Abstract
A large number of soft tissue masses affect the foot and ankle, with the majority being benign. Benign and malignant soft tissue lesions usually present as lumps, and it is important to differentiate between them to allow for optimal management. Imaging, in particular magnetic resonance imaging (MRI), can contribute to narrow the differential diagnosis of soft tissue masses of the foot and ankle by describing its exact location, internal signal characteristics, presence of enhancement, and its relation to adjacent structures. In this review, we review the literature to describe the most common soft tissue masses around the foot and ankle, focusing on the MRI features of the lesions.
Keywords: Ankle, benign, foot, lesions, magnetic resonance imaging, malignant, mass, soft tissue
INTRODUCTION
Soft tissue masses at the foot and ankle are relatively uncommon compared with masses in the other musculoskeletal regions, and thus approaching such masses may create a diagnostic dilemma.[1] Diagnosis of suspicious lesions is usually delayed because some malignant lesions can mimic benign lesions, making it difficult to make a correct diagnosis at an early stage.
The prevalence of tumors of the foot and ankle is about 4–5% of all musculoskeletal tumors, with the vast majority of them being benign.[1–4] Imaging is considered an effective tool to diagnose soft tissue masses, ranging from ultrasound (US) to magnetic resonance imaging (MRI). US evaluation is considered the initial assessment of soft tissue tumors. It helps differentiate the cystic nature that is typical for benign lesions from the solid nature of most malignant lesions. In addition, the use of Doppler ultrasound may aid in detecting the presence of vascular flow within a mass. However, US has its limitations and should be used with caution, as it is operator dependent and can be difficult to properly assess the entire mass, especially when they are localized deep to bone structures and joints for proper preoperative planning.[5,6] Plain radiographs usually have a limited role in evaluating soft tissue lesions, but may be helpful in identifying lesions with mineralization and the extent of involvement of the adjacent bone and joint, which can help in identifying the etiology and in planning management.[7]
MRI is considered the best diagnostic imaging modality for optimal soft tissue mass characterization. It provides precise anatomical localization of the lesion, evaluates the signal characteristics of the soft tissue components, and determines the presence of central necrosis and the relationship between the lesion and adjacent structures, i.e., fascia, muscle, bone, and neurovascular bundles.[5]
Low prevalence, absence of pain in more than half of the lesions, and the fact that some malignant lesions can mimic benign lesions all contribute to the high rate of delay in diagnosis and treatment of soft tissue masses of the foot and ankle.[3,4] In this review, we will focus on the commonest soft tissue tumors of the foot and ankle and highlight the MRI features for each lesion.
For this review, a search was carried out with PubMed, using the following keywords: soft tissue masses, foot and ankle, magnetic resonance imaging, benign lesions, malignant lesions, and the last search was conducted in September 2021.
BENIGN SOFT TISSUE MASSES
A variety of soft tissue lesions can occur in the foot and ankle, the majority of which are benign and may demonstrate characteristic imaging features. Clinical features such as the location of the lesion, pain description, and other risk factors are not reliable indicators to differentiate between benign and malignant lesions. Every malignant soft tissue lesion can mimic benign features; therefore, soft tissue tumors have to be considered malignant until proven otherwise. Benign soft tissue masses can be classified according to the origin of the tumor, such as neural, fibrous, fat, synovial, or degenerative origin, such as ganglion cysts.
Lesions of neural origin
Morton’s neuroma
Morton’s neuromas are benign nonneoplastic lesions that result from neural degeneration and perineural fibrosis of a plantar digital nerve and are classically located at the second or third intermetatarsal spaces.[8] This lesion is a common cause of metatarsalgia, with a prevalence of 30–33% of all benign cases. It occurs predominantly in middle-aged patients, with females being more commonly affected, and bilateral lesions are present in about 20% of the cases.[9] Morton’s neuroma manifests clinically as forefoot pain that is exacerbated by wearing narrow shoes and exercise, resulting in compression to the intermetatarsal space.[8] On clinical examination, a positive Mulder sign may be present.
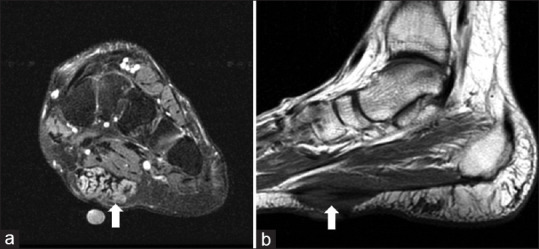
MRI typically demonstrates a well-demarcated tear-shaped lesion located on the plantar side of the deep intermetatarsal ligament of the neurovascular bundle that is isointense to muscle on T1-weighted images and low signal intensity on T2-weighted images with variable enhancement on the post-contrast images [Figure 1].[8,10]
Figure 1.
Morton’s Neuroma (a) Coronal T1, and (b) Coronal T2 fat-saturated MRI images of the forefoot demonstrate a well-defined soft tissue mass lesion within the 2nd intermetatarsal web space demonstrating low signal intensity on both the T1 (arrow) and T2 (arrowhead) weighted images. MRI: Magnetic resonance imaging
Peripheral nerve sheath tumor
Peripheral nerve sheath tumors (PNSTs) are benign soft tissue masses that originate from peripheral nerves and are classified into neurofibroma and schwannoma.[11] There is relatively low incidence of PNSTs around the foot and ankle, as they represent <10% of all soft tissue masses in this region (foot: 5.4%; ankle: 3.9%).[9] Schwannomas are well-encapsulated lesions that originate from Schwann cells of nerve sheaths and are eccentrically placed as they grow, whereas neurofibromas are unencapsulated masses that contain a mixture of fibroblast, myxoid matrix, Schwann cells, and perineural-like cells, and may be associated with NF-1.[11] Both are most frequently seen in patients in their third and fourth decade, with no gender predilection.[9] Clinically, patients usually present with neurological symptoms along with a slow-growing mass.[8] The majority of neurofibromas occur at the heel and big toe along the cutaneous nerves, whereas schwannomas typically present along the flexor surface.[12]
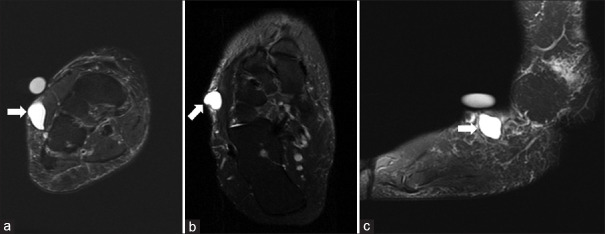
Benign PNSTs share similar MRI features, and it is usually difficult to distinguish between a neurofibroma and a schwannoma. Both lesions appear as a well-defined, fusiform, smooth-bordered mass that is isointense to muscle on T1-weighted and hyperintense to muscle on T2-weighted or short tau inversion recovery (STIR) images. They typically demonstrate heterogeneous avid enhancement on the post-contrast images [Figure 2]. A few signs have been described in the literature that, when seen, should favor the diagnosis of PNST. The first is the split fat sign, which is best seen on a non-fat-saturated T1-weighted sequence and demonstrated as a thin rim of fat signal surrounding the lesion. The second is the target sign, wherein there is a significant high signal intensity of the mass predominantly seen at its peripheral aspect with central low signal intensity fibrous tissue. DWI sequences may demonstrate mild restriction in some cases, but does not differentiate between benign and malignant PNSTs.[8,12,13]
Figure 2.
Peripheral Nerve Sheath Tumor (a) Sagittal STIR, (b) Sagittal T1, and (c) Sagittal T1 fat-saturated post contrast MRI images of the ankle demonstrating large well defined soft tissue mass lesion at the posterior aspect of the ankle along the course of the posterior tibial nerve. It shows homogeneous high signal intensity on the STIR image (arrow) and low signal intensity on the T1 weighted image (arrowhead). On the post contrast images, there is heterogenous enhancement (curved arrow). STIR: Short tau inversion recovery, MRI: Magnetic resonance imaging
Lesions of fibrous origin
Known as Ledderhose disease, plantar fibromatosis is a benign superficial fibroblastic proliferative disorder that arises within the middle and medial aspect of the plantar aponeurosis.[14] In the foot and ankle, the mass represents 15% of benign soft tissue lesions and is associated with other fibromatoses (such as Dupuytren’s contracture and Peyronnie’s disease).[15] Plantar fibromatosis typically presents in patients between the fourth and sixth decade with a male predominance, and bilateral lesions occur in 10–25% of the cases.[9,16] This lesion clinically manifests with a painless fixed palpable nodule or mass at the plantar aspect of the foot.[8,16]
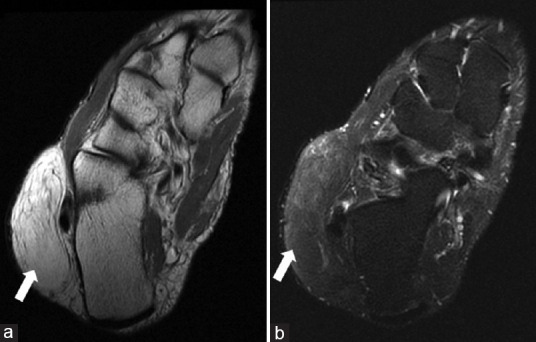
At MRI, plantar fibromatosis is characteristically seen as poorly defined nodules adherent to the plantar aponeurosis, typically at the medial aspect with a well-defined lower margin. The lesion typically demonstrates heterogeneous isointense to hypointense signal relative to skeletal muscle on both the T1- and T2-weighted sequences with variable degrees of enhancement [Figure 3]. They may be seen extending along the aponeurosis, forming a “fascial tail sign.” It has been reported that early growing lesions tend to be hyperintense on T2-weighted images, as they are more cellular, while mature fibrotic lesions lean more to be of low signal intensity on the T2-weighted images.[8,17,18]
Figure 3.
Plantar fibromatosis (Ledderhose disease) (a) Coronal T2 fat-saturated, and (b) Sagittal T1 MRI image demonstrates an ill-defined soft tissue mass lesion at the plantar aspect of the mid-foot along the plantar fascia demonstrating intermediate to low signal intensity on both the T1 and T2 weighted images (arrows). MRI: Magnetic resonance imaging
Lesions of cystic origin
Ganglion cysts are common non-neoplastic cystic lesions that contain viscous mucinous fluid resulting from degeneration of the connective tissue. They may arise from an adjacent joint capsule, ligament, or tendon sheath. Ganglion cysts are relatively common and among the most common incidental masses picked up on routine MRI. The most common soft tissue masses in the foot and ankle are ganglion cyst and can be present in about 40% of patients who undergo MRI due to suspected soft tissue mass.[9,19,20] They are most commonly seen in young adults, with a slight female predilection. When small, these lesions are usually asymptomatic and identified on routine imaging for other reasons. However, when larger, they may present with painful swelling, fluctuation, or symptoms of nerve impingement when located adjacent to neurovascular bundles.[8,9,21]
On MRI, ganglion cysts are typically seen as well-defined, multilobulated cystic lesions with homogenous low signal intensity on T1-weighted images and high signal intensity on T2-weighted images [Figure 4]. On the post-contrast sequences, there is usually faint thin peripheral enhancement without a central enhancing component. However, the MRI appearance of a ganglion cyst can be adjusted by chronic inflammation or hemorrhage, leading to slightly hyperintense signal on the T1-weighted images.[21,22]
Figure 4.
Ganglion cyst (a) Coronal T2 fat-saturated, (b) Axial T2 fat-saturated, and (c) Sagittal T2 fat-saturated MRI images of the right ankle demonstrate a well-defined simple cystic lesion within the subcutaneous soft tissues at the lateral aspect of the mid-foot (arrows) with homogeneous hyperintense signal on the T2 weighted images. No internal septations, mural nodularity or surrounding inflammatory changes. MRI: Magnetic resonance imaging
Lesions of fat origin
Lipoma is a benign well-encapsulated soft tissue tumor of mature white adipocytes.[14,23] Although lipoma is one of the most encountered lesions of all soft tissue masses, it is rarely found in the foot and ankle, with an incidence of up to 2.1 per 100 individuals.[9,24] Lipomas are most commonly encountered in patients between the fourth and sixth decade.[9] In the majority of the cases, lipomas can present clinically as a slow-growing, painless soft tissue swelling.[8]
On MRI, a lipoma usually appears as a well-defined homogenous lesion with signal intensities similar to subcutaneous fat on all pulse sequences. They are usually hyperintense on both T1- and T2-weighted images, with complete suppression of signal on the fat-saturated sequences and without significant enhancement on the post-contrast sequences [Figure 5]. Rarely, alteration of the fat signal can happen secondary to hemorrhage, inflammation, infarction, and calcification.[8,23,25]
Figure 5.
Lipoma (a) Axial PD, and (b) Axial T2 fat-saturated MRI demonstrating a well-defined soft tissue mass lesion within the subcutaneous soft tissues at the lateral aspect of the hindfoot demonstrating hyperintense signal on the PD sequence (arrow) with complete saturation of signal on the fat saturated image (arrowhead) compatible with fat signal. There are few thin internal septations, however no mural soft tissue nodularity. PD: Proton density, MRI: Magnetic resonance imaging
Lesions of synovial origin
Pigmented villonodular synovitis (PVNS) and giant cell tumor of tendon sheath (GCTTS) are benign proliferative nonneoplastic disorders of the synovium. It has recently been termed as tenosynovial giant cell tumor of the diffuse type and localized type, respectively. Histologically, both are composed of multinucleated giant cells with hemosiderin and xanthoma cells deposition intra- and extra-articularly.[23,26] When localized and extra-articular, they are usually termed GCTTS. However, the term PVNS is usually reserved when it is more diffuse and intra-articular.[26] The highest incidence of both lesions occurs within the third to fifth decades of life, and it is more frequently seen in females.[9,26]
Pigmented villonodular synovitis
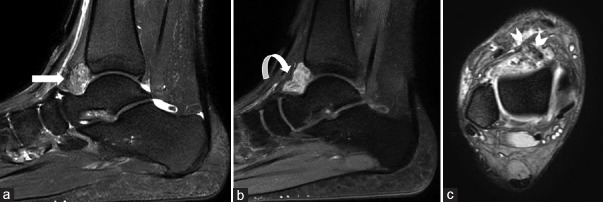
PVNS is a diffuse intra-articular proliferative synovial disorder, primarily affecting single joints.[23] PVNS is usually monoarticular, with the knee followed by the hip being the most frequent locations, whereas the ankle involvement represents the third most common site, with a prevalence of 2.5% among benign tumors of the foot and ankle.[9,26] Clinically, the lesions are usually slowly progressive over years and present with swelling, limited range of motion, pain, and mostly serosanguineous joint effusion.[23,26] On MRI, it typically shows diffuse “mass-like” synovial thickening within the joint, demonstrating heterogenous mixed intermediate to low signal intensity on T1- weighted images, depending on the relative proportions of hemosiderin, collagen, and fat within the lesion. On T2-weighted and STIR images, PVNS has heterogenous signal intensity, with key characteristic finding of blooming artifact on gradient-echo (GRE) sequences as well as hypointense foci on T2-weighted images due to the presence of hemosiderin within the mass. On post-contrast images, there is diffuse heterogeneous enhancement [Figure 6].[23,27–29]
Figure 6.
PVNS (a) Sagittal STIR, (b) Sagittal T1 fat-saturated post contrast, and (c) Axial GRE sequence MRI images demonstrates a well-defined intra-articular soft tissue mass lesion within the anterior aspect of the tibiotalar joint demonstrating intermediate signal intensity on the STIR (arrow) and avid heterogenous enhancement on the post-contrast images (curved arrow). On the GRE sequence, there is multiple areas of low signal intensity foci “blooming artifact” (arrowheads) suggestive of hemosiderin deposit. STIR: Short tau inversion recovery. MRI: Magnetic resonance imaging. PVNS: Pigmented Villonodular Synovitis, GRE: gradient-echo
Giant cell tumor of tendon sheath
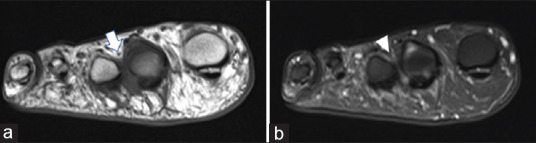
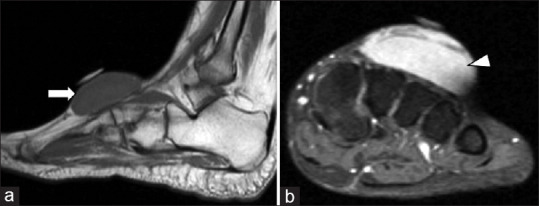
GCTTS is a benign proliferative lesion, also referred to as localized/extra-articular form of PVNS, involving the bursae, tendon, or ligament.[8,23] The majority of the lesions occur in the hand, followed by the foot and ankle, which represent 17% of the lesions, with a predilection among the digits.[9,30] This lesion clinically presents as a well-defined, painless, nodular, slowly growing soft tissue mass.[8,23] On MRI, GCTTS appears as a well-defined oval/round soft tissue lesion. The signal features are similar to PVNS, with marked hypointensity on all image sequences, and usually demonstrate heterogeneous enhancement on the post-contrast sequences.[31,32] Again, due to the presence of hemosiderin within these lesions, they can also demonstrate blooming artifact on the GRE sequences [Figure 7].
Figure 7.
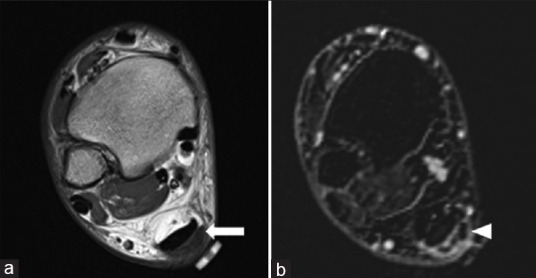
Giant Cell Tumor of the Tendon Sheath (a) Axial T1, and (b) Axial T1 fat-saturated post-contrast subtraction MRI images demonstrates a small well defined soft tissue mass lesion adjacent to the Achilles tendon which shows low signal intensity on the T1 weighted image (arrow) and mild heterogeneous, mainly peripheral enhancement on the post contrast images (arrow head). MRI: Magnetic resonance imaging
Lesions of vascular origin
Vascular lesions are classified into vascular malformation and hemangioma according to the International Society for the Study of Vascular Anomalies (ISSVA). Vascular malformations are nonneoplastic structural abnormalities that are further divided into low (venous, capillary, and lymphatic) and high-flow (arteriovenous and fistula) malformation. On the other hand, hemangiomas are benign proliferative lesions of blood vessels that are further subdivided based on the histologic features into cavernous, venous, arteriovenous, and capillary.[8,33,34] Hemangiomas account for 9% of all benign masses in the foot and ankle, while vascular malformations represent about 3%, most commonly the venous subtype (82%), followed by arteriovenous malformations.[9,33] These lesions are commonly seen in early childhood or early adulthood, and often clinically manifest with painless enlarging palpable mass with or without bluish discoloration of the overlying skin.[8]
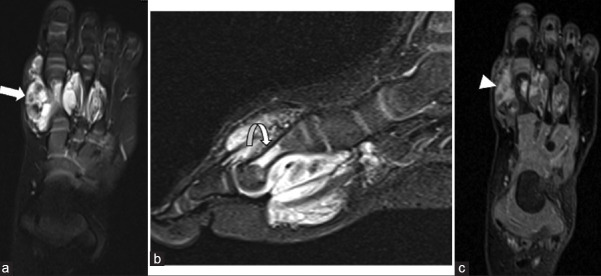
MRI appearance of vascular masses depends on whether it is a low-flow or high-flow malformation. The key to differentiating the two is by the presence of large vascular flow voids adjacent to the mass, representing large feeding arteries or draining veins. If visualized, then this most likely represents a high-flow vascular malformation. Usually, high-flow vascular malformations will have a central nidus of enlarged capillaries with heterogeneous enhancement on the post-contrast images. Low-flow vascular malformations, on the other hand, lack the presence of enlarged vascular flow voids. However, they do demonstrate a well-circumscribed mass insinuating between soft tissue structures that is significantly hyperintense on T2-weighted images with fluid–fluid levels related to the presence of dilated vascular spaces. On T1-weighted images, in most cases, the signal intensity is low, but it can be slightly hyperintense related to internal hemorrhage. Sometimes, small dark foci can be seen within the cystic components of the mass related to phleboliths, and thus correlation with X-rays is very helpful in these cases. On the post-contrast images, venous malformations usually demonstrate slow progressive enhancement, while lymphatic malformations usually show no significant enhancement on the post-contrast images [Figure 8].[8,35–37]
Figure 8.
Hemangioma (a) Axial T2 fat-saturated, (b) Sagittal STIR, and (c) Axial T1 fat-saturated post-contrast images shows an ill-defined infiltrating soft tissue mass lesion within the medial aspect of the forefoot. It demonstrates hyperintense signal on the T2 weighted images (arrows). Also note is made of a small hypointense foci within the mass on T2 weighted images which likely represents small phlebolith. On the post contrast images, there is heterogeneous enhancement (arrowhead). Note is made of intra-osseous extension into the 1st metatarsal shaft (curved arrow). STIR: Short tau inversion recovery
MALIGNANT SOFT TISSUE MASSES
Malignant soft tissue tumors are rare in the foot and ankle. There are certain features in MRI studies that help differentiate benign from malignant soft tissue lesions, including large size (>5 cm), deep site, inhomogeneous signal intensity, hemorrhagic and necrotic, early and inhomogeneous contrast enhancement, irregular margins, surrounding soft tissue edema, and invasion of adjacent structures.[38] The latest evidence suggests that MRI has limitations in providing a specific histologic diagnosis; however, its value is crucial in preoperative planning [Table 1].[12]
Table 1.
The frequency and order of the most common benign and malignant soft tissue tumors of the foot and ankle
| Feature | Benign | Malignant |
|---|---|---|
| Size (cm) | <5 | >5 |
| Location | Superficial | Deep |
| Signal intensity | Homogenous | Heterogenous |
| Margins | Regular well-defined | Irregular ill-defined |
| Hemorrhagic and necrotic component | Absent | Present |
| Surrounding edema | Absent | Present |
| Invasion of adjacent structures | Absent | Present |
Soft tissue sarcoma
In the foot and ankle, the literature suggests that synovial sarcomas are the most common soft tissue sarcoma, although it has also been suggested that the majority of sarcomas are vascular in origin, representing around 30% of all malignant soft tissue tumors of the foot and ankle, followed by synovial sarcomas, which account for one-fifth.[38,39]
It is important to understand that although sarcomas usually demonstrate heterogenous signal intensity with enhancement on MRI, they may also appear non-aggressive and present as a smooth-bordered mass. Ganguly et al.[33] found that soft tissue sarcoma accounted for 4 cases of 417 cases of foot masses (<1%), and 3 out of these 4 cases had heterogenous signal intensity with enhancement.
Synovial sarcoma
Despite the name, synovial sarcoma does not arise from the synovium. Its name is derived from its microscopic resemblance to synovial cells. It is a mesenchymal spindle cell tumor; however, the World Health Organization has classified it as a tumor of uncertain differentiation. Most of the cases are found either adjacent to a joint or around tendon sheaths, and <10% of the lesions grow inside a joint.[38]
Synovial sarcomas were considered the most common malignancies of the foot and ankle in patients aged 6–40 years.[39] Patients classically complain of a palpable deep lump that is painful and tender.[34,38] On MRI, the mass appears as lobulated soft tissue lesions that could be heterogeneously isointense or slightly hyperintense to adjacent muscles on T2-weighted images. Reflecting a combination of cystic (hemorrhagic and necrotic) and solid components, Jones et al.[40] described a triple signal intensity appearance, in reference to intermixed low, intermediate, and high T2 signal within a synovial sarcoma. Nonetheless, this sign is not specific for synovial sarcoma. Fluid–fluid level can be observed in 10% to 25% of the cases. This triple signal with the appropriate age, deep location, and fluid–fluid level should suggest the diagnosis. Contrast enhancement is usually noted, and it is heterogenous, which could be peripheral and nodular.[34,40,41]
Murphey et al. introduced the “bowl of grapes sign” seen in synovial sarcoma, describing it as a combination of a multilobulated mass with heterogenous signal intensity, hemorrhage, fluid-fluid levels, and internal septae.[42] It is important to note that synovial sarcomas can appear as a small nonaggressive lesion with smooth borders and can be mistaken for a cystic lesion, so any cystic lesion with atypical features seen on MRI should mandate IV contrast to determine whether it is a solid or true cyst [Figure 9].[12]
Figure 9.
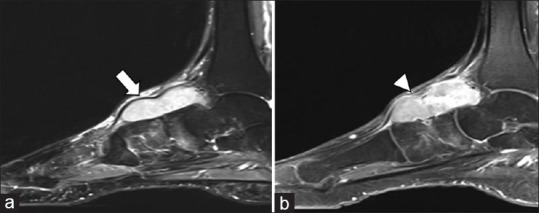
Synovial sarcoma (a) Sagittal STIR, and (b) Sagittal T1 fat saturated post-contrast MRI images demonstrates well defined lobulated soft tissue mass lesion along the dorsal aspect of the foot demonstrating homogeneous hyperintense signal on the STIR images (arrow) and avid homogenous enhancement on the post-contrast images (arrowhead). STIR: Short tau inversion recovery. STIR: Short tau inversion recovery, MRI: Magnetic resonance imaging
Clear cell sarcoma
Clear cell sarcoma (CCS) has been known as malignant melanoma of soft parts, as approximately 50% of these lesions produce melanin. It is a rare malignant tumor that is classified as a neoplasm of uncertain differentiation.[34,43] Unlike the classical melanoma, CCS is a deep lesion that mostly involves tendons, fascia, and aponeurosis.[34,43,44]
This type of tumor affects young adults aged 20–40 years, representing 43% of the cases at the foot and ankle region.[39,43] Symptoms are usually non-specific and clinical presentation is variable from weeks to years prior to diagnosis. Most patients suffer from slowly growing mass that is accompanied with pain and tenderness.[34]
On MRI, CCS usually appears well defined and relatively homogenous, and is often misdiagnosed as benign lesions.[44,45] The effect of melanin in these lesions on MRI can lead to less T1 and T2 relaxation times, showing some degree of hyperintense signal on T1-weighted and hypointense signal on T2-weighted images. Nevertheless, lesions that do not contain melanin can show nonspecific signal intensities.[43] In addition, CCS often shows heterogenous enhancement after the administration of gadolinium contrast.[45]
Malignant peripheral nerve sheath tumor
Malignant PNSTs are rare and account for 3–10% of soft tissue sarcomas. These tumors are usually linked with syndromes such as neurofibromatosis, yet sporadic cases can happen. Malignant PNSTs are hard to differentiate from benign NSTs without explicit malignant features. Patients usually present with complaints of painful or painless masses. On MRI, malignant PNSTs will appear to have low-to-intermediate T1 signal with high T2 signal. The solid components usually demonstrate enhancement on the post-contrast sequences and are often associated with surrounding perilesional edema.[46]
Dermatofibrosarcoma protuberans
Dermatofibrosarcoma protuberans are rare cutaneous malignant tumors that often occur in young adults. They are usually painless and slow-growing superficial masses that could ulcerate. Approximately 85% to 90% of these tumors are usually low grade; therefore, it is unlikely to metastasize, but can be locally aggressive and recur despite surgical excision.[47] MRI is the appropriate diagnostic modality, and it often shows low-to-intermediate T1 signal and high T2 signal with profound internal solid enhancement [Figure 10]. There may also be high T2 signal and enhancement extending through the skin from the tumor.[48]
Figure 10.
DFSP (a) Sagittal T1, and (b) Coronal T1 fat saturated post-contrast MRI images demonstrating a large well defined soft tissue mass lesion within the dorsal aspect of the mid-foot demonstrating low signal intensity on the T1 weighted images (arrow) and avid homogeneous enhancement on the post contrast images (arrowhead). MRI: Magnetic resonance imaging, DFSP: Dermatofibrosarcoma protuberans
Angiosarcoma
Angiosarcoma is an infrequent soft tissue sarcoma that occurs in the inner lining of the blood and lymphatic vessels, accounting for 1–2% of all sarcomas.[49] It usually occurs in patients with a history of chronic lymphedema or previous radiation therapy. However, idiopathic cases have been reported. Angiosarcomas are considered aggressive and have a high potential for metastasis. Patients usually present with a growing reddish mass. On MRI, this type of sarcoma shows a dominant heterogenous T1 hypointense, T2 hyperintense, heterogeneously enhancing mass, and there may also be signs of hemorrhage or necrosis.[46,49]
Liposarcoma
Liposarcomas are malignant tumors of the adipose tissues. They are rare and usually occur in the abdomen and extremities. Patients either present with a painless mass or it is discovered incidentally. Liposarcomas can rarely be seen on X-rays, especially when large, and may appear radiolucent due to its fat content. Small calcifications may also be seen in the setting of fat necrosis. CT can help differentiate liposarcoma from lipoma because the internal nodular soft tissue components, large size, or internal septations thicker than 2 mm favor liposarcoma. On the other hand, MRI results will depend on the histological variation of the tumor. For instance, a well-differentiated liposarcoma almost completely consists of macroscopic fat, and thus it will appear as normal fat on MRI. On the other hand, myxoid liposarcomas often do not contain macroscopic fat, and thus may appear myxomatous with high T2 signal intensity and low T1 signal intensity as well as heterogenous enhancement on the post-contrast sequences.[46]
CONCLUSION
Soft tissue masses of the foot and ankle are considered relatively uncommon. Due to the wide variety of benign and malignant tumors, it may cause a diagnostic dilemma. MRI is the best imaging modality when approaching such tumors. Lesions lacking specific features of benign tumors should be immediately considered as malignant until proven otherwise. Large tumors >5 cm, deep to the fascia, irregular margins, progressive in size with soft tissue and neurovascular involvement are red flags for malignancy. Comprehensive understanding of the features of soft tissue masses around the foot and ankle on imaging will allow physicians to properly diagnose these lesions and better management of patients.
Peer review
This article was peer-reviewed by two independent and anonymous reviewers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chou LB, Ho YY, Malawer MM. Tumors of the foot and ankle:Experience with 153 cases. Foot Ankle Int. 2009;30:836–41. doi: 10.3113/FAI.2009.0836. [DOI] [PubMed] [Google Scholar]
- 2.Pollandt K, Werner M, Delling G. Tumors of the footbones –A report from the Hamburg Bone Tumor Registry. Z Orthop Ihre Grenzgeb. 2003;141:445–51. doi: 10.1055/s-2003-41570. [DOI] [PubMed] [Google Scholar]
- 3.Zeytoonjian T, Mankin HJ, Gebhardt MC, Hornicek FJ. Distal lower extremity sarcomas:Frequency of occurrence and patient survival rate. Foot Ankle Int. 2004;25:325–30. doi: 10.1177/107110070402500509. [DOI] [PubMed] [Google Scholar]
- 4.Rammelt S, Fritzsche H, Hofbauer C, Schaser KD. Malignant tumours of the foot and ankle. Foot Ankle Surg. 2020;26:363–70. doi: 10.1016/j.fas.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Noebauer-Huhmann IM, Weber MA, Lalam RK, Trattnig S, Bohndorf K, Vanhoenacker F, et al. Soft tissue tumors in adults:ESSR-approved guidelines for diagnostic imaging. Semin Musculoskelet Radiol. 2015;19:475–82. doi: 10.1055/s-0035-1569251. [DOI] [PubMed] [Google Scholar]
- 6.Doyle AJ, Miller MV, French JG. Ultrasound of soft-tissue masses:Pitfalls in interpretation. Australas Radiol. 2000;44:275–80. doi: 10.1046/j.1440-1673.2000.00812.x. [DOI] [PubMed] [Google Scholar]
- 7.Hughes P, Miranda R, Doyle AJ. MRI imaging of soft tissue tumours of the foot and ankle. Insights Imaging. 2019;10:60. doi: 10.1186/s13244-019-0749-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Llauger J, Palmer J, Monill JM, Franquet T, Bagué S, Rosón N. MR imaging of benign soft-tissue masses of the foot and ankle. Radiographics. 1998;18:1481–98. doi: 10.1148/radiographics.18.6.9821196. [DOI] [PubMed] [Google Scholar]
- 9.Kransdorf MJ. Benign soft-tissue tumors in a large referral population:Distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164:395–402. doi: 10.2214/ajr.164.2.7839977. [DOI] [PubMed] [Google Scholar]
- 10.Zanetti M, Ledermann T, Zollinger H, Hodler J. Efficacy of MR imaging in patients suspected of having Morton's neuroma. AJR Am J Roentgenol. 1997;168:529–32. doi: 10.2214/ajr.168.2.9016241. [DOI] [PubMed] [Google Scholar]
- 11.Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors:Radiologic-pathologic correlation. Radiographics. 1999;19:1253–80. doi: 10.1148/radiographics.19.5.g99se101253. [DOI] [PubMed] [Google Scholar]
- 12.Hochman MG, Wu JS. MR imaging of common soft tissue masses in the foot and ankle. Magn Reson Imaging Clin N Am. 2017;25:159–81. doi: 10.1016/j.mric.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 13.Lin J, Martel W. Cross-sectional imaging of peripheral nerve sheath tumors:Characteristic signs on CT, MR imaging, and sonography. AJR Am J Roentgenol. 2001;176:75–82. doi: 10.2214/ajr.176.1.1760075. [DOI] [PubMed] [Google Scholar]
- 14.Kirby EJ, Shereff MJ, Lewis MM. Soft-tissue tumors and tumor-like lesions of the foot. An analysis of eighty-three cases. J Bone Joint Surg Am. 1989;71:621–6. [PubMed] [Google Scholar]
- 15.Veith NT, Tschernig T, Histing T, Madry H. Plantar fibromatosis-topical review. Foot Ankle Int. 2013;34:1742–6. doi: 10.1177/1071100713505535. [DOI] [PubMed] [Google Scholar]
- 16.Espert M, Anderson MR, Baumhauer JF. Current concepts review:Plantar fibromatosis. Foot Ankle Int. 2018;39:751–7. doi: 10.1177/1071100718768051. [DOI] [PubMed] [Google Scholar]
- 17.Robbin MR, Murphey MD, Temple HT, Kransdorf MJ, Choi JJ. Imaging of musculoskeletal fibromatosis. Radiographics. 2001;21:585–600. doi: 10.1148/radiographics.21.3.g01ma21585. [DOI] [PubMed] [Google Scholar]
- 18.Morrison WB, Schweitzer ME, Wapner KL, Lackman RD. Plantar fibromatosis:A benign aggressive neoplasm with a characteristic appearance on MR images. Radiology. 1994;193:841–5. doi: 10.1148/radiology.193.3.7972835. [DOI] [PubMed] [Google Scholar]
- 19.Weishaupt D, Schweitzer ME, Morrison WB, Haims AH, Wapner K, Kahn M. MRI of the foot and ankle:Prevalence and distribution of occult and palpable ganglia. J Magn Reson Imaging. 2001;14:464–71. doi: 10.1002/jmri.1208. [DOI] [PubMed] [Google Scholar]
- 20.Tay AY, Tay KS, Thever Y, Hao Y, Yeo NEM. An epidemiological review of 623 foot and ankle soft tissue tumours and pseudo-tumours. Foot Ankle Surg. 2021;27:400–4. doi: 10.1016/j.fas.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Steiner E, Steinbach LS, Schnarkowski P, Tirman PF, Genant HK. Ganglia and cysts around joints. Radiol Clin North Am. 1996;34:395–425. xi-xii. [PubMed] [Google Scholar]
- 22.Feldman F, Singson RD, Staron RB. Magnetic resonance imaging of para-articular and ectopic ganglia. Skeletal Radiol. 1989;18:353–8. doi: 10.1007/BF00361424. [DOI] [PubMed] [Google Scholar]
- 23.Foo LF, Raby N. Tumours and tumour-like lesions in the foot and ankle. Clin Radiol. 2005;60:308–32. doi: 10.1016/j.crad.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 24.Murphey MD, Carroll JF, Flemming DJ, Pope TL, Gannon FH, Kransdorf MJ. From the archives of the AFIP:Benign musculoskeletal lipomatous lesions. Radiographics. 2004;24:1433–66. doi: 10.1148/rg.245045120. [DOI] [PubMed] [Google Scholar]
- 25.Kransdorf MJ, Bancroft LW, Peterson JJ, Murphey MD, Foster WC, Temple HT. Imaging of fatty tumors:Distinction of lipoma and well-differentiated liposarcoma. Radiology. 2002;224:99–104. doi: 10.1148/radiol.2241011113. [DOI] [PubMed] [Google Scholar]
- 26.Dorwart RH, Genant HK, Johnston WH, Morris JM. Pigmented villonodular synovitis of synovial joints:Clinical, pathologic, and radiologic features. AJR Am J Roentgenol. 1984;143:877–85. doi: 10.2214/ajr.143.4.877. [DOI] [PubMed] [Google Scholar]
- 27.Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis:Radiologic-pathologic correlation. Radiographics. 2008;28:1493–518. doi: 10.1148/rg.285085134. [DOI] [PubMed] [Google Scholar]
- 28.Sharma H, Jane MJ, Reid R. Pigmented villonodular synovitis of the foot and ankle:Forty years of experience from the Scottish bone tumor registry. J Foot Ankle Surg. 2006;45:329–36. doi: 10.1053/j.jfas.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Narváez JA, Narváez J, Aguilera C, De Lama E, Portabella F. MR imaging of synovial tumors and tumor-like lesions. Eur Radiol. 2001;11:2549–60. doi: 10.1007/s003300000759. [DOI] [PubMed] [Google Scholar]
- 30.Bakotic BW, Borkowski P. Primary soft-tissue neoplasms of the foot:The clinicopathologic features of 401 cases. J Foot Ankle Surg. 2001;40:28–35. doi: 10.1016/s1067-2516(01)80038-7. [DOI] [PubMed] [Google Scholar]
- 31.Jelinek JS, Kransdorf MJ, Shmookler BM, Aboulafia AA, Malawer MM. Giant cell tumor of the tendon sheath:MR findings in nine cases. AJR Am J Roentgenol. 1994;162:919–22. doi: 10.2214/ajr.162.4.8141018. [DOI] [PubMed] [Google Scholar]
- 32.De Beuckeleer L, De Schepper A, De Belder F, Van Goethem J, Marques MC, Broeckx J, et al. Magnetic resonance imaging of localized giant cell tumour of the tendon sheath (MRI of localized GCTTS) Eur Radiol. 1997;7:198–201. doi: 10.1007/s003300050134. [DOI] [PubMed] [Google Scholar]
- 33.Ganguly A, Aniq H, Skiadas B. Lumps and bumps around the foot and ankle:An assessment of frequency with ultrasound and MRI. Skeletal Radiol. 2013;42:1051–60. doi: 10.1007/s00256-013-1575-x. [DOI] [PubMed] [Google Scholar]
- 34.Schatz J, Soper J, McCormack S, Healy M, Deady L, Brown W. Imaging of tumors in the ankle and foot. Top Magn Reson Imaging. 2010;21:37–50. doi: 10.1097/RMR.0b013e31820ef556. [DOI] [PubMed] [Google Scholar]
- 35.Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS. From the archives of the AFIP. Musculoskeletal angiomatous lesions:Radiologic-pathologic correlation. Radiographics. 1995;15:893–917. doi: 10.1148/radiographics.15.4.7569134. [DOI] [PubMed] [Google Scholar]
- 36.Suh JS, Hwang G, Hahn SB. Soft tissue hemangiomas:MR manifestations in 23 patients. Skeletal Radiol. 1994;23:621–5. doi: 10.1007/BF03372605. [DOI] [PubMed] [Google Scholar]
- 37.Mitsionis GI, Pakos EE, Kosta P, Batistatou A, Beris A. Intramuscular hemangioma of the foot:A case report and review of the literature. Foot Ankle Surg. 2010;16:e27–9. doi: 10.1016/j.fas.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 38.Scully SP, Temple HT, Harrelson JM. Synovial sarcoma of the foot and ankle. Clin Orthop Relat Res. 1999;364:220–6. doi: 10.1097/00003086-199907000-00028. [DOI] [PubMed] [Google Scholar]
- 39.Kransdorf MJ. Malignant soft-tissue tumors in a large referral population:Distribution of diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164:129–34. doi: 10.2214/ajr.164.1.7998525. [DOI] [PubMed] [Google Scholar]
- 40.Jones BC, Sundaram M, Kransdorf MJ. Synovial sarcoma:MR imaging findings in 34 patients. AJR Am J Roentgenol. 1993;161:827–30. doi: 10.2214/ajr.161.4.8396848. [DOI] [PubMed] [Google Scholar]
- 41.Nakanishi H, Araki N, Sawai Y, Kudawara I, Mano M, Ishiguro S, et al. Cystic synovial sarcomas:Imaging features with clinical and histopathologic correlation. Skeletal Radiol. 2003;32:701–7. doi: 10.1007/s00256-003-0690-5. [DOI] [PubMed] [Google Scholar]
- 42.Murphey MD, Gibson MS, Jennings BT, Crespo-Rodríguez AM, Fanburg-Smith J, Gajewski DA. From the archives of the AFIP:Imaging of synovial sarcoma with radiologic-pathologic correlation. Radiographics. 2006;26:1543–65. doi: 10.1148/rg.265065084. [DOI] [PubMed] [Google Scholar]
- 43.Wetzel LH, Levine E. Soft-tissue tumors of the foot:Value of MR imaging for specific diagnosis. AJR Am J Roentgenol. 1990;155:1025–30. doi: 10.2214/ajr.155.5.2120930. [DOI] [PubMed] [Google Scholar]
- 44.Waldt S, Rechl H, Rummeny EJ, Woertler K. Imaging of benign and malignant soft tissue masses of the foot. Eur Radiol. 2003;13:1125–36. doi: 10.1007/s00330-002-1604-y. [DOI] [PubMed] [Google Scholar]
- 45.De Beuckeleer LH, De Schepper AM, Vandevenne JE, Bloem JL, Davies AM, Oudkerk M, et al. MR imaging of clear cell sarcoma (malignant melanoma of the soft parts):A multicenter correlative MRI-pathology study of 21 cases and literature review. Skeletal Radiol. 2000;29:187–95. doi: 10.1007/s002560050592. [DOI] [PubMed] [Google Scholar]
- 46.Singer AD, Datir A, Tresley J, Langley T, Clifford PD, Jose J, et al. Benign and malignant tumors of the foot and ankle. Skeletal Radiol. 2016;45:287–305. doi: 10.1007/s00256-015-2278-2. [DOI] [PubMed] [Google Scholar]
- 47.Porter C, Vincetic A, Saleh ME, Goldstein H. Pigmented dermatofibrosarcoma protuberans of the foot with fibrosarcomatous changes:A review and case presentation. J Foot Ankle Surg. 2002;41:186–91. doi: 10.1016/s1067-2516(02)80070-9. [DOI] [PubMed] [Google Scholar]
- 48.Beaman FD, Kransdorf MJ, Andrews TR, Murphey MD, Arcara LK, Keeling JH. Superficial soft-tissue masses:Analysis, diagnosis, and differential considerations. Radiographics. 2007;27:509–23. doi: 10.1148/rg.272065082. [DOI] [PubMed] [Google Scholar]
- 49.Linda DD, Harish S, Alowami S, DeNardi F, Deheshi BM. Radiology-pathology conference:Cutaneous angiosarcoma of the leg. Clin Imaging. 2013;37:602–7. doi: 10.1016/j.clinimag.2012.08.005. [DOI] [PubMed] [Google Scholar]