Abstract
From the COVID-19 global pandemic to racial injustice and the continued impact of climate change on communities across the globe, the last couple of years have demonstrated the need for a greater understanding of how to protect people from the negative consequences of stress. Here, I outline a perspective on how the brain’s reward system might be an important, but often understudied, protective mechanism for stress resilience and stress-related health outcomes. I describe work suggesting that reward system engagement inhibits the stress response and is associated with improved health outcomes including reduced depressive symptomatology and slowed cancer progression. I then highlight important future directions for translational research and illustrate the value of this perspective for improving behavioral interventions in clinical psychology and beyond.
Keywords: reward, stress, health outcomes, resilience
With the rapid, global spread of the COVID-19 virus and ensuing pandemic came uncertainty, social isolation, and stress. However, COVID-19 is just one example of recent events that have increased stress levels for people. Over the past few years, there has been an increase in catastrophic natural disasters, divisive politics, increased attention to rising inequity and racial injustice. These concerns are raising population stress. Stressful life events have been linked to incidence and exacerbation of physical health concerns (such as cardiovascular disease and viral infection) and mental health concerns (including Post-Traumatic Stress Disorder (PTSD) and depression) (Cohen et al., 2007). The rise in stress levels and the negative repercussions of stress emphasize a growing need for basic research on stress resilience and more effective stress management interventions.
While a rich body of work has explored the effects that stress has on health and well-being, work that seeks to understand how to enhance stress resilience is in its infancy. Initial work on stress resilience traditionally focused on top-down executive control processes, such as cognitive control. For example, a review of the literature finds that neurocognitive processes, such as problem solving, planning and goal-directed behavior, are linked to stress regulation (Williams et al., 2009). However, while there is good empirical support for interventions that improve executive functioning for individuals with deficits in executive functioning, there might be other pathways to stress resilience that are modifiable for the general population. Here, I detail an understudied, and perhaps underappreciated, pathway to stress resilience: the brain’s reward system. I describe the neural reward system’s role in stress reduction and improvements in mental and physical health. I then outline some future directions for research on the relationship between reward and stress resilience. Increased mechanistic and translational research attention would accelerate the development of interventions for improving stress resilience and health.
The Neurobiology of Reward and Stress
Rewarding stimuli are those that are important for an organism’s survival and lead to activation of a network in the brain that identifies the value of the stimulus (Schultz, 2015). The brain’s reward system includes regions in the prefrontal cortex (orbitofrontal cortex/ventromedial prefrontal cortex) and ventral striatum (See Figure 1), and involve the neurotransmitters dopamine and opioids (Haber & Knutson, 2010). This neurobiological reward system is activated to a range of stimuli. Primary rewards are those most typically thought to influence survival, e.g., food and reproduction. However, secondary rewards are those that have been learned to be beneficial to the organism, e.g., money and social support. Research suggests that both types of rewarding stimuli lead to activation of the reward system and have similar affective consequences (Sescousse et al., 2013). Additionally, there are three key psychological components of reward: (1) learning—the process by which a stimulus or experience is learned to be valuable, (2) liking—the pleasant affective experience of receiving or engaging with a reward, and (3) wanting—the motivation or desire to engage with a reward stimulus (Berridge & Robinson, 2003). A great deal of work in the reward literature has found that these processes rely on both common and dissociable neurobiology (Berridge et al., 2009).
Figure 1.
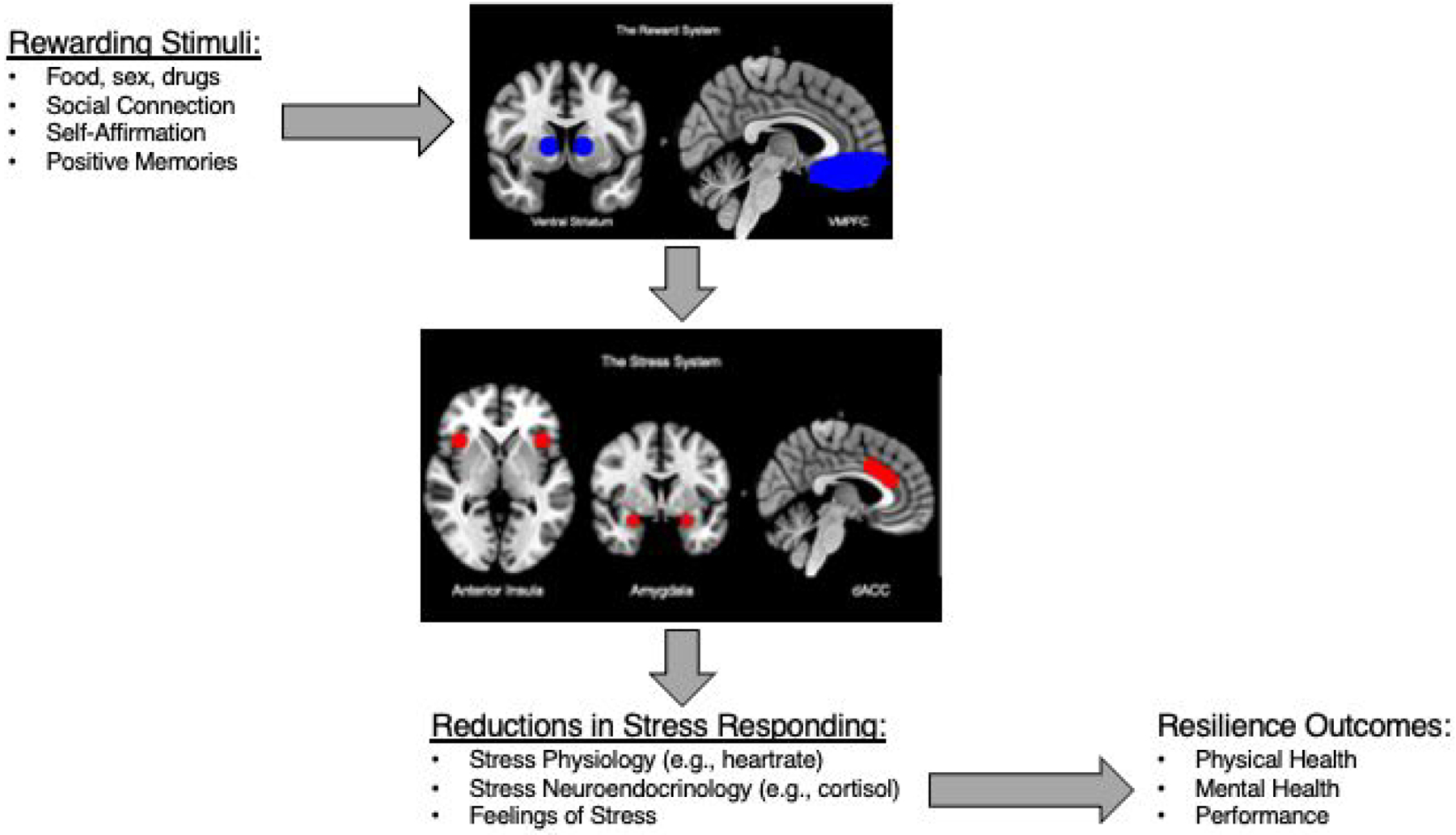
A figure displaying the proposed pathway for how rewarding stimuli lead to reductions in stress responding and subsequent improvements in physical health.
The brain’s stress system, on the other hand, includes regions such as the amygdala, dorsal anterior cingulate cortex, and insula (Ulrich-Lai & Herman, 2009). These regions (see Figure 1) coordinate the physiological stress response. Classically, the physiological stress response is marked by increased activity in the hypothalamic-pituitary adrenal (HPA) axis, a neuroendocrine response leading to a release of the stress hormone cortisol in humans, and the sympathetic nervous system, leading to changes in blood pressure and heart rate (Ulrich-Lai & Herman, 2009). There is also evidence that stress can affect the immune system, leading to an immune response that is similar to what is seen when the body experiences an infection (Cohen et al., 2007). Following the onset of a stressor, the brain coordinates a cascade of these processes to facilitate a response to the stressor. However, repeated, or prolonged stress can result in wear-and-tear on the physiological systems that support stress responding and can lead to health consequences, such as depression or cardiovascular disease (McEwen & Seeman, 1999). Resilience is thought to be the successful coping or adjustment to a stressor and is a pathway for preventing stress-related mental and physical health conditions in the future.
Some initial work shows that reward system regions can inhibit activity in regions in the neural stress system (Eisenberger et al., 2011; Ulrich-Lai & Herman, 2009), which offers the reward system as a biologically plausible mechanism for stress reduction effects. The dynamics of reward-stress system communciation are still being identified, but some human and animal work has begun to identify critical components of this process. For example, reward-system neurotransmitters, such as dopamine and endogenous opioids, have receptors sites that are expressed in regions coordinating the stress response (Drolet et al., 2001). Furthermore, blocking dopamine or opioids by administering antagonists, resulted in exaggerated stress responses in animals (Abercrombie & Jacobs, 1988). Increasing opioids, by administering an agonist, led to lower cortisol stress responding and self-reported stress levels in humans (Bershad et al., 2015). Thus, altering the presence of reward system neurotransmitters has direct effects on stress responding, evidence of the link between the brain’s reward and stress systems.
The Reward System Reduces Stress Reactivity
There is emerging evidence that activating the brain’s reward system leads to reductions in stress responding. Experimental work in humans and animals has found that exposure to rewarding stimuli reduces physiological stress reactivity. For example, rats given sweet drinks or access to sexually receptive mates for several days showed decreased neuroendocrine (HPA axis) and cardiovascular (sympathetic system) stress reactivity responses to restraint stress (Ulrich-Lai et al., 2010). These effects are also seen in humans; for example, viewing rewarding erotic images reduced neuroendocrine cortisol reactivity to a subsequent laboratory stress challenge task (Creswell, Pacilio, et al., 2013). Moreover, this reward-stress buffering link is not just observed with primary rewards. For example, social support activates the reward system in the brain (Eisenberger et al., 2011) and buffers cortisol stress responding (Kirschbaum et al., 1995). Reflecting on an important personal value activates the reward system (Dutcher et al., 2016), reduces neural activity in response to acute stress (Dutcher et al., 2020) and buffers cortisol reactivity to acute stress (Creswell et al., 2005).
Experimental work has also found that exposure to rewarding stimuli reduces behavioral and psychological responses to stress. Indeed, rats who were rewarded demonstrated less anxiety behavior to a stressor (Ulrich-Lai et al., 2010), and even zebra fish show less anxious behavior to a stress paradigm when given rewarding food (Manuel et al., 2015). In human infants, a sweet fluid led to less crying to a blood draw procedure (Abad et al., 1996). Similarly, in adults, receiving either primary or secondary rewards have been linked to better performance on stressful math and verbal exams (Creswell, Dutcher, et al., 2013; Creswell, Pacilio, et al., 2013).
These results suggest that rewarding stimuli can lead to stress reduction acutely. Indeed, this effect is observed across species, which implicates systems in the brain that are shared across animal and human models. Indeed, while some work in stress reduction points to cortical structures (such as executive function in the prefrontal cortex), those are clearly not the only neural systems involved in stress reduction based on the animal work described here. Research in this area should further explore how activating these reward systems in the brain affect stress physiology and subsequent behavior, as well as how enduring these effects are.
Reward-Stress Resilience Pathways and Health
One example of potential enduring effects of reward administration is physical and mental health outcomes. Initial studies in rodents highlight relationships between reward system activation and physical health. For example, experimental activation of the reward system improves immunity and limits cancer progression in mice. Specifically, directly stimulating endogenous dopamine neurons within the mouse reward system led to enhanced adaptive immune responses following a bacterial challenge (Ben-Shaanan et al., 2016). These reward-health effects appear to be driven by stress resilience pathways, as they were mediated by sympathetic nervous system influences on the immune system (Ben-Shaanan et al., 2016). In a separate study, stimulation of the same reward region in the brain led to reductions in tumor weight in mice with tumors, an effect that was mediated by sympathetic nervous system influences on immunity in bone marrow (Ben-Shaanan et al., 2018). Taken together, these studies suggest that direct stimulation of the reward system affects physiological stress systems that link stress to poorer health. Reward-health links have been observed in humans, too. Engaging in rewarding activities, such as taking vacation time, is associated with lower resting blood pressure, lower body mass index (BMI), and decreased risk of metabolic syndrome (Hruska et al., 2020; Pressman et al., 2009). A probable mechanism for these health benefits is activation of the brain’s reward system in response to these rewarding activities, leading to corresponding reductions in stress.
Moreover, greater neural reward reactivity may be protective against the negative effects of stress on mental health. Indeed, taking vacation time is associated with lower depressive symptoms (Pressman et al., 2009). Greater neural reward reactivity to rewarding tasks was associated with longitudinal decreases in depressive symptoms in adolescents (Telzer et al., 2014) and fewer depressive symptoms in young adults reporting high levels of 2016-Presidential election-related distress (Tashjian & Galván, 2018). Individuals with a high degree of recent stress showed lower positive affect when they had low ventral striatum (VS) reward reactivity, but those with high VS reactivity showed higher positive affect, suggesting the protective effects of reward reactivity on vulnerability to depression (Nikolova et al., 2012). Similarly, reward reactivity or stimulation may have benefits in clinical populations, as well. For example, deep brain stimulation of reward-related regions in the brain in patients with refractory major depressive disorder led to a lessening of symptoms (Bewernick et al., 2010). Research on patients with post-traumatic stress disorder (PTSD) also finds that higher reward reactivity might buffer against the psychological externalizing behaviors following trauma (Kasparek et al., 2020) and that high reward activity in the brain to reward (compared to punishment) leads to a decrease in PTSD symptoms (Ben-Zion et al., 2022). These initial findings suggest that reward reactivity may buffer against the mental health consequences of stress or distress, and thus engaging the reward system might have stress-related health benefits.
One of the key challenges and opportunities facing the field is how to best leverage the reward-stress reduction pathway for health. How do acute effects of rewarding stimuli on stress responding link to broader physical and mental health benefits? How do we build reward-activating interventions that support long term stress resilience in at risk patient populations?
Building Interventions that Foster Resilience via the Reward System
While some clinical treatments capitalize on engaging reward pathways (e.g., deep brain stimulation), the field has yet to fully exploit the reward system in behavioral treatments for patients. One notable exception is Behavioral Activation Therapy (Dimidjian et al., 2006). Recognized as an evidence-based treatment for depression, one feature of BA therapy is to have patients schedule more positive, rewarding activities into their day, and to find more opportunities for reaching valued self-identified goals as core elements of the treatment (Dimidjian et al., 2006). While it is not yet clear whether BA therapy itself directly activates the reward system, research has found that in patients with Major Depressive Disorder treatment with BA therapy results in a recovery of activity in reward structures known to be affected in depression in response to reward anticipation and reward feedback (Dichter et al., 2009). There is also the potential for building more rewarding activities into existing behavioral treatments (e.g., daily rewarding activities, increased leisure time), or training clinicians to reinforce those rewarding moments in existing behavioral interventions, as tools for increasing the efficacy of psychological and behavioral treatments. For instance, a combined mindfulness and cognitive behavioral therapy program led depressed patients to report greater appreciation of rewarding and positive experiences in their life, which corresponded to decreases in depression symptoms (Geschwind et al., 2011). Translational research can capitalize on this work showing links between reward system activation and stress resilience to build more powerful and effective stress-reduction interventions.
Here, I will outline six basic and translational research areas that could help facilitate the creation or improvement of stress-reduction interventions and clinical paradigms.
(1). Basic research should continue to explore the neurobiological mechanisms for reward-stress reduction.
Initial neuroanatomical investigations have identified connections between reward and stress systems in the brain, but less work has tested a mechanistic pathway by which rewarding stimuli can reduce stress responding in the brain and body, and under what circumstances that can buffer against the negative health consequences of stress. A model that maps reward system activation to neural stress responding to physiological stress responding and consequently behavioral responding would help home in on the conditions under which intervention could be helpful. One key future direction is a greater understanding of the structural connections (e.g., white matter pathways in the brain) between stress and reward networks in the brain. Another key direction is which reward regions and target stress system regions are critical for stress reduction; animal work has identified a candidate nucleus in the amygdala (Ulrich-Lai et al., 2010), which could help future interventions to target the most essential mechanisms for stress reduction benefits.
(2). An important next step in translational research will be to investigate how presentation of a reward stimulus leading to acute stress reduction subsequently links to long-term stress resilience and health enhancement.
Work has been done focusing on reduction of the acute stress response, as well as lifestyle effects on health, but little work has examined a time course model that would link these intermittent reward-stress reduction effects to subsequent health. For example, some initial work employed a study design where presentation of a stressful stimulus followed a reward stimulus, allowing analyses to focus on stressful events that followed reward compared to stressful events that did not. This design facilitated a greater understanding of the temporal processes of reward-stress reduction. However, it will be key to further probe the temporal process implicated in reward-stress responding, as well as to explore how these neural processes link to downstream stress physiology.
(3). Research should clarify the bidirectional relationship between stress and reward.
Many clinical studies find that patients with a high stress burden or depression demonstrate reduced reward responsivity (Pizzagalli, 2014). Because the relationship between stress and reward is bidirectional, research should clarify the nature of the relationship. Studies on functional and structural connectivity in neuroimaging trials could help elucidate the nature of the association between the reward and stress systems in the brain. For example, are the structural connections between reward and stress regions in the brain bidirectional, or do they leverage separate pathways? This work is critical for understanding who and when a reward-based intervention might work for—for example, do these interventions need to occur prior to the onset of a clinical diagnosis? If a patient is depressed, will a reward intervention be less effective because their reward system shows blunted responding to rewarding stimuli? It is possible that the type of reward may be an important detail for this area of research. Previous work has focused on blunted reward responses to money in clinical patients, which may not be as potent a reward stimulus for patients with depression.
(4). Research should explore whether different types of stressors may influence what reward intervention could be effective, and what type of rewards might be most effective in interventions.
While building interventions that offer intermittent primary rewards could have important stress reduction benefits, they might create practical (or ethical) issues: giving stressed individuals delicious, rewarding food might lead to increased obesity risk, and offering opiates might lead to addiction. Interventions that focus on engaging patients with secondary rewards may have greater translational value. Secondary rewards such as giving and receiving social support and thinking about positive aspects of the self, have been shown to activate the brain’s reward system and buffer against the negative effects of a broad range of stressors (Dutcher & Creswell, 2018). There is a broader potential for secondary rewards and rewarding activities to be part of standard clinical care for individuals with stress-related conditions.
(5). Each component of reward (learning, wanting, liking) might have differential effects on stress reduction and health enhancement.
Most of the work exploring reward-stress reduction effects has focused on the “liking” component of reward or has not separated these reward components during investigation. It may be the case that one component is necessary or solely responsible for subsequent stress dampening effects, which would influence the content of interventions for stress reduction. For example, some evidence suggests that individuals with depression may show greater motivational deficits because of low “wanting” than low feelings of “liking” (Sherdell et al., 2012). This could implicate interventions that maximize opportunities for the pleasurable feelings of a reward.
(6). Finally, essential to broader implementation, testing these reward-based interventions in practice with at-risk populations will be important.
Thus far, research suggests that reward-stress reduction could have preventative effects on health and other stress-related consequences. But work on BA therapy also suggests that reward-based therapies could be effective as treatments for stress-related health conditions such as depression. Investigating the strengths of this account for prevention as well as for treatment will be critical for implementation in healthcare settings. Similarly, understanding the conditions and disease states for which these therapies might be effective would help build an intervention science that could be widely practiced in mental and physical health settings.
Moving Forward: New Directions for Building a Reward-Stress Resilience Literature
Emerging research paints a compelling portrait of how activating the reward system can foster stress reduction and improve stress-related health. I believe there are important new directions for building out translational neuroscience research and intervention science that links rewards, stress resilience, and health. Over the last couple of years, the COVID-19 crisis has affected billions worldwide and strategies for building stress resilience are more important than ever. We can look to resilient responses to other major events for inspiration. For example, following the disastrous wildfires in the American West over the last five years, millions of dollars were donated in fundraisers, survivors formed support groups, and events were planned to celebrate rebuilt homes. It is not a coincidence that the natural tendency after stressful events is to reach out and connect with others, and to donate to recovery efforts—in fact, I suspect that these behaviors result in activation of the reward system, promoting resilience, adjustment, and health. As we continue to work to understand how to support people through difficult major events, the science of stress resilience is more important than ever. Research can continue to map out the neurobiology of stress reduction interventions and their health benefits, and we can build empirically supported, effective ways to help people manage during stressful life events.
Acknowledgements
The author has no conflicts of interest to report with this work. She has received research funding from Headspace Inc. for separate mindfulness intervention research. I thank J. David Creswell for helpful comments on this manuscript.
References
- Abad F, Diaz NM, Domenech E, Robayna M, & Rico J (1996). Oral sweet solution reduces pain-related behaviour in preterm infants. Acta Paediatrica, 85(7), 854–858. [DOI] [PubMed] [Google Scholar]
- Abercrombie ED, & Jacobs BL (1988). Systemic naloxone administration potentiates locus coeruleus noradrenergic neuronal activity under stressful but not non-stressful conditions. Brain Research, 441(1–2), 362–366. 10.1016/0006-8993(88)91415-1 [DOI] [PubMed] [Google Scholar]
- Ben-Shaanan TL, Azulay-Debby H, Dubovik T, Starosvetsky E, Korin B, Schiller M, Green NL, Admon Y, Hakim F, Shen-Orr SS, & others. (2016). Activation of the reward system boosts innate and adaptive immunity. Nature Medicine, 22(8), 940–944. [DOI] [PubMed] [Google Scholar]; One of the first experimental studies to demonstrate, in mice, that direct activation of the reward system could lead to improved adaptive immunity. This work highlights the potential for rewarding activities and interventions to have direct effects on markers of physical health.
- Ben-Shaanan TL, Schiller M, Azulay-Debby H, Korin B, Boshnak N, Koren T, Krot M, Shakya J, Rahat MA, & Hakim F (2018). Modulation of anti-tumor immunity by the brain’s reward system. Nature Communications, 9(1), 2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zion Z, Shany O, Admon R, Keynan NJ, Avisdris N, Balter SR, Shalev AY, Liberzon I, & Hendler T (2022). Neural Responsivity to Reward Versus Punishment Shortly After Trauma Predicts Long-Term Development of Posttraumatic Stress Symptoms. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 7(2), 150–161. [DOI] [PubMed] [Google Scholar]
- Berridge KC, & Robinson TE (2003). Parsing reward. Trends in Neurosciences, 26(9), 507–513. 10.1016/S0166-2236(03)00233-9 [DOI] [PubMed] [Google Scholar]
- Berridge KC, Robinson TE, & Aldridge JW (2009). Dissecting components of reward: ‘Liking’, ‘wanting’, and learning. Current Opinion in Pharmacology, 9(1), 65–73. 10.1016/j.coph.2008.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bershad AK, Jaffe JH, Childs E, & de Wit H (2015). Opioid partial agonist buprenorphine dampens responses to psychosocial stress in humans. Psychoneuroendocrinology, 52, 281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bewernick BH, Hurlemann R, Matusch A, Kayser S, Grubert C, Hadrysiewicz B, Axmacher N, Lemke M, Cooper-Mahkorn D, & Cohen MX (2010). Nucleus accumbens deep brain stimulation decreases ratings of depression and anxiety in treatment-resistant depression. Biological Psychiatry, 67(2), 110–116. [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, & Miller GE (2007). Psychological stress and disease. Jama, 298(14), 1685–1687. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Dutcher JM, Klein WMP, Harris PR, & Levine JM (2013). Self-Affirmation Improves Problem-Solving under Stress. PLoS ONE, 8(5), e62593. 10.1371/journal.pone.0062593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, Pacilio LE, Denson TF, & Satyshur M (2013). Experimental manipulation of primary sexual reward buffers cortisol responses to psychosocial stress in men. Psychosomatic Medicine, 75, 1–7. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Welch WT, Taylor SE, Sherman DK, Gruenewald TL, & Mann T (2005). Affirmation of personal values buffers neuroendocrine and psychological stress responses. Psychol Sci, 16(11), 846–851. [DOI] [PubMed] [Google Scholar]
- Dichter GS, Felder JN, Petty C, Bizzell J, Ernst M, & Smoski MJ (2009). The effects of psychotherapy on neural responses to rewards in major depression. Biological Psychiatry, 66(9), 886–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Gallop R, McGlinchey JB, Markley DK, & Gollan JK (2006). Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology, 74(4), 658. [DOI] [PubMed] [Google Scholar]
- Drolet G, Dumont EC, Gosselin I, Kinkead R, Laforest S, & Trottier JF (2001). Role of endogenous opioid system in the regulation of the stress response. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 25(4), 729–741. [DOI] [PubMed] [Google Scholar]
- Dutcher JM, & Creswell JD (2018). The role of brain reward pathways in stress resilience and health. Neuroscience & Biobehavioral Reviews, 95, 559–567. [DOI] [PubMed] [Google Scholar]; A review that describes the evidence linking reward system activation to stress buffering, and the neurobiological underpinnings of this effect.
- Dutcher JM, Creswell JD, Pacilio LE, Harris PR, Klein WMP, Levine JM, Bower JE, Muscatell KA, & Eisenberger NI (2016). Self-Affirmation Activates the Ventral Striatum: A Possible Reward-Related Mechanism for Self-Affirmation. Psychological Science, 27(4), 455–466. 10.1177/0956797615625989 [DOI] [PubMed] [Google Scholar]
- Dutcher JM, Eisenberger NI, Woo H, Klein WM, Harris PR, Levine JM, & Creswell JD (2020). Neural mechanisms of self-affirmation’s stress buffering effects. Social Cognitive and Affective Neuroscience. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Master SL, Inagaki TK, Taylor SE, Shirinyan D, Lieberman MD, & Naliboff BD (2011). Attachment figures activate a safety signal-related neural region and reduce pain experience. Proceedings of the National Academy of Sciences, 108(28), 11721–11726. 10.1073/pnas.1108239108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geschwind N, Peeters F, Drukker M, van Os J, & Wichers M (2011). Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 79(5), 618. [DOI] [PubMed] [Google Scholar]
- Haber SN, & Knutson B (2010). The Reward Circuit: Linking Primate Anatomy and Human Imaging. Neuropsychopharmacology, 35(1), 4–26. 10.1038/npp.2009.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruska B, Pressman SD, Bendinskas K, & Gump BB (2020). Vacation frequency is associated with metabolic syndrome and symptoms. Psychology & Health, 35(1), 1–15. [DOI] [PubMed] [Google Scholar]
- Kasparek SW, Jenness JL, & McLaughlin KA (2020). Reward processing modulates the association between trauma exposure and externalizing psychopathology. Clinical Psychological Science, 8(6), 989–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirschbaum C, Klauer T, Filipp S-H, & Hellhammer DH (1995). Sex-specific effects of social support on cortisol and subjective responses to acute psychological stress. Psychosomatic Medicine, 57(1), 23–31. [DOI] [PubMed] [Google Scholar]
- Manuel R, Zethof J, Flik G, & van den Bos R (2015). Providing a food reward reduces inhibitory avoidance learning in zebrafish. Behavioural Processes, 120, 69–72. [DOI] [PubMed] [Google Scholar]
- McEwen BS, & Seeman T (1999). Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences, 896(1), 30–47. [DOI] [PubMed] [Google Scholar]
- Nikolova YS, Bogdan R, Brigidi BD, & Hariri AR (2012). Ventral striatum reactivity to reward and recent life stress interact to predict positive affect. Biological Psychiatry, 72(2), 157–163. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA (2014). Depression, stress, and anhedonia: Toward a synthesis and integrated model. Annual Review of Clinical Psychology, 10, 393–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman SD, Matthews KA, Cohen S, Martire LM, Scheier M, Baum A, & Schulz R (2009). Association of enjoyable leisure activities with psychological and physical well-being. Psychosom Med, 71(7), 725–732. [DOI] [PMC free article] [PubMed] [Google Scholar]; An epidemiological study linking engaging in leisure and reward activities to improvements in health and well-being.
- Schultz W (2015). Neuronal reward and decision signals: From theories to data. Physiological Reviews, 95(3), 853–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sescousse G, Caldú X, Segura B, & Dreher J-C (2013). Processing of primary and secondary rewards: A quantitative meta-analysis and review of human functional neuroimaging studies. Neuroscience & Biobehavioral Reviews, 37(4), 681–696. [DOI] [PubMed] [Google Scholar]
- Sherdell L, Waugh CE, & Gotlib IH (2012). Anticipatory pleasure predicts motivation for reward in major depression. Journal of Abnormal Psychology, 121(1), 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashjian SM, & Galván A (2018). The Role of Mesolimbic Circuitry in Buffering Election-Related Distress. Journal of Neuroscience, 2470–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telzer EH, Fuligni AJ, Lieberman MD, & Galván A (2014). Neural sensitivity to eudaimonic and hedonic rewards differentially predict adolescent depressive symptoms over time. Proceedings of the National Academy of Sciences, 111(18), 6600–6605. 10.1073/pnas.1323014111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich-Lai YM, Christiansen AM, Ostrander MM, Jones AA, Jones KR, Choi DC, Krause EG, Evanson NK, Furay AR, Davis JF, Solomon MB, de Kloet AD, Tamashiro KL, Sakai RR, Seeley RJ, Woods SC, & Herman JP (2010). Pleasurable behaviors reduce stress via brain reward pathways. Proc Natl Acad Sci USA, 107(47), 20529–20534. [DOI] [PMC free article] [PubMed] [Google Scholar]; An elegant set of studies demonstrating that, in rats, rewarding stimuli led to reductions in stress responding across multiple methods of assessment including physiological and behavioral indicators of stress.
- Ulrich-Lai YM, & Herman JP (2009). Neural regulation of endocrine and autonomic stress responses. Nature Reviews Neuroscience, 10(6), 397–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PG, Suchy Y, & Rau HK (2009). Individual differences in executive functioning: Implications for stress regulation. Annals of Behavioral Medicine, 37(2), 126–140. [DOI] [PubMed] [Google Scholar]


