PEDIATRIC SLEEP HEALTH DISPARITIES
The National Institute of Minority Health and Health Disparities (NIMHD) defines a health disparity as a health difference that adversely affects disadvantaged populations on one or more health outcomes.1 Health disparity populations include individuals from racially and ethnically minoritized backgrounds, those of lower socioeconomic status (SES) backgrounds, gender minorities, rural populations, and those with identities at the intersection of these and other categories. This article reviews disparities in pediatric sleep health and sleep disorders and potential determinants of these disparities. Much of this research focuses on disparities by race and ethnicity, which are sociopolitical constructs.2,3 Observed disparities do not result from biological differences by race and ethnicity but rather are a manifestation of historical and ongoing racism, discrimination, and oppression that produce differential exposure to adverse social and environmental factors. Accordingly, we apply a socioecological framework4 to examine interacting social and environmental factors that may contribute to pediatric sleep health disparities and their related outcomes (Fig. 1). These factors exist at multiple levels of the social ecology, including the individual child and family levels, the educational and health-care systems levels, and the broader neighborhood/community level and sociocultural context.
Fig. 1.
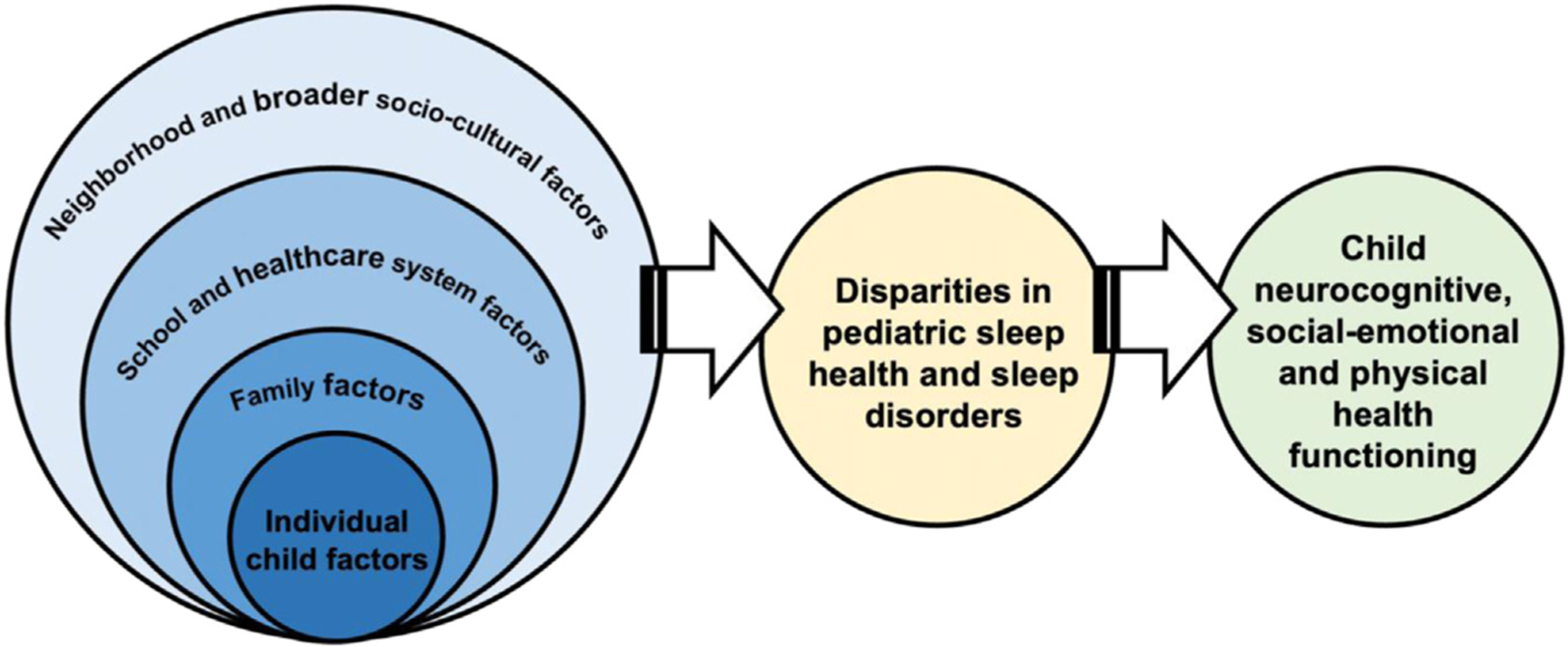
Socioecological framework applied to determinants and consequences of pediatric sleep health disparities.
As defined by Buysse5 and expanded for pediatrics,6 sleep health is a multidimensional construct that encompasses sleep patterns (eg, duration, continuity/awakenings), perceived sleep quality, alertness, and sleep-related behaviors (eg, bedtime routines, electronics usage). Sleep disorders in this review include behavioral concerns, such as insomnia and related symptoms (eg, broad caregiver-perceived or child/adolescentperceived sleep problems, difficulty falling/returning to sleep) and medically based concerns.7 Sleep disorder disparities research is mostly limited to insomnia and sleep disordered breathing (SDB). We review racial, ethnic, and socioeconomic disparities in sleep health and these sleep disorders by age, from early childhood (ages 0–5 years) through middle childhood (6–11 years) and adolescence (12–18 years). We then discuss socioecological contributors to these disparities and future research directions.
DISPARITIES IN SLEEP HEALTH
Early Childhood
Research primarily conducted in the United States (US) has demonstrated that racial, ethnic, and socioeconomic sleep health disparities begin in early development. Most studies have examined sleep duration, continuity (awakenings), and behaviors, particularly bedtime routines. Studies of infants and toddlers show that those of African American/Black (hereafter, “Black”), Hispanic/Latinx (hereafter, “Latinx”), and Asian backgrounds tend to obtain less sleep than their non-Hispanic/Latinx White (hereafter, “White”) counterparts.8–13 A study following 194 infants from ages 1 to 6 months found that Latinx infants’ nighttime sleep duration was approximately 30 minutes less at 1 month and an hour less at 6 months compared with White infants.9 These racial differences in nighttime sleep duration have persisted during the coronavirus pandemic.10 A systematic review of sleep in 2 to 5 year olds found that White children had longer nighttime sleep duration and napped less frequently than Black and Latinx children,14 suggesting that disparities in nighttime sleep duration could be due to differences in daytime sleep. Nonetheless, longitudinal research has demonstrated that despite differences in napping, total (24 hours) sleep duration was shorter in Black, Latinx, and Asian infants from birth to age 2, by approximately 24 minutes, 49 minutes, and 57 fewer minutes of sleep per day, respectively, compared with White infants.11
In some studies, when adjusting for family SES, racial, and ethnic differences in sleep duration attenuate for Latinx and Black children but remain or become stronger for Asian children.12,15 A study of 9-month-olds modeled cumulative exposure to multiple family SES variables, such as maternal education and family poverty, and found that greater cumulative risks were associated with a long sleep onset latency and/or frequent and long night awakenings.16 There is also evidence that young children living in lower-SES neighborhoods, typically indexed according to US Census data, experience later bedtimes, a long sleep onset latency, and short sleep duration compared with those in higher SES neighborhoods, although this research does not always include both family and neighborhood SES.17,18 A study of 80 Black infants found that after controlling for family SES, infants in lower-SES neighborhoods had more night awakenings, suggesting unique neighborhood-level links with sleep.19
Most early childhood sleep health research has focused on bedtime routines, with a systematic review showing that consistent bedtime routines are less prevalent among Latinx and Black children compared with White children.14 In addition to this finding, a study of 3217 3-year-olds found that children with a mother who had less education, those with a lower family income, and those in larger households were also less likely to have a bedtime routine.20 In another study, greater cumulative risk, indexed by family and neighborhood SES as well as caregiver depressive symptoms, was associated with greater likelihood of poor sleep health, including an inconsistent bedtime routine, insufficient sleep duration, and caffeine consumption.21
Middle Childhood
A systematic review of racial and ethnic sleep health disparities in children aged 6 to 19 years found that across ages, White youth consistently obtain more sleep than Black and Latinx youth, with inconclusive results for Asian youth.22 A study of 1293 youth aged 6 to 12 years found that Asian, Black, and Latinx children slept an average of 23, 17, and 14 minutes less than White children.23 A previously discussed longitudinal study found that at every time point from birth to age 7, Black, Latinx, and Asian children were more likely to obtain insufficient sleep compared with White children, although including SES in analyses attenuated differences for Black and Latinx children.12
Compared with early childhood research, fewer studies of socioeconomic sleep health disparities have been conducted with school-aged children. In a study of socioeconomic position (SEP), objective SEP (family income) was related to self-reported child sleep duration, whereas subjective SEP was related to daytime sleepiness and caregiver-reported sleep duration but only in children aged 8 to 13 years but not adolescents.24 In another study, children who grew up in neighborhoods with historically high poverty were more likely to exhibit insufficient sleep duration.25 A study of third-grade and fourth-grade children examined associations among multiple SES indicators and actigraphic sleep, and moderation by race and ethnicity.26 Poor caregiver-perceived economic well-being was linked to short actigraphy-derived sleep minutes and variable sleep onset, while children attending impoverished schools had a short sleep duration. Lower maternal education was linked to low sleep efficiency in Black but not White children, underscoring the importance of examining race, ethnicity, and multiple SES indicators.
Adolescence
As in research on school-aged children, most adolescent sleep health disparities studies have focused on sleep duration. In a systematic review, Black youth obtained less sleep than White and Latinx youth but findings for Asian youth were inconclusive.22 A study of 1543 adolescents found that Black and Latinx youth reported shorter sleep duration than both White and Asian youth.27 The same study found race by gender interactions, with Latinx men obtaining less sleep than White and Asian men, and Black women obtaining less sleep than White women. Another study found that Black adolescents obtained approximately 35 minutes less sleep and more actigraphy-derived wake after sleep onset than both Latinx and Asian youth.28 Another study has shown short actigraphy-derived nighttime sleep duration29 and fragmented sleep30 in Black versus White adolescents, although in one study total 24-hour sleep duration did not differ by race.29
With regard to socioeconomic disparities, a study of adolescents found that those of lower SES backgrounds had a longer sleep onset, shorter duration, and greater weekday to weeknight variability compared with youth of higher-SES.31 In another study of multiple objective and subjective SES factors, objective SEP was related to adolescents’ perceived sleep disturbances, whereas subjective SEP was associated with poor self-reported sleep quality and short caregiver-reported child sleep duration.24 Lower SES may also exacerbate linkages between poor sleep health and adolescent functioning.32 Adjusting for race and ethnicity, shorter and less efficient actigraphy-derived sleep patterns in older adolescents were linked to worse cognitive and behavioral functioning but only among youth from lower SES backgrounds.32
BEHAVIORAL SLEEP DISPARITIES
Early Childhood
One of the few studies examining racial and ethnic differences in caregiver-perceived child sleep problems found that a higher proportion of White mothers of preschoolers reported concerns about their child’s difficulty falling asleep compared with Black but not Latina mothers.33 In another study, Black caregivers reported increased preschooler bedtime difficulties compared with White caregivers but there were no racial differences in the proportion of caregiver-reported overall child sleep problems.34 A study of sleep disorders diagnosed in primary care found that White infants and toddlers were more likely to receive any sleep disorder diagnosis, including insomnia, than those from Black or “other” racial and ethnic backgrounds.7 With regard to socioeconomic variation, research on 14,980 young children found that caregivers living in neighborhoods with the lowest SES, determined via a US Census-based index, were less likely to report a child sleep problem than those in higher SES neighborhoods, despite shorter caregiver-reported child sleep duration and longer sleep onset latencies among those in lower SES neighborhoods.18 Research also indicates that preschoolers exposed to greater cumulative risks, including lower family and neighborhood SES, were more likely to have caregiver-reported insomnia symptoms.21
Middle Childhood
Some school-based research suggests increased caregiver-reported child sleep problems in Latinx and Black children (94%) compared with a sample of predominantly White children (23%).35,36 A retrospective study found that White patients were more likely than Black patients to present to a pediatric sleep clinic with behavioral sleep problems, such as difficulty falling asleep, than with medically-based sleep concerns.37 A study of 271 children showed that having a lower SES background was associated with increased perceived sleep/wake problems and greater daytime sleepiness.38 Other studies have examined interrelations among sociodemographic factors, sleep, and child outcomes. For instance, Black children with sleep problems had worse cognitive and academic functioning compared with White children with sleep problems.39 In another study, Black children experiencing financial hardship exhibited a more variable sleep onset and more self-reported sleep problems compared with Black children without financial hardship, while no such pattern occurred in White children.26
Adolescence
Longitudinal research on a large cohort of youth with childhood insomnia symptoms (CISs) has demonstrated that symptoms tend to persist in Black and Latinx compared with White adolescents.40 CIS persistence rates were higher in White youth from lower SES backgrounds compared with White youth from higher SES backgrounds, whereas persistence rates were higher in racially and ethnically minoritized youth regardless of SES. Trouble sleeping in older adolescents, which may reflect insomnia or the circadian disturbances that are prevalent among teenagers, also varies by family and neighborhood SES. Among older adolescents, lower perceived neighborhood cohesion was associated with trouble sleeping, and this effect was stronger in adolescents with lower maternal education.41 One study found that Latinx adolescents reported fewer difficulties maintaining sleep than non-Latinx adolescents,42 whereas another study found no differences among Black, Latinx, and White adolescents in insomnia prevalence.43 In a study of multiple sociodemographic factors, adolescents identifying as “Mexican” (vs “Mexican-American”) and foreignborn youth were at lower risk for insomnia, and those from lower SES backgrounds were higher risk for insomnia.44
MEDICAL SLEEP DISPARITIES
Early Childhood
Few studies have examined early childhood disparities in medical sleep disorders. Research is generally limited to SDB, a spectrum of breathing difficulties during sleep from mild snoring to severe obstructive sleep apnea (OSA).45,46 One study found that Black infants and toddlers (25%) were more likely to exhibit habitual snoring (≥ nights/wk) than White children (15%).47 In another study, Black and Latinx preschoolers were more than twice as likely than White children to have SDB symptoms.48 A Canadian study found that children aged 2 to 8 years with OSA were more likely to reside in more densely populated neighborhoods with lower average rates of family income and more single-parent households.49
Middle Childhood and Adolescence
SDB affects approximately 10% to 17% of children, with 1% to 3% experiencing OSA.50,51 Black youth are 4 to 6 times more likely to experience SDB than White youth,46,52 with some evidence of increased OSA severity on polysomnogram in Black compared with White children.53 Children from lower-SES families and neighborhoods are also more likely to experience SDB than those living in higher SES contexts.54–56 Disparities also exist in SDB treatment, likely due to differential access to and contact with the health-care system. Several studies indicate that OSA treatment via adenotonsillectomy is less prevalent in Black and Latinx compared with White youth.54,57–59 A recent study found that Black and Latinx youth with Medicaid insurance were less likely to receive SDB surgical treatment compared with White youth, who also had shorter wait times for surgery.60 Some research suggests that adenotonsillectomy for OSA may not improve OSA-related behavioral symptoms as much in Black youth compared with those of White and other racial and ethnic backgrounds.59 Studies using insurance as a proxy for SES have additionally found that compared with those with private insurance, publicly insured youth tend to have lower adenotonsillectomy rates and greater SDB treatment delays, both in initial polysomnography and surgeries.57,61
MULTILEVEL DETERMINANTS OF PEDIATRIC SLEEP DISPARITIES
Bronfenbrenner’s socioecological framework4 (see Fig. 1) has been applied to understand contributors to pediatric sleep health6 and to sleep health disparities across the life span62 and in pediatric SDB.63 The factors outlined below are not an exhaustive list of contributors. Future research is needed to identify how these, and other modifiable factors, can be leveraged to promote sleep health equity. Given its multilevel nature, racism (eg, systemic, structural, institutional; personally mediated; and internalized)64–67 and discrimination are included at each socioecological level.
Child Level
Child characteristics such as prematurity, respiratory issues, and obesity are linked with variation in sleep patterns and SDB and may contribute to disparities.46,52 Early childhood temperament may also influence sleep patterns as a function of caregiver characteristics, such as mood or parenting style.68,69 For example, compared with infants with “easy” temperaments, those with “difficult” temperaments exhibit poor sleep outcomes, including frequent night awakenings and short sleep duration.69 A longitudinal study following mother–infant dyads from birth to age 6 months found that infant temperament moderated maternal emotional availability at bedtime and infant sleep duration, with high-surgency infants exhibiting greater increases in sleep duration in the context of higher maternal bedtime emotional availability.70 As parenting behaviors vary crossculturally, more research is needed on these linkages in racially and ethnically minoritized families and in other countries/regions.
Personally mediated and/or internalized racism and discrimination are other child-level factors linked with poor sleep, primarily in adolescents.28,71–73 Daily discrimination was related to increased same-night sleep disturbances and next-day sleepiness in Asian, Black, and Latinx teens,28 which could contribute to racial and ethnic sleep health disparities. A study of college students also found that discrimination was related to poor sleep, and that this association was stronger among students who also reported higher levels of internalized racism.71
Family Level
Sleep health literacy and beliefs are family factors that also may contribute to sleep health disparities. Lower sleep health literacy, which is correlated with SES, has been associated with poor child sleep health.74,75 Research also shows that the negative sleep-related impacts of having a television in the bedroom are more pronounced among racially and ethnically minoritized children compared with their White peers.76 Qualitative research indicates that limited sleep health knowledge may contribute to poor sleep in racially and ethnically minoritized adolescents.77,78 One of these studies was conducted with American Indian/Alaska Native (AI/AN) teens, who described the importance of family cohesion in helping to maintain stable sleep environments and, in turn, optimal sleep health.77
The sleep environment, which includes sleep arrangements (ie, bed-sharing and room-sharing) as well as light, noise, and temperature, among other factors,79 likely contributes to sleep health disparities. Families of lower-SES may need to bed-share and/or room-share due to limited resources, whereas other families may practice bed-sharing intentionally, as part of their cultural practices and/or preferences, or in response to a child sleep problem.80,81 Generally, African and Asian countries/regions exhibit higher rates of bed-sharing compared with European and American countries/regions.80,82 In one US study of families from low-SES backgrounds, Black and Latinx families were more likely to bed-share than White families.83 The effects of sleep arrangements on child sleep are mixed, and likely depend on the context in which families are bed-sharing/room-sharing. Understanding this context is crucial for identifying how sleep arrangements and aspects of the sleep environment can be enhanced to promote sleep health equity, particularly among families experiencing noisy, crowded, and/or transitional sleep environments.
Qualitative research has also revealed that caregivers cite family work/school schedules, household responsibilities, and other family members’ sleep schedules as barriers to child and family sleep health.84–86 Among Black adolescents, more household chaos was associated with greater disruptions to youth sleep by other household members’ behaviors, including electronics use and evening social visits.87 Family irregularity has been longitudinally associated with more reported child sleep problems, short sleep duration, and long sleep onset.88 Household chaos and family relationships are associated with child sleep in several other studies.89 For instance, there is evidence that household chaos mediates associations between positive parenting and sleep health, and between family resources and child sleep duration.90,91 One study found that better parent–child relationships were associated with decreased insomnia risk, particularly among Latinx adolescents compared with White and Black youth.92
Family members’ experiences of racism and discrimination are also linked to child sleep. Caregiver experiences of racial discrimination, for example, are associated with short early childhood sleep duration.93 Caregivers’ experiences of racism may also impact factors associated with child sleep, including caregiver mood,64–66– parenting,67 and caregivers’ own sleep.94 A study of gendered racial discrimination found that higher levels of mothers’ gendered racial stress was directly associated with poor child sleep, although racial/ethnic discrimination was not.95 This finding highlights the importance of intersectionality in research on the role of racism and discrimination in sleep health disparities.
School/Health-Care Level
Although racism at the school and health-care system levels has not been studied in relation to child sleep, biases in these systems likely contribute to disparities in sleep-related outcomes and treatments. Research shows that teachers and health-care providers hold implicit pro-White/anti-Black biases, which can affect teacher–student and provider–patient interactions and result in differential care.96–99 A systematic review found that health-care providers hold implicit racial and ethnic biases, and that these biases were associated with disparities in treatment recommendations and patient–provider communication, expectations, and empathy.97 Research also suggests that children with public insurance are less likely to be offered an appointment than privately insured children, which may reflect socioeconomic bias.100 More research on how racism and discrimination in school and health-care systems can contribute to disparities in child sleep and related functional outcomes is needed. In addition, given that delaying school start times can benefit adolescent sleep,101 more research is needed on how school schedules could contribute to or buffer against sleep health disparities.
Neighborhood Level
Both physical (eg, air quality, green space) and social (eg, safety) characteristics of neighborhoods impact child sleep, including sleep patterns, insomnia symptoms, and SDB.17 For example, environmental allergens and toxins may lead to increased SDB symptoms via upper airway inflammation.55,56 As previously mentioned, environmental factors such as light, noise, and community violence may contribute to child and family sleep disruptions.26,38,79 Although research examining neighborhood factors is growing, mechanistic studies of modifiable determinants are needed.
SUMMARY AND FUTURE DIRECTIONS
The research in this review suggests that there are well-established racial, ethnic, and socioeconomic sleep health disparities from early childhood through adolescence. At the same time, there are notable research gaps. Most research to date has examined Black–White racial disparities, with less research on other racial and ethnic groups. Only a handful of studies have examined sleep in other NIMHD-designated pediatric health disparity populations, such as gender minorities.102 Even fewer studies have applied an intersectional framework,103 which is critical for understanding the causes and influences of sleep health disparities among those with multiple marginalized identities. Research is also needed on dimensions of sleep health beyond duration, timing, and sleep behaviors such as bedtime routines. Future research should also examine contributors to disparities in the prevalence and outcomes of other behavioral and medical sleep disorders.
As described in the recent NIH workshop report on sleep health disparities, there is a need for mechanistic studies, particularly regarding the role of racism and discrimination in these disparities.3 Interventions that are culturally responsive and address modifiable determinants at multiple socio-ecological levels are also urgently needed.3 The vast majority of pediatric sleep interventions have been tested with predominantly White families and/or those with higher educational levels.104 To avoid perpetuating research-to-practice gaps, future research should focus on adapting and evaluating evidence-based interventions in collaboration with health disparity populations and in accessible care settings.105 Community-engaged research strategies, such as community-based participatory research,3,105 as well as qualitative and mixed methods, and racial and ethnic health equity principles106 should be incorporated in both interventional and mechanistic research seeking to address pediatric sleep health disparities.
KEY POINTS.
Cross-sectional and longitudinal research has established that there are disparities in pediatric sleep health and sleep disorders by race, ethnicity, and socioeconomic status from birth through adolescence.
Factors at multiple socioecological levels (ie, child, family, school, health-care system, neighborhood, and sociocultural), including historical and ongoing racism, discrimination, and oppression, contribute to these disparities.
Mechanistic research and studies using an intersectional lens to understand overlapping marginalized identities are needed to advance sleep health disparities research.
Interventions addressing multilevel socioecological determinants of disparities are needed to promote pediatric sleep health equity.
CLINICS CARE POINTS.
Clinicians should assess for and incorporate multilevel (ie, child, family, school, health-care system, neighborhood, and sociocultural) social and environmental factors when conducting pediatric sleep evaluation, case conceptualization, and treatment-planning.
Focusing on modifiable social and environmental determinants of sleep health disparities can guide equitable sleep health promotion efforts.
Clinical training and practice in pediatric sleep should include approaches to reduce implicit and explicit bias and to enhance equitable, culturally humble, and family-centered care.
DECLARATION OF INTERESTS
Dr A.A. Williamson is funded by grants from the National Child Health and Human Development (K23HD094905) and the National Heart, Lung, and Blood Institute (R01HL152454). The authors have no other funding sources or conflicts of interest to disclose.
REFERENCES
- 1.Minority health, health disparities. Definitions and parameters. NIMHD. Available at: https://www.nimhd.nih.gov/about/strategic-plan/nih-strategicplan-definitions-and-parameters.html. Accessed March 25, 2022. [Google Scholar]
- 2.Boyd RW, Lindo EG, Weeks LD, et al. On racism: a new standard for publishing on racial health inequities. Bethesda, MD: E-publication; 2020. 10.1377/forefront.20200630.939347. [DOI] [Google Scholar]
- 3.Jackson CL, Walker JR, Brown MK, et al. A workshop report on the causes and consequences of sleep health disparities. Sleep 2020; 43(8):zsaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bronfenbrenner U Ecological systems theory. In: Vasta, editor. Six theories of child development: revised formulations and current issues. London, England: Jessica Kingsley Publishers; 1992. p. 187–249. [Google Scholar]
- 5.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep 2014;37(1):9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meltzer LJ, Williamson AA, Mindell JA. Pediatric sleep health: it matters, and so does how we define it. Sleep Med Rev 2021;57:101425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meltzer LJ, Johnson C, Crosette J, et al. Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics 2011;125:e1410–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ash T, Taveras EM, Redline S, et al. Contextual and parenting factors contribute to shorter sleep among hispanic/latinx compared to non-hispanic white infants. Ann Behav Med 2021;55(5):424–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ash T, Davison KK, Haneuse S, et al. Emergence of racial/ethnic differences in infant sleep duration in the first six months of life. Sleep Med X 2019;1: 100003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lucchini M, Kyle M, Pini N, et al. Racial/ethnic disparities in sleep in mothers and infants during the Covid-19 pandemic. Sleep Health 2022;8(5): 429–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nevarez MD, Rifas-Shiman SL, Kleinman KP, et al. Associations of early life risk factors with infant sleep duration. Acad Pediatr 2010;10(3):187–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peña MM, Rifas-Shiman SL, Gillman MW, et al. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep 2016;39(9):1653–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Z, Adamo KB, Ogden N, et al. Longitudinal correlates of sleep duration in young children. Sleep Med 2021;78:128–34. [DOI] [PubMed] [Google Scholar]
- 14.Smith JP, Hardy ST, Hale LE, et al. Racial disparities and sleep among preschool aged children: a systematic review. Sleep Health 2019;5(1):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu X, Quante M, Rueschman M, et al. Emergence of racial/ethnic and socioeconomic differences in objectively measured sleep–wake patterns in early infancy: results of the Rise & SHINE study. Sleep 2021;44(3):zsaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lobermeier M, Staples AD, Peterson C, et al. Cumulative risk, infant sleep, and infant social-emotional development. Infant Behav Dev 2022;67:101713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mayne SL, Mitchell JA, Virudachalam S, et al. Neighborhood environments and sleep among children and adolescents: a systematic review. Sleep Med Rev 2021;57:101465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williamson AA, Gould R, Leichman ES, et al. Socioeconomic disadvantage and sleep in early childhood: real-world data from a mobile health application. Sleep Health 2021;7(2):143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grimes M, Camerota M, Propper CB. Neighborhood deprivation predicts infant sleep quality. Sleep Health 2019;5(2):148–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hale L, Berger LM, LeBourgeois MK, et al. Social and demographic predictors of preschoolers’ bedtime routines. J Dev Behav Pediatr 2009; 30(5):394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williamson AA, Mindell JA. Cumulative sociodemographic risk factors and sleep outcomes in early childhood. Sleep 2020;43(3):zsz233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guglielmo D, Gazmararian JA, Chung J, et al. Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health 2018;4(1):68–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yip T, Cheon YM, Wang Y, et al. Sociodemographic and environmental factors associated with childhood sleep duration. Sleep Health 2020;6(6):767–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychol 2014; 33(3):301–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheehan C, Powers D, Margerison-Zilko C, et al. Historical neighborhood poverty trajectories and child sleep. Sleep Health 2018;4(2):127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Sheikh M, Bagley EJ, Keiley M, et al. Economic adversity and children’s sleep problems: multiple indicators and moderation of effects. Health Psychol 2013;32(8):849–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marczyk Organek KD, Taylor DJ, Petrie T, et al. Adolescent sleep disparities: sex and racial/ethnic differences. Sleep Health 2015;1(1):36–9. [DOI] [PubMed] [Google Scholar]
- 28.Yip T, Cheon YM, Wang Y, et al. Racial disparities in sleep: associations with discrimination among ethnic/racial minority adolescents. Child Dev 2020;91(3):914–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.James S, Chang AM, Buxton OM, et al. Disparities in adolescent sleep health by sex and ethnoracial group. SSM Popul Health 2020;11:100581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matthews KA, Hall M, Dahl RE. Sleep in healthy black and white adolescents. Pediatrics 2014; 133(5):e1189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marco CA, Wolfson AR, Sparling M, et al. Family socioeconomic status and sleep patterns of young adolescents. Behav Sleep Med 2012;10(1):70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El-Sheikh M, Shimizu M, Philbrook LE, et al. Sleep and development in adolescence in the context of socioeconomic disadvantage. J Adolesc 2020; 83(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Milan S, Snow S, Belay S. The context of preschool children’s sleep: racial/ethnic differences in sleep locations, routines, and concerns. J Fam Psychol 2007;21(1):20–8. [DOI] [PubMed] [Google Scholar]
- 34.Patrick KE, Millet G, Mindell JA. Sleep differences by race in preschool children: the roles of parenting behaviors and socioeconomic status. Behav Sleep Med 2015;14(5):467–79. [DOI] [PubMed] [Google Scholar]
- 35.Owens JA, Spirito A, McGuinn M, et al. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr 2000;21(1):27–36. [DOI] [PubMed] [Google Scholar]
- 36.Sheares BJ, Kattan M, Leu CS, et al. Sleep problems in urban, minority, early-school-aged children more prevalent than previously recognized. Clin Pediatr 2013;52(4):302–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubens SL, Patrick KE, Williamson AA, et al. Individual and socio-demographic factors related to presenting problem and diagnostic impressions at a pediatric sleep clinic. Sleep Med 2016;25: 67–72. [DOI] [PubMed] [Google Scholar]
- 38.Bagley EJ, Kelly RJ, Buckhalt JA, et al. What keeps low-SES children from sleeping well: the role of presleep worries and sleep environment. Sleep Med 2015;16(4):496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.El-Sheikh M, Philbrook LE, Kelly RJ, et al. What does a good night’s sleep mean? Nonlinear relations between sleep and children’s cognitive functioning and mental health. Sleep 2019;42(6): zsz078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fernandez-Mendoza J, Bourchtein E, Calhoun S, et al. Natural history of insomnia symptoms in the transition from childhood to adolescence: population rates, health disparities, and risk factors. Sleep 2021;44(3):zsaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Troxel WM, Shih RA, Ewing B, et al. Examination of neighborhood disadvantage and sleep in a multiethnic cohort of adolescents. Health Place 2017; 45:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zapata Roblyer MI, Grzywacz J. Demographic and parenting correlates of adolescent sleep functioning. J Child Fam Stud 2015;24(11):3331–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roberts RE, Roberts CR, Chan W. Ethnic differences in symptoms of insomnia among adolescents. Sleep 2006;29(3):359–65. [DOI] [PubMed] [Google Scholar]
- 44.Roberts RE, Lee ES, Hemandez M, et al. Symptoms of insomnia among adolescents in the lower Rio Grande Valley of Texas. Sleep 2004;27(4): 751–60. [DOI] [PubMed] [Google Scholar]
- 45.Bixler EO, Vgontzas AN, Lin HM, et al. Sleep disordered breathing in children in a general population sample: prevalence and risk factors. Sleep 2009; 32(6):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rosen CL, Larkin EK, Kirchner HL, et al. Prevalence and risk factors for sleep-disordered breathing in 8- to 11-year-old children: association with race and prematurity. J Pediatr 2003;142(4):383–9. [DOI] [PubMed] [Google Scholar]
- 47.Montgomery-Downs HE, Gozal D. Sleep habits and risk factors for sleep-disordered breathing in infants and young toddlers in Louisville, Kentucky. Sleep Med 2006;7(3):211–9. [DOI] [PubMed] [Google Scholar]
- 48.Goldstein NA, Abramowitz T, Weedon J, et al. Racial/ethnic differences in the prevalence of snoring and sleep disordered breathing in young children. J Clin Sleep Med 2011;7(2):163–71. [PMC free article] [PubMed] [Google Scholar]
- 49.Brouillette RT, Horwood L, Constantin E, et al. Childhood sleep apnea and neighborhood disadvantage. J Pediatr 2011;158(5):789–95.e1. [DOI] [PubMed] [Google Scholar]
- 50.Archbold KH, Pituch KJ, Panahi P, et al. Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatr 2002;140(1): 97–102. [DOI] [PubMed] [Google Scholar]
- 51.Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012;130(3):576–84. [DOI] [PubMed] [Google Scholar]
- 52.Redline S, Tishler PV, Schluchter M, et al. Risk factors for sleep-disordered breathing in children: associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med 1999; 159(5):1527–32. [DOI] [PubMed] [Google Scholar]
- 53.Weinstock TG, Rosen CL, Marcus CL, et al. Predictors of obstructive sleep apnea severity in adenotonsillectomy candidates. Sleep 2014;37(2):261–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Boss EF, Smith DF, Ishman SL. Racial/ethnic and socioeconomic disparities in the diagnosis and treatment of sleep-disordered breathing in children. Int J Pediatr Otorhinolaryngol 2011;75(3): 299–307. [DOI] [PubMed] [Google Scholar]
- 55.Spilsbury JC, Storfer-Isser A, Kirchner HL, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr 2006; 149(3):342–7. [DOI] [PubMed] [Google Scholar]
- 56.Wang R, Dong Y, Weng J, et al. Associations among neighborhood, race, and sleep apnea severity in children. A six-city analysis. Ann Am Thorac Soc 2017;14(1):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cooper JN, Koppera S, Boss EF, et al. Differences in tonsillectomy utilization by race/ethnicity, type of health insurance, and rurality. Acad Pediatr 2021; 21(6):1031–6. [DOI] [PubMed] [Google Scholar]
- 58.Kum-Nji P, Mangrem CL, Wells PJ, et al. Black/white differential use of health services by young children in a rural Mississippi community. South Med J 2006;99(9):957–62. [DOI] [PubMed] [Google Scholar]
- 59.Marcus CL, Moore RH, Rosen CL, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med 2013;368(25):2366–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pecha PP, Chew M, Andrews AL. Racial and ethnic disparities in utilization of tonsillectomy among medicaid-insured children. J Pediatr 2021;233: 191–7.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Boss EF, Benke JR, Tunkel DE, et al. Public insurance and timing of polysomnography and surgical care for children with sleep-disordered breathing. JAMA Otolaryngol-Head Neck Surg 2015;141(2): 106–11. [DOI] [PubMed] [Google Scholar]
- 62.Billings ME, Cohen RT, Baldwin CM, et al. Disparities in sleep health and potential intervention models. Chest 2021;159(3):1232–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Williamson AA, Johnson TJ, Tapia IE. Health disparities in pediatric sleep-disordered breathing. Paediatr Respir Rev 2022;S1526–0542(22):00005–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One 2015;10(9):e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pieterse AL, Todd NR, Neville HA, et al. Perceived racism and mental health among Black American adults: a meta-analytic review. J Couns Psychol 2012;59(1):1–9. [DOI] [PubMed] [Google Scholar]
- 66.Trent M, Dooley DG, Dougé J, et al. The impact of racism on child and adolescent health. Pediatrics 2019;144(2):e20191765. [DOI] [PubMed] [Google Scholar]
- 67.Berry OO, Londoño Tobón A, Njoroge WFM. Social determinants of health: the impact of racism on early childhood mental health. Curr Psychiatry Rep 2021;23(5):23. [DOI] [PubMed] [Google Scholar]
- 68.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev 2010;14(2):89–96. [DOI] [PubMed] [Google Scholar]
- 69.Sadeh A, Anders TF. Infant sleep problems: origins, assessment, interventions. Infant Ment Health J 1993;14(1):17–34. [Google Scholar]
- 70.Jian N, Teti DM. Emotional availability at bedtime, infant temperament, and infant sleep development from one to six months. Sleep Med 2016;23:49–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fuller-Rowell TE, Nichols OI, Burrow AL, et al. Dayto-day fluctuations in experiences of discrimination: associations with sleep and the moderating role of internalized racism among African American college students. Cultur Divers Ethnic Minor Psychol 2021;27(1):107–17. [DOI] [PubMed] [Google Scholar]
- 72.Goosby BJ, Cheadle JE, Strong-Bak W, et al. Perceived discrimination and adolescent sleep in a community sample. RSF 2018;4(4):43–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Huynh VW, Gillen-O’Neel C. Discrimination and sleep: the protective role of school belonging. Youth Soc 2016;48(5):649–72. [Google Scholar]
- 74.Bathory E, Tomopoulos S, Rothman R, et al. Infant sleep and parent health literacy. Acad Pediatr 2016;16(6):550–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Owens JA, Jones C. Parental knowledge of healthy sleep in young children: results of a primary care clinic survey. J Dev Behav Pediatr 2011;32(6): 447–53. [DOI] [PubMed] [Google Scholar]
- 76.Cespedes EM, Gillman MW, Kleinman K, et al. Television viewing, bedroom television, and sleep duration from infancy to mid-childhood. Pediatrics 2014;133(5):e1163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Palimaru AI, Dong L, Brown RA, et al. Mental health, family functioning, and sleep in cultural context among American Indian/Alaska native urban youth: a mixed methods analysis. Soc Sci Med 2022;292:114582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Quante M, Khandpur N, Kontos EZ, et al. Let’s talk about sleep”: a qualitative examination of levers for promoting healthy sleep among sleep-deprived vulnerable adolescents. Sleep Med 2019;60:81–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wilson KE, Miller AL, Bonuck K, et al. Sleep environments and sleep durations in a sample of low-income preschool children. J Clin Sleep Med 2014;10(3):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mileva-Seitz VR, Bakersmans-Kraneburg MJ, Battaini C, et al. Parent-child bed-sharing: the good, the bad, and the burden of evidence. Sleep Med Rev 2017;32:4–27. [DOI] [PubMed] [Google Scholar]
- 81.Covington LB, Armstrong B, Black MM. Bed sharing in toddlerhood: choice versus necessity and provider guidelines. Glob Pediatr Health 2019;6. 10.1177/2333794X19843929.2333794X19843929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mindell JA, Sadeh A, Wiegand B, et al. Cross-cultural differences in infant and toddler sleep. Sleep Med 2010;11(3):274–80. [DOI] [PubMed] [Google Scholar]
- 83.Barajas RG, Martin A, Brooks-Gunn J, et al. Motherchild bed-sharing in toddlerhood and cognitive and behavioral outcomes. Pediatrics 2011;128(2): e339–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zambrano DN, Mindell JA, Reyes NR, et al. It’s not all about my baby’s sleep”: a qualitative study of factors influencing low-income african american mothers’ sleep quality. Behav Sleep Med 2016; 14(5):489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Caldwell BA, Ordway MR, Sadler LS, et al. Parent perspectives on sleep and sleep habits among young children living with economic adversity. J Pediatr Health Care 2020;34(1):10–22. [DOI] [PubMed] [Google Scholar]
- 86.Williamson AA, Milaniak I, Watson B, et al. Early childhood sleep intervention in urban primary care: caregiver and clinician perspectives. J Pediatr Psychol 2020;45(8):933–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Spilsbury JC, Patel SR, Morris N, et al. Household chaos and sleep-disturbing behavior of family members: results of a pilot study of African American early adolescents. Sleep Health 2017;3(2): 84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Koopman-Verhoeff ME, Serdarevic F, Kocevska D, et al. Preschool family irregularity and the development of sleep problems in childhood: a longitudinal study. J Child Psychol Psychiatry 2019; 60(8):856–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Covington LB, Patterson F, Hale LE, et al. The contributory role of the family context in early childhood sleep health: a systematic review. Sleep Health 2021;7(2):254–65. [DOI] [PubMed] [Google Scholar]
- 90.Daniel LC, Childress JL, Flannery JL, et al. Identifying modifiable factors linking parenting and sleep in racial/ethnic minority children. J Pediatr Psychol 2020;45(8):867–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fronberg KM, Bai S, Teti DM. Household chaos mediates the link between family resources and child sleep. Sleep Health 2022;8:121–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rojo-Wissar DM, Owusu JT, Nyhuis C, et al. Parent-child relationship quality and sleep among adolescents: modification by race/ethnicity. Sleep Health 2020;6(2):145–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Powell CA, Rifas-Shiman SL, Oken E, et al. Maternal experiences of racial discrimination and offspring sleep in the first 2 years of life: project Viva cohort, Massachusetts, USA (1999–2002). Sleep Health 2020;6(4):463–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Med Rev 2016;18:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cohen MF, Dunlop AL, Johnson DA, et al. Intergenerational effects of discrimination on black american children’s sleep health. Int J Environ Res Public Health 2022;19(7):4021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Blackson EA, Gerdes M, Segan E, et al. Racial bias toward children in the early childhood education setting. J Early Child Res 2022. 10.1177/1476718X221087051.1476718X221087051. [DOI] [Google Scholar]
- 97.Maina IW, Belton TD, Ginzberg S, et al. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med 2018;199:219–29. [DOI] [PubMed] [Google Scholar]
- 98.Starck JG, Riddle T, Sinclair S, et al. Teachers are people too: examining the racial bias of teachers compared to other american adults. Educ Res 2020;49(4):273–84. [Google Scholar]
- 99.van Ryn M Research on the provider contribution to race/ethnicity disparities in medical care. Med Care 2002;40:I140–51. [DOI] [PubMed] [Google Scholar]
- 100.Wang EC, Choe MC, Meara JG, et al. Inequality of access to surgical specialty health care: why children with government-funded insurance have less access than those with private insurance in Southern California. Pediatrics 2004;114(5):e584–90. [DOI] [PubMed] [Google Scholar]
- 101.Yip T, Wang Y, Xie M, et al. School Start Times, Sleep, and Youth Outcomes: A Meta-analysis. Pediatrics 2022;149(6):e2021054068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Levenson JC, Thoma BC, Hamilton JL, et al. Sleep among gender minority adolescents. Sleep 2021; 44(3):zsaa185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Crenshaw K Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum 1989, no. 1 (1989): 139–167. [Google Scholar]
- 104.Schwichtenberg AJ, Abel EA, Keys E, et al. Diversity in pediatric behavioral sleep intervention studies. Sleep Med Rev 2019;47:103–11. [DOI] [PubMed] [Google Scholar]
- 105.Baumann AA, Cabassa LJ. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv Res 2020;20(1):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Andrews K, Parekh J, Peckoo S. How to embed a racial and ethnic equity perspective in research: practical guidance for the research process. Child Trends 2019. Available at: https://www.researchconnections.org/childcare/resources/38276. Accessed May 2, 2022. [Google Scholar]


