Abstract
Rinderpest (RP) and peste-des-petits-ruminants (PPR) are two important diseases of domestic ruminants. To improve on currently available vaccines against PPR, we have created cDNA copies of the RP virus genome in which either the fusion (F) or hemagglutinin (H) gene, or both, was replaced with the corresponding gene from PPR virus. It was necessary to develop a modified rescue system in which the T7 RNA polymerase was provided by a recombinant fowlpox virus and the entire rescue procedure took place in Vero cells before we could obtain live virus from these chimeric constructs. No virus was recovered when only one of the glycoprotein genes was changed, but a chimeric virus containing both F and H genes from PPR virus was reproducibly rescued from cDNA, indicating that a virus-specific functional interaction takes place between the F and H proteins. The rescued virus expressing the PPR glycoproteins grew more slowly in tissue culture than either parental virus and formed abnormally large syncytia. Goats infected with the chimera showed no adverse reaction, as assessed by clinical signs, temperature, leukocyte count, virus isolation, and serology, and were protected from subsequent challenge with wild-type PPR virus.
Rinderpest (RP) and peste-des-petits-ruminants (PPR) are two important diseases of domestic ruminants causing great economic losses due to their high morbidity and mortality. RP is a severe, acute disease of cattle, buffalo, and wild bovids, while PPR is a disease of sheep and goats that clinically resembles RP; both RP and PPR are regarded as List A diseases by the Office International des Epizooties due to their highly contagious nature and consequent capacity for rapid spread. RP virus (RPV) and PPR virus (PPRV) are both members of the Morbillivirus genus of the family Paramyxoviridae, a genus which also includes Measles virus (MV) (humans), Canine distemper virus (CDV) (canids and other wild carnivores), Phocid distemper virus (PDV) (seals), and the morbilliviruses of porpoises and dolphins (PMV/DMV). RP is currently the target of an international eradication campaign (20). Sheep and goats can be infected with RPV, but only the most virulent strains show any clinical disease in these species (7, 16). Because of the cross-reactive and cross-protective antibodies generated by either of these two related viruses, the normal tissue culture-adapted vaccine strain of RPV (RBOK) (37) is commonly used to vaccinate against PPR, as it is known to be both safe and clinically effective (47).
Recently, PPR has become a much more prominent disease because, besides causing disease in small ruminants, it influences diagnosis and vaccination carried out to prevent RP in large ruminants. PPRV can cause a subclinical infection in the latter, and it can be confused with RPV due to cross-reactive antibodies unless virus-specific reagents are used to analyze sera. This has important implications for the ongoing campaign for elimination of RP. In addition, areas which have been declared free of RP can no longer use the RPV vaccine strain to vaccinate against RP or PPR. A vaccine strain of PPRV [derived from PPRV(Nigeria 75/1)] has been isolated but has not yet been widely tested in the field. It would therefore be of great practical use to develop a vaccine against PPR which combines the known safety of the RBOK vaccine with usability in RP-free areas due to a unique serological signature.
Sequence comparisons show that RPV is most closely related to MV (3). Only about half of the sequence of PPRV is known; despite the similarity in the hosts of RPV and PPRV, such sequence data as are known show that PPRV is no more related to RPV than to CDV or PMV/DMV. The viruses all have a negative-strand RNA genome; in RPV it is 15,882 nucleotides in length (3). The morbillivirus genome is tightly encapsidated by the viral N protein and associated with the P and L proteins, which together make the viral polymerase. The nucleocapsid is in turn surrounded by a lipid envelope which contains two glycoproteins, F (fusion) and H (attachment). It is known that these glycoproteins are the major protective immunogens and are responsible for inducing neutralizing antibodies (6, 22, 49, 50). The high degree of sequence conservation between the F proteins of different morbilliviruses (9, 30) probably accounts for the extensive cross-protection observed between different viruses of this genus, enabling, for example, the RPV vaccine to be used to vaccinate against PPRV. The H proteins are more divergent (8) and may play a role in host cell specificity. By changing the F and/or H genes of the RPV vaccine strain for those of PPRV, the immune response can be further directed toward the latter virus.
The techniques by which single-segment, negative-strand RNA viruses can be rescued from cDNA copies of their genomes have already been applied to both MV (38) and RPV (4). Here we describe the rescue of a chimeric RPV in which both the F and H genes have been replaced by those of PPRV. The efficacy of this virus as a vaccine against PPRV infection has also been evaluated.
MATERIALS AND METHODS
Cells and viruses.
Vero cells were grown in Dulbecco's minimal essential medium (MEM) containing 25 mM HEPES (pH 7.2) and 5% fetal calf serum (FCS). 293 cells were grown in Dulbecco's MEM without HEPES and with 10% FCS. B95a cells were grown in RPMI 1640 with 5% FCS. All media contained penicillin (100 IU/ml) and streptomycin (100 μg/ml).
RPV [RPV(Saudi 81/1) or recombinant RPV] was grown in Vero cells unless otherwise indicated. Virus was prepared by a single freeze-thaw cycle of infected cells 3 to 4 days postinfection and removal of cell debris by centrifugation at 1,280 × g for 10 min.
PPRV(Nigeria 75/1) was used at passage 60 in Vero cells and grown for 9 days before harvesting as for RPV. RPV and PPRV were titrated on Vero cells by determination of 50% tissue culture infective dose (TCID50).
Recombinant fowlpox virus FP-T7 was obtained from M. Skinner, IAH Compton, Compton, Newbury, Berkshire, United Kingdom. Virus stocks were prepared in primary chick embryo fibroblast cultures grown in medium 199 containing 10% FCS. Virus was harvested when cytopathic effect (CPE) was extensive (usually 3 to 4 days postinfection); the infected cells were subjected to three cycles of freeze-thawing before clarification as for RPV. Virus stocks were titrated on chick embryo fibroblasts by determination of the TCID50.
Molecular biology techniques.
Plasmids pKSMF, pMDBRPVII, pKSN1, pKS-P, and pGEM-L have been described in reference 4. Plasmid pKSF was derived from pKSMF by removing the SmaI-EcoRI fragment containing most of the F gene and ligating it into similarly cut pKS(+). Plasmid pKSL9, containing the whole of the RPV H gene plus parts of the flanking F and L genes, has been described in reference 3. Mutagenesis by elimination of unique sites was performed essentially as described in reference 18. Quick-Change mutagenesis (Stratagene) was performed as described in the instructions to the Quick-Change kit. All other DNA manipulations and cloning procedures were as previously described (4). RNA was purified from small-scale cultures (35-mm-diameter wells) using Trizol (Life Technologies, Inc.); large-scale preparations from virus-infected cells were performed according to the method of Chomczynski and Sacchi (15). For extraction of RNA from purified peripheral blood leukocytes (PBL), the cells were pelleted (1,280 × g, 10 min), and the pellet was resuspended in 100 μl of phosphate-buffered saline, which was then mixed with 1 ml of Trizol and processed according to the manufacturer's instructions. Ocular swabs were placed in 2-ml screw-cap tubes and extracted with 1 ml of Trizol by vigorous vortexing. The Trizol extract was then processed in the normal way. Reverse transcription-PCR (RT-PCR) was performed using Taq polymerase as described in reference 21. Preparative, gene-copying PCR using the proofreading Pfu polymerase was performed as described in reference 5.
Insertion of new restriction sites into the RPV genome sequence.
A total of four new restriction sites were introduced into the RPV genome cDNA clone. Plasmid pKSL9 was mutated by unique site elimination (USE) mutagenesis to introduce either an AscI site at the position corresponding to 7195 to 7202 in the antigenome (pKSL9FAsc) or a PmlI site at the position corresponding to 9092 to 9097 in the antigenome (pKSL9HPml). The two mutations were combined by exchanging the EcoRI-SphI fragment containing the AscI site in pKSL9FAsc with the corresponding fragment in pKSL9HPml. The SunI-NcoI fragment from the resulting construct was then ligated to NcoI-AatII and AatII-SunI fragments from pRPVII to make pRPV2A. Plasmid pKSF was similarly mutated to introduce an SgfI site at the position corresponding to 5435 to 5442 in the antigenome. Plasmid pKSMF was mutated using the Quick-Change system (Stratagene) to introduce a SwaI site at the position corresponding to 4456 to 4463 in the antigenome. Because we observed mutations at secondary sites when using the Quick-Change system, we sequenced and removed the small AgeI-BsmBI fragment containing the SwaI site and ligated it into a nonmutated copy of pKSMF to give pKSMF-Swa. The Eco47III-NsiI fragment containing the SgfI site in pKSF-Sgf was then used to replace the corresponding section of pKSMF-Swa to give plasmid pKSMFSS. The SphI-SunI fragment from pKSMFSS, containing the P-M intergenic region, the M gene, and most of the F gene, was then ligated to the SunI-ClaI and ClaI-SphI fragments of pRPV2A to give pRPV2B.
RT-PCR and cloning of PPRV glycoprotein coding sequences.
To obtain cDNA copies of the open reading frame (ORF) sequences of the H and F genes of PPRV with the appropriate restriction enzyme sites for cloning into pRPV2B, the two sequences were independently amplified by RT-PCR using RNA from Vero cells infected with the attenuated Nigeria 75/1 vaccine strain of PPRV. The H gene was amplified with primers PPRFAsc (5′-GGCGCGCCCTATTACACATTGGTCATC-3′) and PPRHPml (5′-CACGTGTACTCAGACTGGATTACAT-3′), and the F gene was amplified with primers PPRFSgf (5′-CAATTAGCGATCGCCCATGTATAAACATCAT-3′) and PPRFAscIR1 (5′-GGCGCGCCTTCTGGTCGGTGATCGGA-3′). The amplified DNAs were ligated into pGEM-T and sequenced.
Transfection and virus rescue.
Virus rescue in 293 cells was as previously described (5). For rescue in Vero cells, a new technique involving use of the recombinant fowlpox virus FP-T7 to express the T7 polymerase protein was used (17). Briefly, cells were plated at 2 × 105 cells/well in six-well plates 1 day before use. Cells were approximately 70% confluent at the time of transfection. The cells were infected at a multiplicity of approximately 0.2 with FP-T7 for 1 h and then transfected with pKS-N, pKS-P, pGEM-L, and the appropriate genome cDNA construct, using 1 μg of each plasmid except pGEM-L (50 ng). Transfection was carried out using FuGENE6 (Roche Biologicals) according to the manufacturer's instructions at a ratio of 7.5 μl of FuGENE6 per μg of DNA. Transfected cells were incubated for 4 or 5 days, by which time either CPE was visible (positive controls) or the cells were trypsinized and transferred to 75-cm2 flasks for further growth (chimeric constructs).
Virus characterization.
RT-PCR to characterize recombinant viruses was carried out as described above, using RNA isolated from Vero cells that had been infected with RPV, PPRV, or chimeric virus, along with the following primer pairs: RPVF14 (5′-ACCAAATCCATCCGAGCATC-3′) plus PPRF1 5′-ATCACAGTGTTAAAGCCTGTAGAGG-3′); PPRH1 (5′-TGGTCAGAGGGGAGAAT-3′) plus RPVH6 (5′-GGAGGCCCTGGTTTATAA-3′); and PPRF1 (5′-ATCACAGTGTTAAAGCCTGTAGAGG-3′) plus PPRH11 (5′-ATGTAGGGTCTTTCAATAGTT-3′).
Multistep growth curves were carried out by infecting Vero cells (approximately 70% confluent) with virus at a multiplicity of approximately 0.01. Virus was adsorbed to the cell monolayers in 35-mm-diameter dishes for 1 to 2 h, and then the inoculum removed, and the cells were washed three times with medium. Finally, 2 ml of medium was put into each well, and the cells were incubated for various times. At 0, 12, 24, 36, 48, and 72 h postinfection (hpi), the dishes were frozen at −70°C. Virus was harvested as normal, and the released virus was determined by measuring the TCID50.
Virus-induced CPE was visualized by infecting Vero cells in 35-mm-diameter dishes with 10 to 100 TCID50 of virus. After adsorption for 1 h, the virus inoculum was removed, and the cells were overlaid with 2 ml of 1% carboxymethyl cellulose in Eagle's MEM. Three days postinfection, the overlay was removed and 1 ml of undiluted Giemsa's stain (Merck) added. After 1 h, the stain and any remaining overlay were washed off with water, and the cell monolayer was photographed.
Immunofluorescence microscopy was performed as previously described (5). The antibodies used were C1 and C77 (monoclonal mouse anti-RPV H and anti-PPRV H, respectively) (2) and MB18 (rabbit anti-RPV P) (5).
Animal studies.
Indigenous British white goats between 3 and 12 months of age were used in these experiments, which were carried out under biosafety level 2 with regard to staff and at level 4 with regard to environmental release of pathogens. For vaccination, stocks of RPV2B, PPRV(Nigeria 75/1), and RPV-PPRFH were grown on Vero cells; 104 TCID50 of RPV2B or PPRV, or 103 TCID50 of RPV-PPRFH, was used to vaccinate each animal; 1 ml of virus was inoculated subcutaneously in the shoulder region. Challenge virus was 104 TCID50 of lamb kidney cell-grown PPRV(Ivory Coast 89/1), the kind gift of Adama Diallo, CIRAD/EMVT, Cedex, France. Rectal temperatures were recorded daily, and the animals were examined every second day for specific clinical signs such as oral lesions, salivation, or ocular or nasal discharges. Blood was collected at 2-day intervals for serum (nonheparinized) or PBL counting and purification (heparinized blood). PBL were purified as previously described (34). Swabs were taken at 2-day intervals from both eyes.
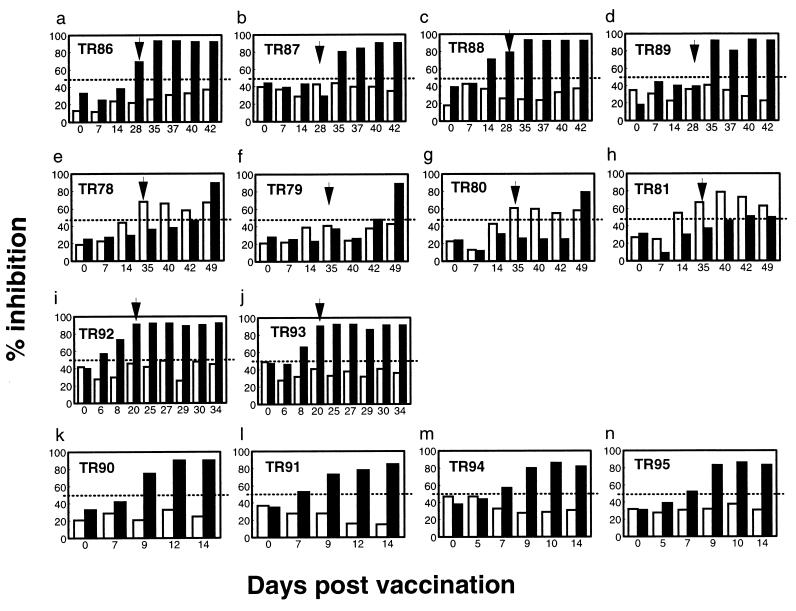
Serum antibody to RPV or PPRV H protein was measured using species-specific competitive enzyme-linked immunosorbent assay (cELISA) as described in reference 2; this assay determines the amount of antibody in a serum sample that recognizes a specific virus antigen by the ability of that sample to inhibit the binding of an antigen-specific monoclonal antibody to viral antigen. Results were expressed as percent inhibition of binding of the control monoclonal antibody.
RESULTS
Plasmid construction.
To construct RPV/PPRV chimeras, it was necessary first to insert suitable restriction sites at the beginning and end of the ORFs to be exchanged. We therefore inserted unique sites (i) just before the beginning of the F ORF (SgfI), (ii) just after the F ORF and before the F-H intergenic sequence (AscI), and (iii) at the end of the H ORF and before the H-L intergenic sequence (PmlI), as described in detail in Materials and Methods. These sites enable us to remove either or both of the sequences encoding the viral glycoproteins. RPVs rescued from the resulting clones of the RPV genome (pRPV2A and -B) were indistinguishable from the original virus in both ease of rescue and growth in tissue culture (not shown).
Clones of the F and H genes of PPRV were prepared by RT-PCR from RNA isolated from cells infected with the attenuated Nigeria 75/1 strain and cloned into pGEM-T. These clones were then sequenced in their entirety and compared to the published sequences. Compared to the previously published sequence of the PPRV F gene (30; accession number Z37017), we found only four silent differences. Three differences were found between our sequence for the H gene of PPRV and that in the database (accession number Z81358), two of which gave rise to conservative changes in amino acid sequence (I212 to M and E535 to D) and one of which gave rise to a nonconservative change (I538 to T); these differences were confirmed by a second independently amplified copy of the PPRV H gene. The PPRV F and H genes and ORFs are the same length as the corresponding genes and ORFs of RPV; however, to make a usable primer at the end of the H gene of PPRV, it was found necessary to eliminate six bases of the PPRV H gene 3′ untranslated region (UTR).
The individual RPV F and H genes in plasmids pRPV2A and -B were then replaced with the corresponding regions from PPRV, giving plasmids pRPV-PPRF and pRPV-PPRH. In addition, the F gene of pRPV-PPRH was replaced with that of PPRV, giving plasmid pRPV-PPRFH.
Rescue of chimeric virus.
All three pRPV-based plasmids were used in rescue experiments as described previously (4, 5). Rescue of each plasmid was tried at least twice, using six 35-mm-diameter wells in each attempt. Although the parental plasmid pRPV2B was always rescued as live virus, no virus was recovered from cells transfected with pRPV-PPRF, pRPV-PPRH, or pRPV-PPRFH. Reasoning that the PPRV glycoproteins came from a virus that had been extensively adapted to Vero cells, and might therefore interact poorly with surface receptors in the initially transfected human cell line (293) or the marmoset lymphoblastoid cell line (B95a) used in the second stage of the rescue protocol, we attempted to perform the primary transfection in Vero cells. However, although the recombinant vaccinia virus MVA-T7 does not replicate in Vero cells, it causes sufficient CPE that most of the Vero cells had died 3 to 4 days after infection with this virus. Rescue of a slow-growing morbillivirus by this system was therefore not possible.
FP-T7, another recombinant poxvirus expressing T7 RNA polymerase, has recently been produced (11). This virus is even more host range restricted than the MVA strain of vaccinia virus, growing only on avian cells. FP-T7-infected Vero cells showed no observable CPE up to 8 days postinfection. We therefore further adapted our rescue protocol to use FP-T7 and repeated the transfection in Vero cells. After transfection, the cells were passaged at 4- to 5-day intervals until CPE could be seen. The CPE due to rescued RPV2B could be seen before the first passage, and virus could reproducibly be rescued from pRPV-PPRFH, although two passages of the transfected cells were necessary before CPE could be seen. Again, despite at least three attempts with each plasmid and passaging of the transfected cells four additional times, no virus could be rescued from pRPV-PPRF or pRPV-PPRH.
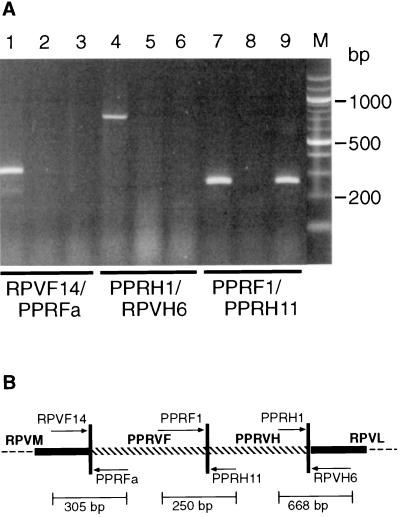
To confirm the identity of the rescued virus as RPV-PPRFH, RT-PCR was performed on RNA from Vero cells infected with the virus, using primer pairs that were specific for the conjunctions of RPV and PPRV sequences that could exist only in the chimeric virus (Fig. 1). As illustrated in Fig. 1B, primers RPVF14 and PPRFa prime in the RPV F gene 5′ UTR and the PPRV F ORF, respectively, and should generate a PCR product of the expected size from RPV-PPRFH but not from either PPRV or RPV. Similarly, primers PPRH1 and RPVH6, which prime in the PPRV H ORF and near the end of the RPV H 3′ UTR, respectively, generate a product from the chimera but not from either parental virus. The third primer pair, PPRF1 plus PPRH11, was used to show that the PPR F and H genes were in the correct positions relative to one another and that the virus was indeed the predicted chimeric construct. No PCR product was generated in parallel reactions from which the reverse transcriptase was omitted (data not shown).
FIG. 1.
Confirmation of gene order in the chimeric virus by RT-PCR. (A) RNA isolated from virus-infected cells was analyzed by RT-PCR using the indicated primer pairs. The virus used was RPV-PPRFH (tracks 1, 4, and 7), RPV (tracks 2, 5, and 8), or PPRV (tracks 3, 6, and 9). (B) Line diagram the F-H gene region that should exist in the chimeric RPV-PPRFH virus. Positions of the primers used in the PCRs are shown, and lengths of the expected amplification products are indicated.
In vitro characterization of the chimeric virus.
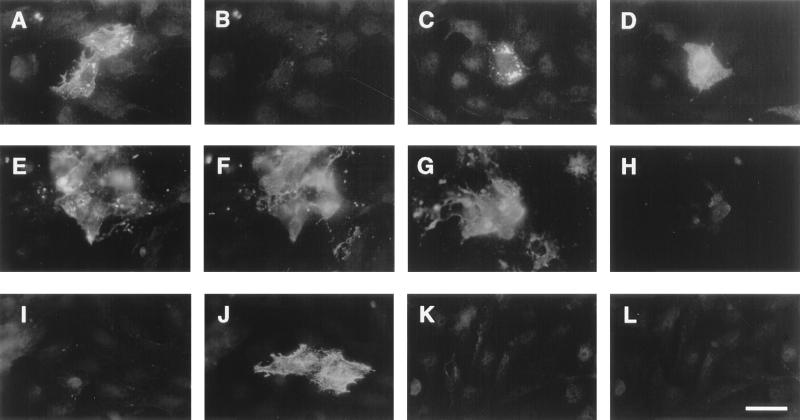
The nature of the recombinant virus was further confirmed by immunofluorescence microscopy on cells infected with RPV, PPRV, or RPV-PPRFH (Fig. 2). Rabbit polyclonal antibody MB18, which was raised against a fusion protein containing the C terminus of the RPV P protein and recognizes RPV P but not PPRV P (Fig. 2), was used to identify cells expressing RPV core proteins. Monoclonal antibodies specific for the H proteins of the parental viruses have been isolated and routinely used in virus-specific ELISAs (2). The chimeric virus produced the PPRV H protein, as seen by reaction with monoclonal antibody C77 (anti-PPRV H) but not with C1 (anti-RPV H). The same cells were also labeled by MB18, unlike cells infected with normal PPRV (Fig. 2), showing that the chimeric virus expresses a different combination of proteins than either parent.
FIG. 2.
Immunofluorescence microscopy of cells infected with parental (RPV or PPRV) or chimeric virus. All cells were incubated with rabbit anti-RPV P protein (MB18) combined with either mouse anti-RPV H protein (C1) or mouse anti-PPRV H protein (C77) and then with fluorescein isothiocyanate-labeled goat anti-rabbit immunoglobulin G combined with Texas red-labeled goat anti-mouse immunoglobulin G. (A to D) RPV2B; (E to H) RPV-PPRFH; (I to L) PPRV. (A, E, and I) Staining with MB18; (B, F, and J) same cells stained with C77; (C, G, and K) staining with MB18; (D, H, and L) same cells stained with C1. Bar in panel L = 10 μm.
To characterize the virus particles produced by the chimera, the monoclonal antibodies specific for each parental virus were used to immunoprecipitate virus from suspension. The titer of virus that was not precipitated was then determined. As can be seen from the data in Table 1, anti-RPV H antibody C1 precipitated RPV but neither PPRV nor RPV-PPRFH. Anti-PPRV H antibody C77, on the other hand, precipitated both PPRV and RPV-PPRFH equally well, indicating that the H glycoprotein, at least, in the chimera was derived from PPRV. Unfortunately, virus-specific reagents that will discriminate the F proteins of RPV and PPRV have not yet been produced.
TABLE 1.
Immunoprecipitation of normal and chimeric viruses by virus-specific antibodiesa
| Virus | Titer
|
||
|---|---|---|---|
| Anti-PPRVH | Anti-RPVH | Anti-BTV | |
| RPV-PPRFH | 0, 101.6 | 102.2, 102.7 | 101.6, 102.6 |
| RPV2B | 102.8, 102.6 | 0, 0 | 102.9, 102.5 |
| PPRV | 0, 101.2 | 102.5, 102.3 | 102.3, 102.3 |
Approximately 103 TCID50 of each virus was incubated with virus-specific antibody, and the unbound virus was assayed by determining the TCID50 titer. Results from two separate experiments are shown. An unrelated anti-bluetongue virus (anti-BTV) was used as a negative control.
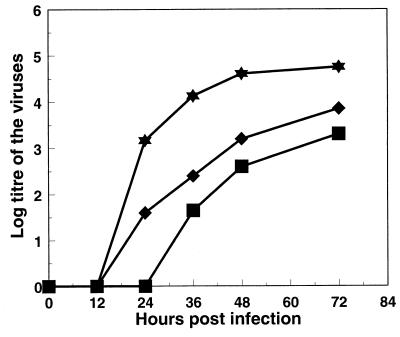
Standard multistep growth curves of RPV, PPRV, and RPV-PPRFH (Fig. 3) showed that the chimera grew more slowly in Vero cells than either parent. At 24 hpi, progeny virus could be detected for both RPV and PPRV, but RPV-PPRFH was detectable only at 36 hpi. Similarly, the final titer reached was lower for RPV-PPRFH than for either parental virus (Fig. 3).
FIG. 3.
Growth of RPV-PPRFH in tissue culture. Vero cells infected with PPRV (diamonds), RPV2B (stars), or RPV-PPRFH (squares) were frozen at different times postinfection, and the titer of virus present was determined as the TCID50.
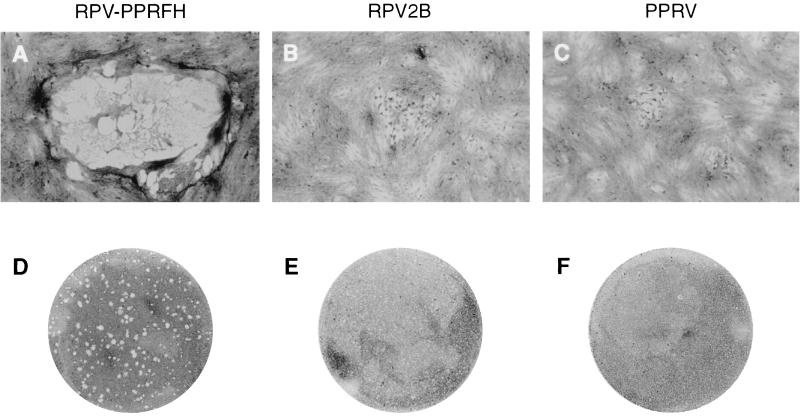
Examination of the CPE caused by each of these three viruses (Fig. 4) showed that despite the apparent low rate of virus replication in the chimera, the numbers of cells infected by cell-cell spread, as indicated by the numbers of cells affected in individual foci of infection, were at least as high in RPV-PPRFH as in either PPRV or RPV. In addition, a very large number of what appear to be disintegrating syncytia were seen in cells infected with the chimera (Fig. 4A and D). This morphology was unique to the chimera and was not seen in cells infected with either RPV or PPRV (compare Fig. 4D with Fig. 4E and F).
FIG. 4.
Plaque morphology of chimeric virus. Vero cells were infected with about 500 TCID50 of each virus and cultured under carboxymethyl cellulose. After staining, the cells were photographed at a magnification of ×100 (A to C) or the tissue culture dishes were photographed directly (D to F).
In vivo characterization of the chimeric virus.
RPV-PPRFH was also tested for efficacy as a vaccine, comparing it to the two parental viruses, RPV and PPRV. We infected four goats with RPV2B, four with RPV-PPRFH, and two with PPRV(Nigeria-75/1); six were left unvaccinated (for clarity, data from only four of these control animals are shown in the following figures). All animals were challenged with a pathogenic strain of PPRV (Ivory Coast) 3 to 5 weeks postvaccination.
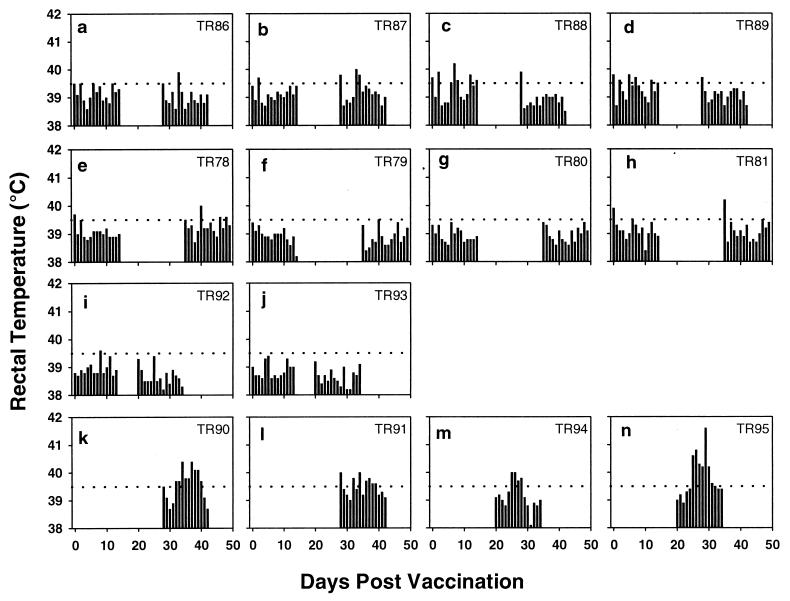
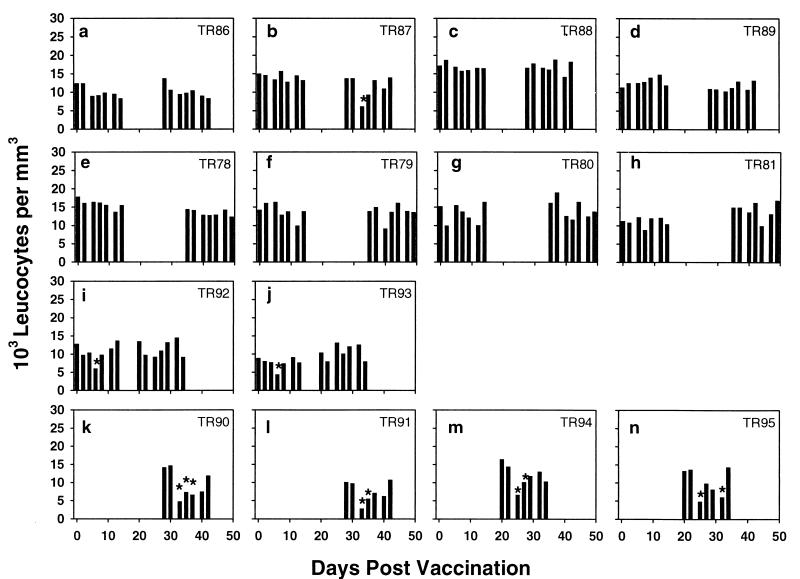
No specific clinical signs were observed in any experimental animal after vaccination. Two animals vaccinated with RPV-PPRFH showed a brief and mild pyrexia (Fig. 5a, TR88 and TR89); otherwise, no animal showed a temperature response due to inoculation of any vaccine (Fig. 5). No leukopenia was seen in animals vaccinated with RPV or RPV-PPRFH, but both animals vaccinated with PPRV showed a transient fall in leukocyte count (Fig. 6). This difference may be due to PPRV being primarily a goat/sheep virus, and RPV primarily a cattle virus, as we see a similar leukopenia in cattle vaccinated with the RPV vaccine strain.
FIG. 5.
Rectal temperatures of animals subjected to vaccination and challenge. Animals were vaccinated with RPV-PPRFH (a to d), RPV2B (e to h), or PPRV (i and j) or were left unvaccinated (k to n). Rectal temperatures were recorded daily for 2 weeks following vaccination and challenge. The temperature (39.5°C) above which the animals were considered to be pyrexic is indicated by a dotted line.
FIG. 6.
Leukocyte counts of animals subjected to vaccination and challenge. Animals were vaccinated as in Fig. 5, and blood samples were taken at 3- to 4-day intervals. Total leukocyte counts were determined as in Materials and Methods. Measurements which were less than 50% of the initial count for a particular animal are indicated by asterisks.
After challenge, the unvaccinated animals all showed the expected pyrexia and leukopenia (Fig. 5 and 6); in addition, the upper and lower gums and lips and the nasal septum showed congestion and subsequent lesions and ulcers. These healed gradually, and all animals had recovered by day 14, following the normal pattern of the disease in British goats. In contrast, none of the vaccinated animals showed any PPR-specific or nonspecific clinical signs following challenge, apart from two animals vaccinated with RPV-PPRFH which showed a brief pyrexia (Fig. 5a, TR86 and TR87). Even for these animals, however, the period of fever was much shorter than that for the unvaccinated controls.
Eye swabs and purified PBL were tested for the presence of viral RNA by RT-PCR following vaccination and challenge. No viral RNA was detected in these samples from the vaccinated animals, whereas the ocular swabs from five of the unvaccinated controls were positive for viral RNA by 7 days postchallenge.
Sera from the experimental animals were assayed by cELISA for antibodies recognizing the RPV and PPRV H proteins (Fig. 7). In these assays, the ELISA plates are coated with virus antigen (RPV or PPRV), and the reaction with a virus-specific monoclonal antibody is measured in the presence or absence of test serum. If the test serum contains antibodies specific for the coating virus, it will inhibit binding of the monoclonal antibody and hence a reduction in color will be observed. A value of 50% inhibition was taken as the cutoff value for a positive result, giving a specificity of 99.5% in distinguishing positive from negative sera. Animals vaccinated with PPRV showed the expected appearance of anti-PPRV H antibodies, which reached maximum value by 20 days postvaccination, i.e., before challenge (Fig. 7i and j). In contrast, only two out of four animals vaccinated with RPV-PPRFH showed detectable anti-PPRV H antibodies before challenge, though all showed a rapid anamnestic rise in such antibodies after challenge (Fig. 7a to d), suggesting that limited replication of the challenge virus was taking place. Despite the absence of detectable anti-PPRV antibodies in some animals, all the animals were protected. Similarly, only three out of four animals vaccinated with RPV2B showed detectable anti-RPV H antibodies during the experiment, yet all four were protected from subsequent challenge with PPRV. Again, all four of the animals in this group developed anti-PPRV H antibodies after challenge (Fig. 7e to h), though more slowly than the unvaccinated animals (Fig. 7k to n).
FIG. 7.
Antibody responses in animals subjected to vaccination and challenge. Serum was isolated at weekly intervals from the animals described in the legends to Fig. 5 and 6, and levels of specific anti-RPV H (open bars) and anti-PPRV H (filled bars) were determined by cELISA. The average of duplicate readings is plotted. Values above 50% inhibition (indicated by the dotted lines) were taken to be positive, and the day of challenge is indicated by an arrow for the vaccinated animals (A to J).
DISCUSSION
All paramyxoviruses have two envelope glycoproteins, one (F) which appears to mediate fusion of the virus envelope with the host cell plasma membrane, and a second (variously H or HN, or G in the pneumoviruses) which is the attachment or receptor-binding protein by which the virus associates with the target cell. In infected cells, or when expressed from cDNA clones, these proteins cause fusion of the plasma membranes of adjacent cells to create syncytia, a characteristic of paramyxovirus cytopathology. Although the F protein of simian virus 5 appears to be able to cause syncytium formation by itself (25, 36), as does that of respiratory syncytial virus (35) and MV (1), other studies with a number of paramyxoviruses have found that both glycoproteins are required for cell-cell fusion (19, 23, 31, 32, 38, 46, 48). This discrepancy has been ascribed to differences in the expression systems used (23). Although it was originally thought that the role of the H/HN protein in syncytium formation was simply to bring cell surfaces close enough together for fusion to take place, a number of studies showed that functional interaction of the two glycoproteins required that they be derived from the same virus (10, 23, 25, 26) and that sometimes even the glycoproteins of different strains of the same virus could not bring about syncytium formation (14). If syncytium formation by a pair of viral glycoproteins can be taken as a measure of the ability of a virus expressing those proteins to enter its host cell, these observations would suggest that any chimera between two paramyxoviruses should contain F and H/HN genes from the same virus. However, two other studies showed that combinations of glycoproteins from two morbilliviruses (CDV and MV) could function together to cause cell fusion (33, 43). The rate of appearance was lower and the syncytia were smaller when a heterologous pair of proteins was used than when both proteins were from the same virus (43), and MV H together with CDV F was more effective than the reverse pairing (33). It was therefore possible that heterologous combinations of RPV and PPRV F and H proteins might function adequately to allow recovery of viable virus.
Despite many attempts, in all of which control RPV genome plasmids were rescued into viable virus, we were unable to rescue virus in which only one of the two glycoprotein genes of RPV was swapped with the corresponding PPRV gene. That the clones of the PPRV F and H genes were functional was demonstrated by the reproducible rescue of RPV-PPRFH. These observations suggest that type-specific interactions between F and H/HN are important not only in syncytium formation but also in virus entry, or possibly in virus assembly and budding. Some combinations of viral proteins, expressed in certain ways, may allow low levels of cell-cell fusion, but this does not appear to mean that these proteins could function in vivo to fuse the viral envelope with the host cell. The only published report of a similar paramyxovirus chimera published, between human parainfluenza virus types 1 and 3 (hPIV1 and hPIV3) (45), also involved a change of both glycoproteins simultaneously.
In tissue culture, RPV-PPRFH grew much more slowly than either of the parental viruses. In this respect, the RPV/PPRV chimera resembled recombinant MVs in which the F and H genes were replaced with the single attachment/fusion glycoprotein G from vesicular stomatitis virus (42). In the same study, it was shown that the cytoplasmic domain of the MV F protein was required for incorporation of the viral M protein into the budding virion. There is also direct evidence for interactions of the M protein of the related Sendai virus with the cytoplasmic domains of both viral glycoproteins (40, 41). It is possible, therefore, that the defective growth of RPV-PPRFH is due to defective interaction of the cytoplasmic domains of one or both of the PPRV glycoproteins with the RPV M protein. However, a number of other observations provide evidence against this hypothesis. The cytoplasmic domains of morbillivirus F proteins are highly conserved, being identical over the last 14 amino acids in all morbilliviruses studied (30), and so the change introduced to this domain in exchanging the F proteins of the two viruses is small. In addition, another study of recombinant MVs (13) showed that changes to the cytoplasmic domains of F and H glycoproteins, including deletion of 14 amino acids from the cytoplasmic domain of H and replacement of the cytoplasmic domain of F with that of Sendai virus F (no sequence similarity to the cytoplasmic domain of MV F), led to viruses which grew to titers similar to those for the parental MV strain, albeit with a highly fusogenic phenotype, with large syncytia, similar to the type of CPE caused by RPV-PPRFH. These viruses with highly altered cytoplasmic domains on their glycoproteins showed reduced incorporation of the M protein into virions, and it was suggested that M protein binding to the one or other of the glycoproteins suppresses fusogenic potential (13) as a means of reducing active fusion of newly synthesized virus with membranes of the host cell. Further studies will be required to determine if our chimera is defective in incorporation of the M protein into virions and if the growth defect can be rectified by including the PPRV M protein as well as the F and H proteins. Since the morbillivirus M protein also interacts specifically with the viral nucleocapsid (24, 44), such a substitution may introduce other defects, and it may prove necessary to identify and swap specific M protein domains which interact with the viral envelope glycoproteins. An important result from these studies has been that the exchange of glycoproteins between two morbilliviruses with relatively closely related sequences led to a defective virus. By contrast, a chimera of hPIV3 containing the F and HN of hPIV1 was fully viable (45). Despite being in the same genus, hPIV3 and hPIV1 show almost no sequence similarity between the corresponding cytoplasmic domains of their glycoproteins. There may therefore be a significant difference in the assembly of viruses of these two groups.
An unexpected finding in this study was that the chimera could not be rescued by transfecting 293 cells. These cells have been used for the rescue of both MV and RPV (4, 38), even though these viruses were not specifically adapted to growth in these cells. It was subsequently observed that the (Vero-adapted) Nigeria strain of PPRV did not appear to grow in this cell line. It may be that these cells lack or are deficient in a specific attachment protein or an intracellular host protein necessary for efficient PPRV replication. The change of glycoproteins appeared to be a strong determinant of host range for the chimera since it readily infected and grew in Vero cells but not in the B95a lymphoblastoid cell line; these cells are a good host for RPV (27) but did not support replication of our PPRV strain unless the virus was adapted through five or six blind passages.
Despite its apparent attenuation in growth relative to its parents, the chimera successfully protected vaccinated animals from subsequent challenge. The effect of PPRV challenge on unvaccinated animals seen here was much less severe than seen in earlier studies on American mixed-breed animals (12). This may be due to differences in the susceptibility of different strains of goat or to the fact that we used PPRV grown in tissue culture rather than whole blood from an infected goat. However, the clinical responses in unvaccinated animals upon challenge in the present study were clear and readily distinguishable from those of vaccinated animals. Although two of the animals vaccinated with RPV-PPRFH showed no serum antibody to PPRV H protein before challenge, all four experimental animals were protected, possibly due to cell-mediated immunity, priming of the antibody response, or a combination of the two. As yet, very little is known about the role of cell-mediated immune responses in protection from RPV or PPRV infection. All animals vaccinated with RPV-PPRFH showed a clear anamnestic response in serum anti-PPRV H after challenge, which is not seen in animals vaccinated with RPV, showing that the antibody response is more PPRV specific in this system. In addition, vaccinated animals should generate a serological signature distinct from that generated by exposure to either RPV or PPRV, with antibodies recognizing unique epitopes on RPV N (28, 29) and on PPRV H (2). This may allow the chimera to be used as a genetically marked vaccine, which will be useful both in the RPV eradication campaign and for the control of PPRV, requiring epidemiological seromonitoring of PPRV prevalence and spread in the presence of vaccination. However, further clinical trials involving animals of different genetic backgrounds, and tests of longevity of the protection afforded by the vaccine, are required to establish its clinical safety and effectiveness.
ACKNOWLEDGMENTS
S. C. Das was the recipient of a Commonwealth Fellowship.
We thank John Anderson for reagents and advice on performing the ELISAs and Brian Taylor and Natasha Smith for assistance with and care of the animals used in these studies.
REFERENCES
- 1.Alkhatib G, Richardson C, Shen S H. Intracellular processing, glycosylation, and cell-surface expression of the measles virus fusion protein (F) encoded by a recombinant adenovirus. Virology. 1990;175:262–270. doi: 10.1016/0042-6822(90)90207-8. [DOI] [PubMed] [Google Scholar]
- 2.Anderson J, McKay J A. The detection of antibodies against peste des petits ruminants virus in cattle, sheep and goats and the possible implications to rinderpest control programmes. Epidemiol Infect. 1994;112:225–231. doi: 10.1017/s0950268800057599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baron M D, Barrett T. Sequencing and analysis of the nucleocapsid (N) and polymerase (L) genes and the terminal extragenic domains of the vaccine strain of rinderpest virus. J Gen Virol. 1995;76:593–602. doi: 10.1099/0022-1317-76-3-593. [DOI] [PubMed] [Google Scholar]
- 4.Baron M D, Barrett T. Rescue of rinderpest virus from cloned cDNA. J Virol. 1997;71:1265–1271. doi: 10.1128/jvi.71.2.1265-1271.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baron M D, Foster-Cuevas M, Baron J, Barrett T. Expression in cattle of epitopes of a heterologous virus using a recombinant rinderpest virus. J Gen Virol. 1999;80:2031–2039. doi: 10.1099/0022-1317-80-8-2031. [DOI] [PubMed] [Google Scholar]
- 6.Belsham G J, Anderson E C, Murray P K, Anderson J, Barrett T. Immune response and protection of cattle and pigs generated by a vaccinia virus recombinant expressing the F-protein of rinderpest virus. Vet Rec. 1989;124:655–658. doi: 10.1136/vr.124.25.655. [DOI] [PubMed] [Google Scholar]
- 7.Bidjeh K, Ouagal M, Diallo A, Bornarel P. Transmission of rinderpest virus strains of different virulence to goats in Chad. Ann Med Vet. 1997;141:65–69. [Google Scholar]
- 8.Blixenkrone-Möller M, Bolt G, Jensen T D, Harder T, Svansson V. Comparative analysis of the attachment protein gene (H) of dolphin morbillivirus. Virus Res. 1996;40:47–55. doi: 10.1016/0168-1702(95)01254-0. [DOI] [PubMed] [Google Scholar]
- 9.Bolt G, Blixenkronemoller M, Gottschalck E, Wishaupt R G A, Welsh M J, Earle J A P, Rima B K. Nucleotide and deduced amino acid sequences of the matrix (M) and fusion (F) protein genes of cetacean morbilliviruses isolated from a porpoise and a dolphin. Virus Res. 1994;34:291–304. doi: 10.1016/0168-1702(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 10.Bousse T, Takimoto T, Gorman W L, Takahashi T, Portner A. Regions on the hemagglutinin-neuraminidase proteins on human parainfluenza virus type-1 and Sendai virus important for membrane fusion. Virology. 1994;204:506–514. doi: 10.1006/viro.1994.1564. [DOI] [PubMed] [Google Scholar]
- 11.Britton P, Green P, Kottier S, Mawditt K L, Penzes P, Cavanagh D, Skinner M A. Expression of bacteriophage T7 RNA polymerase in avian and mammalian cells by a recombinant fowlpox virus. J Gen Virol. 1996;77:963–967. doi: 10.1099/0022-1317-77-5-963. [DOI] [PubMed] [Google Scholar]
- 12.Brown C C, Mariner J C, Olander H J. An immunohistochemical study of the pneumonia caused by peste des petits ruminants. Vet Pathol. 1991;28:166–170. doi: 10.1177/030098589102800209. [DOI] [PubMed] [Google Scholar]
- 13.Cathomen T, Naim H Y, Cattaneo R. Measles virus with altered envelope protein cytoplasmic tails gain cell fusion competence. J Virol. 1998;72:1224–1234. doi: 10.1128/jvi.72.2.1224-1234.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cattaneo R, Rose J K. Cell fusion by the envelope glycoproteins of persistent measles viruses which caused lethal human brain disease. J Virol. 1993;67:1493–1502. doi: 10.1128/jvi.67.3.1493-1502.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chlorofrom extraction. Anal Biochem. 1987;162:156–159. doi: 10.1006/abio.1987.9999. [DOI] [PubMed] [Google Scholar]
- 16.Couacy-Hymann E, Bidjeh K, Angba A, Domenech J, Diallo A. Protection of goats against rinderpest by vaccination with attenuated peste des petits ruminants virus. Res Vet Sci. 1995;59:106–109. doi: 10.1016/0034-5288(95)90041-1. [DOI] [PubMed] [Google Scholar]
- 17.Das, S. C., M. D. Baron, M. Skinner, and T. Barrett. Improved technique for transient expression and negative strand virus rescue using fowlpox T7 recombinant virus in mammalian cells. J. Virol. Methods, in press. [DOI] [PubMed]
- 18.Deng W P, Nickoloff J A. Site-directed mutagenesis of virtually any plasmid by eliminating a unique site. Anal Biochem. 1992;200:81–88. doi: 10.1016/0003-2697(92)90280-k. [DOI] [PubMed] [Google Scholar]
- 19.Ebata S N, Cote M-J, Kang C Y, Dimock K. The fusion and hemagglutinin-neuraminidase glycoproteins of human parainfluenza virus 3 are both required for fusion. Virology. 1991;183:437–441. doi: 10.1016/0042-6822(91)90162-5. [DOI] [PubMed] [Google Scholar]
- 20.Food and Agriculture Organization. Prevention and control of transboundary animal diseases. Report of the FAO expert consultation on the emergency prevention system (EMPRES) for transboundary animal and plant pests and diseases (livestock diseases programme) including the blueprint for global rinderpest eradication. FAO Animal Products Health Paper 133. Rome, Italy: Food and Agriculture Organization; 1997. [Google Scholar]
- 21.Forsyth M A, Barrett T. Evaluation of polymerase chain reaction for the detection and characterization of rinderpest and peste des petits ruminants viruses for epidemiologic studies. Virus Res. 1995;39:151–163. doi: 10.1016/0168-1702(95)00076-3. [DOI] [PubMed] [Google Scholar]
- 22.Giavedoni L, Jones L, Mebus C, Yilma T. A vaccinia virus double recombinant expressing the F and H genes of rinderpest virus protects cattle against rinderpest and causes no pock lesions. Proc Natl Acad Sci USA. 1991;88:8011–8015. doi: 10.1073/pnas.88.18.8011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heminway B R, Yu Y, Galinski M S. Paramyxovirus mediated cell fusion requires coexpression of both the fusion and hemagglutinin-neuraminidase glycoproteins. Virus Res. 1994;31:1–16. doi: 10.1016/0168-1702(94)90066-3. [DOI] [PubMed] [Google Scholar]
- 24.Hirano A, Wang A H, Gombart A F, Wong T C. The matrix proteins of neurovirulent subacute sclerosing panencephalitis virus and its acute measles virus progenitor are functionally different. Proc Natl Acad Sci USA. 1992;89:8745–8749. doi: 10.1073/pnas.89.18.8745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horvath C M, Paterson R G, Shaughnessy M A, Wood R, Lamb R A. Biological activity of paramyxovirus fusion proteins: factors influencing formation of syncytia. J Virol. 1992;66:4564–4569. doi: 10.1128/jvi.66.7.4564-4569.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu X, Ray R, Compans R W. Functional interactions between the fusion protein and hemagglutinin-neuraminidase of human parainfluenza viruses. J Virol. 1992;66:1528–1534. doi: 10.1128/jvi.66.3.1528-1534.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kobune F, Sakata H, Sugiyama M, Sugiura A. B95a, a marmoset lymphoblastoid cell line, as a sensitive host for rinderpest virus. J Gen Virol. 1991;72:687–692. doi: 10.1099/0022-1317-72-3-687. [DOI] [PubMed] [Google Scholar]
- 28.Libeau G, Diallo A, Calvez D, Lefevre P C. A competitive ELISA using anti-N monoclonal antibodies for specific detection of rinderpest antibodies in cattle and small ruminants. Vet Microbiol. 1992;31:147–160. doi: 10.1016/0378-1135(92)90073-3. [DOI] [PubMed] [Google Scholar]
- 29.McCullough K C, Obi T U, Sheshberadaran H. Identification of epitope(s) on the internal virion proteins of rinderpest virus which are absent from peste-des-petits ruminants virus. Vet Microbiol. 1991;26:313–321. doi: 10.1016/0378-1135(91)90025-b. [DOI] [PubMed] [Google Scholar]
- 30.Meyer G, Diallo A. The nucleotide sequence of the fusion protein gene of the peste des petits ruminants virus—the long untranslated region in the 5′-end of the F-protein gene of morbilliviruses seems to be specific to each virus. Virus Res. 1995;37:23–35. doi: 10.1016/0168-1702(95)00013-g. [DOI] [PubMed] [Google Scholar]
- 31.Morrison T, McQuain C, McGinnes L. Complementation between avirulent Newcastle disease virus and fusion protein gene expressed from a retrovirus vector: requirement for membrane fusion. J Virol. 1991;65:813–822. doi: 10.1128/jvi.65.2.813-822.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moscona A, Peluso R W. Fusion properties of cells persistently infected with human parainfluenza virus 3: participation of hemagglutinin-neuraminidase in membrane fusion. J Virol. 1991;65:2773–2777. doi: 10.1128/jvi.65.6.2773-2777.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nussbaum O, Broder C C, Moss B, Stern L B L, Rozenblatt S, Berger E A. Functional and structural interactions between measles virus hemagglutinin and CD46. J Virol. 1995;69:3341–3349. doi: 10.1128/jvi.69.6.3341-3349.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ohishi K, Inui K, Yamanouchi K, Barrett T. Cell-mediated immune responses in cattle vaccinated with a vaccinia recombinant expressing the nucleocapsid protein of rinderpest virus. J Gen Virol. 1999;80:1627–1634. doi: 10.1099/0022-1317-80-7-1627. [DOI] [PubMed] [Google Scholar]
- 35.Olmsted R A, Elango N, Prince G A, Murphy B R, Johnson P R, Channock R M, Collins P L. Expression of the F glycoprotein of respiratory syncitial virus by a recombinant vaccinia virus: comparison of the individual contributions of the F and G glycoproteins to host immunity. Proc Natl Acad Sci USA. 1986;83:7462–7466. doi: 10.1073/pnas.83.19.7462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Paterson R G, Hiebert S W, Lamb R A. Expression at the cell surface of biologically active fusion and hemagglutinin/neuraminidase proteins of the paramyxovirus simian virus 5 from cloned cDNA. Proc Natl Acad Sci USA. 1985;82:7520–7524. doi: 10.1073/pnas.82.22.7520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Plowright W, Ferris R D. Studies with rinderpest virus in tissue culture. The use of attenuated culture virus as a vaccine for cattle. Res Vet Sci. 1962;3:172–182. [Google Scholar]
- 38.Radecke F, Spielhofer P, Schneider H, Kaelin K, Huber M, Dotsch C, Christiansen G, Billeter M A. Rescue of measles viruses from cloned DNA. EMBO J. 1995;14:5773–5784. doi: 10.1002/j.1460-2075.1995.tb00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sakai Y, Shibuta H. Syncytium formation by recombinant vaccinia viruses carrying bovine parainfluenza virus envelope protein genes. J Virol. 1989;63:3661–3668. doi: 10.1128/jvi.63.9.3661-3668.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sanderson C M, McQueen N L, Nayak D P. Sendai virus assembly: M protein binds to viral glycoproteins in transit through the secretory pathway. J Virol. 1993;67:651–653. doi: 10.1128/jvi.67.2.651-663.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanderson C M, Wu H-H, Nayak D P. Sendai virus M protein binds independently to either the F or the HN glycoprotein in vivo. J Virol. 1994;68:69–76. doi: 10.1128/jvi.68.1.69-76.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spielhofer P, Bächi T, Fehr T, Christiansen G, Cattaneo R, Kaelin K, Billeter M A, Naim H Y. Chimeric measles viruses with a foreign envelope. J Virol. 1998;72:2150–2159. doi: 10.1128/jvi.72.3.2150-2159.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stern L, Greenberg M, Gershoni J M, Rozenblatt S. The hemagglutinin envelope protein of canine distemper virus (CDV) confers cell tropism as illustrated by CDV and measles virus complementation analysis. J Virol. 1995;69:1661–1668. doi: 10.1128/jvi.69.3.1661-1668.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suryanarayana K, Baczko K, ter Meulen V, Wagner R R. Transcription inhibition and other properties of matrix proteins expressed by M genes cloned from measles viruses and diseased human brain tissue. J Virol. 1994;68:1532–1543. doi: 10.1128/jvi.68.3.1532-1543.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tao T, Durbin A P, Whitehead S S, Davoodi F, Collins P L, Murphy B R. Recovery of a fully viable chimeric parainfluenza virus (PIV) type 3 in which the hemagglutinin-neuraminidase and fusion glycoproteins have been replaced by those of PIV type 1. J Virol. 1998;72:2955–2961. doi: 10.1128/jvi.72.4.2955-2961.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taylor J, Weinberg R, Tartaglia J, Richardson C, Alkhatib G, Briedis D, Appel M, Norton E, Paoletti E. Nonreplicating viral vectors as potential vaccines—recombinant canarypox virus expressing measles virus fusion (F) and hemagglutinin (HA) glycoproteins. Virology. 1992;187:321–328. doi: 10.1016/0042-6822(92)90321-f. [DOI] [PubMed] [Google Scholar]
- 47.Taylor W P. Protection of goats against peste-des-petits-ruminants with attenuated rinderpest virus. Res Vet Sci. 1979;27:321–324. [PubMed] [Google Scholar]
- 48.Wild T F, Malvoisin E, Buckland R. Measles virus—both the hemagglutinin and fusion glycoproteins are required for fusion. J Gen Virol. 1991;72:439–442. doi: 10.1099/0022-1317-72-2-439. [DOI] [PubMed] [Google Scholar]
- 49.Yamanouchi K, Inui K, Sugimoto M, Asano K, Nishimaki F, Kitching R P, Takamatsu H, Barrett T. Immunization of cattle with a recombinant vaccinia vector expressing the hemagglutinin gene of rinderpest virus. Vet Rec. 1993;132:152–156. doi: 10.1136/vr.132.7.152. [DOI] [PubMed] [Google Scholar]
- 50.Yilma T, Hsu D, Jones L, Owens S, Grubman M, Mebus C, Yamanaka M, Dale B. Protection of cattle against rinderpest with vaccinia virus recombinants expressing the HA or F-gene. Science. 1988;242:1058–1061. doi: 10.1126/science.3194758. [DOI] [PubMed] [Google Scholar]