Abstract
Background:
Cannabis dispensaries have proliferated exponentially in Oklahoma since the state legalized medical cannabis in 2018. Oklahoma is unique from many other legalized states given its high number of lower income, rural, and uninsured residents, who may seek medical cannabis as an alternative to traditional medical treatment.
Methods
This study examined demographic and neighborhood characteristics associated with dispensary density (n = 1,046 census tracts) in Oklahoma.
Results
Compared to census tracts with no dispensaries, those with at least one dispensary had a higher proportion of uninsured individuals living below the poverty level and a greater number of hospitals and pharmacies. Almost half (42.35%) of census tracts with at least one dispensary were classified as a rural locale. In fully adjusted models, percent uninsured, percent of household rentals, and the number of schools and pharmacies were positively associated with greater number of cannabis dispensaries, while the number of hospitals was negatively associated. In the best fitting interaction models, dispensaries were predominant in areas with a higher percentage of uninsured residents and no pharmacies, suggesting that cannabis retailers may capitalize on the health needs of communities with limited healthcare outlets or access to medical treatment.
Conclusions
Policies and regulatory actions that seek to decrease disparities in dispensary locations should be considered. Future studies should examine whether people living in communities with a scarcity of health resources are more likely to associate cannabis with medical uses than those living in communities with more resources.
Keywords: cannabis, dispensaries, census, location, demographics, poverty, Oklahoma, medical
As of October 2022, the majority (37) of states in the U.S. and the District of Columbia have legalized medical cannabis, resulting in a proliferation of medical cannabis dispensaries. The medical cannabis market is expected to raise billions of dollars to improve infrastructure, fund education, and provide jobs for hundreds of thousands of individuals (Decort et al 2020). Despite noted benefits to the economy, studies show that medical cannabis dispensaries cluster in disadvantaged neighborhoods that have higher rates of crime and lower income residents (Morrison et al. 2014; Unger et al. 2020).
Even historically “conservative” leaning states that have traditionally had a zero-tolerance policy about drug use have legalized medical cannabis. Oklahoma is one such conservative-leaning state that legalized medical cannabis in 2018, and has a relatively unique policy environment. First, Oklahoma is one of the few medical cannabis states that does not require a qualifying condition to obtain a medical cannabis license, and minors, in restricted cases, can obtain a license. Easy access to a medical cannabis license in Oklahoma is reflected by the number and proportion of Oklahomans that have been issued a medical cannabis license. As of March 2022, the Oklahoma Medical Marijuana Authority (OMMA) has issued 384,974 patient medical cannabis licenses, reflecting approximately 10% of the population of Oklahoma (Butcher, 2019). Second, the number of dispensaries has grown exponentially in Oklahoma, surpassing that in geographically larger states, like Colorado or California, which have allowed legal medical and recreational cannabis use for years (Keating, 2019). This is likely because, from 2018 to 2022, there was no limit on the number of dispensary licenses issued by the OMMA, [a two-year moratorium on new business licenses was issued in August 2022 (Oklahoma Medical Marijuana Authority, 2022b)] and costs associated with obtaining a dispensary license have been less expensive compared to other states (Americans for Safe Access, 2021). For example, dispensaries in Oklahoma pay between $2,500 and $10,000 in licensing fees (Oklahoma Medical Marijuana Authority, 2022a), based on annual sales; whereas in California, licensing fees can reach up to $96,000 annually (California Department of Cannabis Control, 2022). In Colorado, fees and permits for a medical cannabis store license can be close to $20,000 (Colorado Department of Revenue, 2022). There are also few regulations on where dispensaries can be located in Oklahoma, although sales are prohibited within 1,000 feet of a school (Oklahoma State Department of Health, 2020; Schroyer, 2021). The number of dispensaries in Oklahoma is greater than in any of the other 37 states that allow legal medical cannabis (2,378) and ranks second-highest in the U.S. for dispensaries per capita (15.6/100,000 residents) (Hutchinson and Ray, 2020).
Oklahoma has a high proportion of low- income, rural, uninsured, and medically vulnerable residents. Nearly 15% of Oklahoma’s population is not covered by public or private health insurance, compared to 9.2% nationally (United Health Foundation, 2021). Moreover, a third of Oklahomans live in a rural area, twice as high as the national average (Rural Health Information Hub, 2021). Oklahoma has few rural health clinics and federally qualified health centers outside of urbanized areas compared to other states (Rural Health Information Hub, 2021). Limited access to medical treatment in rural areas could mean that rural Oklahomans seek medical cannabis as an alternative to conventional treatment. Given their high number per capita, dispensaries may be more widely available than traditional medical treatment outlets (e.g., pharmacies, physicians). It may also be possible that those who are uninsured seek out medical cannabis as a form of treatment, as a dispensary visit is a lower-cost alternative to a physician or hospital visit.
Cannabis dispensary density has been associated with several health and safety outcomes in previous work (Boggess et al. 2014; Everson et al. 2019; Hust et al 2020; Liang and Shi, 2019; Shi et al. 2018). Studies show greater density and availability of medical cannabis dispensaries and recreational stores in areas with lower household incomes (Morrison et al., 2014 Shi et al., 2016), greater percent of racial/ethnic minorities (Hughes et al. 2020; Shi et al., 2016; Thomas and Freisthler, 2016a), and greater overall area deprivation (e.g., lower percent owner-occupied housing, higher percent living below poverty level, etc.) (Amiri et al. 2019). Cannabis retailer density has also been associated with increased risk of cannabis-related hospitalizations (Mair et al 2015; 2021), greater alcohol outlet density (Mair et al 2021; Subica et al. 2018) and alcohol use (Garcia et al. 2020), increases in DUI arrests (Hunt et al., 2018), and greater cannabis use frequency (Freisthler & Gruenewald, 2014). However, while some studies have shown increases in crime rate in the block and surrounding areas following the placement of cannabis dispensaries (Hughes et al., 2020; Subica et al., 2018), others have found decreases or no change in crime following the opening of a medical cannabis dispensary in that area (Zakrzewski et al 2020). Further, while most evidence suggests a positive impact of medical cannabis laws on reduction in opioid-related health consequences, some research shows an increase in opioid use disorder and overdose in areas that have a greater density of dispensaries (Freisthler et al. 2020; Liang and Shi, 2019). The links between medical cannabis outlet density and adverse health and safety outcomes remain unclear, and may differ by state.
Despite Oklahoma’s rapid proliferation of cannabis dispensary openings since 2018 (Butler, 2019; Cooper, 2020; Hutchinson & Ray, 2020), and the relatively robust associations between dispensary density and poor health and safety outcomes, questions remain as to whether there is an inequitable distribution of dispensaries across neighborhoods in Oklahoma, as has been demonstrated in other states (Amiri et al 2019; Freisthler et al. 2017; Galea et al. 2007; Kepple and Freisthler, 2012; Morrison et al. 2014; Shi et al. 2016; Subica et al., 2018; Thomas and Freisthler, 2016b). From previous work, dispensaries may be perceived as undesirable establishments that contribute to higher crime, greater health harms, and lower property values (Boggess et al., 2014; Contreras, 2017), but this may not be the case for Oklahoma, given the extremely high number of dispensaries across the state. This exploratory study examined factors associated with the number of cannabis dispensaries per census tract in Oklahoma. Factors included demographics capturing social vulnerability like lower socioeconomic status (SES), racial/ethnic minority status, lack of health insurance coverage, urbanicity, and neighborhood indicators of health (e.g., physician, pharmacy and hospital density, crime). We hypothesized positive associations between the number of cannabis dispensaries and lower SES, rurality, racial/ethnic minority status, lack of health insurance, and greater crime, as well as negative associations between the number of cannabis dispensaries and indicators of health. We also investigated whether associations between lower SES, racial/ethnic minority status, and lack of health insurance coverage with dispensaries would be more pronounced in rural than in urban locations and in areas with fewer healthcare outlets (e.g., pharmacies, hospitals, physicians).
METHODS
The unit of analysis was census tracts, and all census tracts in Oklahoma (n = 1,046) were included. The population size of a census tract ranged between 4 and 15,702, with a mean of 3,746 (SD 1,914) (United States Census Bureau, 2020). The outcome variable of interest was cannabis dispensary counts in each census tract.
Data Sources and Preparation
The list of licensed cannabis dispensary retailers was obtained online from OMMA on February 9, 2021 (Oklahoma Medical Marijuana Authority). An online search was performed for each dispensary to determine address (city, county, and ZIP code were provided on the licensing list) and whether they were open for business. Locations were de-duplicated using Microsoft Excel® de-duplication tool with address, city, and ZIP. There were 1,844 dispensaries listed in the database, 7.9% (n=146) were unable to be geo- located and were not included in our analysis, and 4.9% (n=90) were found to be duplicates. This produced a final list of 1,608 unique licensed cannabis dispensaries with identifiable locations throughout Oklahoma (Figure 1). Dispensaries were geocoded using ArcGIS (ArcMap, version 10.8.1; ESRI Inc., Redlands, CA). Data were spatially joined with census tracts to identify the census tracts with and without cannabis dispensaries, as well as population and neighborhood characteristics for each census tract.
Figure 1.
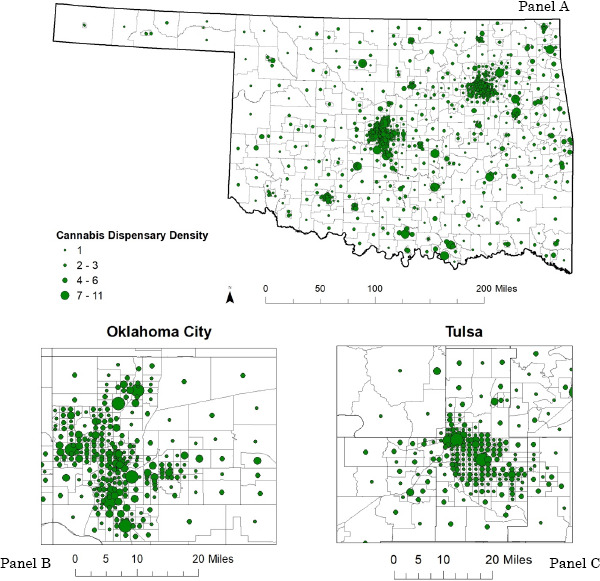
Cannabis dispensary count per census tracts in Oklahoma, 2021 (n=1,046) (panel A); Oklahoma City (panel B), and Tulsa (panel C).
Population Characteristics
The U.S. Census Bureau’s 2014-2018 American Community Survey (ACS) was used for demographic characteristics estimates. The following variables were included: total population, percent under age 18, race/ethnicity (percent Hispanic, non-Hispanic [NH] White, NH Black, NH Asian American, and NH American Indian/Alaska Native), percent living below the federal poverty level, percent unemployed, and percent uninsured. All data were analyzed using the percent of total collected for that variable. The percent of residents below the poverty is based on household income and the number of residents in the household. U.S. employment status includes those employed among the civilian population ages 16 and older. Insurance status included the whole population. ACS asked about private insurance (employer-based, direct-purchase, own employment- based, and TRICARE) and public coverage (Medicare), and means-tested health care (Medicaid, Children’s Health Insurance, state-specific plans, and VA Health care and CHAMPVA). Indian Health Services (IHS) coverage is not health insurance, and thus those with only IHS were considered uninsured. Each dispensary was joined to its census tract level U.S. Census ACS survey data, so that census tract was the unit of analysis.
Neighborhood Characteristics
Neighborhood characteristics included: location (e.g., city, suburb, town, rural), percent of vacant units, percent of household rentals, healthcare availability (i.e., number of hospitals, number of physicians, number of pharmacies), education availability (i.e., number of schools), and crime index. We used the National Center for Education Statistics (NCES) Education Demographic and Geographic Estimates Program (EDGE) Locale boundaries to categorize geographic areas based on U.S. Census Bureau designations (Geverdt, 2015). The NCES Locale boundaries were used because they are updated annually and because, in addition to urban and rural, suburbs and rural towns were included as both are unique populations and geographic locations in Oklahoma. NCES EDGE Locales includes the following four location categories: (1) City, located within a principal city or the largest city in a metropolitan (50,000 or more inhabitants) or a micropolitan (10,000 to 50,000 inhabitants) area; (2) Suburb, located outside a principal city but inside a metropolitan or micropolitan area; (3) Town, located inside an urban cluster (area of at least 2,500 and less than 50,000 inhabitants); and (4) Rural, located outside an urban area, urban cluster, and principal city (Geverdt, 2015). Vacant unit estimates were based on all households (rentals and owned). The ACS also includes information about homeownership status (rent or own) of each household, only for those occupied; for this study, we used the percent of households who rent.
The number of hospitals in each census tract was determined using ESRI ArcGIS online data (ArcGIS, 2020). Hospitals locations were based on the Homeland Infrastructure Foundation-Level Data (HIFLD) database downloaded from ArcGIS online (Homeland Infrastructure Foundation- Level Data et al., 2020). Physician count was determined by using the ESRI ArcGIS online data as well (ArcGIS Provider Practice Locations, American Association of Family Practitioners). For physician density, we included only allopathic and osteopathic physicians (family medicine, general practice, internal medicine, and pediatrics) but excluded emergency medicine, respiratory specialists, nurse practitioners, and physicians’ assistants. These data were based on the Center for Medicaid and Medicare Services (CMS) National Provider Identification (NPI) by Health Landscape from November 2020 and available on ESRI ArcGIS online. Pharmacy count was determined using the Healthcare Ready’s RX Open data from April 2020 and downloaded from ArcGIS online (Ready, 2020). Each facility was summed and analyzed by census tracts. The number of schools for each census tract was determined by using the ArcGIS Map Service. Education data originated from the National Center for Education Statistics (NCES) (ArcGIS & EDGE, 2020). To calculate the rate, we determined the count by summing all public schools (elementary, middle/junior high school, and high schools) by census tract. Schools were included in this study because dispensaries must be at least 1,000 feet from a school, and thus they play an important role in the determining the geography and neighborhood landscape of dispensaries.
Lastly, we used the crime index developed by Applied Geographic Solutions (AGS), which is based on FBI Uniform Crime Reports. These data use several years of crime reports from law enforcement jurisdictions across the U.S. We used the total crime rate for 2020 due to unstable numbers in many rural census tracts. These data have been shown to be a reliable choice for use in public health analysis (Nau et al., 2020).
Statistical Analysis
Geographic analyses were conducted in ArcMap 10.8 (ESRI, Redlands, CA), and all statistical analyses were conducted using SAS v.9.4 (SAS Institute, Cary, NC). Descriptive statistics were first used to examine the distribution of population and neighborhood characteristics for all census tracts and by the presence/absence of at least one dispensary in a census tract. Statistical differences were evaluated using logistic regression. Collinearity among all study variables was assessed (r2≥.80) during this stage. To assess spatial autocorrelation and test for residual spatial dependence, we performed a test for spatial autocorrelation (Moran’s I) on the residuals and they were not clustered (p = 0.91) (Waller and Gotway, 2004).
Using PROC GENMOD procedure, Poisson regression models were conducted to determine which population and neighborhood characteristics had a statistically significant effect on the outcome variable (number of cannabis dispensaries per census tract). To obtain the final model of the most significant explanatory variables, we used manual stepwise selection; a semi-automated process. Goodness-of-fit measures (e.g., Pearson statistic and deviance statistic) were used to compare model and to determine the best fitting model. Covariates that were statistically significant in the bivariate analysis (p≤0.1) using crude (unadjusted) Risk Ratios (RRs) were included in the model building. Next, two-way interaction terms of sociodemographic and neighborhood characteristics, specified a priori, were examined independently. If an interaction emerged, analyses were repeated with stratification, in order to explicate the interaction. If present among a continuous variable, sensitivity analyses were conducted to determine optimal categorization to simplify interpretation and, subsequently, practical public health implications.
Adjusted and unadjusted RRs and corresponding 95% Confidence Intervals (CIs) were calculated. A two-sided p-value of <0.05 was considered statistically significant. Given the exploratory nature of the study, adjustment for multiple comparisons was not made, as there was concern this may unduly increase type II error relative to type I error (Rothman, 1990).
RESULTS
Our study included 1,608 licensed cannabis dispensaries as of February 9, 2021. The number of dispensaries per census tract ranged from 0-11, with an average of 1.54 (SD 1.78) per tract. Descriptive statistics of population and neighborhood characteristics for all census tracts and by presence/absence of at least one dispensary are presented in Table 1. The majority (65.0%, n=680) of census tracts in Oklahoma had at least one dispensary, with more than half of the state’s population (68.9%, n= 2,700,187 individuals) living in those census tracts.
Table 1.
Population and Neighborhood-Level Characteristics of Census Tracts with and Without at Least One Cannabis Dispensary in Oklahoma (N=1,046 Census Tracts)
| TOTAL | Census Tracts with No Dispensaries | Census Tracts with ≥1 Dispensary | |||||
|---|---|---|---|---|---|---|---|
| Mean | ±SD | Mean ±SD | Mean ±SD | p-value | |||
| Census Tracts, n (%) | 1046 | 366 | 34.99% | 680 | 65.00%) | ||
| Population, n (%) | 3,918,137 | 1,217,950 | 31.08% | 2,700,187 | (68.92%) | <.0001 | |
| Population Characteristics (%) | |||||||
| Under 18 years of age | 23.87% | 5.87% | 23.76% | 5.88% | 23.93% | 5.88% | 0.304 |
| White, NH | 71.47% | 15.43% | 71.36% | 16.89% | 71.53% | 14.59% | 0.499 |
| Black, NH | 8.62% | 14.16% | 9.20% | 16.39% | 8.32% | 12.81% | 0.251 |
| AI/AN, NH | 7.33% | 7.23% | 7.34% | 7.21% | 7.33% | 7.26% | 0.850 |
| Asian, NH | 1.92% | 3.21% | 1.95% | 3.36% | 1.91% | 3.13% | 0.339 |
| Hispanic | 10.88% | 13.05% | 9.68% | 11.66% | 11.52% | 13.70% | 0.613 |
| Below Poverty | 17.52% | 11.42% | 16.01% | 11.22% | 18.33% | 11.46% | 0.028 |
| Unemployed | 19.35% | 25.26% | 19.42% | 26.00% | 19.31% | 24.89% | 0.637 |
| Uninsured | 17.49% | 08.29% | 16.12% | 8.14% | 18.22% | 8.27% | <.0001 |
| Neighborhood Characteristics | |||||||
| Location Type, n (%) | 0.012 | ||||||
| Rural | 471 | 45.03% | 183 | 50.00% | 288 | 42.35% | |
| Suburban | 157 | 15.01% | 51 | 13.93% | 106 | 15.59% | |
| Town | 104 | 9.94% | 26 | 7.10% | 78 | 11.47% | |
| City | 314 | 30.02% | 106 | 28.96% | 208 | 30.59% | |
| Percent Vacant Units | 14.78% | 9.02% | 14.73% | 9.91% | 14.80% | 8.51% | 0.901 |
| Percent Household Rentals | 35.58% | 20.38% | 30.98% | 21.15% | 38.05% | 19.53% | <.0001 |
| No. Hospitals (n=163) | 0.16 | 0.43 | 0.12 | 0.39 | 0.18 | 0.45 | 0.033 |
| No. Physicians (n=4148) | 3.97 | 16.47 | 4.48 | 24.65 | 3.69 | 9.52 | 0.382 |
| No. Pharmacies (n=813) | 0.78 | 1.08 | 0.43 | 0.75 | 0.97 | 1.18 | <.0001 |
| No. Schools (n=1827) | 1.75 | 1.71 | 1.60 | 1.68 | 1.83 | 1.72 | 0.093 |
| Total Crime Rate | 0.153 | 0.5676 | 0.1850 | 0.9257 | 0.1358 | 0.1853 | 0.183 |
Note. <SD= Standard deviation;NH= non-Hispanic; AI/AN= American Indian/Alaskan Native; No.= Number.
Logistic regression models showed a higher percentage of individuals living below poverty (18.3% vs. 16.0%) and uninsured individuals (18.2% vs. 16.1%) residing in census tracts with at least one dispensary compared to those census tracts without a dispensary (p’s <0.05). There were significant differences among census tracts with and without a dispensary by location type (p=0.01). Compared to census tracts with no dispensaries, census tracts with at least one dispensary were more likely to be in a suburban area (15.6% vs. 13.9%), a town (11.5% vs. 7.1%), or a city (30.6% vs. 29.0%), and less likely to be in rural areas (42.4% vs. 50.0%). Notably, nearly half (42.4%) of census tracts with a dispensary were rural. The average number of hospitals (0.12 vs. 0.18), pharmacies (0.43 vs. 0.97), and schools (1.60 vs. 1.83) was higher in census tracts with at least one cannabis dispensary compared to census tracts with no dispensaries (p’s <0.05).
Step 1 of Poisson regression models (Table 2) shows the associations of population characteristics with census tracts with and without cannabis dispensaries and Step 2 shows the association of population characteristics that were significant in Step 1 and neighborhood characteristics of census tracts with and without dispensaries. The following variables were statistically significant in the bivariate analyses (crude RRs) and considered in Step 1: percentage under 18 years of age (p=0.03), percentage Hispanic (p=0.02), percentage living below poverty (p<.01), and percentage uninsured (p<.01). Percentage Hispanic was not significant after adjusting for these factors. The following variables were statistically significant in the bivariate analyses and were considered in Step 2: location type (p<.01), percentage of rental households (p<.01), hospital count (p <.01), school count (p=0.01), and pharmacy count (p<.01). Only percent uninsured remained significant (p<0.01) when including significant neighborhood characteristics with the population factors that emerged significant from Step 1.
Table 2.
Risk Ratios (RR) from Poisson Regression Models Predicting Cannabis Dispensary Count Per Census Tracts (n = 1,046)
| Step 1, population characteristics a | Step 2 neighborhood characteristics b | |||||
|---|---|---|---|---|---|---|
| Crude RR (95% CI) | p-value | aRR (95% CI) | p-value | aRR (95% CI) | p-value | |
| Population Characteristics (%) | ||||||
| Under 18 years of age | 0.41 (0.18, 0.94) | 0.03 | 0.35 (0.15, 0.83) | 0.02 | 0.66 (0.29, 1.51) | 0.32 |
| White, NH | 0.95 (0.70, 1.31) | 0.77 | - | - | - | - |
| Black, NH | 0.78 (0.54, 1.12) | 0.17 | - | - | - | - |
| AI/AN, NH | 1.55 (0.80, 2.97) | 0.20 | - | - | - | - |
| Asian, NH | 0.67 (0.14, 3.19) | 0.62 | - | - | - | - |
| Hispanic | 1.52 (1.08, 2.15) | 0.02 | 1.14 (0.74, 1.76) | 0.54 | - | - |
| Living Below Poverty | 3.97 (2.72, 5.80) | <.01 | 2.77 (1.72, 4.48) | <.01 | 1.19 (0.65, 2.18) | 0.57 |
| Unemployed | 0.96 (0.78, 1.18) | 0.69 | - | - | - | - |
| Uninsured | 5.26 (3.01, 9.17) | <.01 | 2.11 (1.03, 4.29) | 0.04 | 3.41 (1.66, 7.01) | <.01 |
| Neighborhood Characteristics | ||||||
| Location Type, (%) | <.01 | - | - | <.01 | ||
| Rural | 0.76 (0.66, 0.87) | - | - | 0.90 (0.76, 1.05) | ||
| Suburban | REF | - | - | REF | ||
| Town | 1.28 (1.07, 1.52) | - | - | 1.03 (0.86, 1.23) | ||
| City | 0.81 (0.70, 0.94) | - | - | 0.79 (0.68, 0.92) | ||
| Percent Vacant Units | 1.27 (0.75, 2.17) | 0.38 | - | - | - | - |
| Percent Rental Households | 3.25 (2.61, 4.04) | <.01 | - | - | 2.64 (1.85, 3.77) | <.01 |
| No. Hospital | 1.32 (1.20, 1.45) | <.01 | - | - | 0.89 (0.80, 1.00) | 0.04 |
| No. Physician | 1.00 (1.00, 1.00) | 0.35 | - | - | - | - |
| No. School | 1.04 (1.01, 1.06) | 0.02 | - | - | 1.05 (1.02, 1.08) | <.01 |
| No. Pharmacy | 1.32 (1.27, 1.36) | <.01 | - | - | 1.29 (1.24, 1.35) | <.01 |
| Total Crime Rate | 0.97 (0.88, 1.08) | 0.55 | - | - | - | - |
Note. RR= risk ratio; aRR=adjusted risk ratio; NH= non-Hispanic; No. = Number.
controlled for: Under 18, Hispanic, living below poverty, and uninsured.
controlled for: Under 18, uninsured, location type, household renters, hospital count, physician count, and pharmacy count.
Statistical interactions (Table 3) were found between: percentage Hispanic and percentage living below poverty (pinteraction<0.01); percentage uninsured and percentage living below poverty (pinteraction=0.01); physician count and location type (pinteraction<.01); pharmacy count and location type (pinteraction<.01); and pharmacy count and percentage of rental households (pinteraction<.01).
Table 3.
Interactions of Population and Neighborhood Factors on Cannabis Dispensary Count Per Census Tracts
| Predictors | Variable 1: Main Effect | Variable 2: Main Effect | Joint Effects | |||
|---|---|---|---|---|---|---|
| Estimate | p-value | Estimate | p-value | Estimate | p-value | |
| Location Type X Per. Below Poverty | Location Coeffs= City: -0.21 Rural: -0.42 Town: -0.01 |
<.01 | Poverty Coeff= 1.23 |
<.01 | City: -0.37 Rural: 0.76 Town: 0.65 |
0.13 |
|
Hispanic X
Per. Below Poverty |
Hispanic Coeff = 1.26 |
<.01 | Poverty Coeff= 1.83 |
<.01 | -4.35 | <.01 |
|
Per. Uninsured X
Per. Below Poverty |
Uninsured Coeff = 1.70 |
<.01 | Poverty Coeff = 1.77 |
<.01 | -3.56 | 0.01 |
| No. Pharmacies X Per. Below Poverty | Pharmacy Coeff = 0.24 | <.01 | Poverty Coeff = 1.39 |
<.01 | 0.21 | 0.18 |
| Location Type X No. Physician | Location Coeff = City: -0.18 Rural: -0.38 Town: 0.24 |
<.01 | Physician Coeff = 0.00 | <.01 | City: -0.01 Rural: 0.04 Town: 0.00 |
<.01 |
| Location Type X Per. Uninsured | Location Coeff= City: -0.29 Rural:-0.28 Town: -0.12 |
0.18 | Uninsured Coeff = 1.87 |
<.01 | City: -0.10 Rural: -0.38 Town: 1.29 |
0.56 |
| Location Type X No. Pharmacies | Location Coeff = City: -0.11 Rural:-0.51 Town: 0.09 | <.01 | Pharmacy Coeff = 0.14 | <.01 | City: -0.04 Rural:0.31 Town: 0.07 | <.01 |
|
No. Pharmacies X Per.
Rentals |
Pharmacy Coeff = 0.43 | <.01 | Rentals Coeff = 1.37 |
<.01 | -0.39 | <.01 |
Note. No.= Number; Per = percent; Coeffs = coefficients. Reference group for location type = Suburban.
Due to significant evidence of effect modification on a multiplicative scale for pharmacy count, the final model was repeated with stratification on the presence/absence of pharmacies in the census tract (Table 4) (Knol & VanderWeel, 2012). There were an average of 1.02 (SD 1.38) dispensaries in census tracts with no pharmacies, and an average of 2.11 (SD 2.00) dispensaries in census tracts with at least one pharmacy. Stratification by the presence of pharmacies revealed that the positive association between percent uninsured and census tracts with cannabis dispensaries was restricted to only census tracts without pharmacies (aRR: 7.81, 95% CI: 3.10, 19.64, p<.01). The positive association between location type and census tracks with a cannabis dispensary was restricted to only census tracts with at least one pharmacy (Rural aRR: 1.17, 95% CI: 0.98, 1.39; Town aRR: 1.27, 95% CI: 1.04, 1.55; aRR: 0.71, 95% CI: 0.59, 0.86; all p’s<.01). A post-hoc analysis showed that census tracts with no pharmacies had a higher percentage of uninsured residents (18.04% vs. 16.85%) and percentage of individuals living below the poverty level (18.14 vs. 16.80) compared to census tracts with at least one pharmacy. Census tracts with at least one pharmacy also had a higher number of hospitals (0.28 vs. 0.05), schools (1.96 vs. 1.60), and dispensaries (2.11 vs. 1.04).
Table 4.
Adjusted Risk Ratio (aRR) of Cannabis Dispensary Count Per Census Tracts Stratified by Presence/Absence of a Pharmacy
| Total (n=1,046 census tracts) | Stratum 1: No Pharmacies (n=560 census tracts) | Stratum 2: >1 Pharmacies (n=486 census tracts) | ||||
|---|---|---|---|---|---|---|
| aRR (95% CI) | p-value | aRR (95% CI) | p-value | aRR (95% CI) | p-value | |
| Per. Uninsured | 2.85 (1.57, 5.17) | <.01 | 7.81 (3.10, 19.64) | <.01 | 1.63 (0.71, 3.74) | 0.24 |
| Per. Rentals | 3.32 (2.54, 4.33) | <.01 | 2.54 (1.65, 3.90) | <.01 | 3.16 (2.16, 4.63) | <.01 |
| Location Type | <.01 | 0.06 | <.01 | |||
| Rural | 0.87 (0.75, 1.01) | 0.70 (0.53, 0.93) | 1.17 (0.98, 1.39) | |||
| Suburban | REF | REF | REF | |||
| Town | 1.13 (0.95, 1.35) | 0.93 (0.65, 1.34) | 1.27 (1.04, 1.55) | |||
| City | 0.68 (0.58, 0.79) | 0.78 (0.58, 1.05) | 0.71 (0.59, 0.86) | |||
Note. aRR = adjusted risk ratio; Per.= percent.
DISCUSSION
Our study found that most census tracts in Oklahoma had at least one licensed dispensary. From bivariate models, census tracts with at least one dispensary had a significantly greater percentage of residents who were Hispanic, living below the poverty level, and uninsured, consistent with previous work published on data from other states (Morrison et al., 2014; Novak et al., 2020; Shi et al., 2016). In these bivariate models, the likelihood of living in a census tract with a dispensary was 52% higher among Hispanic than non-Hispanic residents, and 3-5 times higher among uninsured and low SES individuals. Race was unrelated to dispensary density. It could be that the associations among sociodemographics, census tracts, and dispensaries are better accounted for by lower income and lack of health insurance rather than race, as these factors emerged as significant correlates of census tracts with and without dispensaries in adjusted risk ratio models.
At the neighborhood level, bivariate analysis showed that nearly half of the census tracts with cannabis dispensaries were in rural areas. Notably, just over a third of Oklahomans live in a rural area (Rural Health Information Hub, 2021). The availability of dispensaries in rural areas suggests that many Oklahomans have easy access to medical cannabis. Valencia and colleagues (2017) conducted a systematic review of the structural barriers to accessing medical cannabis, but urbanicity was not examined, thus our findings add to the literature. Finally, in both crude and adjusted models, results showed that hospitals, pharmacies, schools, and rental units were more prevalent in census tracts with at least one dispensary than among those without a dispensary. This may be because of the high concentration of dispensaries in cities and suburban areas, or higher population density in these areas that creates greater demand. Crime was unrelated to dispensary density, inconsistent with previous research (Boggess et al., 2014; Contreras, 2017; Freisthler et al., 2017).
The association of certain sociodemographic factors with cannabis dispensaries differed by the presence or absence of pharmacies in those census tracts, in fully adjusted interaction models. To our knowledge, this is the first study to examine the relationship between cannabis dispensary location and healthcare availability (e.g., pharmacies, hospitals, physicians). Our findings are consistent with a recent systematic review of correlates of geographical accessibility of pharmacies, which found lower pharmacy accessibility in low-income populations and rural areas (Jagadeesan and Wirtz, 2021). Other work has found that dispensaries are spatially related to market potential (Morrison et al 2014). As such, our results suggest that, in Oklahoma, dispensaries may be situated in areas where there are limited healthcare outlets, and in doing so, allow residents to access dispensaries as alternatives to conventional medical treatment. This partially supports our hypothesis that census tracts with lower income and rural locales would be more likely to have a dispensary, as retailers may benefit from the demand for accessible and affordable alternatives to medical treatment in these remote, and, in some cases, under-served locations. The hypothesis that dispensaries might serve as an alternate point for healthcare access should be explored in future research. Other reasons that may drive dispensaries to certain locations were not examined in the study but should be in future studies, include rent/real estate costs, zoning, and social acceptability of cannabis use. Further research is needed to examine the complex relationships among cannabis dispensary density, pharmacy availability, housing tenure and costs, resident insurance coverage, and attitudes about cannabis use. Qualitative studies could examine how residents of areas with high dispensary density perceive and interact with cannabis retail outlets, whether or not residents are using cannabis as an alternative to conventional health care services, and why.
This study had several limitations. First, conclusions cannot be drawn regarding causation, as we did not investigate change over time. Given that the medical cannabis industry in Oklahoma is relatively new, there may be a lag-time associated with the passing of policies, their implementation, and an assessment of the impact. (Hudson et al., 2019). Second, while census tracts are often used as a proxy for neighborhoods in public health research, these areas are not homogeneous, and relationships observed at one level of aggregation may not persist using different spatial units, such as ZIP codes or U.S. Census block groups. Third, while data were not temporally homogenous, they were assessed close in time and we do not believe this significantly impacted the outcomes. Fourth, policy changes in Oklahoma may impact these associations over time. Oklahoma issued up to a two year moratorium on new business licenses, which could impact density. Finally, we did not adjust for multiple comparisons, following recommendations by Rothman. While Type I error rate is possible, such adjustments also increase the likelihood of Type II error rate and thus spurious results (Rothman, 1990).
Conclusions
Results confirm an inequitable distribution of cannabis dispensaries by population and neighborhood demographics in Oklahoma. Higher dispensary density was associated with a greater proportion of uninsured and low income individuals in those areas, which suggests that dispensaries could serve as an alternative access point for healthcare needs for individuals who may have other barriers to accessing traditional healthcare. Even if dispensaries may partially address health needs of individuals living in these areas, disparities in dispensary location could lead to greater social and economic consequences (Kong et al., 2019, 2020; Loomis et al., 2013; Rodriguez et al., 2013). Understanding how Oklahoma’s dispensary distribution is related to population demographics provides valuable information for other states looking to legalize cannabis in the future.
Funding and Acknowledgements:
AMC was supported in part by the University of Oklahoma Health Sciences Center, Oklahoma Tobacco Settlement Endowment Trust (TSET) contract # R22-02 and NCI grant P30CA2255520 awarded to the Stephenson Cancer Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. JC was partially funded by National Institute of General Medical Sciences, Grant/Award Number: U5GM104938 and in part by the National Cancer Institute Cancer Center Support Grant P30CA225520 awarded to the University of Oklahoma Stephenson Cancer Center for use of the Biostatistics and Research Design Shared Resources.
REFERENCES
- Americans for Safe Access. (2021). State of the States Report: An analysis of medical cannabis access in the Unites States. https://www.safeaccessnow.org/sos#:~:text=Each%20year%2C%20Americans%20for%20Safe,cannabis%20programs%20across%20the%20country.
- Amiri, S., Monsivais, P., McDonell, M. G., & Amram, O. (2019). Availability of licensed cannabis businesses in relation to area deprivation in Washington state: A spatiotemporal analysis of cannabis business presence between 2014 and 2017. Drug and Alcohol Review, 38(7), 790–797. [DOI] [PubMed] [Google Scholar]
- Applied Geographic Solutions. (2020). https://www.appliedgeographic.com/files/Snapsite2016A_Documents/AGS%20CrimeRisk%202016A%20Methodology.pdf
- Boggess, L. N., Pérez, D. M., Cope, K., Root, C., & Stretesky, P. B. (2014). Do medical marijuana centers behave like locally undesirable land uses? Implications for the geography of health and environmental justice. Urban Geography, 35(3), 315–336. [Google Scholar]
- Butcher, K. (2019, October 19). 200K medical marijuana patient applications approved in Oklahoma, officials say: https://kfor.com/2019/10/09/200k-medical-marijuana-patient-applications-approved-in-oklahoma-officials-say. KFOR: Oklahoma News 4. https://kfor.com/2019/10/09/200k-medical-marijuana-patient-applications-approved-in-oklahoma-officials-say [Google Scholar]
- Butler, T. (2019, September 6, 2019). Oklahoma ranks as fastest growing marijuana market in the country. Fox 25. https://okcfox.com/news/local/oklahoma-ranks-as-fastest-growing-marijuana-market-in-the-country [Google Scholar]
- California Department of Cannabis Control. (2022). Application and license fees. https://cannabis.ca.gov/applicants/application-license-fees/
- Colorado Department of Revenue. (2022). Marijuana Enforcement Division (MED) Marijuana Regulation Business License Application. https://sbg.colorado.gov/med/new-regulated-marijuana-business-license-application
- Contreras, C. (2017). A block-level analysis of medical marijuana dispensaries and crime in the city of Los Angeles. Justice Quarterly, 34(6), 1069–1095. [Google Scholar]
- Cooper, J. (2020, February 18, 2020). Oklahoma has the 2nd highest number of marijuana dispensaries per capita. Oklahoma's Own News on 6. https://www.newson6.com/story/5e6279d7cd4aa89d1b92f272/oklahoma-has-the-2nd-highest-number-of-marijuana-dispensaries-per-capita [Google Scholar]
- Decorte, T., Lenton, S., & Wilkins, C. (2020). Legalizing cannabis: experiences, lessons and scenarios. Routledge. [Google Scholar]
- Esri ArcGIS. (2020). Hospitals Locations Homeland Infrastructure Foundation-Level Data (HIFLD). https://services1.arcgis.com/Hp6G80Pky0om7QvQ/arcgis/rest/services/Hospitals_1/FeatureServer [Google Scholar]
- Esri ArcGIS & National Center for Education Statistics EDGE. (2020). Public School Locations-Current Homeland Infrastructure Foundation-Level Data (HIFLD). https://services1.arcgis.com/Ua5sjt3LWTPigjyD/arcgis/rest/services/Public_School_Location_201819/FeatureServer [Google Scholar]
- Everson, E. M., Dilley, J. A., Maher, J. E., & Mack, C. E. (2019). Post-Legalization Opening of Retail Cannabis Stores and Adult Cannabis Use in Washington State, 2009– 2016. American Journal of Public Health, 109, 1294–1301. 10.2105/AJPH.2019.305191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler, B., Gaidus, A., Tam, C., Ponicki, W. R., & Gruenewald, P. J. (2017). From medical to recreational marijuana sales: marijuana outlets and crime in an era of changing marijuana legislation. The Journal of Primary Prevention, 38(3), 249–263. https://link.springer.com/content/pdf/10.1007/s10935-017-0472-9.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler, B., & Gruenewald, P. J. (2014). Examining the relationship between the physical availability of medical marijuana and marijuana use across fifty California cities. Drug and Alcohol Dependence, 143, 244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freisthler, B., Sumetsky, N., Kranich, C., Chadwick, C., & Mair, C. (2020). Opioid Misuse and the Availability of Medical Marijuana Through Dispensaries. Journal of studies on alcohol and drugs, 81(4), 489–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea, S., Ahern, J., Tracy, M., & Vlahov, D. (2007). Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. American Journal of Preventive Medicine, 32(6), S195-S202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Ramírez, G., Paschall, M. J., & Grube, J.W. (2020). Retail Availability of Recreational Marijuana and Alcohol in Oregon Counties and Co-Use of Alcohol and Marijuana and Related Beliefs among Adolescents. Substance Use and Misuse, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geverdt, D. E. (2015). Education Demographic and Geographic Estimates Program (EDGE): Locale Boundaries User's Manual. NCES 2016-012 (National Center for Education Statistics, Issue. [Google Scholar]
- Homeland Infrastructure Foundation-Level Data, Oak Ridge National Laboratory, National Geospatial-Intelligence Agency, & Team, H. S. I. P. (2020). Hospitals https://gii.dhs.gov/HIFLD [Google Scholar]
- Hudson, B., Hunter, D., & Peckham, S. (2019). Policy failure and the policy-implementation gap: can policy support programs help? Policy Design and Practice, 2(1), 1–14. 10.1080/25741292.2018.1540378 [DOI] [Google Scholar]
- Hughes, L. A., Schaible, L. M., & Jimmerson, K. (2020). Marijuana dispensaries and neighborhood crime and disorder in Denver, Colorado. Justice Quarterly, 37(3), 461–485. [Google Scholar]
- Hunt, P., Pacula, R. L., & Weinberger, G. (2018). High on crime? Exploring the effects of marijuana dispensary laws on crime in California counties. IZA Institute of Labor Economics, Discussion Paper Series. [Google Scholar]
- Hust, S. J. T., Willoughby, J. F., Li, J., & Couto, L. (2020). Youth’s Proximity to Marijuana Retailers and Advertisements: Factors Associated with Washington State Adolescents’ Intentions to Use Marijuana. Journal of Health Communication, 25, 594–603. 10.1080/10810730.2020.1825568 [DOI] [PubMed] [Google Scholar]
- Hutchinson, D., & Ray, R. (2020). Oklahoma leads nationa in number of cannabis dispensaries. KGOU News. https://www.kgou.org/post/oklahoma-leads-nation-number-cannabis-dispensaries [Google Scholar]
- Jagadeesan, C. T., & Wirtz, V. J. (2021). Geographical accessibility of medicines: a systematic literature review of pharmacy mapping. Journal of pharmaceutical policy and practice, 14(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keating, E. (2019). Which state has the most licensed cannabis dispensaries? The answer may surprise you. Cannabiz Media. Retrieved December 16 from https://cannabiz.media/which-state-has-the-most-licensed-cannabis-dispensaries-the-answer-may-surprise-you/ [Google Scholar]
- Kepple, N. J., & Freisthler, B. (2012). Exploring the ecological association between crime and medical marijuana dispensaries. Journal of Studies on Alcohol and Drugs, 73(4), 523–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knol, M. J., & VanderWeele, T. J. (2012). Recommendations for presenting analyses of effect modification and interaction. International Journal of Epidemiology, 41(2), 514–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong, A. Y., Delamater, P. L., Gottfredson, N. C., Ribisl, K. M., Baggett, C. D., & Golden, S. D. (2021). Sociodemographic inequities in tobacco retailer density: Do neighboring places matter? Health & Place, 71, 102653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong, A. Y., Myers, A. E., Isgett, L. F., & Ribisl, K. M. (2019). Neighborhood racial, ethnic, and income disparities in accessibility to multiple tobacco retailers: Mecklenburg County, North Carolina, 2015. Preventive Medicine Reports, 17, 101031–101031. 10.1016/j.pmedr.2019.101031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, D., & Shi, Y. (2019). The associations of neighborhood availability of marijuana dispensaries and DATA-2000 waivered providers with hospital stays related to opioids. Substance Use and Misuse, 54(14), 2387–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomis, B., Kim, A., Goetz, J., & Juster, H. (2013). Density of tobacco retailers and its association with sociodemographic characteristics of communities across New York. Public Health, 127(4), 333–338. [DOI] [PubMed] [Google Scholar]
- Mair, C., Freisthler, B., Ponicki, W. R., & Gaidus, A. (2015). The impacts of marijuana dispensary density and neighborhood ecology on marijuana abuse and dependence. Drug and Alcohol Dependence, 154, 111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair, C., Sumetsky, N., Kranich, C., & Freisthler, B. (2021). Availability of medical cannabis dispensaries and cannabis abuse/dependence-related hospitalizations in California. Addiction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison, C., Gruenewald, P. J., Freisthler, B., Ponicki, W. R., & Remer, L. G. (2014). The economic geography of medical cannabis dispensaries in California. International Journal of Drug Policy, 25(3), 508–515. 10.1016/j.drugpo.2013.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison, C., Gruenewald, P. J., Freisthler, B., Ponicki, W. R., & Remer, L. G. (2014). The economic geography of medical cannabis dispensaries in California. International Journal of Drug Policy, 25(3), 508–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nau, C., Sidell, M., Clift, K., Koebnick, C., Desai, J., & Rohm-Young, D. (2020). A commercially available crime index may be a reliable alternative to actual census-tract crime in an urban area. Preventive Medicine Reports, 17, 100996. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6909353/pdf/main.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak, P., Sanmartin, M. X., & Ali, M. M. (2020). Geolocation of Maryland Medical Marijuana Dispensaries by Community Income and Racial Characteristics: An Ecological Design. Substance Use and Misuse, 1–9. [DOI] [PubMed] [Google Scholar]
- Oklahoma Medical Marijuana Authority. https://oklahoma.gov/content/dam/ok/en/omma/docs/business-lists/omma_dispensaries_list.pdf
- Oklahoma Medical Marijuana Authority. (2022a). Commercial Licenses. https://oklahoma.gov/omma/businesses/commercial-licenses.html
- Oklahoma Medical Marijuana Authority. (2022b). Moratorium Begins Aug. 1 [2022] for New Grower, Dispensary and Processor License Applications. Retrieved October 20 from https://oklahoma.gov/omma/about/news/2022/ moratorium-begins-aug-1-for-new-grower-dispensary-and-processor-license-applications.html
- Oklahoma State Department of Health. (2020). Title 310. Oklahoma State Department of Health Chapter 681. Medical Marijuana Regulations. In (pp. 38).
- Ready, H. (2020). Open Pharmacies-Rx Open https://rxopen.org/ [Google Scholar]
- Rodriguez, D., Carlos, H. A., Adachi-Mejia, A. M., Berke, E. M., & Sargent, J. D. (2013). [Google Scholar]
- Predictors of tobacco outlet density nationwide: a geographic analysis. Tobacco Control, 22(5), 349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman, K. J. (1990). No adjustments are needed for multiple comparisons. Epidemiology, 43–46. [PubMed] [Google Scholar]
- Rural Health Information Hub. (2021).Oklahoma Health. Retrieved March 10 from https://www.ruralhealthinfo.org/states/oklahoma
- Schroyer, J. (2021). Why red Oklahoma is home to a booming medical marijuana market MJBizDaily. Retrieved September 10 from https://mjbizdaily.com/why-red-oklahoma-is-home-to-a-booming-medical-marijuana-market/ [Google Scholar]
- Shi, Y., Cummins, S. E., & Zhu, S.-H. (2018). Medical marijuana availability, price, and product variety, and adolescents' marijuana use. Journal of Adolescent Health, 63(1), 88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, Y., Meseck, K., & Jankowska, M. M. (2016). Availability of medical and recreational marijuana stores and neighborhood characteristics in Colorado. Journal of Addiction, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subica, A. M., Douglas, J. A., Kepple, N. J., Villanueva, S., & Grills, C. T. (2018). The geography of crime and violence surrounding tobacco shops, medical marijuana dispensaries, and off-sale alcohol outlets in a large, urban low-income community of color. Preventive Medicine, 108, 8–16. [DOI] [PubMed] [Google Scholar]
- Thomas, C., & Freisthler, B. (2016b). Examining the locations of medical marijuana dispensaries in Los Angeles. Drug and Alcohol Review, 35(3), 334–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger, J. B., Vos, R. O., Wu, J. S., Hardaway, K., Sarain, A. Y. L., Soto, D. W., Rogers, C., & Steinberg, J. (2020). Locations of licensed and unlicensed cannabis retailers in California: A threat to health equity? Preventive Medicine Reports, 19, 101165. 10.1016/j.pmedr.2020.101165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Health Foundation. (2021). America's Health Rankings Annual Report. Retrieved October 13 from https://www.americashealthrankings.org/explore/annual/measure/HealthInsurance/state/OK
- United States Census Bureau. (2020). TIGER/Line with Selected Demographic and Economic Data Oklahoma Census Tract 2013-2017. United States Census Bureau. Retrieved 02/11/2021 from https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-data.html
- Valencia, C. I., Asaolu, I. O., Ehiri, J. E., & Rosales, C. (2017). Structural barriers in access to medical marijuana in the USA-a systematic review protocol. Systematic Reviews, 6(1), 154–154. 10.1186/s13643-017-0541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller, L. A., & Gotway, C. A. (2004). Applied spatial statistics for public health data John Wiley & Sons [Google Scholar]
- Zakrzewski Jr, W. J., Wheeler, A. P., & Thompson, A. J. (2020). Cannabis in the capital: exploring the spatial association between medical marijuana dispensaries and crime. Journal of Crime and Justice, 43(1), 1–15. [Google Scholar]


