Abstract
Introduction
Pseudomonas aeruginosa is an opportunistic pathogen, which causes healthcare-associated infections in immunosuppressed patients. They exhibit resistance to multiple classes of antibiotics via various mechanisms such as the over-expression of efflux pumps, decreased production of the outer membrane protein (D2 porin), over-expression of the chromosomally encoded AmpC cephalosporinase, modification of drugs, and mutation(s) at the target site of the drug. The bacteria also develop antibiotic resistance through the acquisition of resistance genes carried on mobile genetic elements. Limited data on phenotypic as well as genotypic characterization of MDR P. aeruginosa in Nepal infers the needs for this study. This study was carried out to determine the prevalence rate of metallo-β-lactamase (MBL-producer) as well as colistin resistant multidrug resistant (MDR) P. aeruginosa in Nepal and also to detect MBL, colistin resistance, and efflux pump encoding genes i.e. blaNDM−1, mcr-1 and MexB respectively in MDR P. aeruginosa isolated from clinical samples.
Methods/methodology
A total of 36 clinical isolates of P. aeruginosa were collected. All bacterial isolates were phenotypically screened for antibiotic susceptibility using Kirby Bauer Disc Diffusion method. All the multidrug resistant P. aeruginosa were phenotypically screened for MBL producer by Imipenem-EDTA combined disc diffusion test (CDDT). Similarly, MIC value for colistin was also determined by broth microdilution method. Genes encoding carbapenemase (blaNDM−1), colistin resistant (mcr-1) and efflux pump activity (MexB) were assayed by PCR.
Results
Among 36 P. aeruginosa, 50% were found to be MDR among which 66.7% were found to be MBL producer and 11.2% were found to be colistin resistant. Among MDR P. aeruginosa, 16.7%, 11.2% and 94.4% were found to be harbouring blaNDM−1, mcr-1 and MexB genes respectively.
Conclusion
In our study, carbapenemase production (encoded by blaNDM−1), colistin resistant enzyme production (encoded by mcr-1), and expression of efflux pump (encoded by MexB) are found to be one of the major causes of antibiotic resistance in P. aeruginosa. Therefore, periodic phenotypic as well as genotypic study in Nepal on P. aeruginosa would provide the scenario of resistance pattern or mechanisms in P. aeruginosa. Furthermore, new policies or rules can be implemented in order to control the P. aeruginosa infections.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12866-023-02906-w.
Keywords: Pseudomonas aeruginosa, blaNDM−1, mcr-1, MexB, Multidrug resistant
Introduction
Pseudomonas aeruginosa is a most common pathogen that causes serious nosocomial and opportunistic infections in immunosuppressed patients [1]. Due to the inherent and acquired mediated resistance to available antibiotics, P. aeruginosa is currently turning into the most terrifying pathogen, or “Superbugˈˈ whose last resort of antibiotics is carbapenem [2, 3]. However, resistance to carbapenem is also emerging rapidly nowadays with the prevalence rate between 5 to 25% in Nepal [4]. As a result, by 2018 WHO has listed such carbapenem resistant P. aeruginosa under critical group for which no new antibiotics are developed till date [2]. Due to this reason, despite having several side effects (i.e. nephrotoxicity and neurotoxicity effect), an old antibiotic i.e. colistin are now used as a last line drugs to treat such emerging pathogens [2, 5]. However, colistin resistant P. aeruginosa is also being reported recently that is in increasing trend globally [6]. Similarly, in P. aeruginosa along with carbapenem and colistin resistant genes, overexpression of efflux pump is also one of the intrinsic mechanism that is serving them to develop into superbugs.
In Pseudomonas spp., mostly metallo-β-lactamases (MBLs) type carbapenemases are of particular concern because of their rapid spread and sturdy carbapenemase activity [3]. Several types of MBLs such as VIM, SPM, IMP, AIM, GIM, FIM and NDM and their variants have been reported [7]. Among them most common type in P. aeruginosa is NDM type; as it is located in plasmid and have a high global dissemination rate [8, 9]. Likewise, in Nepal, the prevalence of colistin resistant P. aeruginosa has increased to 2.8% [6]. Resistance to colistin in bacterial species can be either intrinsic type or acquired via chromosomal mutation or genes carried on plasmid [10]. Thus far, only one mechanism that can be transferred through plasmid (i.e. mcr) has been detected [11]. Even though other variants of mcr (mcr-2 to -9) have been detected, mcr-1 is the most prevalent marker to date globally [8].
In P. aeruginosa, MexAB-OprM is one of the paramount types of efflux pump that is expressed constitutively. It is leading P. aeruginosa to develop into multidrug resistant by targeting multiple classes of antibiotics including β-lactam, fluoroquinolones, tetracyclines, chloramphenicol, macrolides, novobiocin, trimethoprim and sulphonamides [9, 12].
Therefore, overexpression of efflux pump, emergence of carbapenem and colistin resistant P. aeruginosa are leaving no options for treatment of infection caused by P. aeruginosa. If no new antibiotics are developed in future, increase in prevalence of superbugs would be the major cause of high mortality rate in future.
In Nepal, limited studies on carbapenemase producer P. aeruginosa are available. It is essential to report present scenario of prevalence of carbapenem resistant P. aeruginosa. Similarly, there is no report of mcr-1 and MexB harbouring P. aeruginosa in Nepal. Therefore, it is essential to conduct this study to understand the mechanisms of resistance in MDR P. aeruginosa. Similarly, this study also helps to understand global spread scenario of plasmid mediated mcr-1 and blaNDM−1.
Materials and methods
This study was hospital based cross-sectional study. The phenotypic study was conducted in Microbiology Department of Upendra Devkota Memorial National Institute of Neurological and Allied Sciences (UDM-NINAS), Bansbari, Kathmandu from January to August 2021. Further, the genetic analysis was carried out in Central Department of Microbiology, Tribhuvan University, Kirtipur, Kathmandu.
Ethical approval and consent from the participant
The ethical approval (Ref. No.: 117/2021) of the study was obtained from the Institutional Review Committee of UDM-NINAS. Written informed consent was obtained from the patients before collection of specimens and data. The data were kept confidential.
Sample collection and transport
Seven hundred seventy clinical samples including tracheal aspirates, pus, urine, tip of Foley’s catheter, sputum, throat swab, blood, CSF, pleural fluid, CVP tip were collected from all age group of both genders visiting hospital during our study period. All the samples were labelled properly with patient’s ID number, lab ID number, date, time and method of collection and transported to the laboratory following the World Health Organization (WHO) guidelines. Whereas, those samples which were not properly labelled, improperly transported with visible signs of contamination and lacked patients’ complete information were excluded.
Isolation and identification of bacteria
All the samples were inoculated directly into blood agar, MacConkey agar and chocolate agar. P. aeruginosa colonies were identified on the basis of colony characteristics on the respective media. Colonies showing typical P. aeruginosa characteristics on culture and morphology on gram staining were transferred to nutrient agar and incubated at 37 °C for 24 h. Further, identification was done by pyocyanin (blue-green) pigmentation and conventional biochemical tests including catalase and oxidase test. Similarly, P. aeruginosa were separated from other Pseudomonas spp by observing growth on cetrimide agar at 42 °C for 24 h [13].
Antibiotic susceptibility testing
Antibiotic susceptibility tests of all isolates were performed using Kirby Bauer disc diffusion method on Mueller-Hinton Agar with recommended antibiotics by CLSI 2020 guidelines [14].The antibiotics used were gentamicin (GEN,30 µg), amikacin (AK, 10 µg), ciprofloxacin (CIP, 5 µg), ceftazidime (CAZ, 30 µg), cefepime (CPM, 30 µg), aztreonam (AT, 30 µg), imipenem (IPM, 10 µg), piperacillin (PI,30 µg), piperacillin-tazobactam (PIT), meropenem (MRP, 10 µg), ofloxacin (OF, 30 µg), Levofloxacin (LEV, 30 µg) and colistin (CL,10 µg) from Hi-Media, Laboratories Pvt. Ltd. India.
Isolates that were non-susceptible to at least one agent in ≥ 3 antimicrobial categories have been categorized under MDR [15].
Screening for MBL producers
All the multidrug resistant P. aeruginosa were subjected for MBL detection. Phenotypic confirmatory test for MBL producers were carried out by using Imipenem-EDTA combined disc diffusion test (CDDT).
Two imipenem discs were placed on agar plate’s containing lawn culture of test organism. 10 µl of EDTA solution was applied to one of the imipenem disc, placed 25 mm apart (center-center) and the plate was incubated at 37 °C. After 18–24 h of incubation, an increase of ≥ 7 mm in the zone diameter of imipenem-EDTA disc as compared to imipenem disc alone was considered to be positive test for the presence of MBL [14].
Determination of minimum inhibitory concentration of colistin by broth dilution method
Colistin resistance was phenotypically detected by broth microdilution method, using colistin sulphate powder (Sigma- Aldrich). The results of MIC were interpreted according to European Committee on Antimicrobial Susceptibility Testing guidelines (EUCAST) [16].
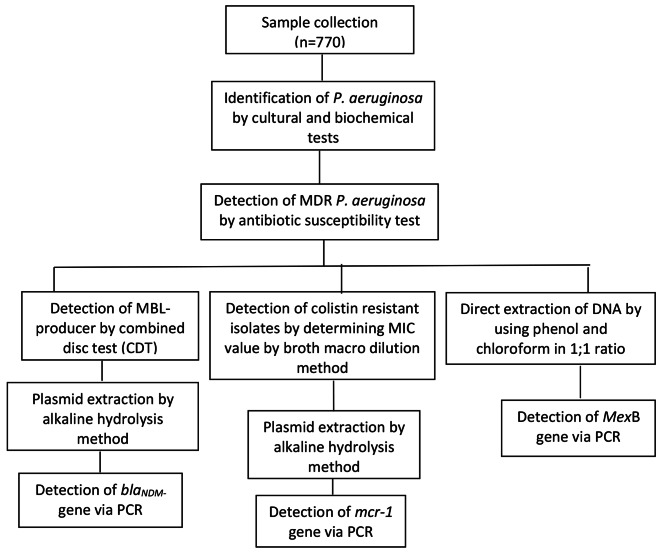
DNA extraction and quantification
For molecular analysis, all MDR P. aeruginosa isolates were subjected to the alkaline lysis method for plasmid DNA extraction and phenol chloroform method for chromosomal DNA extraction [17]. The extracted DNA was quantified by using Nanodrop and its band was visualized on agarose gel stained with ethidium bromide (Fig. 1).
Fig. 1.
Flowchart of the procedure
PCR analysis of blaNDM−1,mcr-1, and MexB genes
PCR of blaNDM−1, mcr-1 and MexB genes were performed as below in the table.
| Genes | Primer | Base pair | PCR reaction mixture | Temperature profile and Reference |
|---|---|---|---|---|
| Bla NDM−1 |
F = GGT TTG GCG ATC TGG TTT TC R=(CGG AAT GGC TCA TCA CGA TC |
621 bp | 8.5 µl of 2X master mix, 0.5 µl of 10 picomolar primer (forward and reverse), 12.5 µl of nuclease free water and 3 µl of extracted DNA template | initial denaturation at 94 °C for 5 min, followed by 36 cycles of 95 °C for 30 s, 52 °C for 40 s and 72 °C for 50 s with final extension at 72 °C for 5 min [18]. |
| Mcr-1 |
F = CGGTCAGTCCGTTTGTTC R = CTTGGTCGGTCTGTAGGG |
309 bp | 21 µl 1X master mix, 0.5 µl of 10 pmolar primer (forward and reverse) and 3 µl of extracted plasmid DNA |
Initial heating at 95 °C for 15 min, then 35 cycles of 94 °C for 10 s, 57 °C for 90 s and 72 °C for 90 s and final extension at 72 °C for 10 min. [19] |
| MexB |
F = TGTCGAAGTTTTTCATTGATAG R = AAGGTCAC GGTGATGGT |
280 bp | 21 µl of 1X Qiagen master mix, 0.5 µl of 10 pmole primers (forward and reverse) and 3 µl of extracted DNA template. | Initial heating at 94 °C for 3 min, then 32 cycles of 94 °C for 30 s, 55 °C for 45 s and 72 °C for 1 min and final extension at 72 °C for 7 min [20]. |
Data analysis
Data obtained were analyzed using SPSS version 18. The p < 0.05 was considered statistically significant.
Results
Growth profile in different clinical samples
Out of total 770 different clinical samples cultured during the study, bacterial growth was observed in 27.4% (n = 211) samples. P. aeruginosa was isolated only from 4.6% (n = 36) samples. Majority of P. aeruginosa isolates were obtained from tracheal aspirates (36.1%), followed by sputum (25%) and blood (13.9%).
Antibiotic susceptibility pattern
Altogether 36 isolates of P. aeruginosa were tested against different antibiotics classes. Among these antibiotics tested more number of P. aeruginosa were found susceptible towards carbapenems and piperacillin + β-lactam inhibitor (66.7%) antibiotic classes (Table 1). Likewise, about 50% of P. aeruginosa isolates were found to be multidrug resistant.
Table 1.
Antibiotic susceptibility pattern of P. aeruginosa
| Antibiotic category | Antibiotics | Antibiotics susceptibility pattern | |
|---|---|---|---|
| Sensitive (%) | Resistant (%) | ||
| Penicillin | Piperacillin | 18(50) | 18(50) |
| Penicillin + β-lactam inhibitor | Piperacillin + tazobactam | 24(66.7) | 12(33.3%) |
| 3rd generation cephalosporin | Ceftazidime | 18(50) | 18(50) |
| 4th generation cephalosporin | Cefepime | 18(50) | 18(50) |
| Monobactams | Aztreonam | 17(47.2) | 19(52.8) |
| Carbapenems | Imipenem | 24(66.7) | 12(33.3) |
| Meropenem | 24(66.7) | 12(33.3) | |
| Aminoglycosides | Amikacin | 18(50) | 18(50) |
| Gentamicin | 18(50) | 18(50) | |
| Fluroquinolones | Ciprofloxacin | 19(52.8) | 17(47.2) |
| Levofloxacin | 17(47.2) | 19(52.8) | |
| Ofloxacin | 17(47.2) | 19(52.8) | |
Metallo-β-lactamase detection
Using CDDT phenotypic method to identify metallo-β-lactamase (MBL), the prevalence of MBL producing P. aeruginosa isolates was found to be 33.3%. There was statistical significant association between MBL producer and MDR isolates (p < 0.001) (Table 2).
Table 2.
Distribution of MBL producers among MDR isolates
| Metallo-β-lactamase | Total | p-value (Fischer’s exact test) | |||
|---|---|---|---|---|---|
| MBL producer (%) | MBL non-producer (%) | ||||
| Multidrug resistant | MDR | 12(66.7) | 6(33.3) | 18 | |
| Non-MDR | 0(0.00) | 18(100) | 18 | 0.000 | |
| 12 | 24 | 36 | |||
Determination of MIC value of colistin
Out of 36 isolates of P. aeruginosa, 2 (11.2%) were found to colistin resistant. MICs of colistin for P. aeruginosa isolates were found to be ranged between 1(µg/ml) to 8(µg/ml). Highest MIC value was found to be 8 µg/ml (Table 3).
Table 3.
MIC value of colistin among P. aeruginosa isolates
| Organism | Number | Concentration of colistin | |||
|---|---|---|---|---|---|
| 1 µg/ml | 2 µg/ml | 4 µg/ml | 8 µg/ml | ||
| P. aeruginosa | 36 |
28 (77.8%) |
6 (16.7%) |
0 |
2 (5.6%) |
Prevalence of NDM-1 among multidrug resistant P. aeruginosa
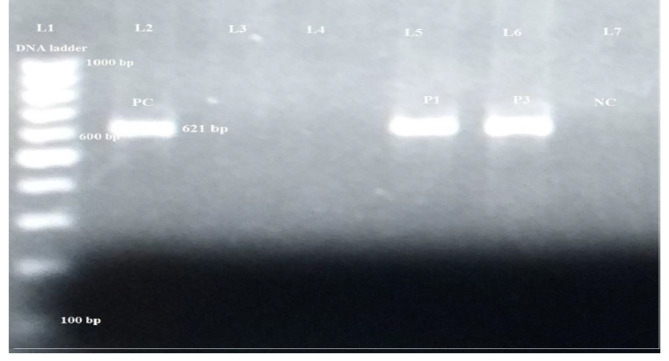
New Delhi metallo β-lactamase-1 (NDM-1) genotypes were detected by conventional PCR method using blaNDM−1 specific primer pair. Among 18 MDR P. aeruginosa, 3 (16.7%) isolates were blaNDM−1 positive. Similarly, 25% of MBL producer harboured blaNDM−1 (Fig. 2).
Fig. 2.
PCR amplification of blaNDM−1 gene in MDR P. aeruginosa isolates
Lane L1: DNA size marker (100–1000 bp); Lane 2: positive control; Lane 3&4: blaNDM−1negative; Lane 5&6: blaNDM−1 positive; Lane 7: negative control.
Characteristics of blaNDM−1 harbouring P. aeruginosa isolates
Three P. aeruginosa, P1, P3 and P6 were isolated from tracheal swab, urine and pus respectively, were found to be harbouring blaNDM−1 genes. All three isolates were susceptible to colistin and were isolated from ICU ward patients (Table 4).
Table 4.
Characteristics of blaNDM−1 harbouring P. aeruginosa isolates
| Characteristics | Patient-1 | Patient-2 | Patient 3 |
|---|---|---|---|
| Isolate Number | P1 | P3 | P6 |
| Age(yr)/Sex | 57y/Female | 59y/Male | 30y/Female |
| Hospital location | ICU | ICU | ICU |
| Specimen source | Tracheal swab | Urine | Pus |
| Underlying disease/diagnosis | Sub-dural haemorrhage | Post stroke seizure | TB meningitis, transverse myelitis and communicating hydrocephalus |
| Co-morbid conditions | Diabetes& hypertension | Diabetes& hypertension | None |
| Antimicrobials used prior to detection of blaNDM−1 | Cefotaxime, gentamicin and ciprofloxacin | Flucloxacillin, meropenem and ciprofloxacin | Nitrofurantoin, ceftriaxone and flucloxacillin |
| Antibiotics tested | |||
| Amikacin | R | R | R |
| Gentamicin | R | R | R |
| Ciprofloxacin | R | R | R |
| Imipenem | R | R | R |
| Meropenem | R | R | R |
| Piperacillin | R | R | R |
| Piperacillin/tazobactam | R | R | R |
| Aztreonam | R | R | R |
| Ofloxacin | R | R | R |
| Levofloxacin | R | R | R |
| Ceftazidime | R | R | R |
| Cefepime | R | R | R |
| Colistin | S | S | S |
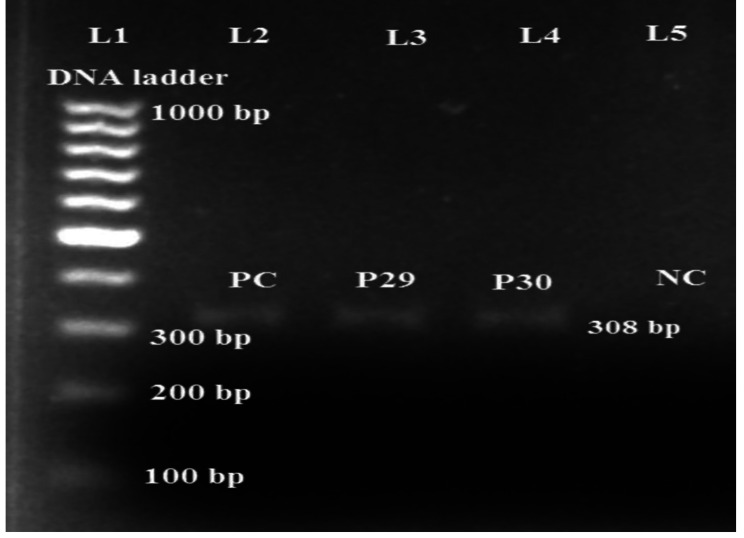
Prevalence of mcr-1 among multidrug resistant P. aeruginosa
mcr-1 gene was detected by conventional PCR method using mcr-1 specific primer pair. Among 18 MDR P. aeruginosa, 2 (11.1%) were mcr-1 positive (Fig. 3).
Fig. 3.
PCR amplification of mcr-1 gene in MDR P. aeruginosa isolates
Lane L1: DNA size marker (100–1000 bp); Lane 2: positive control (mcr-1 positive plasmid DNA); Lane 3&4: mcr-1 positive; Lane 5: negative control.
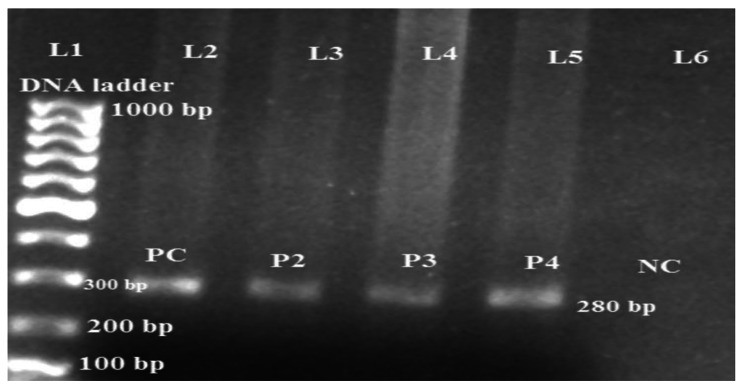
Prevalence of MexB among multidrug resistant P. aeruginosa
Among 18 MDR P. aeruginosa, 17 (94.4%) isolates were MexB positive (Fig. 4).
Fig. 4.
PCR amplification of MexB gene in MDR P. aeruginosa
Lane L1: DNA size marker (100–1000 bp); Lane 2: positive control; Lane 3/4/5: MexB positive; Lane 6: negative control.
Discussion
In this study, a total of 36 P. aeruginosa were isolated and identified from various clinical specimens. 50% of them were found to be MDR and 33.3% were MBL-producer. Among MDR isolates 16.7%, 11.1% and 94.4% of them were found to be harbouring blaNDM−1,mcr-1 and MexB genes respectively.
According to our study, prevalence rate of P. aeruginosa was found to be 4.6%. Variable prevalence rate of P. aeruginosa has been reported from previous studies done in Nepal that ranges from 2.2 to 17.05% [21–23]. Such variations in result might be due to different factors such as; differences in samples, different microbiological methodologies used and variation in geographical location [24]. Furthermore, in our study, highest number of P. aeruginosa were isolated from respiratory samples followed by blood. This result was found similar to the findings of previous studies conducted in Nepal [25, 26]. Therefore, our findings infers that P. aeruginosa is one of the predominant organism to cause respiratory tract infections. P. aeruginosa are developing resistance to different anti-pseudomonal drugs via various mechanisms that is resulting them to develop into most dangerous and dreaded bug [22, 27]. In our study, half of the total isolates were found to be multidrug resistant. Such high rates of MDR P. aeruginosa were also reported in previous studies from Nepal that ranges from 50 to 55.5% [25, 27].
Although carbapenem are considered as a drug of choice to treat P. aeruginosa infections, the emergence of carbapenem resistance significantly decreases its usefulness [8]. In our study, 33.3% of P. aeruginosa isolates were found to be MBL producer. This finding was found similar to the previous study conducted in Nepal [28]. However, some studies in other countries have recorded various percentages of MBL-producing P. aeruginosa such as 38.3% in Brazil, 47.3% in Taiwan, 62% in Greece, 53.4% in Italy, 69.8% in India and 68.7% in Egypt [29–32]. Furthermore, it has also been found that among 18 MDR P. aeruginosa, 12 isolates were MBL producers and their association was statistically significant (p < 0.001).
Among MBL types, detection of blaNDM−1 producer is alarming to clinical settings because presence of blaNDM−1 increases fear of diseases in future not to be cured by antibiotics [9]. In our study, we found that among MBL positive isolates, 25% of them carried blaNDM−1 gene. This result was found higher than the previous study conducted in Nepal [7]. Therefore, our result infers that prevalence of blaNDM−1 harbouring P. aeruginosa is in increasing trend in Nepal. So, periodic detection of carbapenem resistant isolates is necessary in order to implement new antibiotic treatment policies. Furthermore, in our study, it has been found that, these blaNDM−1 positive P. aeruginosa isolates were from the patients of intensive care unit (ICU) from tracheal swab, urine and pus sample and were resistant to all antibiotics tested except colistin. Therefore, this outcome suggests that colistin should be kept as the reserve drug to treat MDR/XDR P. aeruginosa. In addition, as blaNDM−1 positive P. aeruginosa were detected from ICU patients, treatment of them should be done separately because blaNDM−1 is known as rapidly spreading gene that can spread swiftly [7]. Further, the detail clinical characteristics of the three patients harbouring blaNDM−1 positive P. aeruginosa are depicted in Table 3.
Colistin is an oldest antibiotic that has been re-included in the list of useful antibiotics as a ˈreserve drugˈ to treat P. aeruginosa infection. However, resistance to colistin is also increasing recently [5]. In our study, 5.6% of isolates were found to be resistant to colistin with MIC value of 8 µg/ml. This finding differs from those reported from Pakistan [2]. Furthermore, it has been found that all colistin resistant isolates were from ICU patients and were mcr-1 positive. Therefore, our finding indicates that colistin resistant mcr-1gene is spreading across the world which is a global challenge for therapeutic option to treat emerging pathogens in future.
To our knowledge, there exists no report on emergence of plasmid mediated mcr-1 in P. aeruginosa in Nepal. Though reports of mcr-1 in P. aeruginosa in Nepal are not reported till the date, knowledge of its prevalence is important because P. aeruginosa is a ubiquitous organism with high colonization capacity and ability to survive for a long period of time in the hospital settings. In this study, we found that the mcr-1 harbouring isolates were from patients admitted to ICU ward and were resistant to all available antibiotics tested. Therefore, early detection and isolation of patients harbouring superbugs should be done to prevent its further spread.
Multidrug resistance (MDR) pumps play an important role in the antibiotic resistance of P. aeruginosa. MexAB-OprM is the most important efflux pump, overexpression of it plays a significant role in development of MDR strains [33]. To our knowledge, there is no previous report of detection of MexB gene in P. aeruginosa in Nepal. In our study, among MDR P. aeruginosa isolates, 94.4% of them were found to be harbouring MexB gene. This finding is in accordance with the previous study [34]. Detection of MexB in almost all MDR isolates infers that overexpression of MexAB efflux pump might be helping isolates to develop into MDR by pumping antibiotics outside of the cell. Therefore, MexB is also an important antimicrobial resistant biomarker that might help to trace MDR isolates.
Limitations of the study
This study was unable to detect other resistance mechanisms that might also helping P. aeruginosa develop into MDR due to limited resources. Also, this study was conducted for a limited time period on the patients of a single hospital which does not provide the overall scenario of antibiotic resistance of Nepal.
Conclusion
To the best of our knowledge, this study is first to report about the presence of mcr-1 and MexB genes in P. aeruginosa isolates in context of Nepal. Furthermore, detection of blaNDM−1 and mcr-1 in a highly mobile genetic element is a major highlight of our study because of its global threat to antimicrobial therapy that is leading them to evolve into deadest pathogen ‘Superbug’. Therefore, continuous screening and monitoring of phenotypic as well as genotypic phenomenon of resistance in P. aeruginosa are necessary to trace such superbugs. Furthermore, timely control of these resistant pathogens could help to prevent further spread.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We express our sincere gratitude to all the faculties and laboratory assistants of Central Department of Microbiology, Tribhuvan University, Kathmandu, Nepal and Upendra Devkota Memorial National Institute of Neurological and Allied Sciences, Nepal. We are very thankful to University Grants Commission, Nepal for providing financial support for the research work.
Authors’ contributions
S.S. conceived the idea and S.S., M.R.B. and B.M. designed the study. S.S., M.R.B., B.M. and M.D.D. reviewed the literature, extracted data, performed data analysis and drafted the manuscript. M.R.B. supervised the overall data analysis and writing. All the authors read and approved the final manuscript.
Funding
This study was financially supported by University Grants Commission (UGC Master’s thesis support grants MRS 76/77-S&T-31) Bhaktapur, Nepal. The funders had no role in study design, data collection and interpretation or the decision to submit the work for publication.
Data Availability
The data used to support the findings are available from the corresponding author upon request.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by Institutional Review Committee of Upendra Devkota Memorial National Institute of Neurological and Allied Sciences (UDM-NINAS), Kathmandu, Nepal (Ref. No.: 117/2021).We confirmed that the study was performed in accordance with the 1964 declaration of HELSINKI and later amendments as well as Nepal Health Research Council regulations and guidelines. Written informed consent was obtained from the patients before collection of specimens and data. Participating patients were informed that they can withdraw their participation at any time. The data were kept confidential.
Consent for publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Juan C, Pena C, Oliver A. Host and pathogen biomarkers for severe Pseudomonas aeruginosa infections. J Infect Dis. 2017;215(S1):44–51. doi: 10.1093/infdis/jiw299. [DOI] [PubMed] [Google Scholar]
- 2.Hameed F, Khan MA, Muhammad H, Sarwar T, Bilal H, Rehman TU. Plasmid mediated mcr-1 gene in Acinetobacter baumanii and Pseudomonas aeruginosa: first report from Pakistan. J Brazilian Soc Trop Med. 2019;52:1–6. doi: 10.1590/0037-8682-0237-2019. [DOI] [PubMed] [Google Scholar]
- 3.Pragasam AK, Raghanivedha M, Anandan S, Veeraraghavan B. Characterization of Pseudomonas aeruginosa with discrepant carbapenem susceptibility profile. Ann Clin Microbiol Antimicrob. 2016;15(12):1–4. doi: 10.1186/s12941-016-0127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ansari M, Aryal SC, Rai G, Rai KR, Pyakurel S, Bhandari B, Sah AK, Rai SK. Prevalence of multidrug-resistance and blaVIM and blaIMP genes among gram-negative clinical isolatesin tertiary care hospital, Kathmandu, Nepal. Iran J Microbiol. 2020;13(3):303–311PMC8416584. doi: 10.18502/ijm.v13i3.6392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.EI-Gawad MA, Ahmed EI-S, Zhong L-L, Shen C, Yang Y, Doi Y, Tian GB. Colistin and its role in the era of antibiotic resistance:an extended review (2006–2019) Emerg Microbes Infections. 2020;9:868–85. doi: 10.1080/22221751.2020.1754133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Devkota SP, Poudel A. Colistin resistance among Gram-negative isolates in Nepal: a review. J Biomedical Sci. 2020;7(1):33–9. doi: 10.3126/jbs.v7i1.29851. [DOI] [Google Scholar]
- 7.Acharya M, Joshi PR, Thapa K, Aryal R, Kakshapati T, Sharma S. Detection of metallo-β-lactamases-encoding genes among clinical isolates of Pseudomonas aeruginosa in a tertiary care hospital. Kathmandu Nepal. 2017;10:1–5. doi: 10.1186/s13104-017-3068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shahin M, Ahmadi A. Molecular characterization of NDM-1-producing Pseudomonas aeruginosa isolates from hospitalized patients in Iran. Ann Clin Microbiol Antimicrob. 2021;20:1–10. doi: 10.1186/s12941-021-00482-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zafer MM, Amin M, Mahallawy HE, Ashour MS, Agamy MA. First report of NDM-1 producing Pseudomonas aeruginosa in Egypt. Int J Infect Dis. 2014;29:80–1. doi: 10.1016/j.ijid.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Lin KY, Lauderdale TL, Wang JT, Chang SC. Carbapenem-resistant Pseudomonas aeruginosa in Taiwan: prevalence, risk factors, and impact on outcome of infections. J Microbiol Immunol Infect. 2016;49(1):52–9. doi: 10.1016/j.jmii.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Dortet L, Poirel L. Rapid identification of carbapenemase types in Enterobacteriaceae and Pseudomonas spp by using a biochemical test. Antimicrob Agents Chemother. 2012;56(12):6437–70. doi: 10.1128/AAC.01395-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gautam S, Bhattarai NR, Rai K, Poudyal A. B. Khanal. Detection of blaNDM-1 encoding imipenemase among the imipenem-resistant gram-negative bacilli isolated from various clinical samples at a tertiary care hospital of eastern Nepal: a descriptive cross-sectional study. Int J Microbiol. 2020:1–5. 10.1155/2020/8861204 [DOI] [PMC free article] [PubMed]
- 13.Cheesebrough M. District laboratory practice in tropical countries. Part 2.2nd Edition, Cambridge University Press, New York. 2006: 30–71. Available on: https://www.medbox.org/preview/5255d6e1-05d4-41a9-beb2-02b60e695ecc/doc.pdf
- 14.Clinical and Laboratory Standard Institute (CLSI). M100 Performance Standards for Antimicrobial Susceptibility Testing 30th ed.; An Informational Supplement; CLSI: Wayne, PA, USA 2020. Available from: https://www.nih.org.pk/wp-content/uploads/2021/02/CLSI-2020.pdf
- 15.Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Gisake CG, Harbarth S, Hindler JF, Kahimeter G, Oisson-Liljequist B, Paterson DL, Rice LB, Strelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microb Infect. 2011;18:268–81. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 16.European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and Zone diameters. Version 6.0, valid from 2016-01-01. https://www.researchgate.net/file.PostFileLoader.html?id=570cbcccdc332dfb4564237d&assetKey=AS%3A349977533534208%401460452556625
- 17.Green MR, Sambrook J. Preparation of plasmid DNA by alkaline lysis with sodium dodecyl sulphate:minipreps. Cold Spring Harbor Laboratory Press. 2016;911–7. 10.1101/pdb.prot093344 [DOI] [PubMed]
- 18.Zainol Abidin NZ, Sulong A, Alfizah H, Muttaqilla NAS, Ding CH. Molecular detection of the New Delhi metallo-β-lactamase-1 gene in Enterobacteriaceae isolates in a tertiary medical center. Malaysian J Pathol. 2015;37:227–32. [PubMed] [Google Scholar]
- 19.Liu YY, Wang Y, Walsh TR, Yi L, Zhang R, James S. Emergence of plasmid-mediated colistin resistance mechanism mcr-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16(2):1–8. doi: 10.1016/s1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- 20.Abbas HA, Amira EGM, Hend AK. Phenotypic and genotypic detection of antibiotic resistance of Pseudomonas aeruginosa isolated from urinary tract infections. Afr Health Sci. 2018;18(1):11–21. doi: 10.4314/ahs.v18i1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhandari S, Banjara MR, Lekhak B, Bhatta DR, Regmi SR. Multi-drug and pan-drug resistant Pseudomonas aeruginosa: a challenge in post-antibiotic era. Nepal J Sci Technol. 2012;13(2):197–202. doi: 10.3126/njst.v13i2.7736. [DOI] [Google Scholar]
- 22.Chander A, Shahid RM. Antimicrobial susceptibility patterns of Pseudomonas aeruginosa clinical isolates at a tertiary care hospital in Kathmandu, Nepal. Asian J Pharm Clin Res. 2018;6:235–8. doi: 10.3126/jist.v25i2.33734. [DOI] [Google Scholar]
- 23.Gyawali R, Khadka RB, Shrestha B, Manandhar S. Antimicrobial susceptibility patterns of Pseudomonas spp isolated from various clinical samples at a tertiary care hospital. J Inst Sci Technol. 2020;25(2):49–54. doi: 10.3126/jist.v25i2.33734. [DOI] [Google Scholar]
- 24.Besien JV, Uvin P, Abeele AMV, Merckx L. Prevalence, risk factors and clinical relevance of fluoroquinolones-resistant organisms in rectal cultures: Should we target antibiotic prophylaxis prior to prostate biopsy? AdvUrol. 2016; 2016:1–7. 10.1155/2016/5392107 [DOI] [PMC free article] [PubMed]
- 25.Pokharel K, Fawadi BR, Bhatt CP, Gupte S. Prevalence of Pseudomonasaeruginosa and its antibiotic sensitivity pattern. J Nepal Health Res Counc. 2019;17(1):109–13. doi: 10.33314/jnhrc.1877. [DOI] [PubMed] [Google Scholar]
- 26.Ansari S, Dhital R, Shrestha S, Thapa S, Puri R, Chaudhary N, Khatiwada S, Gautam R. Growing menace of antibacterial resistance in clinical isolates of Pseudomonas aeruginosa in Nepal: An insight of beta-lactamase production. BioMed Research International. 2016; 2016: 1–9. 10.1155/2016/6437208 [DOI] [PMC free article] [PubMed]
- 27.Mahaseth SN, Chaurasia L, Jha B, Sanjana RK. Prevalence and antimicrobial susceptibility pattern of Pseudomonas aeruginosa isolated from various clinical samples in a tertiary care hospital. JMCJMS. 2020;8(2):11–7. doi: 10.3126/jmcjms.v8i2.33972. [DOI] [Google Scholar]
- 28.Ansari M. Evaluation of community pharmacies regarding dispensing practices of antibiotics in two districts of central Nepal. PLoS ONE. 2017;12:1–9. doi: 10.1371/journal.pone.0183907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Akya A, Salimi A, Nomanpour B, Ahmadi K. Prevalence and clonal dissemination of metallo-β-lactamase producing Pseudomonas aeruginosa in Kermanshah. Jundishapur J Microbiol. 2015;8(7):1–5. doi: 10.5812/jjm.20980v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saderi H, Owlia P. Detection of multidrug resistant (MDR) and extremely drug resistant (XDR) Pseudomonas aeruginosa isolated from patients in Tehran, Iran. Iran J Pathol. 2015;10(4):265–71. [PMC free article] [PubMed] [Google Scholar]
- 31.Gupta V, Sidhu S, Chander J. Metallo-β-lactamase producing non-fermentative gram-negative bacteria: an increasing clinical threat among hospitalized patients. Asian Pac J Trop Med. 2012;5(9):718–521. doi: 10.1016/s1995-7645(12)60113-8. [DOI] [PubMed] [Google Scholar]
- 32.Zafer MM, Al-Agamy MH, EI-Mahallawy HA, Amin MA, Ashour SED. Dissemination of VIM producing Pseudomonas aeruginosa ST233 at tertiary care hospitals in Egypt. BMC Infect Dis. 2015;15(122):122–9. doi: 10.1186/s12879-015-0861-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kishk RM, Abdalla MO, Hashish AA, Nemr NA, Nahhas NEI, Alkahtani S, Abdel-Daim MM, Kishk SM. MDPI. 2020;9(471):1–13. doi: 10.3390/pathogens9060471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Grawi IGA, Absali AKA, Kareem NH, Belal SA. Occurrence of MexAB-OprM efflux pump operon on septicemicPseudomonas aeruginosa chromosome. The Iraqi Postgraduate Medical Journal. 2012; 11(1): 97–102. Available on: https://iraqjournals.com/article_30185_c861bd2539c6586a5c4885d416f0fd27.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to support the findings are available from the corresponding author upon request.