Abstract
Aims:
The rapidly growing number of adults with type 2 diabetes globally means the uses and benefits of digital health initiatives to enhance self-management of diabetes warrant review. This systematic qualitative literature review aimed to understand usability of digital health initiatives for adults with type 2 diabetes.
Methods:
This systematic qualitative literature review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, the PRISMA 2020 Statement methodology. Three databases were used (SCOPUS, Medline, and CINAHL) to identify studies published from 2016 to 2021 that focused on experiences, evaluations, and usability of digital health initiatives aimed at helping adults with type 2 diabetes to self-manage their condition.
Results:
From the 407 studies identified, 35 studies were assessed for eligibility with 10 studies included in the final synthesis. Five main themes emerged: (1) unmet emotional needs, (2) enhancing self-management, (3) desire for education, (4) usability/user-experience, and (5) risk of biomedical marker reductionism.
Conclusions:
This review identified 5 key themes for consideration to understand usability of digital health initiatives. If these unmet psychosocial needs of adults with type 2 diabetes are better addressed in digital health initiatives, enhanced daily self-management will lead to more optimal diabetes management which can increase overall health outcomes, reduce the risk of longer-term complications, enhance quality of life for type 2 diabetes and improve more widespread adoption of digital health initiatives.
Keywords: digital health, adults with diabetes, adults with type 2 diabetes, self-management
Introduction
Diabetes mellitus (referred to simply as “diabetes”) is one of the most common chronic diseases globally. Diabetes currently affects approximately 463 million people aged between 20 and 79 years with this figure set to rise to 700 million people by 2045 and is one of the fastest growing health pandemics this century. 1 Diabetes is also one of the most common chronic health conditions in Australia with 1.2 million Australians, or approximately 5% of the total population in 2017 to 2018 reported as having diabetes. 2 Type 2 diabetes is the most common form of diabetes and is becoming an important and pressing public health challenge from a prevention and management point of view. 3
Type 2 diabetes is a burdensome disease with high requirements of self-management, of which digital health initiatives (a source that adults with type 2 diabetes use to manage their conditions) have an important role to play because they are cost-effective, readily available, and transcend geographical barriers to accessing care. 4 Additionally, adults with type 2 diabetes only have limited time with their healthcare professionals each year. Being able to access needed educational information to improve self-management and learn about previously unknown relationships such as the relationship between blood glucose levels and stress or HbA1c levels and glycemic variability is an invaluable role of digital health initiatives. 5
The biggest challenges highlighted by research to more widespread adoption of digital health initiatives by adults with type 2 diabetes are usability and unmet psychosocial needs (particularly in the early stages after receiving a type 2 diabetes diagnosis) which remain relatively unaddressed by digital health initiatives, followed by clinical benefit, economic benefit, safety concerns, and data privacy issues.6,7 Even with the ever-growing number of readily available digital health initiatives and advancements, both health experts and research suggest that type 2 diabetes self-management remains difficult, onerous, and complex, and continues to require substantial daily investment by patients.1,4,8 More than 99% of type 2 diabetes care is direct self-management, with adults who have type 2 diabetes spending an average of 6 hours each year with their healthcare professionals.7,9 The limited amount of time spent with healthcare professionals highlights the level of direct responsibility adults with type 2 diabetes have for their day-do-day self-management, including glucose level monitoring, nutritional intake, exercise and medication self-administration. Furthermore, research has demonstrated that clinical care for adults with type 2 diabetes and consultations with healthcare professionals has traditionally suffered from biomedical marker reductionism. 9 Little time is left for direct information provision and minimal attention is paid to psychosocial attributes of living with diabetes. 10 This in turn is reflected in the design of digital health initiatives, especially diabetes-focused mobile health apps available to the public, which also focus on biomedical markers. 11
Type 2 diabetes patient-centered design of digital health initiatives with emphasis on usability and psychosocial needs appear to be largely overlooked by digital health technology developers owing to low levels of engagement with both adults with type 2 diabetes and clinicians. This negatively impacts the potential for more widespread adoption of digital health initiatives. 12 Coupled with the focus on biomedical markers, digital health technology developers have historically relied on the large number of adults with type 2 diabetes worldwide as the basis for generating a return on investment. 6 Several studies have shown digital health initiatives, particularly mobile phone apps, have low usability ratings despite their proliferation.6,7 Only a few studies included adults with type 2 diabetes as participants during evaluations of digital health initiatives for type 2 diabetes self-management.13,14 Whilst biomedical markers are important metrics for adults with diabetes to monitor, there continue to be unmet needs and challenges with diabetes management, particularly patient psychosocial needs. This serves as a barrier to more widespread adoption and effective use of digital health initiatives. 15 This highlights the increasingly important role digital health initiatives can have within diabetes management, particularly if these barriers to greater widespread adoption are addressed. Therefore, this systematic qualitative literature review was conducted to understand the unmet psychosocial needs of diabetes regarding digital health initiatives used to manage adults with type 2 diabetes.
Methods
This systematic qualitative literature review was completed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, the PRISMA 2020 Statement methodology for undertaking a systematic review. 16
Inclusion Criteria
Qualitative studies which satisfied the following criteria were included in this review: original peer-reviewed research from an academic journal that focuses on experiences, evaluations and usability of digital health initiatives aimed at helping adults with type 2 diabetes to self-manage their condition. The studies must be in English, must be from 2016 to 2021 and must only be focused on adults with type 2 diabetes at the exclusion of type 1 diabetes, gestational diabetes, prediabetes as well as pediatric or neonatal diabetes studies. No mixed-diabetes studies were included either, in that, if the study included data or sample participants with either type 1 diabetes or type 2 diabetes, then these studies were excluded. References lists of studies were also cross-checked to ensure no eligible studies were omitted. The general exclusion criteria were studies relating to conference abstracts and book chapters.
Data Sources and Search Strategy
The overall search strategy and process was influenced by Griffith University’s systematic qualitative literature review approach from Pickering and Byrne. 17 A focused literature search was conducted using 3 databases: SCOPUS, Medline and CINAHL. These 3 databases have been chosen because of their extensive collection of articles in the field of health science, including medical technology. The following search terms were entered into the search query for each database: “Digital Health” AND “Diabetes” AND “Type 2,” and the search was limited to studies from 2016 to 2021 to restrict the results to a narrow range given the plethora of articles available in the field of diabetes and digital health. Recency was also important owing to the rapid advancements in technology, which is why the selected timeframe of 2016 onwards was determined. No adjustments were made to this search query, and it was replicated in each of the 3 databases. Additional searches were conducted by reviewing the reference list of identified studies.
Search Outcome
The search identified 407 studies in total, of which 405 were obtained from the 3 database searches: SCOPUS (79 results), Medline (76 results), CINAHL Complete (250 results). The review of reference lists of identified studies added 2 additional studies. All 407 studies were imported into Microsoft Excel and manually searched for duplicates, of which 91 were identified and removed. From the remaining 316 studies, 271 were excluded based on the title not relating to the review question, not being peer reviewed or not being from an academic journal. 45 full-text studies were assessed for eligibility and after reading each abstract and article in full, 35 studies were excluded because they were not relating to the review question in full. For example, if a study included both type 1 and type 2 diabetes, then it was excluded. 10 studies were identified and included in the final synthesis as being eligible after screening and review against the request question. Figure 1 shows the studies’ selection procedure.
Figure 1.
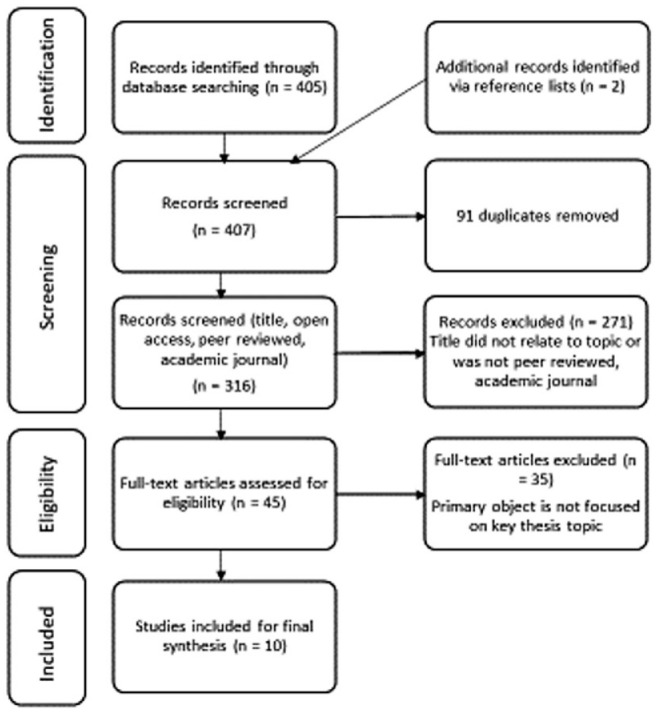
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement results.
Data Extraction
Data was collected from the 10 included studies using a prepared data extraction format in Microsoft Excel with specific criteria. The data extraction criteria included year published, names of all the authors, title of study/article, journal of publication, website address the study was sourced from, study aim, study type, sample size, main findings, and limitations. The data extraction was further extrapolated categories including: the journal discipline, the continents, countries, states and cities examined, the methods used, the type of data (qualitative), what was measured (psychosocial factors, usability, clinical benefits, educational factors and any other miscellaneous factors), the overall results (statistically significant, positive, negative, or neutral), and any comments or gaps observed in the knowledge while reviewing each study.
Quality Assessment
The quality of the 10 included studies were reviewed and assessed by the student author and team mentor independently. The quality of the included studies was reviewed using the Critical Appraisal Skills Program (CASP) as the CASP qualitative research checklist and systematic review checklist are frequently recommended and used to assess both types of studies, particularly in healthcare. 18 Risk of bias and confidence in the evidence was assessed in all studies by evaluating the validity of the results, relevance, methodological limitations, research design, recruitment strategy (where applicable) and determined using CASP that no studies were to be excluded based on the quality assessment scores. Additionally, both the student author and team mentor as independent reviewers involved in the study selection procedure determined there was no risk of bias that may influence the collective evidence in the included studies.
Data Synthesis
This systematic qualitative literature review was synthesized using thematic analysis to analyze and review the unmet psychosocial needs of Diabetes regarding digital health initiatives used to manage adults with type 2 diabetes to determine key considerations for improving usability and promote more widespread adoption.
Results
Description of Included Studies
The main characteristics of the 10 included studies is summarized in Table 1 to 4. Most of the studies were published between 2019 and 2021 (80%). Most studies were conducted in England (n = 4) or the US (n = 2) with the remainder being in Australia (n = 1), Sweden (n = 1), or globally based (n = 2). It was noted that there were no studies which specifically examined Asia, Africa, or South America, with the included studies being predominantly United States and European. The qualitative method was used the most (90% of the studies) and data were gathered using interviews (n = 4), focus groups (n = 2), both interviews and focus groups (n = 1), survey, interviews and focus groups (n = 1), meta-analysis (n = 1), or document analysis (n = 1). For the qualitative method studies, the adults with type 2 diabetes sample size ranged between 19 and 31 with an average of 21.6 participants.
Table 1.
Study Aim, Sample Size, Main Findings, and Limitations From 10 Final Studies Included in the Systematic Qualitative Literature Review.
| Year | Authors | Study aim | Sample size | Main findings | Limitations |
|---|---|---|---|---|---|
| 2020 | Baptista et al. | Assessed user-experience of a self-management app for diabetes (My Diabetes Coach [MDC]) over 12 months to understand the daily needs, preferences and what influences engagement with the app. | 19 adults with T2D | Self-management behavior can be improved by engaging with diabetes early-on following their diagnosis and providing diabetes education and self-management support (ie, via a digital app as a complement to clinical care). | Type 2 diabetes with less technology experience and who are less automous with self-management were under represented in this study. |
| 2019 | Dack et al. | Make transparent the development process and content of a successful digital self-management intervention for type 2 diabetes (HeLP-Diabetes) that is achieving the desired clinical outcomes as a road-map for others. | 20 Adults with T2D | The importance of understanding and addressing the overall impact of a long-term condition (ie, type 2 diabetes) on a patient’s life and sense of self, and the impact this has on self-management when developing a digital health initiative. | Type 2 diabetes for whom self-management is a lower priority were under represented in this study. |
| 2017 | Klonoff and Kerr | To explain why 5 identified key barriers must first be overcome in order to facilite widespread adoption of digital health initiatives for type 2 diabetes. | Observational / author’s opinions | Digital health initiatives are more likely to be adopted if developers can show usability, effectiveness, safety, sound design, and attention to the needs of diabetes. | There needs to be more of an evidence base with digital health initiatives to demonstrate safety, security, effectiveness and data privacy. |
| 2020 | Larbi et al. | To determine how digital health interventions are evaluated and whether type 2 diabetes are involved in these evaluations. | 31 studies included in systematic review | The most evaluated criteria for digital health initiatives were cognitive impact, clinical impact, and usability. Evidence showed involving type 2 diabetes in the evaluation process has a positive impact on self-management and engagement. | The search for studies covered a short period (2015-2018). |
| 2021 | Mellergard | To explore type 2 diabetes needs, views and barriers toward self-management in order to influence the development of digital health initiatives. | 22 Adults with T2D | Type 2 diabetes confirmed their need for accessible, relevant and reliable educational information as influential on their level of engagement with a digital health initiative. The need for emotional support and individualized feedback was also important. | There was no researcher triangulation—only one researcher was involved. Two or more would have been beneficial. |
| 2018 | Pal et al. | Explore unmet type 2 diabetes needs for support and self-management, and the role of digital health initiatives in meeting these needs. | 20 Adults with T2D | A diabetes diagnosis is a significant burden, which has negative impacts on a partient’s emotional well-being, physical health, social life and work. This emphased the importance of ensuring digital health intiatives address emotional needs in addition to medical needs. | People with lower health literacy and from other cultures were not explored in this study. |
| 2020 | Turnbull et al. | Understand why type 2 diabetes use digital health initiatives and how experiences vary. | 21 Adults with T2D | Type 2 diabetes used digital health interventions to help them understand and feel more in control of their bodies, by avoiding stigma and by becoming experts in their disease and/or treatment. | The participant sample was predominantly white and well educated. |
| 2021 | Turnbull et al. | Understand how type 2 diabetes use digital health initiatives and how experiences differ between individuals and social groups. | 21 Adults with T2D | Type 2 diabetes confirmed their healthcare practitioners were not a good source for digital health initiative recommendations or information. Participants relied on their social networks and digital skills instead. | The participant sample was predominantly white and well educated. |
| 2020 | Van Rhoon | Which digital health initiatives were effective with achieving clinically significant weight loss and why. | 19 studies included in systematic review | The integration of digital features and specific behavior change techniques can optimize digital health initiatives (in this example, by achieving clinically significant weight loss). | There were fewer longer-term studies in this review than shorter-term. |
| 2019 | Yingling et al. | Determine the acceptability and feasibility of wearable sensors for type 2 diabetes Hispanics. | 21 adults with T2D | Barriers to acceptability were identified (fear, trust, cost, calibration requirements and comfort) and highlighted preferences for both acceptability and feasibility. | The study was limited to a 7-day time frame and specific population (Hispanic). |
Table 4.
Types of Subjects Examined.
| Year | Authors | Sample size | Type of data | What was measured? (Subject of research) | ||||
|---|---|---|---|---|---|---|---|---|
| Qualitative | Unmet emotional needs | Enhancing self-management | Usability / user-experience | Desire for education | Risk of biomedical marker reductionism | |||
| 2020 | Baptista et al. | 19 adults with T2D | 1 | 1 | 1 | 1 | 1 | |
| 2019 | Dack et al. | 20 adults with T2D | 1 | 1 | 1 | 1 | ||
| 2017 | Klonoff & Kerr | Observational/author’s opinions | 1 | 1 | ||||
| 2020 | Larbi et al. | 31 studies included in systematic review | 1 | 1 | 1 | |||
| 2021 | Mellergard | 22 adults with T2D | 1 | 1 | 1 | 1 | ||
| 2018 | Pal et al. | 20 adults with T2D | 1 | 1 | 1 | 1 | 1 | |
| 2020 | Turnbull et al. | 21 adults with T2D | 1 | 1 | 1 | |||
| 2021 | Turnbull et al. | 21 adults with T2D | 1 | 1 | 1 | |||
| 2020 | Van Rhoon | 19 studies included in systematic review | 1 | 1 | 1 | 1 | ||
| 2019 | Yingling et al. | 21 adults with T2D | 1 | 1 | 1 | 1 | ||
Table 2.
Geographic Scope of Studies.
| Year | Authors | Countries examined | Continents | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Africa | Asia | Australia | New Zealand | United Kingdom | Europe | North America | South America | General | |||
| 2020 | Baptista et al. | Australia | 1 | ||||||||
| 2019 | Dack et al. | England | 1 | ||||||||
| 2017 | Klonoff & Kerr | US | 1 | ||||||||
| 2020 | Larbi et al. | All | 1 | ||||||||
| 2021 | Mellergard | Sweden | 1 | ||||||||
| 2018 | Pal et al. | England | 1 | ||||||||
| 2020 | Turnbull et al. | England | 1 | ||||||||
| 2021 | Turnbull et al. | England | 1 | ||||||||
| 2020 | Van Rhoon | All | 1 | ||||||||
| 2019 | Yingling et al. | United States | 1 | ||||||||
Table 3.
Methods Used for Data Gathering.
| Year | Authors | Methods used | |||||
|---|---|---|---|---|---|---|---|
| Observational Studies | Interviews | Focus groups | Field research | Case studies | Document analysis | ||
| 2020 | Baptista et al. | 1 | |||||
| 2019 | Dack et al. | 1 | 1 | ||||
| 2017 | Klonoff & Kerr | 1 | |||||
| 2020 | Larbi et al. | 1 | 1 | 1 | |||
| 2021 | Mellergard | 1 | |||||
| 2018 | Pal et al. | 1 | |||||
| 2020 | Turnbull et al. | 1 | |||||
| 2021 | Turnbull et al. | 1 | |||||
| 2020 | Van Rhoon | 1 | |||||
| 2019 | Yingling et al. | + | 1 | ||||
Themes and Subthemes
The aim of this systematic qualitative literature review was to explore whether understanding unmet psychosocial needs of adults with type 2 diabetes would help improve the usability and overall patient-centered care of digital health initiatives used to manage adults with type 2 diabetes. More specifically, this review was to synthesize available evidence of digital health initiatives taking into consideration the psychosocial needs of adults with type 2 diabetes from the perspective of patients (as the end user), the existing unmet needs of adults with type 2 diabetes regarding digital health initiatives and critically evaluate the barriers this creates for usability and adoption of digital health initiatives. On evaluating the 10 included studies, 5 main themes emerged. The main themes were that of (1) unmet emotional needs, (2) enhancing self-management, (3) desire for education, (4) usability/user-experience, and (5) risk of biomedical marker reductionism.
Unmet Emotional Needs
A total of 7 studies reported the importance and opportunity for digital health initiatives to address unmet emotional needs for adults with type 2 diabetes. One study noted many participants noted receiving little, if any, support or education after their initial diagnosis. 19 In several cases, this delayed a participant’s engagement with the self-management needed for type 2 diabetes as participants struggled to manage their strong negative emotions including depression, anxiety, guilt, and shame. 20 Participants in another study collectively agreed on the importance of access to a digital health initiative supporting self-management behavior including blood glucose monitoring, medication adherence, physical health, and diet immediately after a diagnosis of type 2 diabetes as a method of coming to terms with their diagnosis and establishing good behaviors early on. 21
Participants in 1 study described emotional barriers such as feeling stressed or not feeling understood by their healthcare professionals, noting that the focus on medical management of their diabetes and general provision of information is unlikely to meet all the needs of adults with type 2 diabetes. 22 Participants in another study revealed that they had difficulties obtaining the information and patient-centered care they needed to support themselves with their self-management when consultations with their healthcare team were time-limited or too process-driven to allow for individual patient needs. 20 This same study outlined that digital health initiatives could be a complement to clinical care by being able to better engage with and address unmet emotional needs of type 2 diabetes. 20
Managing the negative emotions associated with having type 2 diabetes as a key determinant to good self-management was emphasized in the focus group sessions of 1 study. 19 Participants of this study argued that to reduce the feeling of loss which their diagnosis has caused they would be interested in digital health initiatives that help them continue with activities they had previously taken for granted before their diagnosis that they may not be able to do going forward, or that they will need to do differently. 19 Participants in another study described how diabetes impacted the flexibility of daily life and how having to manage and live with diabetes can be socially isolating, and they desired support specifically from others with type 2 diabetes owing to mutual understandings of shared experiences. 5
Enhancing Self-Management
Five studies described the important role of digital health initiatives with enhancing self-management for adults with type 2 diabetes. Optimal diabetes management requires daily self-management owing to the necessary glucose monitoring, physical exercise, nutritional intake, medication calibration, and administering which can enhance overall health outcomes, reduce the risk of complications, and improve quality of life. 21 However, initiating and sustaining these behaviors can be difficult, which is where the discipline and behaviors required to enhance self-management of type 2 diabetes can be greatly supported by digital health initiatives, especially immediately following a diagnosis as confirmed by participants in 1 study. 21 The convenience and accessibility of digital health initiatives, particularly those accessed via mobile phones, can particularly enhance self-management of type 2 diabetes and overcome some self-management barriers currently posed by existing healthcare system limitations such as digital health initiatives being available all hours of the day and improving access to high-quality information. 20
One study, a systematic review assessing digital health initiatives which were effective in helping adults with type 2 diabetes achieve clinically significant weight loss, identified digital features which enhance self-management demonstrating the valuable role digital health initiatives play. 23 The digital features identified in most of the effective digital health initiatives, were (1) activity tracking, (2) health and lifestyle advice and information, and (3) diet and nutrition tracking. Additionally, 3 of the interventions assessed were entirely paper-based with no use of digital health initiatives to monitor physical activity and diet, and all 3 were shown to be ineffective over the long-term further demonstrating the importance of the role digital health initiatives have with enhancing self-management of Types 2 Diabetes. Reminders and prompts were also identified as effective long-term digital features that enhance self-management. 23
Desire for Education
The desire for and importance of education about type 2 diabetes was demonstrated in 5 studies. More importantly, participants in 1 study narrated that digital health initiatives provided a sense of control over the disease with better understanding and knowledge. 24 Being more informed about diabetes in general and having access to information including in some cases personal health records, created a strong sense of agency to affect their behavior, bodies and healthcare, evidencing the desire for and importance of education via digital health initiatives. 24 Type 2 diabetes reported their healthcare practitioners were not a helpful source for digital health initiative recommendations or information, owing mostly to their limited time availability. Participants relied on their social networks and digital skills instead to source digital health initiatives that would provide them with the needed information and ongoing access to educational material about type 2 diabetes. 24
Another study emphasized the ease of access to educational digital health initiatives due to mobile phone usage with all participants except 1 owning a mobile phone. 5 Owing to this, participants in the study noted an increased awareness and improved self-management of type 2 diabetes because they were able to access and learn about previously unfamiliar relationships such as the relationship between their blood glucose levels and stress or HbA1c levels and glycemic variability. 22 Digital disparities caused by unequal internet access has lessened throughout cultural and socio-economic groups, mostly owing to increased mobile phone ownership, better overall signal coverage and data transmission rates, and reduced costs of technology. There is evidence digital health initiatives are effective and acceptable in populations historically considered as underserved by health services. 24 One study reported adults with type 2 diabetes want a digital health initiative to be an all-in-one solution which they could turn to in times of need. 20
Participants in 1 study emphasized the importance of having access to educational information to start engaging with self-management immediately after the initial diagnosis of type 2 diabetes, which can be facilitated more easily through the convenience and centralization of information via digital health interventions, especially on mobile phones. 21 In the same study, it was emphasized that an absence of education caused delays in needed behavioral and self-management changes, and limited time spent with healthcare professionals was a barrier to receiving and understanding sufficient information which educational digital health initiatives could otherwise provide. 21 Additionally, educational support for patients with type 2 diabetes extends beyond the initial discussions with healthcare professionals and 1 study outlined there is generally a need for ongoing diabetes education especially at convenient times for the type 2 diabetes, anonymity and content which is presented in tailored formats including interactive media, videos and gamification. 20
Usability/User-Experience
Usability and user-experience remains challenging and according to 1 study, is the biggest challenge to digital health initiatives achieving widespread adoption for type 2 diabetes. 6 Two of the studies discussed the benefit of involving patients in the development process and regularly obtaining their feedback about digital health initiatives to support engagement and increase usability. 14 One study noted that digital health initiative product developers treat adults with diabetes as a homogenous target population and focus on short-term financial returns based on the large numbers of potential users globally rather than focusing on usability and including patients in the development stage, especially lower socio-economic groups and minorities who have historically higher rates of all forms of diabetes. 6
One study which reviewed 21 different digital health initiatives consistently found 3 specific digital features for improving usability to increase adoption of digital health initiatives for type 2 diabetes which were (1) health and lifestyle advice and information, (2) diet and nutrition tracking, and (3) activity tracking. 23 All these features were shown to be effective when incorporated within a digital health initiative, suggesting that these may comprise a valuable foundational set of features which producers of future digital health initiatives should use as a base standard. 23 Another study noted that usability is enhanced when a greater variety of modes to communicate information (ie, videos, images, text) are included as this considers a range of user preferences rather than treating all type 2 diabetes as a homogenous group. 19
Another theme which 3 studies outlined was that having 1 single digital health initiative rather than multiple different digital health initiatives to use was important for increasing usability. 20 Adults with type 2 diabetes engaged more with the digital devices requiring less input with participants in 1 study suggesting that it would be beneficial if everything could be consolidated onto a singular smart-phone to minimize user burden. 5 Participants in many of the studies reported owning either a mobile phone or 6-phone and described this was their preferred option for reviewing self-monitoring data, as it allows for more discrete usability in public. 6 Additionally, being able to data share with a family member, friend or healthcare team member was also noted in 1 study as being key to increasing usability, especially if the patient could choose with whom they shared their data. 5
Risk of Biomedical Marker Reductionism
Four studies discussed the focus of digital health initiatives on biomedical marker measurement as the almost exclusive evaluation of the impact for adults with type 2 diabetes. 14 One study which reviewed 21 different digital health initiatives noted that HbA1c levels and body weight were important biomedical markers to assess as being able to reduce the risk of type 2 diabetes was linked to clinically significant weight loss, which is contingent on being able to measure and monitor these 2 markers. 23 Another study noted that other than medication management, engagement with adults who have type 2 diabetes did not account for personal circumstances. 21 Although 1 study noted that every percentage point reduction in glycosylated hemoglobin (HbA1c) levels is coupled with a 21% reduction of risk for diabetes related deaths and a 37% reduction of risk for microvascular disease, 19 adults with type 2 diabetes felt their health professional focused mostly on lifestyle changes linked to these outcomes and gave untailored advice to lose weight or increase current exercise levels, with little personalization or emotional support. 22
Another study affirmed the importance of ensuring enjoyment and interest factors are built into digital health initiatives beyond the biomedical marker measurements as having an impact on engagement and overall attrition over time. 20 Only focusing on medical management of type 2 diabetes and providing general information may not satisfy all the needs of adults with type 2 diabetes, and 1 study reported there is insufficient evidence of a causal relationship between having knowledge about type 2 diabetes and adherence in self-management meaning digital health initiatives need to do more to address diabetes management. 22 Participants from another study emphasized that digital health initiatives should consider all parts of living with type 2 diabetes, such as dealing with difficult emotions, navigating work arrangements, managing social events, and constructively engaging with family and friends. 20
Discussion
This systematic qualitative literature review assessed 10 studies with the aim of highlighting the importance of understanding unmet psychosocial needs of adults with type 2 diabetes to help improve usability and overall patient-centered care of digital health initiatives used to manage adults with type 2 diabetes. This review identified 5 key themes for consideration to improve usability of digital health initiatives, all of which if addressed when designing digital health initiatives, have value and importance toward improving usability and more widespread adoption by adults with type 2 diabetes. This review also identified that whilst medical management of biomarkers (such as HbA1c, cholesterol, blood pressure), complication screening, and medication remain important measurable outcomes of using digital health initiatives, managing the negative emotions associated with having type 2 diabetes is a key determinant to good self-management. 19 Not sufficiently addressing or taking this into consideration remains a barrier to more widespread adoption of digital health initiatives.
One of the shortcomings with many digital health technology developers is that they consider adults with diabetes as a large homogenous group 6 and focus on biomarkers when designing digital health initiatives. However, as evidenced in this review, addressing the emotional needs of adults with type 2 diabetes, especially in the early stages of diagnosis, is likely to improve engagement with self-management as many adults with type 2 diabetes struggle to manage their negative emotional needs. 20 This leads to delays in taking positive action with managing their type 2 diabetes. Stigmatization and a variety of negative psychosocial aspects of being diabetes in addition to usability of digital health initiatives are commonly overlooked aspects of diabetes broadly. 20 If digital health technology developers can engage with and help adults with type 2 diabetes address these unmet emotional needs by involving them more in the design process of new digital health initiatives, 14 the convenience and accessibility of digital health initiatives regarding education and self-management may be utilized better and adopted faster.
Several studies identified by this review demonstrated that being more informed about diabetes in general and having access to information including in some cases personal health records, created a strong sense of agency to affect their behavior, bodies and healthcare, evidencing the desire for education via digital health initiatives. 24 This review has also shown that emotional needs need to be addressed for this transition to occur. Additionally, being aware of the risk of biomedical marker reductionism in conjunction with the importance of ensuring enjoyment and interest factors are incorporated in the design of digital health initiatives as well as using varying modalities of communicating information has also been shown to enhance engagement and adoption. 9 If digital health initiatives considered all parts of living with type 2 diabetes and covered at a minimum (1) health and lifestyle advice and information, (2) diet and nutrition tracking, and (3) activity tracking, 23 usability and more widespread adoption would likely be improved.
Strengths and Limitations of this Review
The exclusion of non-English based studies may have missed themes or other unmet psychosocial needs of adults with type 2 diabetes in other languages which could further enhance overall key considerations for improving usability of digital health initiatives. A limitation of this review is that most studies were conducted in England (n=4) or the US (n=2) with the remainder being in Australia (n=1), Sweden (n=1) or globally based (n=2). It was noted that there were no studies which specifically examined Asia, Africa, or South America, with the included studies being predominantly US and European.
The strength of this systematic qualitative literature review is that it is based on a focused and comprehensive literature search, screening, study selection, and analysis of the final 10 included studies, completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, the PRISMA 2020 Statement methodology for undertaking a systematic review. 15 Another strength is the recency of data with most of the final included studies published between 2019 and 2021 (80%). Findings from this review add to the current body of knowledge and complement previous systematic quantitative literature reviews focusing on experiences, evaluations and usability of digital health initiatives aimed at helping adults with type 2 diabetes self-manage their condition.
Conclusion
This systematic qualitative literature review critically synthesized available evidence regarding key considerations for understanding usability of digital health initiatives for adults with type 2 diabetes. It also identified the importance of addressing emotional needs and how overlooking this can cause delays in effective engagement with needed self-management for type 2 diabetes. By engaging with and even reducing associated negative emotions through provision of supportive health and lifestyle advice and information, especially immediately after the initial diagnosis stage, type 2 diabetes create a stronger sense of agency to affect their behavior, bodies, and healthcare by their desire for education through digital health initiatives. The evidence from this review is relevant to adults with type 2 diabetes, digital health product designers, clinicians treating type 2 diabetes, policymakers, and researchers as it describes the factors beyond biomedical markers which are important to engage with improve the self-management of adults with type 2 diabetes.
Footnotes
Abbreviations: CASP, Critical Appraisal Skills Program; HbA1c, hemoglobin; MDC, My Diabetes Coach; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; T2D, type 2 diabetes.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Md Shahidul Islam  https://orcid.org/0000-0001-8984-8689
https://orcid.org/0000-0001-8984-8689
References
- 1.International Diabetes Federation. IDF Diabetes Atlas Ninth Edition 2019. International Diabetes Federation. https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf. Published 2019. Accessed January 18, 2022. [Google Scholar]
- 2.Australian Institute of Health Welfare. Diabetes. Australian Institute of Health and Welfare, 2020. https://www.aihw.gov.au/reports/diabetes/diabetes. Published 2020. Accessed January 18, 2022. [Google Scholar]
- 3.Chakraborty A, Pearson O, Schwartzkopff KM, et al. The effectiveness of in-hospital interventions on reducing hospital length of stay and readmission of patients with Type 2 Diabetes Mellitus: a systematic review. Diabetes Res Clin Pract. 2021;174:108363. doi: 10.1016/j.diabres.2020.108363. [DOI] [PubMed] [Google Scholar]
- 4.Iyengar V, Wolf A, Brown A, Close K. Challenges in diabetes care: can digital health help address them? Clin Diabetes. 2016;34(3):133-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yingling L, Allen NA, Litchman ML, Colicchio V, Gibson BS. An evaluation of digital health tools for diabetes self-management in Hispanic adults: exploratory study. JMIR Diabetes. 2019;4(3):e12936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klonoff DC, Kerr D. Overcoming barriers to adoption of digital health tools for diabetes. J Diabetes Sci Technol. 2018;12(1):3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.An J, Nichols GA, Qian L, et al. Time in suboptimal glycemic control over 10 years for patients newly diagnosed with type 2 diabetes. J Diabetes Complica. 2020;34(8):107607. [DOI] [PubMed] [Google Scholar]
- 8.Cerrato P, Halamka J. The Transformative Power of Mobile Medicine. London, England: Academic Press; 2019. [Google Scholar]
- 9.Rutten G, Alzaid A. Person-centered type 2 diabetes care: time for a paradigm shift. Lancet Diabetes Endocrinol. 2018;6:264-266. [DOI] [PubMed] [Google Scholar]
- 10.Nicolucci A, Kovacs Burns K, Holt RI, et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med. 2013;30:767-777. [DOI] [PubMed] [Google Scholar]
- 11.Majeed-Ariss R, Baildam E, Campbell M, et al. Apps and adolescents: a systematic review of adolescents’ use of mobile phone and tablet apps that support personal management of their chronic or long-term physical conditions. J Med Internet Res. 2015;17:e287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turnbull S, Lucas PJ, Hay AD, Cabral C. The role of economic, educational and social resources in supporting the use of digital health technologies by people with T2D: a qualitative study. BMC Public Health. 2021;21(293):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fu H, McMahon SK, Gross CR, Adam TJ, Wyman JF. Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: A systematic review. Diabetes Res Clin Pract. 2017;131:70-81. [DOI] [PubMed] [Google Scholar]
- 14.Larbi D, Randine P, Arsand E, Antypas K, Bradway M, Gabarron E. Methods and evaluation criteria for apps and digital interventions for diabetes self-management: systematic review. J Med Internet Res. 2020;22(7):e18480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Litterbach E, Holmes-Truscott E, Pouwer F, Speight J, Hendrieckx C. I wish my health professionals understood that it’s not just all about your Hba1c!.’ Qualitative responses from the second diabetes MILES—Australia (MILES-2) study. Diabet Med. 2020;37:971-981. [DOI] [PubMed] [Google Scholar]
- 16.Page M, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2020;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pickering CM, Byrne J. The benefits of publishing systematic quantitative literature reviews for PhD candidates and other early career researchers. Higher Edu Dev. 2014;33:534-548. [Google Scholar]
- 18.Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Military Med Res. 2020;7(1):7. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dack C, Ross J, Stevenson F, et al. A digital self-management intervention for adults with type 2 diabetes: Combining theory, data and participatory design to develop HeLP-Diabetes. Internet Intervent. 2018;17:100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pal K, Dack C, Ross J, et al. Digital health interventions for adults with Type 2 diabetes: qualitative study of patient perspectives on diabetes self-management education and support. J Med Internet Res. 2018;20(2):e40. http://www.jmir.org/2018/2/e40/. Accessed January 18, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baptista S, Wadley G, Bird D, Oldenburg B, Speight J. User experiences with a Type 2 diabetes coaching app: qualitative study. JMIR Diabetes. 2020;5(3):e16692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mellergard E, Johnsson P, Eek F. Developing a web-based support using self-affirmation to motivate lifestyle changes in type 2 diabetes: A qualitative study assessing patient perspectives on self-management and views on a digital lifestyle intervention. Internet Intervent. 2021;24:e100384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Rhoon L, Byrne M, Morrissey E, Murphy J, McSharry J. A systematic review of the behavior change techniques and digital features in technology-driven type 2 diabetes prevention interventions. Digital Health. 2020;6:1-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turnbull S, Lucas PJ, Hay AD, Cabral C. Digital health interventions for people with type 2 diabetes to develop self-care expertise, adapt to identity changes, and influence other’s perception: qualitative study. J Med Internet Res. 2020;22(12):e21328. [DOI] [PMC free article] [PubMed] [Google Scholar]


