Abstract
Objectives
This study aims to compare the effectiveness of palpation-guided and ultrasound (US)-guided platelet-rich plasma (PRP) injections in patients with chronic lateral epicondylitis (LE).
Patients and methods
Between January 2021 and August 2021, a total of 60 patients (34 males, 26 females; mean age: 40.5±10.9 years; range, 22 to 64 years) diagnosed with chronic LE were included. The patients were randomly allocated to either the palpation-guided (n=30) or the US-guided injection group (n=30) before they received PRP injection. All patients were assessed using the Visual Analog Scale (VAS), Disabilities of the Arm, Shoulder and Hand (DASH) scale, and grip strength at baseline and at one, three, and six months after injection.
Results
Baseline sociodemographic and clinical variables were statistically similar between two groups (p>0.05). The VAS and DASH scores improved significantly after the injection at each control, as well as grip strength in both groups (p<0.001). No statistically significant difference was found between the groups regarding VAS and DASH scores, and grip strength at one, three, and six months post-injection (p>0.05). No significant complication related to the injection was observed in any of the groups.
Conclusion
This study demonstrates that both palpation-guided and US-guided PRP injection protocols can improve clinical symptoms and functional parameters of patients with chronic LE.
Keywords: Lateral epicondylitis, platelet-rich plasma, ultrasound.
Introduction
Lateral epicondylitis (LE) is a prevalent musculoskeletal disorder that can lead to chronic pain with a marked functional disability of the arm. It refers to a common painful condition with a prevalence of 1 to 3% that affects the common extensor origin of the forearm.[1] Conservative treatment includes non-steroidal anti-inflammatory drugs, physical therapy, extracorporeal shock wave therapy (ESWT), injections with corticosteroids, autologous blood or platelet-rich plasma (PRP) injections, while controversy exists regarding the most optimal approach for the treatment of chronic LE.[2]
To date, corticosteroid use is not supported in the evidence both for the short and long term, since LE is defined as tendinosis, not tendinitis.[2-5] The PRP is an autologous preparation of peripheral blood which is filtered to obtain a fraction of plasma including high concentrations of platelets. Recently, PRP therapy has become more prevalent in the treatment of LE.[6-8] Application of PRP intratendinously can potentially stimulate the repair mechanisms by delivering several growth factors and cytokines and promotes angiogenesis and tendon healing.[9-11]
Ultrasound (US) is an important, reliable, non-invasive, and inexpensive imaging tool for pain management. However, local injections for pain relief are often performed palpation-guided using surface anatomic landmarks in daily clinical practice.[12] Previous studies have compared the efficacy of US-guided versus palpation or andmark-guided injections for the treatment of joint pathologies.[13,14] The current consensus on a treatment algorithm regarding the efficacy of individual approaches of US-guided injections for LE is obscure in the literature. It is well documented that the utilization of US reduces the risk for damaging the surrounding vulnerable structures such as tendons and vessels, and provides a real-time image of focal inflammation. Therefore, image-guided injections are recommended to improve the accuracy of the intervention.[15]
Overall, the literature is insufficient to show the superiority of US-guided injection over palpationguided injection in the management of chronic LE. In the present study, we aimed to compare the efficacy of direct approach versus US-guided PRP injection in patients with chronic LE.
Patients and Methods
This single-center, prospective, randomized study was conducted at Erzurum Regional Training and Research Hospital, Department of Physical Medicine and Rehabilitation between January 2021 and August 2021. A total of 60 patients (34 males, 26 females; mean age: 40.5±10.9 years; range, 22 to 64 years) who were recently diagnosed with chronic LE (symptoms lasting at least three months or longer) and those referred from outpatient clinics were included. The diagnosis of LE was based on painful local palpation at the humeral epicondyle and positive Cozen’s and middle finger’s tests. All patients underwent US to confirm the diagnosis of LE and one patient was screened with magnetic resonance imaging (MRI) to exclude differential diagnosis before the initiation of the study. Inclusion criteria were as follows: age between 18 and 80 years, diagnosed clinically as chronic LE with a symptom duration of ≥3 months. Exclusion criteria were as follows: glucocorticoid injection, physical therapy or ESWT therapy within the past three months, previous elbow surgery, inflammatory diseases such as rheumatoid arthritis or psoriatic arthritis, neck pain, shoulder pain on the ipsilateral side, radiculopathy, pregnancy, infection at the injection site, use of any agents affecting platelet activation.
The diagnosis was confirmed by a physician who also performed the inclusion, randomization, and treatment procedures. Another blind physician was responsible for outcome evaluations at one, three, and six months. The patients were randomly assigned by a computer-generated randomization program into two groups including the palpation-guided (n=30) and US-guided injection (n=30) group.
Medications except for paracetamol or any other complementary treatments were not allowed, until the final evaluation. All patients been prescribed an application of an ice pack for the first week after injection and a wrist splint. Paracetamol 500 mg was allowed for pain three times a day in all groups. The total amount of paracetamol intake of all patients was questioned at each follow-up. A standard home-based exercise program including wrist and elbow stretching, ball squeeze, wrist extension/flexion strengthening, wrist supination/pronation strengthening was prescribed to all patients. Phone calls were made every two weeks to inform about the necessity of splinting and exercise programs.
Injection techniques
The PRP was obtained by withdrawing 16 mL peripheral blood directly from the patients. I-stem cell® PRP kit (Biostems, South Korea) was used for both groups. A needle of 21-gauge was used, while the syringe contained an anticoagulant to chelate calcium, block the coagulation, and preserve the growth factors. The blood was submitted for a centrifuge process for 6 to 7 min, at 3,000 rpm in fixed-angle centrifuges and 3,400 rpm in swing-rotor centrifuges. Afterward, the blood was separated into red blood cells and plasma. The buffy coat layer above the red blood cells was first taken using the tornado technique with the tip of a 50-mm needle. The outcome of this process was 2 to 3 mL PRP.
In palpation-guided injection technique, the elbow of the patient was flexed to 90° with the forearm in pronation and the radial head on lateral epicondyle was palpated. A single skin entry was made with a 22-gauge needle. The needle was inserted to the most painful and sensitive point localized by palpation on the lateral aspect of the elbow just distal and anterior to the lateral epicondyle. The injection was performed from this point of maximum tenderness towards the humeroradial joint. Pricks were made by moving the needle back and forth around the area of common extensor tendon without emerging from the skin. The area was peppered with these small injections, while PRP solution was injected slowly.
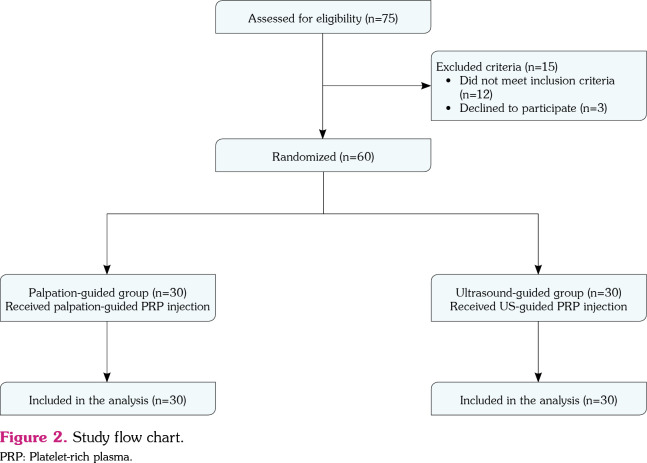
The US-guided injection technique was performed with the elbow bent to 90° and the patients were placed for injection in a seated position facing the physician. The US probe was positioned perpendicular to the common tendon origin to guide all the injections longitudinally. Ultrasound revealed hypoechoic areas and/or loss of normal fibrillar pattern characteristic of tendinopathy in the common extensor tendon. A single skin portal was made immediately distal and anterior to the lateral epicondyle into the common extensor tendon with a 22-gauge needle. The physician was able to follow the route of the needle and PRP was distributed to the pathologic areas of the common extensor tendon identified with US (Figure 1). The US-guided injections were performed using a MyLab60 model US device (Esaote S.p.A., Genova, Italy) with a high resolution and a 7- to 12-MHz linear probe.
Figure 1. (a) Longitudinal ultrasonographic image of the common extensor tendon (*), radial head (RH) and lateral epicondyle (LE). (b) A hypoechoic focus (arrow) compatible with tendinopathy.
Both injection techniques were performed by the same experienced physician with an aseptic procedure. All patients were advised to avoid heavy activities and give rest for the upper limb for three days.
Outcome measures
Evaluations for pain, symptom severity, and functional status were performed at baseline and one, three, and six months after injection. The intensity for pain was determined with Visual Analog Scale (VAS) (the numeric 0-10 ranking), and functionality was evaluated with Disabilities of the Arm, Shoulder and Hand (DASH). The DASH questionnaire including 30 items was used to assess the ability of a patient to fulfill several daily activities of the upper extremity. The patients graded difficulty in daily activities on a Likert scale of 5 points.[16] A dynamometer was used to evaluate grip strength in all patients at each follow-up. Patient discomfort related to the injection was evaluated within one week after local injection in both groups.
Statistical analysis
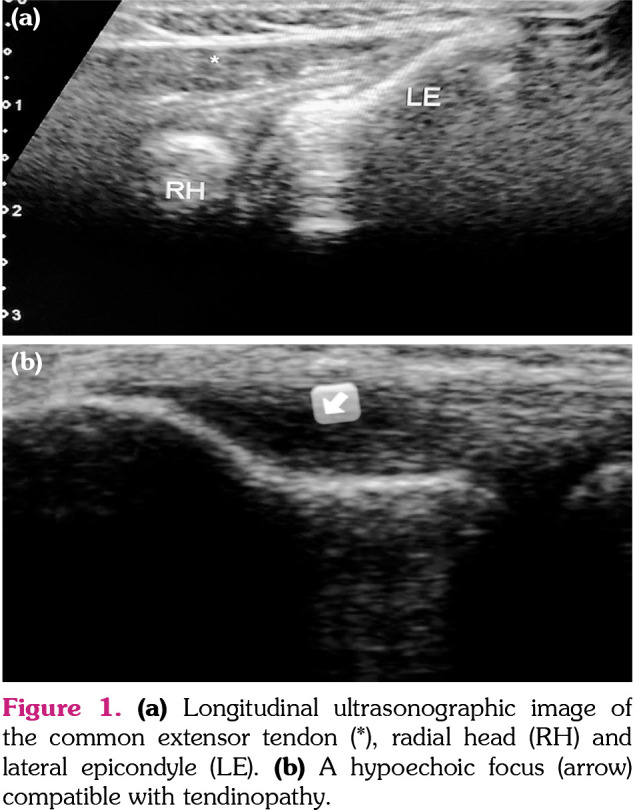
The power of the study was calculated using the NCSS PASS 2000 software (NCSS LLC, Kaysville, Utah, USA) to identify the minimum number of patients to be included in our study population. A 30% change in DASH was used to determine the sample size with a 5% margin of error and a confidence level of 95% (α=0.05). A sample size of 25 patients per group was required to achieve a statistical and clinical difference between the two groups. Envisaging that some of the participants could leave the study within six months, a total of 75 patients were assessed for eligibility and 60 of them were included in the study. All participants, 30 patients per group, completed the study. Figure 2 represents the flowchart of the study.
Figure 2. Study flow chart. PRP: Platelet-rich plasma.
Statistical analysis was performed using the IBM SPSS version 22.0 software (IBM Corp., Armonk, NY, USA). The normal distribution fitness of the variables was evaluated using the Shapiro-Wilk test. Descriptive data were presented in mean ± standard deviation (SD), median (min-max) or number and frequency. The Student t-test was used to compare parameters between the two groups. Analysis of variance (ANOVA) was used for repeated measures and the Bonferroni test to determine the time interval representing the source of differences. The Friedman test was used in evaluating parameters without normal distribution in the repeated measures, and the Wilcoxon signed-rank test was used to determine the time interval representing the source of differences. The chi-square (χ2) test, continuity (Yates) correction, and the Fisher exact test were used in the analysis of qualitative data. A p value of <0.05 was considered statistically significant.
Results
Both groups were similar in terms of age, sex, symptom/function scores, and symptom duration, and grip strength at the baseline. The sociodemographic characteristics of the patients are shown in Table 1. The mean VAS score before injection was 7.2±1.81 in the palpation-guided group and 7.3±1.5 in the US-guided group. The mean value of DASH before administration of PRP was 67.50±6.84 in the palpation-guided group and 69.70±6.25 in the US-guided group. The mean grip strength was 17.8±3.1 kg in the palpation group and 17.6±3.2 kg in the US-guided group. The changes in these clinical parameters at different follow-up visits are given in Table 2. Both groups exhibited a significant improvement in VAS, DASH scores, and grip strength at each control (p<0.001). No statistically significant difference was observed between the groups in terms of the VAS, DASH scores, and grip strength at one, three, and six months after the injection (p>0.05).
Table 1. Comparison of demographic and clinical data between groups.
| Palpation-guided group (n=30) | US-guided group (n=30) | p | |||||
| n | % | Mean±SD | n | % | Mean±SD | ||
| Age (year) | 41.8±10.7 | 39.2±11.3 | 0.36 | ||||
| Sex | |||||||
| Female | 12 | 40.0 | 14 | 46.7 | 0.31 | ||
| Male | 18 | 60.0 | 16 | 53.3 | 0.29 | ||
| BMI (kg/m2) | 26.2±1.4 | 27.4±2.2 | 0.34 | ||||
| Affected site | |||||||
| Dominant | 23 | 76.7 | 24 | 80 | 0.55 | ||
| Non-dominant | 7 | 23.3 | 6 | 20 | 0.45 | ||
| Symptom duration (month) | 6.4±2.2 | 6.1±2.1 | 0.72 | ||||
| Work-related risk factors | 8 | 26.6 | 6 | 20 | 0.27 | ||
| Usage of paracetamol during last six months | 28.1±6.8 | 27.6±10.7 | 0.82 | ||||
| SD: Standard deviation; BMI: Body mass index. | |||||||
Table 2. Intra-group and inter-group analysis of VAS, DASH scores, and grip strength.
| Palpation- guided group | US-guided group | p | |
| Mean±SD | Mean±SD | ||
| Visual Analog Scale | |||
| Baseline | 7.2±1.8 | 7.3±1.5 | 0.81 |
| 1st month | 6.3±0.8 | 6.0±0.8 | 0.06 |
| 3rd month | 2.8±1.9 | 2.1±1.25 | 0.09 |
| 6th month | 2.3±0.7 | 1.9±1.2 | 0.07 |
| p | <0.001 | <0.001 | |
| Disabilities of the arm, shoulder and hand | |||
| Baseline | 67.5±6.8 | 69.70±6.25 | 0.19 |
| 1st month | 45.7±16.4 | 46.15±19.82 | 0.92 |
| 3rd month | 30.0±16.0 | 27.81±9.16 | 0.25 |
| 6th month | 24.0±10.3 | 19.91±11.64 | 0.15 |
| p | <0.001 | <0.001 | |
| Grip strength | |||
| Baseline | 17.8±3.1 | 17.6±3.2 | 0.80 |
| 1st month | 20.2±2.9 | 21.5±1.9 | 0.76 |
| 3rd month | 36.7±3.1 | 37.5±3.5 | 0.35 |
| 6th month | 41.8±1.6 | 42.4±2.3 | 0.24 |
| p | <0.001 | <0.001 | |
| SD: Standard deviation. | |||
No significant complication related to the injection was observed in any of the groups. Swelling occurred in one patient in the palpationguided group at the first week after injection.
Discussion
Recently, minimally invasive treatment options that stimulate cellular proliferation and collagen production, and heal the degenerative structural changes in LE have been investigated.[17,18] One of these emerging interventions is PRP that has been gaining popularity for the treatment of LE due to its safety and simplicity. Animal studies have revealed that PRP helps the formation of active tenocytes that maintain a high proliferation rate, stimulates angiogenesis, and increases blood flow with vascular endothelial growth factors.[19] As a treatment option for initiating a healing response, PRP injection is considered in most cases of chronic LE, and some randomizedcontrolled trials have documented treatment efficacy.[17,20] Mishra et al.[8] explored PRP therapy for patients with LE that failed conventional therapy. A total of 54.0% of PRP-injected patients reported significant pain reduction at 24 weeks, compared to 29.1% in the control group.
Historically, most therapeutic periarticular and intra-articular injections have been performed without live imaging techniques for the elbow area. In theory, US guidance of a local injection can provide exact localization of the tissue target and real-time visualization of the needle during injection. Some studies on joint disorders have examined the additional benefits of US-guided injections, although larger, higher-quality evidence is needed.[21] A review has demonstrated that US-guided injections improve accuracy, efficacy, and cost-effectiveness compared with anatomic landmark-guided injections for large joints such as knees and shoulder.[22]
A limited number of studies have compared US-guided versus palpation-guided injection around the elbow, and all investigated intra-articular approaches.[23,24] High-level evidence is needed to help guide management in the elbow area. There is only one study conducted to compare the efficacy of US-guided and palpation-guided PRP injection. Mcmillan et al.[25] recruited 45 patients with chronic LE, all patients underwent PRP injection, and patients were observed for three months. They reported that the use of US guidance could not appear to improve treatment outcomes compared to blind injection in line with our results. In this single-center, prospective cohort study, the mean DASH score was increased from 45.5 to 31.2 in the US-guided injection group, while the blind injection group had a mean improvement in DASH from 44.4 to 27.7 at the end of three months. No complication due to injection was determined. In another study, Connell et al.[26] showed 60% improvement at eight weeks, 81% improvement at six months compared to their baseline after PRP injection. Similarly, significant recovery was observed in terms of clinical outcomes in both groups at each control in our study.
Due to technical advances in high resolution sonography, clinicians have begun to guide therapeutic injections by US in appropriately selected patients. The proper needle placement into the pathological region is important for the therapeutic effect of the procedure. However, the main finding of this present study was that US-guided PRP injection resulted in similar clinical improvement up to three to six months, compared to palpation-guided PRP injection in chronic LE. Previously, the severity of tendinopathy has been classified into four grades. The diameter of hypoechoic regions is up to 2 mm, 2 to 5 mm, and larger than 5 mm in Grade 2, 3 and 4, respectively. We believe that palpation-guided injection makes it possible to approach the affected portions of common extensor tendon.[27]
As a limitation, this study was lack of a completely untreated control group due to ethical concerns that made it difficult to determine the efficacy of PRP injections in isolation. Despite these limitations, the injection groups were similar regarding all sociodemographic characteristics and clinical parameters before treatment. Before the initiation of this study, a power analysis was performed to achieve the required number of patients throughout the study and to obtain significant results in correlation analyses between data that increased the power of this study. The inclusion of an objective method of evaluation in the form of handgrip strength evaluation also increased the strength of our study. Additionally, patient evaluations and injection procedures were performed by two different physicians under equivalent circumstances for each patient and frequent assessments were carried out at one, three, and six months after the injection.
The guidance of US has advantages of safety, low cost, convenience, and accuracy. Given the success of injection often depends on placing the needle within the intended target, US provides the adequate medication to the target site during the injection procedure and can also avoid accidental injury to surrounding structures. However, US guidance does not seem to be superior than direct approach, while performing PRP injection for LE. We encourage further randomized clinical studies on this topic with longer follow-up periods, particularly emphasizing the best technique of PRP injection, number, and frequency of injections, and standardization of the platelet ratio of PRP.
In conclusion, both palpation-guided and US-guided PRP injections were similarly effective in reducing the pain and symptoms and improving the function in the treatment of LE. Further studies with a large series of patients, as well as longer follow-up are necessary to make more reliable conclusions.
Acknowledgments.
We thank Dr. Kaan Alişar for his expertise and assistance at the Ultrasound unit.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Author Contributions: Conceived and designed the study: G.S., D.Ç.A.; Collected the data: G.S., D.Ç.A.; Data analysis and interpretation: G.S., D.Ç.A.; Prepared the manuscript and reviewed the literature: G.S.; All authors have read the manuscript and agreed to the conclusion.
Financial Disclosure: This study was supported by Intraline Co. Ltd.
References
- 1.Sanders TL Jr, Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: A population-based study. Am J Sports Med. 2015;43:1066–1071. doi: 10.1177/0363546514568087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai WC, Erickson BJ, Mlynarek RA, Wang D. Chronic lateral epicondylitis: Challenges and solutions. Open Access J Sports Med. 2018;9:243–251. doi: 10.2147/OAJSM.S160974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu Q, Chen J, Cheng L. Comparison of platelet rich plasma and corticosteroids in the management of lateral epicondylitis: A meta-analysis of randomized controlled trials. Int J Surg. 2019;67:37–46. doi: 10.1016/j.ijsu.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Bateman M, Titchener AG, Clark DI, Tambe AA. Management of tennis elbow: A survey of UK clinical practice. Shoulder Elbow. 2019;11:233–238. doi: 10.1177/1758573217738199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mi B, Liu G, Zhou W, Lv H, Liu Y, Wu Q, et al. Platelet rich plasma versus steroid on lateral epicondylitis: Meta-analysis of randomized clinical trials. Phys Sportsmed. 2017;45:97–104. doi: 10.1080/00913847.2017.1297670. [DOI] [PubMed] [Google Scholar]
- 6.Mlynarek RA, Kuhn AW, Bedi A. Platelet-Rich Plasma (PRP) in orthopedic sports medicine. Am J Orthop (Belle Mead NJ) 2016;45:290–326. [PubMed] [Google Scholar]
- 7.Tarpada SP, Morris MT, Lian J, Rashidi S. Current advances in the treatment of medial and lateral epicondylitis. J Orthop. 2018;15:107–110. doi: 10.1016/j.jor.2018.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mishra AK, Skrepnik NV, Edwards SG, Jones GL, Sampson S, Vermillion DA, et al. Efficacy of plateletrich plasma for chronic tennis elbow: A double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med. 2014;42:463–471. doi: 10.1177/0363546513494359. [DOI] [PubMed] [Google Scholar]
- 9.Borzini P, Mazzucco L. Tissue regeneration and in loco administration of platelet derivatives: Clinical outcome, heterogeneous products, and heterogeneity of the effector mechanisms. Transfusion. 2005;45:1759–1767. doi: 10.1111/j.1537-2995.2005.00600.x. [DOI] [PubMed] [Google Scholar]
- 10.de Mos M, van der Windt AE, Jahr H, van Schie HT, Weinans H, Verhaar JA, et al. Can platelet-rich plasma enhance tendon repair. A cell culture study. Am J Sports Med. 2008;36:1171–1178. doi: 10.1177/0363546508314430. [DOI] [PubMed] [Google Scholar]
- 11.Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from plateletrich plasma: Implications for wound healing. Plast Reconstr Surg. 2004;114:1502–1508. doi: 10.1097/01.prs.0000138251.07040.51. [DOI] [PubMed] [Google Scholar]
- 12.Bloom JE, Rischin A, Johnston RV, Buchbinder R. Image-guided versus blind glucocorticoid injection for shoulder pain. CD009147Cochrane Database Syst Rev. 2012;(8) doi: 10.1002/14651858.CD009147.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Dogu B, Yucel SD, Sag SY, Bankaoglu M, Kuran B. Blind or ultrasound-guided corticosteroid injections and short-term response in subacromial impingement syndrome: A randomized, double-blind, prospective study. Am J Phys Med Rehabil. 2012;91:658–665. doi: 10.1097/PHM.0b013e318255978a. [DOI] [PubMed] [Google Scholar]
- 14.Rutten MJ, Maresch BJ, Jager GJ, de Waal Malefijt MC. Injection of the subacromial-subdeltoid bursa: Blind or ultrasound-guided. Acta Orthop. 2007;78:254–257. doi: 10.1080/17453670710013762. [DOI] [PubMed] [Google Scholar]
- 15.Jacobson JA. Ultrasound in sports medicine. Radiol Clin North Am. 2002;40:363–386. doi: 10.1016/s0033-8389(02)00005-2. [DOI] [PubMed] [Google Scholar]
- 16.Beaton DE, Davis AM, Hudak PL, McConnell S. DASH (disabilities of the arm, shoulder and hand) outcome measure: What do we know about it now. British Journal of Hand Therapy. 2001;6:109–118. [Google Scholar]
- 17.Brkljac M, Conville J, Sonar U, Kumar S. Long-term follow-up of platelet-rich plasma injections for refractory lateral epicondylitis. J Orthop. 2019;16:496–499. doi: 10.1016/j.jor.2019.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khattab EM, Abowarda MH. Role of ultrasound guided Platelet-Rich Plasma (PRP) injection in treatment of lateral epicondylitis. The Egyptian Journal of Radiology and Nuclear Medicine. 2017;48:403–413. [Google Scholar]
- 19.Chaudhury S, de La Lama M, Adler RS, Gulotta LV, Skonieczki B, Chang A, et al. Platelet-rich plasma for the treatment of lateral epicondylitis: Sonographic assessment of tendon morphology and vascularity (pilot study) Skeletal Radiol. 2013;42:91–97. doi: 10.1007/s00256-012-1518-y. [DOI] [PubMed] [Google Scholar]
- 20.Shergill R, Choudur HN. Ultrasound-guided interventions in lateral epicondylitis. e27-e34J Clin Rheumatol. 2019;25 doi: 10.1097/RHU.0000000000000879. [DOI] [PubMed] [Google Scholar]
- 21.Sussman WI, Williams CJ, Mautner K. Ultrasoundguided elbow procedures. Phys Med Rehabil Clin N Am. 2016;27:573–587. doi: 10.1016/j.pmr.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Finnoff JT, Hall MM, Adams E, Berkoff D, Concoff AL, Dexter W, et al. American Medical Society for Sports Medicine (AMSSM) position statement: Interventional musculoskeletal ultrasound in sports medicine. PM R. 2015;7:151–168. doi: 10.1016/j.pmrj.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Cunnington J, Marshall N, Hide G, Bracewell C, Isaacs J, Platt P, et al. A randomized, double-blind, controlled study of ultrasound-guided corticosteroid injection into the joint of patients with inflammatory arthritis. Arthritis Rheum. 2010;62:1862–1869. doi: 10.1002/art.27448. [DOI] [PubMed] [Google Scholar]
- 24.Kim TK, Lee JH, Park KD, Lee SC, Ahn J, Park Y. Ultrasound versus palpation guidance for intraarticular injections in patients with degenerative osteoarthritis of the elbow. J Clin Ultrasound. 2013;41:479–485. doi: 10.1002/jcu.22071. [DOI] [PubMed] [Google Scholar]
- 25.Mcmillan T, Neilly D, Gardner T, Cairns D, Kumar K, Barker S. Ultrasound guidance does not improve short-term outcomes of lateral epicondylitis treated with platelet-rich plasma injections. Orthopaedic Proceedings. 2018;98-B(Supp 18):1–5. [Google Scholar]
- 26.Connell DA, Ali KE, Ahmad M, Lambert S, Corbett S, Curtis M. Ultrasound-guided autologous blood injection for tennis elbow. Skeletal Radiol. 2006;35:371–377. doi: 10.1007/s00256-006-0081-9. [DOI] [PubMed] [Google Scholar]
- 27.Allen GM, Wilson DJ. Ultrasound in sports medicine- -a critical evaluation. Eur J Radiol. 2007;62:79–85. doi: 10.1016/j.ejrad.2007.01.029. [DOI] [PubMed] [Google Scholar]