Abstract
Background
The chronic disease model of opioid use disorder (OUD) is promoted by many public health authorities, yet high levels of stigma persist along with low support for policies that would benefit people with OUD.
Objective
Determine if a survivorship model of OUD, which does not imply a chronic, relapsing disease state, compared to a chronic disease model improves public stigma and support for opioid-related policies. Explore if race or gender moderates any effect.
Design
Online, vignette-based randomized study.
Participants
US adults recruited through a market research firm.
Intervention
Participants viewed one of 8 vignettes depicting a person with OUD in sustained remission. Vignettes varied in terms of the OUD model (survivorship, chronic disease) and vignette individual’s race (Black, White) and gender (man, woman).
Main Measures
(1) Public stigma measured by desire for social distance, perceptions of dangerousness, and overall feelings toward the vignette individual. (2) Support for 7 opioid-related policies. Overall feelings were measured on a feelings thermometer (0/cold–100/warm). Stigma and policy support responses were measured on Likert scales dichotomized to indicate a positive (4, 5) or negative/indifferent (1–3) response.
Key Results
Of 1440 potential participants, 1172 (81%) were included in the analysis. Exposure to the survivorship model resulted in warmer feelings (mean 72, SD 23) compared to the chronic disease (mean 67, SD 23; difference 4, 95%CI 1–6). There was no effect modification from the vignette individual’s race or gender. There was no significant difference between OUD models on other measures of public stigma or support for policies.
Conclusions
The survivorship model of OUD improved overall feelings compared to the chronic disease model, but we did not detect an effect of this model on other domains of public stigma or support for policies. Further refinement and testing of this novel, survivorship model of OUD could improve public opinions.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07865-y.
KEY WORDS: opioid use disorder, chronic disease, survivorship model, public stigma, policy
INTRODUCTION
The US general public holds highly stigmatized perspectives of people with opioid use disorder (OUD).1–3 As opioid overdoses increase due to the spread of illicitly manufactured fentanyl, higher levels of stigma contribute to opioid-related morbidity and are associated with less support for policies that benefit people with OUD.4 These policies include providing naloxone to friends and family of people with OUD, increasing government spending on addiction treatment, and protecting people who are seeking medical care for an overdose from criminal charges.5 These policies also include evidence-based harm reduction approaches such as access to safe consumption sites and safe supply programs which reduce mortality for people who use opioids but who are not ready for formal treatment.6,7. To address this stigma, national public health authorities characterized OUD and substance use disorders in general as treatable chronic diseases “like diabetes.”8,9 This conceptualization of OUD as a medical condition rather than a behavioral choice is grounded in neurobiological research linking adverse childhood experiences, genetics, and brain function with substance use disorders.10 The chronic disease model can reduce stigma. A US nationally representative study showed that when OUD was described as a “chronically relapsing brain disease,” participants had less stigmatizing blame attributions compared to describing OUD as an “illness” or “problem.”11 However, despite some progress, the general population continues to demonstrate high levels of public stigma toward people with OUD compared to people with other conditions like schizophrenia or major depression.2,3
The chronic disease model of OUD may fail to overcome persistent stigmatization of people with OUD by implying that people with OUD have an essential biological trait which is ever-present, regardless of remission status.12 This model may even perpetuate stigma by affixing an irrevocable label to a person with OUD.12,13 In previous qualitative research, we found that among some people with OUD in sustained remission, a survivorship model of OUD was preferred to a chronic disease model.14 The survivorship model of OUD is analogous to the cancer survivorship model where holistic and specific care is needed even after the illness episode when cancer is not present.15 A survivorship model does not imply that a disease is present or that individuals are likely to return to drug use. Some individuals with OUD in sustained remission preferred a survivorship model because it recognizes ongoing medical and psychological needs related to OUD but does not perpetuate the idea of a “diseased” state.14 Put differently, they do not consider themselves to have a chronic, relapsing disease and this framing perpetuated stigma despite sustained remission.14 A survivorship model of OUD could fit into the existing biomedical understanding of OUD and reframe it in a manner that does not imply a person with OUD lives in a chronic disease state.
Public perceptions and stigma toward people with OUD are also influenced by social constructions of race and gender. For example, media narratives of White people with OUD often referred to them as blameless victims of over-prescribing physicians or outside influence. In contrast, media narratives of Black people with OUD are largely absent, suggesting that they were not newsworthy or noteworthy, and when present often depict them as criminals that pose a threat to society and are less deserving of grace, mercy, or intervention .16–18 These contrasting narratives shape public perception and contribute to racialized policies and structural racism in the healthcare system. For example, minoritized communities are much more likely to have access to opioid treatment programs offering methadone compared to White communities where buprenorphine is available in many office-based (e.g., primary care) settings.19,20 Black people with OUD are therefore disproportionally treated with methadone and impacted by policies restricting methadone to specific clinics and a criminal justice approach to treatment that requires dose surveillance and urine drug testing.19,21–23 Studies on the effect of gender on public perceptions of people with OUD are mixed,24 with some suggestion that women receive more concern and sympathy from the public compared to men.25 Women with substance use disorders perceived stigma during substance use disorder treatment which likely contributes to the finding that women are under-represented in treatment settings.26,27 When developing interventions to reduce stigma, it is necessary to consider how bias and discrimination that occurs as a result of gender and racial constructs intersect with bias and discrimination related to OUD.
To investigate the concept of a survivorship model of OUD, we conducted a randomized study to measure the effects of portraying OUD through a survivorship model on (1) the general public’s stigma toward people with OUD and (2) their support for opioid-related policies. We hypothesized that reframing OUD through a survivorship model would reduce public stigma and improve support for policies relative to framing as a chronic disease. We further explored if race or gender moderated the difference between the survivorship and chronic disease model of OUD when differences between OUD models were observed.
METHODS
We conducted an eight-arm randomized study in which participants were randomly exposed to a single vignette portraying an individual with OUD in sustained remission through a chronic disease or survivorship model. Groups 1–4 were randomly assigned to view the survivorship model vignette and groups 5–8 assigned to view the chronic disease model vignette. Within these groups, each vignette employed a different gender (man, woman) and race (Black, White) combination. The vignettes were modeled on previous studies evaluating message framing on stigma and support for opioid-related policies.2,3,28
Participants
A convenience sample of participants aged ≥ 18 years living in the USA were recruited using the market research firm Dynata (www.dynata.com). Dynata maintains a database of potential participants who are recruited through recruitment campaigns, direct email, and online marketing, and from diverse, affiliated partners and websites. Potential participants are randomly selected to specific surveys if they meet the specific demographic characteristics requested for the survey; participants who agree to participant receive compensation from Dynata. Dynata employs quality verifications and security checks to verify participant information and prevent duplicate enrollment. We used a quota system to recruit a sample that approximated the US population by balancing on gender, age, race, and ethnicity; however, the population recruited is not nationally representative. There were no exclusion criteria.
After consenting, we used block randomization to assign participants to one of the 8 experiment groups. Study data were collected and managed using REDCap.29,30 The study analysis was not pre-registered and is presented here according to Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Intervention
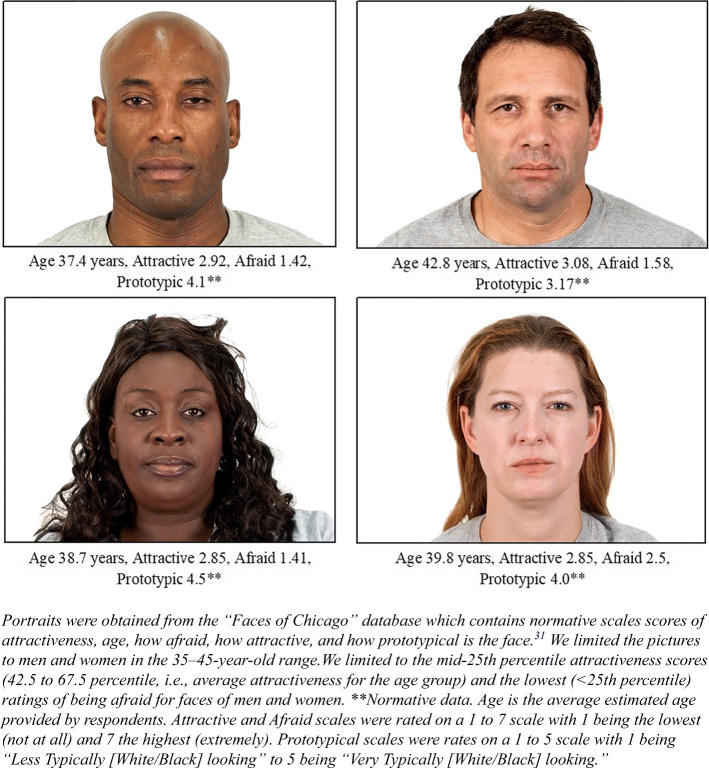
Each experimental group contained a single vignette. The vignette backstory was the same across all groups and portrayed an individual who first used heroin after high school, was diagnosed with OUD, and is now in long-term remission with last heroin use over 10 years ago (Table 1). The vignette individual’s gender was presented both through the text describing “Mike” or “Mary” with corresponding pronouns. Vignette individual’s race was either Black or White and presented with an accompanying portrait (Fig. 1). The portraits were selected from the Chicago Faces to be representative of an individual who is 35–45 years old with average attractiveness for each race and gender.31
Table 1.
Vignette Text with the Consistent and Varying Elements.
| Consistent elements | |
|
Mary is a woman in her mid-30s who has completed high school. Mary used heroin for the first time 1 year after high school while at a party. At first, she only used heroin on weekends. After a few weeks, she found that she increasingly felt the desire to use more heroin. Mary then began using heroin every day. She spent all her savings and borrowed money from friends and her parents to buy more heroin. Each time she tried to cut down, she could not sleep and she felt anxious, sweaty, and nauseated for hours. These symptoms lasted until she used heroin again. Her friends complained that she had become unreliable. She made plans one day and canceled them the next. Her parents said she had changed and that they could no longer count on her. Mary tried to stop using heroin many times, but after a few days she would always go back to using heroin. After living this way for 6 years, Mary went to see a doctor for help. The doctor diagnosed her with an opioid addiction. With her doctor’s help, Mary entered a treatment program for her addiction. She started talking with a doctor regularly and took many steps to improve her life and stop using heroin. As of today, Mary has not used any heroin or other drugs for over 10 years. She lives near her parents; she enjoys spending time outdoors, and takes part in various activities in her community. While Mary still experiences life’s ups and downs, she does not feel she needs to use heroin to cope. | |
| Varying elements | |
| Chronic disease | |
| Mary believes her opioid addiction is a chronic and relapsing disease and it is possible that she will use heroin again. Put differently, her opioid addiction is a chronic disease, like diabetes, which requires ongoing work or treatment. She feels that she is living with the chronic disease of opioid addiction and it will always be present in her body, mind, and life. | |
| Survivorship | |
| Mary believes she survived her opioid addiction, and it is unlikely that she will use heroin again. Put differently, her opioid addiction is a survivable condition, like some cancers, which can be treated and not come back for the rest of her life. She feels that she is a survivor of opioid addiction and it is no longer present in her body, mind, and life. |
Vignettes Describing a Man Use the Name “Mike” and Corresponding Masculine Pronouns
Figure 1.
Portrait of vignette characters for each experimental condition and normative data.
We based the chronic disease model component of the vignette on the currently accepted definition of addiction. 32,33 This emphasizes the chronic, relapsing nature of OUD and its similarity to other chronic conditions that are at risk of exacerbation and require continued treatment.32,33 The survivorship model was informed by the cancer survivorship model and our previous research.14,15 The survivorship model conditions emphasize that the vignette individual could reach a point where OUD is no longer present in their body or life, that OUD is not a perpetually relapsing condition, and that returning to drug use is unlikely. This is reflective of epidemiologic studies showing that once long-term remission from opioid and other drug use is achieved, returning to use is uncommon.34–36
Outcomes
Public Stigma
We assessed public stigma using three measures (Table 2). First, three questions assessed willingness for close social distance on a Likert scale ranging from (1) “definitely unwilling” to (5) “definitely willing.” Second, two questions assessed perceptions of dangerousness on a Likert scale ranging from (1) “definitely unlikely” to (5) “definitely likely.” This scale was reverse-coded so that higher scores corresponded with more positive views and less stigma. Social distance and perceptions of dangerousness were adapted from previous studies.3,28 We dichotomized responses with scores of 4 or 5 (coded as “1”) representing positive responses (i.e., willing to be socially close or perceived as unlikely to be of dangerous) and scores of 1–3 (coded as “0”) representing negative/indifferent responses. Third, a feelings thermometer assessed participants overall feeling toward the vignette individual. Responses could range from 0 to 100 where 0 corresponds to very cold/unfavorable and 100 to very warm/favorable feelings.
Table 2.
Description of the Primary Outcomes of Public Stigma and Opioid-Related Policy Support
| I. Public stigma | |
| Social distance scalea | |
| 1 | How willing would you be to have a person with an opioid addiction marry into your family? (“Marry”) |
| 2 | How willing would you be to have a person with an opioid addiction live next door? (“Neighbor”) |
| 3 | How willing would you be to have a person with an opioid addiction be a friend of yours? (“Friend”) |
| Perceptions of dangerousness scalea | |
| 1 | How likely is it that a person with an opioid addiction would do something violent toward other people? (“Other”) |
| 2 | How likely is it that a person with an opioid addiction would do something violent toward themself? (“Self”) |
| Feelings thermometer | |
| 1 | Think about the person you read about and rate how warm/favorable or cold/unfavorable you feel toward them. Ratings between 0 and 50 degrees mean that you feel unfavorable/cold. Ratings between 50 and 100 degrees mean that you feel favorable/warm. A rating of 50 degrees means you do not feel particularly cold/unfavorable or warm/favorable toward the person. |
| II. Policy supportb | |
| 1 |
Medications to treat opioid addiction include buprenorphine, methadone, and naltrexone. Unlike medications for other common conditions (like diabetes or high blood pressure), some insurance companies do not pay for these medications or put time limits on how long they will pay for the medications. Do you support or oppose government rules requiring insurance companies to pay for medications to treat opioid addiction without time limits? (“Medication Coverage Parity”) |
| 2 | Do you support or oppose increasing government spending on the treatment of opioid addiction? (“Government Spending”) |
| 3 | Do you support or oppose increasing government spending on programs to subsidize housing costs for people with an opioid addiction? (“Housing Subsidies”) |
| 4 | Syringe Services Programs are programs where people who inject heroin or other drugs can get sterile (new) syringes and safely dispose of used ones. Do you support or oppose the legalization of Syringe Services Programs in your community? (“Syringe Services”) |
| 5 |
Methadone for the treatment of opioid addiction is only available from specialty treatment programs, sometimes referred to as “methadone clinics.” Do you support or oppose allowing primary care doctors to prescribe methadone for opioid addiction in your community? (“Primary Care Methadone”) |
| 6 | Safe Consumption Sites are places where people can bring previously purchased opioids and other drugs and legally use them under medical supervision. Do you support or oppose the legalization of safe Consumption Sites in your community? (“Safe Consumption Sites”) |
| 7 | Heroin is often contaminated (“laced”) with a powerful opioid called fentanyl. Safe Supply Programs allow people who use heroin to receive prescription-grade opioids from a physician to reduce unintentional overdose from fentanyl. Do you support or oppose the legalization of Safe Supply Programs in your community? (“Safe Supply Programs”) |
Policy Support
Participants were asked to provide the level of support for 7 opioid-related policies (Table 2). Participants provided their level of support on a Likert scale ranging from (1) “strongly oppose” to (5) “strongly support.” Responses were dichotomized with scores of 4 or 5 (coded as “1”) representing positive response (i.e., support for policy) and scores of 1–3 (coded as “0”) representing negative/indifferent response.
Analysis
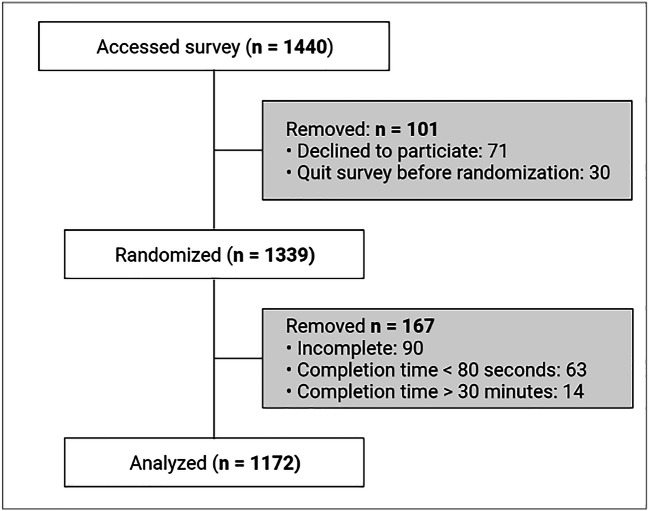
Participants with incomplete data and those who completed the study in <80 s or >30 min were removed. These outlying short and long completion times likely indicate the participants did not carefully read the vignette or were interrupted during the study, respectively. A sensitivity analysis including these participants in the analysis did not change the results (eFig. 3).
We tested differences in observed participant characteristics between experimental groups using Pearson’s chi-square test. Logistic regression models tested the effect of exposure to a survivorship model compared to chronic disease model and included variables for the vignette individual’s race and gender. If a significant difference between the OUD model exposure (chronic disease versus survivorship) and participant responses to public stigma and policy support items was observed, we explored if the vignette individual’s gender or race modified the effect by interacting these terms with the OUD model exposure. For ease of interpretation, differences between OUD models are presented as change in probability of a positive response by calculating the average marginal effects using the “margins” package for R.37 Analogous linear regression models examined the relationship between the exposures and feelings thermometer response. The prespecified analytic plan dichotomized all Likert scale items. We felt this approach would provide more meaningful results, for example, by stating how the disease model exposure would impact the probability of a participant’s willingness to support a policy. We also conducted a sensitivity analysis using ordinal logistic regression to model the effect of exposure to a survivorship model compared to chronic disease model on participants’ responses on the 5-point Likert scale. The sensitivity analysis provides information on odds of having a relatively lower or higher response on the 5-point Likert scale.
A simulation power analysis based on previous nationally representative data2 suggested a sample of 1000 participants could detect a 10% difference between disease model conditions on willingness for social distance with 97% power at α = 0.05. Power to detect the interaction between disease model and race or gender on the primary outcomes would be 56% at α = 0.05 and is therefore considered exploratory. The study was approved by a Johns Hopkins School of Medicine Institute Review Board and data collection took place on December 5th–7th, 2022. Analysis was conducted on January 7th–March 1st, 2022, using R.38
RESULTS
There were 1440 potential participants recruited and 1172 (81%) of those were included in the analysis (Fig. 2; eFig. 1). The experimental groups had between 137 and 157 participants for analysis and there were no significant differences between the groups on the observed characteristics (Table 3; eTable 1). A total of 539 (51%) participants were exposed to a chronic disease model and 510 (49%) participants were exposed to a survivorship disease model. The average time to complete the study was 4.9 min (SD 2.6).
Figure 2.
Study flow diagram. See supplement eFigure 1 for a detailed study flow diagram showing all 8 groups.
Table 3.
Participant Characteristics
| N = 1172 (%) | Test of randomization across 8 conditionsa | |
|---|---|---|
| Age, years | p = 0.90 | |
| 18–29 | 251 (21) | |
| 30–44 | 339 (29) | |
| 45–60 | 292 (25) | |
| 60+ | 290 (25) | |
| Self-reported gender | p = 0.18 | |
| Man | 603 (52) | |
| Woman | 561 (48) | |
| Non-binary | 8 (<1) | |
| Race | p = 0.14 | |
| White | 955 (82) | |
| Black | 122 (10) | |
| Otherb | 95 (8) | |
| Ethnicity | p = 0.34 | |
| Non-Hispanic | 1076 (92) | |
| Hispanic | 96 (8) | |
| Education | p = 0.51 | |
| Some high school | 36 (3) | |
| High school diploma | 295 (25) | |
| Some college | 247 (21) | |
| Associates degree/Certificate/License | 149 (13) | |
| Bachelor’s degree | 280 (24) | |
| Master’s degree or higher | 165 (14) | |
| Employment | p = 0.92 | |
| Employed | 642 (55) | |
| Unemployed | 153 (13) | |
| Retired | 239 (20) | |
| Other (e.g., disabled, homemaker, other) | 138 (12) | |
| Income | p = 0.11 | |
| < $10,000 | 86 (7) | |
| $10,000–24,999 | 145 (12) | |
| $25,000–49,999 | 331 (28) | |
| $50,000–74,999 | 238 (20) | |
| ≥ $75,000 | 372 (32) | |
| Political affiliation | p = 0.39 | |
| Democrat | 237 (20) | |
| Independent/No party affiliation | 210 (18) | |
| Republican | 370 (32) | |
| US Census Region | p = 0.81 | |
| Midwest | 254 (22) | |
| Northeast | 250 (21) | |
| South | 491 (42) | |
| West | 177 (15) |
aPearson chi-square test. See supplement eTable 2 for demographic characteristic each experimental group
bIncludes: American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander, Multiple, or other race not specified
Effect of OUD Model on Public Stigma
There was no significant effect of exposure to a survivorship model compared to chronic disease model on willingness to be socially close to a person with OUD or on perceptions that a person with OUD was unlikely to be violent toward others or themselves (Table 4). Across all conditions, 46% of participants were willing to be a friend with a person with OUD, 34% of participants were willing to be a neighbor to a person with OUD, and 28% of participants were willing to have a person with OUD marry into the family. For perceptions of dangerousness, 13% of participants reported it was unlikely for a person with OUD to be violent toward others and 8% reported it was unlikely for a person with OUD to be violent toward themselves.
Table 4.
Predicted Probabilities and Difference in Favorable Response on Public Stigma and Policy Support Items by Disease Model Exposure
| Chronic disease | Survivorship | Average marginal effect | p value | |
|---|---|---|---|---|
| Probability (SD) | Probability (SD) | Difference (95% CI) | ||
| Public stigma | ||||
| Willingness of close social distance | ||||
| Marry | 27.3 (2.0) | 28.9 (2.1) | 1.6 (−3.5, 6.8) | 0.46 |
| Neighbor | 34.9 (0.5) | 32.7 (0.5) | −2.2 (−7.6, 3.2) | 0.76 |
| Friend | 47.4 (1.6) | 44.7 (1.6) | −2.8 (−8.5, 2.9) | 0.54 |
| Violence is unlikely | ||||
| Others | 13.3 (1.0) | 13.5 (1.0) | 0.2 (−3.7, 4.1) | 1.00 |
| Self | 7.8 (0.8) | 8.9 (0.9) | 1.1 (−2.1, 4.3) | 0.64 |
| Policy support | ||||
| Medication coverage parity | 70.7 (2.7) | 69.4 (2.7) | −1.3 (−6.6, 3.9) | 0.89 |
| Government spending | 67.9 (1.3) | 69.0 (1.3) | 1.1 (−4.2, 6.4) | 0.71 |
| Housing subsidies | 50.2 (2.7) | 47.6 (2.3) | −2.6 (−8.3, 3.1) | 0.62 |
| Syringe services | 46.6 (2.5) | 43.4 (2.4) | −3.2 (−8.9, 2.5) | 0.42 |
| Primary care methadone | 62.1 (3.0) | 58.0 (3.1) | −4.1 (−9.7, 1.5) | 0.22 |
| Safe consumption sites | 40.3 (0.1) | 38.0 (0.1) | −2.3 (−7.9, 3.3) | 0.49 |
| Safe supply programs | 43.4 (0.8) | 42.6 (0.8) | −0.9 (−6.6, 4.8) | 0.96 |
Chronic disease and survivorship columns represent the probability of favorable response on each item. The average marginal effect is the expected change in probability on each item when comparing survivorship to the chronic disease model exposures
There was a significant effect of exposure to the survivorship model compared to the chronic disease model on the feelings thermometer score. The mean feelings thermometer score for participants exposed to the survivorship model vignette was 72 (SD 23) which was 4 points (95% CI, 1, 6) higher than the mean feelings score for participants exposed to the chronic disease model vignette (67, SD 23). The effect size of the survivorship model compared to the chronic disease model on the feelings thermometer score was small (Cohen’s f2 = 0.07). The interpretation is that exposure to the survivorship model resulted in significantly warmer/positive feelings compared to the chronic disease model. When the disease model exposure was interacted with the vignette individual’s race or gender, we did not observe effect modification by the vignette individual’s race (interaction term β = 0.2, 95% CI, −5.5, 5.2) or gender (interaction term β=1.8, 95% CI, −3.5, 7.2).
Effect of Disease Model on Policy Support
There was no significant effect of exposure to the survivorship model compared to the chronic disease model on the probability of support for each policy scale item (Table 4). Across all conditions, most participants support spending on treatment (68%), medication coverage parity (70%), and primary care methadone treatment (60%). Fewer participants support increased housing (49%) or legalizing syringe exchange (45%), safe supply programs (43%), and safe consumption sites (39%).
Sensitivity Analyses
The distribution of the participant response by exposure to the survivorship or chronic disease model is shown in supplement eFig. 2. Like the primary analysis, there was no significant effect of exposure to the survivorship model compared to the chronic disease model on odds of having a more favorable response on willingness to be socially close to a person with OUD, perceptions that a person with OUD was unlikely to be violent toward others or themselves, or support for each policy scale item (supplement eTable 2).
DISCUSSION
Using a sample of the US general public, we found that portraying OUD through a survivorship model resulted in warmer feelings toward people with OUD compared to chronic disease model portrayals. People with OUD overcome many obstacles to achieve OUD remission and the label of a survivor could signal to the general public the strength and perseverance required to achieve remission. It is possible that by framing individuals as “survivors,” participants recognized this effort and felt more positive emotions associated with overcoming OUD. However, there was no effect of exposure to a survivorship model compared to chronic disease model on social distance or perceptions of dangerousness measures. Across all conditions, high levels of stigma toward people with OUD were observed with less than half of participants willing to be socially close and fewer than one-in-seven participants perceived violence was unlikely.
In our study, exposure to the OUD survivorship model had a positive effect on overall feelings and no effect on social distance and perceptions of dangerousness. These mixed findings are similar to Kelly et al. (2021) who similarly showed that various descriptions of OUD can have a differential effect on dimensions of public stigma.11 Describing OUD as a “chronic relapsing disease of the brain,” “brain disease,” “disease,” “illness”, “disorder,” or “problem” had no effect on social distance measures. While describing OUD as a “problem,” the “chronically relapsing brain disease” description resulted in less perceived danger. We included a measure of overall feelings toward people with OUD and found there were more favorable feelings when participants were exposed to the survivorship model, though the effect size was small.
While the current study’s population of interest was the general public, it is possible that presenting OUD through a survivorship model could influence healthcare providers’ feelings toward people with OUD and potentially improve patient outcomes. For example, in clinical settings, a tenet of effective motivational interviewing is empathetic communication and having unconditional positive regard for the patient.39,40 If clinicians were exposed to a survivorship model of OUD, it could increase positive feelings toward their patients with OUD and improve therapeutic alliance and the effectiveness of behavioral interventions. We suspect that healthcare providers who are more familiar with a chronic disease model of OUD would need repeated exposures to the survivorship model of OUD to convince them that the model is true or accurate to have an effect on measures of public stigma and improve perceptions of patients with OUD.
Participant showed broad support (e.g., >50%) for policies that require insurance companies to provide coverage for medications for OUD, allowing methadone to be prescribed in primary care for the treatment of OUD, and increasing government spending on addiction treatment. There was less support for harm reduction policies including legalizing syringe exchange services, safe consumption sites, and safe supply programs. Furthermore, there was no effect of OUD model portrayal on support for public policies which has significant public health implications since these are evidence-based approaches to reduce mortality. Previous research has shown that public support for these programs is lower when the general public has higher levels of stigma.5 Therefore, new approaches to reduce stigma are necessary to increase public support for public health–oriented policies.
The key difference between the survivorship and chronic disease model was the persistence of a diseased state and likelihood of returning to substance use. By describing OUD as a condition that is not currently present, we sought to overcome the key criticisms that the chronic disease model implies an essential biologic trait that is fixed and ever-present and build on our previous research findings.12–14 Notably, we did not observe a difference on most of our outcomes and it is possible that participants focused on other salient factors that were common across all conditions. First, the vignettes depict a person who used heroin. While a recent study showed no difference between portrayals of heroin and prescription opioid use on public stigma toward pregnant women with OUD,41 heroin use has historically been portrayed as more dangerous and associated with crime, and the public has supported criminal justice–focused and highly punitive responses to its use and possession.16,18,21 Second, portraying OUD as a treatable condition is known to reduce stigma and all conditions were narratives depicting the development, treatment, and remission from OUD.28 It is possible that participants anchored on these factors which providers stronger influence on their perceptions than the OUD model portrayed. Future studies need to explore the influence of how the type of opioid influences public perceptions. In addition, the inclusion of a true control could help isolate what factors are most influential. Finally, it is possible that the survivorship model “medicalizes” OUD equivalently to a chronic disease model and it is the biogenic explanations for OUD that induce public stigma.12 The harm reduction model is one well-established model of addiction that shifts away from the medical models of OUD and could improve public perceptions.42 By deemphasizing the goal for treatment to reach sustained abstinence from opioid use, a harm reduction model which prioritizes health and respect for an individual’s desire for pleasure, comfort, and care could reduce public stigma and increase support for harm reduction–oriented policies.42
Limitations
There are limitations that should be considered. First, we attempted to balance the participants to match a general population, but this was not a nationally representative sample. It is possible that our participants are systematically different from the general population given their willingness to engage in these types of studies and thus limits our generalizability. Additionally, we tested a novel idea of a survivorship model of OUD. The description was developed by the study authors and was not validated or tested prior to this study. It is possible that additional information or variation in the presentation is needed to ensure participants believe a survivorship model is a valid model and the core concept is being understood. Further qualitative work is needed to understand how framing the different models changes understanding and reactions from patients, healthcare clinicians, and the general public.
CONCLUSION
In conclusion, we observed improved feelings toward individuals with OUD with the survivorship model, but no increased in support for policies which would benefit people with OUD and no change in desire for social distance of perceptions of dangerousness. Improving public perception of people with OUD has proven difficult but remains necessary to reduce stigma and enact policies to reduce opioid-related morbidity and mortality.
Supplementary Information
(DOCX 720 kb)
Authors Contribution
JDP conducted all data analysis and drafted the manuscript. EEM provided input on analytic plan. JDP, GC, APT, EEM, and SMO provided input on experiment design, exposures, and outcomes. All authors listed have made a substantial contribution to this manuscript and approved it for publication.
Funding
This project has been supported through a Gender and Racial Justice Scholars Award, an outgrowth of Johns Hopkins University’s Women’s Suffrage Centennial Commemoration. GC receives funding from K24 AA027483 the National Institute on Alcohol Abuse and Alcoholism, NIH.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Volkow ND. Stigma and the toll of addiction. N Engl J Med. 2020;382(14):1289–1290. doi: 10.1056/NEJMp1917360. [DOI] [PubMed] [Google Scholar]
- 2.Perry BL, Pescosolido BA, Krendl AC. The unique nature of public stigma toward non-medical prescription opioid use and dependence: a national study. Addiction. 2020;115(12):2317–2326. doi: 10.1111/add.15069. [DOI] [PubMed] [Google Scholar]
- 3.Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry. 2010;167(11):1321–1330. doi: 10.1176/appi.ajp.2010.09121743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ciccarone D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry. 2021;34(4):344–350. doi: 10.1097/YCO.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kennedy-Hendricks A, Barry CL, Gollust SE, Ensminger ME, Chisolm MS, McGinty EE. Social stigma toward persons with prescription opioid use disorder: associations with public support for punitive and public health-oriented policies. Psychiatr Serv Wash DC. 2017;68(5):462–469. doi: 10.1176/appi.ps.201600056. [DOI] [PubMed] [Google Scholar]
- 6.Harocopos A, Gibson BE, Saha N, et al. First 2 months of operation at first publicly recognized overdose prevention centers in US. JAMA Netw Open. 2022;5(7):e2222149. doi: 10.1001/jamanetworkopen.2022.22149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ivsins A, Boyd J, Beletsky L, McNeil R. Tackling the overdose crisis: the role of safe supply. Int J Drug Policy. 2020;80:102769. doi: 10.1016/j.drugpo.2020.102769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Spotlight on Opioids. HHS; 2018. https://addiction.surgeongeneral.gov/sites/default/files/Spotlight-on-Opioids_09192018.pdf [PubMed]
- 9.American Society of Addiction Medicine. Public policy statement: definition of addiction 2019. Published September 15, 2019. Accessed October 2, 2020. https://www.asam.org/Quality-Science/definition-of-addiction
- 10.Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363–371. doi: 10.1056/NEJMra1511480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly JF, Greene MC, Abry A. A US national randomized study to guide how best to reduce stigma when describing drug-related impairment in practice and policy. Addiction. 2021;116(7):1757–1767. doi: 10.1111/add.15333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kvaale EP, Haslam N, Gottdiener WH. The ‘Side Effects’ of medicalization: a meta-analytic review of how biogenetic explanations affect stigma. Clin Psychol Rev. 2013;33(6):782–794. doi: 10.1016/j.cpr.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Phelan JC. Geneticization of deviant behavior and consequences for stigma: the case of mental illness. J Health Soc Behav. 2005;46(4):307–322. doi: 10.1177/002214650504600401. [DOI] [PubMed] [Google Scholar]
- 14.Pytell JD, Sklar MD, Carrese J, Rastegar DA, Gunn C, Chander G. “I’m a survivor”: perceptions of chronic disease and survivorship among individuals in long-term remission from opioid use disorder. J Gen Intern Med. 2022;37(3):593–600. doi: 10.1007/s11606-021-06925-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shapiro CL. Cancer survivorship. N Engl J Med. 2018;379(25):2438–2450. doi: 10.1056/NEJMra1712502. [DOI] [PubMed] [Google Scholar]
- 16.Netherland J, Hansen HB. The war on drugs that wasn’t: wasted whiteness, “dirty doctors,” and race in media coverage of prescription opioid misuse. Cult Med Psychiatry. 2016;40(4):664–686. doi: 10.1007/s11013-016-9496-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mendoza S, Rivera AS, Hansen HB. Re-racialization of addiction and the redistribution of blame in the white opioid epidemic. Med Anthropol Q. 2019;33(2):242–262. doi: 10.1111/maq.12449. [DOI] [PubMed] [Google Scholar]
- 18.Hansen H, Netherland J. Is the prescription opioid epidemic a white problem? Am J Public Health. 2016;106(12):2127–2129. doi: 10.2105/AJPH.2016.303483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andraka-Christou B. Addressing racial and ethnic disparities in the use of medications for opioid use disorder. Health Aff (Millwood). 2021;40(6):920–927. doi: 10.1377/hlthaff.2020.02261. [DOI] [PubMed] [Google Scholar]
- 20.Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76(9):979–981. doi: 10.1001/jamapsychiatry.2019.0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alexander M, West C.The New Jim Crow: Mass Incarceration in the Age of Colorblindness. Revised edition. New Press; 2012.
- 22.Stein BD, Dick AW, Sorbero M, et al. A population-based examination of trends and disparities in medication treatment for opioid use disorders among medicaid enrollees. Subst Abuse. 2018;39(4):419–425. doi: 10.1080/08897077.2018.1449166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hansen H, Roberts SK. Two tiers of biomedicalization: methadone, buprenorphine, and the racial politics of addiction treatment. In: Netherland J, ed. Advances in Medical Sociology. Emerald Group Publishing Limited; 2012:79-102. 10.1108/S1057-6290(2012)0000014008
- 24.Kulesza M, Matsuda M, Ramirez JJ, Werntz AJ, Teachman BA, Lindgren KP. Towards greater understanding of addiction stigma: intersectionality with race/ethnicity and gender. Drug Alcohol Depend. 2016;169:85–91. doi: 10.1016/j.drugalcdep.2016.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wirth JH, Bodenhausen GV. The role of gender in mental-illness stigma: a national experiment. Psychol Sci. 2009;20(2):169–173. doi: 10.1111/j.1467-9280.2009.02282.x. [DOI] [PubMed] [Google Scholar]
- 26.Terplan M, Kennedy-Hendricks A, Chisolm MS. Prenatal substance use: exploring assumptions of maternal unfitness. Subst Abuse Res Treat. 2015;9(Suppl 2):1–4. doi: 10.4137/SART.S23328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris MTH, Laks J, Stahl N, Bagley SM, Saia K, Wechsberg WM. Gender dynamics in substance use and treatment: a women’s focused approach. Med Clin North Am. 2022;106(1):219–234. doi: 10.1016/j.mcna.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McGinty EE. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci. Published online 2015:13. [DOI] [PubMed]
- 29.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95(May). 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed]
- 30.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ma DS, Correll J, Wittenbrink B. The Chicago face database: a free stimulus set of faces and norming data. Behav Res Methods. 2015;47(4):1122–1135. doi: 10.3758/s13428-014-0532-5. [DOI] [PubMed] [Google Scholar]
- 32.ASAM Definition of Addiction. Accessed January 21, 2021. https://www.asam.org/Quality-Science/definition-of-addiction
- 33.Heilig M, MacKillop J, Martinez D, Rehm J, Leggio L, Vanderschuren LJMJ. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2021;46(10):1715–1723. doi: 10.1038/s41386-020-00950-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lopez-Quintero C, Hasin DS, de Los Cobos JP, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the national epidemiologic survey on alcohol and related conditions. Addict Abingdon Engl. 2011;106(3):657–669. doi: 10.1111/j.1360-0443.2010.03194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robins LN, Davis DH, Nurco DN. How permanent was Vietnam drug addiction? Am J Public Health. 1974;64(Suppl 12):38–43. doi: 10.2105/ajph.64.12_suppl.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hagman BT, Falk D, Litten R, Koob GF. Defining recovery from alcohol use disorder: development of an NIAAA research definition. Am J Psychiatry. Published online April 12, 2022:appi.ajp.21090963. 10.1176/appi.ajp.21090963 [DOI] [PubMed]
- 37.Leeper T. margins: Marginal Effects for Model Objects. Published online 2021.
- 38.R Core Team. R: a language and environment for statistical computing. Published online 2021.
- 39.Rogers CR. The necessary and sufficient conditions of therapeutic personality change. J Consult Psychol. 1957;21(2):95–103. doi: 10.1037/h0045357. [DOI] [PubMed] [Google Scholar]
- 40.Miller WR, Rollnick S.Motivational Interviewing: Helping People Change. 3rd ed. Guilford Press; 2013.
- 41.Schiff DM, Stoltman JJK, Nielsen TC, et al. Assessing stigma towards substance use in pregnancy: a randomized study testing the impact of stigmatizing language and type of opioid use on attitudes toward mothers with opioid use disorder. J Addict Med. 2022;16(1):77–83. doi: 10.1097/ADM.0000000000000832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lie AK, Hansen H, Herzberg D, et al. The harms of constructing addiction as a chronic, relapsing brain disease. Am J Public Health. 2022;112(S2):S104–S108. doi: 10.2105/AJPH.2021.306645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McGinty EE, Barry CL, Stone EM, et al. Public support for safe consumption sites and syringe services programs to combat the opioid epidemic. Prev Med. 2018;111:73–77. doi: 10.1016/j.ypmed.2018.02.026. [DOI] [PubMed] [Google Scholar]
- 44.McGinty EE, Stone EM, Kennedy-Hendricks A, Bachhuber MA, Barry CL. Medication for opioid use disorder: a national survey of primary care physicians. Ann Intern Med. 2020;173(2):160–162. doi: 10.7326/M19-3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calcaterra SL, Bach P, Chadi A, et al. Methadone matters: what the United States can learn from the global effort to treat opioid addiction. J Gen Intern Med. 2019;34(6):1039–1042. doi: 10.1007/s11606-018-4801-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 720 kb)