Abstract
Objective
Awareness and substantial understanding of obesity are essential components in its prevention and treatment. This study aimed to determine the degree of obesity awareness and its relationship to various sociodemographic characteristics among Filipino adults working from home (WFH).
Methodology
This is a cross-sectional survey conducted in Metro Cebu, Philippines. Included were non-healthcare WFH professionals aged 18-64. Researcher-made Obesity Awareness Questionnaire (OAC-20) was used.
Results
A total of 458 employees participated in the study; mean age was 30.33 years (SD=6.96), mostly female (71.40%) and majority single (77.07%). The mean obesity awareness score was 79.18% (SD=9.02). Age (p=0.198), BMI (p=0.397), work hours/day (p=0.101), and hours of physical activity/day (p=0.458) were not associated with obesity awareness. Similarly, male vs. female (p=0.515), and single vs. married respondents (p=0.629) did not differ significantly in terms of average scores. However, higher educational attainment (p=0.044) and higher socio-economic status (p=0.002) were significantly associated with higher obesity awareness scores.
Conclusion
The surveyed WFH adults were aware of the majority of the important concepts on obesity. Educational attainment and socio-economic status were significant determinants of obesity awareness.
Keywords: obesity, awareness, work-from-home
INTRODUCTION
Obesity is an accumulation of excess body fat which if not treated, may lead to other serious debilitating health conditions. Unfortunately, the worldwide prevalence of obesity has tripled between 1975 and 2016. In 2016, the World Health Organization (WHO) estimated that more than 1.9 billion adults were overweight and over 650 million were obese.1 In the Philippines, the prevalence of obesity shows a gradually increasing trend as well. According to the recent Expanded National Nutrition Survey (2018), the prevalence of obesity increased from 20.2% in 1998 to 37.2 percent in 2018.2
The employed sector is not exempt from the obesity pandemic. The 2010 National Health Interview Survey conducted in the United States of America (USA) revealed that those with longer working hours and who work in companies with a large number of employees were mostly overweight or obese.3 A local study showed a 57% prevalence among employees, most of whom have sedentary work.4 This problem is expected to worsen with the recent work environment restrictions brought about by the coronavirus pandemic. Due to the work-from-home (WFH) policies intermittently imposed for long periods from 2020-2021, an overall decrease in physical activity and an increase in meal frequency and snacking was noted among the adult working population.5 , 6
Various disease conditions are linked to obesity such as cardiovascular disease, type 2 diabetes mellitus (T2DM) and cancer among others.1 It is concerning that in the 2020 Philippine Statistics Authority (PSA) data, 5 of the 10 leading causes of death were obesity-related complications.7
Obesity is even a risk factor for the dreaded severe coronavirus (COVID-19) infection which continues to wreak havoc on our country and the world.8 With its devastating effects on health, WHO declared an obesity epidemic in 1997 and spearheaded public awareness campaigns. They also developed “A Global Action Plan on Physical Activity for 2018-2030,” to address this pressing problem.1
In our country, the National Nutrition Council of the Department of Health conducted virtual forums on obesity awareness to continue the advocacy, promotion and provision of health and nutrition information to the general public during the COVID-19 pandemic.9 Moreover, various medical societies formulated clinical practice guidelines to guide clinical practitioners. In the Philippines, there are clinical practice recommendations on obesity from the Philippine Association for the Study of Overweight and Obesity (PASOO) and the Family Medicine Research Group (FMRG) Guidelines of the University of the Philippines-Philippine General Hospital.10
Huge advancements in diagnosis have taken place over the years. While body mass index (BMI) is still commonly used to diagnose obesity, numerous imaging procedures are now utilized to refine this diagnosis. Similarly, development of obesity treatment strategies proceeds at an accelerated pace, with numerous pharmacologic and surgical interventions to complement the fundamentally crucial adherence to diet, lifestyle and behavioral modification.11 Multiple programs from government and the private sector were initiated to help solve the obesity problem, including information campaigns and lay fora on obesity and the operation of weight loss clinics.12,13
Unfortunately, in spite of all these interventions, the incidence of obesity continues to rise. Awareness and a substantial understanding of its pathophysiology and its consequences are essential components in its prevention and treatment. Several studies involving students, employees and the general population revealed that these cohorts have ample knowledge on the basic concepts of obesity, specifically its risk factors.14-16 However, one study highlighted the public’s unawareness on the link of obesity to cancer.17 Majority were also unfamiliar about treatment options and most do not try to prevent themselves from becoming obese.
To date, there is no local data evaluating the degree of knowledge of this disease, especially among the employed, who are at most risk of becoming obese due to their current WFH set up. We lack evidence locally whether sociodemographics play a role in influencing the degree of obesity awareness.
The general objective of this study was to determine the awareness on obesity and its relationship to various socio-demographic variables among Filipino adults WFH in Metro Cebu, Philippines. The specific objectives were: (1) to describe the study population’s sociodemographic profile; (2) to assess their level of awareness according to the following: obesity as a disease and its risk factors, complications, diagnosis and management of obesity and (3) to determine if a relationship exists between the degree of obesity awareness and the sociodemographic factors studied.
METHODOLOGY
This was a cross-sectional survey conducted in Metro Cebu, Philippines, which included Filipino adult WFH employees aged 18 years and above. Subjects were non-healthcare professionals and were self-employed or employed in a company under a full WFH scheme/set-up or combined office work-WFH set-up during the survey period.
Excluded from the study were healthcare professionals such as medical doctors, nursing professionals, midwives, dentists, pharmacists, nurse practitioners, physician's assistants, emergency medical technicians, dieticians and nutritionists, and physiotherapists.18
A sample size of at least 384 respondents was computed using EPI Info Stat Calculator for population surveys/descriptive studies and was based on the Philippines Statistics Authority (PSA) - Region VII’s labor force census.19
This study sampled workers using the non-probability snowball sampling method from specified cities in Metro Cebu to ensure that these areas are well represented. Researchers had key contact persons—WFH employees from Cebu City, Mandaue City, Lapu-Lapu City and Talisay City. These key persons were asked to recruit other participants to join this study. Recruitment was done via various social media apps and email until the required sample size was surpassed.
The respondents were asked to answer a researcher-made instrument. The first part of the tool gathered various sociodemographic characteristics of WFH employees such as age, sex, marital status, height, weight, BMI, highest educational attainment, socio-economic status based on monthly household income, hours of work per day and hours of physical activity/exercise per day.
The second part, the Obesity Awareness Questionnaire (OAC-20), assessed the respondents’ awareness on obesity. OAQ-20 is made up of 20 items covering the following: obesity as a disease and its risk factors (7 items), complications of obesity (7 items), diagnosis of obesity (2 items) and management of obesity (6 items). All statements in the questionnaire were true regarding obesity. Respondents answered questions covering the aforementioned areas using a 5-point Likert Scale: 5-strongly agree, 4-agree, 3-undecided, 2-disagree and 1-strongly disagree.
The research instrument was subjected to content validity and reliability testing procedures. Content validity was done by a panel of experts: endocrinologists, clinical nutritionists and other internists. Content Validity Indices such as Item-level Content Validity Index (I-CVI) and Scale-Level Content Validity Index (S-CVI) were calculated. Furthermore, Attribute Agreement Analysis, a form of inter-reliability measure, was done to assess whether the experts’ relevance ratings were consistent with one another and if observer agreement was due to chance or not.
Content validation was done in the original 22-item tool. I-CVI is 1.00 for all items except 8 and 18. S-CVI is 0.98. All content validity indices were acceptable, thus, the proposed obesity awareness questionnaire achieved a satisfactory level of content validity. Items 8 and 18 were omitted in the final tool. To determine whether agreement among experts was due to chance, the p-values for each attribute’s Fleiss Kappa were compared to the significance level. With the p<0.05, all appraiser agreements then were not due to chance. Assessments made for each item, therefore, were consistent among appraisers and thus, reliable.
Finally, a total of 3 rounds of pre-testing was conducted. Results of these pre-tests were the bases for internal consistency or reliability testing (Cronbach’s alpha), and item analyses. The tool was evaluated as a unidimensional instrument, all 20 items measuring a single latent trait, in this case, obesity awareness. The over-all Cronbach alpha was 0.86. With a relatively high coefficient, this means that the items of the survey can reliably assess the same construct, obesity awareness, whether among healthcare professional or lay persons.
The Cronbach alpha for each sub-construct were as follows: obesity as a disease and its risk factors (7 items), 0.7; complications of obesity (7 items), 0.9; diagnosis of obesity (2 items), 0.4; and management of obesity (4 items), 0.4. The low value of alpha for the last two groupings could be due to the small number of questions, which came from a decision to include only extremely necessary items.
For example, the clinical diagnosis of obesity relies primarily on the patient’s BMI and/or waist circumference, hence, only these 2 were included in the assessment of awareness on the diagnosis of obesity.
Furthermore, the proposed instrument measures obesity awareness among the general public who we do not expect to be aware of less commonly used diagnostic measures which are costly, unstandardized or not widely available. So, BMI and/or waist circumference would suffice in both clinical and general settings. The same principle was applied in the finalization of the items for the management of obesity.
Nevertheless, we feel that these low ratings in the last 2 groupings should not devalue the proposed instrument, as alphas have been proven to be affected by the number of questions. Also, all 4 were necessary sub-constructs of obesity awareness as per content validation. There is a need to look into all these key areas to properly represent the entire spectrum of obesity awareness.
Remarkably, the Cronbach alpha for the non-healthcare professionals pre-testing and that of the healthcare professionals pre-testing were similar, 0.79 and 0.80, respectively. With similar Cronbach alpha values (≅0.80) for both test groups, this further indicates that items meant to assess awareness obesity may work for both populations.
The validated questionnaire was also translated into the Bisaya language. Forward translation was done by a certified linguist who is fluent in both the source and target language and is knowledgeable about health care terminology. The linguist was briefed by the authors regarding the content area of the construct of the instrument in the desired target language. Another linguist of the same caliber was tasked to perform blind back-translation.
The instructions, items and the response format of the translated and back-translated versions of the instruments were compared to the original regarding ambiguities and discrepancies of words, sentences and meanings. All comparisons were discussed, ambiguities and discrepancies were dealt with and resolved. Consensus was achieved thus generating the Bisaya version of the Obesity Awareness Questionnaire (OAC-20-B). The said version was subjected to the same rounds of pre-testing as indicated above. The over-all computed Cronbach’s alpha was 0.90.
Actual data collection was done from June 15 to July 31, 2021. Due to COVID-19 pandemic restrictions and for the safety of researchers and respondents, a self-administered survey was conducted online via Google Forms. The study was approved by the Cebu Doctors’ University Hospital Technical Review Board and Institutional Research Ethics Committee.
In the analysis of data, descriptive statistics (mean, SD, median, IQR, minimum and maximum Values) were used to describe the distribution of WFH employees in terms of numerical profile characteristics and obesity awareness assessment scores of respondents. Frequency and simple percentage were used to determine the distribution of respondents in terms of different categorical variables. Spearman’s Correlation was used to determine if there was association between numerical variables such as awareness scores and numerical/ordinal profile variables. Mann-Whitney U Test was used to determine if there was significant difference between 2 groups of respondents in terms of their obesity awareness scores. For all tests, confidence interval was set at 95%, relationship or comparison significant at <0.05, all hypotheses were tested at 0.05 level of significance. Data were entered with Microsoft Excel Spreadsheet and then analyzed with Minitab version 19.0 for Mac Mojave OS.
RESULTS
A total of 458 WFH employees participated in the study. As shown in Table 1, the mean age of the cohort was 30.33 years and ranged from 18-64 years. There were 327 females (71.40%) and 131 males (28.6%). The married respondents comprised 22.93% of the population and 77.07% were single.
Table 1.
Sociodemographic characteristics of work-from-home employees in Metro Cebu
| Respondents' sociodemographic profile | N=458 | ||
|---|---|---|---|
| Mean (SD) | Median (IQR) | Min-Max | |
| Age in years | 30.33 (6.96) | 29 (26-33) | 18-64 |
| Height in m | 1.59 (0.09) | 1.58 (1.52-1.65) | 1.25-1.88 |
| Weight in kg | 63 (15.73) | 60 (53-70) | 30-155 |
| BMI in kg/m2 | 24.75 (5.13) | 24.1 (21.7-26.6) | 12.82-64.08 |
| Number | % | ||
| Age groups | |||
| Teens | 2 | 0.44 | |
| Twenties | 250 | 54.59 | |
| Thirties | 168 | 36.68 | |
| Forties | 27 | 5.90 | |
| Fifties | 8 | 1.75 | |
| Sixties | 3 | 0.66 | |
| BMI classification (Asian) | |||
| Underweight | 20 | 4.42 | |
| Normal | 159 | 35.18 | |
| Overweight | 85 | 18.81 | |
| Pre-Obese | 148 | 32.74 | |
| Obese | 40 | 8.85 | |
| Sex | |||
| Female | 327 | 71.40 | |
| Male | 131 | 28.60 | |
| Marital status | |||
| Single | 353 | 77.07 | |
| Married | 105 | 22.93 | |
| Highest educational attainment | |||
| Elementary | 2 | 0.44 | |
| High school | 16 | 3.49 | |
| College | 378 | 82.53 | |
| Graduate (master’s) studies | 59 | 12.88 | |
| Post-graduate (doctorate) | 3 | 0.66 | |
| studies | |||
| Respondents' sociodemographic profile | N=458 | ||
| Number | % | ||
| Socio-economic status based on monthly household income | |||
| Level 1-Less than PhP 10,481 | 32 | 7.06 | |
| Level 2-Between PhP 10,481 and PhP 20,962 | 127 | 28.04 | |
| Level 3-Between PhP 20,962 and PhP 41,924 | 164 | 36.20 | |
| Level 4-Between PhP 41,924 and PhP 73,367 | 63 | 13.91 | |
| Level 5-Between PhP 73,367 and PhP 125,772 | 33 | 7.28 | |
| Level 6-Between PhP 125,772 and PhP 209,620 | 16 | 3.53 | |
| Level 7-PhP 209,620 and above | 18 | 3.97 | |
| Hours of work per day | |||
| Less than 8 hours | 93 | 20.31 | |
| 8 hours | 314 | 68.56 | |
| 12 hours | 39 | 8.52 | |
| More than 12 hours | 12 | 2.62 | |
| Hours of physical activity/exercise per day | |||
| Less than 30 minutes | 237 | 51.97 | |
| About 30 minutes | 113 | 24.78 | |
| About 1 hour | 72 | 15.79 | |
| About 2 hours | 21 | 4.61 | |
| More than 2 hours | 13 | 2.85 | |
Self-reported height ranged from 1.25-1.88 meters while the self-reported weight ranged from 30-155 kg. Majority of the respondents had reported BMIs that were above normal. Using the Asia-Pacific cutoff, the computed BMI revealed 20 (4.42%) respondents were underweight, 159 (35.18%) were normal, 85 (18.81%) were overweight, 148 (32.74%) were pre-obese and 40 (8.85%) were obese.
Majority of the respondents were college graduates (82.53%) and more than 50% of respondents had level 2-3 monthly household income (PhP 10,481 to 41,924). Sixty-nine percent of the WFH employees worked 8 hours per day. It is noteworthy that more than half of the respondents had only 30 minutes or less of physical activity/exercise per day.
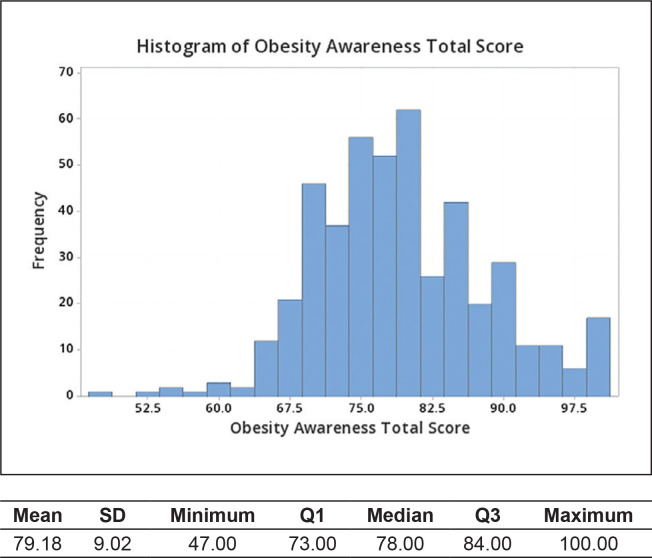
As shown in Figure 1, the mean total obesity awareness score of the respondents was 79.18 with a standard deviation of 9.02 points. The lowest score was 47. About 25% of the awareness scores in the sampled population were less than or equal to 73 (Q1). The median score was 78, which means that half of the sampled population scored below this value. About 25% of the scores in the sampled population were greater than 84, i.e., 75% of the respondents scored 84 and below in obesity awareness. The highest obesity awareness score was 100.
Figure 1.
Summary of respondents’ total obesity awareness scores.
To better understand the respondents’ awareness on obesity, item scores were computed and these are presented in Table 2. When it comes to obesity as a disease and its risk factors, most respondents were aware that hormonal imbalances can affect a person’s weight. The mean score for this item was 4.30 (SD=0.63). WFH employees, however, were least aware of how common obesity is among Filipinos. The mean score for that item was 3.51 (SD=1.23).
Table 2.
Respondents’ scores on obesity awareness
| Subscales and items on obesity awareness | N=458 | |||
|---|---|---|---|---|
| Mean (SD) | Median (Q1-Q3) | Subscale awareness ranking | Overall awareness ranking | |
| Obesity as a disease and its risk factors | ||||
| 1-Obesity is a disease. | 3.96 (1.06) | 4 (3-5) | 5 | 12 |
| 2-Obesity is not rare among Filipinos. | 3.51 (1.23) | 4 (2-4) | 7 | 19 |
| 3-Overeating is not the only known cause of obesity. | 4.17 (0.87) | 4 (4-5) | 3 | 7 |
| 4-People who have minimal physical activity are at risk for obesity. | 4.19 (0.86) | 4 (4-5) | 2 | 6 |
| 5-Certain medications such as steroids may contribute to weight gain. | 3.90 (0.83) | 4 (3-5) | 6 | 13 |
| 6-Genes have a role in the development of obesity | 4.05 (0.74) | 4 (4-5) | 4 | 10 |
| 7-Hormonal imbalances can affect a person’s weight. | 4.30 (0.63) | 4 (4-5) | 1 | 2 |
| Complications of obesity | ||||
| 8-Obesity is associated with elevated blood pressure and cardiovascular diseases. | 4.22 (0.78) | 4 (4-5) | 1 | 4 |
| 9-Being overweight increases one’s risk of developing colon cancer. | 3.72 (0.83) | 4 (3-4) | 6 | 16 |
| 10-Obesity is a risk factor for severe COVID 19 disease. | 3.68 (1.02) | 4 (3-5) | 7 | 17 |
| 11-Type II Diabetes mellitus is related to obesity. | 3.79 (0.85) | 4 (3-4) | 4 | 14 |
| 12-Overweight can be related to infertility. | 3.73 (0.91) | 4 (3-4) | 5 | 15 |
| 13-Obesity has been linked to Fatty Liver and Gallbladder diseases. | 4.08 (0.79) | 4 (4-5) | 2 | 9 |
| 14-Depression is considered both a risk factor and a complication of obesity | 4.04 (0.81) | 4 (4-5) | 3 | 11 |
| Diagnosis of obesity | ||||
| 15-Body Mass Index is used to determine whether a person is overweight or not. | 4.31 (0.74) | 4 (4-5) | 1 | 1 |
| 16-Obesity can be diagnosed by determining Waist Circumference. | 3.32 (1.09) | 3 (2-4) | 2 | 20 |
| Management of obesity | ||||
| 17-When one is trying to lose weight, it is ideal to seek professional advice. | 4.19 (0.76) | 4 (4-5) | 2 | 5 |
| 18-Moderate intensity exercises, such as brisk walking, can help you achieve a healthy weight. | 4.22 (0.71) | 4 (4-5) | 1 | 3 |
| 19-Taking weight loss medications is not enough to manage obesity. | 4.12 (0.87) | 4 (4-5) | 3 | 8 |
| 20-There are surgical options that can help treat obesity. | 3.68 (0.87) | 4 (3-4) | 4 | 18 |
In terms of complications, most respondents were aware that obesity is associated with elevated blood pressure and cardiovascular diseases as evidenced by a mean item score of 4.22 (SD=0.78). However, they were relatively less aware that obesity is actually associated with T2D, infertility, colon cancer and severe COVID-19 infection.
As far as diagnosis of obesity is concerned, most of the respondents were aware that BMI is commonly used to determine if a person is overweight or not, as evidenced by a mean item score of 4.31 (SD=0.74). However, much of the sampled population did not know that obesity can also be diagnosed by measuring waist circumference as well. A mean score of 3.32 (SD=1.09) supported this finding.
Respondents were also assessed in terms of their awareness in the management of obesity. WFH employees were aware that moderate intensity exercises can help achieve a healthy weight (mean score 4.22, SD=0.71) and that professional advice should be sought before losing weight (mean score 4.19, SD=0.76). On the other hand, only a few were aware that there are surgical treatment options for obesity (mean score 3.68, SD=0.87).
Table 3 presents the results when assessing the relationship (or differences in terms sex and marital status) between the obesity awareness scores and various sociodemographic variables of the respondents. Age (p=0.198), BMI (p=0.397), hours of work per day (p=0.465) and hours of physical activity per day (p=0.765) were not associated with obesity awareness among the studied population. Sex (p=0.515) and marital status (p=0.629) were also not significantly associated with obesity awareness. On the other hand, educational attainment (p=0.044) and socio-economic status (p=0.002) were both associated with the respondents’ obesity awareness scores. For highest educational attainment and obesity awareness, the computed value (Spearman’s Rho) of 0.1 indicates that a positive monotonic correlation exists between the 2 variables. This means that higher levels of education were associated with higher obesity awareness scores. There was also a positive monotonic correlation between socio-economic status and obesity awareness scores as indicated by the computed value of 0.147. Similarly, higher socio-economic statuses were associated with higher obesity awareness scores. It must be noted, however, that these correlations do not imply a causal relationship (cause and effect).
Table 3.
Awareness on obesity and sociodemographic characteristics
| Variables | Computed Values | p |
|---|---|---|
| Obesity awareness and | ||
| Age | 0.060 a | 0.198 |
| Sex | Female η1=78; Male η2=78b |
0.515 |
| Marital status | Married η1=78; Single η2=79b |
0.629 |
| Body Mass Index | 0.040a | 0.397 |
| Highest educational attainment | 0.094a | 0.044 |
| Socio-economic status | 0.147a | 0.002 |
| Hours of work per day | 0.077a | 0.101 |
| Hours of physical activity per day | 0.035a | 0.458 |
Spearman’s rho; value computed using Spearman’s Rank Correlation; significant at <0.05
Median values; Comparison done with Mann-Whitney U Test; significant at <0.05
DISCUSSION
In the Philippines, the prevalence of obesity showed a gradual increasing trend with 3 out of 10 adult Filipinos being overweight and obese.2 To date, there are no studies focusing on obesity awareness among Filipinos, much less on the locally-employed sector.
The sampled population of Filipino adults WFH in Metro Cebu were aware of most of the important concepts on obesity as a disease and its risk factors, complications, diagnosis and management as evidenced by an overall average score of 79.18%, covering therefore nearly 80% of the salient facts regarding obesity. Perhaps the ease of accessing information through the internet may be the reason for their high level of awareness. The results in other countries are polarized with studies in China, Pakistan and India revealing cohorts who were knowledgeable on the core principles of obesity while studies done in the USA and United Kingdom (UK) showed otherwise.14-17,20
The item that the respondents were most aware of is that BMI is a diagnostic tool for obesity. This is because BMI is commonly used and is regarded as the most useful population-level measure of overweight and obesity.1 The second highest ranking in the overall awareness is that hormonal imbalances can affect a person’s weight. Hormonal influence is usually cited as one of the causes of obesity.21 Although we are unsure how the respondents are particularly aware of this fact, it is nevertheless reassuring to know that this cohort realizes that obesity is a multifactorial condition, requiring holistic treatment and inputs from multiple disciplines.
On the other hand, the knowledge of waist circumference as an obesity diagnostic tool had the lowest awareness score. This was similarly noted in a study by Dunkley et al., (2009) were almost half the subjects had no previous knowledge of the importance of waist circumference measurement in screening for obesity.22
Majority of the respondents are not aware of the increasing prevalence of obesity in the country. This might be because many people are unable to recognize those who are already overweight/obese which is supported in studies by Nanda (2021) and DeVille-Almond et al (2011).20,23 This may be problem because recognizing a disease condition precedes treatment. In spite of the development of obesity treatment strategies,11 our study revealed that too many respondents were still unaware that there are surgical options for treating obesity. This is likely because surgery is not usually discussed with the patient at the onset of treatment. Lifestyle and behavioral modifications are rightfully given greater emphasis in obesity management.1 Surgical options such as gastric bypass are only suitable for a select group of morbidly obese patients or obese patients with co-morbidities.11
Only a few respondents recognized cancer as an obesityrelated complication,17 including in our study were mostly it ranked at the bottom half of the overall awareness ranking. This relatively low awareness regarding obesity and its complications is concerning since 5 of the 10 leading causes of death are obesity-related according to the 2020 PSA data.7
Despite having sufficient awareness about obesity, the majority of the respondents had reported BMIs above normal. This is probably due to the significant reduction in physical activity, along with the tendency to overeat due to the sudden shift to WFH set-up for millions of employees around the world, the Philippines included, during the COVID-19 pandemic.24-27 Another possible explanation of abnormal BMIs despite sufficient awareness is their misperception of weight and obesity, common among overweight/obese adults.23 Nanda et al., showed that only a few persons knew their BMIs.20
In addition, our study showed the respondents were knowledgeable on the nature of obesity, how it develops, what its predisposing factors are, and how to combat the disease. However, they were relatively less informed on its complications. This might be why this cohort is wellversed on obesity but are themselves above their ideal weight. Knowledge can strengthen one's determination to adhere to approved medical measures to treat obesity. By educating the public on the serious complications of obesity, the problem will transcend mere aesthetics and may motivate people to avoid and prevent this medical condition.
A previous study by the Canadian Institute for Health Information (2011) has concluded that there were associations between the sociodemographic factors and the likelihood of being overweight or obese.28 However, this study did not assess the level of obesity awareness.
Our study also showed that obesity awareness is significantly related to the socioeconomic status. The higher the household monthly income, the higher the level of awareness. This may be due to the more ready access to obesity education similar to a study in Latin America.29
There was also a significant relationship between higher educational attainment and obesity awareness. Those with lower educational levels were expected to score low, thus, less likely to be knowledgeable in lifestyle diseases such as obesity.30 Having said that, it is interesting to note that the latest National Nutrition Survey showed that higher educational attainment had higher odds of becoming overweight/obese.31 This implies that there is a gap in the knowledge on obesity and in the application of its concepts.
In interpreting the results of the study, there were few limitations that should be considered. Our study was sampled via non-probability, snow-ball sampling due to COVID-19 restrictions. Further, the weight and the height of the respondents were self-reported. Thus, responses were limited to the honesty of the participants. Also, this study did not look into confounding variables such as the participant’s access to social media, awareness of current events, current medical conditions and access to a healthcare practitioner which might have influenced awareness.
CONCLUSION
The sampled population of Filipino adults WFH in Metro Cebu were aware of majority of the important concepts on obesity as a disease and its risk factors, complications, diagnosis and management.
Age, BMI, hours of work per day, and hours of physical activity per day were not associated with obesity awareness among the studied population. Similarly, male and female, as well as single and married respondents do not differ significantly in terms of their average obesity awareness scores. However, higher educational attainment and socio-economic status were associated with higher obesity awareness.
Recommendations
This study provides novel information on the awareness on obesity among Cebuanos. However, the researchers recommend that a larger and a more diverse population be studied. Larger studies may also be done to establish cut-off scores. We also recommend community-wide workshops, not just lectures, with greater emphasis on the application of learned concepts.
Statement of Authorship
The authors certified fulfillment of the ICMJE authorship criteria.
CRediT Author Statement
JLG: Conceptualization, Methodology, Investigation, Resources, Writing – original draft preparation, Writing – review and editing, Visualization, Funding Acquisition; AC: Conceptualization, Methodology, Investigation, Resources, Writing – original draft preparation, Writing – review and editing, Visualization, Funding Acquisition; TL: Conceptualization, Methodology, Investigation, Writing – original draft preparation, Writing – review and editing, Supervision. Project Administration; AP: Methodology, Software, Validation, Formal analysis, Writing – original draft preparation, Writing – review and editing.
Author Disclosure
The authors declared no conflict of interest.
Funding Source
None.
References
- 1.Obesity and overweight. World Health Organization. Accessed November 4, 2021. https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight. [Google Scholar]
- 2.Patalen CF. Health and Nutritional Status of Filipino Adults, 20-59 years old. Accessed November 4, 2021. http://enutrition.fnri.dost.gov.ph/site/uploads/Adults_and_Elderly.pdf.
- 3.Park S, Pan L, Lankford T. Relationship between employment characteristics and obesity among employed U.S. Adults. Am J Health Promot. 2014;28(6):389-96. PMID: . PMCID: . 10.4278/ajhp.130207-QUAN-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degay IO. Prevalence of overweight and obesity among employees of selected regional line agencies in the Cordillera Administrative Region, Philippines. MJSIR. 2019;79 (2 Suppl 1):90-100. [Google Scholar]
- 5.Abed Alah M, Abdeen S, Kehyayan V, Bougmiza I. The Impact of Changes in Work Arrangements During COVID-19 Pandemic on the Lifestyle of Qatar's Working Population. J Occup Environ Med. 2022. Feb 1;64(2):e53-e59. doi: 10.1097/JOM.0000000000002443. PMID: ; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bennett G, Young E, Butler I, Coe S. The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: A scoping review. Front Nutr. 2021;8:626432. PMID: . PMCID: . 10.3389/fnut.2021.626432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Causes of deaths in the Philippines (Preliminary): January to December 2020. Philippine Statistics Authority. Accessed November 4, 2021. https://psa.gov.ph/content/causes-deaths-philippines-preliminary-january-december-2020. [Google Scholar]
- 8.CDC . Underlying medical conditions associated with higher risk for severe COVID-19: Information for healthcare providers. Accessed November 4, 2021. Cdc.gov. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html.
- 9.Palaubsanon ML. Nutrition council: Eat healthy food. The Philippine Star. September 28, 2020. Accessed November 4, 2021. https://www.philstar.com/the-freeman/cebu-news/2020/09/28/2045684/nutrition-council-eat-healthy-food. [Google Scholar]
- 10.Jasul G, Philippine Association for the Study of Overweight and Obesity . Obesity treatment recommendations in the Philippines: Perspective on their utility and implementation in clinical practice. J ASEAN Fed Endocr Soc. 2011;26(2):122–8. [Google Scholar]
- 11.Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. Harrison’s Principles of Internal Medicine, vol. 1, 20th ed. McGrawHill Education/Medical; 2018. [Google Scholar]
- 12.Novo Nordisk PH launches #BeatObesityWithMe movement during World Obesity Day. Inquirer.net. March 30, 2021. Accessed November 4, 2021. https://globalnation.inquirer.net/194689/novo-nordisk-philippines-launches-beatobesitywithme-movement-as-it-celebrates-world-obesity-day. [Google Scholar]
- 13.Surhone LM, Timpledon MT, Marseken SF, et al. OpenVPN: Virtual Private Network, Pre-Shared Key, Certificate Authority, NetBSD, FreeBSD, OpenBSD, Linux, Solaris (Operating System), Transport Layer Security. Betascript Publishing; 2010. [Google Scholar]
- 14.Xue B, Zhang X, Li T, et al. Knowledge, attitude, and practice of obesity among university students. Ann Palliat Med. 2021;10(4):4539-46. PMID: . 10.21037/apm-21-573. [DOI] [PubMed] [Google Scholar]
- 15.Laar RA, Shusheng S, Ashraf MA, Khan MN, Bibi J, Liu Y. Impact of physical activity on challenging obesity in Pakistan: A Knowledge, Attitude, and Practice (KAP) Study. Int J Environ Res Public Health. 2020;17(21):7802. PMID: . PMCID: . 10.3390/ijerph17217802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jajulwar M, Meshram P, Saji D. To assess the knowledge, attitude and practices of people regarding overweight and obesity: A crosssectional study. Int J Community Med Public Health. 2017;4(9):3113-6. 10.18203/2394-6040.ijcmph20173634. [DOI] [Google Scholar]
- 17.Hooper L, Anderson AS, Birch J, et al. Public awareness and healthcare professional advice for obesity as a risk factor for cancer in the UK: A cross-sectional survey. J Public Health (Oxf). 2018;40(4):797–805. PMID: . PMCID: . 10.1093/pubmed/fdx145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Transforming and scaling up Health Professionals' Education and Training: World Health Organization Guidelines 2013. Geneva: World Health Organization; 2013. Annex 1, Definition and list of health professionals. Accessed January 7, 2022. https://www.ncbi.nlm.nih.gov/books/NBK298950/. [PubMed] [Google Scholar]
- 19.July 2020 employment situation of Central Visayas. Philippine Statistics Authority: Region VII-Central Visayas. Accessed November 5, 2021. http://rsso07.psa.gov.ph/article/july-2020-employment-situation-central-visayas. [Google Scholar]
- 20.Nanda S, Mohabbat AB, Nagaraju D, et al. Improving awareness of patients with obesity and its healthcare implications. Qual Prim Care. 2015;23(4):201-4. Accessed November 5, 2021. https://primarycare.imedpub.com/improving-awareness-of-patients-with-obesityand-its-healthcare-implications.pdf. [Google Scholar]
- 21.Obesity. Mayoclinic.org. Accessed November 5, 2021. https://www.mayoclinic.org/diseases-conditions/obesity/symptoms-causes/syc-20375742. [Google Scholar]
- 22.Dunkley AJ, Stone MA, Patel N, Davies MJ, Khunti K. Waist circumference measurement: knowledge, attitudes and barriers in patients and practitioners in a multi-ethnic population. Fam Pract. 2009;26(5):365–71. PMID: . 10.1093/fampra/cmp048. [DOI] [PubMed] [Google Scholar]
- 23.DeVille-Almond J, Tahrani AA, Grant J, Gray M, Thomas GN, Taheri S. Awareness of obesity and diabetes: A survey of a subset of British male drivers. Am J Mens Health. 2011;5(1):30–7. PMID: . 10.1177/1557988309359803. [DOI] [PubMed] [Google Scholar]
- 24.Van Der Meer E. Why working from home can make you put on weight (and how to stop it). Accessed November 5, 2021. https://coach.nine.com.au/lifecoach/working-from-home-weight-gain/751c8cdf-a902-4d8e-8b58-7f1830b30e09.
- 25.Physical inactivity is a leading cause of disease and disability, warns WHO. J Adv Nurs. 2002;39(6):518. PMID: . [PubMed] [Google Scholar]
- 26.Technology and the evolving world of work. Global Research Study; 2020. Accessed November 5, 2021. https://news.lenovo.com/wp-content/uploads/2020/07/Technology-and-the-Evolving-World-of-Work_Lenovo-IDG-Global-Research-Report_FINAL.pdf. [Google Scholar]
- 27.Pearl RL. Weight stigma and the “quarantine-15.” Obesity (Silver Spring). 2020;28(7):1180–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Craig CL, Cameron C, Cameron C, et al. Socio-demographic and lifestyle correlates of obesity: Technical report on the secondary analyses using the 2000-2001 Canadian Community Health Survey. Canadian Institute for Health Information; 2005. Accessed November 27, 2022. https://policycommons.net/artifacts/1222383/socio-demographic-and-lifestyle-correlates-of-obesity/1775459/. [Google Scholar]
- 29.McArthur L, Peña M, Holbert D. Effects of socioeconomic status on the obesity knowledge of adolescents from six Latin American cities. Int J Obes (Lond). 2001;25(8):1262–8. PMID: . 10.1038/sj.ijo.0801674. [DOI] [PubMed] [Google Scholar]
- 30.Ndungi F, Egerton University . Socio-economic status, knowledge, awareness and attitudes of the Swahili community in relation to dietary habits, obesity and lifestyle diseases. Afr J Food Agric Nutr Dev. 2017;17(01):11709–26. 10.18697/ajfand.77.16335. [DOI] [Google Scholar]
- 31.Duante CA, Canag JLQ, Patalen CF, Austria REG, Acuin CCS. Factors associated with overweight and obesity among adults 20.0 years and over: Results from the 2013 National Nutrition Survey, Philippines. Philipp J Sci. 2019;148(1):7-20. https://philjournalsci.dost.gov.ph/images/pdf/pjs_pdf/vol148no1/factors_associated_with_overweight_and_obesity_among_adults_.pdf. [Google Scholar]