Abstract
Background:
Previous systematic reviews have aimed to clarify the effect of telemedicine on diabetes. However, such reviews often have a narrow focus, which calls for a more comprehensive systematic review within the field. Hence, the objective of the present systematic review, meta-analysis, and meta-regression is to evaluate the effectiveness of telemedicine solutions versus any comparator without the use of telemedicine on diabetes-related outcomes among adult patients with type 2 diabetes (T2D).
Methods:
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We considered telemedicine randomized controlled trials (RCT) including adults (≥18 years) diagnosed with T2D. Change in glycated hemoglobin (HbA1c, %) was the primary outcome. PubMed, EMBASE, and the Cochrane Library Central Register of Controlled Trials (CENTRAL) were searched on October 14, 2020. An overall treatment effect was estimated using a meta-analysis performed on the pool of included studies based on the mean difference (MD). The revised Cochrane risk-of-bias tool was applied and the certainty of evidence was graded using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach.
Results:
The final sample of papers included a total of 246, of which 168 had sufficient information to calculate the effect of HbA1c%. The results favored telemedicine, with an MD of −0.415% (95% confidence interval [CI] = −0.482% to −0.348%). The heterogeneity was great (I2 = 93.05%). A monitoring component gave rise to the higher effects of telemedicine.
Conclusions:
In conclusion, telemedicine may serve as a valuable supplement to usual care for patients with T2D. The inclusion of a telemonitoring component seems to increase the effect of telemedicine.
Keywords: telemedicine, diabetes mellitus, type 2, systematic review, meta-analysis, meta-regression, Denmark
Introduction
Diabetes is one of the most common chronic diseases and a major health care problem worldwide.1,2 In 2017, an estimated 8.4% of the adult global population had diabetes, which is expected to increase to approximately 9.9% (700 million) in 2045, primarily due to an increase in unhealthy dietary habits, obesity, and sedentary lifestyle.1,2 The global prevalence is predicted to increase mostly in low- and middle-income countries. 3 The economic impact of diabetes is considerable, spans health care services, and affects individuals, families, and national productivity.1,4
Type 2 diabetes (T2D) constitutes approximately 90% to 95% of diabetes cases.1,5 The T2D is a progressive disease associated with significant premature mortality, morbidity, and several complications, such as cardiovascular disease, nephropathy, neuropathy, and retinopathy.6,7 Diabetes patient care is a multifaceted and complex process, mainly aimed at attaining optimal glycemic control to prevent and control diabetes-related complications. 8 However, sustaining optimal glycemic control for people with diabetes is both demanding and challenging because it requires numerous daily self-management decisions and care activities. 9 These challenges include estimating the appropriate diabetes medication dosage to avoid hypoglycemic and hyperglycemic events and adherence to obstacles in terms of following the recommended guidelines.8,9 Adherence to the complex T2D treatment regimen is difficult to maintain 10 and medial adherence rates have been reported to range from 36% to 93%. 11
Self-management strategies are considered an essential part of diabetes treatment and are associated with improvements in health-related outcomes. 9 A potential solution to support ongoing diabetes self-management support is the use of telemedicine, 12 which has been suggested as a promising but unproven approach to support people with diabetes in the management of their disease. 13 Telemedicine can be defined as the delivery of health care services over a distance using information and communication technologies. 14 However, no definitive definition exists. 14 Telemedicine solutions may include a variety of different technologies and various delivery forms, including monitoring, education, consultative services, coaching, and counseling tasks.13,15-17 Telemedicine interventions constitute different constellations, such as simple reminders via text messaging, video consultation, and transmission of patient data (eg, blood glucose, blood pressure, dietary and medication intake, and physical activity) with feedback from health care professionals via web portals or via telephone.13,15,16 As diabetes predominantly needs to be managed outside health care facilities and to a large extent requires self-management, telemedicine holds the potential to provide sufficient self-management support to people with T2D.18,19
Previous systematic reviews have aimed to clarify the effect of telemedicine on diabetes.15-17,20-28 However, these previous reviews have often focused on a specific type of telemedicine, a specific outcome, and/or a specific comparator, which calls for a more comprehensive and inclusive systematic review seeking to compare and synthesize findings for treatment outcomes while adjusting for different study characteristics. In addition, the field of telemedicine is developing rapidly; thus, a large number of studies likely have been published recently, calling for an updated review. 29 Hence, the objective of the present systematic review, meta-analysis, and meta-regression was to evaluate the effectiveness of telemedicine solutions versus any comparator without the use of telemedicine on diabetes-related outcomes among adult patients with T2D.
Methods
Study Design
This systematic review, meta-analysis, and meta-regression was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 30 A comprehensive search protocol was published elsewhere 31 and PROSPERO-registered with identification CRD42020123565 on April 2020. The search was part of a comprehensive search that included T2D as well as type 1 diabetes (T1D) and gestational diabetes 31 , which will be reported separately.
Eligibility Criteria
Studies were considered if they included adults (≥18 years) diagnosed with T2D. Studies that included mixed populations (eg, T1D and T2D) were only included if the data for the T2D population were reported separately. Studies were excluded if only participants at risk of diabetes or participants with prediabetes were included. Furthermore, the studies must have included telemedicine interventions that were substituted for usual practice or served as an alternative to usual practice. The telemedicine interventions had to include remote feedback/communication between a patient and health care professional(s). Alternatively, feedback/communication could occur between the patient and a trained peer. Telemedicine interventions that were wholly automatic were also considered.
Studies that reported on any relevant patient diabetes-related outcome were included. The primary outcome was change in glycated hemoglobin (HbA1c, %).
We only considered randomized controlled trials (RCTs)—both parallel and crossover designs. Studies published in English, Danish, Norwegian, and Swedish as peer-reviewed full-text papers were included. All studies published before October 14, 2020, were considered.
Information Sources
The search was performed in PubMed, EMBASE, the Cochrane Library Central Register of Controlled Trials (CENTRAL), and CINAHL. Two authors performed the database searches (S.H.L. and S.H.). A research librarian assisted. Additional citation searches were performed in the Web of Science, SCOPUS, and Google Scholar.
Search Strategy
Initially, an unstructured search was performed in PubMed, CINAHL, and Google Scholar to identify relevant search terms and thus qualify the systematic search. The systematic search followed the initial search. The search strategy was adapted for each database. The search terms included various synonyms, near-synonyms, acronyms, and spellings for all keywords and index terms. A variety of search functions were applied, including thesaurus, Boolean operators, abstract/title/keywords, phrase, truncation, free text, and advanced search. Citation searches were applied to identify additional studies.
Selection Process
First, all of the identified papers were uploaded into RefWorks (ProQuest RefWorks 2.0, 2010). Second, duplicates were removed using the functions Exact duplicates and Close duplicates. Third, titles and abstracts were screened by two authors with respect to the eligibility criteria of the review (S.H. and S.H.L.). Fourth, the remaining studies underwent full review by three authors with respect to the eligibility criteria of the review (S.H., S.H.L., and J.D.A.). Disagreement between the authors was resolved through discussion by the three authors alone or by inclusion of other authors. During the full review, the reasons for exclusion of studies were recorded, and afterward, a final sample of papers was identified.
Data Extraction
Data were extracted by three independent authors (S.H., S.H.L., and J.D.A.) using a standardized sheet in Microsoft Excel (2016). Extracted data included trial characteristics (author, publication year, country, sample size, and study duration), patient characteristics (age, sex, and body mass index [BMI]), and HbA1c outcomes. In addition, the characteristics of the telemedicine interventions were extracted, including the frequency of contact, implementation setting (primary care, hospital, specialized outpatient clinic, university, community or cross-sectional), peripherals (eg, glucometers, pedometers, blood pressure monitors, and scales), and the general purpose of intervention components (monitoring, consultation, counseling, coaching, education, mentoring, and reminding). Disagreements between the authors were resolved through discussion. Additional authors were included in the discussions when necessary.
Risk of Bias Assessment
The revised Cochrane risk-of-bias tool was applied. 32 Four reviewers (J.D.A., S.H., T.K., and F.W.U.) assessed the included studies independently and resolved potential disagreements by discussion.
Data Synthesis
All statistical analyses were performed in Stata 16 (Stata Statistical Software: Release 16, StataCorp 2019.; StataCorp LLC, College Station, Texas). Reported medians, interquartile ranges, ranges, and confidence intervals were transformed to means and standard deviations by traditional methods33,34 and scaled to HbA1c% when relevant (eg, if outcome was reported as mmol/mol). An overall treatment effect was estimated with a meta-analysis of the pool of included studies based on the mean difference (MD). Heterogeneity was assessed statistically using I2 tests. The results were combined with a random-effects model (due to heterogeneity, ie, an I2 statistic > 50%). Univariate a priori subgroup analyses based on meta-regression of the telemedicine characteristics were conducted and combined with post hoc analyses of the association of study and patient characteristics with the treatment effect of telemedicine. Publication bias was evaluated using visual inspection of the funnel plot and Egger test.
Certainty Assessment
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach was applied. A summary of findings (SoF) table was created using GRADEPro GDT 2015 (McMaster University, Ontario, Canada),35,36 which presents the absolute risks for the groups (treatment and control), estimates of relative risk, and ranking of the quality of the evidence, which is based on the risk of bias, 37 indirectness, 38 imprecision, 39 inconsistency, 40 and risk of publication bias. 41
Results
The flowchart in Figure 1 describes our selection of studies. In the literature search, 16 309 studies were found and 1125 eligible studies were assessed by full-text reading after screening titles and abstracts. After full-text assessment, 246 articles met our inclusion criteria.
Figure 1.
Flowchart.
Abbreviation: RCT, randomized controlled trial.
The characteristics of the individual studies are presented in Table 1. One study was multinational, 88 articles were conducted in North America (36%), 84 in Asia (35%), 44 in Europe (18%), 16 in Australia/New Zealand (7%), five in Africa (2%), and five in South America (5%). Four studies were published before 2000 (2%), 50 in the 2000s (21%), 165 in the 2010s (68%), and 24 (10%) in 2020. Sample sizes ranged from 17 to 4078, with an average of 251 participants per study. The study duration ranged from one to 96 months, with a study average of 8.5 months. Across studies, the mean proportion of men was 50.4% (range = 15%-100%), the average age at baseline was 57 (range = 37-73) years, and the baseline mean BMI was 30 (range = 22-40). The average baseline HbA1c% levels ranged from 5.70% to 11.05%, with an average of 8.33%.
Table 1.
Study and Participant Characteristics.
| Study | Publication year | Country | Sample size | Duration (months) | Mean age years | Male % | Baseline BMI | Baseline HbA1c |
|---|---|---|---|---|---|---|---|---|
| Abaza and Marschollek 42 | 2017 | Egypt | 90 | 3 | 52 | 44 | NA | 9.66 |
| Agarwal et al 43 | 2019 | Canada | 50 | 4 | 64 | 55 | NA | 7.44 |
| Agarwal et al 44 | 2019 | Canada | 240 | 3 | 52 | 52 | NA | 8.96 |
| Aguiar et al 45 | 2018 | Brazil | 80 | 12 | 62 | 67 | NA | 8.95 |
| Akinci et al 46 | 2018 | Turkey | 66 | 2 | 52 | 36 | 32 | 8.34 |
| Al Omar et al 47 | 2020 | United Arab Emirates | 218 | 6 | 42 | 42 | NA | 8.45 |
| Alanzi et al 48 | 2018 | Saudi Arabia | 20 | 6 | NA | 75 | NA | 8.53 |
| Albikawi et al 49 | 2016 | Jordan | 168 | 3 | 51 | 46 | NA | NA |
| Alghafri et al 50 | 2018 | Oman | 232 | 3 | 44 | 43 | 33 | 7.96 |
| Ali et al 51 | 2016 | India & Pakistan | 1146 | 30 | 54 | 46 | 27 | 9.90 |
| Ali et al 52 | 2020 | India | 404 | 24 | 53 | 41 | 27 | 9.15 |
| Aliha et al 53 | 2013 | Iran | 61 | 3 | 53 | 50 | 28 | 9.70 |
| Alonso-Domínguez et al 54 | 2019 | Spain | 204 | 3 | 61 | 54 | 30 | 6.85 |
| Alotaibi et al 55 | 2016 | Saudi Arabia | 20 | 6 | 45 | NA | NA | 8.55 |
| Anderson et al 56 | 2009 | USA | 310 | 24 | 56 | 41 | 34 | 7.48 |
| Anderson et al 57 | 2010 | USA | 295 | 12 | NA | 42 | 35 | 8.00 |
| Anderson-Loftin et al 58 | 2005 | USA | 97 | 6 | 57 | 23 | 35 | 7.90 |
| Andreae et al 59 | 2020 | USA | 230 | 3 | 59 | 20 | NA | 8.29 |
| Anzaldo-Campos et al 60 | 2016 | Mexico | 301 | 10 | 52 | 38 | 31 | 11.05 |
| Arora et al 61 | 2014 | USA | 128 | 6 | 51 | 36 | NA | 10.10 |
| Asante et al 62 | 2020 | Ghana | 60 | 3 | 56 | 22 | 28 | 8.95 |
| Avdal et al 63 | 2011 | Turkey | 122 | 6 | 52 | 49 | NA | 8.07 |
| Azizi et al 64 | 2016 | Iran | 72 | 4 | 55 | 50 | NA | NA |
| Benson et al 65 | 2018 | USA | 120 | 12 | 60 | 55 | 37 | 8.20 |
| Blackberry et al 66 | 2013 | Australia | 473 | 18 | 63 | 57 | NA | 8.06 |
| Bluml et al 67 | 2019 | USA | 446 | 3 | 54 | 41 | 37 | 10.25 |
| Boels et al 12 | 2019 | Netherlands | 230 | 6 | 59 | 60 | 32 | 8.20 |
| Bogner et al 68 | 2012 | USA | 182 | 3 | 57 | 32 | 34 | 7.10 |
| Bohingamu Mudiyanselage et al 69 | 2018 | Australia | 177 | 12 | 70 | 53 | NA | 5.70 |
| Lashkari et al 70 | 2013 | Iran | 50 | 3 | NA | NA | 29 | 9.68 |
| Browning et al 71 | 2016 | China | 711 | 12 | 64 | 52 | 26 | 10.45 |
| Bujnowska-Fedak et al 72 | 2011 | Poland | 100 | 6 | 55 | 54 | 25 | 7.65 |
| Buysse et al 73 | 2019 | Belgium | 153 | 24 | 37 | 50 | NA | 8.30 |
| Capozza et al 74 | 2015 | USA | 156 | 6 | 53 | 37 | NA | 9.11 |
| Carter et al 75 | 2011 | USA | 47 | 9 | 51 | 36 | 36 | 8.91 |
| Castelnuovo et al 76 | 2011 | Italy | 72 | 12 | 52 | 52 | NA | NA |
| Chao et al 77 | 2019 | Taiwan | 121 | 3 | NA | NA | 25 | 8.70 |
| Chen et al 78 | 2008 | Taiwan | 78 | 6 | 59 | 44 | 26 | 9.61 |
| Chen et al 79 | 2018 | China | 233 | NA | 59 | 51 | NA | NA |
| Chiu et al 80 | 2016 | Taiwan | 182 | 8 | 65 | 52 | 26 | 7.65 |
| Cho et al 81 | 2006 | Korea | 80 | 30 | 53 | 54 | 23 | 7.60 |
| Cho et al 82 | 2017 | Korea | 484 | 6 | 53 | 64 | 26 | 7.84 |
| Choe et al 83 | 2005 | USA | 80 | 14 | 52 | 47 | NA | 10.15 |
| Choudhry et al 84 | 2018 | USA | 4078 | 12 | 60 | 55 | NA | 9.65 |
| Clark et al 85 | 2004 | UK | 100 | 12 | 60 | 58 | 31 | 8.42 |
| Crowley et al 86 | 2013 | USA | 369 | 12 | 61 | 28 | NA | 8.00 |
| Crowley et al 87 | 2016 | USA | 50 | 6 | 60 | 96 | NA | 10.45 |
| Dale et al 88 | 2009 | UK | 231 | 6 | NA | 60 | NA | 8.56 |
| Dario et al 89 | 2017 | Italy | 299 | 12 | 73 | 56 | NA | 7.94 |
| Davis et al 90 | 2010 | USA | 165 | 12 | 60 | 25 | 37 | 8.96 |
| Del Prato et al 91 | 2012 | Italy | 291 | 5.5 | 58 | 52 | 30 | 8.86 |
| Delahanty et al 92 | 2019 | USA | 211 | 12 | 62 | 45 | 35 | 7.70 |
| Doupis et al 7 | 2019 | Greece | 457 | 8 | 63 | 51 | 31 | 7.85 |
| Dugas et al 93 | 2018 | USA | 27 | 3 | NA | 89 | NA | 9.23 |
| Duruturk and Özköslü 94 | 2019 | Turkey | 50 | 1.5 | 53 | NA | 31 | 7.36 |
| Döbler et al 95 | 2018 | Germany | 249 | 12 | 52 | 70 | 36 | 7.70 |
| Eakin et al 96 | 2013 | Australia | 302 | 6 | 58 | 56 | 33 | 7.45 |
| Eakin et al 97 | 2014 | Australia | 302 | 24 | 58 | 56 | 33 | 7.45 |
| Egede et al 98 | 2017 | USA | 113 | 6 | 54 | 19 | 36 | 10.10 |
| Egede et al 99 | 2018 | USA | 90 | 12 | 63 | 98 | NA | 7.11 |
| Estey et al 100 | 1990 | Canada | 60 | 4 | NA | 46 | NA | 6.21 |
| Faridi et al 101 | 2008 | USA | 30 | 3 | 56 | 37 | 36 | 6.45 |
| Farsaei et al 102 | 2011 | Iran | 172 | 3 | 53 | 34 | NA | 9.10 |
| Fernandes et al 103 | 2016 | Brazil | 219 | 6 | 63 | 31 | 29 | 8.07 |
| Fortmann et al 104 | 2017 | USA | 126 | 6 | 48 | 25 | 32 | 9.55 |
| Fottrell et al 105 | 2019 | Bangladesh | 2470 | 18 | NA | 47 | 22 | NA |
| Fountoulakis et al 106 | 2015 | Greece | 80 | 12 | 62 | 69 | 30 | 9.80 |
| Franc et al 107 | 2020 | France | 665 | 12 | 39 | 48 | 26 | 9.10 |
| Franciosi et al 108 | 2011 | Italy | 62 | 6 | 49 | 74 | 31 | 7.90 |
| Frosch et al 109 | 2011 | USA | 201 | 6 | 55 | 52 | 33 | 9.60 |
| García et al 110 | 2015 | USA | 72 | 6 | 50 | 33 | 36 | 8.60 |
| Garg et al 111 | 2017 | USA | 184 | 12 | 64 | 60 | 35 | 9.05 |
| Gagliardino et al 112 | 2013 | Argentina | 198 | 12 | 61 | 49 | 33 | 7.21 |
| Wasif Gillani 113 | 2016 | Malaysia | 150 | 6 | 53 | 55 | 28 | 9.89 |
| Gimbel et al 114 | 2020 | USA | 240 | 12 | 63 | 62 | 33 | 7.55 |
| Glasgow et al 115 | 2006 | USA | 327 | 2 | 62 | 50 | 32 | 7.45 |
| Glasgow et al 116 | 2006 | USA | 327 | 2 | 61 | 55 | 33 | 7.25 |
| Glasgow and Toobert 117 | 2000 | USA | 320 | 6 | 59 | 39 | NA | 7.60 |
| Glasgow et al 118 | 2002 | USA | 320 | 12 | 59 | 39 | NA | 7.59 |
| Glasgow et al 119 | 2005 | USA | 886 | 12 | 63 | 49 | NA | 7.32 |
| Goodarzi et al 120 | 2012 | Iran | 100 | 3 | 54 | 22 | 28 | 7.87 |
| Goodarzi et al 121 | 2018 | Iran | 76 | 3 | 57 | 100 | NA | NA |
| Graziano and Gross 122 | 2009 | USA | 120 | 3 | 62 | 55 | NA | 8.65 |
| Griffin et al 123 | 2014 | UK | 478 | 12 | 60 | 62 | 33 | 7.12 |
| Gupta et al 124 | 2020 | India | 81 | 4 | 50 | 52 | 28 | 8.45 |
| Haider et al 125 | 2019 | Australia | 229 | 6 | 59 | 83 | 31 | NA |
| Hansen et al 126 | 2017 | Denmark | 165 | 8 | 58 | 64 | 34 | 9.30 |
| Hare et al 127 | 2011 | Australia | 223 | 33 | 55 | 56 | 32 | 7.55 |
| Hee-Sung 128 | 2007 | South Korea | 60 | 3 | 50 | 42 | 24 | 6.82 |
| Heisler et al 129 | 2019 | USA | 290 | 6 | 63 | 98 | NA | 9.10 |
| Hidrus et al 130 | 2020 | Malaysia | 100 | 3 | NA | 50 | NA | NA |
| Hokanson et al 131 | 2006 | USA | 114 | 6 | 54 | 57 | 33 | 8.60 |
| Holbrook et al 132 | 2009 | Canada | 511 | 6 | 61 | 51 | 32 | 7.05 |
| Holmen et al 133 | 2014 | Norway | 151 | 12 | 57 | 55 | 31 | 8.25 |
| Hordern et al 134 | 2009 | Australia | 223 | 12 | 56 | 55 | 32 | 7.55 |
| Huang et al 135 | 2019 | Singapore | 50 | 3 | 52 | 49 | 29 | 8.65 |
| Huizinga et al 136 | 2010 | USA | 165 | 24 | 56 | 60 | 34 | 6.64 |
| Hunt et al 137 | 2014 | USA | 17 | 3 | NA | 41 | NA | 6.59 |
| Iljaž et al 138 | 2017 | Slovenia | 120 | 12 | 55 | 30 | 32 | 6.95 |
| Islam et al 139 | 2019 | Bangladesh | 239 | 6 | 48 | 46 | NA | NA |
| Jahangard-Rafsanjani et al 140 | 2015 | Iran | 101 | 5 | 57 | 50 | 29 | 7.56 |
| Jain et al 141 | 2018 | India | 299 | 6 | 57 | 57 | 24 | 8.16 |
| Jarab et al 142 | 2012 | Jordan | 171 | 6 | 64 | 57 | 33 | 8.45 |
| Jennings et al 143 | 2014 | Australia | 436 | 8 | 58 | 52 | 33 | NA |
| Jeong et al 144 | 2018 | Korea | 338 | 6 | 53 | 67 | 25 | 8.30 |
| Jiwani et al 145 | 2020 | USA | 26 | 6 | 58 | 30 | 39 | 9.30 |
| Kardas et al 146 | 2016 | Poland | 62 | 1.5 | 59 | 60 | 31 | 6.81 |
| Kassavou et al 147 | 2020 | UK | 135 | 3 | NA | 54 | NA | NA |
| Kempf et al 148 | 2017 | Germany | 202 | 12 | 59 | 54 | 36 | 8.30 |
| Keogh et al 149 | 2011 | Ireland | 121 | 6 | 59 | 63 | 32 | 9.18 |
| Kim and Utz 150 | 2019 | South Korea | 155 | 3 | 51 | 48 | NA | 9.14 |
| Kim 151 | 2007 | Korea | 60 | 3 | 47 | 43 | 24 | 7.84 |
| Kim and Jeong 152 | 2007 | Korea | 60 | 6 | 47 | 43 | 24 | 7.84 |
| Kim and Song 153 | 2008 | Korea | 40 | 12 | 47 | 47 | 25 | 7.85 |
| Kim and Kim 154 | 2008 | Korea | 40 | 6 | 47 | 47 | 25 | 7.85 |
| Kim and Oh 155 | 2003 | Korea | 50 | 3 | 60 | 30 | 24 | 8.50 |
| Kim et al 156 | 2005 | Korea | 35 | 3 | 61 | 36 | 24 | 8.60 |
| Kim and Kang 157 | 2006 | Korea | 73 | 3 | 55 | 53 | NA | 7.94 |
| Kim et al 158 | 2009 | USA | 83 | 6.5 | 56 | 56 | 26 | 9.25 |
| Kim et al 159 | 2010 | Korea | 100 | 3 | 48 | 50 | 24 | 9.80 |
| Kim et al 160 | 2015 | Korea | 70 | 6 | 66 | 50 | 25 | 8.55 |
| Kim et al 161 | 2016 | China | 220 | 6 | 54 | 48 | 26 | 7.95 |
| King et al 162 | 2006 | USA | 335 | 2 | 61 | 49 | 32 | NA |
| Kirkman et al 163 | 1994 | USA | 275 | 12 | 64 | 99 | NA | 10.70 |
| Kleinman et al 164 | 2017 | India | 91 | 6 | 48 | 70 | 29 | 9.25 |
| Krein et al 165 | 2004 | USA | 246 | 18 | 61 | 97 | NA | 9.25 |
| Ku et al 166 | 2020 | Australia | 40 | 3 | 50 | 35 | 28 | 8.95 |
| Kusnanto et al 167 | 2019 | Indonesia | 30 | 3 | NA | 43 | NA | 8.46 |
| Kwon et al 168 | 2004 | Korea | 110 | 3 | 54 | 61 | 24 | 7.39 |
| Lauffenburger et al 169 | 2019 | USA | 1400 | 12 | 55 | 63 | NA | 9.35 |
| Lazo-Porras et al 170 | 2020 | Peru | 172 | 18 | 61 | 37 | 28 | 8.55 |
| Lee et al 171 | 2017 | Malaysia | 85 | 3 | 53 | 51 | 30 | 8.74 |
| Lee et al 172 | 2020 | South Korea | 72 | 6 | NA | NA | 26 | 7.44 |
| Lee et al 173 | 2019 | Malaysia | 240 | 12 | 56 | 54 | NA | 9.00 |
| Li et al 174 | 2016 | China | 53 | 6 | 62 | 53 | 24 | 7.73 |
| Liebreich et al 175 | 2009 | Canada | 49 | 3 | 54 | 41 | 34 | NA |
| Lim et al 176 | 2011 | Korea | 154 | 6 | 68 | 21 | 25 | 7.85 |
| Lim et al 177 | 2016 | Korea | 100 | 6 | 65 | 75 | 26 | 8.00 |
| Lorig et al 178 | 2010 | USA | 761 | 6 | 54 | 29 | NA | 6.41 |
| Lujan et al 179 | 2007 | USA | 150 | 6 | 58 | 22 | NA | 7.96 |
| Luley et al 180 | 2011 | Germany | 70 | 6 | 58 | 49 | 35 | 7.55 |
| Lutes et al 181 | 2017 | USA | 200 | 12 | 53 | NA | 38 | 9.09 |
| Lynch et al 182 | 2014 | USA | 61 | 6 | 54 | 33 | 36 | 7.65 |
| MacPhail et al 183 | 2014 | Australia | 87 | 4 | 68 | NA | 31 | NA |
| Marios et al 184 | 2012 | Australia | 39 | 6 | 63 | 53 | 33 | 7.73 |
| Maslakpak et al 185 | 2017 | Iran | 90 | 3 | 50 | 60 | 29 | 8.00 |
| Mayberry et al 186 | 2020 | USA | 379 | 6 | 57 | 46 | NA | 8.13 |
| McEwen et al 187 | 2017 | USA | 157 | 9 | 54 | 35 | 33 | 9.93 |
| McKay et al 188 | 2001 | USA | 78 | 2 | 52 | 47 | NA | NA |
| McKay et al 189 | 2002 | USA | 160 | 3 | 59 | 45 | NA | 7.48 |
| McKee et al 190 | 2011 | USA | 55 | 6 | 60 | 33 | 33 | 8.22 |
| McMahon et al 191 | 2012 | USA | 152 | 12 | 61 | 93 | 34 | 9.85 |
| Mease 192 | 2000 | USA | 28 | 3 | 63 | 39 | NA | 9.50 |
| Mons et al 193 | 2013 | Germany | 204 | 18 | 68 | 61 | NA | 8.10 |
| Moriyama et al 194 | 2009 | Japan | 75 | 12 | 66 | 46 | NA | 7.47 |
| Mwangi et al 195 | 2020 | Kenya | 104 | 3 | 62 | 32 | 25 | NA |
| Namjoo Nasab et al 196 | 2017 | Iran | 64 | 3 | 52 | 48 | 27 | NA |
| Nesari et al 197 | 2010 | Iran | 61 | 3 | 51 | 28 | 28 | 9.26 |
| Nicolucci et al 198 | 2015 | Italy | 302 | 12 | 58 | 65 | 29 | 7.95 |
| Niswender et al 199 | 2014 | Several | 611 | 6 | 57 | 51 | 34 | 7.95 |
| O’Neil et al 200 | 2016 | USA | 563 | 12 | NA | 29 | NA | 8.32 |
| Odegard and Christensen 201 | 2012 | USA | 165 | 12 | 63 | 48 | NA | NA |
| Odnoletkova et al 202 | 2016 | Belgium | 574 | 18 | 63 | 62 | 30 | 7.00 |
| Oh et al 203 | 2003 | Korea | 50 | 3 | 61 | 36 | 25 | 8.55 |
| Orsama et al 204 | 2013 | Finland | 56 | 10 | 62 | 54 | 32 | 6.98 |
| Owolabi et al 205 | 2019 | South Africa | 216 | 6 | NA | 16 | 32 | NA |
| Parsons et al 206 | 2019 | UK | 446 | 12 | 62 | 57 | 33 | 8.60 |
| Patja et al 207 | 2012 | Finland | 1535 | 12 | 65 | 57 | 32 | 7.57 |
| Peasah et al 208 | 2019 | USA | 78 | 3 | 62 | 53 | 35 | 8.20 |
| Peimani et al 209 | 2016 | Iran | 150 | 3 | 52 | 53 | 28 | 7.41 |
| Piette et al 210 | 2011 | USA | 339 | 12 | 56 | 49 | 38 | 7.60 |
| Plotnikoff et al 211 | 2013 | Canada | 287 | 12 | 62 | 51 | 30 | 7.16 |
| Presley et al 212 | 2020 | USA | 120 | 6 | 55 | 28 | 35 | 9.98 |
| Quinn et al 213 | 2017 | USA | 142 | 12 | 52 | 51 | 35 | 9.59 |
| Quinn et al 214 | 2011 | USA | 213 | 12 | 53 | 51 | 35 | 9.24 |
| Raj and Mathews 215 | 2020 | India | 50 | 6 | 69 | 54 | NA | 10.26 |
| Ralston et al 216 | 2009 | USA | 83 | 12 | 57 | 51 | NA | 8.05 |
| Ramadas et al 217 | 2018 | Malaysia | 132 | 12 | 51 | 69 | NA | 9.00 |
| Rasmussen et al 218 | 2016 | Denmark | 40 | 6 | 63 | 68 | 32 | 8.55 |
| Rodríguez-Idígoras et al 219 | 2009 | Spain | 328 | 12 | 64 | 52 | NA | 7.51 |
| Ruggiero et al 220 | 2014 | USA | 270 | 12 | 53 | 32 | 33 | 8.63 |
| Sacco et al 221 | 2009 | USA | 62 | 6 | 52 | 42 | 36 | 8.50 |
| Sacco et al 222 | 2012 | USA | 62 | 6 | 52 | 42 | 36 | 8.50 |
| Samuel-Hodge et al 223 | 2009 | USA | 201 | 12 | 59 | 36 | 35 | 7.78 |
| Sarayani et al 224 | 2018 | Iran | 100 | 9 | 55 | 58 | 30 | 7.95 |
| Saslow et al 225 | 2020 | USA | 64 | 12 | NA | NA | NA | NA |
| Sazlina et al 226 | 2015 | Malaysia | 69 | 8 | 64 | 57 | 27 | 8.20 |
| Schillinger et al 227 | 2009 | USA | 339 | 12 | 56 | 39 | 31 | 9.35 |
| Shahid et al 228 | 2015 | Pakistan | 440 | 4 | 49 | 61 | 27 | 9.97 |
| Shahsavari and Bakhshandeh Bavarsad 229 | 2020 | Iran | 60 | 3 | NA | 15 | 29 | 8.93 |
| Shetty et al 230 | 2011 | India | 215 | 12 | 50 | NA | 27 | 9.00 |
| Shreck et al 231 | 2014 | USA | 526 | 12 | 56 | 33 | NA | 8.65 |
| Sigurdardottir et al 232 | 2009 | Iceland | 58 | 6 | 61 | 68 | 32 | 7.99 |
| Skelly et al 233 | 2009 | USA | 180 | 9 | 67 | NA | NA | 8.37 |
| Sone et al 234 | 2002 | Japan | 2205 | 36 | 59 | 55 | 23 | 7.74 |
| Sone et al 235 | 2010 | Japan | 2033 | 96 | 59 | 46 | 23 | 7.85 |
| Song and Kim 236 | 2009 | Korea | 49 | 3 | 50 | 43 | 25 | 9.20 |
| Spencer et al 237 | 2018 | USA | 222 | 6 | 49 | 39 | 33 | 7.93 |
| Steventon et al 238 | 2014 | England | 513 | 12 | 65 | 58 | 31 | 8.42 |
| Sun et al 239 | 2019 | China | 91 | 6 | 68 | 46 | 23 | 7.86 |
| Sunil Kumar et al 240 | 2020 | India | 300 | 6 | 65 | 60 | NA | 7.60 |
| Takenga et al 241 | 2014 | Democratic Republic of Congo | 40 | 2 | NA | 73 | NA | 8.63 |
| Tamban et al 242 | 2013 | Philippines | 104 | 6 | 50 | 27 | 28 | 7.84 |
| Tan et al 243 | 2018 | Singapore | 142 | 2 | 62 | NA | NA | 9.72 |
| Tang et al 244 | 2013 | USA | 415 | 12 | 54 | 60 | NA | 9.26 |
| Teston et al 245 | 2017 | Brazil | 134 | 5 | NA | 32 | NA | NA |
| Thom et al 246 | 2013 | USA | 299 | 6 | 55 | 48 | 34 | 9.99 |
| Torbjørnsen et al 247 | 2014 | Norway | 164 | 4 | 58 | 59 | 32 | 7.85 |
| Tu et al 248 | 1993 | USA | 31 | 3 | 65 | 33 | NA | NA |
| Van Dyck et al 249 | 2013 | Belgium | 92 | 12 | 62 | 69 | 30 | 7.30 |
| Van Dyck et al 250 | 2011 | Belgium | 92 | 12 | 62 | NA | 30 | NA |
| Van Vugt et al 251 | 2016 | The Netherlands | 132 | 6 | 68 | 53 | 30 | 6.59 |
| Varney et al 252 | 2014 | Australia | 94 | 12 | 62 | 68 | 32 | 8.35 |
| Vaughan et al 253 | 2020 | USA | 89 | 6 | 55 | 28 | 34 | 8.86 |
| Vervloet et al 254 | 2014 | The Netherlands | 604 | 24 | 55 | 55 | NA | NA |
| Vinithia et al 255 | 2019 | India | 248 | 24 | 43 | 68 | 27 | 9.50 |
| Von Storch et al 256 | 2019 | Germany | 2441 | 3 | 59 | 81 | 31 | 6.99 |
| Wakefield et al 257 | 2011 | USA | 302 | 12 | 68 | 94 | 33 | 7.15 |
| Wakefield et al 258 | 2012 | USA | 302 | 12 | 68 | 94 | 33 | 7.15 |
| Wakefield et al 259 | 2014 | USA | 108 | 6 | 60 | 44 | NA | 7.30 |
| Waki et al 260 | 2014 | Japan | 54 | 3 | 57 | 76 | 27 | 7.05 |
| Walker et al 261 | 2011 | USA | 527 | 12 | 56 | 33 | 31 | 8.65 |
| Wang et al 262 | 2020 | Mongolia | 171 | 12 | 55 | 48 | 26 | 9.15 |
| Wang et al 263 | 2019 | China | 120 | 6 | 45 | 32 | NA | 8.65 |
| Wang et al 264 | 2017 | China | 212 | 6 | 54 | 55 | 25 | 7.95 |
| Warren et al 265 | 2018 | Australia | 157 | 6 | 61 | 55 | 34 | 8.27 |
| Weinberger et al 266 | 1995 | USA | 275 | 12 | 64 | 99 | NA | 10.70 |
| Whittemore et al 267 | 2004 | USA | 53 | 6 | 58 | NA | 35 | 7.65 |
| Wichit et al 268 | 2017 | Thailand | 140 | 3 | 58 | 27 | 27 | 6.65 |
| Wild et al 269 | 2016 | UK | 321 | 9 | 61 | 67 | 33 | 8.85 |
| Williams et al 270 | 2012 | Australia | 120 | 6 | 57 | 65 | 33 | 8.55 |
| Williams et al 271 | 2017 | New Zealand | 138 | 6 | 55 | 38 | 40 | 8.15 |
| Wolever et al 272 | 2010 | USA | 56 | 6 | 53 | 23 | NA | 7.93 |
| Wolf et al 273 | 2004 | USA | 147 | 12 | 53 | 40 | 38 | 7.70 |
| Wu et al 274 | 2017 | Australia & Taiwan | 181 | 1 | 66 | 61 | NA | NA |
| Yang et al 275 | 2020 | South Korea | 401 | 3 | 56 | 51 | 26 | 7.96 |
| Yasmin et al 276 | 2020 | Bangladesh | 320 | 12 | 52 | 23 | NA | NA |
| Yoo et al 277 | 2009 | Korea | 123 | 3 | 58 | 59 | 26 | 7.50 |
| Yoon and Kim 278 | 2008 | South Korea | 60 | 12 | 47 | 43 | 24 | 7.83 |
| Young et al 279 | 2005 | UK | 591 | 12 | 67 | 58 | 30 | 7.93 |
| Yu et al 280 | 2019 | China | 185 | 6 | 52 | 28 | 26 | 8.60 |
| Zamanzadeh et al 281 | 2017 | Iran | 66 | 3 | 49 | 41 | NA | NA |
| Zhou et al 282 | 2014 | China | 114 | 3 | NA | NA | 24 | 8.33 |
Abbreviations: BMI, body mass index; HbA1c, glycated hemoglobin; NA, not available.
Table 2 illustrates the telemedicine technologies implemented across studies. Seventy-one studies (29%) were conducted in a hospital setting, 58 studies (24%) in the primary care sector, 37 in communities (15%), 34 in specialized outpatient clinics (14%), 14 in a university setting (6%), and four in cross-sectorial implementations (2%). The frequency of contact with patients across studies was daily (30 studies, 12%), weekly (83 studies, 34%), every two weeks (26 studies, 11%), monthly (40 studies, 16%), and more rarely (12 studies, 5%). Twenty-four (10%) of the studies reported a “tailored” number of contacts with participants (10%). Across studies, the explicitly reported peripherals were scales (13 studies, 5%), glucometers (45 studies, 19%), blood pressure monitors (19 studies, 8%), and pedometers (16 studies, 7%).
Table 2.
Telemedicine Intervention Characteristics.
| Study | Publication year | Setting | Frequency of contact | Included peripherals | Intervention components | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Glucometer | Pedometer | BP monitor | Scale | Monitoring | Consultation | Counseling | Coaching | Education | Mentoring | Reminding | ||||
| Abaza and Marschollek 42 | 2017 | Hospital | Daily | x | x | x | x | |||||||
| Agarwal et al 43 | 2019 | Community | Weekly | x | ||||||||||
| Agarwal et al 44 | 2019 | Hospital | Daily | x | x | |||||||||
| Aguiar et al 45 | 2018 | Hospital | Once | x | ||||||||||
| Akinci et al 46 | 2018 | University | x | |||||||||||
| Al Omar et al 47 | 2020 | Primary | Daily | x | ||||||||||
| Alanzi et al 48 | 2018 | Community | x | x | ||||||||||
| Albikawi et al 49 | 2016 | Specialized | Once | x | ||||||||||
| Alghafri et al 50 | 2018 | Primary | Monthly | x | ||||||||||
| Ali et al 51 | 2016 | Specialized | Monthly | x | ||||||||||
| Ali et al 52 | 2020 | Hospital | Weekly | x | ||||||||||
| Aliha et al 53 | 2013 | Specialized | Weekly | x | ||||||||||
| Alonso-Domínguez et al 54 | 2019 | Primary | Daily | x | ||||||||||
| Alotaibi et al 55 | 2016 | Hospital | Weekly | x | x | x | ||||||||
| Anderson et al 56 | 2009 | Community | Monthly | x | ||||||||||
| Anderson et al 57 | 2010 | Community | Tailored | x | x | |||||||||
| Anderson-Loftin et al 58 | 2005 | Primary | Weekly | x | x | |||||||||
| Andreae et al 59 | 2020 | Community | Weekly | x | ||||||||||
| Anzaldo-Campos et al 60 | 2016 | Primary | x | x | x | |||||||||
| Arora et al 61 | 2014 | Hospital | Daily | x | x | |||||||||
| Asante et al 62 | 2020 | Specialized | Weekly | x | ||||||||||
| Avdal et al 63 | 2011 | University | x | x | ||||||||||
| Azizi et al 64 | 2016 | Specialized | x | x | ||||||||||
| Benson et al 65 | 2018 | Primary | Monthly | x | x | |||||||||
| Blackberry et al 66 | 2013 | Primary | Monthly | x | ||||||||||
| Bluml et al 67 | 2019 | Primary | Weekly | x | x | |||||||||
| Boels et al 12 | 2019 | Hospital | Daily | x | ||||||||||
| Bogner et al 68 | 2012 | Primary | Twice | x | x | |||||||||
| Bohingamu Mudiyanselage et al 69 | 2018 | Community | Daily | x | ||||||||||
| Lashkari et al 70 | 2013 | Weekly | x | |||||||||||
| Browning et al 71 | 2016 | Community | Monthly | x | ||||||||||
| Bujnowska-Fedak et al 72 | 2011 | Primary | Weekly | x | x | |||||||||
| Buysse et al 73 | 2019 | Hospital | Monthly | x | ||||||||||
| Capozza et al 74 | 2015 | Primary | Daily | x | x | |||||||||
| Carter et al 75 | 2011 | Primary | Weekly | x | x | x | x | x | ||||||
| Castelnuovo et al 76 | 2011 | Hospital | Fortnight | x | x | x | ||||||||
| Chao et al 77 | 2019 | Hospital | x | |||||||||||
| Chen et al 78 | 2008 | Hospital | Weekly | x | ||||||||||
| Chen et al 79 | 2018 | Hospital | Weekly | x | ||||||||||
| Chiu et al 80 | 2016 | Community | Weekly | x | ||||||||||
| Cho et al 81 | 2006 | Hospital | Weekly | x | ||||||||||
| Cho et al 82 | 2017 | Specialized | Weekly | x | x | x | ||||||||
| Choe et al 83 | 2005 | University | Monthly | x | ||||||||||
| Choudhry et al 84 | 2018 | Primary | x | |||||||||||
| Clark et al 85 | 2004 | Specialized | Fortnight | x | ||||||||||
| Crowley et al 86 | 2013 | Primary | Monthly | x | ||||||||||
| Crowley et al 87 | 2016 | Hospital | Fortnight | x | x | |||||||||
| Dale et al 88 | 2009 | Primary | Tailored | x | x | |||||||||
| Dario et al 89 | 2017 | Tailored | x | x | ||||||||||
| Davis et al 90 | 2010 | Community | Monthly | x | x | |||||||||
| Del Prato et al 91 | 2012 | x | x | |||||||||||
| Delahanty et al 92 | 2019 | Community | Weekly | x | ||||||||||
| Doupis et al 7 | 2019 | Specialized | Weekly | x | ||||||||||
| Dugas et al 93 | 2018 | Specialized | Daily | x | x | x | ||||||||
| Duruturk and Özköslü 94 | 2019 | Hospital | Weekly | x | ||||||||||
| Döbler et al 95 | 2018 | Specialized | Monthly | x | ||||||||||
| Eakin et al 96 | 2013 | Primary | Fortnight | x | x | x | ||||||||
| Eakin et al 97 | 2014 | Primary | Fortnight | x | x | x | ||||||||
| Egede et al 98 | 2017 | Community | Weekly | x | x | x | ||||||||
| Egede et al 99 | 2018 | Community | ||||||||||||
| Estey et al 100 | 1990 | University | Fortnight | x | x | |||||||||
| Faridi et al 101 | 2008 | Community | Daily | x | x | |||||||||
| Farsaei et al 102 | 2011 | Specialized | Weekly | x | ||||||||||
| Fernandes et al 103 | 2016 | Primary | Monthly | x | ||||||||||
| Fortmann et al 104 | 2017 | Community | Daily | x | x | x | ||||||||
| Fottrell et al 105 | 2019 | Community | Weekly | x | ||||||||||
| Fountoulakis et al 106 | 2015 | Hospital | Tailored | x | x | |||||||||
| Franc et al 107 | 2020 | Primary | Daily | x | ||||||||||
| Franciosi et al 108 | 2011 | Specialized | Monthly | x | x | |||||||||
| Frosch et al 109 | 2011 | Primary | Tailored | x | ||||||||||
| García et al 110 | 2015 | Community | Fortnight | x | x | |||||||||
| Garg et al 111 | 2017 | Hospital | Weekly | x | x | |||||||||
| Gagliardino et al 112 | 2013 | Specialized | Tailored | x | ||||||||||
| Wasif Gillani 113 | 2016 | Hospital | Twice | x | x | |||||||||
| Gimbel et al 114 | 2020 | Primary | Daily | x | x | |||||||||
| Glasgow et al 115 | 2006 | Primary care | Twice | x | ||||||||||
| Glasgow et al 116 | 2006 | Twice | x | |||||||||||
| Glasgow and Toobert 117 | 2000 | Specialized | Fortnight | x | ||||||||||
| Glasgow et al 118 | 2002 | Specialized | Fortnight | x | ||||||||||
| Glasgow et al 119 | 2005 | Primary care | x | |||||||||||
| Goodarzi et al 120 | 2012 | Tailored | x | |||||||||||
| Goodarzi et al 121 | 2018 | University | Weekly | x | ||||||||||
| Graziano and Gross 122 | 2009 | Cross-sectional | Daily | x | x | |||||||||
| Griffin et al 123 | 2014 | Primary | Monthly | x | ||||||||||
| Gupta et al 124 | 2020 | Hospital | Weekly | x | x | |||||||||
| Haider et al 125 | 2019 | Hospital | Weekly | x | ||||||||||
| Hansen et al 126 | 2017 | Hospital | Monthly | x | x | |||||||||
| Hare et al 127 | 2011 | Hospital | Tailored | x | ||||||||||
| Hee-Sung 128 | 2007 | Hospital | Monthly | x | x | x | ||||||||
| Heisler et al 129 | 2019 | Hospital | Monthly | x | ||||||||||
| Hidrus et al 130 | 2020 | Hospital | Daily | x | ||||||||||
| Hokanson et al 131 | 2006 | Specialized | Tailored | x | ||||||||||
| Holbrook et al 132 | 2009 | Primary | x | |||||||||||
| Holmen et al 133 | 2014 | Primary | Monthly | x | x | |||||||||
| Hordern et al 134 | 2009 | Hospital | Tailored | x | x | |||||||||
| Huang et al 135 | 2019 | Specialized | Daily | x | ||||||||||
| Huizinga et al 136 | 2010 | University | Monthly | x | ||||||||||
| Hunt et al 137 | 2014 | Specialized | Weekly | x | ||||||||||
| Iljaž et al 138 | 2017 | Primary | Tailored | x | x | x | ||||||||
| Islam et al 139 | 2019 | Hospital | Daily | x | ||||||||||
| Jahangard-Rafsanjani et al 140 | 2015 | Community | Monthly | x | ||||||||||
| Jain et al 141 | 2018 | Community | Weekly | x | x | |||||||||
| Jarab et al 142 | 2012 | Specialized | Weekly | x | ||||||||||
| Jennings et al 143 | 2014 | x | ||||||||||||
| Jeong et al 144 | 2018 | Hospital | Twice | x | x | x | ||||||||
| Jiwani et al 145 | 2020 | Community | Weekly | x | ||||||||||
| Kardas et al 146 | 2016 | Primary | x | x | x | x | x | |||||||
| Kassavou et al 147 | 2020 | Primary | Weekly | x | ||||||||||
| Kempf et al 148 | 2017 | Specialized | Weekly | x | ||||||||||
| Keogh et al 149 | 2011 | Specialized | Once | x | ||||||||||
| Kim and Utz 150 | 2019 | Hospital | Weekly | x | x | |||||||||
| Kim 151 | 2007 | Hospital | Weekly | x | x | |||||||||
| Kim and Jeong 152 | 2007 | Hospital | Weekly | x | x | |||||||||
| Kim and Song 153 | 2008 | Hospital | Weekly | x | x | |||||||||
| Kim and Kim 154 | 2008 | Hospital | Weekly | x | x | |||||||||
| Kim and Oh 155 | 2003 | Hospital | Weekly | x | x | |||||||||
| Kim et al 156 | 2005 | Hospital | Weekly | x | x | |||||||||
| Kim and Kang 157 | 2006 | Hospital | Tailored | x | ||||||||||
| Kim et al 158 | 2009 | Community | Monthly | x | x | x | x | |||||||
| Kim et al 159 | 2010 | Hospital | Daily | x | x | x | ||||||||
| Kim et al 160 | 2015 | Hospital | x | |||||||||||
| Kim et al 161 | 2016 | Hospital | Tailored | x | ||||||||||
| King et al 162 | 2006 | Primary | Twice | x | ||||||||||
| Kirkman et al 163 | 1994 | Primary | Monthly | x | ||||||||||
| Kleinman et al 164 | 2017 | Specialized | x | x | ||||||||||
| Krein et al 165 | 2004 | Specialized | x | |||||||||||
| Ku et al 166 | 2020 | Hospital | Weekly | x | x | x | ||||||||
| Kusnanto et al 167 | 2019 | Primary | Daily | x | ||||||||||
| Kwon et al 168 | 2004 | Hospital | Tailored | x | x | |||||||||
| Lauffenburger et al 169 | 2019 | Weekly | x | x | ||||||||||
| Lazo-Porras et al 170 | 2020 | Hospital | Weekly | x | x | |||||||||
| Lee et al 171 | 2017 | Community | x | x | x | x | ||||||||
| Lee et al 172 | 2020 | Hospital | Weekly | x | x | |||||||||
| Lee et al 173 | 2019 | Primary | Weekly | x | x | |||||||||
| Li et al 174 | 2016 | Hospital | Monthly | x | x | |||||||||
| Liebreich et al 175 | 2009 | Weekly | x | x | ||||||||||
| Lim et al 176 | 2011 | Hospital | x | x | ||||||||||
| Lim et al 177 | 2016 | Hospital | x | x | x | |||||||||
| Lorig et al 178 | 2010 | Weekly | x | |||||||||||
| Lujan et al 179 | 2007 | Community | Fortnight | x | x | |||||||||
| Luley et al 180 | 2011 | Hospital | Weekly | x | x | x | ||||||||
| Lutes et al 181 | 2017 | Primary | Monthly | x | x | x | x | |||||||
| Lynch et al 182 | 2014 | Community | Weekly | x | ||||||||||
| MacPhail et al 183 | 2014 | Primary | Twice | x | ||||||||||
| Marios et al 184 | 2012 | Primary | Weekly | x | x | |||||||||
| Maslakpak et al 185 | 2017 | Weekly | x | |||||||||||
| Mayberry et al 186 | 2020 | Primary | Monthly | x | ||||||||||
| McEwen et al 187 | 2017 | Community | Tailored | x | ||||||||||
| McKay et al 188 | 2001 | Weekly | x | x | ||||||||||
| McKay et al 189 | 2002 | Primary | Weekly | x | ||||||||||
| McKee et al 190 | 2011 | Community | x | x | x | x | ||||||||
| McMahon et al 191 | 2012 | Tailored | x | x | x | |||||||||
| Mease 192 | 2000 | Primary | Weekly | x | x | |||||||||
| Mons et al 193 | 2013 | Primary | Monthly | x | ||||||||||
| Moriyama et al 194 | 2009 | Hospital | Fortnight | x | x | |||||||||
| Mwangi et al 195 | 2020 | Hospital | Monthly | x | x | |||||||||
| Namjoo Nasab et al 196 | 2017 | Community | Weekly | x | ||||||||||
| Nesari et al 197 | 2010 | Specialized | Weekly | x | x | |||||||||
| Nicolucci et al 198 | 2015 | Primary | Monthly | x | x | x | x | x | ||||||
| Niswender et al 199 | 2014 | Cross-sectional | Fortnight | x | ||||||||||
| O’Neil et al 200 | 2016 | University | Weekly | x | x | |||||||||
| Odegard and Christensen 201 | 2012 | Community | Monthly | x | x | |||||||||
| Odnoletkova et al 202 | 2016 | Fortnight | x | |||||||||||
| Oh et al 203 | 2003 | Hospital | Weekly | x | x | |||||||||
| Orsama et al 204 | 2013 | Community | Tailored | x | x | x | x | x | ||||||
| Owolabi et al 205 | 2019 | Primary | Daily | x | x | x | ||||||||
| Parsons et al 206 | 2019 | Primary | Weekly | x | x | |||||||||
| Patja et al 207 | 2012 | Primary | Monthly | x | ||||||||||
| Peasah et al 208 | 2019 | Primary | Weekly | x | x | |||||||||
| Peimani et al 209 | 2016 | Hospital | Weekly | x | ||||||||||
| Piette et al 210 | 2011 | Community | Weekly | x | ||||||||||
| Plotnikoff et al 211 | 2013 | Community | Tailored | x | ||||||||||
| Presley et al 212 | 2020 | Community | Weekly | x | x | |||||||||
| Quinn et al 213 | 2017 | Community | Tailored | x | x | |||||||||
| Quinn et al 214 | 2011 | Community | Tailored | x | x | |||||||||
| Raj and Mathews 215 | 2020 | Hospital | Weekly | x | x | |||||||||
| Ralston et al 216 | 2009 | Hospital | Weekly | x | ||||||||||
| Ramadas et al 217 | 2018 | Hospital | x | x | ||||||||||
| Rasmussen et al 218 | 2016 | Specialized | x | |||||||||||
| Rodríguez-Idígoras et al 219 | 2009 | Community | Tailored | x | x | |||||||||
| Ruggiero et al 220 | 2014 | Primary | Monthly | x | ||||||||||
| Sacco et al 221 | 2009 | University | Weekly | x | ||||||||||
| Sacco et al 222 | 2012 | University | Weekly | x | ||||||||||
| Samuel-Hodge et al 223 | 2009 | Community | Monthly | x | ||||||||||
| Sarayani et al 224 | 2018 | Weekly | x | |||||||||||
| Saslow et al 225 | 2020 | University | Daily | x | ||||||||||
| Sazlina et al 226 | 2015 | Primary | x | x | ||||||||||
| Schillinger et al 227 | 2009 | Weekly | x | |||||||||||
| Shahid et al 228 | 2015 | Specialized | Weekly | x | x | x | ||||||||
| Shahsavari and Bakhshandeh Bavarsad 229 | 2020 | Specialized | Weekly | x | ||||||||||
| Shetty et al 230 | 2011 | Specialized | Weekly | x | ||||||||||
| Shreck et al 231 | 2014 | Fortnight | x | |||||||||||
| Sigurdardottir et al 232 | 2009 | Specialized | Weekly | x | ||||||||||
| Skelly et al 233 | 2009 | Cross-sectional | Fortnight | x | x | |||||||||
| Sone et al 234 | 2002 | Specialized | Fortnight | x | x | |||||||||
| Sone et al 235 | 2010 | Specialized | Fortnight | x | x | x | ||||||||
| Song and Kim 236 | 2009 | Specialized | Weekly | x | x | |||||||||
| Spencer et al 237 | 2018 | Community | Fortnight | x | x | |||||||||
| Steventon et al 238 | 2014 | Cross-sectional | Daily | x | x | x | x | |||||||
| Sun et al 239 | 2019 | Hospital | Daily | x | x | x | x | |||||||
| Sunil Kumar et al 240 | 2020 | Hospital | Daily | x | x | x | ||||||||
| Takenga et al 241 | 2014 | Hospital | x | |||||||||||
| Tamban et al 242 | 2013 | Weekly | x | |||||||||||
| Tan et al 243 | 2018 | Primary | Fortnight | x | ||||||||||
| Tang et al 244 | 2013 | x | x | x | ||||||||||
| Teston et al 245 | 2017 | Fortnight | x | |||||||||||
| Thom et al 246 | 2013 | Community | Fortnight | x | x | |||||||||
| Torbjørnsen et al 247 | 2014 | Monthly | x | x | ||||||||||
| Tu et al 248 | 1993 | Hospital | Weekly | x | x | |||||||||
| Van Dyck et al 249 | 2013 | Hospital | Fortnight | x | x | x | ||||||||
| Van Dyck et al 250 | 2011 | Hospital | Fortnight | x | x | x | ||||||||
| Van Vugt et al 251 | 2016 | Primary | x | x | ||||||||||
| Varney et al 252 | 2014 | Hospital | Monthly | x | ||||||||||
| Vaughan et al 253 | 2020 | Primary | Weekly | x | x | |||||||||
| Vervloet et al 254 | 2014 | x | ||||||||||||
| Vinithia et al 255 | 2019 | Hospital | Weekly | x | x | |||||||||
| Von Storch et al 256 | 2019 | Weekly | x | x | x | |||||||||
| Wakefield et al 257 | 2011 | Primary | Daily | x | x | x | x | |||||||
| Wakefield et al 258 | 2012 | Primary | Daily | x | x | x | x | |||||||
| Wakefield et al 259 | 2014 | University | Tailored | x | x | x | ||||||||
| Waki et al 260 | 2014 | University | Tailored | x | x | x | x | x | ||||||
| Walker et al 261 | 2011 | Specialized | Monthly | x | ||||||||||
| Wang et al 262 | 2020 | Hospital | Weekly | x | ||||||||||
| Wang et al 263 | 2019 | Hospital | Weekly | x | x | |||||||||
| Wang et al 264 | 2017 | Hospital | Fortnight | x | x | x | ||||||||
| Warren et al 265 | 2018 | Primary | Daily | x | x | x | x | |||||||
| Weinberger et al 266 | 1995 | Primary | Monthly | x | x | |||||||||
| Whittemore et al 267 | 2004 | Specialized | Monthly | x | ||||||||||
| Wichit et al 268 | 2017 | Hospital | Once | x | x | |||||||||
| Wild et al 269 | 2016 | Primary | x | x | x | x | ||||||||
| Williams et al 270 | 2012 | Hospital | Weekly | x | ||||||||||
| Williams et al 271 | 2017 | Primary | Monthly | x | ||||||||||
| Wolever et al 272 | 2010 | Weekly | x | |||||||||||
| Wolf et al 273 | 2004 | Primary | Monthly | x | x | |||||||||
| Wu et al 274 | 2017 | University | Once | x | x | |||||||||
| Yang et al 275 | 2020 | Primary | Daily | x | x | |||||||||
| Yasmin et al 276 | 2020 | Hospital | Fortnight | x | x | x | ||||||||
| Yoo et al 277 | 2009 | University | Tailored | x | x | x | x | x | ||||||
| Yoon and Kim 278 | 2008 | Hospital | Weekly | x | x | |||||||||
| Young et al 279 | 2005 | Primary | Monthly | x | x | |||||||||
| Yu et al 280 | 2019 | Hospital | Daily | x | x | |||||||||
| Zamanzadeh et al 281 | 2017 | Daily | x | |||||||||||
| Zhou et al 282 | 2014 | Hospital | Fortnight | x | x | x | x | x | ||||||
Abbreviation: BP, blood pressure.
The final sample included 86 studies (35%) with a monitoring component in the telemedicine intervention, 22 studies with a consultation opportunity (9%), 53 studies with a counseling purpose (22%), 63 studies with an opportunity for patients to receive coaching (26%), 81 studies with a patient education component (33%), and eight studies with the possibility of mentoring (3%). Furthermore, 38 studies were able to send reminders (16%).
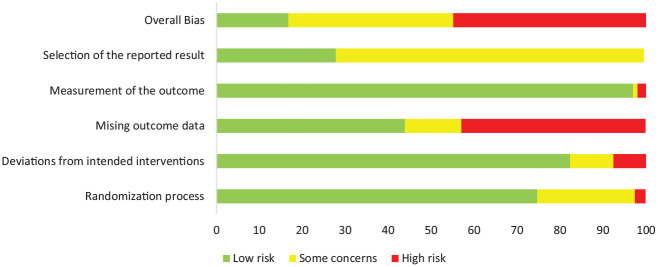
The evaluation of risk of bias is described for each study in Online Appendix 1 and across studies in Figure 2. Overall, there was a high risk of bias in 45% of the included studies, a moderate risk in 38% and a low risk in 17%. This result was largely attributed to two factors. First were missing outcomes at follow-up, where a high proportion of studies (43%) only reported results of a complete case or per-protocol analysis without appropriate consideration of the relationship with covariates and missingness (ie, tests for missing completely at random or an assumption of missing at random with imputation and/or tests for association with baseline variables and missingness and/or adjusted analyses). Second, there were some concerns regarding the risk of selecting published results, especially due to a lack of registered or published research protocols in the majority of studies (72%).
Figure 2.
Summary of risk of bias assessment.
Effect on HbA1c%
Of the 243 studies, 168 had sufficient information to calculate an MD with standard errors for the effect on HbA1c% and reported treatment effects of telemedicine from one to 96 months. Figure 3 and Table 3 present the results from the individual studies and the meta-analysis. Overall, the results favored telemedicine, with an MD of −0.415%, which was statistically significant (95% confidence interval [CI] = −0.482% to −0.348%). The heterogeneity was great (I2 = 93.05%).
Figure 3.

Forest plot of the meta-analysis (magenta line is effect size difference of 0).
Table 3.
Meta-Analysis Summary.
| Study | MD | Lower 95% CI | Higher 95% CI | Weight |
|---|---|---|---|---|
| Abaza and Marschollek 42 | −0.11 | −0.72 | 0.50 | 0.47 |
| Aguiar et al 45 | −0.63 | −1.08 | −0.18 | 0.57 |
| Akinci et al 46 | −0.57 | −1.21 | 0.07 | 0.45 |
| Alanzi et al 48 | −1.25 | −2.14 | −0.36 | 0.33 |
| Ali et al 51 | −0.40 | −0.59 | −0.22 | 0.73 |
| Aliha et al 53 | −1.30 | −1.88 | −0.72 | 0.49 |
| Alotaibi et al 55 | −0.74 | −1.56 | 0.08 | 0.36 |
| Anderson et al 56 | −0.29 | −0.60 | 0.02 | 0.66 |
| Anderson-Loftin et al 58 | −1.00 | −1.56 | −0.44 | 0.50 |
| Anzaldo-Campos et al 60 | −1.37 | −1.81 | −0.94 | 0.58 |
| Arora et al 61 | −0.13 | −0.56 | 0.31 | 0.58 |
| Avdal et al 63 | −0.69 | −1.04 | −0.35 | 0.64 |
| Azizi et al 64 | −0.40 | −0.55 | −0.25 | 0.74 |
| Blackberry et al 66 | −0.06 | −0.27 | 0.15 | 0.72 |
| Bogner et al 68 | −1.20 | −1.52 | −0.88 | 0.65 |
| Lashkari et al 70 | −0.99 | −1.62 | −0.36 | 0.46 |
| Browning et al 71 | 0.03 | −0.16 | 0.22 | 0.73 |
| Bujnowska-Fedak et al 72 | −0.06 | −0.71 | 0.59 | 0.45 |
| Chen et al 78 | −0.76 | −1.33 | −0.19 | 0.49 |
| Cho et al 81 | −0.70 | −1.16 | −0.24 | 0.56 |
| Cho et al 82 | −0.15 | −0.32 | 0.02 | 0.74 |
| Choe et al 83 | −1.30 | −1.88 | −0.72 | 0.49 |
| Crowley et al 86 | −0.10 | −0.17 | −0.04 | 0.76 |
| Crowley et al 87 | −1.00 | −1.35 | −0.65 | 0.64 |
| Dale et al 88 | 0.10 | −0.23 | 0.43 | 0.65 |
| Dario et al 89 | 0.01 | −0.23 | 0.25 | 0.70 |
| Davis et al 90 | −0.70 | −0.90 | −0.50 | 0.72 |
| Del Prato et al 91 | 0.00 | −0.06 | 0.06 | 0. 77 |
| Dugas et al 93 | 0.18 | −0.87 | 1.23 | 0.27 |
| Döbler et al 95 | −0.80 | −1.11 | −0.49 | 0.66 |
| Eakin et al 96 | 0.00 | −0.29 | 0.29 | 0.67 |
| Estey et al 100 | −0.20 | −0.77 | 0.37 | 0.49 |
| Faridi et al 101 | −0.40 | −0.98 | 0.18 | 0.49 |
| Farsaei et al 102 | −1.50 | −1.85 | −1.15 | 0.64 |
| Fortmann et al 104 | −0.90 | −1.34 | −0.46 | 0.58 |
| Fountoulakis et al 106 | −0.70 | −1.16 | −0.24 | 0.56 |
| Franciosi et al 108 | −0.50 | −0.74 | −0.26 | 0.70 |
| Frosch et al 109 | −0.30 | −0.42 | −0.18 | 0.75 |
| García et al 110 | −1.20 | −1.45 | −0.95 | 0.69 |
| Garg et al 111 | −0.30 | −0.65 | 0.05 | 0.64 |
| Gagliardino et al 112 | −0.20 | −0.51 | 0.11 | 0.66 |
| Glasgow and Toobert 117 | 0.10 | −0.27 | 0.47 | 0.62 |
| Glasgow et al 118 | −0.20 | −0.55 | 0.15 | 0.64 |
| Glasgow et al 119 | 0.01 | −0.13 | 0.15 | 0.74 |
| Glasgow et al 115 | −0.20 | −0.48 | 0.08 | 0.68 |
| Glasgow et al 116 | 0.00 | −0.27 | 0.27 | 0.68 |
| Goodarzi et al 120 | −0.46 | −0.88 | −0.04 | 0.59 |
| Graziano and Gross 122 | −0.07 | −0.45 | 0.31 | 0.62 |
| Griffin et al 123 | −0.01 | −0.18 | 0.16 | 0.73 |
| Hare et al 127 | −0.10 | −0.41 | 0.21 | 0.66 |
| Hee-Sung 128 | −0.43 | −0.81 | −0.05 | 0.62 |
| Holbrook et al 132 | −0.50 | −0.71 | −0.30 | 0.72 |
| Holmen et al 133 | −0.20 | −0.68 | 0.28 | 0.55 |
| Hordern et al 134 | −0.70 | −0.99 | −0.41 | 0.67 |
| Iljaž et al 138 | −0.30 | −0.69 | 0.09 | 0.61 |
| Jahangard-Rafsanjani et al 140 | −0.40 | −0.89 | 0.09 | 0.54 |
| Jarab et al 142 | −0.90 | −1.46 | −0.34 | 0.50 |
| Jeong et al 144 | −0.12 | −0.40 | 0.16 | 0.68 |
| Kardas et al 146 | −0.03 | −0.51 | 0.45 | 0.55 |
| Kempf et al 148 | −0.60 | −0.91 | −0.29 | 0.66 |
| Keogh et al 149 | −0.39 | −0.78 | 0.00 | 0.61 |
| Kim and Oh 155 | −1.20 | −1.74 | −0.66 | 0.51 |
| Kim et al 156 | −1.00 | −1.63 | −0.38 | 0.46 |
| Kim and Kang 157 | −0.90 | −1.58 | −0.22 | 0.43 |
| Kim 151 | −0.72 | −1.22 | −0.22 | 0.54 |
| Kim and Jeong 152 | −0.66 | −1.20 | −0.12 | 0.51 |
| Kim and Song 153 | −1.52 | −2.02 | −1.02 | 0.54 |
| Kim and Kim 154 | −0.59 | −1.21 | 0.03 | 0.46 |
| Kim et al 158 | −0.90 | −1.40 | −0.40 | 0.54 |
| Kim et al 159 | −0.40 | −0.74 | −0.06 | 0.64 |
| Kim et al 160 | −0.70 | −1.13 | −0.27 | 0.58 |
| Kim et al 161 | −0.70 | −0.96 | −0.44 | 0.69 |
| Kleinman et al 164 | −0.30 | −0.77 | 0.17 | 0.56 |
| Krein et al 165 | 0.10 | −0.28 | 0.48 | 0.62 |
| Kwon et al 168 | −0.68 | −0.82 | −0.55 | 0.75 |
| Lee et al 171 | −0.93 | −1.49 | −0.37 | 0.50 |
| Li et al 174 | −0.35 | −0.95 | 0.25 | 0.48 |
| Lim et al 176 | −0.40 | −0.79 | −0.01 | 0.61 |
| Lim et al 177 | −0.60 | −1.00 | −0.20 | 0.60 |
| Lorig et al 178 | −0.11 | −0.26 | 0.05 | 0.74 |
| Lujan et al 179 | −0.25 | −0.68 | 0.18 | 0.58 |
| Luley et al 180 | −1.00 | −1.33 | −0.67 | 0.65 |
| Lutes et al 181 | −0.26 | −0.66 | 0.14 | 0.60 |
| Marios et al 184 | 0.49 | −0.25 | 1.23 | 0.40 |
| Maslakpak et al 185 | −0.50 | −1.09 | 0.09 | 0.48 |
| McEwen et al 187 | −0.01 | −0.46 | 0.44 | 0.57 |
| McKay et al 189 | 0.36 | −0.17 | 0.89 | 0.52 |
| McKee et al 190 | −0.60 | −1.39 | 0.19 | 0.37 |
| McMahon et al 191 | −0.10 | −0.56 | 0.36 | 0.56 |
| Nesari et al 197 | −1.56 | −2.18 | −0.94 | 0.46 |
| Nicolucci et al 198 | −0.34 | −0.57 | −0.11 | 0.71 |
| Niswender et al 199 | −0.13 | −0.17 | −0.10 | 0.77 |
| Odnoletkova et al 202 | −0.10 | −0.27 | 0.07 | 0.73 |
| Oh et al 203 | −1.30 | −1.88 | −0.72 | 0.49 |
| O’Neil et al 200 | −0.39 | −0.59 | −0.19 | 0.72 |
| Orsama et al 204 | −0.44 | −0.88 | 0.01 | 0.58 |
| Peimani et al 209 | −0.49 | −0.95 | −0.03 | 0.56 |
| Piette et al 210 | 0.00 | −0.28 | 0.28 | 0.68 |
| Plotnikoff et al 211 | 0.21 | 0.13 | 0.29 | 0.76 |
| Quinn et al 214 | −0.80 | −1.26 | −0.34 | 0.56 |
| Ramadas et al 217 | 0.10 | −0.39 | 0.59 | 0.55 |
| Rodríguez-Idígoras et al 219 | 0.05 | −0.18 | 0.28 | 0.70 |
| Sacco et al 221 | −0.40 | −0.95 | 0.15 | 0.51 |
| Samuel-Hodge et al 223 | −0.10 | −0.19 | −0.01 | 0.76 |
| Sarayani et al 224 | −0.30 | −0.80 | 0.20 | 0.54 |
| Schillinger et al 227 | −0.30 | −0.66 | 0.06 | 0.63 |
| Shahid et al 228 | −0.73 | −0.94 | −0.52 | 0.72 |
| Sigurdardottir et al 232 | 0.25 | −0.26 | 0.76 | 0.53 |
| Sone et al 234 | −0.17 | −0.26 | −0.08 | 0.76 |
| Sone et al 235 | 0.10 | 0.01 | 0.20 | 0.76 |
| Song and Kim 236 | −1.50 | −2.13 | −0.87 | 0.46 |
| Tamban et al 242 | −0.35 | −0.71 | 0.01 | 0.63 |
| Tan et al 243 | −0.38 | −0.77 | 0.01 | 0.61 |
| Tang et al 244 | −0.23 | −0.48 | 0.02 | 0.69 |
| Thom et al 246 | −0.57 | −0.90 | −0.24 | 0.65 |
| Torbjørnsen et al 247 | 0.00 | −0.41 | 0.41 | 0.60 |
| Tu et al 248 | 0.43 | −0.65 | 1.51 | 0.26 |
| Van Dyck et al 249 | −0.30 | −0.79 | 0.19 | 0.55 |
| Varney et al 252 | −0.20 | −0.65 | 0.25 | 0.57 |
| Wakefield et al 259 | −0.10 | −0.26 | 0.06 | 0.74 |
| Waki et al 260 | −0.40 | −0.91 | 0.11 | 0.53 |
| Walker et al 261 | 0.10 | 0.04 | 0.16 | 0.77 |
| Wang et al 264 | −0.60 | −0.87 | −0.33 | 0.68 |
| Warren et al 265 | −0.57 | −0.89 | −0.24 | 0.65 |
| Weinberger et al 266 | −0.60 | −0.74 | −0.46 | 0.74 |
| Whittemore et al 267 | 0.00 | −0.56 | 0.56 | 0.50 |
| Wichit et al 268 | −0.30 | −0.68 | 0.08 | 0.62 |
| Wild et al 269 | −0.50 | −0.75 | −0.25 | 0.69 |
| Williams et al 270 | −0.80 | −1.22 | −0.38 | 0.59 |
| Wolever et al 272 | −0.50 | −1.22 | 0.22 | 0.41 |
| Yoo et al 277 | −0.50 | −0.84 | −0.17 | 0.65 |
| Yoon and Kim 278 | −1.63 | −2.11 | −1.15 | 0.55 |
| Zhou et al 282 | −0.76 | −1.20 | −0.32 | 0.58 |
| Agarwal et al 43 | 0.80 | 0.13 | 1.47 | 0.44 |
| Alghafri et al 50 | 0.30 | −0.01 | 0.61 | 0.66 |
| Al Omar et al 47 | −0.70 | −1.05 | −0.35 | 0.63 |
| Andreae et al 59 | −0.10 | −0.46 | 0.26 | 0.63 |
| Asante et al 62 | −1.30 | −2.02 | −0.58 | 0.41 |
| Bluml et al 67 | 0.00 | −0.25 | 0.25 | 0.69 |
| Boels et al 12 | −0.20 | −0.52 | 0.12 | 0.66 |
| Bohingamu Mudiyanselage et al 69 | −0.21 | −0.41 | −0.01 | 0.72 |
| Buysse et al 73 | −0.10 | −0.67 | 0.47 | 0.49 |
| Chao et al 77 | −0.90 | −1.35 | −0.45 | 0.57 |
| Choudhry et al 84 | 0.10 | 0.02 | 0.19 | 0.76 |
| Delahanty et al 92 | 0.00 | −0.37 | 0.37 | 0.62 |
| Doupis et al 7 | 0.10 | −0.04 | 0.24 | 0.74 |
| Duruturk and Özköslü 94 | −1.99 | −2.80 | −1.18 | 0.36 |
| Gupta et al 124 | −0.52 | −0.98 | −0.06 | 0.56 |
| Haider et al 125 | −0.40 | −0.75 | −0.05 | 0.64 |
| Huang et al 135 | −0.40 | −1.18 | 0.38 | 0.37 |
| Jain et al 141 | 0.26 | −0.08 | 0.60 | 0.64 |
| Jiwani et al 145 | −2.20 | −3.26 | −1.14 | 0.26 |
| Kim and Utz 150 | 0.24 | −0.18 | 0.66 | 0.59 |
| Ku et al 166 | −1.20 | −1.91 | −0.49 | 0.41 |
| Kusnanto et al 167 | −0.27 | −1.02 | 0.48 | 0.39 |
| Lauffenburger et al 169 | −0.06 | −0.21 | 0.09 | 0.74 |
| Lee et al 172 | −0.50 | −0.94 | −0.06 | 0.58 |
| Parsons et al 206 | −0.97 | −1.20 | −0.74 | 0.71 |
| Peasah et al 208 | 0.00 | −0.52 | 0.52 | 0.53 |
| Presley et al 212 | 0.50 | 0.00 | 1.00 | 0.54 |
| Shahsavari and Bakhshandeh Bavarsad 229 | −1.38 | −1.89 | −0.87 | 0.53 |
| Sun et al 239 | −0.38 | −0.75 | −0.01 | 0.62 |
| Sunil Kumar et al 240 | −0.87 | −1.11 | −0.63 | 0.70 |
| Vaughan et al 253 | −0.67 | −1.24 | −0.10 | 0.49 |
| Vinithia et al 255 | −0.40 | −0.71 | −0.10 | 0.66 |
| Von Storch et al 256 | −0.37 | −0.45 | −0.29 | 0.76 |
| Wang et al 263 | −0.80 | −1.32 | −0.28 | 0.53 |
| Yu et al 280 | −0.40 | −0.92 | 0.12 | 0.53 |
| Overall | −0.42 | −0.48 | −0.35 | 100.00 |
Abbreviations: CI, confidence interval; MD, mean difference.
A series of univariate meta-regressions are illustrated in Table 4 and were assessed with a 5% significance level. Compared with North American studies (the reference), Asian studies reported larger effects of telemedicine (difference in MD = −0.287, P = .000), as did studies with higher baseline HbA1c% levels (difference in MD = −0.086 per %, P = .008). Compared with primary care settings (reference), hospital settings were also associated with an increase in the effect of telemedicine (difference in MD = −0.290, P = .004). Furthermore, a monitoring component gave rise to greater effects of telemedicine (difference in MD = −0.195, P = .004). Treatment effects of telemedicine were lesser for studies with longer duration (difference in MD = 0.008 per month, P = .015) and for studies with higher proportions of men (difference in MD = 0.005 per %, P = .035) and higher age (difference in MD = 0.022 per year, P = .000). A coaching component led to a lower effect (difference in MD = 0.215, P = .007). There were no statistically significant associations between the effect of telemedicine on HbA1c% levels and publication date, baseline BMI, contact frequency, the included peripherals, or risk of bias.
Table 4.
Association Between Study Covariates and Effect of Telemedicine on HbA1c% (Meta-Regression).
| Covariate | N | Difference in MD (SE) | P value | I2 (%) |
|---|---|---|---|---|
| Study characteristics | ||||
| Publication decade | ||||
| Before 2020 | 4 | Reference | 92.86 | |
| 2020s | 50 | −0.175 (0.287) | .542 | |
| 2010s | 165 | −0.082 (0.281) | .769 | |
| 2020 | 24 | −0.418 (0.312) | .180 | |
| Continent | ||||
| North America | 88 | Reference | 91.15 | |
| Europe | 44 | −0.037 (0.095) | .696 | |
| South America | 5 | −0.104 (0.303) | .731 | |
| Africa | 5 | −0.366 (0.362) | .312 | |
| Asia | 84 | −0.287 (0.078) | .000* | |
| Australia/New Zealand | 16 | −0.040 (0.140) | .773 | |
| Study duration (range = 1-96 months) | 168 | 0.008 per month (0.003) | .015* | 92.60 |
| Proportion of men (range = 15%-100%) | 159 | 0.005 per % (0.002) | .035* | 93.05 |
| Age (range = 37-73 years) | 157 | 0.022 per year (0.006) | .000* | 92.64 |
| Baseline BMI (range = 22-40) | 123 | 0.018 per score (0.010) | .066 | 92.51 |
| Baseline HbA1c% (range = 5.70%-11.05%) | 165 | −0.093 per % (0.035) | .007* | 92.80 |
| Telemedicine characteristics | ||||
| Setting | ||||
| Primary care | 58 | Reference | 90.25 | |
| Community | 37 | −0.019 (0.116) | .868 | |
| Hospital | 71 | −0.290 (0.100) | .004* | |
| Specialized outpatient clinic | 34 | −0.148 (0.114) | .194 | |
| University | 14 | −0.180 (0.169) | .287 | |
| Cross-sectorial | 4 | 0.203 (0.301) | .500 | |
| Contact frequency | ||||
| Daily | 30 | Reference | 91.42 | |
| Weekly | 83 | −0.150 (0.129) | .246 | |
| Every two weeks | 26 | 0.045 (0.157) | .776 | |
| Monthly | 40 | 0.101 (0.144) | .481 | |
| More seldom | 12 | −0.006 (0.199) | .977 | |
| Tailored | 24 | 0.076 (0.148) | .611 | |
| Included peripherals | ||||
| Glucometer | 45 | −0.052 (0.081) | .523 | 92.81 |
| Pedometer | 16 | 0.102 (0.132) | .440 | 92.96 |
| BP monitor | 19 | −0.008 (0.132) | .953 | 93.09 |
| Scale | 13 | 0.014 (0.137) | .919 | 93.12 |
| Intervention components | ||||
| Monitoring | 86 | −0.195 (0.068) | .004* | 92.30 |
| Consultation | 22 | −0.015 (0.114) | .895 | 92.25 |
| Counseling | 53 | −0.030 (0.083) | .720 | 92.95 |
| Coaching | 63 | 0.215 (0.080) | .007* | 92.44 |
| Education | 81 | −0.125 (0.072) | .085 | 92.76 |
| Mentoring | 8 | 0.265 (0.201) | .188 | 93.03 |
| Reminding | 38 | −0.151 (0.092) | .100 | 92.87 |
| Risk of bias | ||||
| Low | 33 | Reference | 92.82 | |
| Some concerns | 76 | −0.101 (0.100) | .310 | |
| High | 88 | −0.067 (0.100) | .492 | |
Abbreviations: HbA1c%, glycated hemoglobin; MD, mean difference; BMI, body mass index; BP, blood pressure.
Statistically significant at a 5% level.
Certainty of the Evidence
Table 5 summarizes the findings. Overall, the certainty of evidence of the calculated effect on HbA1c% was judged as low due to serious problems with the risk of bias and inconsistency.
Table 5.
Summary of Findings Table.
| Certainty assessment | No of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Telemedicine | Usual practice | Relative (95% CI) | Absolute (95% CI) | ||
| HbA1c% | ||||||||||||
| 243 | Randomized trials | Serious a | Serious b | Not serious | Not serious | None | 29 671 | 27 465 | − | MD 0.415 lower (0.482 lower to 0.348 lower) | ⨁⨁◯◯ LOW | IMPORTANT |
Abbreviations: CI, confidence interval; HbA1c%, glycated hemoglobin; MD, mean difference.
The size of the review implies that no single study contributes dominant weights in the meta-analysis. Indeed, study weights range from 0.26 to 0.77. The correlation between effect size, that is, the MD, and risk of bias across studies was low and insignificant (Spearman ρ = −0.06, P = .3961). However, only 17% of the studies were evaluated to have a low risk of bias. Consequently, the risk of bias was downgraded to one level and assessed as serious.
Effect size point estimates vary widely between studies, with significant effects favoring both alternatives. I2 was high, both with and without controlling for statistically significant study covariates simultaneously in the meta-regression (I2 = 87.8% and I2 = 93%).
Discussion
This review aimed to evaluate the effectiveness of telemedicine solutions among adult patients with T2D. Overall, the results favored telemedicine. Asian studies, studies with higher baseline HbA1c% levels, and studies in hospital settings reported larger effects of telemedicine. Moreover, inclusion of a monitoring component in the telemedicine solution gave rise to a higher effect of telemedicine, whereas inclusion of a coaching component led to a lower effect. The results reflect the findings from previous systematic reviews, which have found significant reductions in HbA1c favoring telemedicine.13,22,283,284 In line with our findings, Faruque et al and Wu et al found a larger effect among studies with a higher baseline HbA1c.13,283 In contrast to our findings, Faruque et al found a larger effect in studies that used web portals or text messaging. 13 In terms of telemonitoring, Hanlon et al found improved glycemic control in studies that included telemonitoring with feedback 17 and Jaana et al found significantly reduced HbA1 through telemonitoring. 22 Hence, the ideal telemedicine setup remains to be determined, although the inclusion of a telemonitoring component seems advisable.
The heterogeneity of the included studies was large (I2 = 93.05%), which is often seen in reviews of telemedicine.13,15,284-286 In the before-mentioned systematic review by Faruque et al, the heterogeneity (I2) ranged from 58% to 75% depending on the time point Hba1c was measured. 13 A systematic review and meta-analysis by Tchero found a heterogeneity (I2) of 99% in studies comparing telemedicine with usual care in T2D. 284 Hence, the large heterogeneity found in the present review is not unusually large when compared with similar reviews. The large heterogeneity found in the present review may be explained by differences in the inclusion criteria and context of studies that vary greatly in terms of patient subgroup, provider, technology, organization, communication frequency, outcome, and so on. Moreover, the inclusion of studies from the 1990s and 2000s may have added to the heterogeneity. Telemedicine interventions in diabetes have evolved significantly during the last decades due to technological advances and differences in the interventions are thus expected to have affected heterogeneity. However, the inclusion of studies from the 1990s and 2000s has maintained the broad and inclusive scope that was intended for the present review.
The certainty of the evidence was judged as poor. First, most of the evidence (45%) stems from studies with a high risk of bias and only 17% stems from studies with a low risk of bias. However, the size of the review implies that no single study contributed dominant weights in the meta-analysis, where study weights ranged from 0.26 to 0.77. The correlation between effect size, that is, the MD, and risk of bias across studies was low and nonsignificant (Spearman ρ = −0.06, P = .3961). Taken together, the certainty of evidence was downgraded one level due to risk of bias. Second, imprecision was assessed as not serious, as the effect size was statistically significant, and the MD and lower confidence limit (MD = −0.415, 95% CI = −0.482% to −0.348%) were both clinically relevant, and all were comparable with expected effects for other quality improvement strategies, 287 which is also why no upgrading due to large effects was conducted. The total number of patients (N = 57 136) included in the review was also much higher than the optimal information size threshold (the OIS criterion). Third, inconsistency was assessed as serious. Although confidence intervals overlap considerably, effect size point estimates vary widely between studies, with significant effects favoring both alternatives. I2 was high both with and without controlling for statistically significant study covariates simultaneously in the meta-regression (I2 = 87.8% and I2 = 93%). Fourth, indirectness was not serious in this review, as all included studies were head-to-head experimental trials assessing the same outcome, and the inclusion criteria for both the population and type of intervention were broad. Fifth, although publication bias cannot be rejected with high confidence, the risk of publication bias was evaluated as undetected. Less than 100 participants were included in 35% of the studies. The Egger test for small-study effects was statistically significant (P < .000) and the funnel plot in Figure 4 reveals studies reporting both significant and insignificant positive and negative effects. The funnel plot is somewhat asymmetrical, with more studies demonstrating significant effects favoring telemedicine than negative effects. Of the 243 included studies, 32 reported industry sponsorship and 44 studies did not report whether there were sponsorships or other relevant conflicts of interest. However, the relationship between disclosed industry sponsorship and/or undisclosed relationships with both study size (above/below 100 participants) and MD (above/below mean effect across studies) was statistically nonsignificant (Fisher exact test = 0.31 and 0.11, respectively). Finally, no dose-response gradient was detected, as the contact frequency was insignificant in the meta-regression (Table 4).
Figure 4.

Funnel plot.
Abbreviation: CI, confidence interval.
The present systematic review has some limitations. First, more baseline data, such as diabetes years, blood pressure, cholesterol levels, and medication, could have been extracted. However, due to differences in reporting style, such an extraction would have resulted in a high proportion of missing data in the analysis. Second, we could have contacted the authors of the individual studies to minimize the amount of missing HbA1c data. However, due to the large sample of included papers, such a search for data was deemed too time-consuming. Third, relevant studies may have been overlooked. Although a very broad search was conducted, the search was still limited to English and Scandinavian.
Conclusion
Telemedicine may serve as an effective supplement to usual care for patients with T2D. The inclusion of a telemonitoring component seems to increase the effect of telemedicine. It seems that those with a higher HbA1c are more likely to benefit from telemedicine. Patients with poor glycemic control may benefit more from telemedicine interventions, as a high HbA1c level leaves further room for improvement. However, the ideal glycemic target group for telemedicine in T2D remains to be determined.
Supplemental Material
Supplemental material, sj-docx-1-dst-10.1177_19322968211064633 for The Effectiveness of Telemedicine Solutions for the Management of Type 2 Diabetes: A Systematic Review, Meta-Analysis, and Meta-Regression by Stine Hangaard, Sisse H. Laursen, Jonas D. Andersen, Thomas Kronborg, Peter Vestergaard, Ole Hejlesen and Flemming W. Udsen in Journal of Diabetes Science and Technology
Acknowledgments
The authors would like to thank the research librarian Connie Skrubbeltrang, who assisted in the literature search.
Footnotes
Abbreviations: GRADE, The Grading of Recommendations, Assessment, Development and Evaluation; HbA1c, glycated hemoglobin A1c; MD, mean difference; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; RCT, randomized controlled trial; T1D, type 1 diabetes; T2D, type 2 diabetes.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This is an independent manuscript commissioned and jointly funded by the Steno Diabetes Center North Denmark and Aalborg University.
ORCID iDs: Stine Hangaard  https://orcid.org/0000-0003-0395-3563
https://orcid.org/0000-0003-0395-3563
Jonas D. Andersen  https://orcid.org/0000-0001-6619-9161
https://orcid.org/0000-0001-6619-9161
Flemming W. Udsen  https://orcid.org/0000-0003-2293-9169
https://orcid.org/0000-0003-2293-9169
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271-281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 2.Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Global Status Report on Noncommunicable Diseases 2014. World Health Organization; 2014. http://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf?sequence=1. Accessed November 26, 2021. [Google Scholar]
- 4.Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14:88-98. doi: 10.1038/nrendo.2017.151. [DOI] [PubMed] [Google Scholar]
- 5.Xu G, Liu B, Sun Y, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ. 2018;362:k1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonora E, DeFronzo RA. Diabetes Complications, Comorbidities and Related Disorders. Springer; 2018. doi: 10.1007/978-3-319-44433-8. [DOI] [Google Scholar]
- 7.Doupis J, Alexandrides T, Elisaf M, et al. Influence of supervised disease understanding and diabetes self-management on adherence to oral glucose-lowering treatment in patients with type 2 diabetes. Diabetes Ther. 2019;10:1407-1422. doi: 10.1007/s13300-019-0648-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Diabetes Association. Standards of medical care in diabetes—2020 abridged for primary care providers. Clin Diabetes. 2020;38:10-38. doi: 10.2337/cd20-as01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care. 2015;38:1372-1382. doi: 10.2337/dc15-0730. [DOI] [PubMed] [Google Scholar]
- 10.Edelman S, Polonsky W. Type 2 diabetes in the real world: the elusive nature of glycemic control. Diabetes Care. 2017;40:1425-1432. doi: 10.2337/dc16-1974. [DOI] [PubMed] [Google Scholar]
- 11.Cramer JA. A systematic review of adherence with medications for diabetes. Diabetes Care. 2004;27:1218-1224. [DOI] [PubMed] [Google Scholar]
- 12.Boels AM, Vos RC, Dijkhorst-Oei LT, Rutten GEHM. Effectiveness of diabetes self-management education and support via a smartphone application in insulin-treated patients with type 2 diabetes: results of a randomized controlled trial (TRIGGER study). BMJ Open Diabetes Res Care. 2019;7:e000981. doi: 10.1136/bmjdrc-2019-000981. [DOI] [Google Scholar]
- 13.Faruque LI, Wiebe N, Ehteshami-Afshar A, et al. Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. Cmaj. 2017;189:E341-E364. doi: 10.1503/cmaj.150885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO Global Observatory for eHealth. Telemedicine: opportunities and developments in member states. Observatory. 2010;2:96. [Google Scholar]
- 15.Baron J, Mcbain H, Newman S, Psych D, Hons M. The impact of mobile monitoring technologies on glycosylated. J Diabetes Sci Technol. 2012;6:1185-1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed J E Health. 2012;18(3):175-184. [DOI] [PubMed] [Google Scholar]
- 17.Hanlon P, Daines L, Campbell C, McKinstry B, Weller D, Pinnock H. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res. 2017;19(5):e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crico C, Renzi C, Graf N, et al. mHealth and telemedicine apps: in search of a common regulation. Ecancermedicalscience. 2018;12:853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahar JH, Rosencrance GJ, Rasmussen PA. Telemedicine: past, present, and future. Cleve Clin J Med. 2018;85(12):938-942. [DOI] [PubMed] [Google Scholar]
- 20.Greenwood DA, Young HM, Quinn CC. Telehealth remote monitoring systematic review. J Diabetes Sci Technol. 2014;8(2):378-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaana M, Paré G. Home telemonitoring of patients with diabetes: a systematic assessment of observed effects. J Eval Clin Pract. 2007;13:242-253. doi: 10.1111/j.1365-2753.2006.00686.x. [DOI] [PubMed] [Google Scholar]
- 22.Pare G, Janna M, Sicotte C. Systematic review of home telemonitoring for chronic diseases: the evidence base home telemonitoring: a definition. J Am Med Informatics Assoc. 2007;14(3):269-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu L, Forbes A, Griffiths P, Milligan P, While A. Telephone follow-up to improve glycaemic control in patients with type 2 diabetes: systematic review and meta-analysis of controlled trials. Diabet Med. 2010;27(11):1217-1225. [DOI] [PubMed] [Google Scholar]
- 24.Yun JE, Park JE, Park HY, Lee HY, Park DA. Comparative effectiveness of telemonitoring versus usual care for heart failure: a systematic review and meta-analysis. J Card Fail. 2018;24(1):19-28. [DOI] [PubMed] [Google Scholar]
- 25.Cassimatis M, Kavanagh DJ. Effects of type 2 diabetes behavioural telehealth interventions on glycaemic control and adherence: a systematic review. J Telemed Telecare. 2012;18(8):447-450. [DOI] [PubMed] [Google Scholar]
- 26.Lee SWH, Ooi L, Lai YK. Telemedicine for the management of glycemic control and clinical outcomes of type 1 diabetes mellitus: a systematic review and meta-analysis of randomized controlled studies. Front Pharmacol. 2017;8:330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kongstad MB, Valentiner LS, Ried-Larsen M, Walker KC, Juhl CB, Langberg H. Effectiveness of remote feedback on physical activity in persons with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. J Telemed Telecare. 2019;25(1):26-34. [DOI] [PubMed] [Google Scholar]
- 28.Hu Y, Wen X, Wang F, et al. Effect of telemedicine intervention on hypoglycaemia in diabetes patients: a systematic review and meta-analysis of randomised controlled trials. J Telemed Telecare. 2019;25(7):402-413. [DOI] [PubMed] [Google Scholar]
- 29.European Commission. Tools and methodologies to assess the efficiency of health care services in Europe. An overview of current approaches and opportunities for improvement. Luxembourg; 2019. https://op.europa.eu/en/publication-detail/-/publication/27d2db38-76bc-11e9-9f05-01aa75ed71a1. Accessed November 26, 2021.
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laursen S, Hangaard S, Udsen F, Vestergaard P, Hejlesen O. Effectiveness of telemedicine solutions for the management of patients with diabetes: protocol for a systematic review and meta-analysis. JMIR Res Protoc. 2020;9:e22062. doi: 10.2196/22062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 33.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guyatt GH, Thorlund K, Oxman AD, et al. GRADE guidelines: 13. Preparing Summary of Findings tables and evidence profiles—continuous outcomes. J Clin Epidemiol. 2013;66:173-183. doi: 10.1016/j.jclinepi.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Guyatt G, Oxman AD, Sultan S, et al. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol. 2013;66:151-157. doi: 10.1016/j.jclinepi.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 37.Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). J Clin Epidemiol. 2011;64:407-415. doi: 10.1016/j.jclinepi.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 38.Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol. 2011;64:1303-1310. doi: 10.1016/j.jclinepi.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 39.Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines 6. Rating the quality of evidence—imprecision. J Clin Epidemiol. 2011;64:1283-1293. doi: 10.1016/j.jclinepi.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 40.Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol. 2011;64:1294-1302. doi: 10.1016/j.jclinepi.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 41.Guyatt GH, Oxman AD, Montori V, et al. GRADE guidelines: 5. Rating the quality of evidence—publication bias. J Clin Epidemiol. 2011;64:1277-1282. doi: 10.1016/j.jclinepi.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 42.Abaza H, Marschollek M. SMS education for the promotion of diabetes self-management in low & middle income countries: a pilot randomized controlled trial in Egypt. BMC Public Health. 2017;17:962. doi: 10.1186/s12889-017-4973-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agarwal G, Gaber J, Richardson J, et al. Pilot randomized controlled trial of a complex intervention for diabetes self-management supported by volunteers, technology, and interprofessional primary health care teams. Pilot Feasibility Stud. 2019;5:118. doi: 10.1186/s40814-019-0504-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Agarwal P, Mukerji G, Desveaux L, et al. Mobile app for improved self-management of type 2 diabetes: multicenter pragmatic randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:e10321. doi: 10.2196/10321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aguiar PM, da Silva CHP, Chiann C, Dórea EL, Lyra DP, Storpirtis S. Pharmacist-physician collaborative care model for patients with uncontrolled type 2 diabetes in Brazil: results from a randomized controlled trial. J Eval Clin Pract. 2018;24:22-30. doi: 10.1111/jep.12606. [DOI] [PubMed] [Google Scholar]
- 46.Akinci B, Yeldan I, Satman I, Dirican A, Ozdincler AR. The effects of Internet-based exercise compared with supervised group exercise in people with type 2 diabetes: a randomized controlled study. Clin Rehabil. 2018;32:799-810. doi: 10.1177/0269215518757052. [DOI] [PubMed] [Google Scholar]
- 47.Al Omar M, Hasan S, Palaian S, Mahameed S. The impact of a self-management educational program coordinated through WhatsApp on diabetes control. Pharm Pract (Granada). 2020;18:1841. doi: 10.18549/PharmPract.2020.2.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alanzi T, Alanazi NR, Istepanian R, Philip N. Evaluation of the effectiveness of mobile diabetes management system with social networking and cognitive behavioural therapy (CBT) for T2D. Mhealth. 2018;4:35-35. doi: 10.21037/mhealth.2018.06.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Albikawi ZF, Petro-Nustas W, Abuadas M. Self-care management intervention to improve psychological wellbeing for Jordanian patients with type two diabetes mellitus. Issues Ment Health Nurs. 2016;37:190-201. doi: 10.3109/01612840.2015.1122118. [DOI] [PubMed] [Google Scholar]
- 50.Alghafri TS, Alharthi SM, Al-Farsi Y, et al. “MOVEdiabetes”: a cluster randomized controlled trial to increase physical activity in adults with type 2 diabetes in primary health in Oman. BMJ Open Diabetes Res Care. 2018;6:e000605. doi: 10.1136/bmjdrc-2018-000605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ali MK, Singh K, Kondal D, et al. Effectiveness of a multicomponent quality improvement strategy to improve achievement of diabetes care goals a randomized, controlled trial. Ann Intern Med. 2016;165:399-408. doi: 10.7326/M15-2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ali MK, Chwastiak L, Poongothai S, et al. Effect of a collaborative care model on depressive symptoms and glycated hemoglobin, blood pressure, and serum cholesterol among patients with depression and diabetes in India: the INDEPENDENT randomized clinical trial. JAMA. 2020;324:651-662. doi: 10.1001/jama.2020.11747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aliha JM, Asgari M, Khayeri F, Ramazani M, Farajzadegan Z, Javaheri J. Group education and nurse-telephone follow-up effects on blood glucose control and adherence to treatment in type 2 diabetes patients. Int J Prev Med. 2013;4:797-802. [PMC free article] [PubMed] [Google Scholar]
- 54.Alonso-Domínguez R, Patino-Alonso MC, Sánchez-Aguadero N, García-Ortiz L, Recio-Rodríguez JI, Gómez-Marcos MA. Effect of a multifactorial intervention on the increase in physical activity in subjects with type 2 diabetes mellitus: a randomized clinical trial (EMID Study). Eur J Cardiovasc Nurs. 2019;18:399-409. doi: 10.1177/1474515119835048. [DOI] [PubMed] [Google Scholar]
- 55.Alotaibi MM, Istepanian R, Philip N. A mobile diabetes management and educational system for type-2 diabetics in Saudi Arabia (SAED). Mhealth. 2016;2:33-33. doi: 10.21037/mhealth.2016.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Anderson RM, Funnell MM, Aikens JE, et al. Evaluating the efficacy of an empowerment-based self-management consultant intervention: results of a two-year randomized controlled trial. Ther Patient Educ. 2009;1:3-11. doi: 10.1051/tpe/2009002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Anderson DR, Christison-Lagay J, Villagra V, Liu H, Dziura J. Managing the space between visits: a randomized trial of disease management for diabetes in a community health center. J Gen Intern Med. 2010;25:1116-1122. doi: 10.1007/s11606-010-1419-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Anderson-Loftin W, Barnett S, Bunn P, Sullivan P, Hussey J, Tavakoli A. Soul food light: culturally competent diabetes education. Diabetes Educ. 2005;31:555-563. doi: 10.1177/0145721705278948. [DOI] [PubMed] [Google Scholar]
- 59.Andreae SJ, Andreae LJ, Richman JS, Cherrington AL, Safford MM. Peer-delivered cognitive behavioral training to improve functioning in patients with diabetes: a cluster-randomized trial. Ann Fam Med. 2020;18:15-23. doi: 10.1370/afm.2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Anzaldo-Campos MC, Contreras S, Vargas-Ojeda A, Menchaca-Díaz R, Fortmann A, Philis-Tsimikas A. Dulce wireless Tijuana: a randomized control trial evaluating the impact of project Dulce and short-term mobile technology on glycemic control in a family medicine clinic in Northern Mexico. Diabetes Technol Ther. 2016;18:240-251. doi: 10.1089/dia.2015.0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arora S, Peters AL, Burner E, Lam CN, Menchine M. Trial to examine text message-based mhealth in emergency department patients with diabetes (TExT-MED): a randomized controlled trial. Ann Emerg Med. 2014;63:745-754.e6. doi: 10.1016/j.annemergmed.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 62.Asante E, Bam V, Diji AKA, et al. Pilot mobile phone intervention in promoting type 2 diabetes management in an urban area in Ghana: a randomized controlled trial. Diabetes Educ. 2020;46:455-464. doi: 10.1177/0145721720954070. [DOI] [PubMed] [Google Scholar]
- 63.Avdal EÜ, Kizilci S, Demirel N. The effects of web-based diabetes education on diabetes care results: a randomized control study. Comput Informatics Nurs. 2011;29:101-106. doi: 10.1097/NCN.0b013e3181fcbdc6. [DOI] [PubMed] [Google Scholar]
- 64.Azizi A, Aboutorabi R, Mazloum-Khorasani Z, Afzal-Aghaea M, Tabesh H, Tara M. Evaluating the effect of web-based Iranian diabetic personal health record app on self-care status and clinical indicators: randomized controlled trial. JMIR Med Informatics. 2016;4:e32. doi: 10.2196/medinform.6433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Benson GA, Sidebottom A, Hayes J, et al. Impact of ENHANCED (diEtitiaNs Helping pAtieNts CarE for Diabetes) telemedicine randomized controlled trial on diabetes optimal care outcomes in patients with type 2 diabetes. J Acad Nutr Diet. 2019;119:585-598. doi: 10.1016/j.jand.2018.11.013. [DOI] [PubMed] [Google Scholar]
- 66.Blackberry ID, Furler JS, Best JD, et al. Effectiveness of general practice based, practice nurse led telephone coaching on glycaemic control of type 2 diabetes: the Patient Engagement and Coaching for Health (PEACH) pragmatic cluster randomised controlled trial. BMJ. 2013;347:f5272. doi: 10.1136/bmj.f5272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bluml BM, Kolb LE, Lipman R. Evaluating the impact of year-long, augmented diabetes self-management support. Popul Health Manag. 2019;22:522-528. doi: 10.1089/pop.2018.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bogner H, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: a randomized controlled trial. Ann Fam Med. 2012;10:15-22. doi: 10.1370/afm.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bohingamu Mudiyanselage S, Stevens J, Watts JJ, et al. Personalised telehealth intervention for chronic disease management: a pilot randomised controlled trial. J Telemed Telecare. 2019;25:343-352. doi: 10.1177/1357633X18775850. [DOI] [PubMed] [Google Scholar]
- 70.Lashkari T, Borhani F, Sabzevari S, Abbaszadeh A. Effect of telenursing (telephone follow-up) on glycemic control and body mass index (BMI) of type 2 diabetes patients. Iran J Nurs Midwifery Res. 2013;18:451-456. [PMC free article] [PubMed] [Google Scholar]
- 71.Browning C, Chapman A, Yang H, et al. Management of type 2 diabetes in China: the Happy Life Club, a pragmatic cluster randomised controlled trial using health coaches. BMJ Open. 2016;6:e009319. doi: 10.1136/bmjopen-2015-009319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bujnowska-Fedak MM, Puchała E, Steciwko A. The impact of telehome care on health status and quality of life among patients with diabetes in a primary care setting in Poland. Telemed J E Health. 2011;17:153-163. doi: 10.1089/tmj.2010.0113. [DOI] [PubMed] [Google Scholar]
- 73.Buysse H, Coremans P, Pouwer F, Ruige J. Sustainable improvement of HbA1c and satisfaction with diabetes care after adding telemedicine in patients on adaptable insulin regimens: results of the TeleDiabetes randomized controlled trial. Health Informatics J. 2020;26:628-641. doi: 10.1177/1460458219844369. [DOI] [PubMed] [Google Scholar]
- 74.Capozza K, Woolsey S, Georgsson M, et al. Going mobile with diabetes support: a randomized study of a text message-based personalized behavioral intervention for type 2 diabetes self-care. Diabetes Spectr. 2015;28:83-91. doi: 10.2337/diaspect.28.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Carter EL, Nunlee-Bland G, Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspect Health Inf Manag. 2011;8:1b. [PMC free article] [PubMed] [Google Scholar]
- 76.Castelnuovo G, Manzoni GM, Cuzziol P, et al. TECNOB study: ad interim results of a randomized controlled trial of a multidisciplinary telecare intervention for obese patients with type-2 diabetes. Clin Pract Epidemiol Ment Heal. 2011;7:44-50. doi: 10.1186/1471-2458-10-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chao DY, Lin TM, Ma W-Y. Enhanced self-efficacy and behavioral changes among patients with diabetes: cloud-based mobile health platform and mobile app service. JMIR Diabetes. 2019;4:e11017. doi: 10.2196/11017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen HS, Wu TE, Jap TS, Lin SH, Hsiao LC, Lin HD. Improvement of glycaemia control in subjects with type 2 diabetes by self-monitoring of blood glucose: comparison of two management programs adjusting bedtime insulin dosage. Diabetes Obes Metab. 2008;10:34-40. doi: 10.1111/j.1463-1326.2006.00676.x. [DOI] [PubMed] [Google Scholar]
- 79.Chen T, Zhu W, Tang B, et al. A mobile phone informational reminder to improve eye care adherence among diabetic patients in rural China: a randomized controlled trial. Am J Ophthalmol. 2018;194:54-62. doi: 10.1016/j.ajo.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 80.Chiu CJ, Hu YH, Wray LA, et al. Dissemination of evidence-base minimal psychological intervention for diabetes management in Taiwan adults with type 2 diabetes. Int J Clin Exp Med. 2016;9:14489-14498. [Google Scholar]
- 81.Cho JH, Chang SA, Kwon HS, et al. Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care. 2006;29:2625-2631. doi: 10.2337/dc05-2371. [DOI] [PubMed] [Google Scholar]
- 82.Cho JH, Kim H, Yoo SH, et al. An Internet-based health gateway device for interactive communication and automatic data uploading: clinical efficacy for type 2 diabetes in a multi-centre trial. J Telemed Telecare. 2017;23:595-604. doi: 10.1177/1357633X16657500. [DOI] [PubMed] [Google Scholar]
- 83.Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11:253-260. [PubMed] [Google Scholar]
- 84.Choudhry NK, Isaac T, Lauffenburger JC, et al. Effect of a remotely delivered tailored multicomponent approach to enhance medication taking for patients with hyperlipidemia, hypertension, and diabetes the STIC2IT cluster randomized clinical trial. JAMA Intern Med. 2018;178:1190-1198. doi: 10.1001/jamainternmed.2018.3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Clark M, Hampson SE, Avery L, Simpson R. Effects of a brief tailored intervention on the process and predictors of lifestyle behaviour change in patients with type 2 diabetes. Psychol Heal Med. 2004;9:440-449. doi: 10.1080/13548500412331292250. [DOI] [PubMed] [Google Scholar]
- 86.Crowley MJ, Powers BJ, Olsen MK, et al. The Cholesterol, Hypertension, and Glucose Education (CHANGE) study: results from a randomized controlled trial in African Americans with diabetes. Am Heart J. 2013;166:179-186. doi: 10.1016/j.ahj.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 87.Crowley MJ, Edelman D, McAndrew AT, et al. Practical telemedicine for veterans with persistently poor diabetes control: a randomized pilot trial. Telemed J E Health. 2016;22:376-384. doi: 10.1089/tmj.2015.0145. [DOI] [PubMed] [Google Scholar]
- 88.Dale J, Caramlau I, Sturt J, Friede T, Walker R. Telephone peer-delivered intervention for diabetes motivation and support: the telecare exploratory RCT. Patient Educ Couns. 2009;75:91-98. doi: 10.1016/j.pec.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 89.Dario C, Toffanin R, Calcaterra F, et al. Telemonitoring of type 2 diabetes mellitus in Italy. Telemed J E Health. 2017;23:143-152. doi: 10.1089/tmj.2015.0224. [DOI] [PubMed] [Google Scholar]
- 90.Davis RM, Hitch AD, Salaam MM, Herman WH, Zimmer-Galler IE, Mayer-Davis EJ. TeleHealth improves diabetes self-management in an underserved community: diabetes TeleCare. Diabetes Care. 2010;33:1712-1717. doi: 10.2337/dc09-1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Del Prato S, Nicolucci A, Lovagnini-Scher AC, Turco S, Leotta S, Vespasiani G. Telecare provides comparable efficacy to conventional self-monitored blood glucose in patients with type 2 diabetes titrating one injection of insulin glulisine—the ELEONOR study. Diabetes Technol Ther. 2012;14:175-182. doi: 10.1089/dia.2011.0163. [DOI] [PubMed] [Google Scholar]
- 92.Delahanty LM, Levy DE, Chang Y, et al. Effectiveness of lifestyle intervention for type 2 diabetes in primary care: the REAL HEALTH-diabetes randomized clinical trial. J Gen Intern Med. 2020;35:2637-2646. doi: 10.1007/s11606-019-05629-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dugas M, Crowley K, Gao GG, et al. Individual differences in regulatory mode moderate the effectiveness of a pilot mHealth trial for diabetes management among older veterans. PLoS One. 2018;13:e0192807. doi: 10.1371/journal.pone.0192807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Duruturk N, Özköslü MA. Effect of tele-rehabilitation on glucose control, exercise capacity, physical fitness, muscle strength and psychosocial status in patients with type 2 diabetes: a double blind randomized controlled trial. Prim Care Diabetes. 2019;13:542-548. doi: 10.1016/j.pcd.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 95.Döbler A, Belnap BH, Pollmann H, Farin E, Raspe H, Mittag O. Telephone-delivered lifestyle support with action planning and motivational interviewing techniques to improve rehabilitation outcomes. Rehabil Psychol. 2018;63:170-181. doi: 10.1037/rep0000224. [DOI] [PubMed] [Google Scholar]
- 96.Eakin EG, Reeves MM, Winkler E, et al. Six-month outcomes from living well with diabetes: a randomized trial of a telephone-delivered weight loss and physical activity intervention to improve glycemic control. Ann Behav Med. 2013;46:193-203. doi: 10.1007/s12160-013-9498-2. [DOI] [PubMed] [Google Scholar]
- 97.Eakin EG, Winkler EA, Dunstan DW, et al. Living well with diabetes: 24-month outcomes from a randomized trial of telephone-delivered weight loss and physical activity intervention to improve glycemic control. Diabetes Care. 2014;37:2177-2185. doi: 10.2337/dc13-2427. [DOI] [PubMed] [Google Scholar]
- 98.Egede LE, Williams JS, Voronca DC, Knapp RG, Fernandes JK. Randomized controlled trial of technology-assisted case management in low income adults with type 2 diabetes. Diabetes Technol Ther. 2017;19:476-482. doi: 10.1089/dia.2017.0006. [DOI] [PubMed] [Google Scholar]
- 99.Egede LE, Walker RJ, Payne EH, Knapp RG, Acierno R, Frueh BC. Effect of psychotherapy for depression via home telehealth on glycemic control in adults with type 2 diabetes: subgroup analysis of a randomized clinical trial. J Telemed Telecare. 2018;24:596-602. doi: 10.1177/1357633X17730419. [DOI] [PubMed] [Google Scholar]
- 100.Estey AL, Tan MH, Mann K. Follow-up intervention: its effect on compliance behavior to a diabetes regimen. Diabetes Educ. 1990;16:291-295. doi: 10.1177/014572179001600408. [DOI] [PubMed] [Google Scholar]
- 101.Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients’ self-management: the NICHE pilot study. J Eval Clin Pract. 2008;14:465-469. doi: 10.1111/j.1365-2753.2007.00881.x. [DOI] [PubMed] [Google Scholar]
- 102.Farsaei S, Sabzghabaee A, Zargarzadeh A. Effect of pharmacist-led patient education on glycemic control of type 2 diabetes: a randomized controlled trial. J Res Med Sci. 2011;16:43-49. [PMC free article] [PubMed] [Google Scholar]
- 103.Fernandes BSM, Reis IA, Torres HdC. Evaluation of the telephone intervention in the promotion of diabetes self-care: a randomized clinical trial. Rev Lat Am Enfermagem. 2016;24:e2719. doi: 10.1590/1518-8345.0632.2719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fortmann AL, Gallo LC, Garcia MI, et al. Dulce digital: an mHealth SMS-based intervention improves glycemic control in Hispanics with type 2 diabetes. Diabetes Care. 2017;40:1349-1355. doi: 10.2337/dc17-0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fottrell E, Ahmed N, Morrison J, et al. Community groups or mobile phone messaging to prevent and control type 2 diabetes and intermediate hyperglycaemia in Bangladesh (DMagic): a cluster-randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7:200-212. doi: 10.1016/S2213-8587(19)30001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fountoulakis S, Papanastasiou L, Gryparis A, Markou A, Piaditis G. Impact and duration effect of telemonitoring on HbA1c, BMI and cost in insulin-treated diabetes mellitus patients with inadequate glycemic control: a randomized controlled study. Hormones. 2015;14:632-643. doi: 10.14310/horm.2002.1603. [DOI] [PubMed] [Google Scholar]
- 107.Franc S, Hanaire H, Benhamou PY, et al. DIABEO system combining a mobile app software with and without telemonitoring versus standard care: a randomized controlled trial in diabetes patients poorly controlled with a basal-bolus insulin regimen. Diabetes Technol Ther. 2020;22:904-911. doi: 10.1089/dia.2020.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Franciosi M, Lucisano G, Pellegrini F, et al. ROSES: role of self-monitoring of blood glucose and intensive education in patients with type 2 diabetes not receiving insulin. A pilot randomized clinical trial. Diabet Med. 2011;28:789-796. doi: 10.1111/j.1464-5491.2011.03268.x. [DOI] [PubMed] [Google Scholar]
- 109.Frosch DL, Uy V, Ochoa S, Mangione CM. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med. 2011;171:2011-2017. doi: 10.1001/archinternmed.2011.497. [DOI] [PubMed] [Google Scholar]
- 110.García AA, Brown SA, Horner SD, Zuñiga J, Arheart KL. Home-based diabetes symptom self-management education for Mexican Americans with type 2 diabetes. Health Educ Res. 2014;30:484-496. doi: 10.1093/her/cyv018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Garg R, Hurwitz S, Rein R, Schuman B, Underwood P, Bhandari S. Effect of follow-up by a hospital diabetes care team on diabetes control at one year after discharge from the hospital. Diabetes Res Clin Pract. 2017;133:78-84. doi: 10.1016/j.diabres.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 112.Gagliardino J, Arrechea V, Assad D, et al. Type 2 diabetes patients educated by other patients perform at least as well as patients trained by professionals. Diabetes Metab Res Rev. 2013;29:152-160. doi: 10.1002/dmrr. [DOI] [PubMed] [Google Scholar]
- 113.Wasif Gillani S. Determining effective diabetic care; a multicentre—longitudinal Interventional Study. Curr Pharm Des. 2016;22:6469-6476. doi: 10.2174/1381612822666160813235704. [DOI] [PubMed] [Google Scholar]
- 114.Gimbel RW, Rennert LM, Crawford P, et al. Enhancing patient activation and self-management activities in patients with type 2 diabetes using the US Department of Defense mobile health care environment: feasibility study. J Med Internet Res. 2020;22:e17968. doi: 10.2196/17968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Glasgow RE, Nutting PA, Toobert DJ, et al. Effects of a brief computer-assisted diabetes self-management intervention on dietary, biological and quality-of-life outcomes. Chronic Illn. 2006;2:27-38. doi: 10.1179/174592006X93851. [DOI] [PubMed] [Google Scholar]
- 116.Glasgow RE, Strycker LA, King DK, Toobert DJ, Rahm AK, Jex M. Robustness of a computer-assisted diabetes self-management intervention across patient characteristics, healthcare settings, and intervention staff. Am J Manag Care. 2006;12:137-145. [PubMed] [Google Scholar]
- 117.Glasgow R, Toobert D. Brief, computer-assisted diabetes dietary self-management counseling: effects on behavior, physiologic outcomes, and quality of life. Med Care. 2000;38:1062-1073. [DOI] [PubMed] [Google Scholar]
- 118.Glasgow RE, Toobert DJ, Hampson SE, Strycker LA. Implementation, generalization and long-term results of the “choosing well” diabetes self-management intervention. Patient Educ Couns. 2002;48:115-122. doi: 10.1016/S0738-3991(02)00025-3. [DOI] [PubMed] [Google Scholar]
- 119.Glasgow R, Nutting P, King D, et al. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care. 2005;28:33-39. [DOI] [PubMed] [Google Scholar]
- 120.Goodarzi M, Ebrahimzadeh I, Rabi A, Saedipoor B, Jafarabadi MA. Impact of distance education via mobile phone text messaging on knowledge, attitude, practice and self efficacy of patients with type 2 diabetes mellitus in Iran. J Diabetes Metab Disord. 2012;11:10. doi: 10.1186/2251-6581-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Goodarzi F, Zahed S, Esfahani A, Nourian M, Zamani-Alavijeh F. The effects of mobile text messages on raising knowledge of men with type 2 diabetes. Electron Physician. 2018;10:7243-7248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Graziano JA, Gross CR. A randomized controlled trial of an automated telephone intervention to improve glycemic control in type 2 diabetes. Adv Nurs Sci. 2009;32:42-57. doi: 10.1097/ANS.0b013e3181b117a9. [DOI] [PubMed] [Google Scholar]
- 123.Griffin SJ, Simmons RK, Prevost AT, et al. Multiple behaviour change intervention and outcomes in recently diagnosed type 2 diabetes: the ADDITION-Plus randomised controlled trial. Diabetologia. 2014;57:1308-1319. doi: 10.1007/s00125-014-3236-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gupta U, Gupta Y, Jose D, et al. Effectiveness of a video-based lifestyle education program compared to usual care in improving HbA1c and other metabolic parameters in individuals with type 2 diabetes: an open-label parallel arm randomized control trial (RCT). Diabetes Ther. 2020;11:667-679. doi: 10.1007/s13300-020-00769-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Haider R, Hyun K, Cheung NW, Redfern J, Thiagalingam A, Chow CK. Effect of lifestyle focused text messaging on risk factor modification in patients with diabetes and coronary heart disease: a sub-analysis of the TEXT ME study. Diabetes Res Clin Pract. 2019;153:184-190. doi: 10.1016/j.diabres.2019.04.030. [DOI] [PubMed] [Google Scholar]
- 126.Hansen C, Perrild H, Koefoed B, Zander M. Video consultations as add-on to standard care among patients with type 2 diabetes not responding to standard regimens: a randomized controlled trial. Eur J Endocrinol. 2017;176:727-736. [DOI] [PubMed] [Google Scholar]
- 127.Hare JL, Hordern MD, Leano R, Stanton T, Prins JB, Marwick TH. Application of an exercise intervention on the evolution of diastolic dysfunction in patients with diabetes mellitus efficacy and effectiveness. Circ Hear Fail. 2011;4:441-449. doi: 10.1161/CIRCHEARTFAILURE.110.959312. [DOI] [PubMed] [Google Scholar]
- 128.Hee-Sung K. Impact of web-based nurse’s education on glycosylated haemoglobin in type 2 diabetic patients. J Clin Nurs. 2007;16;1361-1366. doi: 10.1111/j.1365-2702.2005.01506.x. [DOI] [PubMed] [Google Scholar]
- 129.Heisler M, Choi H, Mase R, Long J, Reeves PJ. Effectiveness of technologically enhanced peer support in improving glycemic management among predominantly African American, low-income adults with diabetes. Diabetes Educ. 2019;45:260-271. doi: 10.1177/0145721719844547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hidrus A, Kueh YC, Norsaádah B, et al. Effects of brain breaks videos on the motives for the physical activity of Malaysians with type-2 diabetes mellitus. Int J Environ Res Public Health. 2020;17:2507. doi: 10.3390/ijerph17072507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hokanson JM, Anderson RL, Hennrikus DJ, Lando HA, Kendall DM. Integrated tobacco cessation counseling in a diabetes self-management training program: a randomized trial of diabetes and reduction of tobacco. Diabetes Educ. 2006;32:562-570. doi: 10.1177/0145721706289914. [DOI] [PubMed] [Google Scholar]
- 132.Holbrook A, Thabane L, Keshavjee K, et al. Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ. 2009;181:37-44. doi: 10.1503/cmaj.081272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Holmen H, Torbjørnsen A, Wahl AK, et al. A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes, part 2: one-year results from the Norwegian randomized controlled trial RENEWING HEALTH. JMIR Mhealth Uhealth. 2014;2:e57. doi: 10.2196/mhealth.3882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hordern MD, Coombes JS, Cooney LM, Jeffriess L, Prins JB, Marwick TH. Effects of exercise intervention on myocardial function in type 2 diabetes. Heart. 2009;95:1343-1349. doi: 10.1136/hrt.2009.165571. [DOI] [PubMed] [Google Scholar]
- 135.Huang Z, Tan E, Lum E, Sloot P, Boehm BO, Car J. A smartphone app to improve medication adherence in patients with type 2 diabetes in Asia: feasibility randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:e14914. doi: 10.2196/14914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Huizinga MM, Gebretsadik T, Garcia Ulen C, et al. Preventing glycaemic relapse in recently controlled type 2 diabetes patients: a randomised controlled trial. Diabetologia. 2010;53:832-839. doi: 10.1007/s00125-010-1658-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hunt CW, Sanderson BK, Ellison KJ. Support for diabetes using technology: a pilot study to improve self-management. Medsurg Nurs. 2014;23:231-237. [PubMed] [Google Scholar]
- 138.Iljaž R, Brodnik A, Zrimec T, Cukjati I. E-healthcare for diabetes mellitus type 2 patients—a randomised controlled trial in Slovenia. Zdr Varst. 2017;56:150-157. doi: 10.1515/sjph-2017-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Islam SMS, Peiffer R, Chow CK, et al. Cost-effectiveness of a mobile-phone text messaging intervention on type 2 diabetes—a randomized-controlled trial. Heal Policy Technol. 2020;9:79-85. doi: 10.1016/j.hlpt.2019.12.003. [DOI] [Google Scholar]
- 140.Jahangard-Rafsanjani Z, Sarayani A, Nosrati M, et al. Effect of a community pharmacist–delivered diabetes support program for patients receiving specialty medical care: a randomized controlled trial. Diabetes Educ. 2015;41:127-135. doi: 10.1177/0145721714559132. [DOI] [PubMed] [Google Scholar]
- 141.Jain V, Joshi R, Idiculla J, Xavier D. Community health worker interventions in type 2 diabetes mellitus patients: assessing the feasibility and effectiveness in Rural Central India. J Cardiovasc Dis Res. 2018;9:127-133. doi: 10.5530/jcdr.2018.3.29. [DOI] [Google Scholar]
- 142.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18:516-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Jennings CA, Vandelanotte C, Caperchione CM, Mummery WK. Effectiveness of a web-based physical activity intervention for adults with type 2 diabetes—a randomised controlled trial. Prev Med. 2014;60:33-40. doi: 10.1016/j.ypmed.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 144.Jeong JY, Jeon JH, Bae KH, et al. Smart care based on telemonitoring and telemedicine for type 2 diabetes care: multi-center randomized controlled trial. Telemed J E Health. 2018;24:604-613. doi: 10.1089/tmj.2017.0203. [DOI] [PubMed] [Google Scholar]
- 145.Jiwani R, Wang J, Berndt A, et al. Changes in patient-reported outcome measures with a technology-supported behavioral lifestyle intervention among patients with type 2 diabetes: pilot randomized controlled clinical trial. JMIR Diabetes. 2020;5:e19268. doi: 10.2196/19268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kardas P, Lewandowski K, Bromuri S. Type 2 diabetes patients benefit from the COMODITY12 mHealth system: results of a randomised trial. J Med Syst. 2016;40:259. doi: 10.1007/s10916-016-0619-x. [DOI] [PubMed] [Google Scholar]
- 147.Kassavou A, Mirzaei V, Brimicombe J, et al. A highly tailored text and voice messaging intervention to improve medication adherence in patients with either or both hypertension and type 2 diabetes in a UK primary care setting: feasibility randomized controlled trial of clinical effectiveness. J Med Internet Res. 2020;22:e16629. doi: 10.2196/16629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kempf K, Altpeter B, Berger J, et al. Efficacy of the telemedical lifestyle intervention program TeLiPro in advanced stages of type 2 diabetes: a randomized controlled trial. Diabetes Care. 2017;40:863-871. doi: 10.2337/dc17-0303. [DOI] [PubMed] [Google Scholar]
- 149.Keogh KM, Smith SM, White P, et al. Psychological family intervention for poorly controlled type 2 diabetes. Am J Manag Care. 2011;17:105-113. [PubMed] [Google Scholar]
- 150.Kim SH, Utz S. Effectiveness of a social media-based, health literacy-sensitive diabetes self-management intervention: a randomized controlled trial. J Nurs Scholarsh. 2019;51:661-669. doi: 10.1111/jnu.12521. [DOI] [PubMed] [Google Scholar]
- 151.Kim HS. A randomized controlled trial of a nurse short-message service by cellular phone for people with diabetes. Int J Nurs Stud. 2007;44:687-692. doi: 10.1016/j.ijnurstu.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 152.Kim HS, Jeong HS. A nurse short message service by cellular phone in type-2 diabetic patients for six months. J Clin Nurs. 2007;16:1082-1087. doi: 10.1111/j.1365-2702.2007.01698.x. [DOI] [PubMed] [Google Scholar]
- 153.Kim HS, Song MS. Technological intervention for obese patients with type 2 diabetes. Appl Nurs Res. 2008;21:84-89. doi: 10.1016/j.apnr.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 154.Kim SI, Kim HS. Effectiveness of mobile and Internet intervention in patients with obese type 2 diabetes. Int J Med Inform. 2008;77:399-404. doi: 10.1016/j.ijmedinf.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 155.Kim HS, Oh JA. Adherence to diabetes control recommendations: impact of nurse telephone calls. J Adv Nurs. 2003;44:256-261. doi: 10.1046/j.1365-2648.2003.02800.x. [DOI] [PubMed] [Google Scholar]
- 156.Kim HS, Oh JA, Lee HO. Effects of nurse-coordinated intervention on patients with type 2 diabetes in Korea. J Nurs Care Qual. 2005;20:154-160. doi: 10.1097/00001786-200504000-00011. [DOI] [PubMed] [Google Scholar]
- 157.Kim CJ, Kang DH. Utility of a web-based intervention for individuals with type 2 diabetes: the impact on physical activity levels and glycemic control. Comput Informatics Nurs. 2006;24:337-345. doi: 10.1097/00024665-200611000-00008. [DOI] [PubMed] [Google Scholar]
- 158.Kim MT, Han HR, Song HJ, et al. A community-based, culturally tailored behavioral intervention for Korean Americans with type 2 diabetes. Diabetes Educ. 2009;35:986-994. doi: 10.1177/0145721709345774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kim CS, Park SY, Kang JG, et al. Insulin dose titration system in diabetes patients using a short messaging service automatically produced by a knowledge matrix. Diabetes Technol Ther. 2010;12:663-669. doi: 10.1089/dia.2010.0031. [DOI] [PubMed] [Google Scholar]
- 160.Kim KM, Park KS, Lee HJ, et al. Efficacy of a new medical information system, ubiquitous healthcare service with voice inception technique in elderly diabetic patients. Sci Rep. 2015;5:18214. doi: 10.1038/srep18214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kim HS, Sun C, Yang SJ, et al. Randomized, open-label, parallel group study to evaluate the effect of Internet-based glucose management system on subjects with diabetes in China. Telemed J E Health. 2016;22:666-674. doi: 10.1089/tmj.2015.0170. [DOI] [PubMed] [Google Scholar]
- 162.King DK, Estabrooks PA, Strycker LA, Toobert DJ, Bull SS, Glasgow RE. Outcomes of a multifaceted physical activity regimen as part of a diabetes self-management intervention. Ann Behav Med. 2006;31:128-137. doi: 10.1207/s15324796abm3102_4. [DOI] [PubMed] [Google Scholar]
- 163.Kirkman MS, Weinberger M, Landsman PB, et al. A telephone-delivered intervention for patients with NIDDM: effect on coronary risk factors. Diabetes Care. 1994;17:840-846. doi: 10.2337/diacare.17.8.840. [DOI] [PubMed] [Google Scholar]
- 164.Kleinman NJ, Shah A, Shah S, Phatak S, Viswanathan V. Improved medication adherence and frequency of blood glucose self-testing using an m-health platform versus usual care in a multisite randomized clinical trial among people with type 2 diabetes in India. Telemed J E Health. 2017;23:733-740. doi: 10.1089/tmj.2016.0265. [DOI] [PubMed] [Google Scholar]
- 165.Krein SL, Klamerus ML, Vijan S, et al. Case management for patients with poorly controlled diabetes: a randomized trial. Am J Med. 2004;116:732-739. doi: 10.1016/j.amjmed.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 166.Ku EJ, Park JI, Jeon HJ, Oh T, Choi HJ. Clinical efficacy and plausibility of a smartphone-based integrated online real-time diabetes care system via glucose and diet data management: a pilot study. Intern Med J. 2020;50:1524-1532. doi: 10.1111/imj.14738. [DOI] [PubMed] [Google Scholar]
- 167.Kusnanto Widyanata KAJ, Suprajitno, Arifin H. DM-calendar app as a diabetes self-management education on adult type 2 diabetes mellitus: a randomized controlled trial. J Diabetes Metab Disord. 2019;18:557-563. doi: 10.1007/s40200-019-00468-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kwon HS, Cho JH, Kim HS, et al. Establishment of blood glucose monitoring system using the Internet. Diabetes Care. 2004;27:478-483. doi: 10.2337/diacare.27.2.478. [DOI] [PubMed] [Google Scholar]
- 169.Lauffenburger JC, Ghazinouri R, Jan S, et al. Impact of a novel pharmacist-delivered behavioral intervention for patients with poorly-controlled diabetes: the ENhancing outcomes through Goal Assessment and Generating Engagement in Diabetes Mellitus (ENGAGE-DM) pragmatic randomized trial. PLoS One. 2019;14:e0214754. doi: 10.1371/journal.pone.0214754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lazo-Porras M, Bernabe-Ortiz A, Taype-Rondan A, et al. Foot thermometry with mHeath-based supplementation to prevent diabetic foot ulcers: a randomized controlled trial. Wellcome Open Res. 2020;5:23. doi: 10.12688/wellcomeopenres.15531.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lee JY, Wong CP, Tan CSS, Nasir NH, Lee SWH. Telemonitoring in fasting individuals with type 2 diabetes mellitus during Ramadan: a prospective, randomised controlled study. Sci Rep. 2017;7:10119. doi: 10.1038/s41598-017-10564-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lee DY, Yoo SH, Min KP, Park CY. Effect of voluntary participation on mobile health care in diabetes management: randomized controlled open-label trial. JMIR Mhealth Uhealth. 2020;8:e19153. doi: 10.2196/19153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lee JY, Chan CKY, Chua SS, et al. Telemonitoring and team-based management of glycemic control on people with type 2 diabetes: a cluster-randomized controlled trial. J Gen Intern Med. 2019;35:87-94. doi: 10.1007/s11606-019-05316-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Li F, Yao P, Hsue C, Xu J, Lou Q. Impact of “Conversation Maps” on diabetes distress and self-efficacy of Chinese adult patients with type 2 diabetes: a pilot study. Patient Prefer Adherence. 2016;10:901-908. doi: 10.2147/PPA.S95449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Liebreich T, Plotnikoff RC, Courneya KS, Boulé N. Diabetes NetPLAY: a physical activity website and linked email counselling randomized intervention for individuals with type 2 diabetes. Int J Behav Nutr Phys Act. 2009;6:18. doi: 10.1186/1479-5868-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lim S, Kang SM, Shin H, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care. 2011;34:308-313. doi: 10.2337/dc10-1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Lim S, Kang SM, Kim KM, et al. Multifactorial intervention in diabetes care using real-time monitoring and tailored feedback in type 2 diabetes. Acta Diabetol. 2016;53:189-198. doi: 10.1007/s00592-015-0754-8. [DOI] [PubMed] [Google Scholar]
- 178.Lorig K, Ritter PL, Laurent DD, et al. Online diabetes self-management program: a randomized study. Diabetes Care. 2010;33:1275-1281. doi: 10.2337/dc09-2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lujan J, Ostwald SK, Ortiz M. Promotora diabetes intervention for Mexican Americans. Diabetes Educ. 2007;33:660-670. doi: 10.1177/0145721707304080. [DOI] [PubMed] [Google Scholar]
- 180.Luley C, Blaik A, Reschke K, Klose S, Westphal S. Weight loss in obese patients with type 2 diabetes: effects of telemonitoring plus a diet combination—the Active Body Control (ABC) Program. Diabetes Res Clin Pract. 2011;91:286-292. doi: 10.1016/j.diabres.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 181.Lutes LD, Cummings DM, Littlewood K, Dinatale E, Hambidge B. A community health worker–delivered intervention in African American women with type 2 diabetes: a 12-month randomized trial. Obesity. 2017;25:1329-1335. doi: 10.1002/oby.21883. [DOI] [PubMed] [Google Scholar]
- 182.Lynch EB, Liebman R, Ventrelle J, Avery EF, Richardson DJ. A self-management intervention for African Americans with comorbid diabetes and hypertension: a pilot randomized controlled trial. Prev Chronic Dis. 2014;11:E90. doi: 10.5888/pcd11.130349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.MacPhail M, Mullan B, Sharpe L, MacCann C, Todd J. Using the health action process approach to predict and improve health outcomes in individuals with type 2 diabetes mellitus. Diabetes Metab Syndr Obes Targets Ther. 2014;7:469-479. doi: 10.2147/DMSO.S68428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Marios T, Dalton S, Smart NA. The effect of tele-monitoring on exercise training adherence, functional capacity, quality of life and glycemic control in patients with type II diabetes. J Sport Sci Med. 2012;11:51-56. [PMC free article] [PubMed] [Google Scholar]
- 185.Maslakpak MH, Razmara S, Niazkhani Z. Effects of face-to-face and telephone-based family-oriented education on self-care behavior and patient outcomes in type 2 diabetes: a randomized controlled trial. J Diabetes Res. 2017;2017:8404328. doi: 10.1155/2017/8404328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Mayberry LS, Berg CA, Greevy RA, et al. Mixed-methods randomized evaluation of FAMS: a mobile phone-delivered intervention to improve family/friend involvement in adults’ type 2 diabetes self-care. Ann Behav Med. 2021;55:165-178. doi: 10.1093/abm/kaaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.McEwen MM, Pasvogel A, Murdaugh C, Hepworth J. Effects of a family-based diabetes intervention on behavioral and biological outcomes for Mexican American adults. Diabetes Educ. 2017;43:272-285. doi: 10.1177/0145721717706031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The Diabetes Network Internet-based physical activity intervention. Diabetes Care. 2001;24:1328-1334. [DOI] [PubMed] [Google Scholar]
- 189.McKay HG, Glasgow RE, Feil EG, Boles SM, Barrera MJ. Internet-based diabetes self-management and support: initial outcomes from the Diabetes Network project. Rehabil Psychol. 2002;47:31-48. doi: 10.1037/0090-5550.47.1.31. [DOI] [Google Scholar]
- 190.McKee MD, Fletcher J, Sigal I, Giftos J, Schechter C, Walker EA. A collaborative approach to control hypertension in diabetes: outcomes of a pilot intervention. J Prim Care Community Health. 2011;2:148-152. doi: 10.1177/2150131911401028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.McMahon GT, Fonda SJ, Gomes HE, Alexis G, Conlin PR. A randomized comparison of online- and telephone-based care management with Internet training alone in adult patients with poorly controlled type 2 diabetes. Diabetes Technol Ther. 2012;14:1060-1067. doi: 10.1089/dia.2012.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Mease A. Telemedicine improved diabetic management. Mil Med. 2000;165:579-584. doi: 10.1093/milmed/165.8.579. [DOI] [PubMed] [Google Scholar]
- 193.Mons U, Raum E, Krämer HU, et al. Effectiveness of a supportive telephone counseling intervention in type 2 diabetes patients: randomized controlled study. PLoS One. 2013;8:e77954. doi: 10.1371/journal.pone.0077954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Moriyama M, Nakano M, Kuroe Y, Nin K, Niitani M, Nakaya T. Efficacy of a self-management education program for people with type 2 diabetes: results of a 12 month trial. Japan J Nurs Sci. 2009;6:51-63. doi: 10.1111/j.1742-7924.2009.00120.x. [DOI] [PubMed] [Google Scholar]
- 195.Mwangi N, Bascaran C, Ng’ang’a M, et al. Feasibility of a cluster randomized controlled trial on the effectiveness of peer–led health education interventions to increase uptake of retinal examination for diabetic retinopathy in Kirinyaga, Kenya: a pilot trial. Pilot Feasibility Stud. 2020;6:102. doi: 10.1186/s40814-020-00644-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Namjoo Nasab M, Ghavam A, Yazdanpanah A, Jahangir F, Shokrpour N. Effects of self-management education through telephone follow-up in diabetic patients. Health Care Manag (Frederick). 2017;36:273-281. doi: 10.1097/HCM.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 197.Nesari M, Zakerimoghadam M, Rajab A, Bassampour S, Faghihzadeh S. Effect of telephone follow-up on adherence to a diabetes therapeutic regimen. Japan J Nurs Sci. 2010;7:121-128. doi: 10.1111/j.1742-7924.2010.00146.x. [DOI] [PubMed] [Google Scholar]
- 198.Nicolucci A, Cercone S, Chiriatti A, et al. A randomized trial on home telemonitoring for the management of metabolic and cardiovascular risk in patients with type 2 diabetes. Diabetes Technol Ther. 2015;17:563-570. doi: 10.1089/dia.2014.0355. [DOI] [PubMed] [Google Scholar]
- 199.Niswender K, Piletic M, Andersen H, Conradsen Hiort L, Hollander P. Weight change upon once-daily initiation of insulin detemir with or without dietary intervention in overweight or obese insulin-naïve individuals with type 2 diabetes: results from the DIET trial. Diabetes Obes Metab. 2014;16:186-192. doi: 10.1111/dom.12218. [DOI] [PubMed] [Google Scholar]
- 200.O’Neil PM, Miller-Kovach K, Tuerk PW, et al. Randomized controlled trial of a nationally available weight control program tailored for adults with type 2 diabetes. Obesity. 2016;24:2269-2277. doi: 10.1002/oby.21616. [DOI] [PubMed] [Google Scholar]
- 201.Odegard P, Christensen D. MAP study: RCT of a medication adherence program for patients with type 2 diabetes. J Am Pharm Assoc (2003). 2012;52:753-762. [DOI] [PubMed] [Google Scholar]
- 202.Odnoletkova I, Goderis G, Nobels F, et al. Optimizing diabetes control in people with Type 2 diabetes through nurse-led telecoaching. Diabet Med. 2016;33:777-785. doi: 10.1111/dme.13092. [DOI] [PubMed] [Google Scholar]
- 203.Oh JA, Kim HS, Yoon KH, Choi ES. A telephone-delivered intervention to improve glycemic control in type 2 diabetic patients. Yonsei Med J. 2003;44:1-8. [DOI] [PubMed] [Google Scholar]
- 204.Orsama AL, Lähteenmäki J, Harno K, et al. Active assistance technology reduces glycosylated hemoglobin and weight in individuals with type 2 diabetes: results of a theory-based randomized trial. Diabetes Technol Ther. 2013;15:662-669. doi: 10.1089/dia.2013.0056. [DOI] [PubMed] [Google Scholar]
- 205.Owolabi EO, Goon D, Ter Ajayi AI. Efficacy, acceptability and feasibility of daily text-messaging in promoting glycaemic control and other clinical outcomes in a low-resource setting of South Africa: a randomised controlled trial. PLoS One. 2019;14:e0224791. doi: 10.1371/journal.pone.0224791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Parsons SN, Luzio SD, Harvey JN, et al. Effect of structured self-monitoring of blood glucose, with and without additional TeleCare support, on overall glycaemic control in non-insulin treated Type 2 diabetes: the SMBG Study, a 12-month randomized controlled trial. Diabet Med. 2019;36:578-590. doi: 10.1111/dme.13899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Patja K, Absetz P, Auvinen A, et al. Health coaching by telephony to support self-care in chronic diseases: clinical outcomes from The TERVA randomized controlled trial. BMC Health Serv Res. 2012;12:147. doi: 10.1186/1472-6963-12-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Peasah SK, Granitz K, Vu M, Jacob B. Effectiveness of a student pharmacist-led telephone follow-up intervention to improve hemoglobin A 1C in diabetic patients. J Pharm Pract. 2020;33:832-837. doi: 10.1177/0897190019857409. [DOI] [PubMed] [Google Scholar]
- 209.Peimani M, Rambod C, Omidvar M, et al. Effectiveness of short message service-based intervention (SMS) on self-care in type 2 diabetes: a feasibility study. Prim Care Diabetes. 2016;10:251-258. doi: 10.1016/j.pcd.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 210.Piette J, Richardson C, Himle J, et al. A randomized trial of telephone counseling plus walking for depressed diabetes patients. Med Care. 2011;49:641-648. doi: 10.1038/jid.2014.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Plotnikoff RC, Karunamuni N, Courneya KS, Sigal RJ, Johnson JA, Johnson ST. The Alberta diabetes and physical activity trial (ADAPT): a randomized trial evaluating theory-based interventions to increase physical activity in adults with type 2 diabetes. Ann Behav Med. 2013;45:45-56. doi: 10.1007/s12160-012-9405-2. [DOI] [PubMed] [Google Scholar]
- 212.Presley C, Agne A, Shelton T, Oster R, Cherrington A. Mobile-enhanced peer support for African Americans with type 2 diabetes: a randomized controlled trial. J Gen Intern Med. 2020;35:2889-2896. doi: 10.1007/s11606-020-06011-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Quinn CC, Swasey KK, Crabbe JCF, et al. The impact of a mobile diabetes health intervention on diabetes distress and depression among adults: secondary analysis of a cluster randomized controlled trial. JMIR Mhealth Uhealth. 2017;5:e183. doi: 10.2196/mhealth.8910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes Care. 2011;34:1934-1942. doi: 10.2337/dc11-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Raj JP, Mathews B. Effect of behavioral intervention on medication adherence among elderly with select non-communicable diseases (ENDORSE): pilot randomized controlled trial. Geriatr Gerontol Int. 2020;20:1079-1084. doi: 10.1111/ggi.14032. [DOI] [PubMed] [Google Scholar]
- 216.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes a pilot randomized trial. Diabetes Care. 2009;32:234-239. doi: 10.2337/dc08-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Ramadas A, Chan CKY, Oldenburg B, Hussein Z, Quek KF. Randomised-controlled trial of a web-based dietary intervention for patients with type 2 diabetes: changes in health cognitions and glycemic control. BMC Public Health. 2018;18:716. doi: 10.1186/s12889-018-5640-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Rasmussen OW, Lauszus FF, Loekke M. Telemedicine compared with standard care in type 2 diabetes mellitus: a randomized trial in an outpatient clinic. J Telemed Telecare. 2016;22:363-368. doi: 10.1177/1357633X15608984. [DOI] [PubMed] [Google Scholar]
- 219.Rodríguez-Idígoras MI, Sepúlveda-Muñoz J, Sánchez-Garrido-Escudero R, et al. Telemedicine influence on the follow-up of type 2 diabetes patients. Diabetes Technol Ther. 2009;11:431-437. doi: 10.1089/dia.2008.0114. [DOI] [PubMed] [Google Scholar]
- 220.Ruggiero L, Riley BB, Hernandez R, et al. Medical assistant coaching to support diabetes self-care among low-income racial/ethnic minority populations: randomized controlled trial. West J Nurs Res. 2014;36:1052-1073. doi: 10.1177/0193945914522862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Sacco WP, Malone JI, Morrison AD, Friedman A, Wells K. Effect of a brief, regular telephone intervention by paraprofessionals for type 2 diabetes. J Behav Med. 2009;32:349-359. doi: 10.1007/s10865-009-9209-4. [DOI] [PubMed] [Google Scholar]
- 222.Sacco WP, Bykowski CA, Mayhew LL, White KE. Educational attainment moderates the effect of a brief diabetes self-care intervention. Diabetes Res Clin Pract. 2012;95:62-67. doi: 10.1016/j.diabres.2011.08.027. [DOI] [PubMed] [Google Scholar]
- 223.Samuel-Hodge CD, Keyserling TC, Park S, Johnston LF, Gizlice Z, Bangdiwala SI. A randomized trial of a church-based diabetes self-management program for African Americans with type 2 diabetes. Diabetes Educ. 2009;35:439-454. doi: 10.1177/0145721709333270. [DOI] [PubMed] [Google Scholar]
- 224.Sarayani A, Mashayekhi M, Nosrati M, et al. Efficacy of a telephone-based intervention among patients with type-2 diabetes; a randomized controlled trial in pharmacy practice. Int J Clin Pharm. 2018;40:345-353. doi: 10.1007/s11096-018-0593-0. [DOI] [PubMed] [Google Scholar]
- 225.Saslow LR, Moskowitz JT, Mason AE, et al. Intervention enhancement strategies among adults with type 2 diabetes in a very low-carbohydrate web-based program: evaluating the impact with a randomized trial. JMIR Diabetes. 2020;5:e15835. doi: 10.2196/15835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Sazlina SG, Browning CJ, Yasin S. Effectiveness of personalized feedback alone or combined with peer support to improve physical activity in sedentary older Malays with type 2 diabetes: a randomized controlled trial. Front Public Heal. 2015;3:178. doi: 10.3389/fpubh.2015.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Schillinger D, Handley M, Wang MS, Hammer H. Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes: a three-arm practical clinical trial. Diabetes Care. 2009;32:559-566. doi: 10.2337/dc08-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Shahid M, Mahar SA, Shaikh S, Shaikh ZUD. Mobile phone intervention to improve diabetes care in rural areas of Pakistan: a randomized controlled trial. J Coll Physicians Surg Pak. 2015;25:166-171. doi:03.2015/JCPSP.166171. [PubMed] [Google Scholar]
- 229.Shahsavari A, Bakhshandeh Bavarsad M. Is telenursing an effective method to control BMI and HbA1c in illiterate patients aged 50 years and older with type 2 diabetes? a randomized controlled clinical trial. J Caring Sci. 2020;9:73-79. doi: 10.34172/jcs.2020.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Shetty AS, Chamukuttan S, Nanditha A, Raj RKC, Ramachandran A. Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message service (SMS)—a pilot study. J Assoc Physicians India. 2011;59:711-714. [PubMed] [Google Scholar]
- 231.Shreck E, Gonzalez JS, Cohen HW, Walker EA. Risk perception and self-management in urban, diverse adults with type 2 diabetes: the improving diabetes outcomes study. Int J Behav Med. 2014;21:88-98. doi: 10.1007/s12529-013-9291-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Sigurdardottir AK, Benediktsson R, Jonsdottir H. Instruments to tailor care of people with type 2 diabetes. J Adv Nurs. 2009;65:2118-2130. doi: 10.1111/j.1365-2648.2009.05040.x. [DOI] [PubMed] [Google Scholar]
- 233.Skelly AH, Carlson J, Leeman J, Soward A, Burns D. Controlled trial of nursing interventions to improve health outcomes of older African American women with type 2 diabetes. Nurs Res. 2009;58:410-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Sone H, Katagiri A, Ishibashi S, et al. Effects of lifestyle modifications on patients with type 2 diabetes: the Japan Diabetes Complications Study (JDCS) study design, baseline analysis and three year-interim report. Horm Metab Res. 2002;34:509-515. doi: 10.1055/s-2002-34791. [DOI] [PubMed] [Google Scholar]
- 235.Sone H, Tanaka S, Iimuro S, et al. Long-term lifestyle intervention lowers the incidence of stroke in Japanese patients with type 2 diabetes: a nationwide multicentre randomised controlled trial (the Japan Diabetes Complications Study). Diabetologia. 2010;53:419-428. doi: 10.1007/s00125-009-1622-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Song MS, Kim HS. Intensive management program to improve glycosylated hemoglobin levels and adherence to diet in patients with type 2 diabetes. Appl Nurs Res. 2009;22:42-47. doi: 10.1016/j.apnr.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 237.Spencer MS, Kieffer EC, Sinco B, et al. Outcomes at 18 months from a community health worker and peer leader diabetes self-management program for Latino adults. Diabetes Care. 2018;41:1414-1422. doi: 10.2337/dc17-0978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Steventon A, Bardsley M, Doll H, Tuckey E, Newman SP. Effect of telehealth on glycaemic control: analysis of patients with type 2 diabetes in the Whole Systems Demonstrator cluster randomised trial. BMC Health Serv Res. 2014;14:334. doi: 10.1186/1472-6963-14-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Sun C, Sun L, Xi S, et al. Mobile phone–based telemedicine practice in older Chinese patients with type 2 diabetes mellitus: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7:e10664. doi: 10.2196/10664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Sunil Kumar D, Prakash B, Subhash Chandra BJ, et al. Technological innovations to improve health outcome in type 2 diabetes mellitus: a randomized controlled study. Clin Epidemiol Glob Heal. 2021;9:53-56. doi: 10.1016/j.cegh.2020.06.011. [DOI] [Google Scholar]
- 241.Takenga C, Berndt RD, Musongya O, et al. An ICT-based diabetes management system tested for health care delivery in the African context. Int J Telemed Appl. 2014;2014:437307. doi: 10.1155/2014/437307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Tamban C, Isip-Tan IT, Jimeno C. Use of short message services (SMS) for the management of type 2 diabetes mellitus: a randomized controlled trial. J ASEAN Fed Endocr Soc. 2013;28:143-149. doi: 10.15605/jafes.028.02.08. [DOI] [Google Scholar]
- 243.Tan CCL, Cheng KKF, Hwang SW, Zhang N, Holydard E, Wang W. Effect of a diabetes self-efficacy enhancing program on older adults with type 2 diabetes: a randomized controlled trial. Clin Nurs Res. 2020;29:293-303. doi: 10.1177/1054773818792480. [DOI] [PubMed] [Google Scholar]
- 244.Tang PC, Overhage JM, Chan AS, et al. Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Informatics Assoc. 2013;20:526-534. doi: 10.1136/amiajnl-2012-001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Teston EF, Arruda GO, de Sales CA, Serafim D, Marcon SS. Nursing appointment and cardiometabolic control of diabetics: a randomized clinical trial. Rev Bras Enferm. 2017;70:468-474. doi: 10.1590/0034-7167-2016-0352. [DOI] [PubMed] [Google Scholar]
- 246.Thom DH, Ghorob A, Hessler D, DeVore D, Chen E, Bodenheimer TA. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann Fam Med. 2013;11:137-144. doi: 10.1370/afm.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Torbjørnsen A, Jenum AK, Småstuen MC, et al. A low-intensity mobile health intervention with and without health counseling for persons with type 2 diabetes, part 1: baseline and short-term results from a randomized controlled trial in the Norwegian part of RENEWING HEALTH. JMIR Mhealth Uhealth. 2014;2:e52. doi: 10.2196/mhealth.3535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Tu KS, McDaniel G, Templeton Gay J. Diabetes self-care knowledge, behaviors, and metabolic control of older adults—the effect of a posteducational follow-up program. Diabetes Educ. 1993;19:25-30. doi: 10.1177/014572179301900105. [DOI] [PubMed] [Google Scholar]
- 249.Van Dyck D, De Greef K, Deforche B, et al. The relationship between changes in steps/day and health outcomes after a pedometer-based physical activity intervention with telephone support in type 2 diabetes patients. Health Educ Res. 2013;28:539-545. doi: 10.1093/her/cyt038. [DOI] [PubMed] [Google Scholar]
- 250.Van Dyck D, De Greef K, Deforche B, et al. Mediators of physical activity change in a behavioral modification program for type 2 diabetes patients. Int J Behav Nutr Phys Act. 2011;8:105. doi: 10.1186/1479-5868-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Van Vugt M, De Wit M, Sieverink F, et al. Uptake and effects of the e-vita personal health record with self-management support and coaching, for type 2 diabetes patients treated in primary care. J Diabetes Res. 2016;2016:5027356. doi: 10.1155/2016/5027356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Varney JE, Weiland TJ, Inder WJ, Jelinek GA. Effect of hospital-based telephone coaching on glycaemic control and adherence to management guidelines in type 2 diabetes, a randomised controlled trial. Intern Med J. 2014;44:890-897. doi: 10.1111/imj.12515. [DOI] [PubMed] [Google Scholar]
- 253.Vaughan EM, Hyman DJ, Naik AD, Samson SL, Razjouyan J, Foreyt JP. A Telehealth-supported, Integrated care with CHWs, and MEdication-access (TIME) program for diabetes improves HbA1c: a randomized clinical trial. J Gen Intern Med. 2021;36:455-463. doi: 10.1007/s11606-020-06017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Vervloet M, van Dijk L, de Bakker DH, et al. Short- and long-term effects of real-time medication monitoring with short message service (SMS) reminders for missed doses on the refill adherence of people with type 2 diabetes: evidence from a randomized controlled trial. Diabet Med. 2014;31:821-828. doi: 10.1111/dme.12439. [DOI] [PubMed] [Google Scholar]
- 255.Vinitha R, Nanditha A, Snehalatha C, et al. Effectiveness of mobile phone text messaging in improving glycaemic control among persons with newly detected type 2 diabetes. Diabetes Res Clin Pract. 2019;158:107919. doi: 10.1016/j.diabres.2019.107919. [DOI] [PubMed] [Google Scholar]
- 256.Von Storch K, Graaf E, Wunderlich M, Rietz C, Polidori MC, Woopen C. Telemedicine-assisted self-management program for type 2 diabetes patients. Diabetes Technol Ther. 2019;21:514-521. doi: 10.1089/dia.2019.0056. [DOI] [PubMed] [Google Scholar]
- 257.Wakefield BJ, Holman JE, Ray A, et al. Effectiveness of home telehealth in comorbid diabetes and hypertension: a randomized, controlled trial. Telemed J E Health. 2011;17:254-261. doi: 10.1089/tmj.2010.0176. [DOI] [PubMed] [Google Scholar]
- 258.Wakefield BJ, Holman JE, Ray A, et al. Outcomes of a home telehealth intervention for patients with diabetes and hypertension. Telemed J E Health. 2012;18:575-579. doi: 10.1089/tmj.2011.0237. [DOI] [PubMed] [Google Scholar]
- 259.Wakefield BJ, Koopman RJ, Keplinger LE, et al. Effect of home telemonitoring on glycemic and blood pressure control in primary care clinic patients with diabetes. Telemed J E Health. 2014;20:199-205. doi: 10.1089/tmj.2013.0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Waki K, Fujita H, Uchimura Y, et al. DialBetics: a novel smartphone-based self-management support system for type 2 diabetes patients. J Diabetes Sci Technol. 2014;8:209-215. doi: 10.1177/1932296814526495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Walker EA, Shmukler C, Ullman R, Blanco E, Scollan-Koliopoulus M, Cohen HW. Results of a successful telephonic intervention to improve diabetes control in urban adults: a randomized trial. Diabetes Care. 2011;34:2-7. doi: 10.2337/dc10-1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Wang X, Liu D, Du M, Hao R, Zheng H, Yan C. The role of text messaging intervention in Inner Mongolia among patients with type 2 diabetes mellitus: a randomized controlled trial. BMC Med Inform Decis Mak. 2020;20:90. doi: 10.1186/s12911-020-01129-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Wang Y, Li M, Zhao X, et al. Effects of continuous care for patients with type 2 diabetes using mobile health application: a randomised controlled trial. Int J Health Plann Manage. 2019;34:1025-1035. doi: 10.1002/hpm.2872. [DOI] [PubMed] [Google Scholar]
- 264.Wang G, Zhang Z, Feng Y, et al. Telemedicine in the management of type 2 diabetes mellitus. Am J Med Sci. 2017;353:1-5. [DOI] [PubMed] [Google Scholar]
- 265.Warren R, Carlisle K, Mihala G, Scuffham PA. Effects of telemonitoring on glycaemic control and healthcare costs in type 2 diabetes: a randomised controlled trial. J Telemed Telecare. 2018;24:586-595. doi: 10.1177/1357633X17723943. [DOI] [PubMed] [Google Scholar]
- 266.Weinberger M, Kirkman MS, Saa GP, et al. A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: impact on glycemic control and health-related quality of life. J Gen Intern Med. 1995;10:59-66. doi: 10.1007/BF02600227. [DOI] [PubMed] [Google Scholar]
- 267.Whittemore R, Melkus G, Sullivan A, Grey M. A nurse-coaching intervention for women with type 2 diabetes. Diabetes Educ. 2004;30:795-804. doi: 10.1177/014572170403000515. [DOI] [PubMed] [Google Scholar]
- 268.Wichit N, Mnatzaganian G, Courtney M, Schulz P, Johnson M. Randomized controlled trial of a family-oriented self-management program to improve self-efficacy, glycemic control and quality of life among Thai individuals with type 2 diabetes. Diabetes Res Clin Pract. 2017;123:37-48. doi: 10.1016/j.diabres.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 269.Wild SH, Hanley J, Lewis SC, et al. Supported telemonitoring and glycemic control in people with type 2 diabetes: the telescot diabetes pragmatic multicenter randomized controlled trial. PLoS Med. 2016;13:e1002098. doi: 10.1371/journal.pmed.1002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Williams ED, Bird D, Forbes AW, et al. Randomised controlled trial of an automated, interactive telephone intervention (TLC Diabetes) to improve type 2 diabetes management: baseline findings and six-month outcomes. BMC Public Health. 2012;12:602. doi: 10.1186/1471-2458-12-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Williams M, Cairns S, Simmons D, Rush E. Face-to-face versus telephone delivery of the green prescription for Māori and New Zealand Europeans with type-2 diabetes mellitus: influence on participation and health outcomes. N Z Med J. 2017;130:71-79. [PubMed] [Google Scholar]
- 272.Wolever RQ, Dreusicke M, Fikkan J, et al. Integrative health coaching for patients with type 2 diabetes: a randomized clinical trial. Diabetes Educ. 2010;36:629-639. doi: 10.1177/0145721710371523. [DOI] [PubMed] [Google Scholar]
- 273.Wolf A, Conaway M, Crowther J, et al. Translating lifestyle intervention to practice in obese patients with type 2 diabetes. Diabetes Care. 2004;27:1570-1576. [DOI] [PubMed] [Google Scholar]
- 274.Wu CJJ, Sung HC, Chang AM, Atherton J, Kostner K, McPhail SM. Cardiac-diabetes self-management program for Australians and Taiwanese: a randomized blocked design study. Nurs Heal Sci. 2017;19:307-315. doi: 10.1111/nhs.12346. [DOI] [PubMed] [Google Scholar]
- 275.Yang Y, Lee EY, Kim HS, Lee SH, Yoon KH, Cho JH. Effect of a mobile phone-based glucose-monitoring and feedback system for type 2 diabetes management in multiple primary care clinic settings: cluster randomized controlled trial. JMIR Mhealth Uhealth. 2020;8:e16266. doi: 10.2196/16266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Yasmin F, Yasmin F, Nahar N, et al. The influence of mobile phone-based health reminders on patient adherence to medications and healthy lifestyle recommendations for effective management of diabetes type 2: a randomized control trial in Dhaka, Bangladesh. BMC Health Serv Res. 2020;20:520. doi: 10.1186/s12913-020-05387-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Yoo HJ, Park MS, Kim TN, et al. A Ubiquitous Chronic Disease Care system using cellular phones and the Internet. Diabet Med. 2009;26:628-635. doi: 10.1111/j.1464-5491.2009.02732.x. [DOI] [PubMed] [Google Scholar]
- 278.Yoon KH, Kim HS. A short message service by cellular phone in type 2 diabetic patients for 12 months. Diabetes Res Clin Pract. 2008;79:256-261. doi: 10.1016/j.diabres.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 279.Young R, Taylor J, Friede T, et al. Pro-active call center treatment support (PACCTS) to improve glucose control in type 2 diabetes: a randomized controlled trial. Diabetes Care. 2005;28:278-282. [DOI] [PubMed] [Google Scholar]
- 280.Yu Y, Yan Q, Li H, et al. Effects of mobile phone application combined with or without self-monitoring of blood glucose on glycemic control in patients with diabetes: a randomized controlled trial. J Diabetes Investig. 2019;10:1365-1371. doi: 10.1111/jdi.13031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Zamanzadeh V, Zirak M, Hemmati Maslakpak M, Parizad N. Distance education and diabetes empowerment: a single-blind randomized control trial. Diabetes Metab Syndr Clin Res Rev. 2017;11:S247-S251. doi: 10.1016/j.dsx.2016.12.039. [DOI] [PubMed] [Google Scholar]
- 282.Zhou P, Xu L, Liu X, Huang J, Xu W, Chen W. Web-based telemedicine for management of type 2 diabetes through glucose uploads: a randomized controlled trial. Int J Clin Exp Pathol. 2014;7:8848-8854. [PMC free article] [PubMed] [Google Scholar]
- 283.Wu C, Wu Z, Yang L, et al. Evaluation of the clinical outcomes of telehealth for managing diabetes: a PRISMA-compliant meta-analysis. Medicine (Baltimore). 2018;97:e12962. doi: 10.1097/MD.0000000000012962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Tchero H, Kangambega P, Briatte C, Brunet-Houdard S, Retali GR, Rusch E. Clinical effectiveness of telemedicine in diabetes mellitus: a meta-analysis of 42 randomized controlled trials. Telemed J E Health. 2019;25:569-583. doi: 10.1089/tmj.2018.0128. [DOI] [PubMed] [Google Scholar]
- 285.Ekeland AG, Bowes A, Flottorp S. Methodologies for assessing telemedicine: a systematic review of reviews. Int J Med Inform. 2012;81:1-11. doi: 10.1016/j.ijmedinf.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 286.Soriano JB, García-Río F, Vázquez-Espinosa E, et al. A multicentre, randomized controlled trial of telehealth for the management of COPD. Respir Med. 2018;144:74-81. doi: 10.1016/j.rmed.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 287.Shojania KG, Ranji SR, McDonald KM, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296:427-440. doi: 10.2337/diaclin.25.4.155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dst-10.1177_19322968211064633 for The Effectiveness of Telemedicine Solutions for the Management of Type 2 Diabetes: A Systematic Review, Meta-Analysis, and Meta-Regression by Stine Hangaard, Sisse H. Laursen, Jonas D. Andersen, Thomas Kronborg, Peter Vestergaard, Ole Hejlesen and Flemming W. Udsen in Journal of Diabetes Science and Technology