Abstract
Background
The federal Earned Income Tax Credit (EITC) is the primary income support program for low-income workers in the U.S., but its design may hinder its effectiveness when poor health limits, but does not preclude, work.
Methods
Cross-sectional analysis of nationally-representative U.S. Census Current Population Survey (CPS) data covering 2019. Working-age adults eligible to receive federal EITC were included in this study. Poor health, as indicated by self-report of at least one problem with hearing, vision, cognitive function, mobility, dressing and bathing, or independence, was the exposure. The main outcome was federal EITC benefit category, categorized as no benefit, phase-in (income too low for the maximum benefit), plateau (maximum benefit), phase-out (income above threshold for maximum benefit), or earnings too high to receive any benefit. We estimated EITC benefit category probabilities by health status using multinomial logistic regression. We further examined whether other government benefits provided additional income support to those in poor health.
Results
41,659 participants (representing 87.1 million individuals) were included. 2,724 participants (representing 5.6 million individuals) reported poor health. In analyses standardized over age, gender, race, and ethnicity, those in poor health, compared with those not in poor health, were more likely to be in the no benefit (2.40% vs. 0.30%, risk difference 2.10 percentage points [95%CI 1.75 to 2.46 percentage points]), and phase-in (9.28% vs. 2.74%, risk difference 6.54 percentage points [95%CI 5.82 to 7.26 percentage points]) categories. Differences in resources by health status persisted even after accounting for other government benefits.
Conclusions
EITC program design creates an important gap in income support for those for whom poor health limits work, which is not closed by other programs. Filling this gap is an important public health goal.
Keywords: Socioeconomic factors, Earned income tax credit, Social policy, Social insurance, Health equity
Highlights
-
•
The earned income tax credit (EITC) is the primary income support program for low-income working families.
-
•
EITC uses a ‘phase-in’ design, meaning lower earners do not receive maximum benefits.
-
•
This could create a gap in income support when poor health lessens, but does not eliminate the ability to work.
-
•
In nationally-representative data, those with EITC benefits in the ‘phase-in’ range were disproportionately in poor health.
-
•
Moreover, other income support programs did not make up the difference.
1. Introduction
Given the close connection between income and health, income support programs can improve health for lower income Americans(Aizer, Hoynes, & Lleras-Muney, 2022; Arno, House, Viola, & Schechter, 2011; Matthew & Brodersen, 2018; Sherman, DeBot, & Huang, 2016). The federal Earned Income Tax Credit (EITC), meant to encourage paid labor, is the primary income support program for low-wage workers in the U.S., distributing $62 billion in benefits to over 25 million workers in 2019(Statistics for Tax Returns with the Earned Income Tax Credit (EITC) | Earned Income Tax Credit, n.d.). Further, evidence suggests that federal EITC is associated with improved health, particularly maternal and child health(Arno, Sohler, Viola, & Schechter, 2009; Averett & Wang, 2018; Batra, Karasek, & Hamad, 2022; Batra & Hamad, 2021; Boyd-Swan, Herbst, Ifcher, & Zarghamee, 2016; Chetty & Friedman, 2011; Collin et al., 2021; Courtin, Aloisi, et al., 2020; Courtin et al., 2018; Courtin, Kim, Song, Yu, & Muennig, 2020; Duncan & Murnane, 2016; Evans & Garthwaite, 2014; Halpern-Meekin, Greene, Levin, & Edin, 2018; Hamad & Rehkopf, 2015; Hoynes, Miller, & Simon, 2015; Markowitz, Komro, Livingston, Lenhart, & Wagenaar, 2017; Muennig, Mohit, Wu, Jia, & Rosen, 2016; Rehkopf, Strully, & Dow, 2014; Simon et al., 2018).
For those whose poor health prevents Substantial Gainful Activity(Substantial Gainful Activity, n.d.), social insurance in the form of disability income, such as Social Security Disability Income (SSDI) or Supplemental Security Income (SSI), can provide needed income support(Brucker & Garrison, 2021). Although administrative barriers mean that many who might qualify do not receive disability income(Deshpande & Li, 2019), the income support system overall is designed to address this situation.
However, disability income is typically not available for those whose poor health limits but does not preclude the ability to work. This could represent an important gap in the income support system. EITC is seemingly well-positioned to fill this gap, as EITC is explicitly intended as an income supplement for those with low, but some, earnings. However, aspects of EITC design may hinder rather than help those in poor health. Two relatively unique features of EITC, compared with other income support programs that help individuals in similar income ranges, such as SNAP (Supplemental Nutrition Assistance Program) and TANF (Temporary Assistance to Needy Families), are that EITC is ‘income-tested’ (individuals are required to have earnings to receive any benefits), and that benefits ‘phase-in’, or initially increase as earnings increase. The idea is that this structure incentivizes labor force participation. Indeed, several studies, although not all, find support for the idea that EITC increases labor force participation among single parent households with lower educational attainment (Jones & Ziliak, 2019; Kleven, 2019; Rothstein, 2010; Whitmore Schanzenbach & Strain, 2021). However, this benefit design comes with a trade-off: those with the lowest income receive the least income support. Thus a potential unintended consequence of the phase-in design may be that those in the phase-in range are disproportionately people whose earnings are limited, not by lack of incentive, but by poor health. This could set up a vicious cycle, or ‘poverty-health trap’, whereby poor health worsens the ability to earn income, and low earnings combined with a gap in income support policies further worsen health(Khullar & Chokshi, 2018). Such a cycle has been observed, for example, in the case of food insecurity, which is one mechanism linking low income and worse health(Johnson, Palakshappa, Basu, Seligman, & Berkowitz, 2021; Weinstein, Kahkoska, & Berkowitz, 2022).
Whether these potential problems with EITC occur in practice is important to understand, as EITC is the main federal income support program for low-income workers. Further, the debate over benefit design has been rekindled by recent reforms to the Child Tax Credit (CTC). For much of its history, the CTC had a phase-in structure similar to EITC(What's New with theChild Tax Creditafter Tax Reform | Internal Revenue Service, n.d.). Reforms in 2021 abandoned the phase-in in favor of a uniform benefit level for lower-income families based only on the number and age of qualifying dependents. These reforms have since expired, and further changes are a current topic of legislative discussion (Child Tax Credit, n.d.; What's New with theChild Tax Creditafter Tax Reform | Internal Revenue Service, n.d.).
Concerns about federal EITC highlight two important research questions that, to our knowledge, remain unanswered: 1) to what extent, especially among those with some earnings, is poor health associated with being in the phase-in part of the federal EITC benefit structure?; and 2) to what extent do other federal programs make up for possibly lower income support from EITC among those in poor health? These questions are the focus of this study. We hypothesized that 1) those in poor health would be represented disproportionately in the phase-in part of the EITC benefit structure, and 2) other programs would not fully make up the difference, resulting in lower overall resource levels for those individuals with poor health.
2. Materials and methods
2.1. Data source, setting, and study sample
This cross-sectional study used data from the 2020 Annual Social and Economic Supplement (ASEC) of the U.S. Census Bureau and Bureau of Labor Statistics’ Current Population Survey (CPS)(US Census Bureau, n.d.-a). These data covered the tax year 2019 and are the most recent data prior to economic disruption from the COVID-19 pandemic. The Current Population Survey is a nationally-representative survey designed to estimate labor force statistics for the U.S. population.
In studies of income, the household is the unit across which resources are pooled and, often, benefits are calculated. For this study, we defined the household as the ASEC ‘resource unit’, which is used to calculate the Supplemental Poverty Measure (SPM). The estimated EITC benefit is calculated at this household level. To avoid correlation issues within households and possible ‘doubling counting’ of shared benefits, we included only one individual per SPM resource unit—the person identified as the head of the SPM household. For this reason, we refer to individuals rather than SPM resource units as the unit of analysis. To focus on working-age adults potentially eligible for EITC, we restricted the sample to individuals aged between 18 and 64 years. Further, we excluded those under age 25 without dependents, because they are not eligible for EITC per IRS regulations for tax year 2019(Internal Revanue Service, n.d., p. 596).
The University of North Carolina at Chapel Hill institutional review board did not consider these analyses of de-identified data to constitute human subjects research.
2.2. Indicators of poor health
The primary exposure in this study was poor health, defined as a composite of the presence of any one of six health indicators that federal surveys include under the Affordable Care Act (1 if any condition present, 0 otherwise)(CDC, 2019). These relate to problems with hearing, vision, cognitive function, mobility, dressing and bathing, and independence in attending doctor's visits or other errands. We note that these are often termed ‘disability indicators’, but this can be confusing as the presence of any of these conditions is a separate concept from a legal determination of disability status, so we refer to them as indicators of poor health in this study, even though that term is itself imperfect, as some individuals with these limitations may not view their health as poor. In exploratory analyses, we considered a three category variable (0 indicators, 1 indicator, or 2 or more indicators).
We considered two additional indicators of poor health for use as robustness checks. One was whether the individual responded that they have “a health problem or a disability which prevents work or which limits the kind or amount of work.” The other was self-rated health status, categorized as poor health (those who rated their health as “fair” or “poor”) and not being in poor health (those rating their health as “excellent”, “very good”, or “good”).
2.3. Earned income tax credit
EITC is an annual benefit that varies based on qualifying earnings for the tax year, tax filing status, and the number of dependents(Earned Income and Earned Income Tax Credit (EITC) Tables | Internal Revenue Service, n.d.). In brief, the structure is: $0 benefit if no qualifying earnings, a ‘phase-in’ where benefit increases with earnings, a ‘plateau’ where the maximum benefit is received regardless of earnings, a ‘phase-out’ where the benefit decreases with earnings, and a level at which earnings are too high to receive any benefit (Fig. S1 in the supplement)(Earned Income and Earned Income Tax Credit (EITC) Tables | Internal Revenue Service, n.d.).
The main outcome for our analyses was the EITC benefit category. We characterized the EITC benefit category for each individual as: no benefit, phase-in, plateau, phase-out, or earnings too high. To do this, we compared the EITC benefit for each individual (as estimated within ASEC by the U.S. Census using a tax simulator) to the maximum benefit for the household's number of dependents and tax filing status. Those receiving the maximum benefit were categorized in the plateau category. We distinguished between those receiving sub-maximal (but non-zero) benefits by examining their qualifying earnings. For example, those with sub-maximal EITC and qualifying earnings below the level needed for the maximum benefit were categorized as ‘phase-in,’ while those with sub-maximal EITC and qualifying earnings above the level needed for the maximum benefit were categorized as ‘phase-out’. Similarly, for those with $0 EITC benefits, we distinguished between those without qualifying income (‘no benefit’) and those whose earnings were too high for any benefit (or whose income came only from non-qualifying sources, such as investment income) (‘too high’). To determine qualifying earnings and number of dependents, we used the TAXSIM program provided by the U.S. Census Bureau and hosted by the National Bureau of Economic Research(TAXSIM CPS Code, n.d.; Taxsim - NBER, n.d.).
Thirty-one states have EITC programs, which are typically structured as providing a percentage of the federal benefit(States and Local Governments with Earned Income Tax Credit | Internal Revenue Service, 2022). The amounts are typically modest—around 2/3 of states that do have a state EITC program offer benefit levels that are 20% or less of the federal EITC(States and Local Governments with Earned Income Tax Credit | Internal Revenue Service, 2022). We did not consider state EITC programs in our analyses because state EITCs are structured to offer a percentage of the benefits of the federal program. Therefore, including them would not change the category of EITC benefits (e.g., phase-in or plateau) that individuals are in, and thus would not change the results of our analyses.
2.4. Supplemental Poverty Measure
To answer questions about whether those in poor health may receive assistance from other sources that could make up for shortfalls in EITC benefits, we examined the Census' SPM resources. SPM resources include estimates of “cash income, plus non-cash benefits that resource units can use to meet their FCSU [Food, Clothing, Shelter, and Utility] needs, minus taxes (or plus tax credits), work expenses, medical expenses, and child support paid to another household”(US Census Bureau, n.d.-b). Thus the SPM gives a more comprehensive measure of benefits, both cash (e.g., SSI and TANF) and non-cash (e.g., SNAP), including EITC, available to a person. For analysis, we expressed the individual's SPM resources as a ratio relative to the SPM poverty level for their household size (e.g., SPM resources equal to the poverty threshold for a given household size yields an SPM resource ratio of 1).
2.5. Covariates
The goal in these analyses was to examine the experience of those with poor health with regard to income support programs, rather than to establish poor health as an etiologic agent for particular program outcomes. Thus, we did not attempt to adjust for every potential cause of poor health. Nevertheless, because some common demographic factors are strongly associated with poor health and study outcomes, we sought to standardize the study estimates over these factors. To do this, we extracted data from the ASEC on age, gender, race, and ethnicity. We used the race categories (White Alone, Black Alone, Asian Alone, and a joint category of American Indian, Alaska Native, Pacific Islander, Multiracial) and ethnicity categories (Hispanic or non-Hispanic) defined within the ASEC. We included the race and ethnicity variables in our analysis as indicators of exposure to racism, which may be associated with both health status and study outcomes(Breathett et al., 2021).
2.6. Statistical analyses
We compared how the distribution of EITC benefit category, the main outcome, varied by health status, the main exposure. We particularly focused on whether those with poor health were more likely to be in the two worst-off categories concerning EITC benefit—no benefit or phase-in. This comparison is particularly policy relevant as eliminating the earned income requirement and phase-in (changes recently enacted in CTC reform) may be especially helpful for those less able to work due to poor health.
Low earned income, which is proximately related to EITC benefits, and poor health are known to have a bidirectional relationship—low income can worsen health, and worse health can make it more difficult to earn income(Kawachi, Subramanian, & Almeida-Filho, 2002; Lynch et al., 2004; Pickett & Wilkinson, 2015). As noted above, the goal in these cross-sectional analyses was not to disentangle this relationship. Instead, the goal was to examine the experience of those with poor health, whatever the cause, with regard to income support programs that could help them meet basic needs and provided resources needed to manage chronic conditions going forward.
For analysis, we fit a multinomial logistic regression model (which makes no assumptions about the relationship of the EITC categories to each other) accounting for health status, age, gender, race, and ethnicity, and then produced estimates of the probability of being in each of the EITC categories using predictive margins(Graubard & Korn, 1999). We report results on the absolute scale and test the difference in predicted probability between those in versus not in poor health for statistical significance (‘risk difference’). For further illustration of the findings, we also report results on the relative scale (the ratio of predicted probabilities, or ‘relative risk’). As exploratory analyses, we examined these relationships within categories of gender, race, and ethnicity. We did this to examine the relationship between poor health and EITC benefit category among those who may have experienced structural barriers to economic opportunities, such as sexism or racism. Our primary method of accounting for differences in the number of dependents within households was through the construction of the outcome, which assigns an outcome category based on the appropriate income and benefit level thresholds for a given household size. In a sensitivity analysis, we examined results in each subgroup, defined by number of dependents: 0, 1, 2, or 3+. In exploratory analyses, we repeated our main analyses in a sample that was restricted to individuals who had earned at least some qualifying income.
To investigate whether the SPM resource ratio differed by health status, we fit generalized linear models with a log link and gamma error distribution, adjusting for age, gender, race, and ethnicity. We used predictive margins to express and compare results. We examined this both in the entire sample, and in a sample restricted to those with incomes of 400% or less of the SPM poverty level—to focus on those for whom income support programs are most likely to be relevant(Frequently Asked Questions Related to the Poverty Guidelines and Poverty, n.d.). Of particular interest was how SPM resources were distributed among those with no and phase-in categories of EITC benefit.
Because the COVID-19 pandemic partially interrupted data collection for the 2020 CPS ASEC, we compared, as a sensitivity analysis, the distribution of EITC categories by poor health indicators observed using 2020 data to those observed using 2019 CPS ASEC data, to examine whether this interruption may have affected study findings. We also repeated our main analyses using 2019 CPS ASEC data, to see if the patterns found using data from the 2020 CPS ASEC held in the prior year.
All analyses used the SPM unit representativeness weights provided in the ASEC(US Census Bureau, n.d.-a). We followed Census Bureau guidance in accounting for the complex survey design by using BRR (balanced repeated replication) standard error estimation using the Census-provided replicates(US Census Bureau, n.d.-a). We used complete case analysis, and did not pursue imputation as there was less than 5% missing data when considering all study variables. A two-sided p-value less than 0.05 was taken to indicate statistical significance. Analyses were conducted in SAS 9.4, Stata 16, and R 3.5.3.
3. Results
A total of 41,659 ASEC participants, representing 87.1 million individuals, met eligibility criteria. The mean age was 45.1 (SD 12.2) years, 46.8% were women, and 39.4% had at least one dependent. 2,724 participants, representing 5.6 million individuals, reported poor health (Table 1). The distribution of individuals in poor health across EITC categories is presented in Table S1 in the supplement.
Table 1.
Demographics.
| Overall N=41659 |
Does Not Report Poor Health N=38935 |
Reports Poor Health N=2724 |
P-value | |
|---|---|---|---|---|
| Mean (SE) or N (weighted %) | Mean (SE) or N (weighted %) | Mean (SE) or N (weighted %) | ||
| Age, years | 45.11 (0.03) | 44.60 (0.03) | 52.55 (0.14) | <.0001 |
| Female | 19793 (46.75) | 18450 (46.61) | 1343 (48.87) | 0.0001 |
| Race | <.0001 | |||
| White | 32537 (77.45) | 30400 (77.31) | 2137 (79.39) | |
| Black | 4848 (12.96) | 4462 (12.84) | 386 (14.70) | |
| Asian | 2730 (6.28) | 2653 (6.55) | 77 (2.38) | |
| Other | 1544 (3.31) | 1420 (3.30) | 124 (3.54) | |
| Hispanic Ethnicity (any race) | 7157 (16.06) | 6777 (16.30) | 380 (12.60) | <.0001 |
| Adjusted gross income, $ | 99679 (406) | 102516 (428) | 58114 (834) | <.0001 |
| Any dependents | 18887 (39.40) | 18131 (40.26) | 756 (25.83) | <.0001 |
| Number of dependents | 0.73 (0.00) | 0.75 (0.00) | 0.43 (0.01) | <.0001 |
| Any Disability Income | 2040 (4.84) | 1272 (3.19) | 768 (28.93) | <.0001 |
| Mean Disability Income, if any, $ | 17036 (264) | 15485 (355) | 19544 (392) | <.0001 |
Percentages are weighted to be nationally representative.
P-values for comparison between those who do and do not report poor health.
Within EITC categories, 0.47%, representing 384 thousand individuals, were in the no-benefit category; 3.05%, representing 2.5 million individuals, were in the phase-in category; 2.16%, representing 1.8 million individuals, were in the plateau category; 10.17%, representing 8.3 million individuals, were in the phase-out category; and 84.13%, representing 68.6 million individuals, had earnings too high to qualify for benefits (Table 2).
Table 2.
Unadjusted probability of earned income tax credit benefit category membership by health status.
| Primary Poor Health Status Indicator | ||||
|---|---|---|---|---|
| EITC Benefit Category | Overall N=41659 | Not in Poor Health N=38935 | In Poor Health N=2724 | P |
| No Benefit | 0.47% | 0.29% | 3.77% | <.0001 |
| Phase-In | 3.05% | 2.75% | 8.43% | <.0001 |
| Plateau | 2.16% | 2.06% | 4.05% | <.0001 |
| Phase-Out | 10.18%v | 10.00% | 13.41% | <.0001 |
| Too High | 84.13% | 84.90% | 70.35% | <.0001 |
|
| ||||
| Limited Ability to Work Health Status Indicator | ||||
| EITC Benefit Category |
Overall N=41659 |
Not in Poor Health N=39185 |
In Poor Health N= 2474 |
P |
| No Benefit | 0.47% | 0.25% | 4.63% | <.0001 |
| Phase-In | 3.05% | 2.70% | 9.53% | <.0001 |
| Plateau | 2.16% | 2.02% | 4.78% | <.0001 |
| Phase-Out | 10.18% | 10.03% | 12.95% | <.0001 |
| Too High | 84.13% | 84.99% | 68.11% | <.0001 |
|
| ||||
| Self-Rated Health Status Indicator | ||||
| EITC Benefit Category |
Overall N=41659 |
Not in Poor Health N=38206 |
In Poor Health N=3453 |
P |
| No Benefit | 0.47% | 0.29% | 2.70% | <.0001 |
| Phase-In | 3.05% | 2.70% | 7.42% | <.0001 |
| Plateau | 2.16% | 1.97% | 4.63% | <.0001 |
| Phase-Out | 10.18% | 9.72% | 16.01% | <.0001 |
| Too High | 84.13% | 85.32% | 69.25% | <.0001 |
Percentages are weighted to be nationally representative.
P-value compares those in poor health with those not in poor health.
In unadjusted analyses, the income distribution for those in poor health was downshifted relative to the income distribution of those not in poor health. This means that, at the higher end of the income distribution, relatively more individuals in poor health still have income low enough to qualify for EITC, and end up in the phase out and plateau groups (p < .0001 for all comparisons). Thus they may benefit disproportionately from federal EITC. For example, 13.41% of individuals in poor health were in the phase-out category, compared with 10.00% of individuals not in poor health. However, the downshifted income distribution, combined with the phase-in design of EITC, also means that relatively more individuals in poor health have income low enough that they receive only phase-in range benefits, or have no earned income and receive no federal EITC benefits at all. For example, only 0.29% of those not in poor health had no EITC benefit, but 3.77% of those in poor health had no benefit (p < .0001), and 2.75% of those not in poor health, compared with 8.73% of those in poor health were in the phase-in category (p < .0001).
Comparisons between 2019 and 2020 CPS data did not reveal evidence of meaningful changes related to the interruption in data collection caused by the COVID-19 pandemic (Table S2).
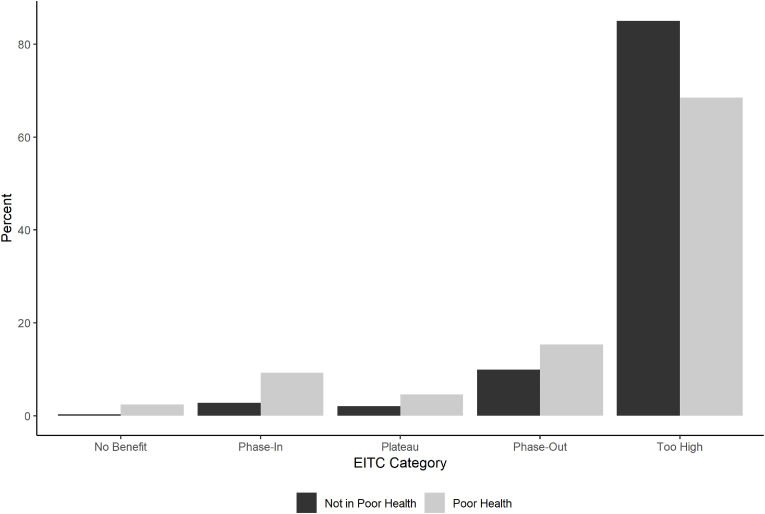
The same pattern was present in analyses standardized over age, gender, race, and ethnicity (Fig. 1, Table 3, and Fig. S2). Those in poor health, compared with those not in poor health, were more likely to be in the no benefit (2.40% vs. 0.30%, risk difference 2.10 percentage points [95%CI 1.75 to 2.46 percentage points], relative risk 8.09 [95%CI 6.68 to 9.79], p <.0001), and phase-in categories (9.28% vs. 2.74%, risk difference 6.54 percentage points [95%CI 5.82 to 7.26 percentage points], relative risk 3.39 [95%CI 3.12 to 3.69], p <.0001). Results were similar when using different indicators of poor health (Table 3), including a three category indicator of poor health (Table S3). Results were also similar when examining subgroups defined by number of dependents in the household (Table S4), using data from the 2019 CPS ASEC (covering tax year 2018, Table S5) and in analyses restricted to individuals who had earned at least some qualifying income (Table S6).
Fig. 1.
Distribution of EITC Benefit Categories
Distribution of EITC benefit categories, standardized for age, gender, race, and ethnicity.
Table 3.
Probability of Earned Income Tax Credit Benefit Category Membership by Health Status, standardized for age, gender, race, and ethnicity.
| Primary Poor Health Status Indicator | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| EITC Benefit Category | Not in Poor Health | In Poor Health | Risk Difference | Lower Confidence Limit of Risk Difference | Upper Confidence Limit of Risk Difference | Relative Risk | Lower Confidence Limit of Relative Risk | Upper Confidence Limit of Risk Relative Risk | P |
| No Benefit | 0.30% | 2.40% | 2.10% | 1.75% | 2.46% | 8.09 | 6.68 | 9.79 | <.0001 |
| Phase-In | 2.74% | 9.28% | 6.54% | 5.82% | 7.26% | 3.39 | 3.12 | 3.69 | <.0001 |
| Plateau | 2.04% | 4.59% | 2.55% | 2.00% | 3.09% | 2.25 | 1.99 | 2.54 | <.0001 |
| Phase-Out | 9.92% | 15.30% | 5.38% | 4.46% | 6.30% | 1.54 | 1.45 | 1.64 | <.0001 |
| Too High | 85.00% | 68.43% | −16.57% | −17.65% | −15.49% | 0.81 | 0.79 | 0.82 | <.0001 |
| Limited Ability to Work Health Status Indicator | |||||||||
| No Benefit | 0.26% | 3.14% | 2.88% | 2.47% | 3.30% | 12.31 | 10.17 | 14.90 | <.0001 |
| Phase-In | 2.70% | 10.00% | 7.30% | 6.44% | 8.16% | 3.71 | 3.39 | 4.06 | <.0001 |
| Plateau | 2.01% | 5.20% | 3.18% | 2.56% | 3.80% | 2.58 | 2.29 | 2.91 | <.0001 |
| Phase-Out | 9.99% | 14.15% | 4.16% | 3.17% | 5.15% | 1.42 | 1.32 | 1.52 | <.0001 |
| Too High | 85.05% | 67.52% | −17.53% | −18.77% | −16.29% | 0.79 | 0.78 | 0.81 | <.0001 |
| Self-Rated Health Status Indicator | |||||||||
| No Benefit | 0.30% | 1.97% | 1.67% | 1.40% | 1.95% | 6.50 | 5.43 | 7.79 | <.0001 |
| Phase-In | 2.70% | 7.62% | 4.92% | 4.31% | 5.54% | 2.82 | 2.60 | 3.07 | <.0001 |
| Plateau | 1.96% | 4.76% | 2.80% | 2.25% | 3.34% | 2.43 | 2.15 | 2.74 | <.0001 |
| Phase-Out | 9.69% | 16.62% | 6.93% | 6.03% | 7.83% | 1.72 | 1.62 | 1.81 | <.0001 |
| Too High | 85.35% | 69.03% | −16.32% | −17.33% | −15.31% | 0.81 | 0.80 | 0.82 | <.0001 |
Probabilities estimated by fitting multinomial logistic regression models followed by predictive margins, standardized for age, gender, race, and ethnicity.
The over-representation of those in poor health in the phase-in group was typically greater when considering populations that may experience structural barriers to economic opportunities (Table S7).
Examining SPM resources, and again standardizing over age, gender, and race and ethnicity, those in poor health had a lower mean SPM resource ratio in both the overall cohort (2.70 versus 3.67, difference −0.96, 95% CI -1.02 to −0.91, p <.0001), and in a cohort restricted to those under 400% of the SPM resources to SPM poverty ratio (1.93 versus 2.21, difference −0.27, 95% CI -0.30 to −0.25, p <.0001). This finding suggests that, overall, other programs did not make up the difference in earnings related to poor health.
Examining differences by EITC category, however, revealed a heterogeneous pattern (Table 4). In analyses by EITC category, standardized as before, the mean SPM resource ratio for those in poor health and in the no-benefit category was 1.63 (SE: 0.07), and 26.81% were considered poor by the SPM resources definition. This suggests that other income support programs provide substantial resources for individuals in poor health who do not have earned income—enough that most are not in poverty. However, the mean SPM resource ratio for those in poor health and in the phase-in category was 0.92 (SE: 0.02), and 60.63% were considered poor by the SPM resources definition. This suggests that there is a substantial gap in support available for those in poor health who continue to work. Income support programs used are described in Table S8.
Table 4.
Supplemental poverty measure resource measures for those in poor health by primary indicator.
| EITC Benefit Category | Ratio of SPM Resources to Poverty Threshold | Lower 95% CI | Upper 95% CI | % Experiencing Poverty | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|---|
| No Benefit | 1.63 | 1.47 | 1.77 | 26.81% | 20.59% | 30.02% |
| Phase-In | 0.92 | 0.88 | 0.97 | 60.63% | 56.35% | 64.91% |
Results from fitting gamma or logistic regression models followed by predictive margins, standardized for age, gender, race, and ethnicity.
4. Discussion
In this study of nationally-representative U.S. Census Bureau data, being in poor health was associated greater probability of receiving lower EITC benefits. Moreover, when considering a more complete picture of resources available, individuals in poor health who had no earned income and no EITC benefits often received meaningful resources from other programs. However, there was another category of individuals with earned income, who had low EITC benefits and low overall resources—60% were in poverty despite working. These findings highlight an important gap in income support policy for those in poor health, particularly for individuals who are still able to work—their financial situation seems to be worse than not only those in good health, but also those in poor health who are unable to work.
Because this study is cross-sectional, we are not able to determine the benefits from EITC that individuals receive over time. If individuals’ health improves and they are able to work more, EITC could then offer them more support. However, it is important to note that while individuals are experiencing poor health, they are more likely to receive lower levels of EITC benefits than those who are not experiencing poor health.
This study is consistent with and expands findings from prior studies documenting a nuanced relationship between EITC and health. Prior studies have found health benefits associated with EITC, particularly for children and maternal health (Arno et al., 2009; Averett & Wang, 2018; Batra et al., 2022; Batra & Hamad, 2021; Boyd-Swan et al., 2016; Chetty & Friedman, 2011; Collin et al., 2021; Courtin, Aloisi, et al., 2020; Courtin et al., 2018; Courtin, Kim, et al., 2020; Duncan & Murnane, 2016; Evans & Garthwaite, 2014; Halpern-Meekin et al., 2018; Hamad & Rehkopf, 2015; Hoynes et al., 2015; Markowitz et al., 2017; Muennig et al., 2016; Rehkopf et al., 2014; Simon et al., 2018). However, these studies compared health outcomes for those receiving different levels of EITC benefits (including $0), rather than comparing different designs of income support programs (for example, comparing EITC-like programs that might provide monthly versus annual benefits), and thus cannot separate the health impacts of the money received from impacts related to program design. Further, other work has found downsides to EITC's design. First, administrative barriers mean that around 20% of eligible individuals do not claim the credit(Jones & Ziliak, 2019; Linos et al., n.d.). This burden is unequally shared, falling more heavily on those with lower incomes and/or who have been minoritized(Maag, 2005). Moreover, structuring EITC as a wage subsidy means that much of the program benefit is captured by employers, with spillover effects of decreased wages for other workers(Rothstein, 2010). Our study adds to this literature by documenting aspects of EITC's design that render it less effective for providing income support to those in poor health. Further, because EITC benefit level is tied to labor market earnings, those who experience systemic discrimination (for example, in the educational system or the labor market) and thus have lower labor market earnings may receive less EITC support than similar individuals who did not experience such discrimination. This speaks to potential unintended consequences of ‘phase-in’ designs in public programs that occur in the setting of ongoing oppression, such as racism and sexism.
An important task for the field is synthesizing both the positive and negative findings regarding EITC. One interpretation of these prior studies is that they provide proof of principle that cash transfers can improve health for individuals with lower income, but that how best to deliver that income support remains an open question. An important direction for future research is to test variations in income support policies, such as removing work requirements and the phase-in(Jones & Marinescu, 2022; Silver & Zhang, 2022), and variation in payment frequency, enrollment procedures, and payment amounts, in order to more fully understand how best to support lower income individuals in poor health. Further, although the phase-in structure of federal EITC seems to create a gap in income support for workers in poor health, that does not necessarily mean that changing federal EITC is the best way to close this gap. Future studies should examine whether changes to disability income programs, or other programs, might be good ways to address this issue. Another important area for future study is whether the patterns observed in this study still hold once COVID-era income support programs have expired.
The results from this study should be interpreted in light of important limitations. Most importantly, census methodology assumes all individuals receive the EITC their income entitles them to. In reality, approximately 20% of eligible individuals do not receive it(Jones & Ziliak, 2019). This will tend to overstate the impact of EITC on poverty alleviation and income support. Second, the objective in this study was to understand the income supports received by those in poor health, rather than to evaluate whether poor health caused the differences in income support. Thus, there may be confounding factors that serve as common causes of both poor health and less income support. However, we view the causal relationship between poor health and benefits received as less policy relevant since, whatever the cause of poor health, those with lower earned income need income support to meet basic consumption needs. Third, ‘poor health’ is a multi-dimensional construct, and indicators used in this study may not fully capture all of its aspects. We did not have data on clinical conditions like such as diabetes, cardiovascular disease, kidney disease, asthma, COPD, arthritis, cancer, which could be alternative ways of indicating poor health. Nevertheless, we do think the indicators used are meaningful, as attested to by their use in government surveys to track functional limitations and health status. These limitations are balanced by several strengths, including the use of nationally-representative data, and EITC benefit calculation software that has been shown to perform well compared with observed IRS records(Jones & Ziliak, 2019).
5. Conclusions
Federal EITC is an important income support for many Americans. However, using nationally-representative data, we found an important gap for those for whom poor health limits, but does not preclude, the ability to work. EITC benefits are low for these individuals, and other programs do not take up the slack. This leaves millions of Americans without resources needed to escape poverty, with important implications for their health. Filling this gap with income support programs that do not diminish the support provided to those whose poor health limits the ability to work should be an important public health goal.
Funding
Seth Berkowitz's work on this project was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K23DK109200. Gaurav Dave's work on this project was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number R01HL150909 and R01HL157255. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Role of the funder
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of interest
SAB reports research grants from NIH, North Carolina Department of Health and Human Services, Blue Cross Blue Shield of North Carolina, and Feeding America, and personal fees from the Aspen Institute, Rockefeller Foundation, Gretchen Swanson Center for Nutrition, and Kaiser Permanente, outside of the submitted work. GD reports research grants from NIH, HRSA, North Carolina Department of Health and Human Services and Robert Wood Johnson Foundation, outside of the submitted work. ASV reports research grants from the NIH, Robert Wood Johnson Foundation, and Independence Blue Cross outside of the submitted work.
Prior presentation
None.
Author statement
SAB conceived of the study, analyzed the data, and drafted the manuscript. GD and AV conceived of the study and revised the manuscript draft critically for intellectual content. All three authors give approval of the final version of the manuscript for submission.
Ethical statement
The institutional review board at the University of North Carolina at Chapel Hill determined that this secondary analysis of deidentified data did not constitute human subjects research.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2023.101429.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
Data availability
Analysis code is available upon request. Data are freely available for download from the U.S. Census
References
- Aizer A., Hoynes H.W., Lleras-Muney A. National Bureau of Economic Research; 2022. Children and the US social safety net: Balancing disincentives for adults and benefits for children. Working Paper No. 29754; Working Paper Series) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arno P.S., House J.S., Viola D., Schechter C. Social security and mortality: The role of income support policies and population health in the United States. Journal of Public Health Policy. 2011;32(2):234–250. doi: 10.1057/jphp.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arno P.S., Sohler N., Viola D., Schechter C. Bringing health and social policy together: The case of the earned income tax credit. Journal of Public Health Policy. 2009;30(2):198–207. doi: 10.1057/jphp.2009.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Averett S., Wang Y. Effects of higher EITC payments on children's health, quality of home environment, and noncognitive skills. Public Finance Review. 2018;46(4):519–557. doi: 10.1177/1091142116654965. [DOI] [Google Scholar]
- Batra A., Hamad R. Short-term effects of the earned income tax credit on children's physical and mental health. Annals of Epidemiology. 2021;58:15–21. doi: 10.1016/j.annepidem.2021.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batra A., Karasek D., Hamad R. Racial differences in the association between the U.S. Earned income tax credit and birthweight. Women's Health Issues: Official Publication of the Jacobs Institute of Women’s Health. 2022;32(1):26–32. doi: 10.1016/j.whi.2021.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd-Swan C., Herbst C.M., Ifcher J., Zarghamee H. The earned income tax credit, mental health, and happiness. Journal of Economic Behavior & Organization. 2016;126(PA):18–38. [Google Scholar]
- Breathett K., Spatz E.S., Kramer D.B., Essien U.R., Wadhera R.K., Peterson P.N., et al. The groundwater of racial and ethnic disparities research: A statement from circulation: Cardiovascular quality and outcomes. Circulation. Cardiovascular Quality and Outcomes. 2021;14(2) doi: 10.1161/CIRCOUTCOMES.121.007868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brucker D.L., Garrison V.H. Health disparities among Social Security Disability Insurance and Supplemental Security Income beneficiaries who participate in federal rental housing assistance programs. Disability and Health Journal. 2021;14(3) doi: 10.1016/j.dhjo.2021.101098. [DOI] [PubMed] [Google Scholar]
- CDC Disability and health—disability data | CDC. Centers for disease control and prevention. 2019. https://www.cdc.gov/ncbddd/disabilityandhealth/datasets.html
- Chetty R., Friedman J.N. 2011. New evidence on the long-term impacts of tax credits 1. [Google Scholar]
- Child Tax Credit. (n.d.). U.S. Department of the Treasury. Retrieved April 12, 2022, from https://home.treasury.gov/policy-issues/coronavirus/assistance-for-american-families-and-workers/child-tax-credit.
- Collin D.F., Shields-Zeeman L.S., Batra A., White J.S., Tong M., Hamad R. The effects of state earned income tax credits on mental health and health behaviors: A quasi-experimental study. Social Science & Medicine. 2021;276 doi: 10.1016/j.socscimed.2020.113274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtin E., Aloisi K., Miller C., Allen H.L., Katz L.F., Muennig P. The health effects of expanding the earned income tax credit: Results from New York city. Health Affairs. 2020;39(7):1149–1156. doi: 10.1377/hlthaff.2019.01556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtin E., Kim S., Song S., Yu W., Muennig P. Can social policies improve health? A systematic review and meta-analysis of 38 randomized trials. The Milbank Quarterly. 2020;98(2):297–371. doi: 10.1111/1468-0009.12451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtin E., Muennig P., Verma N., Riccio J.A., Lagarde M., Vineis P., et al. Conditional cash transfers and health of low-income families in the US: Evaluating the family rewards experiment. Health Affairs. 2018;37(3):438–446. doi: 10.1377/hlthaff.2017.1271. [DOI] [PubMed] [Google Scholar]
- Deshpande M., Li Y. Who is screened out? Application costs and the targeting of disability programs. American Economic Journal: Economic Policy. 2019;11(4):213–248. doi: 10.1257/pol.20180076. [DOI] [Google Scholar]
- Duncan G.J., Murnane R.J. Rising inequality in family incomes and children's educational outcomes. RSF: The Russell Sage Foundation Journal of the Social Sciences. 2016;2(2):142–158. doi: 10.7758/rsf.2016.2.2.06. [DOI] [Google Scholar]
- Earned income and earned income tax credit (EITC) Tables | internal Revenue Service. https://www.irs.gov/credits-deductions/individuals/earned-income-tax-credit/earned-income-and-earned-income-tax-credit-eitc-tables n.d.). Retrieved April 13, 2022, from.
- Evans W.N., Garthwaite C.L. Giving mom a break: The impact of higher EITC payments on maternal health. American Economic Journal: Economic Policy. 2014;6(2):258–290. doi: 10.1257/pol.6.2.258. [DOI] [Google Scholar]
- Frequently asked questions related to the poverty Guidelines and poverty. https://aspe.hhs.gov/topics/poverty-economic-mobility/poverty-guidelines/frequently-asked-questions-related-poverty-guidelines-poverty (n.d.). ASPE. Retrieved April 12, 2022, from.
- Graubard B.I., Korn E.L. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- Halpern-Meekin S., Greene S.S., Levin E., Edin K. The rainy day earned income tax credit: A reform to boost financial security by helping low-wage workers build emergency savings. RSF: The Russell Sage Foundation Journal of the Social Sciences. 2018;4(2):161–176. doi: 10.7758/rsf.2018.4.2.08. [DOI] [Google Scholar]
- Hamad R., Rehkopf D.H. Poverty, pregnancy, and birth outcomes: A study of the earned income tax credit. Paediatric & Perinatal Epidemiology. 2015;29(5):444–452. doi: 10.1111/ppe.12211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoynes H., Miller D., Simon D. Income, the earned income tax credit, and infant health. American Economic Journal: Economic Policy. 2015;7(1):172–211. doi: 10.1257/pol.20120179. [DOI] [Google Scholar]
- Internal Revanue Service. (n.d.). Publication 596: Earned income credit (EIC)—For use in preparing 2019 Returns. Retrieved September 13, 2022, from Earned Income Credit (EIC) For use in preparing 2019 Returns.
- Johnson K.T., Palakshappa D., Basu S., Seligman H., Berkowitz S.A. Examining the bidirectional relationship between food insecurity and healthcare spending. Health Services Research. 2021 doi: 10.1111/1475-6773.13641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D., Marinescu I. The labor market impacts of universal and permanent cash transfers: Evidence from the Alaska permanent fund. American Economic Journal: Economic Policy. 2022;14(2):315–340. doi: 10.1257/pol.20190299. [DOI] [Google Scholar]
- Jones M.R., Ziliak J.P. Working papers (No. 19–14; working papers) Center for Economic Studies, U.S. Census Bureau; 2019. The antipoverty impact of the EITC: New estimates from survey and administrative tax records.https://ideas.repec.org/p/cen/wpaper/19-14.html [Google Scholar]
- Kawachi I., Subramanian S.V., Almeida-Filho N. A glossary for health inequalities. Journal of Epidemiology & Community Health. 2002;56(9):647–652. doi: 10.1136/jech.56.9.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khullar D., Chokshi D.A. Health, income, & poverty: Where we are & what could help | health Affairs brief. 2018. https://www.healthaffairs.org/do/10.1377/hpb20180817.901935/full/
- Kleven H. NBER working papers (No. 26405; NBER working papers) National Bureau of Economic Research, Inc; 2019. The EITC and the extensive margin: A reappraisal.https://ideas.repec.org/p/nbr/nberwo/26405.html [Google Scholar]
- Linos, E., Prohofsky, A., Ramesh, A., Rothstein, J., & Unrath, M. (n.d.). Can Nudges Increase Take-up of the EITC?: Evidence from Multiple Field Experiments. American Economic Journal: Economic Policy. 10.1257/pol.20200603. [DOI]
- Lynch J., Smith G.D., Harper S., Hillemeier M., Ross N., Kaplan G.A., et al. Is income inequality a determinant of population health? Part 1. A systematic review. The Milbank Quarterly. 2004;82(1):5–99. doi: 10.1111/j.0887-378x.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maag E. 2005. Disparities in knowledge of the EITC. [Google Scholar]
- Markowitz S., Komro K.A., Livingston M.D., Lenhart O., Wagenaar A.C. Effects of state-level Earned Income Tax Credit laws in the U.S. on maternal health behaviors and infant health outcomes. Social Science & Medicine. 2017;194:67–75. doi: 10.1016/j.socscimed.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthew P., Brodersen D.M. Income inequality and health outcomes in the United States: An empirical analysis. The Social Science Journal. 2018;55(4):432–442. doi: 10.1016/j.soscij.2018.05.001. [DOI] [Google Scholar]
- Muennig P.A., Mohit B., Wu J., Jia H., Rosen Z. Cost effectiveness of the earned income tax credit as a health policy investment. American Journal of Preventive Medicine. 2016;51(6):874–881. doi: 10.1016/j.amepre.2016.07.001. [DOI] [PubMed] [Google Scholar]
- Pickett K.E., Wilkinson R.G. Income inequality and health: A causal review. Social Science & Medicine. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Rehkopf D.H., Strully K.W., Dow W.H. The short-term impacts of Earned Income Tax Credit disbursement on health. International Journal of Epidemiology. 2014;43(6):1884–1894. doi: 10.1093/ije/dyu172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein J. Is the EITC as good as an NIT? Conditional cash transfers and tax incidence. American Economic Journal: Economic Policy. 2010;2(1):177–208. doi: 10.1257/pol.2.1.177. [DOI] [Google Scholar]
- Sherman A., DeBot B., Huang C.-C. Boosting low-income children's opportunities to succeed through direct income support. Academic Pediatrics. 2016;16(3 Suppl):S90–S97. doi: 10.1016/j.acap.2016.01.008. [DOI] [PubMed] [Google Scholar]
- Silver D., Zhang J. National Bureau of Economic Research; 2022. Impacts of basic income on health and economic well-being: Evidence from the VA's disability compensation program. Working Paper No. 29877; Working Paper Series) [DOI] [Google Scholar]
- States and local governments with earned income tax credit | internal Revenue Service. 2022. https://www.irs.gov/credits-deductions/individuals/earned-income-tax-credit/states-and-local-governments-with-earned-income-tax-credit
- Statistics for tax Returns with the earned income tax credit (EITC) | earned income tax credit. https://www.eitc.irs.gov/eitc-central/statistics-for-tax-returns-with-eitc/statistics-for-tax-returns-with-the-earned-income (n.d.). Retrieved April 12, 2022, from.
- Substantial gainful activity. https://www.ssa.gov/oact/cola/sga.html (n.d.). Retrieved April 12, 2022, from.
- TAXSIM CPS code. https://users.nber.org/~taxsim/to-taxsim/cps27/cps-uchicago/ (n.d.). Retrieved April 12, 2022, from.
- Taxsim—NBER https://users.nber.org/~taxsim/to-taxsim/ (n.d.). Retrieved April 12, 2022, from.
- Simon D., McInerny M., Goodell S. The earned income tax credit, poverty, and health | health Affairs brief. 2018. https://www.healthaffairs.org/do/10.1377/hpb20180817.769687/full/
- US Census Bureau. (n.d.-a) Annual social and economic supplements. The United States census Bureau. https://www.census.gov/data/datasets/time-series/demo/cps/cps-asec.html Retrieved March 11, 2021, from.
- US Census Bureau. (n.d.-b The supplemental poverty measure: 2019. Census.Gov. https://www.census.gov/library/publications/2020/demo/p60-272.html Retrieved April 12, 2022, from.
- Weinstein J.M., Kahkoska A.R., Berkowitz S.A. Food insecurity, missed workdays, and hospitalizations among working-age US adults with diabetes. Health Affairs. 2022;41(7):1045–1052. doi: 10.1377/hlthaff.2021.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- What's new with the child tax credit after tax reform | Internal Revenue Service. https://www.irs.gov/newsroom/whats-new-with-the-child-tax-credit-after-tax-reform (n.d.). Retrieved April 12, 2022, from.
- Whitmore Schanzenbach D., Strain M.R. Employment effects of the earned income tax credit: Taking the long view. Tax Policy and the Economy. 2021;35:87–129. doi: 10.1086/713494. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Analysis code is available upon request. Data are freely available for download from the U.S. Census