chain Management: Drug movement can be traced using blockchain technology and other medical supplies from manufacturers to patients, which can assist in preventing fraud and guaranteeing that patients receive products that are both safe and effective.
Clinical Trials: Using blockchain technology, a safe and open system can be developed for tracking and sharing data from clinical trials, which can help to increase trust in the results and speed up the development of new treatments
Micro-insurance and Medical Claims: Using blockchain technology, a safe and open system for managing financial transactions for micro-insurance and medical claims, which can help to increase access to healthcare for people in developing countries who are not covered by traditional insurance.
Telemedicine: Patients in rural and underdeveloped areas may have greater access to healthcare if blockchain technology is used to create a secure and transparent system for remote consultations and medical treatment.
However, it’s worth noting that blockchain technology is still in the early stages of development and it’s important to be aware of its limitations and potential barriers. Additionally, it’s also important to consider the regulatory and legal frameworks that exist in each country as well as the cultural and socioeconomic adoption factors and success of blockchain-based healthcare systems in developing countries. The barriers to adopting blockchain technology are listed in Table 2.
Table 2.
BT adoption in public healthcare: key barriers.
| Code | Barriers | Description | Industry |
|---|---|---|---|
| BT-1 |
Absence of trust among parties (Bublitz et al., 2019; Esmaeilzadeh & Mirzaei, 2019; Randall et al., 2017) |
The hospital administration, private parties, and suppliers all lack sufficient synchronization and coordination, which results in poor levels of party coordination. | Healthcare |
| BT-2 |
Limited data repository infrastructure (A. Alam et al., 2021; Fang et al., 2021; Lenert et al., 2021; Yang et al., 2021; Hemalatha, 2021) |
lack of ability for expansion accommodate patient development beyond a particular limit | Healthcare |
| BT-3 |
Scaling up of data (Fang et al., 2021; Hussien et al., 2021) |
Real-time data interchange in blockchains may be hindered due to a low level of data upscaling | Healthcare |
| BT-4 |
Data stewardship (Ali et al., 2021; Fang et al., 2021; Siqueira et al., 2021) |
The centralised data access that is exclusively available to hospital administration. It lessened the advantages of data reuse | Healthcare |
| BT-5 |
High maintenance costs (Hussey & Kennedy, 2021; Kohn et al., 2022 |
Healthcare are skeptical about the returns after deploying BT as the industry is still in its infancy | Healthcare |
| BT-6 |
Lack of Health Informatics Standards (F. A. Reegu et al., 2021; Hussey & Kennedy, 2021; Shuaib et al., 2021a) |
Standards for heath data on blockchains and accessing them are currently being developed. | Healthcare |
| BT-7 |
Data Risk Management (Hemalatha, 2021; Yaqoob et al., 2021) |
Security issues are connected to BT. | Healthcare |
| BT-8 |
Low investments on R&D (Bublitz et al., 2019; Esmaeilzadeh & Mirzaei, 2019) |
Public hospitals give developing technologies like BT and health informatics low R&D priorities. | General |
| BT-9 |
low understanding of BT (Bublitz et al., 2019; Esmaeilzadeh & Mirzaei, 2019; F. Reegu et al., 2021); L. Sharma et al., 2021) |
Traditional healthcare practitioners are not concerned with using BT in the healthcare sector | Healthcare |
| BT-10 |
low understanding of the legal implications of BT (Balasubramanian et al., 2021; Bittins et al., 2021; Shuaib et al., 2021b) |
The legal aspects of deploying BT are poorly understood, which provides a barrier to future upgrades. | Government/Regulatory bodies |
| BT-11 | Lack of envision future for technological projects (Gill, 2021; Yaqoob et al., 2021) | The top level management lacks commitments since they have a dim view of the future and see no advantages beyond financial advantages from implementing BT | Healthcare |
| BT-12 |
a lack of dedication on the part of higher authorities (Alzahrani et al., 2022) |
Low degree of commitment to BT adoption and implementation is caused by high level management's lack of a vision and roadmap. | Healthcare |
| BT-13 | Low technical skills among working executives (L. Sharma et al., 2021; Nasr et al., 2021) | Low technical competency due to shortage of technical knowledge. | Healthcare |
| BT-14 |
Low/ inadequate infrastructure to support BT adoption and implementation (Hemalatha, 2021; Yaqoob et al., 2021) |
Low integration in cyber-physical interface is brought about by a lack of infrastructure | Healthcare |
| BT-15 | Privacy and data security (A. Alam et al., 2021) | High standards of data security and privacy ensure the effectiveness of IT infrastructure. Thus, poor security can end up in dedicated privacy problems, including digital theft and fraud. | Healthcare |
The case location for the current study was one of the government hospitals in the state capital. According to the literature-identified adoption hurdles for BT, the respondents in the healthcare industry include important decision-makers, top managers, and important beneficiaries, such as patients from the institute.
3. Research methodology
To enhance the results and address numerous managerial problems, decision-makers used mathematical modelling and sophisticated statistical analysis (Siqueira et al., 2021; Zavadskas et al., 2014). The scientific fields that have used it include business and management (Kazimieras Zavadskas et al., 2018; Zopounidis & Doumpos, 2002; Fang et al., 2021), Tourism (Hosseini et al., 2021; Lin, 2020; Mailly et al., 2014), Aviation (Rasmussen et al., 2023), banking and insurance (Katsimperis & Andrikopoulos, 2021; Korhonen & Voutilainen, 2006; Shen et al., 2017; Wanke et al., 2022), computer science (Eri\cskin, 2021; Yadegaridehkordi et al., 2019), energy (Kandakoglu et al., 2019; Kundakci, 2019; Lak Kamari et al., 2020; Shahnazari et al., 2020), oil & gas (Kandakoglu et al., 2019; Shahi & Dia, 2019; Y. Wang & Hajli, 2017), tourism (Hosseini et al., 2021; Vatankhah et al., 2023), health and medical (Ali et al., 2021; Gardas et al., 2022; Gardas, 2022; Laganà & Colapinto, 2022), and engineering (Ajibade et al., HYPERLINK \l “2021; Cricelli et al., HYPERLINK \l ”2020), are some of the scientific industries that have used it. Public enterprises including telecommunication, electricity, education and healthcare utilise dynamic nature and complexity of the demand, numerous data analysis technologies are employed to assess the routine rating and criteria weights. As a consequence, many precise modelling approaches may be used to assess risks and create rules and regulations. When there are multiple conflicting criteria, decision-makers can utilise MCDM (Multiple Criteria Decision Making) addresses to choose from an array of alternatives. These approaches have been recognised as an operative way to equilibrium numerous factors while making a decision from a restricted array of alternatives. Various MCDM techniques are deployed in the literature for various industries' operations as well as decision-making processes. Some typical MCDM strategies include:
AHP:This technique organises the criteria and alternatives using a hierarchical framework, and it uses pairwise contrasts to ascertain the relative position of every criteria and the comparative efficacy of each alternative.
TOPSIS: Every option is assessed using this method based on the degree to which it resembles an ideal and a fewer-than-perfect respond to which the decision maker had chosen.
PROMETHEE: This method generates a preference ranking of the alternatives through a pairwise comparison of the alternatives based on a set of criteria.
Electre (Elimination Et Choix Traduisant la REalité): This technique uses outranking relationship based on a set of criteria and generates a preference ranking of the alternatives.
MOORA: This technique uses the ratio of the performance of each alternative to the ideal solution to generate a preference ranking of the alternatives.
These are some of the most common MCDM techniques, besides there are many other techniques available under MCDM techniques depending on the specific decision-making problem. Also, MCDM techniques are useful in cost optimisation, risk assessment, supplier selection, green and sustainable supply chains and systems for health. This section discusses the approach for evaluating implementation barriers of blockchain technology in public healthcare. The MCDM techniques- ISM (Interactive Simple Multi-Attribute Rating Technique) and MICMAC (Method of Independent Comparison of Multiple Attributes with Controlled Attribute Weights) are used to evaluate alternatives based on multiple criteria. Conceptually, ISM is an interactive technique where the decision maker assigns scores to alternatives based on their performance on each criteria. The scores are then used to calculate the overall performance of each alternative and generate a preference ranking. The main advantage of ISM is its simplicity and ease of use. MICMAC, on the other hand, is a more complex technique that uses a set of attribute weights, which are determined by the decision maker, to compare the alternatives on each criteria. The alternatives are then ranked based on their overall performance. The main advantage of MICMAC is its ability to control the relative importance of each criteria, which can help to eliminate bias and ensure a fair comparison. Both ISM and MICMAC are widely used in various fields such as engineering, management, and operations research. They are often used in situations where the decision maker has a clear understanding of the alternatives and criteria, and the decision-making problem is relatively simple and well-defined. The present study employs Interpretive Structural Modeling (ISM) to develop hierarchical structures for the variables and identify their relationships. These techniques have been used in previous research to identify adoption barriers (M. Sharma & Joshi, 2019; M. Sharma et al., 2020; Singh et al., 2020). In order to understand and analyse the relationship between various Blockchain adoption barriers, this study employed ISM and Fuzzy MICMAC. Figure 4 demonstrate the ISM-Fuzzy MICMAC process deployed for the study.
Figure 4.
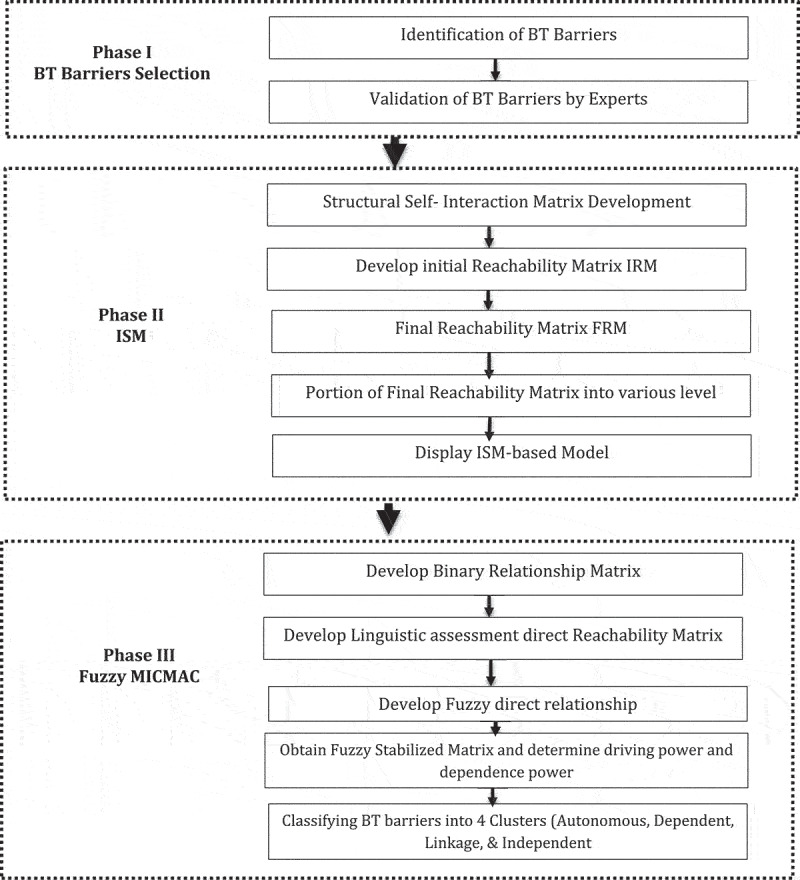
ISM-Fuzzy MICMAC process.
The procedures are explained below:
3.1. Interpretative structural model
Warfield’s comprehensive planned model’s attributes are combined using this method (1974). With the help of an interactive learning process, this strategy arranges several closely connected parts into a comprehensive model (Pradhan & Bhattacharya, 2021; Qarnain et al., 2021). This method’s objective is to divide complex systems into a variety of smaller subsystems and create a hierarchical structure using the expertise and experience of professionals (Kannan et al., 2009). Steps includes:
Step 1: Determining the barriers from prior literature and validating them with the help of local experts.
Step 2: Creating a linkage between each barrier
Step 3: Create a structural self-interaction matrix (SSIM) using four variables (V, A, X, and O) to indicate how the obstacles relate to one another (i and j). Where v denotes that barrier, I will make barrier j worse; A, that barrier j will make barrier I worse; X, that barrier I and barrier j will make each other worse; and O, that barrier I and barrier j are unrelated.
Step 4 and 5: Initial reachability matrix (IRM) development and transitivity testing.
The final reachability matrix is created and divided into several levels in step 5.
Step 6: Create a diagraph and remove all transitive ties from it.
Step 7: A review and conceptual consistency check of the established model is performed.
3.2. Fuzzy MICMAC method
The Fuzzy MICMAC (Method for Intensity Comparison and Mathematical Analysis) method is a multi-criteria decision-making (MCDM) method that is used to evaluate and rank alternatives based on multiple criteria. These are the procedures for applying MICMAC’s fuzzy (Matrice d’impacts croisés multiplication appliqué á un classment) algorithm.
Step 1: Creating a reachability matrix for binary direct from ISM variables: Transitivity is disregarded and the diagonal values are substituted with zero.
Step 2: Experts undertake the responses for the fuzzy binary direct relationship matrix, which is based on the fuzzy set theory.
Step3: Stabilized matrix for fuzzy-MICMAC: The matrix is multiplied repeatedly until the values of the driving and dependency powers are constant.
3.3. Data collection
The public healthcare systems served as a source for data collection. Table 3 depicts the demography of the experts chosen for this study. The specialists are made up of physicians, workers, an IT manager, and an administration manager.
Table 3.
Level segmentation Iterations.
| ITERATION I | ||||||
|---|---|---|---|---|---|---|
| Reachability values | Antecedent values | Intersection values | LEVEL | |||
| 1,2,3,4,5,6,7,13,14,15 | 1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 | 1,2,3,4,5,6,7,13,14,15 | I | |||
| 1,2,3,4,5,6,7,13,14,15 | 1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 | 1,2,3,4,5,6,7,13,14,15 | I | |||
| 1,2,3,4,5,6,7,13,14,15 | 1,2,3,4,5,6,7,8,9,11,12,13,14,15 | 1,2,3,4,5,6,7,13,14,15 | I | |||
| 1,2,3,4,5,6,7,13,14,15 | 1,2,3,4,5,6,7,8,9,11,12,13,14,15 | 1,2,3,4,5,6,7,13,14,15 | ||||
| 1,2,3,4,5,7 | 1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 | 1,2,3,4,5,7 | I | |||
| 1,2,3,4,5,6,7,13,14,15 | 1,2,3,4,6,7,8,9,10,11,12,13,14,15 | 1,2,3,4,6,7,13,14,15 | ||||
| 1,2,3,4,5,6,7,13,14,15 | 1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 | 1,2,3,4,5,6,7,13,14,15 | I | |||
| 1,2,3,4,5,6,7,8,9,10,11,13,14,15 | 8,9,10,11,12 | 8,9,10,11 | ||||
| 1,2,3,4,5,6,7,8,9,11,13,14,15 | 8,9,10,11,12 | 8,9,11 | ||||
| 1,2,4,5,6,7,8,9,10,12 | 8,10,11,12 | 8,10,12 | ||||
| 1,2,3,4,5,6,7,8,9,10,11,13,14,15 | 8,10,11,12 | 8,10,11 | ||||
| 1,2,3,4,5,6,7,8,9,10,11,12,13,14,15 | 10,12 | 10,12 | ||||
| 1,2,3,4,5,6,7,13,14,15 | 1,2,3,4,6,7,8,9,11,12,13,15 | 1,2,3,4,6,7,13,15 | ||||
| 1,2,3,4,5,6,7,14,15 | 1,2,3,4,6,7,8,9,11,12,13,14,15 | 1,2,3,4,6,7,14,15 | ||||
| 1,2,3,4,5,6,7,13,14,15 |
1,2,3,4,6,7,8,9,11,12,13,14,15 |
1,2,3,4,6,7,14,15 |
|
|||
| ITERATION II | ||||||
| 6,13,14,15 | 6,8,9,10,11,12,13,14,15 | 6,13,14,15 | II | |||
| 6,8,9,10,11,13,14,15 | 8,9,10,11,12 | 8,9,10,11 | ||||
| 6,8,9,11,13,14,15 | 8,9,10,11,12 | 8,9,11 | ||||
| 6,8,9,10,12 | 8,10,11,12 | 8,10,12 | ||||
| 6,8,9,10,11,13,14,15 | 8,9,11,12 | 8,9,11 | ||||
| 6,8,9,10,11,12,13,14,15 | 10,12 | 10,12 | ||||
| 6,13,14,15 | 6,8,9,11,12,13,15 | 6,13,15 | ||||
| 6,14,15 | 6,8,9,11,12,13,14,15 | 6,14,15 | II | |||
| 6,13,14,15 |
6,8,9,11,12,13,14,15 |
6,13,14,15 |
|
II |
||
| ITERATION III | ||||||
| 8,9,10,11,13 | 8,9,10,11,12 | 8,9,10,11 | ||||
| 8,9,11,13 | 8,9,10,11,12 | 8,9,11 | ||||
| 8,9,10,12 | 8,10,11,12 | 8,10,12 | ||||
| 8,9,10,11,13 | 8,9,11,12 | 8,9,11 | ||||
| 8,9,10,11,12,13 | 10,12 | 10,12 | ||||
|
13 |
8,9,11,12,13 |
13 |
|
III |
||
| ITERATION IV | ||||||
| 8,9,10,11 | 8,9,10,11 | 8,9,10,11 | 8,9,10,11 | |||
| 8,9,11 | 8,9,11 | 8,9,11 | IV | |||
| 8,9,10,12 | 8,9,10,12 | 8,9,10,12 | 8,9,10,12 | |||
| 8,9,10,11 |
8,9,10,11 |
8,9,10,11 |
|
8,9,10,11 |
||
| ITERATION V | ||||||
| 10,12 | 10,12 | 10,12 | V | |||
4. Models application
ISM and Fuzzy MICMAC applications follow the step-by-step methodology described in the previous section.
4.1. ISM application
The matrices of the ISM application were created using expert input. The ISM methodology’s procedures, which are described in section 3.1, were used to produce the tables SSIM, IRM, level segmentation, and FRM. Transitivity tests were carried out using the MATLAB software. Table 4 demonstrate initial reachability matix
Table 4.
Experts details.
| Variables | Number of experts |
|---|---|
| GENDER | |
| Female | 8 |
| Male | 7 |
| AGE (in years) | |
| 25–30 | 8 |
| 31–35 | 3 |
| 36–40 | 2 |
| 41–45 | 1 |
| 46–50 | 1 |
| EDUCATION | |
| Ph.D. | 3 |
| MD/MBBS | 4 |
| Post- Graduation | 2 |
| Graduation (Btech, BSc.) | 6 |
| EXPERIENCE (in years) | |
| 0–5 | 4 |
| 6–10 | 5 |
| 11–15 | 3 |
| > 15 | 3 |
| ROLE | |
| Surgeon | 4 |
| Nurse staff | 3 |
| Patients | 2 |
| Functional Manager | 2 |
| Technical Manager | 4 |
For each barrier, the reachability set and the precursor set are determined. When it comes to reachability and intersection sets, the top order barriers in the ISM hierarchy are those that have the same values. Iterations are carried out in order to create a hierarchical structure. Table 5 demonstrate the level segmentation.
Table 5.
ISM-Fuzzy MICMAC process.
| BT-1 | BT-2 | BT-3 | BT-4 | BT-5 | BT-6 | BT-7 | BT-8 | BT-9 | BT-10 | BT-11 | BT-12 | BT-13 | BT-14 | BT-15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BT-1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| BT-2 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| BT-3 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| BT-4 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| BT-5 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| BT-6 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| BT-7 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| BT-8 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 |
| BT-9 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| BT-10 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| BT-11 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 |
| BT-12 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| BT-13 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| BT-14 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| BT-15 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
4.2. Fuzzy MICMAC application
MICMAC application utilises the ISM results.The detailed process described in section 3.2 is used to create a fuzzy MICMAC stabilised matrix. The stabilised matrix is used to form four clusters: the autonomous, connecting, and driving clusters, which are seen in Figure 3.
5. Findings and discussion
This is one of pioneer research studies that aims to analyse the BT adoption levels in public healthcare on a hierarchical scale. An integrated ISM-Fuzzy MICMAC technique was used to generate hierarchical levels of BT in public healthcare.
Figure 2 shows the ISM findings. low understanding of BT (BT-9),Low investments on R&D (BT-8), Low future projections for technical projects (BT-11), low understanding of the legal implications of BT (BT-10), lack of dedication on the part of higher authorities (BT-12) are the key drivers for all the other block chain adoption barriers. low understanding of the legal implications of BT (BT-10), lack of dedication on the part of higher authorities (BT-12) have been found to be the strongest driving force, which resolves the initial research question. The Fuzzy MICMAC technique, which classifies adoption barriers in BC into three primary clusters, validates the findings. Cluster I has no existing barriers. This indicates that the study does not have any weak barriers.
Dependant variables from Cluster II, linkage variables from Cluster III, and driving variables from Cluster IV based on the driving forces and reliance. Cluster II includes the barriers with strong support but modest driving forces. The lack of trust between parties (BT-1), a lack of adequate infrastructure for data repositories (BT-2), the scaling up of data (BT-3), data stewardship (BT-4), high maintenance costs (BT-5), data risk (BT-7), the absence of standards for health informatics (BT-6), the lack of adequate infrastructure to facilitate the adoption of BT (BT-14), and privacy and data security are among the barriers in this cluster (BT-15). All other obstacles must reduce the effect of dependent barriers on overall performance in order to avoid these barriers. Executives lack technical expertise and knowledge (BT-13). Cluster III contains the linkage barrier, which has a strong driving and dependency power. Driving obstacles are a part of Cluster IV. These barriers have the strongest driving force and a moderate dependant power. The main obstacles are low R&D expenditures (BT-8), low BT awareness (BT-9), low future planning for technology projects (BT-11), ignorance of BT’s legal implications (BT-10), and a lack of commitment from higher authorities (BT-12). At the lowest ISM level, these restrictions were reached. Figure 5 explain the ISM levels. Whereas, Figure 6 depicts the fuzzy MICMAC.
Figure 5.
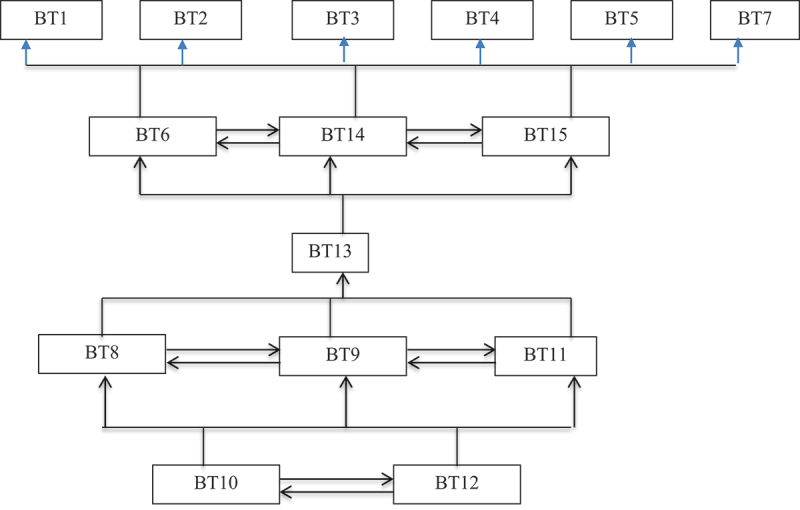
ISM levels.
Figure 6.

FUZZY-MICMAC diagram.
5.1. Industrial implications
The study’s findings not only add to the body of knowledge in the field but also provide a thorough understanding of the barriers to BT adoption in healthcare settings in developing nations. Future researchers and decision-makers may benefit from the study’s insights by better understanding BT adoption barriers. The study suggest few policy implications, including:
i) Secured medical Data
Integration of the various partners in the medical supply chain with shared data from EHRs, medical equipment, patient biomarkers, and patient feedback. For the information to flow freely, security-related barriers should be eliminated.
ii) Reliable partnership
BT can help in reducing the fake and other threats of healthcare. Tracking of the drug supply chain con- nected to a BT enabled healthcare system for fast delivery.
iii) Integrated Quality Management
The technology relies on exchange which is based on validation, so this study is helpful for automatically verifying the claims via network execution. Since there is no central authority, there won’t be any errors or frauds.
5.2. System impact of implementation of blockchain in public healthcare
The blockchain adoption is greatly enhance the efficiency, security, and privacy of healthcare data management. Some potential benefits include:
5.2.1. Improved data security
Blockchain’s decentralised and immutable nature can protect against data breaches and unauthorised access to sensitive patient information.
5.2.2. Increased data sharing
By creating a secure and transparent way to share medical records, blockchain can facilitate better communication and collaboration between healthcare providers, researchers, and patients.
5.2.3. Improved supply chain management
With the goal to increase transparency and lower the possibility of receiving counterfeit or obsolete goods, blockchain technology has the potential to improve the healthcare supply chain.
5.2.4. Streamlined administrative processes
Blockchain can automate many administrative tasks, such as claims processing and medical billing, reducing costs and increasing efficiency.
5.2.5. Enhanced privacy and control over personal data
Blockchain allows patients to have more control over their personal medical data, which can be shared only with authorised parties, and also allows them to be rewarded for sharing their data with researchers. However, there are also potential barriers that must be addressed in order for blockchain to be successfully implemented in the public healthcare system. Some of them are:
5.2.6. Complexity of integration and coordination
mplementing blockchain technology in a public healthcare system requires coordination and collaboration between multiple stakeholders, including government, healthcare providers, and technology companies. This can be a complex and time-consuming process.
5.2.7. Technical barriers
Blockchain technology is still relatively new, and there are still barriers related to scalability, interoperability and regulatory compliance that need to be addressed before it can be widely adopted in public healthcare systems.
5.2.8. Cost considerations
Implementing blockchain technology in a public healthcare system can be expensive, and it is important to consider the costs and benefits before making a decision to adopt it.
5.2.9. Lack of standardisation
One of the biggest barriers facing blockchain in healthcare is the lack of standardisation, which makes it difficult for different systems to communicate and share data.
5.2.10. Limited adoption
It's essential to keep in mind that the blockchain technology is still in its earliest stages of growth and has not yet been widely incorporated into the public healthcare system, so more research and development are needed before it can be fully integrated. It is significant to understand that the success of blockchain in healthcare depends on the ability of different stakeholders to come together and develop common standards for data governance, as well as addressing the technical and cost barriers mentioned above. Furthermore, it is crucial to have a clear understanding of the specific use cases where blockchain can bring the most value, and to pilot and test the technology before a wide- scale implementation.
6. Strategic roadmap
The study’s primary research goals are to assess BT’s potential in public healthcare and the obstacles to its implementation in the industry. Decision-makers can use the study’s findings to develop a strategic plan for incorporating digital technologies into public healthcare, such as blockchain technology. The study’s fundamental finding is to understand the interrelationships among adoption-related hurdles to BT as well as the basis of causality and importance. Due to several obstacles, BT adoption has to be more widespread in emerging economies. If health systems and politicians know the barriers to BT’s successful deployment and the connections between them, BT implementation can be improved, especially for public health. Findings from the study must be considered when assessing the effects of various obstacles to adopting BT in healthcare systems, including:
The establishment of a centralised blockchain-enabled platform for collaboratively developing new, open healthcare systems with industrial symbiosis networks that provide a beneficial digital ecosystem for resource sharing between parties.
The top management’s dedication to sustainable practices will make the health organisation’s focus on cooperating on BT implementation more acute.
The broader Strategic roadmap for blockchain technology in public healthcare, includes:
Identify specific use cases: Determine how blockchain technology can be applied to improve specific areas of public healthcare, such as medical record keeping, supply chain management, and secure communication between healthcare providers.
Build a coalition: Assemble a team of healthcare professionals, government officials, and blockchain experts to develop a strategic roadmap for implementing blockchain technology in public healthcare.
Develop a proof-of-concept: Create a pilot project to test the feasibility and effectiveness of using blockchain technology in a specific area of public healthcare.
Secure funding: Obtain the necessary funding to implement the blockchain solution on a larger scale.
Implement and Scale: Roll out the blockchain solution to a larger group of healthcare providers and patients, and continually monitor its effectiveness.
Regulate and Standardize : Establish regulations and standards for the use of blockchain technology in healthcare to ensure the security, privacy and integrity of medical data.
Continual Improvement : Continuously assess and improve the blockchain solution through feedback and data analysis to ensure it remains effective and relevant.
6.1. Conclusion, limitations and open research barriers
The public healthcare sector has much potential to be transformed by blockchain technology (BT). If applied properly, several operational difficulties can be readily managed, including the cost of maintaining public hospital records, ineffective healthcare procedures, and data breaches. The general expertise BT has gained in public healthcare can assist hospitals and public healthcare facilities in managing the COVID-19 pandemic outbreak and adequately securing patient data and records. With the government’s support, private organisations and NGOs can take more initiatives to address ongoing societal issues and offer public services that promote economic health. BT in public health is an important area of research to explore collaboration, interdependencies, electronic resource sharing, and public services. Rarely have researchers used fuzzy-MICMAC analysis to determine the link between the variables and validate the ISM results. The outcomes of our modelling indicate the many obstacles about how significant they are on the scales of dependency, autonomy, connection, and independence. In speaking with specialists, it has been noted that they are still keeping an eye on how the top athletes are utilising technology to determine how it will affect their performance and day-to-day activities. Since adopting a BC is an expensive process, they do not want to take a chance. Quantitative research on the potential advantages of BT in public health in developing nations is scarce. The top-level management is also more concerned about the need for functional skills, infrastructure support, and adoption readiness. Another issue in a nation like India is the lack of specialists in the merging of healthcare systems and BT. Top-level management typically consists of doctors. Due to the current IT laws, this technology encounters difficulties in the Indian healthcare sector According to Information technology Act, any compromise of personal data should result in compensation for the victim. The creation of data, its security, and the reduction of operational costs for the two primary stakeholders – the patient and the healthcare provider – are all major difficulties for the healthcare system at the moment. BT can also aid in the detection of phoney and inferior pharmaceuticals. BC technology can be used to trace the drug supply chain that is linked to a healthcare system to assure the right quality and timely delivery.
6.2. Limitations and future research directions
Healthcare systems might grow more transparent, secure, and efficient thanks to blockchain technology, but there are also limitations that have to be given consideration. Some of the limitations include scalability, interoperability, and regulatory compliance. Scalability is a major issue for blockchain in health- care, as current systems are not able to handle the large amounts of data and transactions that are typically present in healthcare systems. The lack of interaction between different blockchain systems, making it hard to transmit data between different healthcare institutions, is another problem with interoperability. Regulatory compliance is another limitation, as the use of blockchain in healthcare raises a number of legal and privacy concerns. These include issues related to data security and patient privacy, as well as questions about the legal status of blockchain- based medical records. The authors aims to highlight the barriers that BT adoption in public healthcare faces.To this end, they have used a multi-criteria deci- sion-making technique. Future research may docu- ment the impact of obstacles to BT adoption in the public health sector in emerging economies. Additionally, selected case studies can be created, and empirical evidence can be gathered to support the findings. As per the study and from the perspective of the public health-care system there is a need to develop an integrated implementation roadmap to design, manage, and use blockchain technology all through public hospitals and healthcare systems.
Several technologies, such as those mentioned above and the digital technology, can be applied to generate, collect, and access data in order to create a secure and decentralised public ledger for a blockchain that is helpful for public healthcare. Future research might be subjected to empirical investigations to assess the hurdles to BT adoption and its effects on the healthcare sector. Future research directions for blockchain in health-care include developing solutions to address scalability and interoperability, as well as exploring ways to ensure regulatory compliance. Additionally, research should focus on developing specific use cases for blockchain in healthcare, such as in the areas of supply chain management, clinical trials, and medical record keeping.
Acknowledgments
The authors are thankful to editors and anonymous reviewers for their valuable comments that improved the quality of the paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ajibade, F. O., Ajibade, T. F., Idowu, T. E., Nwogwu, N. A., Adelodun, B., Lasisi, K. H., Opafola, O. T., Ajala, O. A., Fadugba, O. G., & Adewumi, J. R. (2021). Flood-prone area mapping using GIS-based analytical hierarchy frameworks for Ibadan city, Nigeria. Journal of Multi-Criteria Decision Analysis, 28(5–6), 283–295. 10.1002/mcda.1759 [DOI] [Google Scholar]
- Alam, A., Rashid, I., & Raza, K. (2021). Application, functionality, and security issues of data mining techniques in healthcare informatics. In Khalid Raza & Nilanjan Dey (Eds.), Translational bioinformatics in healthcare and medicine (pp. 149–156). Elsevier. [Google Scholar]
- Ali, O., Jaradat, A., Kulakli, A., & Abuhalimeh, A. (2021). A comparative study: Blockchain technology utilization benefits, challenges and functionalities. Institute of Electrical and Electronics EngineersAccess, 9, 12730–12749. 10.1109/ACCESS.2021.3050241 [DOI] [Google Scholar]
- Alonso-Coello, P., Schünemann, H. J., Moberg, J., Brignardello-Petersen, R., Akl, E. A., Davoli, M., Treweek, S., Mustafa, R. A., Rada, G., Rosenbaum, S., Morelli, A., Guyatt, G. H., & Oxman, A. D. (2016). GRADE Evidence to Decision (EtD) frameworks: A systematic and transparent approach to making well informed healthcare choices. 1: Introduction. Bmj, 353, i2016. 10.1136/bmj.i2016 [DOI] [PubMed] [Google Scholar]
- Alzahrani, S., Daim, T., & Choo, K. -K.R. (2022). Assessment of the blockchain technology adoption for the management of the electronic health record systems. IEEE Transactions on Engineering Management. [Google Scholar]
- Amarakoon, P., Hewapathirana, R., & Dissanayake, V. H. W. (2021). mHealth in public health sector: Challenges and opportunities in low-and middle-income countries: A case study of Sri Lanka. In S. Syed-Abdul, Xinxin Zhu & L. Fernandez-Luque (Eds.), Digital health (pp. 123–142). Elsevier. [Google Scholar]
- Archibald, M. M., Radil, A. I., Zhang, X., & Hanson, W. E. (2015). Current mixed methods practices in qualitative research: A content analysis of leading journals. International Journal of Qualitative Methods, 14(2), 5–33. 10.1177/160940691501400205 [DOI] [Google Scholar]
- Arfi, W. B., Nasr, I. B., Kondrateva, G., & Hikkerova, L. (2021). The role of trust in intention to use the IoT in eHealth: Application of the modified UTAUT in a consumer context. Technological Forecasting and Social Change, 167, 120688. 10.1016/j.techfore.2021.120688 [DOI] [Google Scholar]
- Badhotiya, G. K., Sharma, V. P., Prakash, S., Kalluri, V., & Singh, R. (2021). Investigation and assessment of blockchain technology adoption in the pharmaceutical supply chain. Materials Today: Proceedings, 46, 10776–10780. [Google Scholar]
- Balasubramanian, S., Shukla, V., Sethi, J. S., Islam, N., & Saloum, R. (2021). A readiness assessment framework for Blockchain adoption: A healthcare case study. Technological Forecasting and Social Change, 165, 120536. 10.1016/j.techfore.2020.120536 [DOI] [Google Scholar]
- Bittins, S., Kober, G., Margheri, A., Masi, M., Miladi, A., & Sassone, V. (2021). Healthcare Data Management by Using Blockchain Technology. In: S. Namasudra, & G.C. Deka (Eds.), Applications of Blockchain in Healthcare (Vol. 83, pp. 1–27). Singapore: Springer. 10.1007/978-981-15-9547-9_1 [DOI] [Google Scholar]
- Blijleven, V., Jaspers, M., Wetzels, M., Koelemeijer, K., & Mehrsai, A. (2016). A meta-modeling technique for analyzing, designing and adapting healthcare processes: A process-deliverable perspective. 2016 IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI), NV, USA · United States, 316–319. [Google Scholar]
- Blijleven, V., Koelemeijer, K., & Jaspers, M. (2019). SEWA: A framework for sociotechnical analysis of electronic health record system workarounds. International Journal of Medical Informatics, 125, 71–78. 10.1016/j.ijmedinf.2019.02.012 [DOI] [PubMed] [Google Scholar]
- Brereton, P., Kitchenham, B. A., Budgen, D., Turner, M., & Khalil, M. (2007). Lessons from applying the systematic literature review process within the software engineering domain. The Journal of Systems and Software, 80(4), 571–583. 10.1016/j.jss.2006.07.009 [DOI] [Google Scholar]
- Bublitz, M., Oetomo, F., Sahu, A. S., Kuang, K., Fadrique, A. X., Velmovitsky, L. E., Nobrega, P. M., & Morita, P. (2019). Disruptive technologies for environment and health research: An overview of artificial intelligence, blockchain, and internet of things. International Journal of Environmental Research and Public Health, 16(20), 3847. 10.3390/ijerph16203847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciamani, G. E., Chu, T. N., Sanford, D. I., Abreu, A., Duddalwar, V., Oberai, A., Kuo, C. -C.J., Liu, X., Denniston, A. K., Vasey, B., McCulloch, P., Wolff, R. F., Mallett, S., Mongan, J., Kahn, C. E., Sounderajah, V., Darzi, A., Dahm, P., Moons, K. G. M. … Hung, A. J. (2023). PRISMA AI reporting guidelines for systematic reviews and meta-analyses on AI in healthcare. Nature Medicine, 29(1), 1–2. 10.1038/s41591-022-02139-w [DOI] [PubMed] [Google Scholar]
- Carson, J., Prescott, J., Allen, R., & McHugh, S. (2020). Winter is coming: Age and early psychological concomitants of the Covid-19 pandemic in England. Journal of Public Mental Health, 19(3), 221–230. [Google Scholar]
- Chaudhary, S., Kakkar, R., Jadav, N. K., Nair, A., Gupta, R., Tanwar, S., Agrawal, S., Alshehri, M. D., Sharma, R., Sharma, G., & Davidson, I. E. (2022). A taxonomy on smart healthcare technologies: Security framework, case study, and future directions. Journal of Sensors, 2022, 1–30. 10.1155/2022/1863838 [DOI] [Google Scholar]
- CHELLADURAI, M. U., Pandian, S., & Ramasamy, K. (2021). A blockchain based patient centric electronic health record storage and integrity management for e-Health systems. Health Policy and Technology, 10(4), 100513. 10.1016/j.hlpt.2021.100513 [DOI] [Google Scholar]
- Cheong, H. J., Shin, N. Y., & Joeng, Y. B. (2009). Improving Korean service delivery system in health care: Focusing on national E-health system. 2009 International Conference on EHealth, Telemedicine, and Social Medicine, 263–268. [Google Scholar]
- Clohessy, T., Acton, T., & Rogers, N. (2019). Blockchain Adoption: Technological, Organisational and Environmental Considerations. In: H. Treiblmaier, & R. Beck (Eds.), Business Transformation Through Blockchain. Palgrave Macmillan: Cham. 10.1007/978-3-319-98911-2_2 [DOI] [Google Scholar]
- Coorevits, P., Sundgren, M., Klein, G. O., Bahr, A., Claerhout, B., Daniel, C., Dugas, M., Dupont, D., Schmidt, A., & Singleton, P. (2013). Electronic health records: New opportunities for clinical research. Journal of Internal Medicine, 274(6), 547–560. 10.1111/joim.12119 [DOI] [PubMed] [Google Scholar]
- Costa, L. B. M., & Godinho Filho, M. (2016). Lean healthcare: Review, classification and analysis of literature. Production Planning\& Control, 27(10), 823–836. 10.1080/09537287.2016.1143131 [DOI] [Google Scholar]
- Coupet, S., Nicolas, G., Louder, C. N., & Meyer, M. (2021). When public health messages become stressful: Managing chronic disease during COVID-19. Social Sciences\& Humanities Open, 4(1), 100150. 10.1016/j.ssaho.2021.100150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cricelli, L., Famulari, F. M., Greco, M., & Grimaldi, M. (2020). Searching for the one: Customer relationship management software selection. Journal of Multi-Criteria Decision Analysis, 27(3–4), 173–188. 10.1002/mcda.1687 [DOI] [Google Scholar]
- Demiris, G. (2004). Electronic home healthcare: Concepts and challenges. International Journal of Electronic Healthcare, 1(1), 4–16. 10.1504/IJEH.2004.004655 [DOI] [PubMed] [Google Scholar]
- Drosatos, G., & Efraimidis, P. S. (2011). Privacy-preserving statistical analysis on ubiquitous health data. Proceedings Trust, Privacy and Security in Digital Business: 8th International Conference, TrustBus 2011, Toulouse France, August 29-September 2, 2011. 8, 24–36. [Google Scholar]
- Dutot, V., Bergeron, F., Rozhkova, K., & Moreau, N. (2018). Factors affecting the adoption of connected objects in e-health: A mixed methods approach. Systèmes d’information et Management, 23(4), 31–66. 10.3917/sim.184.0031 [DOI] [Google Scholar]
- Dwivedi, A. D., Malina, L., Dzurenda, P., & Srivastava, G. (2019, July). Optimized blockchain model for internet of things based healthcare applications. In 2019 42nd international conference on telecommunications and signal processing (TSP) (pp. 135–139). IEEE. [Google Scholar]
- Eri\cskin, L. (2021). Preference modelling in sorting problems: Multiple criteria decision aid and statistical learning perspectives. Journal of Multi-Criteria Decision Analysis, 28(5–6), 203–219. 10.1002/mcda.1737 [DOI] [Google Scholar]
- Esmaeilzadeh, P., & Mirzaei, T. (2019). The potential of blockchain technology for health information exchange: Experimental study from patients’ perspectives. Journal of Medical Internet Research, 21(6), e14184. 10.2196/14184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach, G. (2000). Consumer health informatics. Bmj, 320(7251), 1713–1716. 10.1136/bmj.320.7251.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang, H. S. A., Tan, T. H., Tan, Y. F. C., & Tan, C. J. M. (2021). Blockchain personal health records: Systematic review. Journal of Medical Internet Research, 23(4), e25094. 10.2196/25094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farouk, A., Alahmadi, A., Ghose, S., & Mashatan, A. (2020). Blockchain platform for industrial healthcare: Vision and future opportunities. Computer Communications, 154, 223–235. 10.1016/j.comcom.2020.02.058 [DOI] [Google Scholar]
- Gardas, B. B. (2022). Organizational hindrances to healthcare 4.0 adoption: An multi-criteria decision analysis framework. Journal of Multi-Criteria Decision Analysis, 29(1–2), 186–195. 10.1002/mcda.1766 [DOI] [Google Scholar]
- Gardas, B. B., Ghongade, N. P., & Jagtap, A. H. (2022). Application of multi-criteria decision-making approach in healthcare surgical management. Journal of Multi-Criteria Decision Analysis, 29(1–2), 92–109. 10.1002/mcda.1753 [DOI] [Google Scholar]
- Garrido, A., Lopez, L. J. R., & Álvarez, N. B. (2021). A simulation-based AHP approach to analyze the scalability of EHR systems using blockchain technology in healthcare institutions. Informatics in Medicine Unlocked, 24, 100576. 10.1016/j.imu.2021.100576 [DOI] [Google Scholar]
- Gauttam, P., Patel, N., Singh, B., Kaur, J., Chattu, V. K., & Jakovljevic, M. (2021). Public health policy of India and COVID-19: Diagnosis and prognosis of the combating response. Sustainability, 13(6), 3415. 10.3390/su13063415 [DOI] [Google Scholar]
- Gebayew, C., Hardini, I. R., Panjaitan, G. H. A., & Kurniawan, N. B., (2018). A systematic literature review on digital transformation. 2018 International Conference on Information Technology Systems and Innovation (ICITSI), 260–265. [Google Scholar]
- Gill, S. S. (2021). Quantum and blockchain based serverless edge computing: A vision, model, new trends and future directions. Internet Technology Letters, e275. 10.1002/itl2.275 [DOI] [Google Scholar]
- Golinelli, D., Boetto, E., Carullo, G., Nuzzolese, A. G., Landini, M. P., & Fantini, M. P. (2020). Adoption of digital technologies in health care during the COVID-19 pandemic: Systematic review of early scientific literature. Journal of Medical Internet Research, 22(11), e22280. 10.2196/22280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasselgren, A., Kralevska, K., Gligoroski, D., Pedersen, S. A., & Faxvaag, A. (2020). Blockchain in healthcare and health sciences—A scoping review. International Journal of Medical Informatics, 134, 104040. 10.1016/j.ijmedinf.2019.104040 [DOI] [PubMed] [Google Scholar]
- Hatef, E., Weiner, J. P., & Kharrazi, H. (2019). A public health perspective on using electronic health records to address social determinants of health: The potential for a national system of local community health records in the United States. International Journal of Medical Informatics, 124, 86–89. 10.1016/j.ijmedinf.2019.01.012 [DOI] [PubMed] [Google Scholar]
- Hemalatha, P. (2021). Monitoring and securing the healthcare data harnessing IOT and blockchain technology. Turkish Journal of Computer and Mathematics Education (TURCOMAT), 12(2), 2554–2561. 10.17762/turcomat.v12i2.2213 [DOI] [Google Scholar]
- Hosseini, A., Pourahmad, A., Ayashi, A., Tzeng, G. -H., Banaitis, A., & Pourahmad, A. (2021). Improving the urban heritage based on a tourism risk assessment using a hybrid fuzzy MADM method: The case study of Tehran’s central district. Journal of Multi-Criteria Decision Analysis, 28(5–6), 248–268. 10.1002/mcda.1746 [DOI] [Google Scholar]
- Hussey, P., & Kennedy, M. A. (2021). Health Informatics Standards. In P. Hussey & M. A. Kennedy (Eds.), Introduction to Nursing Informatics. Cham: Springer. 10.1007/978-3-030-58740-6_6 [DOI] [Google Scholar]
- Hussien, H. M., Yasin, S. M., Udzir, N. I., Ninggal, M. I. H., & Salman, S. (2021). Blockchain technology in the healthcare industry: Trends and opportunities. Journal of Industrial Information Integration, 22, 100217. 10.1016/j.jii.2021.100217 [DOI] [Google Scholar]
- Jeet, R., & Kang, S. S. (2020). Investigating the progress of human e-healthcare systems with understanding the necessity of using emerging blockchain technology. Materials Today: Proceedings. [Google Scholar]
- Joshi, S., (2013). E-supply chain collaboration and integration: implementation issues and challenges. In. E-logistics and e-supply chain management: Applications for evolving business. (pp. 9-26). IGI Global. DOI: 10.4018/978-1-4666-3914-0.ch002 [DOI] [Google Scholar]
- Joshi, S., Sharma, M., Das, R. P., Muduli, R., Narkhede, B. E., & Misra, A., (2022). Assessing effectiveness of humanitarian activities against COVID-19 disruption: the role of blockchain-enabled digital humanitarian network (BT-DHN). Sustainability, 14(3), 1904. 10.3390/su14031904 [DOI] [Google Scholar]
- Joshi, S., Singh, R. K., & Sharma, M. (2020). Sustainable agri-food supply chain practices: Few empirical evidences from a developing economy. Global Business Review, 0972150920907014. 10.1177/0972150920907014 [DOI] [Google Scholar]
- Joshi, S., & Sharma, M., (2022). Digital technologies (DT) adoption in agri-food supply chains amidst COVID-19: An approach towards food security concerns in developing countries. Journal of Global Operations and Strategic Sourcing, 15(2), 262–282. 10.1108/JGOSS-02-2021-0014 [DOI] [Google Scholar]
- Justvig, S. P., Haynes, L., Karpowicz, K., Unsworth, F., Petrosino, S., Peltz, A., Jones, B. L., Hickingbotham, M., Cox, J., & Wu, A. C. (2022). The role of social determinants of health in the use of telemedicine for asthma in children. The Journal of Allergy and Clinical Immunology in Practice, 10(10), 2543–2549. 10.1016/j.jaip.2022.07.005 [DOI] [PubMed] [Google Scholar]
- Kandakoglu, A., Frini, A., & Ben Amor, S. (2019). Multicriteria decision making for sustainable development: A systematic review. Journal of Multi-Criteria Decision Analysis, 26(5–6), 202–251. 10.1002/mcda.1682 [DOI] [Google Scholar]
- Kannan, G., Pokharel, S., & Kumar, P. S. (2009). A hybrid approach using ISM and fuzzy TOPSIS for the selection of reverse logistics provider. Resources Conservation and Recycling, 54(1), 28–36. 10.1016/j.resconrec.2009.06.004 [DOI] [Google Scholar]
- Katsimperis, V., & Andrikopoulos, A. (2021). Creating a flexible business credit rating model using multicriteria decision analysis. Journal of Multi-Criteria Decision Analysis, 28(1–2), 45–67. 10.1002/mcda.1726 [DOI] [Google Scholar]
- Kazimieras Zavadskas, E., Antucheviciene, J., & Chatterjee, P. (2018). Multiple-criteria decision-making (MCDM) techniques for business processes information management. Information, 10(1), 4. MDPI. [Google Scholar]
- Kitchenham, B., Brereton, O. P., Budgen, D., Turner, M., Bailey, J., & Linkman, S. (2009). Systematic literature reviews in software engineering–a systematic literature review. Information and Software Technology, 51(1), 7–15. 10.1016/j.infsof.2008.09.009 [DOI] [Google Scholar]
- Kohn, M. S., Topaloglu, U., Kirkendall, E. S., Dharod, A., Wells, B. J., & Gurcan, M. (2022). Creating learning health systems and the emerging role of biomedical informatics. Learning Health Systems, 6(1), e10259. 10.1002/lrh2.10259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korhonen, P., & Voutilainen, R. (2006). Finding the most preferred alliance structure between banks and insurance companies. European Journal of Operational Research, 175(2), 1285–1299. 10.1016/j.ejor.2005.04.046 [DOI] [Google Scholar]
- Kundakc\i, N. (2019). An integrated method using MACBETH and EDAS methods for evaluating steam boiler alternatives. Journal of Multi-Criteria Decision Analysis, 26(1–2), 27–34. 10.1002/mcda.1656 [DOI] [Google Scholar]
- Laganà, I. R., & Colapinto, C. (2022). Multiple criteria decision-making in healthcare and pharmaceutical supply chain management: A state-of-the-art review and implications for future research. Journal of Multi-Criteria Decision Analysis, 29(1–2), 122–134. 10.1002/mcda.1778 [DOI] [Google Scholar]
- Lak Kamari, M., Isvand, H., & Alhuyi Nazari, M. (2020). Applications of multi-criteria decision-making (MCDM) methods in renewable energy development: A review. Renewable Energy Research and Applications, 1(1), 47–54. [Google Scholar]
- Lee, D., & Yoon, S. N. (2021). Application of artificial intelligence-based technologies in the healthcare industry: Opportunities and challenges. International Journal of Environmental Research and Public Health, 18(1), 271. 10.3390/ijerph18010271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenert, L. A., Ding, W., & Jacobs, J. (2021). Informatics for public health and health system collaboration: Applications for the control of the current COVID-19 pandemic and the next one. Journal of the American Medical Informatics Association, 28(8), 1807–1811. 10.1093/jamia/ocab066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. -L. (2020). Establishing environment sustentation strategies for urban and rural/town tourism based on a hybrid MCDM approach. Current Issues in Tourism, 23(19), 2360–2395. 10.1080/13683500.2019.1642308 [DOI] [Google Scholar]
- Luthra, S., Sharma, M., Kumar, A., Joshi, S., Collins, E., & Mangla, S. (2022). Overcoming barriers to cross-sector collaboration in circular supply chain management: a multi-method approach. Transportation Research Part E: Logistics and Transportation Review, 157, 102–582.. 10.1016/j.tre.2021.102582 [DOI] [Google Scholar]
- Mailly, D., Abi-Zeid, I., & Pepin, S. (2014). A multi-criteria classification approach for identifying favourable climates for tourism. Journal of Multi-Criteria Decision Analysis, 21(1–2), 65–75. 10.1002/mcda.1507 [DOI] [Google Scholar]
- Malhotra, A., O’Neill, H., & Stowell, P. (2022). Thinking strategically about blockchain adoption and risk mitigation. Business Horizons, 65(2), 159–171. 10.1016/j.bushor.2021.02.033 [DOI] [Google Scholar]
- Manish Katiyar, D., & Singhal, S., (2021). Blockchain technology in management of clinical trials: A review of its applications, regulatory concerns and challenges. Materials Today: Proceedings, 47, 198–206. 10.1016/j.matpr.2021.04.095 [DOI] [Google Scholar]
- Meade, M. O., & Richardson, W. S. (1997). Selecting and appraising studies for a systematic review. Annals of Internal Medicine, 127(7), 531–537. 10.7326/0003-4819-127-7-199710010-00005 [DOI] [PubMed] [Google Scholar]
- Meline, T. (2006). Selecting studies for systemic review: Inclusion and exclusion criteria. Contemporary Issues in Communication Science and Disorders, 33(Spring), 21–27. 10.1044/cicsd_33_S_21 [DOI] [Google Scholar]
- Miller, J. W., Naimi, T. S., Brewer, R. D., & Jones, S. E. (2007). Binge drinking and associated health risk behaviors among high school students. Pediatrics, 119(1), 76–85. 10.1542/peds.2006-1517 [DOI] [PubMed] [Google Scholar]
- Mitchell, M., & Kan, L. (2019). Digital technology and the future of health systems. Health Systems\& Reform, 5(2), 113–120. 10.1080/23288604.2019.1583040 [DOI] [PubMed] [Google Scholar]
- Mohammad, A. -M., Chowdhury, T., Biswas, B., & Absar, N. (2018). Food poisoning and intoxication: A global leading concern for human health. In Alexandru Mihai Grumezescu & Alina Maria Holban (Eds.), Food safety and preservation (pp. 307–352). Elsevier. [Google Scholar]
- Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), 1–9. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira, A. C., & Silva, P. M. F. D. (2016). Complaint behaviour by third parties: Exploring service quality, customer satisfaction and word-of-mouth in health clubs. International Journal of Sport Management and Marketing, 16(3–6), 152–171. 10.1504/IJSMM.2016.077923 [DOI] [Google Scholar]
- Nasr, J., Nuce, M., Vasiliu-Feltes, I., Hurley, D., Fox, M., Sneha, S., Charles, W., Nasr, J., & Iyengar, R. (2021). Blockchain predictions for health care in 2021. Blockchain in Healthcare Today, 4. 10.30953/bhty.v4.162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okpala, C. O. R., Sardo, G., Vitale, S., Bono, G., & Arukwe, A. (2018). Hazardous properties and toxicological update of mercury: From fish food to human health safety perspective. Critical Reviews in Food Science and Nutrition, 58(12), 1986–2001. 10.1080/10408398.2017.1291491 [DOI] [PubMed] [Google Scholar]
- Onik, M. M. H., Aich, S., Yang, J., Kim, C. -S., & Kim, H. -C. (2019). Blockchain in healthcare: Challenges and solutions. In Nilanjan Dey, Himansu Das & Himansu Sekhar Behera (Eds.), Big data analytics for intelligent healthcare management (pp. 197–226). Elsevier. [Google Scholar]
- Osipov, V. S., & Skryl, T. V. (2021). Impact of digital technologies on the efficiency of healthcare delivery. In Gonçalo Marques, Akash Kumar Bhoi, C. Victor Hugo, de Albuquerque & K. S. Hareesha (Eds.), IoT in Healthcare and Ambient Assisted Living (pp. 243–261). Springer. [Google Scholar]
- Osipov, V. S., & Skryl, T. V. (2021). Impact of digital technologies on the efficiency of healthcare delivery. In IoT in Healthcare and Ambient Assisted Living (pp. 243–261). Singapore: Springer Singapore. [Google Scholar]
- Pérez, P. F. (2021). Health spending and hospitals in the world in a long-term perspective. In The emergence of modern hospital management and organisation in the world 1880s–1930s (Frontiers of Management History) (pp. 1–18). Bingley: Emerald Publishing Limited. 10.1108/978-1-78769-989-220211002 [DOI] [Google Scholar]
- Pollock, A., & Berge, E. (2018). How to do a systematic review. International Journal of Stroke, 13(2), 138–156. [DOI] [PubMed] [Google Scholar]
- Pradhan, V., & Bhattacharya, S. (2021). Benchmarking model for culture of urban traffic-safety management in India: Interpretive structural modeling framework. International Journal of Innovation Science, 13(1), 34–52. 10.1108/IJIS-09-2020-0168 [DOI] [Google Scholar]
- Pratt, R., Gyllstrom, B., Gearin, K., Lange, C., Hahn, D., Baldwin, L. M., & Zahner, S. (2018). Identifying barriers to collaboration between primary care and public health: Experiences at the local level. Public Health Reports, 133(3), 311–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protti, D. J. (2015). Missed connections: The adoption of information technology in Canadian healthcare. CD Howe Institute. [Google Scholar]
- Puri, V., Kataria, A., & Sharma, V. (2021). Artificial intelligence‐powered decentralized framework for Internet of Things in Healthcare 4.0. Transactions on Emerging Telecommunications Technologies, e4245. [Google Scholar]
- Purushotham, S., Meng, C., Che, Z., & Liu, Y. (2018). Benchmarking deep learning models on large healthcare datasets. Journal of Biomedical Informatics, 83, 112–134. 10.1016/j.jbi.2018.04.007 [DOI] [PubMed] [Google Scholar]
- Qarnain, S. S., Muthuvel, S., & Sankaranarayanan, B. (2021). Analysis of energy conservation factors in buildings using interpretive structural modeling methodology: An Indian perspective. Journal of the Institution of Engineers (India): Series A, 102, 43–61. 10.1007/s40030-020-00483-z [DOI] [Google Scholar]
- Queiroz, M. M., & Wamba, S. F. (2019). Blockchain adoption challenges in supply chain: An empirical investigation of the main drivers in India and the USA. International Journal of Information Management, 46, 70–82. 10.1016/j.ijinfomgt.2018.11.021 [DOI] [Google Scholar]
- Rai, R., El-Zaemey, S., Dorji, N., Rai, B. D., & Fritschi, L. (2021). Exposure to occupational hazards among health care workers in low-and middle-income countries: A scoping review. International Journal of Environmental Research and Public Health, 18(5), 2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall, D., Goel, P., & Abujamra, R. (2017). Blockchain applications and use cases in health information technology. Journal of Health\& Medical Informatics, 8(3), 1–17. 10.4172/2157-7420.1000276 [DOI] [Google Scholar]
- Rasmi, M., Alazzam, M. B., Alsmadi, M. K., Almarashdeh, I. A., Alkhasawneh, R. A., & Alsmadi, S. (2020). Healthcare professionals’ acceptance electronic health records system: Critical literature review (Jordan case study). International Journal of Healthcare Management, 13(sup1), 48–60. 10.1080/20479700.2017.1420609 [DOI] [Google Scholar]
- Rasmussen, A., Sabic, H., Saha, S., & Nielsen, I. E. (2023). Supplier selection for aerospace\& defense industry through MCDM methods. Cleaner Engineering and Technology, 12, 100590. 10.1016/j.clet.2022.100590 [DOI] [Google Scholar]
- Reegu, F. A., Al-Khateeb, M. O., Zogaan, W. A., Al-Mousa, M. R., Alam, S., & Al-Shourbaji, I. (2021). Blockchain-based framework for interoperable electronic health record. Annals of the Romanian Society for Cell Biology, 6486–6495. [Google Scholar]
- Reegu, F., Daud, S. M., & Alam, S. (2021). Interoperability challenges in healthcare blockchain system-A systematic review. Annals of the Romanian Society for Cell Biology, 15487–15499. http://annalsofrscb.ro/index.php/journal/article/view/5177 [Google Scholar]
- Rethlefsen, M. L., Kirtley, S., Waffenschmidt, S., Ayala, A. P., Moher, D., Page, M. J., & Koffel, J. B. (2021). PRISMA-S: An extension to the PRISMA statement for reporting literature searches in systematic reviews. Systematic Reviews, 10(1), 1–19. 10.1186/s13643-020-01542-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehrs, A., da Costa, C. A., & da Rosa Righi, R. (2017). OmniPHR: A distributed architecture model to integrate personal health records. Journal of Biomedical Informatics, 71, 70–81. 10.1016/j.jbi.2017.05.012 [DOI] [PubMed] [Google Scholar]
- Saxena, D., & Verma, J. K. (2020). Blockchain for public health: Technology, applications, and a case study. In Computational Intelligence and Its Applications in Healthcare (pp. 53–61). Academic Press. [Google Scholar]
- Schmidt, K., & Sandner, P. (2017). Solving challenges in developing countries with blockchain technology. Frankfurt School Blockchain Center Working Paper. Retrieved March, 2, 2018. [Google Scholar]
- Schuetz, S., & Venkatesh, V. (2020). Blockchain, adoption, and financial inclusion in India: Research opportunities. International Journal of Information Management, 52, 101936. 10.1016/j.ijinfomgt.2019.04.009 [DOI] [Google Scholar]
- Schulz, K. A., Gstrein, O. J., & Zwitter, A. J. (2020). Exploring the governance and implementation of sustainable development initiatives through blockchain technology. Futures, 122. 10.1016/j.futures.2020.102611 [DOI] [Google Scholar]
- Shahi, S. K., & Dia, M. (2019). Efficiency measurement of Ontario’s sawmills using bootstrap data envelopment analysis. Journal of Multi-Criteria Decision Analysis, 26(5–6), 272–295. 10.1002/mcda.1695 [DOI] [Google Scholar]
- Shahnazari, A., Rafiee, M., Rohani, A., Nagar, B. B., Ebrahiminik, M. A., & Aghkhani, M. H. (2020). Identification of effective factors to select energy recovery technologies from municipal solid waste using multi-criteria decision making (MCDM): A review of thermochemical technologies. Sustainable Energy Technologies and Assessments, 40, 100737. 10.1016/j.seta.2020.100737 [DOI] [Google Scholar]
- Sharma, M., & Joshi, S., (2021). Barriers to blockchain adoption in health-care industry: an Indian perspective. Journal of Global Operations and Strategic Sourcing, 14(1), 134–169. 10.1108/JGOSS-06-2020-0026 [DOI] [Google Scholar]
- Sharma, M., Gupta, M., & Joshi, S. (2020). Adoption barriers in engaging young consumers in the Omni-channel retailing. Young Consumers, 21(2), 193–210. 10.1108/YC-02-2019-0953 [DOI] [Google Scholar]
- Sharma, M., & Joshi, S. (2019). Brand sustainability among young consumers: An AHP-TOPSIS approach. Young Consumers, 20(4). 10.1108/YC-12-2018-0914 [DOI] [Google Scholar]
- Sharma, M., Kumar, A., Luthra, S., Joshi, S., & Upadhyay, A. (2022). The impact of environmental dynamism on low‐carbon practices and digital supply chain networks to enhance sustainable performance: An empirical analysis. Business Strategy and the Environment, 31(4), 1776–1788. 10.1002/bse.2983 [DOI] [Google Scholar]
- Sharma, M., Joshi, S., & Govindan, K. (2021). Issues and solutions of electronic waste urban mining for circular economy transition: An Indian context. Journal of Environmental Management, 290, 112–373.. 10.1016/j.jenvman.2021.112373 [DOI] [PubMed] [Google Scholar]
- Sharma, L., Olson, J., Guha, A., & McDougal, L. (2021). How blockchain will transform the healthcare ecosystem. Business Horizons, 64(5), 673–682. 10.1016/j.bushor.2021.02.019 [DOI] [Google Scholar]
- Shen, K. -Y., Hu, S. -K., & Tzeng, G. -H. (2017). Financial modeling and improvement planning for the life insurance industry by using a rough knowledge based hybrid MCDM model. Information Sciences, 375, 296–313. 10.1016/j.ins.2016.09.055 [DOI] [Google Scholar]
- Shuaib, M., Alam, S., Alam, M. S., & Nasir, M. S. (2021a). Compliance with HIPAA and GDPR in blockchain-based electronic health record. Materials Today: Proceedings. 10.1016/j.matpr.2021.03.059 [DOI] [Google Scholar]
- Shuaib, M., Alam, S., Alam, M. S., & Nasir, M. S. (2021b). Self-sovereign identity for healthcare using blockchain. Materials Today: Proceedings. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikandar, H., Abbas, A. F., Khan, N., & Qureshi, M. I. (2022). Digital technologies in healthcare: A systematic review and bibliometric analysis. International Journal of Online and Biomedical Engineering, 18(8), 34–48. 10.3991/ijoe.v18i08.31961 [DOI] [Google Scholar]
- Singh, R. K., Joshi, S., & Sharma, M. (2020). Modelling supply chain flexibility in the Indian personal hygiene industry: An ISM-Fuzzy MICMAC approach. Global Business Review, 0972150920923075. 10.1177/0972150920923075 [DOI] [Google Scholar]
- Siqueira, A., Da Conceição, A. F., & Rocha, V. (2021). Blockchains and self-sovereign identities applied to healthcare solutions: A systematic review. ArXiv Preprint ArXiv:2104.12298.
- Siyal, A. A., Junejo, A. Z., Zawish, M., Ahmed, K., Khalil, A., & Soursou, G. (2019). Applications of blockchain technology in medicine and healthcare: Challenges and future perspectives. Cryptography, 3(1), 3. 10.3390/cryptography3010003 [DOI] [Google Scholar]
- Tahan, M., Tsoutsanis, E., Muhammad, M., & Karim, Z. A. A. (2017). Performance-based health monitoring, diagnostics and prognostics for condition-based maintenance of gas turbines: A review. Applied Energy, 198, 122–144. 10.1016/j.apenergy.2017.04.048 [DOI] [Google Scholar]
- Tandon, A., Dhir, A., Islam, A. K. M. N., & Mäntymäki, M. (2020). Blockchain in healthcare: A systematic literature review, synthesizing framework and future research agenda. Computers in Industry, 122, 103290. 10.1016/j.compind.2020.103290 [DOI] [Google Scholar]
- Tanwar, S., Parekh, K., & Evans, R. (2020). Blockchain-based electronic healthcare record system for healthcare 4.0 applications. Journal of Information Security and Applications, 50, 102407. 10.1016/j.jisa.2019.102407 [DOI] [Google Scholar]
- Tharmalingam, S., Hagens, S., & Zelmer, J. (2016). The value of connected health information: Perceptions of electronic health record users in Canada. BMC Medical Informatics and Decision Making, 16(1), 1–9. 10.1186/s12911-016-0330-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toufaily, E., Zalan, T., & Dhaou, S. B. (2021). A framework of blockchain technology adoption: An investigation of challenges and expected value. Information\& Management, 58(3), 103444. 10.1016/j.im.2021.103444 [DOI] [Google Scholar]
- Tuisku, O., Pekkarinen, S., Hennala, L., & Melkas, H. (2019). “Robots do not replace a nurse with a beating heart” the publicity around a robotic innovation in elderly care. Information Technology\& People, 32(1), 47–67. 10.1108/ITP-06-2018-0277 [DOI] [Google Scholar]
- Vaismoradi, M., Turunen, H., & Bondas, T. (2013). Content material evaluation and thematic evaluation: Implications for conducting a qualitative descriptive research. Nurs Heal Sci, 15(3), 398–405. 10.1111/nhs.12048 [DOI] [PubMed] [Google Scholar]
- van Gemert-Pijnen, J. E. W. C., Nijland, N., van Limburg, M., Ossebaard, H. C., Kelders, S. M., Eysenbach, G., & Seydel, E. R. (2011). A holistic framework to improve the uptake and impact of eHealth technologies. Journal of Medical Internet Research, 13(4), e1672. 10.2196/jmir.1672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vatankhah, S., Darvishmotevali, M., Rahimi, R., Jamali, S. M., & Ale Ebrahim, N. (2023). MCDM in travel and tourism research since 1997: A bibliometric approach. International Journal of Contemporary Hospitality Management. 10.2139/ssrn.4324990 [DOI] [Google Scholar]
- Veinot, T. C., Mitchell, H., & Ancker, J. S. (2018). Good intentions are not enough: How informatics interventions can worsen inequality. Journal of the American Medical Informatics Association, 25(8), 1080–1088. 10.1093/jamia/ocy052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wamba, S. F., Queiroz, M. M., & Trinchera, L. (2020). Dynamics between blockchain adoption determinants and supply chain performance: An empirical investigation. International Journal of Production Economics, 229, 107791. 10.1016/j.ijpe.2020.107791 [DOI] [Google Scholar]
- Wang, Y., & Hajli, N. (2017). Exploring the path to big data analytics success in healthcare. Journal of Business Research, 70, 287–299. 10.1016/j.jbusres.2016.08.002 [DOI] [Google Scholar]
- Wanke, P., Azad, M. A. K., Tan, Y., & Pimenta, R. (2022). Financial performance drivers in BRICS healthcare companies: Locally estimated scatterplot smoothing partial utility functions. Journal of Multi-Criteria Decision Analysis, 29(1–2), 173–185. 10.1002/mcda.1761 [DOI] [Google Scholar]
- Warfield, J. N. (1974). Developing interconnection matrices in structural modeling. IEEE Transactions on Systems, Man, and Cybernetics, 1(1), 81–87. 10.1109/TSMC.1974.5408524 [DOI] [Google Scholar]
- Warkentin, M., & Orgeron, C. (2020). Using the security triad to assess blockchain technology in public sector applications. International Journal of Information Management, 52, 102090. 10.1016/j.ijinfomgt.2020.102090 [DOI] [Google Scholar]
- Wenzl, M. (2019). 2 new ways of delivering care for OECD health policy studies health in the 21st century putting data to work for stronger health systems: putting data to work for stronger health systems. OECD , Health in the 21st Century: Putting Data to Work for Stronger Health Systems, OECD Health Policy Studies. Paris: OECD Publishing. 10.1787/e3b23f8e-en [DOI] [Google Scholar]
- Yadegaridehkordi, E., Nilashi, M., Shuib, L., Asadi, S., & Ibrahim, O. (2019). Development of a SaaS adoption decision-making model using a new hybrid MCDM approach. International Journal of Information Technology\& Decision Making, 18(06), 1845–1874. 10.1142/S0219622019500366 [DOI] [Google Scholar]
- Yang, H., Zhang, S., Liu, R., Krall, A., Wang, Y., Ventura, M., & Deflitch, C. (2021). Epidemic informatics and control: A holistic approach from system informatics to epidemic response and risk management in public health. AI and Analytics for Public Health-Proceedings of the 2020 INFORMS International Conference on Service Science, 1–46. [Google Scholar]
- Yaqoob, I., Salah, K., Jayaraman, R., & Al-Hammadi, Y. (2021). Blockchain for healthcare data management: Opportunities, challenges, and future recommendations. Neural Computing & Applications, 34(14), 1–16. 10.1007/s00521-020-05519-w34305326 [DOI] [Google Scholar]
- Zarour, M., Alenezi, M., Ansari, M. T. J., Pandey, A. K., Ahmad, M., Agrawal, A., Kumar, R., & Khan, R. A. (2021). Ensuring data integrity of healthcare information in the era of digital health. Healthcare Technology Letters, 8(3), 66–77. 10.1049/htl2.12008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zavadskas, K., Turskis, Z., & Kildienė, S. (2014). State Of art surveys of overviews on MCDM/MADM methods. Journal of Technological and Economic Development, 20(1), 165–179. 10.3846/20294913.2014.892037 [DOI] [Google Scholar]
- Zopounidis, C., & Doumpos, M. (2002). Multi-criteria decision aid in financial decision making: Methodologies and literature review. Journal of Multi-Criteria Decision Analysis, 11(4–5), 167–186. 10.1002/mcda.333 [DOI] [Google Scholar]


