Abstract
For all clinical purposes, cornual, angular, and interstitial pregnancies are considered ectopic pregnancies that can have grave consequences for the patient. In this article, we describe and distinguish 3 types of ectopic pregnancies in the cornual region of the uterus. The authors advocate using the “cornual pregnancy” term only for ectopic pregnancies in malformed uteruses. We describe an ectopic pregnancy in a 25-year-old G2P1 patient in the cornual region of the uterus that was missed twice sonographically in the second trimester and had almost fatal consequences in the patient. Radiologists and sonographers should be aware of the sonographic diagnosis of angular, cornual and interstitial pregnancies. Whenever possible, first-trimester transvaginal ultrasound scanning is crucial for diagnosing these 3 types of ectopic pregnancies in the cornual region. In the second and third trimesters, ultrasound tends to become equivocal; hence alternate imaging, such as MRI, might add additional value to the management of the patient. A case report assessment and a comprehensive literature review comprising 61 case reports of ectopic pregnancy in the second and third trimesters are diligently undertaken in the Medline, Embase and Web of Science databases. The major strength of our study is that it is one of the few studies that describe a literature review of ectopic pregnancy in the cornual region exclusively in the second and third trimesters.
Keywords: Angular, Cornual, Endometrium, Interstitial, Uterine malformation
Introduction
Implantation of a developing blastocyst outside the endometrial cavity is known as an ectopic pregnancy. Statistically, approximately 2%-5% of these occur in the interstitial or cornual regions of the uterus [1,2]. Clinicians commonly regard all types of ectopic pregnancies in the normal cornual region of the uterus as “Cornual” ectopic pregnancy [3,4,8]. It is essential to understand the terminology surrounding cornual, angular, or interstitial pregnancies because the findings, management, and outcomes are different in each of the 3 ectopic pregnancies [5]. These 3 forms of ectopic pregnancies are often lumped together, and clinicians sometimes have ambiguity in arriving at a correct diagnosis based on history and imaging [6]. Interstitial pregnancies account for 2%-11% of tubal ectopic pregnancies and constitute approximately 20% of deaths [7]. Radiologists and several practitioners have used the term cornual and interstitial ectopic pregnancy interchangeably [7,8]. In the literature, true cornual pregnancy is located in the rudimentary horn of the unicornuate uterus or the rudimentary horn of a septate or bicornuate uterus [9], [10], [11], [12]. Therefore, some authors synonymously use the term “cornual” pregnancy with “rudimentary horn” pregnancy [13]. To add to this incertitude, most obstetricians and gynecologists still use the term "cornual pregnancy" to describe any pregnancy in the normal anatomical cornual regions of the uterus [14]. In this article, we chose to use the term “cornual” pregnancy only for pregnancies in the uterus presenting with congenital anomalous presentation, that is, rudimentary, septate, bicornuate, unicornuate, or any other uterine malformation. Regardless of the confusion around the terminology for cornual pregnancy, the sonographic criteria for this type of pregnancy are an empty uterine cavity, a gestational sac located eccentrically (1 cm from the lateral wall of the uterine cavity), and a thin myometrial layer (<5 mm) surrounding the gestational sac [10]. The biggest concern for cornual pregnancy is the potential to rupture due to the lack of myometrial support surrounding the delicate gestational sac [15].
An interstitial pregnancy is an ectopic pregnancy implanted in the interstitial part of the fallopian tube and close to the uterine musculature. Interstitial pregnancies implant lateral to the round ligament and are approximately 1-2 cm within the intra-myometrial region of the tube, with the gestational sac surrounded by less than 5 mm of the myometrium in all scanning planes, a chorionic sac separate (> 1 cm) from the lateral edge of the uterine cavity, and the presence of an interstitial line sign [6,16,17,18]. In the literature, the sensitivity and specificity of the sonographic “interstitial line sign” varies from 80% to 100% [16,11,20]. The interstitial line sign is thought to be a sonographic impression that represents an echogenic line from the mass or gestational/interstitial sac to the endometrial echo complex [11,18,21]. Some authors believe these criteria are more valid in the first trimester and tend to lose sensitivity after this period [19]. The interstitial uterine region is prone to rupture owing to increased distensibility and hypervascularity [6,9]. Therefore, it is vital to diagnose ectopic pregnancy in the first trimester for conservative treatment such as methotrexate to be effective. A delay in the diagnosis of interstitial pregnancy may lead to cornual uterine resection. Some studies have reported a mortality rate of 2%-3% with interstitial pregnancy [22].
Angular pregnancy is the third type of pregnancy in the normal cornual region of the uterus and is a differential diagnosis of interstitial or true cornual pregnancy. Anatomically, angular pregnancy implants medial to the round ligament, at the lateral angle of the endometrial/uterine cavity, and just medial to the uterotubal junction [17]. Angular pregnancy can progress to term because it is technically inside the uterine/endometrial cavity [5,23,24]. Some authors discourage the association of ectopic term with angular pregnancy due to the intrauterine or eccentric endometrial location of the developing fetus [25]. The myometrial mantle thickness in angular pregnancy is > 5 mm without an interstitial line sign [25]. Angular pregnancy has been associated with uterine rupture in up to 23%-29% of cases [8,26,27]. Angular pregnancy has been classified as a type of ectopic pregnancy owing to its proximity to the cornual region [28]. Another reason that angular pregnancy is regarded as a type of ectopic pregnancy is that it is difficult to differentiate interstitial from angular pregnancy, especially during the first trimester, and it also presents similar symptomatology to a typical ectopic pregnancy [9,17,29,30,31].
The diagnosis of these 3 types of pregnancies in the second trimester brings numerous challenges as far as management is concerned. For instance, angular pregnancy can mimic the clinical presentations of typical ectopic pregnancy, such as persistent pelvic pain and bleeding, uterine rupture, spontaneous abortion, postpartum endometritis, and severe bleeding leading to hysterectomy [24,47]. On the other hand, a relatively late diagnosis of cornual pregnancy is a prominent exacerbating factor for impending grave hemorrhage [32,33]. Interstitial ectopic pregnancy continues to progress into the second trimester owing to greater distensibility and hypervascularity, as mentioned above, leading to an inevitably worse prognosis in most cases [5,9].
Etiology and pathogenesis
In general, there are numerous risk factors for ectopic pregnancies, such as tubal pregnancy, ectopic pregnancy, intrauterine devices, pelvic inflammatory diseases, salpingitis and infertility. Furthermore` exposure to diethylstilbesterol, age > 40 years, smoking, previous pelvic surgeries and assisted reproduction techniques have been implicated as potential risk factors for ectopic pregnancy [11,17,34]. Ipsilateral salpingectomy is the only known etiological factor specific to interstitial ectopic pregnancy [35].
Case report
A 25-year-old female G2P1, visited our emergency department (ED) with complaints of sharp, constant lower abdominal pain and no vaginal spotting/bleeding. The patient also had a history of polycystic ovarian syndrome (PCOS) and a cesarean section 2 years ago. Based on her health records, the patient was presumed to be in the second trimester.
The patient was admitted to the ED observation ward with stable vital signs. Late evening the patient developed vaginal spotting that quickly progressed to vaginal bleeding, superimposed with blood clots and severe cramping that radiated to the back. The ED physician ordered an urgent obstetric ultrasound on the same day to assess for threatened abortion. An urgent obstetric scan in our ultrasound department revealed a single live intrauterine pregnancy at 16 weeks. The technologist noted that the internal orifice of the cervix uteri (internal os) was not retraceable into the uterine cavity. Therefore, endovaginal or transvaginal scanning was performed to visualize the internal cervical os and to rule out vasa previa and placenta previa. (Fig. 1A-C)
Fig. 1.
(A) Sagittal: Visualization of the cervical canal was difficult because the large size of the extrauterine pregnancy was displacing the cervix/uterus posteriorly and to the right. (B) Sagittal: A rough estimate for the potential distance from the lower edge of the placenta to the internal os was attempted. (C). Sagittal: Colour Doppler showing retroplacental flow extending to an area of myometrium near the suspected cervix.
The radiologist noted the sonographer's impression (Fig. 1A–C) and suggested a repeat ultrasound at 20 weeks to better visualize the internal cervical os. The patient was sent back to the ED and subsequently discharged from our hospital, thus missing a potential ectopic pregnancy.
The patient returned to ED in less than 2 weeks, complaining of generalized abdominal pain, chest pain and lower back pain that was not positional or relieved with antianalgesics. In about a few hours, the patient reported that the pain had migrated to the right lower quadrant (RLQ) and flank area with episodes of nausea and vomiting. An emergent ultrasound was ordered to rule out appendicitis, right kidney and right ovarian pathology, and retroplacental abruption.
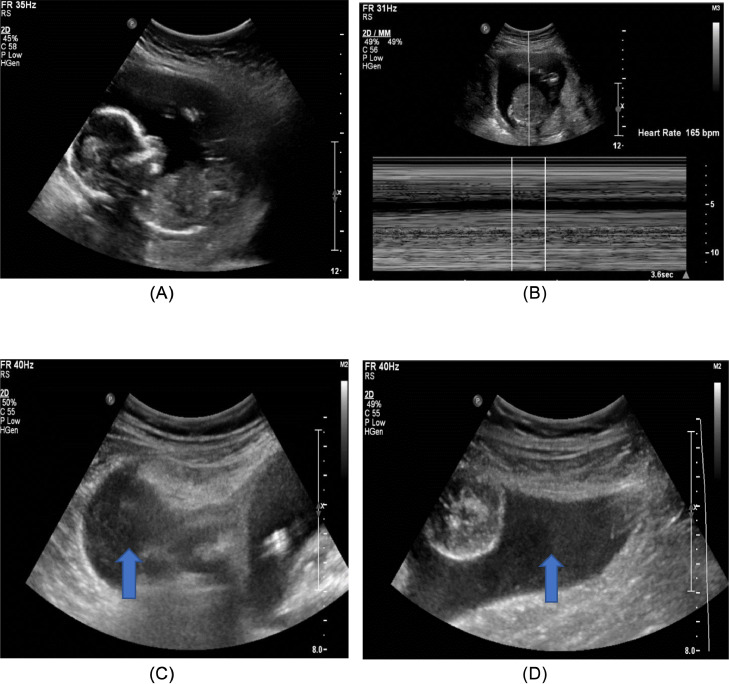
Upon scanning the patient, for the second time, age-appropriate gestation was documented without any signs of distress in the fetus (Fig. 2A andB). Furthermore, a mild to moderate amount of echogenic free fluid (FF) was noted in the pelvic region, especially the RLQ, denoting hemoperitoneum (Fig. 2C and D).
Fig. 2.
(A) Normal fetal development at 17 weeks. (B) Normal fetal heart rate. (C) Transverse: Echogenic FF in RLQ (arrow). (D) Sagittal: Echogenic FF in RLQ (arrow).
The area of extreme tenderness in the RLQ was scanned diligently. On the transabdominal scan, the sonographer suspected a uterus-like structure with a thin endometrial stripe. (Fig. 3A) The cine loop/video nicely reveals the separation of the uterus from the amniotic cavity upon a gradual transabdominal pressure with the transducer. (Supplementary Video 1) To further investigate this speculation, transvaginal scanning was performed.
Fig. 3.
(A) Transabdominal sagittal plane: A presumed uterus is seen in the right adnexal region. Arrowhead denotes a potential endometrial stripe. (Supplementary Video 2Fig. 3A). (B) Sagittal: Transvaginal ultrasound confirmed the uterus in the right adnexa. (C) Endovaginal transverse plane: The arrowhead depicts an empty left lateral endometrial region. (Supplementary Video 3Fig. 3C). (D). Sagittal: Transvaginal image of the cervix & uterine body. The arrowheads show communication of the cervix with the uterine cavity. (Supplementary Video 4Fig. 3D).
In our department, transvaginal scanning is not a routine examination in the second trimester and is required only in challenging cases to establish a diagnosis. The 8.6 cm structure in the right adnexal region was felt to be a retroverted uterus with an empty endometrial cavity and normal bilateral endometrial border at the fundus region of the uterus in the transverse scanning plane (Fig. 3C). The technologist attempted to convince the radiologist in his images by demonstrating the endocervical canal in communication with the uterine body, thereby lending more support to the fact that the endometrial cavity is empty in this nonpregnant uterus (Fig. 3D).
Upon scanning the right and left upper quadrants, free fluid was visualized in the hepatorenal (Morrison's pouch) and splenorenal recesses without any evidence of hydronephrosis in either kidney (Fig. 4A and B).
Fig. 4.
(A). Sagittal: Free fluid in the hepatorenal recess. (B) Sagittal: Free fluid in the splenorenal recess.
Despite the compelling sonographic images, the radiologist did not acknowledge the technologist's impression. Once again, the diagnosis of normal intrauterine pregnancy, along with numerous differential diagnoses, was provided in the report. Some of the differential diagnoses documented in the report were hemorrhagic neoplasm, heterotopic pregnancy, red degeneration of the fibroid, dermoid cyst, or decidualized endometrioma, and an ovarian origin mass with associated ovarian torsion. The patient was sent back to the ED for a second time. The patient was discharged after performing the necessary blood tests. Thus, the ED physician and the radiologist again missed the likelihood of a grave impending ectopic pregnancy in the cornual region (based on clinical symptomatology and pertinent imaging).
Surgical history
Four days after the last discharge, the patient developed hypotension and was immediately transferred to OR at a nearby tertiary hospital. For the first time, the obstetrical team diagnosed ectopic pregnancy in this patient and called it a “cornual ectopic pregnancy” to the left of the uterine cavity. The left cornual region of the uterus was ruptured, leading to hemoperitoneum and hypotension and the fetus was presumed to be in the abdomen without any signs of fetal heart activity. The obstetrician delivered the stillborn fetus and repaired the left uterine cornual area along with a left salpingo-oophorectomy (LSO). Ligation of the internal iliac artery was also performed to control the excessive bleeding associated with uterine rupture. Owing to the patient's life-threatening hemorrhage, a massive transfusion protocol was initiated in this case. Guidelines on massive transfusion protocols in adults vary worldwide, depending on the institution's preference or experience and patient's hemodynamic status. Obstetric bleeding presents additional challenges for clinicians. In this patient, the massive transfusion protocol consisted of 9 units of packed RBC, 1 Liter fresh frozen plasma (FFP), 4 g fibrinogen, 1 unit of platelets, and 6.5 Liter IV fluid. The products of conception (POC) were sent for pathological evaluation.
Pathological diagnosis
The pathologist also agreed with the obstetrician's impression of “cornual ectopic pregnancy” and reported the association of the decidua and myometrium with chorionic villi in the cornual region of the uterus. Additionally, the tissue around the left cornual region is reported necrotic, consistent with a left ruptured cornual ectopic pregnancy. The fetus, chorionic villi, tri-vascular umbilical cord, and fetal membranes were identified by microscopic examination of the gross pathological specimen. Products of conception were appropriately recognized on gross examination, but for technical reasons, gross pathological images of the POC cannot be obtained for publication purposes.
Our perspective
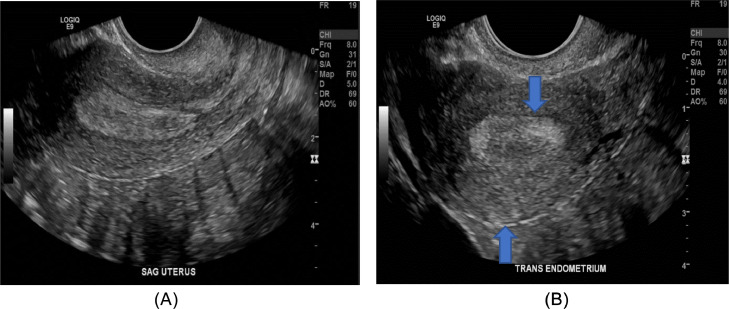
We followed up on the patient's earlier imaging 3 years ago at another tertiary hospital in the city. On this ultrasound scan, no evidence of uterine malformation was visualized sonographically. Based on this finding, the radiologist reported the normal shape of the uterus. If we were to apply the definition of true cornual ectopic to this case, it would not support the obstetrician or the pathologist's diagnosis based on the sonographic images (Fig. 3A–D, Fig. 5A and B) and the radiologist's impression documented 3 years earlier. We feel there is ambiguity in the correct diagnosis of this patient. Fig. 3B and C, and the supplementary videos 3 and 4 demonstrate the retroverted uterus with empty left lateral endometrium, thereby making the likelihood of angular pregnancy extremely unusual at this location. We believe that the most likely diagnosis in our patient was interstitial rather than cornual or angular due to the normal shape of the uterus and the empty left fundal endometrial cavity. We speculate that the obstetrician, in this case, might have based the clinical insight on cornual ectopic pregnancy due to the mass effect of the pregnancy in the cornual region of the uterus on laparotomy. Unfortunately, the patient did not have first-trimester scans for the current pregnancy, and thus, the diagnosis of angular or interstitial ectopic pregnancy is hard to elucidate with certainty. Regardless, as stated earlier, we postulate that the current ectopic pregnancy is probably interstitial rather than cornual or angular, owing to the recent ultrasound images in our department and prior sonographic imaging 3 years ago depicting the normal shape of the uterus (Fig. 3B and C, Fig.5A and B plus Supplementary videos 2, 3, and 4).
Fig. 5.
(A) Sagittal Normal contour of the uterine fundus and body. (B) Transverse Normal contour of endometrium & fundus (arrows).
Literature review
Methodology
The authors (G.D., R.C., and L.Z.) searched for cornual, angular, and interstitial pregnancies in the second and third trimesters using the MedLine, Embase, and Web of Science databases. We adapted our search terms and techniques to all 3 databases. For instance, we used the following MeSH search terms for Medline: (pregnancy, cornual), (pregnancy, angular), (pregnancy, interstitial), (pregnancy trimester, second), and (pregnancy trimester, third). Likewise, instead of MeSH, Emtree was used in Embase by selecting “map terms to subject heading.” Other keywords used were ectopic pregnancy, 13-to-40-week pregnancy, and rudimentary horn pregnancy. All gray literature was excluded, and only peer-reviewed case report articles were included in our final list. The search results were exported from all 3 databases to the Zotero 6.0.20 reference manager. Zotero was used to compile search results from all 3 databases into a single folder named “interstitial pregnancy,” from which the process of deduplication or merging of the articles was performed.
We searched for cornual, interstitial and angular pregnancies only in the second and third trimesters to replicate our case report in terms of symptomatology, prognosis, and outcome. Considering the rapid advances in the technological capabilities of imaging equipment, all case reports published before 2000 were excluded from our study. We excluded all systematic reviews and more extensive case series. We only included case reports in English to better understand the in-depth case history, diagnosis, treatment, and outcome in individual cases. The search results from Zotero were imported into Rayyan software to appropriately apply the above limitations/inclusion/exclusion criteria to the articles. Tables 1, 2 and 3 present the final lists of the selected case report articles.
Table 1.
Angular pregnancy case reports and sonographic features in the second or third trimester (2000-2023). Search performed on February 10, 2023.
| Author | Year | Number of cases | Myometrial/endometrial thickness | Gestational age at presentation | Outcome |
|---|---|---|---|---|---|
| Mustafa et al. [43] | 2021 | 1 | Not reported | 18 wk | Uterine rupture; fetal demise |
| Martinez et al. [44] | 2008 | 1 | thin myometrial wall | 22 | Hysterectomy at 22 wk |
| Yao et al. [45] | 2021 | 1 | Not reported | 25 wk 6 d | 5 cm of cornual region rupture; fetus status not reported distinctly |
| Hasanzadeh et al. [46] | 2017 | 1 | Not reported | 20 wk 2 d | Left lateral endometrial angle rupture and repair of the uterus; a nonviable fetus. |
| Alanbay et al. [47] | 2016 | 1 | Endometrial thickness continuous with the central endometrial lining | 32 wk | Viable female fetus |
| Marfori et al. [48] | 2018 | 1 | Myometrial mantle at 5 mm throughout the pregnancy | 37 wk | Viable male fetus |
| Shekhar et al. [49] | 2010 | 1 | Thinned out with the potential of imminent Rupture | 30 wk | Asphyxiated female fetus delivered. |
| Martadiansyah et al. [50] | 2022 | 1 | Thin myometrium | 24 wk | A viable fetus was delivered but died soon after hysterotomy |
| Alves et al. [51] | 2011 | 1 | 3 mm myometrial layer | 36 wk | Viable female neonate |
| Kwon et al. [52] | 2011 | 2 | 2 mm myometrium fetus 1 Not reported for fetus 2 |
16 wk fetus1; 25 wk fetus2 | Both fetuses died after delivery. |
| Baldawa & Chaudhari et al. [53] | 2008 | 1 | Not reported | 14 wk | Right lateral wall uterine rupture; subtotal hysterectomy with right salpingectomy; fetus in the peritoneal cavity. |
Table 2.
Interstitial pregnancy case reports and sonographic features in the second or third trimester. (2000-2023) Search performed on February 10, 2023.
| Author | year | Number of cases | Myometrial thickness | Interstitial Line | Gestational age | Outcome |
|---|---|---|---|---|---|---|
| Hill et al.[54] | 2013 | 1 | Not reported | Not reported | 32 wk | Viable fetus |
| Valbo et al.[55] | 2008 | 1 | Not reported | Not reported | 22 wk | Fundal uterine rupture; subtotal hysterectomy; fetus status not reported |
| Najib et al. [56] | 2021 | 1 | Not reported | Not reported | 38 wk | Viable fetus |
| Nagayama et al. [57] | 2020 | 1 | Not reported | Not reported | 28 wk 1/7 d | Viable fetus |
| Pedroso et al. [58] | 2014 | 1 | Not reported | Not reported | 15 wk | Fetal demise |
| Nkurunziza et al. [59] | 2020 | 3 | Not reported | Not reported | 18 wk | Right interstitial pregnancy plus 2 intrauterine fetal demises; subtotal hysterectomy |
| Ahlschlager et al. [19] | 2021 | 1 | Not reported | Not reported | 15 wk 3 d | Left interstitial pregnancy |
| Scarella et al. [60] | 2012 | 1 | Reduced myometrial thickness | Not reported | 28 wk | Nonviable fetus |
| Dendas et al. [61] | 2017 | 2 | Not reported for interstitial pregnancy | Not reported | 16 wk 2 d | Viable one intrauterine fetus is delivered at 33 wk; Ruptured right uterine cornua with subsequent delivery of a fetus in the abdomen. |
| Noor & Alias. [62] | 2023 | 1 | Not reported | Not reported | 27 wk | Ruptured right interstitial; both mom and fetus died |
Table 3.
Cornual/rudimentary horn/malformed uterus pregnancy case reports and sonographic features in the second or third trimester (2000-2023). Search performed on February 10, 2023.
| Author | Year | Number of cases | Myometrial thickness | Pregnancy location/uterine anomaly | Gestational age | Outcome |
|---|---|---|---|---|---|---|
| Nash et al. [63] | 2020 | 1 | 1 mm (pathology) 6mm (MRI) |
Cornual region | 19 wk | Abdominal hysterectomy |
| Corte et al.[64] | 2019 | 1 | Not reported | Unicornuate with communicating rudimentary horn | 20 wk | Fetal demise; rudimentary horn excision; uterus anatomy restored. |
| Has et al.,[65] | 2002 | 1 | Not reported | Rudimentary horn | 13 wk | Ruptured rudimentary horn resection; fetal demise |
| Fekih et al. [66] | 2009 | 1 | Not reported | Rudimentary horn | 30 wks | Viable fetus |
| Brewer et al. [67] | 2005 | 1 | Not reported | Cornual | 28 wk 5/7 d | Uterine rupture; viable fetus |
| Shin & Kim [68] | 2005 | 1 | Not reported | Rudimentary horn | 34 wk | Viable fetus; rudimentary horn resection |
| Hassan et al. [69] | 2011 | 1 | Not reported | Rudimentary horn | 19 wk | Nonviable fetus |
| Wang et al. [70] | 2018 | 2 | Not reported | Cornual region | 33 wks, 3rd trimester (2nd case) | Fetal demise in both cases |
| Parveen, R [71] | 2019 | 1 | Not reported | Rudimentary horn; unicornuate association | 17 wk | Missed abortion; rudimentary horn resection |
| Nathan and Sornum [72] | 2013 | 1 | Not reported | Rudimentary horn; unicornuate association | 15 wk | Nonviable; right horn resection and salpingectomy |
| Kozar et al. [73] | 2020 | 1 | Not reported | Rudimentary horn | 14 wk | Nonviable; uterine and rudimentary horn rupture. |
| Zhang et al. [74] | 2020 | 1 | Not reported | Rudimentary horn | 38 wk | Viable fetus |
| Contreras et al. [75] | 2008 | 1 | Not reported | Rudimentary horn | 19 wk | Nonviable |
| Shahid et al. [76] | 2009 | 1 | Not reported | Rudimentary horn | 16 wk | Nonviable |
| Safiee & Ghazali [77] | 2021 | 1 | Not reported | Right cornual region | 19 wk 3 d | Live fetus; Pregnancy terminated |
| Ozeren et al. [78] | 2004 | 1 | Not reported | Rudimentary horn | 17 wk | Live fetus; Pregnancy terminated |
| Prenaud et al. [79] | 2017 | 1 | Not reported | Right Cornual region | Very early gestation | Right uterine rupture with salpingectomy; hemoperitoneal aspiration of the fetus. |
| Singh et al. [80] | 2015 | 1 | Not reported | Rudimentary horn | 20 wk | No Fetal heart rate was reported at the time of diagnosis |
| Lennox et al. [81] | 2013 | 1 | Not reported | Rudimentary horn | 16 wk | Pregnancy termination with rudimentary horn resection |
| Upadhyaya [82] | 2011 | 1 | Not reported | Rudimentary horn | 14 wk | Fetal demise; emergent laparotomy |
| Feteh et al. [83] | 2016 | 1 | Not reported | Right rudimentary horn of a unicornuate uterus | 42 wk 5 d | Fetal demise at 36 wk; excision of right with salpingectomy. |
| Kawthalkar et al.[84] | 2011 | 1 | Not reported | Left Unicornuate uterus with right noncommunicating rudimentary horn | 37 wk | Viable fetus; total hysterectomy |
| Fitzmaurice et al.[85] | 2010 | 1 | Not reported | Unicornuate; Right rudimentary horn | 24 wk 3 d | Fetal demise at delivery; hysterectomy 3 mo after c-section |
| Allouche et al. [86] | 2010 | 1 | Not reported | Noncommunicating rudimentary uterine horn | 26 wk | Viable fetus; hemihysterectomy |
| Arslan et al. [87] | 2009 | 1 | Not reported | Noncommunicating rudimentary horn | 37 wk | Viable fetus; rudimentary horn excision plus ipsilateral salpingectomy |
| Rajbhandary et al. [88] | 2020 | 1 | Not reported | Right Rudimentary horn of the unicornuate uterus | 15 wk | Nonviable fetus; ruptured rudimentary horn excision plus ipsilateral salpingectomy |
| Kuscu et al. [89] | 2002 | 1 | Not reported | Right rudimentary horn; unicornuate uterus | 15 wk | Ruptured rudimentary horn; emergency laparotomy; POC resected |
| Jerbi et al. [90] | 2005 | 1 | Not reported | Rudimentary horn | 18 wks | Excision of Ruptured rudimentary horn and ipsilateral salpingectomy; nonviable fetus. |
| Al Qarni et al. [91] | 2005 | 1 | Not reported | Left Rudimentary horn; bicornuate uterus. | 32 wks | Excision of left ruptured rudimentary horn with salpingectomy; alive fetus |
| Mishra et al. [92] | 2015 | 1 | Not reported | Left rudimentary horn; unicornuate uterus | 16 wks | Left rudimentary horn and ipsilateral salpingectomy excision; nonviable fetus |
| Stern el al. [93] | 2018 | 1 | Cornual pregnancy | 15 wks | Hysterectomy; nonviable fetus | |
| Jomaa et al. [94] | 2021 | 1 | Less than 2 mm | Left Rudimentary horn pregnancy; unicornuate association | 16 wk | Rudimentary horn and salpingectomy excision; nonviable fetus |
| Demishev et al. [95] | 2014 | 1 | Not reported | Left cornual region | 30 wk 4 d | Left cornual perforation; Viable fetus |
| Rana et al. [96] | 2008 | 1 | Not reported | Left rudimentary horn | 27 wk 5 d | Ruptured rudimentary horn and extrusion of fetus into abdomen and survival for 1 mo; ex uterine nonviability; excision of the horn. |
| Gaber-patel & Smith [97] | 2009 | 1 | Not reported | Right cornua of the uterus | 13 wk | Right cornual wedge resection; a nonviable fetus. |
| Thurber & Fleischer [98] | 2018 | 1 | Not reported | Right rudimentary horn | 19 wk 4 d | Horn resection; nonviable fetus |
| Cuppett et al. [99] | 2011 | 1 | Not reported | Right horn | 32 wk | Viable fetus |
| Goel et al. [100] | 2007 | 1 | Not reported | Unicornuate uterus; rudimentary horn | 41 wk 3 d | Viable fetus |
| Patra et al. [101] | 2007 | 1 | Not reported | Rudimentary horn | 37 wk | Viable fetus |
| Mitouarda et al. [102] | 2016 | 1 | Not reported | Left rudimentary horn | 28 wk | Viable fetus |
Discussion
A total of 61 case reports satisfied our inclusion criteria for ectopic pregnancy in the cornual region of the uterus. In the second and third trimesters, we assessed 11 and 10 case reports of angular and interstitial ectopic pregnancies, respectively. In contrast, cornual ectopic pregnancy included 40 case reports, constituting the majority of our search results. It is evident from the interstitial case reports that the sonographic “interstitial line” was not reported to be present in the second and third trimesters in all the studies and, thus is not helpful for the diagnosis. This further supports the argument that the interstitial line sign is only visible in the first trimester. In our search results, most articles described cornual ectopic pregnancies in the second and third trimesters. Most cornual ectopic pregnancy case reports describe gestation in the rudimentary horn of the uterus. In the case of angular pregnancy, 7 of the 11 case reports described the presence of the myometrium around the gestational sac, possibly due to its location within the endometrium. Hence, angular pregnancy carries the highest amount of myometrium around the gestational sac relative to interstitial and cornual ectopic pregnancy, achieving the most success for carrying the pregnancy to term.
Many authors feel uncomfortable with the notion that angular pregnancy is a type of ectopic pregnancy because it is eccentric and still in the endometrium [18]. Angular pregnancy, in essence, occurs within the endometrium; thus, technically, it does not fit the stringent definition of ectopic pregnancy. Therefore, it is expected that angular pregnancies are more successful in progressing to full-term pregnancies [9,25,30,35]. We believe that the distinction between interstitial and angular pregnancy becomes even more complicated when gestation enters the second trimester, as the interstitial line is lost [17]. Moawad et al. [9] suggested that interstitial pregnancy is occasionally referred to as cornual pregnancy and incorrectly confused with angular pregnancy. Early diagnosis of cornual or interstitial pregnancy is recommended by many authors to appropriately manage these pregnancies [33,34]. Gestational age is critical for managing cornual, interstitial or angular pregnancies. Angular pregnancy has the added advantage of being in the endometrium and having relatively more myometrial support than the other 2 types of ectopic pregnancies [18].
Interstitial pregnancies can continue to grow past the first trimester until they manifest life-threatening symptomatology later in pregnancy, especially in the second trimester [31]. It is unfortunate that none of the healthcare professionals were thinking about ectopic pregnancy in the cornual region in our patient. Timely diagnosis of this abnormal pregnancy would have prevented the patient from experiencing life-threatening hemorrhage or a worse prognosis. This case illustrates the need for clinicians to understand this dubious diagnosis in any pregnant woman presenting with complex symptomatology in the pelvic region, particularly during the second and third trimesters.
Moreover, it is regrettable that in this case, no alternative modality was considered to diagnose this complex second-trimester gestation, especially when ultrasound was equivocal despite the apparent clinical symptomatology in the patient. We speculate that MRI would have been very beneficial in diagnosing this pregnancy in the cornual region, potentially saving the patient from life-threatening hemorrhage. Three-dimensional sonography and MRI can help distinguish interstitial ectopic pregnancy from normal intrauterine pregnancy, particularly in the first trimester [34,36]. Judicious use of 2-D, 3-D and transvaginal ultrasound is vital to correctly diagnose each of the 3 types of pregnancies. If ultrasound findings are ambiguous or inconclusive, many authors recommend using MRI or, very rarely, a CT scan for such cases [19,37,38]. 3-D MRI has brought innovation to the diagnosis and distinction between angular and interstitial ectopic pregnancies [39].
Currently, medical and conservative surgical approaches are utilized to achieve the best outcomes of the 3 ectopic pregnancies in the cornual region of the uterus [20,40]. Surgical treatment is preferred in cases of pregnancy rupture, anemia, impending low blood pressure, gestational sac diameter > 4 cm on ultrasonography scan, or lower abdominal/pelvic pain that persists for more than 24 hours [41]. Laparotomy with cornual resection or hysterectomy is the most common surgical approach for ruptured interstitial pregnancies, especially after the first trimester [29,42]. In contrast to the past, because of advances in laparoscopic techniques, cornual resection, cornuostomy or hysteroscopic removal of ectopic interstitial tissue is performed laparoscopically [29]. Hysterectomy is generally considered acceptable in cases of life-threatening hemorrhage [22].
Strength and limitations
Based on a comprehensive literature search, we understand that our study is one of the few that concisely attempts to delineate some salient features separating cornual, interstitial and angular pregnancies in the second and third trimesters. Our case report reminds clinicians and technologists about the peculiarities and ambiguity involved in differentiating these 3 ectopic pregnancies in the cornual region of the uterus, especially after the first trimester. One of the shortcomings of our study is that we included only case reports and excluded all systematic reviews and larger case series. Moreover, we excluded all case reports published before 2000. The rationale behind choosing these inclusion and exclusion criteria is described in the Methodology section.
Conclusion
It is well known that there is ample confusion among radiologists and obstetricians regarding terminology surrounding ectopic pregnancy in the cornual region of the uterus. To remain consistent, we advocate using the term “cornual ectopic pregnancy” only for pregnancies involving uterine malformations. Regardless, any eccentric location of the gestational sac in the uterus should raise concerns among sonographers and radiologists for a potential angular, interstitial or cornual ectopic pregnancy. Hence, the first-trimester transvaginal scan is exceptionally critical for determining the exact type of ectopic pregnancy in the cornual region of the uterus. The first trimester is the only period in pregnancy when it is possible to establish subtle sonographic signs for the accurate diagnosis of ectopic pregnancy in the cornual region of the uterus. During the first trimester, it is vital to visualize the endometrium around the gestational sac in all the scanning planes. After the first trimester, the enlarging gestational sac inevitably obliterates the distinction between the 3 easily confused pregnancies in the cornual area, as mentioned above.
Furthermore, a transvaginal scan should be attempted if transabdominal scanning does not demonstrate communication between the internal cervical os and uterine cavity in the second trimester. The inability to extrapolate internal os to the uterine cavity should be perceived as a sonographic impression of a potential ectopic in the cornual region. Although ultrasound is the primary diagnostic radiological modality in pregnant patients, clinicians should not be afraid to explore other imaging modalities for the patient's benefit, especially when sonographic images are equivocal or inconclusive. Robust collaboration between sonographers, radiologists, and obstetricians is vital for the management of angular, interstitial and cornual pregnancies. We conclude that extreme caution should be exercised when diagnosing and differentiating angular, interstitial, or cornual pregnancy whenever the gestational sac is visualized in the cornual region of the uterus, preferably in the first trimester.
Author contributions
GD: conception and design of the study, literature review including analysis and interpretation of data, drafting the article, and revising the manuscript critically. AG: revising the manuscript critically for intellectual content and final approval before submission. LZ and RC: literature review and final approval of the manuscript. MF: revision and final approval of the manuscript. AB: obtained patient consent, revision, and final approval of the manuscript.
Patient consent
Written informed consent was obtained from the patient for this case study on January 17, 2023. The case study received formal approval from the Research Ethics and Compliance Committee (affiliated with the University of Manitoba) for publication, Dated: February 28, 2023, with the following REB number: REB Registry Number: H2023:043 (HS25876)
Footnotes
Acknowledgments: We acknowledge Dr Iain Kirkpatrick affiliated with the radiology section of the University of Manitoba, for providing insights into developing an appropriate title for our topic. We would also like to acknowledge all the staff, including radiologists, sonographers, and administrators at the prestigious St. Boniface Hospital, Winnipeg, Manitoba, for supporting us in publishing this case study and the literature review with Elsevier.
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2023.04.028.
Appendix A. Supplementary materials
References
- 1.Emery A, Buentipo B. Sonographic detection of cornual ectopic pregnancy. J Diagn Med Sonogr. 2008;24(4):252–256. [Google Scholar]
- 2.Marion L.L., Meeks G.R. Ectopic pregnancy: history, incidence, epidemiology, and risk factors. Clinical Obstet Gynecol. 2012;55(2):376–386. doi: 10.1097/GRF.0b013e3182516d7b. [DOI] [PubMed] [Google Scholar]
- 3.Nadi M, Richard C, Filipuzzi L, Bergogne L, Douvier S, Sagot P. Interstitial, angular and cornual pregnancies: diagnosis, treatment and subsequent fertility. Gynecol Obstet Fertil Senol. 2017;45(6):340–347. doi: 10.1016/j.gofs.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Finlinson A.R., Bollig K.J., Schust D.J. Differentiating pregnancies near the uterotubal junction (angular, cornual, and interstitial): a review and recommendations. Fertil Res Pract. 2020;6(1):8. doi: 10.1186/s40738-020-00077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gurgel Alves JA, Alves NG, Alencar Junior CA, Lucena Feitosa FE, Costa F da S. Term angular pregnancy: successful expectant management. J Obstet Gynaecol Res. 2011;37(6):641–644. doi: 10.1111/j.1447-0756.2010.01405.x. [DOI] [PubMed] [Google Scholar]
- 6.Slaoui A, Slaoui A, Zeraidi N, Lakhdar A, Kharbach A, Baydada A. Interstitial pregnancy is one of the most serious and uncommon ectopic pregnancies: case report. Int J Surg Case Rep. 2022;95:107195. doi: 10.1016/j.ijscr.2022.107195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Long Y, Zhu H, Hu Y, Shen L, Fu J, Huang W. Interventions for non-tubal ectopic pregnancy. Cochrane Database Syst Rev. 2020;7(7):CD011174. doi: 10.1002/14651858.CD011174.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baltarowich O.H. The term "Cornual Pregnancy" should be abandoned. JUltrasound Med. 2017;36(6):1081–1087. doi: 10.1002/jum.14207. [DOI] [PubMed] [Google Scholar]
- 9.Moawad NS, Mahajan ST, Moniz MH, Taylor SE, Hurd WW. Current diagnosis and treatment of interstitial pregnancy. Am J Obstet Gynecol. 2010;202(1):15–29. doi: 10.1016/j.ajog.2009.07.054. [DOI] [PubMed] [Google Scholar]
- 10.Biffi A., Damiani G.R., Pellegri A.M., Quartucci A., Di Gennaro D., Boca G.D. Cornual pregnancy. J Minim Invas Gynecol. 2022;29(3):327–328. doi: 10.1016/j.jmig.2021.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Santos L.T.R., Oliveira S.C., de S., Rocha L.G.A., Sousa N.D.S., Figueiredo R.de S. Interstitial Pregnancy: case report of atypical ectopic pregnancy. In Cureus. 2020;12(5) doi: 10.7759/cureus.8081. e8081–e8081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rathod S., Samal S. A true cornual pregnancy with placenta percreta resulting in a viable fetus. Int J Appl Basic Med Res. 2015;5(3):203–205. doi: 10.4103/2229-516X.165364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Babu K., De J. Rupture of rudimentary horn pregnancy. Med J. Armed Forces India. 2007;63(1):75–76. doi: 10.1016/S0377-1237(07)80119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maher P.J., Grimwade J.C. Cornual pregnancy ... diagnosis before rupture a report of 2 cases. Aust NZ J Obstet Gynaecol. 1982;22(3):172–174. doi: 10.1111/j.1479-828X.1982.tb01437.x. [DOI] [PubMed] [Google Scholar]
- 15.Nikodijevic K., Bricou A., Benbara A., Moreaux G., Nguyen C., Carbillon L., et al. Cornual pregnancy: management and subsequent fertility. Gynécol Obstét Fertil. 2016;44(1):11–16. doi: 10.1016/j.gyobfe.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 16.Mokashi T., Dutta S., Das S. VP59.31: Interstitial pregnancy a diagnostic dilemma with favourable surgical outcomes. Ultrasound Obstet Gynecol. 2020;56(S1):322. doi: 10.1002/uog.23314. [DOI] [Google Scholar]
- 17.Cordeiro D.E.F., Alves J.A.G., Feitosa F.E.L. Interstitial and angular pregnancies: Case reports and differential diagnosis. The Journal of Obstetrics and Gynaecology Research. 2018;44(10):1999–2002. doi: 10.1111/jog.13748. [DOI] [PubMed] [Google Scholar]
- 18.Arleo E.K., DeFilippis E.M. Cornual, interstitial, and angular pregnancies: clarifying the terms and a review of the literature. Clin Imag. 2014;38(6):763–770. doi: 10.1016/j.clinimag.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 19.Ahlschlager L.M., Mysona D., Beckham A.J. The elusive diagnosis and emergent management of a late-presenting ruptured interstitial pregnancy: a case report. BMC Pregn Childbirth. 2021;21(1):553. doi: 10.1186/s12884-021-04026-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ackerman T.E., Levi C.S., Dashefsky S.M., Holt S.C., Lindsay D.J. Interstitial line: sonographic finding in interstitial (cornual) ectopic pregnancy. Radiology. 1993;189(1):83–87. doi: 10.1148/radiology.189.1.8372223. [DOI] [PubMed] [Google Scholar]
- 21.Jiang L.-Y., Wang P.-H. Interstitial pregnancy: cornuostomy or wedge resection? J Chin Med Assoc. 2019;82(3):167–168. doi: 10.1097/JCMA.0000000000000072. [DOI] [PubMed] [Google Scholar]
- 22.Bahall V., Cozier W., Latchman P., Elias S.-A., Sankar S. Interstitial ectopic pregnancy rupture at 17 weeks of gestation: a case report and literature review. Case Rep Women's Health. 2022;36:e00464. doi: 10.1016/j.crwh.2022.e00464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jansen R.P.S., Elliott P.M. Angular Intrauterine Pregnancy. Obstet Gynecol (New York. 1953) 1981;58(2):167–175. [PubMed] [Google Scholar]
- 24.Meichen Y., Jing F., Lingyun Z., Jianwei Z. Two cases of angular pregnancy with incomplete abortion treated with hysteroscopy: a case report and review of literature. BMC Surg. 2021;21(1):76. doi: 10.1186/s12893-021-01077-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Durand Y.G., Capoccia-Brugger R., Vial Y., Balaya V. Diagnostic dilemma between angular and interstitial ectopic pregnancy: 3D ultrasound features. J Ultrasound. 2022;25(4):989–994. doi: 10.1007/s40477-022-00668-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lau S., Tulandi T. Conservative medical and surgical management of interstitial ectopic pregnancy. Fertil Steril. 1999;72(2):207–215. doi: 10.1016/S0015-0282(99)00242-3. [DOI] [PubMed] [Google Scholar]
- 27.Malinowski A., Bates S.K. Semantics and pitfalls in the diagnosis of cornual/interstitial pregnancy. Fertil Steril. 2006;86(6):1764.e11–1764.e14. doi: 10.1016/j.fertnstert.2006.03.073. [DOI] [PubMed] [Google Scholar]
- 28.Nakatsuka E., Mimura K., Endo M., Miyake T., Kakigano A., Matsuzaki S., et al. Conservative management for adherent placenta after live birth in angular or interstitial pregnancies: a new entity "angular placenta attachment". Taiwanese J Obstet Gynecol. 2020;59(6):975–979. doi: 10.1016/j.tjog.2020.09.033. [DOI] [PubMed] [Google Scholar]
- 29.Faraj R., Steel M. Management of cornual (interstitial) pregnancy. Obstet Gynaecol. 2007;9(4):249–255. doi: 10.1576/toag.9.4.249.27355. [DOI] [Google Scholar]
- 30.D'hoore E., D'hoore L., Van den Berghe S., Roets E., van Wessel S., Hamerlynck T. Operative hysteroscopy in the minimally invasive management of interstitial pregnancy and interstitially retained products of conception: a case report and systematic literature review. Eur J Obstet Gynecol Reprod Biol. 2021;265:54–59. doi: 10.1016/j.ejogrb.2021.07.025. [DOI] [PubMed] [Google Scholar]
- 31.Laus K., Louis P., Douglass L. A novel approach to management of angular pregnancies: a case series. J Minim Invas Gynecol. 2019;26(1):178–181. doi: 10.1016/j.jmig.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Soriano David, Vicus Danielle, Mashiach Roy, Schiff Eyal, Seidman Daniel, Goldenberg Motti. Laparoscopic treatment of cornual pregnancy: a series of 20 consecutive cases. Fertil Steril. 2008;90(3):839–843. doi: 10.1016/j.fertnstert.2007.07.1288. [DOI] [PubMed] [Google Scholar]
- 33.Dagar M., Srivastava M., Ganguli I., Bhardwaj P., Sharma N., Chawla D. Interstitial and cornual ectopic pregnancy: conservative surgical and medical management. J Obstet Gynaecol India. 2018;68(6):471–476. doi: 10.1007/s13224-017-1078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sherer D.M., Roach C., Gerren A., Granderson F., Kheyman M., Dalloul M. Sonographic diagnosis of an interstitial pregnancy in an asymptomatic patient at 7 weeks' gestation. Radiol Case Rep. 2022;17(12):4850–4854. doi: 10.1016/j.radcr.2022.08.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tulandi T., Monton L. Conservative surgical management of interstitial pregnancy. Fertility and Sterility. 1990;53(3):581. doi: 10.1016/S0015-0282(16)53364-0. [DOI] [PubMed] [Google Scholar]
- 36.Dibble E.H., Lourenco A.P. Imaging unusual pregnancy implantations: rare ectopic pregnancies and more. Am J Roentgenol (1976) 2016;207(6):1380–1392. doi: 10.2214/AJR.15.15290. [DOI] [PubMed] [Google Scholar]
- 37.Kao L.Y., Scheinfeld M.H., Chernyak V., Rozenblit A.M., Oh S., Dym R.J. Beyond ultrasound: CT and MRI of ectopic pregnancy. Am J Roentgenol (1976) 2014;202(4):904–911. doi: 10.2214/AJR.13.10644. [DOI] [PubMed] [Google Scholar]
- 38.Tsafrir A., Rojansky N., Sela H.Y., Gomori J.M., Nadjari M. Rudimentary horn pregnancy: first trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med. 2005;24(2):219–223. doi: 10.7863/jum.2005.24.2.219. [DOI] [PubMed] [Google Scholar]
- 39.Gao F., Sun M., Fu L. The role of three-dimensional MRI in the differentiation between angular pregnancy and interstitial pregnancy. BMC Pregn Childbirth. 2022;22(1):133. doi: 10.1186/s12884-022-04470-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Capmas Perrine, Bouyer J., Fernandez Hervé. Treatment of ectopic pregnancies in 2014: new answers to some old questions. Fertil Steril. 2014;101(3):615–620. doi: 10.1016/j.fertnstert.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 41.Rana P., Kazmi I., Singh R., Afzal M., Al-Abbasi F.A., Aseeri A., et al. Ectopic pregnancy: a review. Arch Gynecol Obstet. 2013;288(4):747–757. doi: 10.1007/s00404-013-2929-2. [DOI] [PubMed] [Google Scholar]
- 42.Siow Anthony, Ng Selma. Laparoscopic management of 4 cases of recurrent cornual ectopic pregnancy and review of literature. J Minim Invas Gynecol. 2011;18(3):296–302. doi: 10.1016/j.jmig.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 43.Mustafa N, Mushtaq Q, Bilal Shah SM. Angular pregnancy: an eccentric implantation within uterine cavity. J Ayub Med Coll Abbottabad JAMC. 2021;33(4):702–703. [PubMed] [Google Scholar]
- 44.Cruz Martínez R, García Salazar N, Manzanares G. [Non-broken, angular, and ectopic pregnancy of 22 weeks. Case report and literature review] Ginecol Obstet Mex. 2008;76(7):417–420. [PubMed] [Google Scholar]
- 45.Yao F.X., Fan Y.F., Shao L.N., Miao P., Ding H.Q., Yang M. The dilemmas in the diagnosis and management of angular pregnancy. Taiwanese J Obstet Gynecol. 2021;60(3):582–583. doi: 10.1016/j.tjog.2021.03.040. [DOI] [PubMed] [Google Scholar]
- 46.Hasanzadeh M., Dadgar S., Arian Y., Yousefi Y. Angular ectopic pregnancy presenting as rupture of lateral wall of the uterus: late presentation in gestation week 20. Iran J Med Sci. 2017;42(3):314–317. [PMC free article] [PubMed] [Google Scholar]
- 47.Alanbay İbrahim, Öztürk M., Karaşahin K.E., Yenen M.C. Angular pregnancy. J Turkish Soc Obstet Gynecol. 2016;13(4):218–220. doi: 10.4274/tjod.42402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marfori C.Q., Kotzen M. Angular vs. interstitial pregnancy: a case report highlighting diagnostic nuances with stark management differences. Case Rep Womens Health [Internet] 2018;19 doi: 10.1016/j.crwh.2018.e00068. http://www.journals.elsevier.com/case-reports-in-womens-health/ (Marfori, Kotzen) Department of Obstetrics&Gynecology, The George Washington University, 2150 Pennsylvania Ave NW, Suite 6A, Washington, DC 20037, United States):e00068. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shekhar S., Verma S., Motey R., Kaushal R. Hysterotomy for retained placenta with imminent uterine rupture in a preterm angular pregnancy. Acta obstetricia et gynecologica Scandinavica. 2010;89(12):1615–1616. doi: 10.3109/00016349.2010.516354. [DOI] [PubMed] [Google Scholar]
- 50.Martadiansyah A., Bernolian N., Mirani P., Lestari P.M., Dewi C., Pangemanan W.T., et al. Placenta accreta spectrum disorder in a primigravida with angular pregnancy: a case report. Med J Indonesia. 2022;31(2):126–131. doi: 10.13181/mji.cr.226011. [DOI] [Google Scholar]
- 51.Alves J.A.G., Alves N.G., Alencar Júnior C.A., Feitosa F.E.L., da Silva Costa F. Term angular pregnancy: successful expectant management. J Obstet Gynaecol Res. 2011;37(6):641–644. doi: 10.1111/j.1447-0756.2010.01405.x. [DOI] [PubMed] [Google Scholar]
- 52.Kwon J.Y., Hwang S.J., Shin J.E., Yoon W.S., Shin J.C., Park I.Y. Two cases of angular pregnancy complicated by preterm labor and placental abruption at mid-pregnancy. J Obstet Gynaecol Res. 2011;37(7):958–962. doi: 10.1111/j.1447-0756.2010.01460.x. [DOI] [PubMed] [Google Scholar]
- 53.Baldawa P.S., Chaudhari H.K. Angular ectopic pregnancy presenting as rupture of lateral wall of the uterus. J Human Reprod Sci. 2008;1(1):33–34. doi: 10.4103/0974-1208.38970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hill A.J., Van Winden K.R., Cook C.R. A True Cornual (Interstitial) Pregnancy Resulting in a Viable Fetus. Obstet Gynecol (New York. 1953) 2013;121(2):427–430. doi: 10.1097/AOG.0b013e3182677a10. Part 2. [DOI] [PubMed] [Google Scholar]
- 55.Valbø A., Langeland J.P., Lobmaier I.V.K. A woman in the second trimester of pregnancy with acute abdominal pain. Tidsskrift for den Norske Lægeforening. 2008;128(19):2198–2199. [PubMed] [Google Scholar]
- 56.Najib F.S., Vafaei H., Foroughi A.A., Namazi N. Diagnosis pitfall of interstitial pregnancy: a case report of a term pregnancy with abnormal placentation. BMC Pregn Childbirth. 2021;21(1):699–705. doi: 10.1186/s12884-021-04153-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nagayama S., Takahashi H., Tozawa S., Narumi R., Usui R., Ohkuchi A., Matsubara S. Interstitial pregnancy in the third trimester with severe preeclampsia: a case report and literature review. Case Rep Obstet Gynecol. 2020;2020:9408501–9408505. doi: 10.1155/2020/9408501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pedroso C, Lermann R, Amaral N, Condeço P. Interstitial pregnancy rupture at 15 weeks of pregnancy. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-203979. bcr2014203979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nkurunziza C., Rurangwa T., Ngendahimana V., Magriples U. Second trimester heterotopic triplet pregnancy with intrauterine twin pregnancy and ruptured interstitial pregnancy: a maternal near-miss case report. Case Rep Obstet Gynecol. 2020;2020 doi: 10.1155/2020/5240848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Scarella A., Marquez R., Schilling H., Palomino A. Antenatal diagnosis of a third trimester interstitial pregnancy: A case report. J Obstet Gynaecol Res. 2012;38(3):570–573. doi: 10.1111/j.1447-0756.2011.01750.x. [DOI] [PubMed] [Google Scholar]
- 61.Dendas W., Schobbens J.-C., Mestdagh G., Meylaerts L., Verswijvel G., Van Holsbeke C. Management and outcome of heterotopic interstitial pregnancy: case report and review of literature. Ultrasound. 2017;25(3):134–142. doi: 10.1177/1742271X17710965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mohd Noor M.S., Zamaliana Alias W.Z. Ruptured interstitial pregnancy: a case report of a sudden maternal death in the late second trimester from a rare cause. Pathology. 2023;55 doi: 10.1016/j.pathol.2022.12.297. S89–S89. [DOI] [Google Scholar]
- 63.Nash C., Fortuna T., Schollenberg E., Rittenberg D. A 20-week cornual ectopic pregnancy. J Obstet Gynaecol Canada. 2020;42(12):1455. doi: 10.1016/j.jogc.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 64.Della Corte L., Fabozzi A., Giampaolino P., Saccone G., Pizzuti L.M., Romeo V., et al. A case of 20-week abortion in a rare communicating rudimentary horn of a misinterpreted unicornuate uterus, incorrectly diagnosed as bicornuate: A serious hazard. Eur J Obstet Gynecol Reprod Biol. 2019;235:133–135. doi: 10.1016/j.ejogrb.2019.02.018. [DOI] [PubMed] [Google Scholar]
- 65.Has R., Ermis H., Yildirim A. A malformed fetus in a rudimentary uterine horn pregnancy. Ultrasound Obstet Gynecol. 2000;16(2):200–202. doi: 10.1046/j.1469-0705.2000.00207.x. [DOI] [PubMed] [Google Scholar]
- 66.Meriem F., Anis M., Sonia N., Lassad B.R., Sassi B., Habib E., et al. Asymptomatic horn rudimentary pregnant uterine rupture with a viable fetus. Tunisie Med. 2009;87(9):633–636. [PubMed] [Google Scholar]
- 67.Brewer H., Gefroh S., Bork M., Munkarah A., Hawkins R., Redman M.E. Asymptomatic uterine rupture of a cornual pregnancy in the third trimester: A case report. J Reprod Med. 2005;50(9):715–718. [PubMed] [Google Scholar]
- 68.Shin J.W., Kim H.J. Case of live birth in a noncommunicating rudimentary horn pregnancy. J Obstet Gynaecol Res. 2005;31(4):329–331. doi: 10.1111/j.1447-0756.2005.00296.x. [DOI] [PubMed] [Google Scholar]
- 69.Hassan C.H.C., Karim A.K.A., Ismail N.A.M., Omar M.H. Case report of ruptured noncommunicating right rudimentary horn pregnancy: an acute emergency. Acta Medica Lékarskí Fakulty Univerzity Karlovy v Hradci Králove. 2011;54(3):125–126. doi: 10.14712/18059694.2016.34. [DOI] [PubMed] [Google Scholar]
- 70.Wang S., Zhang Y., Zhao Y.Y., Lu S. Cornual pregnancy in 2 cases. Beijing da xue xue bao. J Peking University. Yi xue ban. 2018;50(3):576–579. [PubMed] [Google Scholar]
- 71.Parveen R. Detection and management of pregnancy in rudimentary horn of uterus. J Coll Physic Surg–Pakistan : JCPSP. 2019;29(6):S70–S72. doi: 10.29271/jcpsp.2019.06.S70. [DOI] [PubMed] [Google Scholar]
- 72.Nathan H., Sornum A. Diagnosis and management of a ruptured rudimentary horn pregnancy in a low-resource setting. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-009957. bcr2013009957–bcr2013009957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kozar N., Serdinšek T., Tašner T., Reljič M., Gavrić Lovrec V., Kovač V. Diagnosis and management of rudimentary horn pregnancy rupture, misinterpreted as bicornuate uterus in the 14th week of pregnancy. J Obstet Gynaecol Res. 2021;47(2):843–846. doi: 10.1111/jog.14586. [DOI] [PubMed] [Google Scholar]
- 74.Zhang Y., Pang Y., Zhang X., Zhao Z., Liu P. Full-term pregnancy in a rudimentary horn with a live fetus: a case report. Medicine (Baltimore) 2020;99(34) doi: 10.1097/MD.0000000000021604. e21604–e21604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Contreras Karenrose R., Rothenberg Jeffrey M., Kominiarek Michelle A., Raff Gregory J. Hand-assisted laparoscopic management of a midtrimester rudimentary horn pregnancy with placenta increta: a case report and literature review. J Minim Invas Gynecol. 2008;15(5):644–648. doi: 10.1016/j.jmig.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 76.Shahid A., Olowu O., Kandasamy G., O'Donnell C., Odejinmi F. Laparoscopic management of a 16-week ruptured rudimentary horn pregnancy: a case and literature review. Arch Gynecol Obstet. 2010;282(2):121–125. doi: 10.1007/s00404-009-1212-z. [DOI] [PubMed] [Google Scholar]
- 77.Safiee A., Ghazali W. Laparoscopic wedge resection in a late second trimester cornual pregnancy. Gynecol Minim Invas Ther. 2021;10(1):47–49. doi: 10.4103/GMIT.GMIT_22_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ozeren S., Caliskan E., Corakci A., Ozkan S., Demirci A. Magnetic resonance imaging and angiography for the prerupture diagnosis of rudimentary uterine horn pregnancy. Acta Radiologica (1987) 2004;45(8):878–881. doi: 10.1080/02841850410008252. [DOI] [PubMed] [Google Scholar]
- 79.Prenaud C., Scherier S., Malgras B. Management of a cornual ectopic pregnancy. J Visc Surg. 2017;154(6):467–468. doi: 10.1016/j.jviscsurg.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 80.Singh P., Gupta R., Das B., Bajaj S.K., Misra R. Midtrimester spontaneous torsion of unruptured gravid rudimentary horn: Presurgical diagnosis on magnetic resonance imaging. J Obstet Gynaecol Res. 2015;41(9):1478–1482. doi: 10.1111/jog.12722. [DOI] [PubMed] [Google Scholar]
- 81.Lennox Genevieve, Pantazi Sophia, Keunen Johannes, Van Mieghem Tim, Allen Lisa. Minimally invasive surgical management of a second trimester pregnancy in a rudimentary uterine horn. J Obstet Gynaecol Canada. 2013;35(5):468–472. doi: 10.1016/S1701-2163(15)30938-5. [DOI] [PubMed] [Google Scholar]
- 82.Upadhyaya I. Non-communicating rudimentary uterine horn pregnancy. J Nepal Med Assoc. 2011;51(4):199–202. doi: 10.31729/jnma.31. [DOI] [PubMed] [Google Scholar]
- 83.Feteh V.F., Dimala C.A., Njim T., Fuka B. Post term pregnancy in a noncommunicating rudimentary horn of a unicornuate uterus. BMC Res Notes. 2016;9(1):209. doi: 10.1186/s13104-016-2013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kawthalkar A.S., Gawande M.S., Jain S.H., Joshi S.A., Ghike S.D., Bhalerao A.V. Rare case of live birth in a ruptured rudimentary horn pregnancy. J Obstet Gynaecol Res. 2011;37(8):1169–1172. doi: 10.1111/j.1447-0756.2010.01497.x. [DOI] [PubMed] [Google Scholar]
- 85.Fitzmaurice Laura E., Ehsanipoor Robert M., Porto Manuel. Rudimentary horn pregnancy with herniation into the main uterine cavity. Am J Obstet Gynecol. 2010;202(3):e5–e6. doi: 10.1016/j.ajog.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 86.Allouche M., Tanguy le Gac Y., Parant O. Rudimentary horn pregnancy: an unusual cause of spontaneous hemoperitoneum during the second-trimester of pregnancy. Gynécol, Obstét Fertilité. 2011;39(2):e44–e46. doi: 10.1016/j.gyobfe.2010.08.032. [DOI] [PubMed] [Google Scholar]
- 87.Arslan Tonguç, Bilgiç Ergün, Şentürk M.Baki, Yücel Neşe. Rudimentary uterine horn pregnancy: a mystery diagnosis. Fertil Steril. 2009;92(6):2037.e1–2037.e3. doi: 10.1016/j.fertnstert.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 88.Rajbhandary S., Das A., Rai M., Sah A.K. Rupture of noncommunicating rudimentary horn pregnancy at 15 weeks with previous normal pregnancies: a case report. JNMA; J Nepal Med Assoc. 2020;58(228):614–617. doi: 10.31729/jnma.5104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kuşcu N.K., Laçin S., Kartal Özgür, Koyuncu F. Rupture of rudimentary horn pregnancy at the 15th week of gestation: a case report. Eur J Obstet Gynecol Reprod Biol. 2002;102(2):209–210. doi: 10.1016/S0301-2115(01)00600-5. [DOI] [PubMed] [Google Scholar]
- 90.Jerbi M., Trimech A., Choukou A., Hidar S., Bibi M., Chaieb A., et al. Rupture of rudimentary horn pregnancy at the 18th week of gestation: a case report. Gynécol, Obstét Fertilité. 2005;33(7-8):505–507. doi: 10.1016/j.gyobfe.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 91.Al Qarni A.A., Al-Braikan N., Al-Hanbali M.M., Alharmaly A.H. Rupture rudimentary horn pregnancy at 31 week. Saudi Med J. 2017;38(2):201–203. doi: 10.15537/smj.2017.2.16016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mishra N., Yadav N., Koshiya D., Jhanwar V. Ruptured rudimentary horn pregnancy with a history of an uneventful vaginal delivery. J MedUltras (2001) 2015;42(1):117–120. doi: 10.1007/s10396-014-0582-4. [DOI] [PubMed] [Google Scholar]
- 93.Stern E., Chanda M., Thorne J. Rupturing cornual pregnancy diagnosed at laparoscopy. J Obstet Gynecol Canada. 2019;41(3):265. doi: 10.1016/j.jogc.2017.11.038. [DOI] [PubMed] [Google Scholar]
- 94.Jomaa S., Ahmad A., Adwan D. Successful diagnosis and management of prerupture rudimentary horn pregnancy in the second trimester: a case report. Radiol Case Rep. 2021;16(10):3068–3071. doi: 10.1016/j.radcr.2021.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Demishev M., Avila C., Figueroa R., Hellinger J.C., Ogburn P. Successful pregnancy outcome after conservative management of second-trimester cornual uterine rupture. J Ultrasound Med. 2014;33(11):2037–2046. doi: 10.7863/ultra.33.11.2037. [DOI] [PubMed] [Google Scholar]
- 96.Rana A, Gurung G, Rawal S, Bista KD, Adhukari S, Ghimire RK. Surviving 27 weeks fetus expelled out of the ruptured rudimentary horn and detected a month later as a secondary abdominal pregnancy. J Obstet Gynaecol Res. 2008;34(2):247–251. doi: 10.1111/j.1447-0756.2008.00763.x. [DOI] [PubMed] [Google Scholar]
- 97.Gaber-Patel Karen, Smith Michael D. Thirteen-week cornual ectopic pregnancy. Am J Emerg Med. 2009;27(7):900.e1–900.e2. doi: 10.1016/j.ajem.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 98.Thurber B.W., Fleischer A.C. Ultrasound features of rudimentary horn ectopic pregnancies. J Ultrasound Med. 2019;38(6):1643–1647. doi: 10.1002/jum.14847. [DOI] [PubMed] [Google Scholar]
- 99.Cuppett C.D., Stitely M.L., Toffle R.C. Unruptured 32-week rudimentary horn pregnancy presenting as right upper quadrant pain. West Virginia Med J. 2011;107(4):8–10. [PubMed] [Google Scholar]
- 100.Goel Poonam, Saha PradipKumar, Mehra Reeti, Huria Anju. Case Report-Unruptured postdated pregnancy with a live fetus in a noncommunicating rudimentary horn. Indian J Med Sci. 2007;61(1) [PubMed] [Google Scholar]
- 101.Patra S., Puri M., Trivedi S.S., Yadav R., Bali J. Unruptured term pregnancy with a live fetus with placenta percreta in a noncommunicating rudimentary horn. Congen Anomal. 2007;47(4):156–157. doi: 10.1111/j.1741-4520.2007.00163.x. [DOI] [PubMed] [Google Scholar]
- 102.Le Mitouard M, Huissoud C, Fichez A, Roumieu F, Allias F, Rudigoz RC, et al. [Uterine rupture plugged by omentum in a rudimentary horn pregnancy: About a rare case] J Gynecol Obstet Biol Reprod (Paris) 2016;45(5):521–524. doi: 10.1016/j.jgyn.2016.02.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.