@jamieseanbenson; @stasamato; @gary_an
Between 2005 and 2020, the U.S. gained 31% more Level I/II trauma centers. Yet, @UVMLarnerMed researchers estimate that resulted in only a 6.9% increase in access to this essential care. Further, this access may not be distributed equitably across the nation.
KEY WORDS: Trauma center, GIS, county level, access to care, social determinants of health
BACKGROUND
Timely access to high-level (I/II) trauma centers (HLTCs) is essential to minimize mortality after injury. Over the last 15 years, there has been a proliferation of HLTC nationally. The current study evaluates the impact of additional HLTC on population access and injury mortality.
METHODS
A geocoded list of HLTC, with year designated, was obtained from the American Trauma Society, and 60-minute travel time polygons were created using OpenStreetMap data. Census block group population centroids, county population centroids, and American Communities Survey data from 2005 and 2020 were integrated. Age-adjusted nonoverdose injury mortality was obtained from CDC Wide-ranging Online Data for Epidemiologic Research and the Robert Wood Johnson Foundation. Geographically weighted regression models were used to identify independent predictors of HLTC access and injury mortality.
RESULTS
Over the 15-year (2005–2020) study period, the number of HLTC increased by 31.0% (445 to 583), while population access to HLTC increased by 6.9% (77.5–84.4%). Despite this increase, access was unchanged in 83.1% of counties, with a median change in access of 0.0% (interquartile range, 0.0–1.1%). Population-level age-adjusted injury mortality rates increased by 5.39 per 100,000 population during this time (60.72 to 66.11 per 100,000). Geographically weighted regression controlling for population demography and health indicators found higher median income and higher population density to be positively associated with majority (≥50%) HLTC population coverage and negatively associated with county-level nonoverdose mortality.
CONCLUSION
Over the past 15 years, the number of HLTC increased 31%, while population access to HLTC increased only 6.9%. High-level (I/II) trauma center designation is likely driven by factors other than population need. To optimize efficiency and decrease potential oversupply, the designation process should include population level metrics. Geographic information system methodology can be an effective tool to assess optimal placement.
LEVEL OF EVIDENCE
Prognostic and Epidemiological; Level IV.

Appropriate and timely access to care after injury improves survival and functional outcomes. Among the severely injured, best outcomes are achieved when definitive care is provided at high-level (level I/II) trauma centers (HLTCs) that are designated by state and/or verified by the American College of Surgeons Committee on Trauma (ACS-COT).1–3 For the benefits of definitive care at HLTC to accrue at the population level, there needs to be population level access to HLTC care as demonstrated in studies evaluating outcomes within organized state and regional trauma systems.4–6
Over the past 15 years, there has been a rapid increase in the number of designated/verified HLTC in the United States.7,8 However, there is paucity of research on how this increase impacts population level access to care and injury related mortality. The current study uses geographic information systems (GIS) to address this gap in knowledge and aims at (1) evaluating changes in population level access to HLTC care over time and (2) determining the impact of timely access to HLTC care on injury mortality. In addition, the study evaluates demographic and socioeconomic factors associated with HLTC access and injury mortality.
PATIENTS AND METHODS
Study Design
Cross-sectional study that uses GIS to determine county-level timely (≤60 minutes) access to HLTC and how the access has changed over the study period (2005–2020). Geographically weighted regression (GWR) was used to associate county level access and injury-related mortality and to identify demographic and socioeconomic factors associated with access to HLTC. Institutional review board approval was obtained for this study (study ID, CHRMS 17-0467). Reporting of this work adheres to Strengthening the Reporting of Observational Studies in Epidemiology guidelines (Supplemental Digital Content, Supplementary Data 1, http://links.lww.com/TA/C905).
Data Sources
Census block groups were used as the unit of analysis for calculating access. Block group access was then summarized up to the county level for analyses. The GIS and GWR models were created with data on current (2020) US hospitals, including geocoordinates, trauma center designation, and bed capacity obtained from the Trauma Information Exchange Program, which were cross-referenced with State Health Department websites for accuracy.9 In case of discrepancy, the highest level of designation/verification was assigned to the facility. Historic (2005 and 2012) trauma center designation and geolocation data were obtained from the Penn Injury Science Center.10 Trauma center data were obtained for the years 2005, 2012, and 2020, covering roughly even intervals during the study period. Helicopter and aeromedical emergency medical services (HEMS) station locations were obtained from the Department of Homeland Security.11 In addition, a geocoded set of air rescue stations run by the US Coast Guard was obtained from Jarman.12
Census county and block group demographics were obtained from the 2005–2009, 2011–2015, and 2016–2020 American Communities Surveys and temporally matched to county and block group population centroids obtained from the US Census Bureau (based on 2000, 2010, and 2020 decennial census data).13,14 Census block groups were used to calculate access, as they are the smallest geographic unit for which detailed demographic information is available, typically containing 600 to 3,000 persons. Counties and statistical equivalents (henceforth all referred to as counties) were used to associate variation among their contained block groups to population health outcomes, as they are static across intercensal years and have detailed data available from a variety of sources. Injury mortality rates by bridged race category and year for all US counties were obtained from the CDC Wide-ranging ONline Data for Epidemiologic Research (WONDER).15 Additional detailed county-level demographic data were obtained from the Robert Wood Johnson Foundation County Health Rankings data set.16
Coverage and Access Time Estimates
OpenStreetMap and the OpenRouteService were used to calculate 60-minute emergency medical services (EMS) ground transport isochrones around each trauma center.17 Trauma centers were considered to cover a population centroid that fell within its defined 60-minute drive time isochrone. A 60-minute cutoff was chosen because of the widely studied mortality impact of definitive trauma center care received within this “golden hour,” although the construct has been contested in large-scale retrospective studies.7,8,18 Helicopter and aeromedical EMS travel time was calculated according to methods described by Jarman et al.,19 where the straight-line distance from base to centroid, and centroid to hospital was converted to time at a constant flight velocity of 120 mph, with added constant delays for dispatch (4.4 minutes), chute (11.9 minutes), and scene time (33.6 minutes).
This methodology of population-level access presumes homogenous injury distribution. To ensure that the results were not skewed because of this assumption, sensitivity analysis was performed using temporally matched, geocoded motor vehicle fatality data from the US Department of Transportation Fatality Analysis Reporting System data set as a measure of real-world traumatic injury distribution.20
Population Characteristics and Mortality
Overlays of population-level demographics from census block groups and counties were used to identify demographic and socioeconomic factors predictive of timely trauma center access. Demographic covariates were selected for inclusion based upon previous literature on trauma care access, investigator discretion, collinearity, and significance in univariate models.
Injury mortality rates were calculated to include only nonoverdose deaths, as identified by International Classification of Disease, Tenth Revision, underlying cause-of-death code. Codes X40 to X44 (unintentional overdose), X60 to X64 (suicide by overdose), X85 (homicide by overdose), and Y10 to Y14 (overdose, undetermined intent) were excluded.21
Statistical Analysis
Generalized binomial and Poisson GWRs were used to estimate county-level factors associated with access (measured by EMS ground transport coverage to a trauma center within 60 minutes) and the impact of trauma center access on injury mortality rates (per 100,000). For the global access model, data were available for 3,133 counties (97.27%), and for the mortality model, 2020 data were available for 1,632 counties (50.67%). Longitudinal mortality data covering 2005 through 2020 were only available for 1,359 counties (42.19%). This discrepancy is due to limitation of the WONDER data set that suppresses mortality data from counties with ≤10 fatalities. Counties with suppressed fatality numbers are sparsely populated representing ≤10% of the US population and hence unlikely to affect the analysis. Spatial dependence was assessed using Moran's I, and was accounted for in GWR models, as described by Fotheringham et al.22 An adaptive bisquare kernel was used to determine bandwidth and coefficients for each model, allowing for individual county regression parameters. Variance inflation factor (VIF) was used to assess local and global multicollinearity—variables with a VIF of ≥10 were stepwise removed from the model until no variable had a VIF of ≥10.
All covariates except population density and median income were entered into the model as rates per 100 (percentages). Median income was scaled to $1,000s (e.g., 52,000 became 52), while population density was unscaled (persons per square kilometer). Following model estimation, coefficients were exponentiated into incidence rate ratios (IRRs). All analyses were conducted in R 4.2.1, using OpenStreetMap for routing, GWmodel for GWR analysis, dplyr for data manipulation, ggplot and tmap for map creation, and Stargazer and kableExtra for table generation.23–30 Group comparisons were performed using χ2 and analysis of variance for categorical variables, t tests for normally distributed continuous variables, and nonparametric tests for not normally distributed variables as appropriate.
RESULTS
Changes in Access
The 3,133 counties included in the analysis contained 211,005 and 242,335 block groups in 2005 and 2020, respectively. During the 15-year (2005–2020) study period, the US population grew by 12.41%, from 295,516,599 to 331,449,281, and the included counties contained 99.51% of the 2020 US population. In the same period, the numbers of HLTC increased by 31.01% (445–583). High-level (I/II) trauma center growth by year is visualized in Supplemental Digital Content, Appendix A1, http://links.lww.com/TA/C906. High-level (I/II) trauma center proliferation was not temporally constant, adding only 13 centers from 2005 to 2012: 90.59% of the growth in HLTCs occurred in the latter half of the study period (2012–2020). Despite this significant increase in the numbers of HLTC, population access to HLTC care within 60 minutes by ground ambulance grew by only 6.9% (from 77.5% in 2005 to 79.07% in 2012, and to 84.4% in 2020).
When HEMS coverage was added to these estimates, population access improved only marginally (adding 1.8% coverage in 2005, 1.4% in 2012, and 0.8% in 2020). Sociodemographic details of counties categorized in access quartiles are presented in Table 1. In general, when compared with counties in the highest quartile of coverage, counties in the lowest quartile were more rural (70.8% vs. 38.1%), had a greater proportion of population identifying as White (81.4% vs. 79.8%), had lower median household income (US $47,707 vs. US $60,701), worse (fair or poor) overall health status (18.7% vs. 16.8%), and higher rates of uninsured (12.6% vs. 9.9%) (p<0.05 for all).
TABLE 1.
County Characteristics by Ground HLTC Access: 2020
| HLTC Access Quartile | ||||||
|---|---|---|---|---|---|---|
| County Characteristic (2020) | Overall | 0–24% | 25–49% | 50–74% | 75–100% | Missing, % |
| n | 3,221 | 1,668 | 181 | 223 | 1,149 | |
| Injury deaths per 100,000*,** | 64.8 [51.9–81.2] | 78.2 [62.9–94.9] | 72.6 [62.1–84.5] | 69.7 [57.8–86.6] | 57.5 [47.3–70.6] | 49.3 |
| Race: White, % | 81.2 (17.3) | 81.4 (18.7) | 84.1 (15.6) | 84.6 (15.1) | 79.8 (15.7) | 0.0 |
| Age older than 65 y, % | 19.3 (4.7) | 20.6 (4.9) | 20.0 (3.6) | 19.4 (3.8) | 17.2 (4.0) | 2.5 |
| Population rurality, % | 58.6 (31.5) | 70.8 (27.5) | 73.0 (23.0) | 65.5 (22.6) | 38.1 (28.5) | 2.7 |
| Median income, $ US** | 50,566.5 [43,680.5–58,840.5] | 46,930.0 [40,795.0–53,187.5] | 50,376.0 [43,755.0–55,334.0] | 49,344.0 [43,946.0–56,779.0] | 57,675.0 [50,122.0–67,434.0] | 2.5 |
| Fair or poor health status, % | 17.9 (4.7) | 18.7 (5.2) | 18.5 (4.6) | 18.4 (4.7) | 16.8 (3.8) | 2.5 |
| Uninsured, % | 11.5 (5.1) | 12.6 (5.3) | 11.3 (4.9) | 11.4 (4.9) | 9.9 (4.5) | 2.5 |
Differences between groups are all significant at p < 0.05.
All variables are summarized as mean (SD) unless otherwise specified.
Descriptive statistics of US counties as of 2020, stratified by ground HLTC access in 2020. Means, medians, ranges, SDs, and missingness are reported for each variable, as well as the total across all counties, regardless of coverage status.
*WONDER data at the county level are only available for counties with at least 10 fatalities.
**Described using median [interquartile range].
Data sources: CDC WONDER, US Census Bureau, Robert Wood Johnson Foundation, OpenStreetMap, and NHGIS.
To compare counties with changing or static coverage over time, counties that changed overall access by at least one quartile were considered expanding if coverage increased by at least one quartile, contracting if coverage decreased by at least one quartile, and static if the coverage did not change. Even though overall US population access to HLTC improved by 6.9%, at the county level, the change in access was not uniform. Access expanded in 409 (12.7%), contracted in 142 (4.2%), and was static in the remaining 2,649 counties (83.1%) (Fig. 1).
Figure 1.

Visualization of the percentage change in county-level access to ground HLTC care within 60 minutes between 2005 and 2020. Counties with increased coverage are lighter (yellow), decreased coverage darker (purple), and counties with constant coverage are in between (green).
Among the expanding counties, population-level access increased by a median 63.6%, while, in contracting counties, population-level access decreased by a median of 31.5% (Table 2). When expanding and contracting counties were compared in terms of sociodemographics, expanding counties resembled counties in the highest access quartile, and the contracting counties were similar to the lowest access quartile (Tables 1 and 2).
TABLE 2.
County Characteristics by Ground HLTC Coverage Change: 2005 to 2020
| HLTC Access Change | |||||
|---|---|---|---|---|---|
| County Characteristic | Overall | Contracting | Static | Expanding | Missing (%) |
| n | 3221 | 142 | 2649 | 409 | |
| Injury mortality change ('20 − '05), rate*,** | 4.9 [−4.1 to 15.1] | 8.8 [0.1–16.7] | 4.9 [−3.7 to 15.1] | 3.3 [−5.7 to 15.1] | 57.8 |
| HLTC access change ('20 − '05), %** | 0.0 [0.0–1.1] | −31.5 [−68.5 to −17.6] | 0.0 [0.0–0.0] | 63.6 [32.8–90.5] | 0.7 |
| Race: White, % | 81.2 (17.3) | 82.8 (18.8) | 81.1 (17.5) | 82.0 (15.1) | 0.0 |
| Age older than 65 y, % | 19.3 (4.7) | 19.3 (3.5) | 19.3 (4.8) | 19.2 (4.8) | 2.5 |
| Population rurality, % | 58.6 (31.5) | 62.2 (27.3) | 58.2 (32.2) | 59.7 (27.9) | 2.7 |
| Median income, $ US** | 50,566.5 [43,680.5–58,840.5] | 50,187.5 [44,375.2–56,047.2] | 50,391.5 [43,495.8–59,265.8] | 51,487.0 [44,903.0–57,676.0] | 2.5 |
| Fair or poor health status, % | 0.2 (0.0) | 0.2 (0.1) | 0.2 (0.0) | 0.2 (0.0) | 2.5 |
| Uninsured, % | 11.5 (5.1) | 10.1 (4.2) | 11.5 (5.2) | 11.9 (5.1) | 2.5 |
Differences between groups are all significant at p = 0.05.
All variables are summarized as mean (SD) unless otherwise specified.
Counties that changed from a lower quartile in 2005 to a higher one in 2020 were considered “Expanding,” while those that changed from a higher quartile to a lower one were considered “Contracting.” Those that did not change access quartile were considered “Static.” Means, medians, ranges, SDs, and missingness are reported for each variable, as well as the total across all counties, regardless of coverage status.
*WONDER data at the county level are only available for counties with at least 10 fatalities.
**Described using median [interquartile range].
Data sources: CDC WONDER, US Census Bureau, Robert Wood Johnson Foundation, OpenStreetMap, and NHGIS.
Injury-Related Mortality
The overall age-adjusted, nonoverdose injury-related mortality across the United States increased from 60.72 per 100,000 population in 2005 to 66.11 per 100,000 population in 2020. At the county level, there was a serial decrease in mortality across the access spectrum (Table 1) with the highest mortality observed in counties falling in the lowest access quartile and the lowest mortality observed in those in the highest access quartile (p<0.001). In line with the national increase in injury related mortality, increased mortality was observed in counties with expanding, contracting or static coverage. However, the greatest increase in mortality was observed in counties with contracting coverage (from 64.3 to 72.4 per 100,000 population), and the lowest increase in counties where coverage was expanding (from 65.5 to 69.6 per 100,000 population) (p<0.05; Table 2).
Geographically Weighted Regression
Both HLTC access and injury mortality were found to be spatially dependent via Moran's I (0.595 and 0.390, respectively), strongly suggesting the inclusion of geography in these models. In the global binomial model of county level HLTC access, higher median income (IRR, 1.53; 95% confidence interval [CI], 1.404–1.690) and higher population density (IRR, 7.234; 95% CI, 5.120–10.428) were found to be associated with majority (≥50%) HLTC population coverage. Rurality (IRR, 0.938; 95% CI, 0.902–0.975), higher proportion of age 65 years and older (IRR, 0.520; 95% CI, 0.409–0.657), and higher proportion of uninsured (IRR, 0.669; 95% CI, 0.551–0.811) were predictive of minority (<50%) population HLTC coverage (Table 1). Counties with majority (≥50%) HLTC access had lower nonoverdose injury-related mortality (IRR, 0.933; 95% CI, 0.921–0.946).
In addition, counties with higher median income (IRR, 0.912; 95% CI, 0.907–0.917) and higher population density (IRR, 0.992; 95% CI, 0.991–0.993) had lower mortality. Conversely, counties that were more rural (IRR, 1.041; 95% CI, 1.038–1.044), with higher proportion of population of 65 years or older (IRR, 1.027; 95% CI, 1.011–1.043), with higher proportion uninsured (IRR, 1.067; 95% CI, 1.052–1.081), and with higher proportion of non-Whites (IRR, 1.069; 95% CI, 1.065–1.073) had higher injury mortality (Table 1). The higher mortality observed among non-Whites was despite overall greater access. Maps displaying the spatial variation in GWR local model coefficients are available in Supplemental Digital Content (Appendix A2–A7, http://links.lww.com/TA/C906).
Sensitivity Analyses
Estimated HLTC coverage of ultimately fatal motor vehicle collisions (MVCs) reported to the US Department of Transportation was universally lower than estimates derived from population centroids. In 2005, 66.44% of fatal MVCs occurred within 60 minutes of HLTC access by ground EMS. In 2012, this had increased by 0.57% to 67.01%; by 2020, it increased another 9.23% to 76.15% of MVCs. These measures are a relative 14.32%, 15.25%, and 9.80% lower than their corollary 2005, 2012, and 2020 population-level estimates of HLTC coverage. This suggests that, while population-based models are not perfect because of the assumption of uniform injury distribution, they function well as a “best guess” of the true injury location coverage, bolstering the validity of these methods. A detailed summary of coverage estimates by facility, transport type, and data year are available in Table 2.
Comparative population-level mortality data in rural counties were often censored for privacy, leading to a high degree of missingness for cross-year comparisons, and, in turn, a risk of biased model results. However, with these counties being highly rural, cross-year mortality data were available for more than 90% of the US population, minimizing the effect of this bias. To test this assumption using a naive approach to imputation, we ran the global models including these missing-data counties. These counties were assigned an injury mortality rate equivalent to the population mean for low access counties (79.2 per 100,000, Table 1). The new imputed model coefficients carry similar sign, significance, and scale to previous models, apart from age 65 years and older, which returns as nonsignificant (likely being collinear with rurality). Our main independent variable (majority HLTC coverage) remains consistent in effect size, significance, and sign. We take this to suggest that our exclusion of these counties, although their mortality data are not missing completely at random because of rurality, is not likely to impact the validity of our models as presented.31
DISCUSSION
Summary of Results
The current study describes national changes in trauma center access within 60 minutes in the United States, over a 15-year period spanning 2005 to 2020. Analysis was carried out using a population-level spatial accessibility and injury-covering model, which could inform assessment and direction of US trauma systems.32 Despite a 31.0% increase in the number of HLTC during the study period, population coverage increased by only 6.9%. Addition of HEMS into this model resulted in minimal coverage gains. We posit that this difference between the large increase in trauma centers and a much smaller gain in population level access is a factor of location: the vast majority of newly designated/verified HLTC were colocated inside of existing coverage areas.
Geographically weighted regression uncovered strong sociodemographic predictors of county-level HLTC access and nonoverdose injury mortality. In global models, densely populated, high-income, younger, insured, and urban communities had greater access to prompt HLTC care. Strong independent predictors of lower county-level injury mortality included high median income, younger age distribution, low rurality, and a lower non-White population percentage (Table 3). Controlling for these factors, counties with higher HLTC coverage had lower injury mortality.
TABLE 3.
Independent Predictors of County-Level HLTC Access and Injury Mortality
| Model | ||
|---|---|---|
| ≥50% HLTC Access (y/n) | Injury Mortality Rate (per 100K) | |
| ≥50% HLTC coverage (y/n) | 0.933* (0.921–0.946) | |
| Race: non-White, % | 0.998 (0.933–1.066) | 1.069* (1.065–1.073) |
| Population/km2 | 7.234* (5.120–10.428) | 0.992* (0.991–0.993) |
| Rurality, % | 0.938* (0.902–0.975) | 1.041* (1.038–1.044) |
| Median income (US $1,000) | 1.539* (1.404–1.690) | 0.912* (0.907–0.917) |
| Population older than 65 y, % | 0.520* (0.409–0.657) | 1.027* (1.011–1.043) |
| Uninsured, % | 0.669* (0.551–0.811) | 1.067* (1.052–1.081) |
| Intercept | 0.338** (0.145–0.787) | 77.515* (73.454–81.804) |
| Observations | 3, 133 | 1, 632 |
| Log likelihood | −1, 540.590 | −8, 378.057 |
| Akaike information criterion | 3, 095.180 | 16, 772.110 |
*p < 0.01.
**p < 0.05.
†p < 0.1.
Global model results from binomial and Poisson GWRs predicting ≥% HLTC coverage and injury mortality rate, respectively. All output is shown as IRR (95% CI). Incidence rate ratios for race, rurality, population age, and uninsured rate represent a 10% increase in the predictor. The IRR for population density reflects a 100 persons/(km2) increase, and IRR for median income represents a $10,000 increase.
Y/N, Yes (Covered)/No (Uncovered).
Contextualization With the Literature
Evaluating predictors and barriers to trauma center care access and identifying geographic disparities can facilitate objective and data-driven trauma system planning.8,33,34 National trauma center access and geographic trends over time have not been well studied, and there is discordance among the few reports covering this topic. Geographic access to trauma centers was first comprehensively described in 2005 by the Trauma Resource Allocation Model for Ambulances and Hospitals project, which found that an estimated 69.2% and 84.1% of all US residents had access to a HLTC within 45 and 60 minutes, respectively.7
In a recent cross-sectional study of US trauma center access, an estimated 22.8% of the population was found to lack access to any trauma center within 60 minutes, and the proportion of the population with timely access was reported to not improve significantly between 2010 and 2019.19 Another geographic analysis evaluating 60-minute access to ACS-COT–verified trauma centers found an increase in population coverage between 2013 and 2019 from 78% to 91%, respectively.31 While the current study's findings of population level access improvement is more congruent with the latter of these two reports, we found that the increased designation/verification of HLTC between 2005 and 2020 resulted in a disproportionately lower improvement in population coverage.
There are few studies that have evaluated the association between population level timely HLTC access and injury mortality, and there are no study that we are aware of has done so with county-level granularity. In a state-level analysis of adult trauma deaths reported to the Centers for Disease Control (1999–2016), states with more HLTC access had a lower age-adjusted mortality rate, and states with a high prehospital death burden had a lower proportion of population with access to HLTC within 60 minutes.8 The current study validates this association by demonstrating a univariate and multivariate reduction in county-level age-adjusted, injury mortality as HLTC access increases. This relationship has been challenged by conflicting studies, which have found minimal effects of trauma center and EMS care falling within the 60-minute golden hour, emphasizing the need for higher level evidence to form a clear picture of this relationship.35–37
When controlling for geographic and demographic factors, the current study found that higher median income is significantly associated with HLTC access and lower age-adjusted injury mortality. In addition, at the county level, as the proportion of uninsured population increased, there was significantly less access and higher mortality. These findings taken together suggest that economic drivers as opposed to population benefit likely play a major role in hospitals seeking HLTC designation/verification. A cross-sectional geographic study in the state of Maryland found that odds of death decreased by 27% when neighborhood per-capita income was greater than $25,000, supporting the finding that socioeconomically disadvantaged counties have worse outcomes.38 In addition to median income, the current study also supports the findings of multiple other studies that there are significant geographic and socioeconomic disparities in access to trauma center care within the United States.19,34,38–43
Despite greater access to HLTC, after controlling for other factors, counties with higher proportion of non-Whites had higher nonoverdose injury mortality incidence. Racial disparities in access to HLTCs have been demonstrated in three major US cities in small-area analyses of trauma deserts, defined as travel distance >5 miles to the nearest HLTC. These analyses found that Black majority census areas are more likely than White majority areas to be located within a trauma desert in Chicago, Los Angeles, and New York.44 Independent of other socioeconomic factors, it has been demonstrated that Black patients experience higher odds of trauma mortality in comparison with White patients.42 Strong advocacy is needed for targeted solutions to resolve racial and socioeconomic inequities among injured patients.45
In the context of US public policy, the passage of the 2010 Affordable Care Act (ACA) saw massive changes to funding and evaluation structures available to hospital systems. One such change relevant to this study was the allocation of increased funding for trauma care centers in the form of federal grants and uncompensated care awards.46 A 2022 meta-analysis found that the implementation of the ACA was associated with increased postacute care access but had limited effect on trauma mortality.47 In their 2017 paper, Scott et al.48 estimated that the expanded insurance coverage offered by the ACA has the potential to increase national reimbursement for inpatient trauma care by more than $1 billion. This finding suggests that ACA provisions may have afforded economic viability for the expansion of trauma care centers nationwide. Our present study bolsters these findings, with the majority (90.59%) of growth in HLTC occurring from 2012 to 2020, after the ACA was enacted. Although direct causality cannot be made between the ACA and the rapid growth in HLTC, future work with state-level claims data could be conducted to elucidate this relationship.
Way Forward
For optimized trauma system design, data-driven approaches with geographic and population need based analyses should be considered when allocating resources and center designation.34,49 Establishing new trauma centers without identification of populations in greatest need could compromise the quality of regional trauma care by generating oversupply and competition while neglecting underserved areas.45 The ACS-COT advocates that trauma center designation be based upon the needs of the population, rather than the needs of individual health care organizations or hospital groups, and HLTC designation be balanced, fair, and equitable.49
While the addition of new trauma centers is an appropriate means of improving access to timely trauma care, other strategies should also be considered. Hospital systems must approach increasing access to trauma from a multifocal lens, including discussions about the roles EMS, barriers to transportation and trauma training protocols. A systematic review found that shorter transfer time and swift transport to the care facility by EMS is associated with a decreased odds of mortality.50 Current literature demonstrates that transportation barriers pose a credible threat to timely access to care, particularly among uninsured and lower income communities.51
The findings of the current study clearly demonstrate that factors other than the needs of the population are the primary drivers of new HLTC designation/verification. The Needs Based Assessment of Trauma Systems has been proposed as an objective method of assessing where additional trauma centers and EMS resources should be located.52 The current study demonstrates that geospatial analysis can inform objective, data-driven trauma system organization and supplement Needs Based Assessment of Trauma Systems methodology.
Based on the findings of the current study, actionable areas for trauma system planning should focus on (1) regions with high injury mortality that have low population access to HLTC (red in Fig. 2) that will benefit from additional HLTC designation, and (2) regions with both high access and high injury mortality (purple in Fig. 2) likely represent either a disproportionate number of nonsurvivable injuries (e.g., firearm injury) or poor system performance. These areas will benefit from performance improvement programs and strong injury prevention initiatives.
Figure 2.
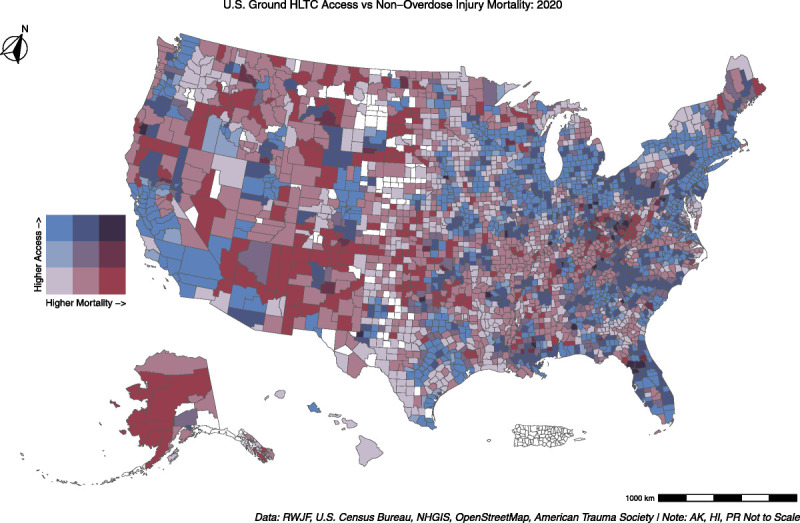
Bivariate map comparing tertiles of county-level HLTC coverage and nonoverdose injury mortality. Counties with increased coverage are lighter blue, and those with higher injury mortality are darker red. Counties with high injury mortality and low HLTC coverage will be only dark red, while those with high coverage and low mortality will be only light blue. Counties falling in the middle are categorized by the respective hue in the legend.
Additional studies focusing on specific regions and discrepancies in access and outcomes could facilitate the identification of gaps and approaches for targeted interventions and outcome improvement. State and regional studies could help to objectively and appropriately identify specific facilities for targeted HLTC upgrades and improved population access. Future investigations could also explore barriers to upgrading existing hospitals to HLTC in regions with low access and high mortality rates.
LIMITATIONS
Like all studies, the current study has limitations. First, the model estimates for ground access are based on estimated road network EMS travel time, and because of data availability cannot be compared with similar, real-world EMS data. To mitigate this limitation, models were calculated using OpenStreetMap's transport layer, which is well validated and commonly used in this setting.53–56 In addition, although the HEMS time estimates include scene, chute, and response time, ground EMS estimates do not. Thus, our coverage estimates represent a “best-case” scenario with instant ground EMS availability, and true population coverage is likely lower than our estimates (Table 4).
TABLE 4.
Change in US County-Level Trauma Center Access, 2005 to 2020
| Level | Coverage Estimate Type | |||||||
|---|---|---|---|---|---|---|---|---|
| Population Centers, % | MVC Fatality, % | |||||||
| 2005 | 2012 | 2020 | Diff. | 2005 | 2012 | 2020 | Diff. | |
| Ground and HEMS | ||||||||
| Level I | 66.85 | 67.72 | 70.72 | 3.87 | 53.59 | 54.13 | 59.64 | 6.05 |
| Level II | 63.20 | 64.63 | 72.47 | 9.27 | 51.09 | 51.81 | 62.80 | 11.71 |
| Level I/II | 79.30 | 80.51 | 85.21 | 5.91 | 68.28 | 68.45 | 77.05 | 8.77 |
| Ground | ||||||||
| Level I | 65.96 | 67.29 | 70.71 | 4.75 | 52.85 | 53.88 | 59.64 | 6.79 |
| Level II | 57.95 | 59.99 | 70.03 | 12.08 | 46.63 | 47.91 | 60.05 | 13.42 |
| Level I/II | 77.54 | 79.07 | 84.42 | 6.88 | 66.44 | 67.01 | 76.15 | 9.71 |
| HEMS | ||||||||
| Level I | 22.38 | 21.60 | 21.75 | −0.63 | 13.19 | 13.27 | 15.40 | 2.21 |
| Level II | 12.18 | 12.45 | 12.95 | 0.77 | 8.03 | 8.23 | 9.23 | 1.2 |
| Level I/II | 27.02 | 26.58 | 27.03 | 0.01 | 16.90 | 17.19 | 19.53 | 2.63 |
Differences between groups are all significant at p < 0.05.
This table shows the change in trauma center access between 2005, 2012, and 2020, for each level of trauma center, as well as grouped I/II (HLTC), broken out by ground access, air access (HEMS), and combined (ground + HEMS access).
Data source: Fatality Analysis Reporting System and US Census Bureau.
Diff., Difference from 2005 to 2020 (2020-2005).
Second, WONDER and Robert Wood Johnson Foundation age-adjusted county-level injury mortality rates have been used, as opposed to individual-level, risk-adjusted data points. This limitation is common to cross-sectional studies of this nature and introduces the possibility of ecologic fallacy influencing the measured associations. Because of this potential bias, results from cross-sectional studies should be interpreted with some caution and their associations tested for replicability and causal directionality.
Third, population centroid density moderately correlates with optimal EMS base locations and does not mirror actual geographic injury density as evidenced by our sensitivity analysis.56 Future studies of this nature should attempt to obtain incident location information to better calibrate coverage estimates. These calibrated models could use multiple weighting methods to obtain a CI of coverage for multiple mechanisms of injury, better reflecting the landscape of care.
CONCLUSION
Over the past 15 years, despite a 30% increase in the number of HLTC, population access increased by only 7%. Counties with expanding HLTC access experienced lower age-adjusted injury mortality rates. Prioritization of HLTC expansion should occur in regions with high mortality and low population coverage, while targeted quality improvement and/or injury prevention programs could benefit regions with both high population HLTC coverage and injury mortality. Geographic information systems methodology can be a vital tool in objectively identifying existing centers that, if upgraded to HLTC, would benefit the population maximally.
Supplementary Material
AUTHORSHIP
A.K.M. is chief investigator. A.K.M., J.S.B., and S.A. drafted the manuscript. J.S.B. and S.A. conceived the study concept and design, in concert with all authors. All authors had access to the study data, contributed to analysis and interpretation, and reviewed and approved the final manuscript. A.K.M. had final responsibility for the decision to submit for publication.
ACKNOWLEDGMENTS
We thank the community of data scientists, health researchers, and physicians collecting and disseminating open-source data sets, which have made this work possible. In addition, we wish to extend our gratitude to Dr. Molly P. Jarman of Brigham and Women's Hospital and Dr. Lance Sherry of George Mason University for their generous provision of data sets on aeromedical rescue base locations and capabilities as well as Dr. Douglas J. Wiebe of the University of Pennsylvania for his provision of historical US Trauma Center GIS data sets. Map data copyrighted OpenStreetMap contributors and available from https://www.openstreetmap.org.
DISCLOSURE
The authors declare no conflicts of interest.
Footnotes
Published online: March 7, 2023.
S.A. and J.S.B. are co-first authors.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Stas Amato, Email: stas.amato@uvmhealth.org.
Barclay Stewart, Email: barclays@uw.edu.
Ashwini Sarathy, Email: ashwini.sarathy@med.uvm.edu.
Turner Osler, Email: Turner.Osler@uvm.edu.
David Hosmer, Email: dhosmer@umass.edu.
Gary An, Email: Gary.An@uvmhealth.org.
Alan Cook, Email: adcookmd@gmail.com.
Robert J. Winchell, Email: row9057@med.cornell.edu.
Ajai K. Malhotra, Email: Ajai.Malhotra@uvmhealth.org.
REFERENCES
- 1.Sampalis JS Lavoie A Boukas S Tamim H Nikolis A Frechette P, et al. Trauma center designation: initial impact on trauma-related mortality. J Trauma. 1995;39(2):232–237. [DOI] [PubMed] [Google Scholar]
- 2.MacKenzie EJ Rivara FP Jurkovich GJ Nathens AB Frey KP Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–378. [DOI] [PubMed] [Google Scholar]
- 3.American College of Surgeons . Verification, Review, and Consultation Program. ACS. 2022. Available at: https://www.facs.org/quality-programs/trauma/quality/verification-review-and-consultation-program/. Accessed July 30, 2022. [Google Scholar]
- 4.Mullins RJ Veum-Stone J Hedges JR Zimmer-Gembeck MJ Mann NC Southard PA, et al. Influence of a statewide trauma system on location of hospitalization and outcome of injured patients. J Trauma. 1996;40(4):536–545; discussion 545-6. [DOI] [PubMed] [Google Scholar]
- 5.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283(15):1990–1994. [DOI] [PubMed] [Google Scholar]
- 6.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48(1):25–30; discussion 30-31. [DOI] [PubMed] [Google Scholar]
- 7.Branas CC MacKenzie EJ Williams JC Schwab CW Teter HM Flanigan MC, et al. Access to trauma centers in the United States. JAMA. 2005;293(21):2626–2633. [DOI] [PubMed] [Google Scholar]
- 8.Hashmi ZG Jarman MP Uribe-Leitz T Goralnick E Newgard CD Salim A, et al. Access delayed is access denied: relationship between access to trauma center care and pre-hospital death. J Am Coll Surg. 2019;228(1):9–20. [DOI] [PubMed] [Google Scholar]
- 9.American Trauma Society . Trauma Information Exchange Program (TIEP). 2020. Available at: https://www.amtrauma.org/page/TIEP. Accessed January 24, 2022.
- 10.Douglas J. Wiebe, PhD. TRAMAH Hospital GIS Files. 2021. Available at: https://hifld-geoplatform.opendata.arcgis.com/datasets/emergency-medical-service-ems-stations/. Accessed November 11, 2021.
- 11.US Department of Homeland Security . Emergency Medical Service (EMS) Stations. 2021. Available at: https://hifld-geoplatform.opendata.arcgis.com/datasets/emergency-medical-service-ems-stations/. Accessed January 24, 2022.
- 12.Jarman M, PhD . USCG Air Base Locations. 2022.
- 13.US Census Bureau . Centers of Population. Census.gov. 2020. Available at: https://www.census.gov/geographies/reference-files/time-series/geo/centers-population.html. Accessed January 24, 2022.
- 14.US Census Bureau . 2020 American Communities Survey. United States Census Bureau; 2020. Available at: https://data.census.gov/mdat/#/search?ds=ACSPUMS1Y2019. Accessed April 9, 2021. [Google Scholar]
- 15.Centers for Disease Control and Prevention, National Center for Health Statistics . National Vital Statistics System, Mortality 1999–2020 on CDC WONDER Online Database. 2021. Available at: http://wonder.cdc.gov/ucd-icd10.html. Accessed July 29, 2022.
- 16.University of Wisconsin Population Health Institute . County Health Rankings & Roadmaps, 2020. 2020. Available at: http://www.countyhealthrankings.org.
- 17.OpenStreetMap Foundation . OpenStreetMap. 2020. Available at: http://download.geofabrik.de/north-america.html. Accessed January 24, 2022.
- 18.Lansink KW, Gunning AC, Leenen LP. Cause of death and time of death distribution of trauma patients in a level I trauma centre in the Netherlands. Eur J Trauma Emerg Surg. 2013;39(4):375–383. [DOI] [PubMed] [Google Scholar]
- 19.Jarman MP, Dalton MK, Askari R, Sonderman K, Inaba K, Salim A. Accessibility of level III trauma centers for underserved populations: a cross-sectional study. J Trauma Acute Care Surg. 2022. Available at: 10.1097/TA.0000000000003725. Accessed April 11, 2023. [DOI] [PubMed] [Google Scholar]
- 20.National Highway Traffic Safety Administration . Fatality Analysis Reporting System (FARS) | NHTSA. 2020. Available at: https://www.nhtsa.gov/research-data/fatality-analysis-reporting-system-fars. Accessed July 10, 2022.
- 21.U.S. Centers for Disease Control and Prevention . Prescription drug overdose data & statistics: guide to ICD-9-CM and ICD-10 codes related to poisoning and pain. 2013. Available at: https://stacks.cdc.gov/view/cdc/59394. Accessed July 30, 2022.
- 22.Fotheringham . The Problem of Spatial Autocorrelation, and Local Spatial Statistics. 2009. Available at: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1538-4632.2009.00767.x. Accessed January 24, 2022.
- 23.R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2021. [Google Scholar]
- 24.Tennekes M Nowosad J Gombin J Jeworutzki S Russell K Zijdeman R, et al. tmap: Thematic Maps. 2021. Available at: https://CRAN.R-project.org/package=tmap. Accessed January 24, 2022.
- 25.GIScience Research Group and HeiGIT . openrouteservice R client. 2022. Available at: https://github.com/GIScience/openrouteservice-r. Accessed January 24, 2022.
- 26.Heidelberg Institute for Geoinformation Technology (HeiGIT) . Openrouteservice. Available at: https://openrouteservice.org/. Accessed January 24, 2022.
- 27.Lu B Harris P Charlton M Brunsdon C Nakaya T Murakami D, et al. GWmodel: Geographically-Weighted Models. 2021. Available at: https://CRAN.R-project.org/package=GWmodel. Accessed January 24, 2022.
- 28.Zhu H Travison T Tsai T Beasley W Xie Y Yu G, et al. kableExtra: Construct Complex Table with “kable” and Pipe Syntax. 2021. Available at: https://CRAN.R-project.org/package=kableExtra. Accessed July 30, 2022.
- 29.Hlavac M. stargazer: Well-Formatted Regression and Summary Statistics Tables. 2022. Available at: https://CRAN.R-project.org/package=stargazer. Accessed April 11, 2023.
- 30.Wickham H Averick M Bryan J Chang W McGowan LD François R, et al. Welcome to the tidyverse. Journal of Open Source Software. 2019;4(43):1686. [Google Scholar]
- 31.Choi J, Karr S, Jain A, Harris TC, Chavez JC, Spain DA. Access to American College of Surgeons Committee on Trauma–verified trauma centers in the US, 2013–2019. JAMA. 2022;328(4):391–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amato SS Benson JS Murphy S Osler TM Hosmer D Cook AD, et al. Geographic coverage and verification of trauma centers in a rural state: highlighting the utility of location allocation for trauma system planning. J Am Coll Surg. 2021;232(1):1–7. [DOI] [PubMed] [Google Scholar]
- 33.Abbasi AB Dumanian J Okum S Nwaudo D Lee D Prakash P, et al. Association of a new Trauma center with racial, ethnic, and socioeconomic disparities in access to trauma care. JAMA Surg. 2021;156(1):97–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Winchell RJ. The invisible hand guiding trauma center designation: it is time for a different paradigm. J Am Coll Surg. 2021;232(2):224. [DOI] [PubMed] [Google Scholar]
- 35.Newgard CD Schmicker RH Hedges JR Trickett JP Davis DP Bulger EM, et al. Emergency medical services intervals and survival in trauma: assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010;55(3):235–246.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lerner EB, Moscati RM. The golden hour: scientific fact or medical “urban legend”? Acad Emerg Med. 2001;8(7):758–760. [DOI] [PubMed] [Google Scholar]
- 37.Okada K, Matsumoto H, Saito N, Yagi T, Lee M. Revision of “golden hour” for hemodynamically unstable trauma patients: an analysis of nationwide hospital-based registry in Japan. Trauma Surg Acute Care Open. 2020;5(1):e000405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jarman MP, Curriero FC, Haut ER, Pollack Porter K, Castillo RC. Associations of distance to trauma care, community income, and neighborhood median age with rates of injury mortality. JAMA Surg. 2018;153(6):535–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jarman MP, Castillo RC, Carlini AR, Kodadek LM, Haider AH. Rural risk: geographic disparities in trauma mortality. Surgery. 2016;160(6):1551–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ali MT Hui X Hashmi ZG Dhiman N Scott VK Efron DT, et al. Socioeconomic disparity in inpatient mortality after traumatic injury in adults. Surgery. 2013;154(3):461–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carr BG Bowman AJ Wolff CS Mullen MT Holena DN Branas CC, et al. Disparities in access to trauma care in the United States: a population-based analysis. Injury. 2017;48(2):332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haider AH Weygandt PL Bentley JM Monn MF Rehman KA Zarzaur BL, et al. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74(5):1195–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hsia R, Shen Y-C. Possible geographical barriers to trauma center access for vulnerable patients in the United States: an analysis of urban and rural communities. Arch Surg. 2011;146(1):46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tung EL, Hampton DA, Kolak M, Rogers SO, Yang JP, Peek ME. Race/ethnicity and geographic access to urban trauma care. JAMA Netw Open. 2019;2(3):e190138–e190138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Knowlton LM. Racial and ethnic disparities in geographic access to trauma care—a multiple-methods study of US urban trauma deserts. JAMA Netw Open. 2019;2(3):e190277–e190277. [DOI] [PubMed] [Google Scholar]
- 46.Patient Protection and Affordable Care Act; HHS Notice of Benefit and Payment Parameters for 2012, 78 Fed. Reg. 15410 (March 11, 2013) (to be codified at 45 C.F.R. pts. 153, 155, 156, 157, & 158).
- 47.Newsome K, Autrey C, Sen-Crowe B, Ang D, Elkbuli A. The affordable care act and its effects on trauma care access, short- and long-term outcomes and financial impact: a review article. Ann Surg Open. 2022;3(1):e145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Scott JW Neiman PU Najjar PA Tsai TC Scott KW Shrime MG, et al. Potential impact of Affordable Care Act–related insurance expansion on trauma care reimbursement. J Trauma Acute Care Surg. 2017;82(5):887–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.American College of Surgeons . Statement on trauma center designation based upon system need | The Bulletin. 2015. Available at: https://bulletin.facs.org/2015/01/statement-on-trauma-center-designation-based-upon-system-need. Accessed July 30, 2022. [PubMed]
- 50.Harmsen AMK, Giannakopoulos GF, Moerbeek PR, Jansma EP, Bonjer HJ, Bloemers FW. The influence of prehospital time on trauma patients outcome: a systematic review. Injury. 2015;46(4):602–609. [DOI] [PubMed] [Google Scholar]
- 51.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Uribe-Leitz T Esquivel MM Knowlton LM Ciesla D Lin F Hsia RY, et al. The American College of Surgeons needs-based assessment of trauma systems: estimates for the state of California. J Trauma Acute Care Surg. 2017;82(5):861–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fleischman RJ, Lundquist M, Jui J, Newgard CD, Warden C. Predicting ambulance time of arrival to the emergency department using global positioning system and Google maps. Prehosp Emerg Care. 2013;17(4):458–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weiss DJ Nelson A Vargas-Ruiz CA Gligorić K Bavadekar S Gabrilovich E, et al. Global maps of travel time to healthcare facilities. Nat Med. 2020;26(12):1835–1838. [DOI] [PubMed] [Google Scholar]
- 55.Tenkanen H, Saarsalmi P, Järv O, Salonen M, Toivonen T. Health research needs more comprehensive accessibility measures: integrating time and transport modes from open data. Int J Health Geogr. 2016;15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Røislien J van den Berg PL Lindner T Zakariassen E Uleberg O Aardal K, et al. Comparing population and incident data for optimal air ambulance base locations in Norway. Scand J Trauma Resusc Emerg Med. 2018;26(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


