Abstract
BACKGROUND
This study evaluates and describes the pattern of services provided for people living with multiple sclerosis (MS) in a local area as a starting point for a more global assessment.
METHODS
A health care ecosystem approach has been followed using an internationally standardized service classification instrument–the Description and Evaluation of Services and DirectoriEs for Long Term Care (DESDE-LTC)–to identify and describe all services providing care to people with MS in the Australian Capital Territory, Australia. Available services were classified according to the target population into those specifically dedicated to people living with MS and those providing general neurologic services, both public and private, and across both social and health sectors.
RESULTS
A limited range of services was available. There were no local facilities providing or coordinating multidisciplinary integrated care specific to people with MS. Subspecialty services specific to MS were limited in number (6 of the 28 services), and use of specialist services provided in neighboring states was frequently reported. Overall, very few services were provided outside the core health sector (4%).
CONCLUSIONS
The provision of care to people living with MS in the Australian Capital Territory is fragmented and relies heavily on generic neurology services in the public and private sectors. More widespread use of the DESDE-LTC as a standardized method of service classification in MS will facilitate comparison with other local areas, allow monitoring of changes over time, and permit comparison with services provided for other health conditions (eg, dementia, mental disorders).
Keywords: DESDE-LTC, multiple sclerosis, health care system, service mapping
Multiple sclerosis (MS) is the most common disabling neurologic condition of young adults, typically diagnosed between 20 and 40 years of age. The global prevalence of MS is currently estimated to be 2 million to 2.5 million cases, representing a 10.4% increase since 1990.1 It is a chronic disease: Its diverse symptoms, clinical course, and complications necessitate comprehensive multidisciplinary assessment and management plans for optimal patient care.2,3 Development of a comprehensive model of care requires evidence-informed health care planning to ensure adequate availability of both the necessary services and an appropriately skilled workforce.4 A detailed description of current services available is a necessary first step for such planning to identify and prioritize strategies and resource allocation. This is particularly relevant to the management of MS, which requires input from a range of health care professionals from different sectors during the disease course, especially in light of the growing number of treatment strategies available.5–7
Existing information on the availability of MS-related health care resources is very limited globally, and nonexistent in Australia. For example, none of the 4 books in the Australian Atlas of Healthcare Variation series provides information relating to neurologic conditions or MS in particular.8
The World Health Organization’s One Health model calls for a holistic and collaborative approach to programs, policies, legislation, and research.9 Unfortunately, obtaining information about services available for neurologic diseases is subject to serious methodological limitations. Current classification systems, such as the Organization for Economic Co-operation and Development’s System of Health Accounts, do not provide a complete picture of local care provision because they10 exclude sectors such as social services. Moreover, previous experience with services for other complex conditions, such as drug and alcohol or mental health services, shows variable or ambiguous terminology (eg, “rehabilitation services” can encompass very different types of care provision). Another potential source of error is “ecological fallacy,” ie, incorrect assumptions about a local area based on aggregate data relating to the whole country: “Top down” national indicators cannot be used to determine the existing levels of services, beds, and professionals in a particular locality.11
This study begins to address the current gap in knowledge by demonstrating the usability of a standard approach to evaluate the service delivery system for MS in a catchment area. Eventually, this should be extended globally as previously shown for mental health care.12 As the starting point, we used the Description and Evaluation of Services and DirectoriEs for Long Term Care (DESDE-LTC)13,14 to evaluate and describe the availability of MS-related services in the Australian Capital Territory (ACT).
METHODS
Ethics approval for this study was granted by the ACT Health Human Research Ethics Committee.
Study Area
The ACT is a federal territory of approximately 2300 km2 with a population of approximately 429,000 people. Canberra, the territory’s only city and the nation’s capital, is home to approximately 400,000 people, representing 90% of the ACT population. It provides medical services to surrounding areas of southern New South Wales, many of which are 3 hours’ drive away. The ACT has a high local prevalence of MS (third-highest in Australia after Tasmania and South Australia), with an estimated total of 538 people with MS (or 131.1 per 100,000 population) in 2020.15,16
Inclusion Criteria
All services located within the boundaries of the ACT providing direct care or support to people with MS, including those providing information and coordination to support people in the management of their illness, were included in the analysis, provided they were temporally and administratively stable.
Instrument
The instrument used to collect and analyze the data was the DESDE-LTC, an internationally standardized tool validated in 6 European countries from Western and Eastern Europe for the description and classification of services across different sectors.13 It enables valid comparison across local areas and countries despite differing levels of care, units of analysis, and terminology.12,17,18
The DESDE-LTC is conceptually based on a health care ecosystems research approach, which takes a whole systems approach to health care, “facilitating analysis of the complex environment and context of mental health systems, and translation of this knowledge into policy and practice.”14
A health ecosystem is the totality of circumstances relating to a given health condition in a defined environment.14 This whole systems approach includes all sectors and workers providing care (not just those providing clinical health care) to a defined population group to provide a comprehensive profile of the availability and workforce capacity of the care system in a particular region. The DESDE-LTC provides the crucial first step in the analysis of service systems by assessing actual service availability in a region. This information can then be used to facilitate further analyses, such as financing networks or assessment of quality.
The DESDE-LTC classifies and codes services providing care or support according to 4 different axes: (1) target population (age group and the health condition), (2) sector of care (eg, health/social/education/employment), (3) main type of care (MTC) the service provides, and (4) workforce (the number and type of professionals providing direct support to the service user; not included in this study). The DESDE-LTC provides a taxonomy of care types from which the MTC provided by each team providing care is identified and coded. This taxonomy is based on criteria such as service acuity, mobility (center based or outreach), availability to the service user (eg, daily, weekly), and whether health related or other.
First, each team providing care within each organization is identified. These are described as a basic stable input of care (BSIC) (ie, a care team). Then, the MTC delivered by each BSIC is described according to the 6 main branches of the taxonomy: (1) residential care, (2) day care, (3) outpatient care, (4) accessibility of care, (5) information care, and (6) self-help and volunteer care.
Each of these branches is divided further according to the criteria noted previously herein (acuity, etc). The MTC code is added to those describing target population and sector of care to provide a highly granular and multiaxial final code describing the care provided by a BSIC. This standardized approach allows an accurate and meaningful comparison with other regions. See APPENDIX S1, available online at IJMSC.org, and the eDESDE-LTC website (http://www.edesdeproject.eu) for more details.
Data Collection
The following steps were conducted between May 2021 and August 2021:
Initial search identifying eligible services: Online, telephone directory, and official service directories were scanned for relevant services. People with MS and experts in the field were also consulted.
Webpage content extraction: Information required for description/classification of the services, such as location, administration, temporal stability, governance, and financing mechanisms, was manually collected from the webpages of the identified service providers. Any missing information was requested at interview (step 4).
Contacting organizations and arranging interviews: Relevant organizations were contacted directly to arrange interviews with their representatives to collect details of services provided to people with MS.
Interviewing representatives: A representative from each identified organization was interviewed using the DESDE-LTC service inventory questionnaire (Appendix S1).13
Meeting with focus group: An expert panel of 5 consumers (people with MS) and 4 health service researchers was established to obtain feedback and provide external validation of collected data.
Service Coding and Analysis
A DESDE-LTC code was allocated to each service identified by the previously described processes that fulfilled the inclusion criteria. The number of BSICs and their MTC were analyzed and described according to the availability of MTC per 100,000 adult population in the study area.
Spider plots were used to display the distribution of the different MTCs and depict the mixture of service types (ie, pattern of care) in the area. Each point on the 24 radii of a spider plot represents the number of a particular MTC per 100,000 adult population in the study area.
RESULTS
General Overview of MTC
In the ACT, 16 organizations provide care to people with MS (TABLE S1). They had 25 BSICs, which, in turn, provided 28 MTCs. The MTCs provided by the care teams fell into 5 of the 6 main DESDE-LTC categories and into 11 of the possible 24 clusters of type of care. Of the 5 categories, outpatient care accounted for the greatest proportion of care provided (67%), followed by residential care (11%), day services (11%), accessibility services (7%), and self-help volunteer care (4%) (Table S1). We did not identify any service falling into the category of information care.
Specialist medical services were provided mostly in the public sector by Canberra Hospital and Calvary Public Hospital. MS Ltd, a national not-for-profit organization supporting people living with MS, was the main organization providing access to social and disability services for this group. This organization provides support and also helps coordinate support from other sectors.
Subspecialized vs Specialized Services
Of the 25 BSICs, 5 provided 6 subspecialized services specifically for people with MS. Twenty BSICs provided 22 specialized services for people with any neurologic problem, including MS (Table S1).
FIGURE 1 is a spider plot showing the relative patterns of general neurologic and subspecialized services for people with MS. Subspecialized services were largely limited to health-related, nonacute, nonmobile outpatient care along with some accessibility services. General specialist neurology services accounted for most of the available acute outpatient care for people with MS, but they also provided residential inpatient acute and nonacute hospital care and nonacute day care services. Overall, most service provision was center based, ie, provided in nonacute, nonmobile outpatient settings. This was followed by nonacute, mobile, social-type outpatient care. There were low levels of service provision in acute health-related outpatient care and accessibility services, and very low rates of service provision in day services and alternatives to hospital care.
FIGURE 1.
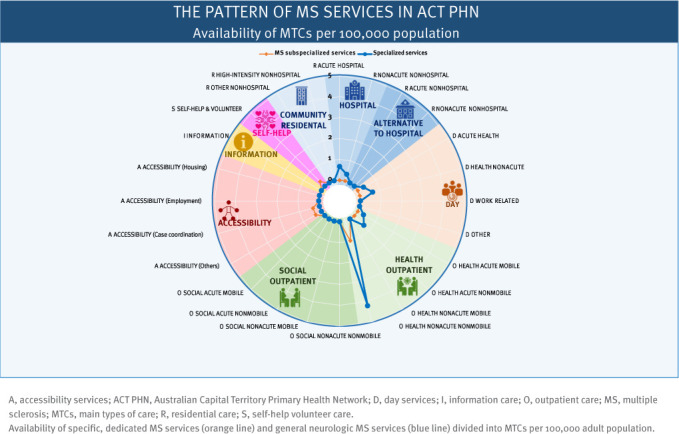
Availability of Care: Specific MS Services vs General Neurologic MS Services
As Table S1 and Figure 1 show, subspecialized services (services dedicated specifically to people with MS) comprised only a small proportion of total neurologic care delivered in the ACT. There were approximately 2 sessions per week of dedicated MS clinic in Canberra Hospital, both staffed by a consultant neurologist; 1 of these was also staffed by a neurology registrar and an MS nurse. In total, 0.8 full-time equivalent (FTE) neurologist, 3 nurse professionals, 3 rehabilitation professionals, and 3 case managers or social workers were dedicated specifically to caring for people with MS in the ACT. The general neurology workforce in the public sector comprised 6.6 FTE neurology consultants (10 individuals) and 8.0 FTE neurology registrars.
Public vs Private Services
Of the 16 organizations identified, 5 (with 13 BSICs and 16 MTCs) provided public services free of charge and 11 (with 12 BSICs and 11 MTCs) charged for their services, meaning that clients had to have private insurance, have access to special government funding (eg, Department of Veterans’ Affairs or National Disability Insurance Scheme), or pay out of pocket. FIGURE 2 shows that the public sector provided a range of services from residential to self-help/volunteer services, whereas the private sector provided only outpatient center–based services. Private services were provided mostly by neurologists in their offices (Table S1).
FIGURE 2.
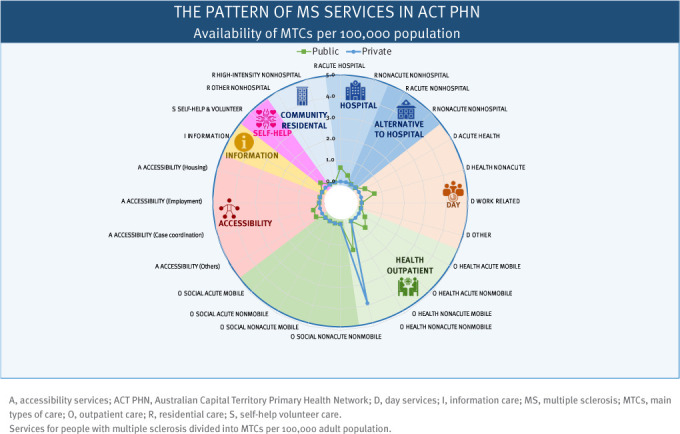
Availability of MS Care: Public vs Private
Health vs Social Services
Medical management of MS is only 1 aspect of overall care. Other elements, such as social support and accessibility to support and information, must be provided by other agencies, of which there were only 2 in the ACT: MS Ltd and a self-help/volunteer service. The MS care available in the ACT was provided by the health sector and core health professionals, ie, neurologists, nurses, physiotherapists and exercise therapists, and case managers and social workers.
DISCUSSION
The aim of this study was to investigate the provision and pattern of care services available to people with MS in a specified local area, the ACT, with a view to beginning a global process. The included services were all specialized and subspecialized services, public and private care, health and social care. The findings revealed that subspecialized services specific to MS were limited and predominantly health related. Care was delivered largely in the context of general specialized neurology services, public and private. There were no social or coordination services dedicated specifically to people with MS. Because of the overall limitations in the ACT, many people with MS accessed dedicated subspecialty services in New South Wales or Victoria. It was not possible to obtain information relating to the number and extent of these non-ACT services for the purposes of this study.
Multiple sclerosis has become a subspecialty within neurology, making it difficult for general neurologists to keep pace with the increasing complexity of diagnostic and treatment strategies.19 The Consortium of Multiple Sclerosis Centers’ US Framework Taskforce described care provision patterns and care team profiles necessary for the optimal treatment of MS.2,3 According to this taskforce, the core of the MS care unit should ideally include neurologists subspecialized in MS, nursing professionals, physiatrists, mental health professionals, social workers, urologists, and rehabilitation professionals, along with physician assistants, orthopedists, patient advocates, primary care clinicians, and pharmacists. This core team should collaborate with an expanded network of additional specialists such as dietitians, speech therapists, and continence specialists.19
Considering the wide variation in the clinical manifestations and the course of the disease, different patterns of care must be made available.20 This requires an integrated, person-centered approach, as recommended by the World Health Organization.21 This approach, in turn, requires greater multidisciplinary involvement and a shift toward community-based provision of service,22 something acknowledged by Australian health system planning.23
In the past 2 decades, improvement in disease-modifying therapies has meant a large reduction in need for hospitalization and/or acute care for people with MS, resulting in an increased demand for community-based care.22 This demand has not yet been addressed through necessary but challenging changes in the design and planning of the overall provision of care to people with MS.24–26 Community care may have more cost benefit for patients27 and be more effective in improving access to specialist care,28 but it is more complex, requiring a high level of coordination to avoid providing fragmented care, in comparison to a traditional model of care that is limited to hospital services.29 Without careful planning, a shift from hospital-based to community-based care could create new types of inefficiency along with case management and service navigation difficulties, creating new challenges for both patients and professionals.
People with MS may have significant nonmedical social needs that impact their health and quality of life, and these should be considered when developing individual management plans.30 Unfortunately, a significant obstacle to developing and integrating social services into health care is generated by the financial incentives associated specifically with health-related services: There is minimal incentive for health systems to develop systems of care that comprehensively integrate social services.30
Although evaluating the number of professionals dedicated to the care of patients with neurologic diseases in the ACT was not the focus of this study, we identified 6.6 FTE consultants and 8.0 FTE registrars in the public sector in the ACT (ie, Canberra Hospital and Calvary Public Hospital). Overall, only 11.3 FTEs were specifically dedicated to MS. These FTEs were neurologists, registrars, nurse professionals, case managers, social workers, and rehabilitation professionals, providing 11 of the 24 types of care for people with MS in the ACT. Overall, the limited resources tended to work in isolation; they were fragmented and not well coordinated.
This MS care assessment is the first of its kind performed anywhere in the world. Consequently, similar data are not available to allow direct comparison with any other area, including Australia. In absolute terms, service provision in ACT fell below the standard of care recommended in recent publications for people with MS,2,3 but this may prove to be universal when other Australian jurisdictions are assessed in a similar way. Recent recommendations call for a multidisciplinary plan to support the different management clusters that individuals may need during the course of their disease.20 The gradual movement of MS care from hospitals to nonhospitals22 means that alternative community care units should be introduced to provide an appropriate multidisciplinary plan of care. This should encompass outpatient centers, day care, supported accommodation, and other alternatives of community care.31
A comprehensive model for care of people with chronic conditions should involve both health and social services.31 However, there are almost no MS-directed social services in the ACT. At this stage, it is not yet possible to compare this finding with other regions in Australia or the world. To the best of our knowledge, this is the first study describing service provision in MS using a standard classification to allow comparisons across jurisdictions and over time. A factor that does need to be considered is that a lack of locally available sufficient and equitable care may be less problematic if services cooperate.31 Therefore, even if the establishment of further services is not practical because of insufficient demand, coordinating the available local and adjacent services could improve the efficacy of the whole system.
A strength of the present study is that it incorporates a standardized description of the local patterns of service delivery from a whole-system perspective. Such standardized descriptions are critical to prevent ambiguity and improve planning, allocation of resources, and future service provision, as shown previously in relation to mental health care.32 This study provides information specific to the availability of care for people with MS. Therefore, we have included general neurology services that provide care for MS but not all the available services for all neurologic conditions in the ACT.
A limitation of the present study is that assessment of medical input was limited to subspecialized and specialized services in neurology, including rehabilitation services with special programs for people with MS. The separation of subspecialized and specialized services was based on the allocation of services to people with MS or any neurologic diseases: Lack of knowledge about the level of training in both groups is a limitation of this study. Other specialized services, such as urology or psychiatry, and generalized services, such as general practitioners, also provide care to people with MS: For logistical reasons, these were not included in this study. They could form part of a more comprehensive study in the future.
It is also important to bear in mind that MS is only 1 of many different conditions treated by neurology services. There will be competition for scarce resources, but more widespread application of tools such as the DESDE-LTC would facilitate equitable distribution. The DESDE-LTC was originally validated for the coding of chronic care in 6 Western and Eastern European countries, and although the extent and psychometric depth of its validation surpasses that of other global service assessment tools,33 extending this validation to other parts of the world would be beneficial. A final strength is that this study’s methods can be repeated, enabling follow-up over time to monitor the impact of plans and changes,34 such as the introduction of new services, particularly if coupled with assessment of health-related quality of life and satisfaction of care provided to people living with MS.
Future developments will include the release of an Integrated Atlas of Care for Multiple Sclerosis in the ACT that could be used for local planning and resource allocation, and encouraging similar studies in other health districts, Australia, and internationally. This would allow health system comparison across jurisdictions.
CONCLUSIONS
This study shows that a standardized classification tool can be used to determine the availability of subspecialized and specialized MS services in a local health district. The overall findings suggest that although recommended components of care (ie, MS care units, social care, home care, neurorehabilitation) were available, increased input is required to meet the standard of care recommended by the Consortium of Multiple Sclerosis Centers.2,3 This finding is likely to apply to other areas. Standardized assessments of this kind and their widespread incorporation into the whole system would allow local and national care systems to be compared with each other and against recommended models of care, as well as with care systems related to people with other diseases. In addition, standardized assessments would allow for accurate tracking of changes over time after the implementation of any new decisions. We believe that there is significant value in widespread adoption of this process.
PRACTICE POINTS
This study demonstrates the usability and practicality of the Description and Evaluation of Services and DirectoriEs for Long Term Care as a standard description of multiple sclerosis care at a subspecialized and specialized level.
The local understanding of service provision should be filled to allow for evidence-informed planning in multiple sclerosis service provision. Increased input is required to meet the standard level of care recommended by the Consortium of Multiple Sclerosis Centers.
Supplementary Material
ACKNOWLEDGMENTS:
The authors thank the Our Health in Our Hands (OHIOH) Health Experience MS team members, who provided invaluable comments regarding MS care in the ACT: Dr Jane Desborough, Ms Janet Drew, Dr Anne Parkinson, Associate Professor Anne Brustle, Dr Vanessa Fanning, Ms Helena Paul, Ms Katrina Chisholm, Dr Mary Webb, and Mr Mark Elisha.
Funding Statement
FUNDING/SUPPORT: This work was funded by an Incubator Grant from MS Research Australia (application number: 19–0656) and was supported by OHIOH, a strategic initiative of the Australian National University created in partnership with ACT Health.
Footnotes
FINANCIAL DISCLOSURES: The authors declare no conflicts of interest.
REFERENCES
- 1.GBD 2016 Multiple Sclerosis Collaborators Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol . 2019;18(3):269–285. doi: 10.1016/S1474-4422(18)30443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Newsome SD, Aliotta PJ, Bainbridge J et al. A framework of care in multiple sclerosis, part 2: symptomatic care and beyond. Int J MS Care . 2017;19(1):42–56. doi: 10.7224/1537-2073.2016-062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newsome SD, Aliotta PJ, Bainbridge J et al. A framework of care in multiple sclerosis, part 1: updated disease classification and disease-modifying therapy use in specific circumstances. Int J MS Care . 2016;18(6):314–323. doi: 10.7224/1537-2073.2016-051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Furst MA, Salinas-Perez JA, Gutiérrez-Colosia MR, Salvador-Carulla L. A new bottom-up method for the standard analysis and comparison of workforce capacity in mental healthcare planning: demonstration study in the Australian Capital Territory. PLoS One . 2021;16(7):e0255350. doi: 10.1371/journal.pone.0255350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gottberg K, Einarsson U, Ytterberg C, Fredrikson S, von Koch L, Holmqvist LW. Use of health care services and satisfaction with care in people with multiple sclerosis in Stockholm County: a population-based study. Mult Scler . 2008;14(7):962–971. doi: 10.1177/1352458508089688. [DOI] [PubMed] [Google Scholar]
- 6.Goldschmidt C, McGinley MP. Advances in the treatment of multiple sclerosis. Neurol Clin . 2021;39(1):21–33. doi: 10.1016/j.ncl.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romeo MAL, Martinelli V, Dalla Costa G et al. Assessing the role of innovative therapeutic paradigm on multiple sclerosis treatment response. Acta Neurol Scand . 2018;138(5):447–453. doi: 10.1111/ane.12999. [DOI] [PubMed] [Google Scholar]
- 8. Healthcare variation. Australian Commission on Safety and Quality in Health Care. Accessed October 8, 2021. https://www.safetyandquality.gov.au/our-work/healthcare-variation.
- 9.One Health Q&A World Health Organization. September 21, 2017. Accessed December 8, 2021. https://www.who.int/news-room/q-a-detail/one-health.
- 10.OECD/Eurostat/World Health Organization A System of Health Accounts 2011 Revised Edition . OECD Publishing; 2017. Classification of health care providers (ICHA-HP) [Google Scholar]
- 11.Rosen A, Rock D, Salvador-Carulla L. The interpretation of beds: more bedtime stories, or maybe they’re dreaming? Aust N Z J Psychiatry . 2020;54(12):1154–1156. doi: 10.1177/0004867420969813. [DOI] [PubMed] [Google Scholar]
- 12.Romero-López-Alberca C, Gutiérrez-Colosía MR, Salinas-Pérez JA et al. Standardized description of health and social care: a systematic review of use of the ESMS/DESDE (European Service Mapping Schedule/Description and Evaluation of Services and DirectoriEs) Eur Psychiatry . 2019;61:97–110. doi: 10.1016/j.eurpsy.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Salvador-Carulla L, Alvarez-Galvez J, Romero C et al. Evaluation of an integrated system for classification, assessment and comparison of services for long-term care in Europe: the eDESDE-LTC study. BMC Health Serv Res . 2013;13:218. doi: 10.1186/1472-6963-13-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Furst MA, Bagheri N, Salvador-Carulla L. An ecosystems approach to mental health services research. BJPsych Int . 2021;18(1):23–25. doi: 10.1192/bji.2020.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Key facts and figures about multiple sclerosis. MS Australia. Updated September 2020. Accessed May 9, 2021. https://www.msaustralia.org.au/wp-content/uploads/2021/09/msa-key-facts-figures_2020-2.pdf.
- 16. Health Economic Impact of Multiple Sclerosis in Australia in 2017 Menzies Health Economics Research Group for Multiple Sclerosis Research Australia. August 2018. Accessed May 9, 2021. https://msra.org.au/wp-content/uploads/2018/08/health-economic-impact-of-ms-in-australia-in-2017_ms-research-australia_web.pdf.
- 17.Gutiérrez-Colosía MR, Salvador-Carulla L, Salinas-Pérez JA et al. Standard comparison of local mental health care systems in eight European countries. Epidemiol Psychiatr Sci . 2019;28(2):210–223. doi: 10.1017/S2045796017000415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ala-Nikkola T, Pirkola S, Kaila M et al. Identifying local and centralized mental health services: the development of a new categorizing variable. Int J Environ Res Public Health . 2018;15(6):1131. doi: 10.3390/ijerph15061131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soelberg Sorensen P, Giovannoni G, Montalban X, Thalheim C, Zaratin P, Comi G. The multiple sclerosis care unit. Mult Scler . 2019;25(5):627–636. doi: 10.1177/1352458518807082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roux J, Kingwell E, Zhu F, Tremlett H, Leray E;, BeAMS Study Group Care consumption of people with multiple sclerosis: a multichannel sequence analysis in a population-based setting in British Columbia, Canada. Mult Scler . 2022;28(2):309–322. doi: 10.1177/13524585211016726. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization WHO global strategy on integrated people-centered health services 2016–2026. July 24, 2015. Accessed October 8, 2021. https://interprofessional.global/wp-content/uploads/2019/11/WHO-2015-Global-strategy-on-integrated-people-centred-health-services-2016-2026.pdf. [Google Scholar]
- 22.Marrie RA, Elliott L, Marriott J et al. Dramatically changing rates and reasons for hospitalization in multiple sclerosis. Neurology . 2014;83(10):929–937. doi: 10.1212/Wnl.0000000000000753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lukersmith S, Salvador-Carulla L, Sturmberg J, Huckel Schneider C, Wilson A, Gillespie J. Expert Commentary What Is the State of the Art in PersonCentered Care? Menzies Centre for Health Policy; 2016. [Google Scholar]
- 24.Rosen A, Gill NS, Salvador-Carulla L. The future of community psychiatry and community mental health services. Curr Opin Psychiatry . 2020;33(4):375–390. doi: 10.1097/YCO.0000000000000620. [DOI] [PubMed] [Google Scholar]
- 25.Salvador-Carulla L, Costa-Font J, Cabases J, McDaid D, Alonso J. Evaluating mental health care and policy in Spain. J Ment Health Policy Econ . 2010;13(2):73–86. [PubMed] [Google Scholar]
- 26.Hashtarkhani S, Tabatabaei-Jafari H, Kiani B, Furst M, Salvador-Carulla L, Bagheri N. Use of geographical information systems in multiple sclerosis research: a systematic scoping review. Mult Scler Relat Disord . 2021;51:102909. doi: 10.1016/j.msard.2021.102909. [DOI] [PubMed] [Google Scholar]
- 27.Rotstein Z, Hazan R, Barak Y, Achiron A. Perspectives in multiple sclerosis health care: special focus on the costs of multiple sclerosis. Autoimmun Rev . 2006;5(8):511–516. doi: 10.1016/j.autrev.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Sibbald B, McDonald R, Roland M. Shifting care from hospitals to the community: a review of the evidence on quality and efficiency. J Health Serv Res Policy . 2007;12(2):110–117. doi: 10.1258/135581907780279611. [DOI] [PubMed] [Google Scholar]
- 29.Freeman JA, Thompson AJ. Community services in multiple sclerosis: still a matter of chance. J Neurol Neurosurg Psychiatry . 2000;69(6):728–732. doi: 10.1136/jnnp.69.6.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feinglass J, Norman G, Golden RL, Muramatsu N, Gelder M, Cornwell T. Integrating social services and home-based primary care for high-risk patients. Popul Health Manag . 2018;21(2):96–101. doi: 10.1089/pop.2017.0026. [DOI] [PubMed] [Google Scholar]
- 31.Desborough J, Brunoro C, Parkinson A et al. ‘It struck at the heart of who I thought I was’: a meta-synthesis of the qualitative literature examining the experiences of people with multiple sclerosis. Health Expect . 2020;23(5):1007–1027. doi: 10.1111/hex.13093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Castelpietra G, Simon J, Gutierrez-Colosia MR, Rosenberg S, Salvador-Carulla L. Disambiguation of psychotherapy: a search for meaning. Br J Psychiatry . 2021;219(4):532–537. doi: 10.1192/bjp.2020.196. [DOI] [PubMed] [Google Scholar]
- 33.Furst MA, Gandré C, Romero López-Alberca C, Salvador-Carulla L. Healthcare ecosystems research in mental health: a scoping review of methods to describe the context of local care delivery. BMC Health Serv Res . 2019;19(1):173. doi: 10.1186/s12913-019-4005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fernandez A, Salinas-Perez JA, Gutierrez-Colosia MR et al. Use of an integrated Atlas of Mental Health Care for evidence informed policy in Catalonia (Spain) Epidemiol Psychiatr Sci . 2015;24(6):512–524. doi: 10.1017/S2045796014000511. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


