Abstract
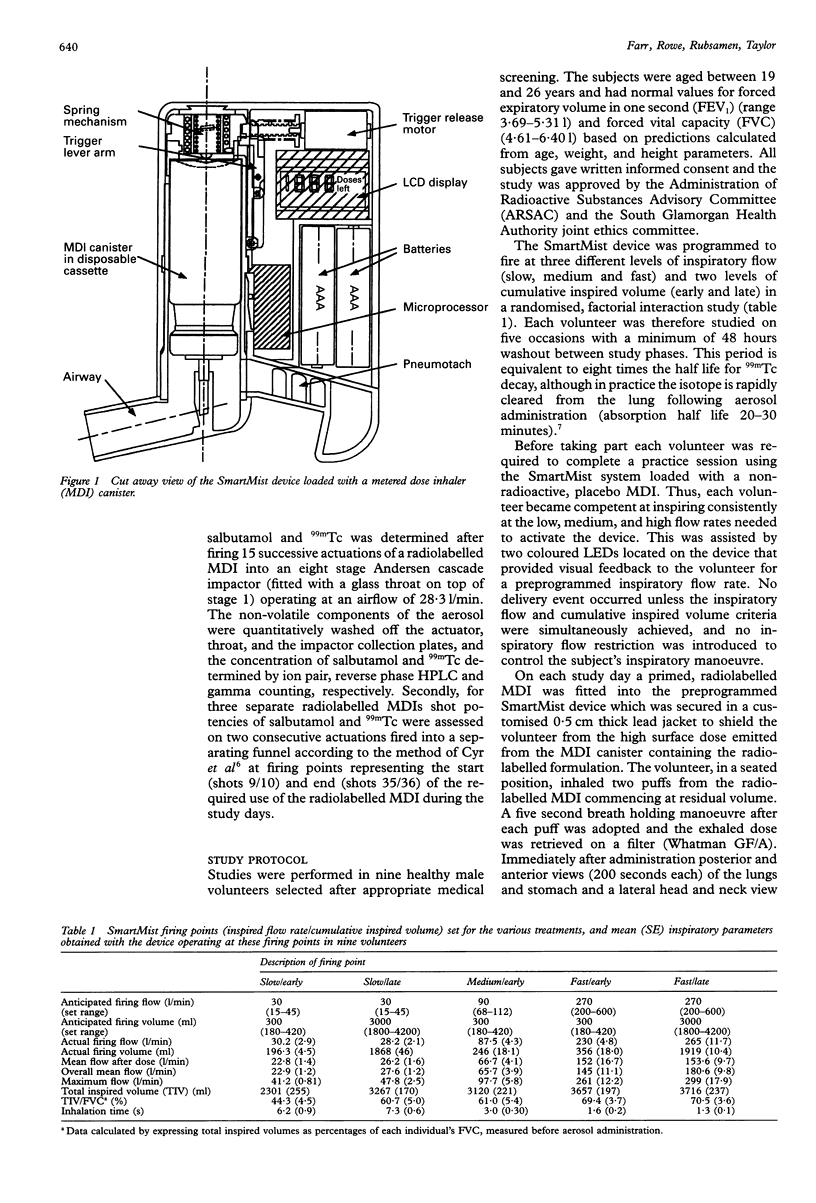
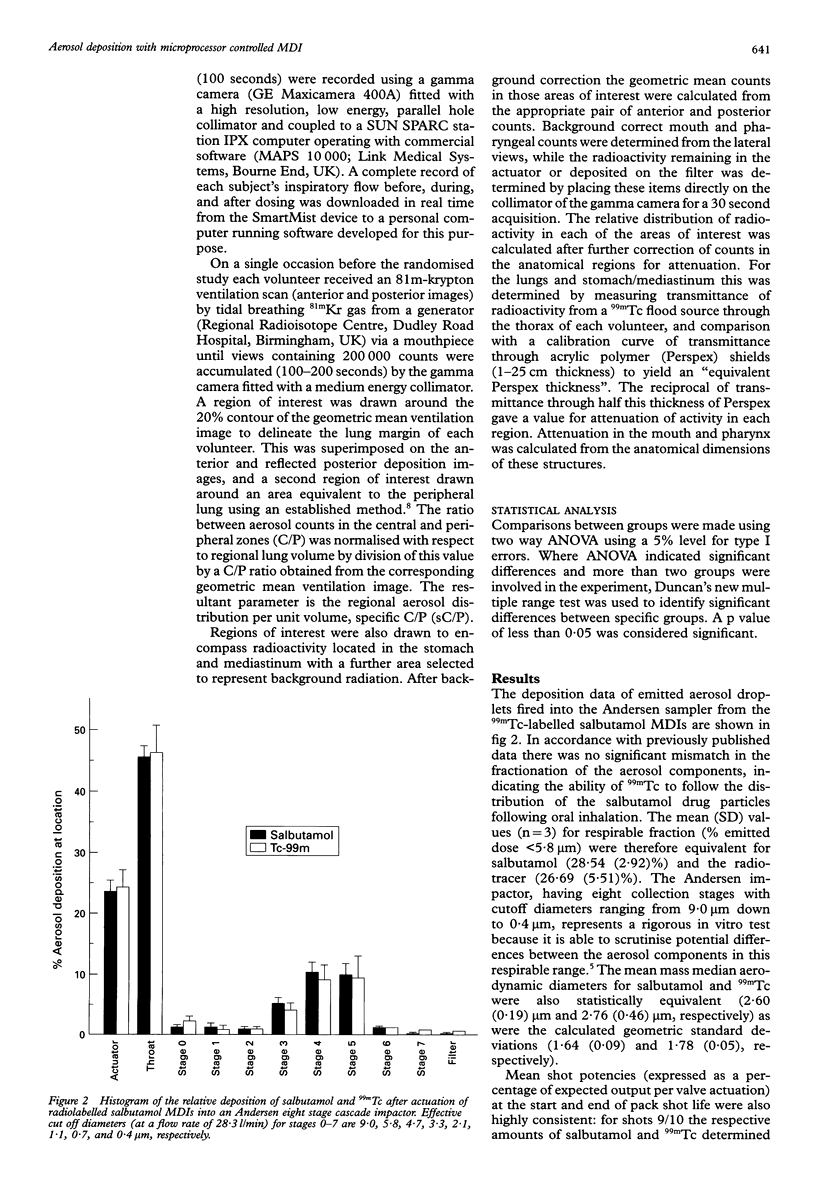
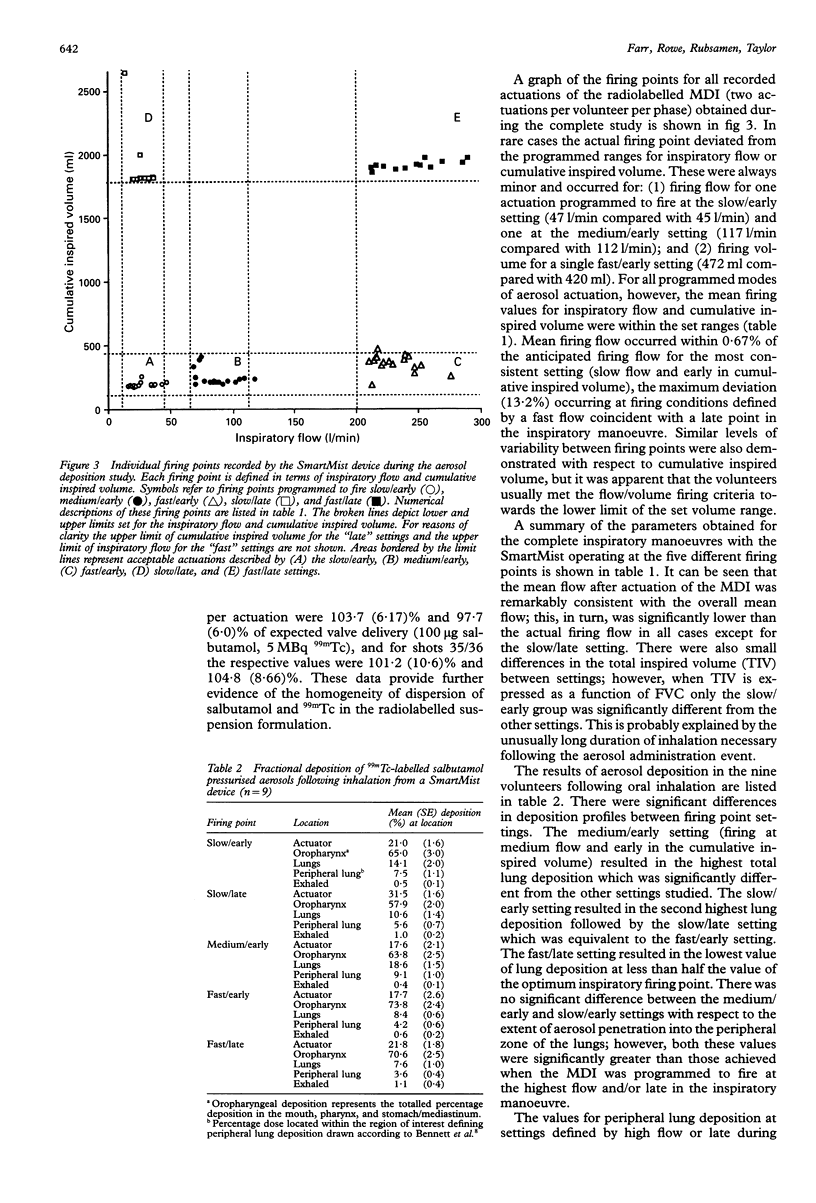
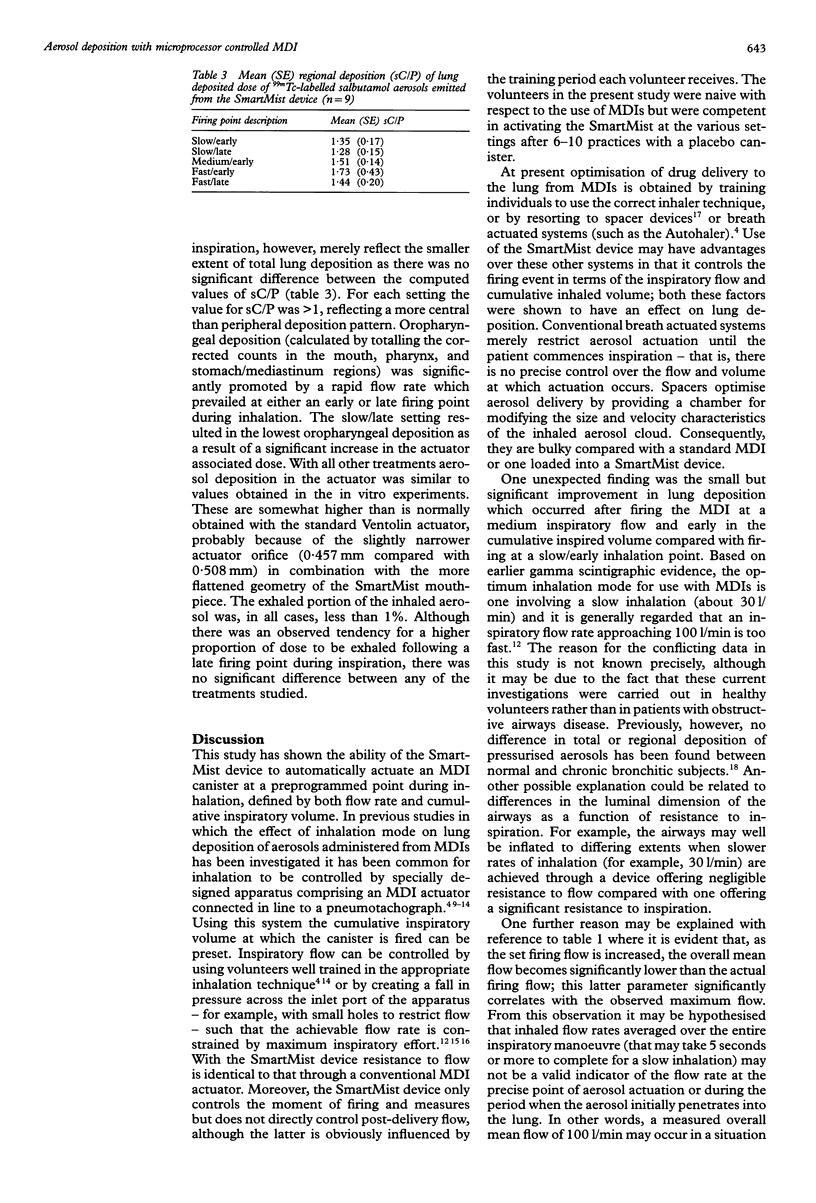
BACKGROUND--Gamma scintigraphy was employed to assess the deposition of aerosols emitted from a pressurised metered dose inhaler (MDI) contained in a microprocessor controlled device (SmartMist), a system which analyses an inspiratory flow profile and automatically actuates the MDI when predefined conditions of flow rate and cumulative inspired volume coincide. METHODS--Micronised salbutamol particles contained in a commercial MDI (Ventolin) were labelled with 99m-technetium using a method validated by the determination of (1) aerosol size characteristics of the drug and radiotracer following actuation into an eight stage cascade impactor and (2) shot potencies of these non-volatile components as a function of actuation number. Using nine healthy volunteers in a randomised factorial interaction design the effect of inspiratory flow rate (slow, 30 l/min; medium, 90 l/min; fast, 270 l/min) combined with cumulative inspired volume (early, 300 ml; late, 3000 ml) was determined on total and regional aerosol lung deposition using the technique of gamma scintigraphy. RESULTS--The SmartMist firing at the medium/early setting (medium flow and early in the cumulative inspired volume) resulted in the highest lung deposition at 18.6 (1.42)%. The slow/early setting gave the second highest deposition at 14.1 (2.06)% with the fast/late setting resulting in the lowest (7.6 (1.15)%). Peripheral lung deposition obtained for the medium/early (9.1 (0.9)%) and slow/early (7.5 (1.06)%) settings were equivalent but higher than those obtained with the other treatments. This reflected the lower total lung deposition at these other settings as no difference in regional deposition, expressed as a volume corrected central zone:peripheral zone ratio, was apparent for all modes of inhalation studied. CONCLUSIONS--The SmartMist device allowed reproducible actuation of an MDI at a preprogrammed point during inspiration. The extent of aerosol deposition in the lung is affected by a change in firing point and is promoted by an inhaled flow rate of up to 90 l/min-that is, the slow and medium setting used in these studies.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bennett W. D., Messina M. S., Smaldone G. C. Effect of exercise on deposition and subsequent retention of inhaled particles. J Appl Physiol (1985) 1985 Oct;59(4):1046–1054. doi: 10.1152/jappl.1985.59.4.1046. [DOI] [PubMed] [Google Scholar]
- Colthorpe P., Farr S. J., Taylor G., Smith I. J., Wyatt D. The pharmacokinetics of pulmonary-delivered insulin: a comparison of intratracheal and aerosol administration to the rabbit. Pharm Res. 1992 Jun;9(6):764–768. doi: 10.1023/a:1015851521551. [DOI] [PubMed] [Google Scholar]
- Cyr T. D., Graham S. J., Li K. Y., Lovering E. G. Low first-spray drug content in albuterol metered-dose inhalers. Pharm Res. 1991 May;8(5):658–660. doi: 10.1023/a:1015825311750. [DOI] [PubMed] [Google Scholar]
- Dolovich M., Ruffin R. E., Roberts R., Newhouse M. T. Optimal delivery of aerosols from metered dose inhalers. Chest. 1981 Dec;80(6 Suppl):911–915. [PubMed] [Google Scholar]
- Laube B. L., Georgopoulos A., Adams G. K., 3rd Preliminary study of the efficacy of insulin aerosol delivered by oral inhalation in diabetic patients. JAMA. 1993 Apr 28;269(16):2106–2109. [PubMed] [Google Scholar]
- Newman S. P., Clark A. R., Talaee N., Clarke S. W. Pressurised aerosol deposition in the human lung with and without an "open" spacer device. Thorax. 1989 Sep;44(9):706–710. doi: 10.1136/thx.44.9.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman S. P., Millar A. B., Lennard-Jones T. R., Morén F., Clarke S. W. Improvement of pressurised aerosol deposition with Nebuhaler spacer device. Thorax. 1984 Dec;39(12):935–941. doi: 10.1136/thx.39.12.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman S. P., Pavia D., Clarke S. W. Improving the bronchial deposition of pressurized aerosols. Chest. 1981 Dec;80(6 Suppl):909–911. [PubMed] [Google Scholar]
- Newman S. P., Pavia D., Garland N., Clarke S. W. Effects of various inhalation modes on the deposition of radioactive pressurized aerosols. Eur J Respir Dis Suppl. 1982;119:57–65. [PubMed] [Google Scholar]
- Newman S. P., Pavia D., Morén F., Sheahan N. F., Clarke S. W. Deposition of pressurised aerosols in the human respiratory tract. Thorax. 1981 Jan;36(1):52–55. doi: 10.1136/thx.36.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman S. P. Scintigraphic assessment of therapeutic aerosols. Crit Rev Ther Drug Carrier Syst. 1993;10(1):65–109. [PubMed] [Google Scholar]
- Newman S. P., Weisz A. W., Talaee N., Clarke S. W. Improvement of drug delivery with a breath actuated pressurised aerosol for patients with poor inhaler technique. Thorax. 1991 Oct;46(10):712–716. doi: 10.1136/thx.46.10.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiro S. G., Singh C. A., Tolfree S. E., Partridge M. R., Short M. D. Direct labelling of ipratropium bromide aerosol and its deposition pattern in normal subjects and patients with chronic bronchitis. Thorax. 1984 Jun;39(6):432–435. doi: 10.1136/thx.39.6.432. [DOI] [PMC free article] [PubMed] [Google Scholar]


