Abstract
Investments in digital health technologies such as artificial intelligence, wearable devices, and telemedicine may support Africa achieve United Nations (UN) Sustainable Development Goal for Health by 2030. We aimed to characterize and map digital health ecosystems of all 54 countries in Africa in the context of endemic infectious and non-communicable diseases (ID and NCD). We performed a cross-national ecological analysis of digital health ecosystems using 20-year data from the World Bank, UN Economic Commission for Africa, World Health Organization, and Joint UN Programme on HIV/AIDS. Spearman’s rank correlation coefficients were used to characterize ecological correlations between exposure (technology characteristics) and outcome (IDs and NCDs incidence/mortality) variables. Weighted linear combination model was used as the decision rule, combining disease burden, technology access, and economy, to explain, rank, and map digital health ecosystems of a given country. The perspective of our analysis was to support government decision-making. The 20-year trend showed that technology characteristics have been steadily growing in Africa, including internet access, mobile cellular and fixed broadband subscriptions, high-technology manufacturing, GDP per capita, and adult literacy, while many countries have been overwhelmed by a double burden of IDs and NCDs. Inverse correlations exist between technology characteristics and ID burdens, such as fixed broadband subscription and incidence of tuberculosis and malaria, or GDP per capita and incidence of tuberculosis and malaria. Based on our models, countries that should prioritize digital health investments were South Africa, Nigeria, and Tanzania for HIV; Nigeria, South Africa, and Democratic Republic of the Congo (DROC) for tuberculosis; DROC, Nigeria, and Uganda for malaria; and Egypt, Nigeria, and Ethiopia for endemic NCDs including diabetes, cardiovascular disease, respiratory diseases, and malignancies. Countries such as Kenya, Ethiopia, Zambia, Zimbabwe, Angola, and Mozambique were also highly affected by endemic IDs. By mapping digital health ecosystems in Africa, this study provides strategic guidance about where governments should prioritize digital health technology investments that require preliminary analysis of country-specific contexts to bring about sustainable health and economic returns. Building digital infrastructure should be a key part of economic development programs in countries with high disease burdens to ensure more equitable health outcomes. Though infrastructure developments alongside digital health technologies are the responsibility of governments, global health initiatives can cultivate digital health interventions substantially by bridging knowledge and investment gaps, both through technology transfer for local production and negotiation of prices for large-scale deployment of the most impactful digital health technologies.
Subject terms: Infectious diseases, Cardiovascular diseases
Introduction
The United Nations (UN) Sustainable Development Goal 3 (SDG 3) has been in effect since 2015 in response to the demand for ensuring healthy lives and promoting well-being for everyone by 2030, where endemic infectious and non-communicable diseases (IDs and NCDs) hold top priority. SDG 3 includes a specific target for endemic IDs (SDG 3.3) that anticipates ending by 2030 the epidemics of AIDS (SDG 3.3.1), tuberculosis (SDG 3.3.2), malaria (SDG 3.3.3), and hepatitis (SDG 3.3.4). Similarly, SDG 3 constitutes a specific target for NCDs (SDG 3.4) that anticipates reducing by 2030 one-third of premature mortality from NCDs, with target 3.4.1 focusing specifically on reducing the mortality rate attributed to diabetes mellitus, cardiovascular disease, respiratory diseases, and malignant neoplasms that account for 80% of all premature NCD deaths. In the last two decades, substantial global and domestic investments have been made to prevent and manage these diseases, including a range of options for antiretroviral treatment (ART) that helped people with HIV (PWH) live longer with the disease1–4. In contrast, the implications of longevity with IDs and their predisposition to chronic NCDs are underexplored and considerably neglected5–7.
Some of the most critical targets in SDG 3 could be addressed with the use of digital health interventions where digital and mobile technologies are used and implemented in different ways to support health system needs. These technologies could be telemedicine, artificial intelligence, wearable devices, cloud-based applications, mobile health, big data, and electronic health records. Following the onset of the COVID-19 pandemic, the utility of digital health interventions in combating IDs and NCDs has boldly come into focus8–10. For example, there were transformative tools and technologies implemented to prevent, control, diagnose, communicate, manage, and treat diseases during lockdowns and other tumultuous periods. In addition, wearable smartwatch devices have been adapted to detect physiological responses following COVID-19 vaccination10 and audio-based digital testing of COVID-1911.
There is a growing debate that digital health technologies could assist Africa in realizing the SDG 3 targets and leaving no one behind12–15. The growing need for home-grown creativity and international partnerships for co-development of digital health technologies in Africa is promising, which also coincides with the World Health Organization’s (WHO) global strategy on digital health that encourages cross-country collaboration and knowledge transfer in the area16. On the other hand, proactive investment in and deployment of digital health technologies intersects with technology characteristics of a given country, including information technology (IT) infrastructure such as access to the internet and mobile phones, electricity, technology intensity, economy, and population literacy. Countries in Africa with weak technology characteristics may fail to deploy and implement digital health technologies successfully. Simultaneously, for efficient use of scarce resources in Africa, it will be important to cultivate synergies with industry for return on investment, market access, entrepreneurship, local production, venture funds, and long-lasting effects.
Drawing on these debates and recognizing the critical role Africa is playing in global health targets and the global economy, there is a dearth of robust information about the ecological facets of digital health interventions in Africa. Important studies and policy insights inform the extent to which digital health interventions have been implemented in Africa and the barriers for the success or lack thereof17–23. Full adoption and implementation of digital health technologies in Africa require more training, access to better devices and infrastructure, and more investigations on emerging technologies including artificial intelligence, wearable devices, and big data to provide robust evidence of their potential in Africa12,15. However, literature is lacking that characterizes the cross-national dynamics of the macro-level digital health ecosystem in Africa and strategically maps countries of high priority for meaningful and sustainable effects of digital health technologies on the health and well-being of citizens.
Hence, we used international data repositories to characterize and map the digital health ecosystems of all 54 countries in Africa in the context of endemic IDs and NCDs. The research questions examined include: 1) which countries of Africa currently hold relatively better digital infrastructure to drive digital health?; 2) which countries are currently most affected by endemic IDs (HIV, TB, malaria) and NCDs (diabetes mellitus, cardiovascular disease, respiratory diseases, malignant neoplasms)?; 3) what ecological associations exist between technology characteristics and burden of IDs and NCDs in Africa?; and 4) which countries of Africa are high-priority for investment in and deployment of digital health technologies on endemic IDs and NCDs? This study aims to provide strategic guidance for governments about where to prioritize efforts in the implementation of digital health technologies in Africa as key steps to accelerate UN SDG 3 and WHO global strategy on digital health 2020–2025 targets.
Results
Technology characteristics
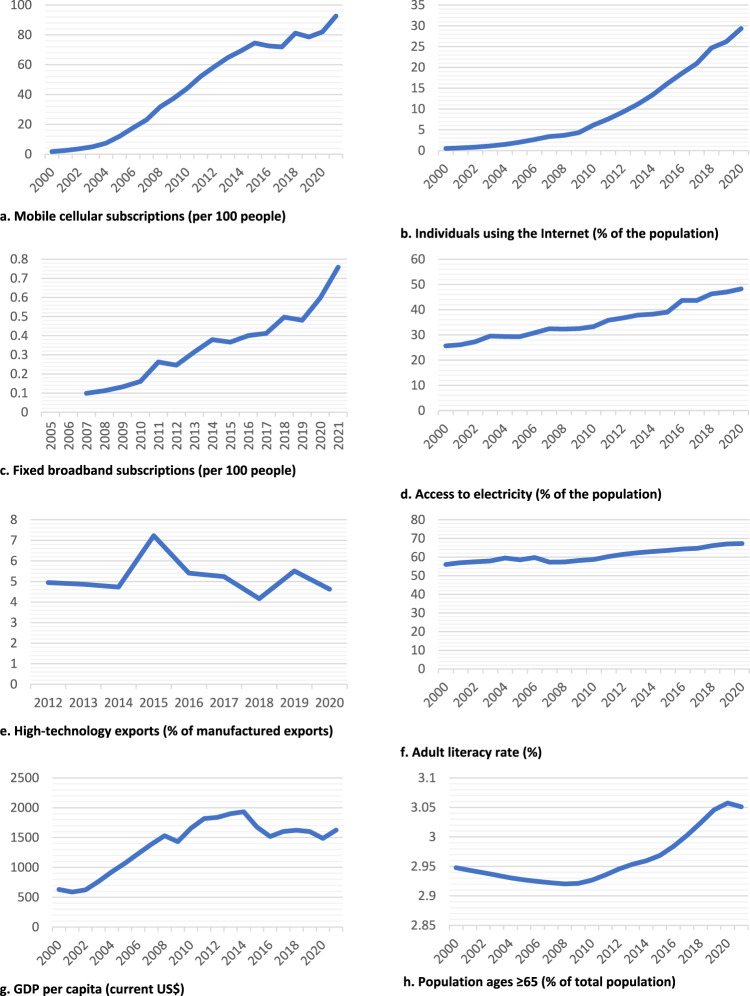
In 2022, a total estimated population of 1.4 billion people lived in Africa which includes 54 independent countries, with 30% of the population using the internet, 83% having mobile cellular subscriptions, 0.60 per 100 people having fixed broadband subscriptions, and 48.4% having access to electricity. From 2000 to 2021, increases were observed in mobile cellular subscriptions, individuals using the internet, fixed broadband subscriptions, access to electricity, GDP per capita, and adult literacy rates (Fig. 1). The continent had a GDP of US$1.92 trillion with an annual percentage growth of 4.1%, foreign direct investments totaling US$1.7 trillion, and an adult literacy rate of 66%. In 2022, the GDP per capita in Africa reached US$2,150.6, which includes all goods and services produced regardless of their purpose. The overall GDP, with international dollars (INT$) at Purchasing Power Parity (PPP), in 2021, was the highest in Egypt ($1.38 trillion), Nigeria ($1.14 trillion), South Africa ($861.93 billion), Algeria ($532.57 billion), Morocco ($302.77 billion), and Ethiopia ($298.57 billion).
Fig. 1. Trends in technology characteristics in Africa, 2000–2021.
Trends in technology characteristics in Africa, represented by (a) Mobile cellular subscriptions (per 100 people), b Individuals using the Internet (% of the population), c Fixed broadband subscriptions (per 100 people), d Access to electricity (% of the population), e High-technology exports (% of manufactured exports), f Adult literacy rate (%), g GDP per capita (current US$), h Population ages ≥ 65 (% of total population).
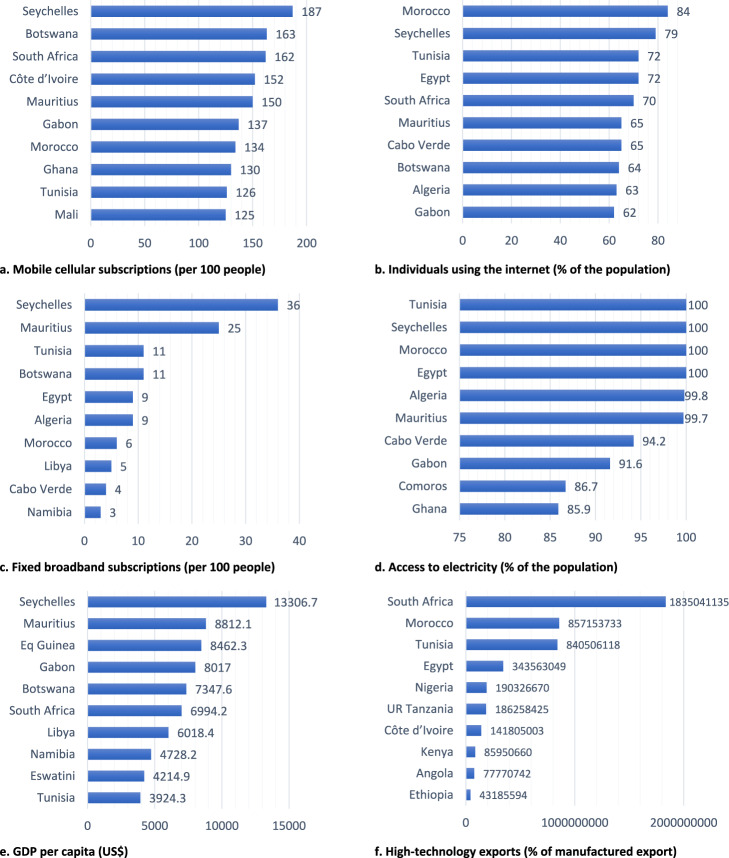
Seychelles is the leading African country in mobile and fixed broadband subscriptions, adult literacy, and GDP per capita. Morocco is the leading in individual internet users’ percentage at 84%; Tunisia, Seychelles, Morocco, and Egypt had 100% electricity access; and South Africa was the leading exporter of high-technology products, more than double that of other African countries. Figure 2 illustrates the top 10 countries by the end of 2021 in each technology characteristics variable.
Fig. 2. Top 10 countries of Africa with higher technology characteristics, 2021.
Top 10 African countries with relatively higher technology characteristics in 2021, represented by (a) Mobile cellular subscriptions (per 100 people), b Individuals using the Internet (% of the population), c Fixed broadband subscriptions (per 100 people), d Access to electricity (% of the population), e GDP per capita (current US$), f High-technology exports (% of manufactured export).
Endemic infectious and non-communicable diseases
Of the estimated 38,400,000 PWH at the end of 2021, 25,780,000 (67%) were living in Africa: 20,600,000 (79.9%) in East and Southern Africa, 5,000,000 (19.4%) in West and Central Africa, and 180,000 (0.7%) in Middle East and North Africa. In 2021, 85% of people living with HIV knew their HIV status, 88% of these were accessing ART, and 92% of those accessing ART were virally suppressed. Worldwide, an estimated 9.9 million people fell ill with TB in 2020, where 2,460,000 (25%) of cases were from Africa. Additionally, there were an estimated 241 million cases of malaria worldwide in 2020, of which 95% were from Africa. See comparision of the global versus African burden of endemic IDs in Supplementary information (refer to Supplementary Table 1).
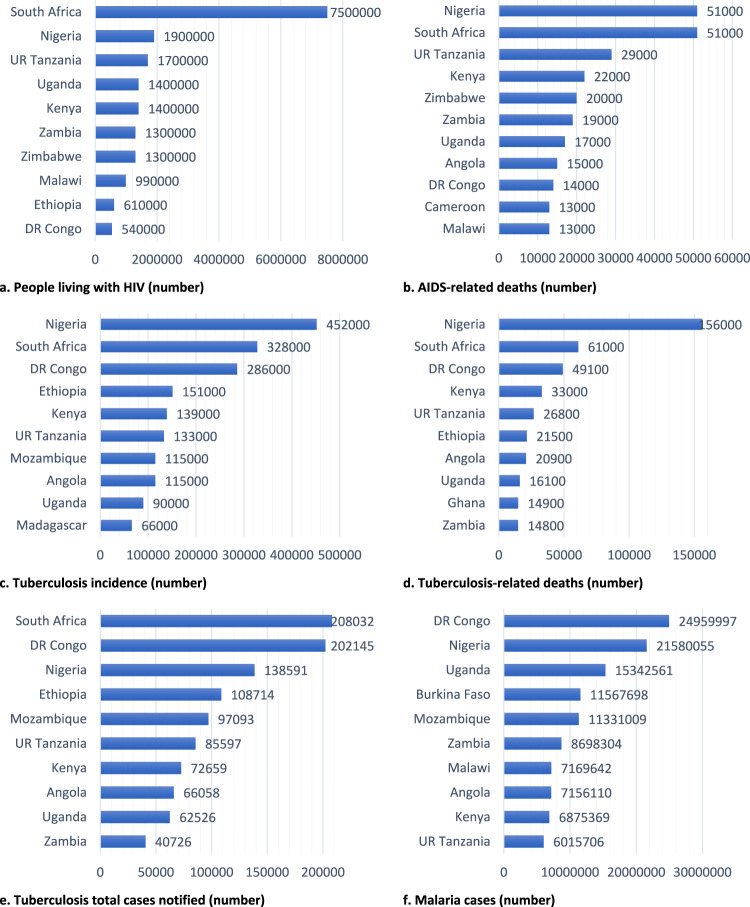
Absolute numbers of people living with HIV was the highest in South Africa [7,500,000 (32.4%)], Nigeria [1,900,000 (8.2%)], and the United Republic (UR) of Tanzania [1,700,000 (7.3%)]; TB incidence was the highest in Nigeria [452,000, (17.7%)], South Africa [328,000 (12.9%)], and Democratic Republic of Congo [286,000 (11.2%)]; and malaria cases were the highest in DR Congo [24,959,997 (14.3%)], Nigeria [21,580,255 (12.4%)], and Uganda [15,342,561, (8.8%)]. South Africa had the highest number of laboratory-confirmed MDR/RR TB cases, while Burundi and Mozambique had the highest TB treatment success rates. Tunisia was the only country that covered 100% of its TB treatment funding from domestic sources (Fig. 3).
Fig. 3. Top 10 countries of Africa with a high burden of endemic infectious diseases, 2021.
Top 10 countries of Africa with high HIV, TB, and malaria burden, represented by (a) People living with HIV (number), b AIDS-related deaths (number), c Tuberculosis incidence (number), d Tuberculosis-related deaths (number), e Tuberculosis total cases notified (number), f Malaria cases (number).
For NCDs, of the estimated 40.8 million people globally who died due to NCDs in 2019, 7.1% (2,889,945) were from Africa. Africa’s share of global disease-specific deaths was 11% for DM (1,954,067 vs. 215,071), 6.1% for cardiovascular disease (17,900,000 vs. 1,093,577), 4.5% for respiratory diseases (4,136,899 vs. 185,472), and 5.7% for malignant neoplasms (9,296,641 vs. 534,293). The 20-year trends showed that deaths due to NCDs are steadily increasing in Africa, an increase in 789,105 annual deaths compared with 2001 (2,100,840) (refer to Supplementary Fig. 1).
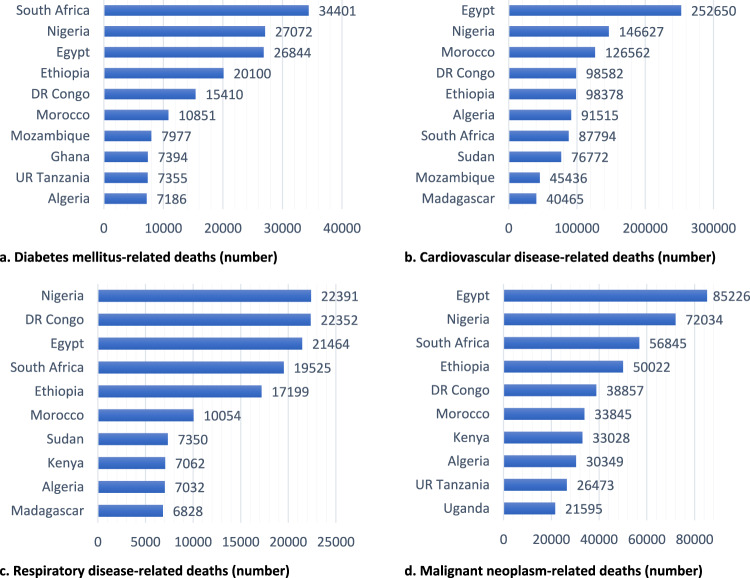
Egypt had the highest number of cardiovascular disease, malignant neoplasm, and total NCD deaths in Africa. South Africa had the largest number of diabetes-related deaths. Nigeria had the largest number of respiratory disease deaths. Mauritius had the highest prevalence of diabetes among people aged 20 to 79 (Fig. 4).
Fig. 4. Top 10 countries of Africa with a high burden of endemic non-communicable diseases, 2020.
Top 10 African countries with a high burden of endemic non-communicable diseases, represented by the number of deaths attributed to (a). diabetes mellitus, b Cardiovascular disease. c Respiratory disease. d Malignant neoplasm.
Correlation between exposure and outcome variables
Fixed broadband subscription was negatively correlated with TB incidence (r = −0.279; p = 0.043), TB-related deaths (r = −0.322; p = 0.019), and malaria incidence (r = −0.469; p = 0.001). The percentage of the population using the internet was negatively correlated with malaria incidence (r = −0.353; p = 0.016). GDP per capita was negatively correlated with TB incidence (r = −0.322; p = 0.017), TB-related deaths (r = −0.331; p = 0.015), and malaria incidence (r = −0.402; p = 0.006). Access to electricity was negatively correlated with HIV prevalence (r ≤ −0.291), TB-related deaths (r ≤ −0.281), and malaria incidence (r = −0.519); p < 0.05. High-technology capacity was negatively correlated with malaria incidence. Mobile subscriptions and adult literacy rate were not correlated with the burden of any infectious diseases (p > 0.05) An increase in high-technology exports was correlated with an increase in the burden of NCDs (r ≥ 0.651; p < 0.05), while the rest drivers of digital health variables had no association with any NCDs (Table 1).
Table 1.
Correlations between exposure (technology characteristics) and outcome (ID and NCD incidence and deaths) variables.
| Items | Mobile cellular subscription, per 100 pn. | Individuals using the Internet, % | Fixed broadband subscription, per 100 pn. | Access to electricity, % of pn | High-technology exports, US$ | Adult literacy rate, % | GDP per capita, US$ |
|---|---|---|---|---|---|---|---|
| HIV | |||||||
| People living with HIV (n) | 0.060 | −0.077 | −0.196 | −0.291* | 0.454* | 0.128 | −0.060 |
| AIDS-related deaths (n) | 0.053 | −0.078 | −0.234 | −0.327* | 0.448* | 0.084 | −0.074 |
| Tuberculosis | |||||||
| Incidence (n) | −0.147 | −0.214 | −0.279* | −0.350* | 0.538* | −0.130 | −0.322* |
| Incidence rate (per 100,000 pn) | −0.203 | −0.174 | −0.241 | −0.332* | 0.164 | 0.090 | −0.126 |
| TB-related deaths (n) | −0.204 | −0.259 | −0.322* | −0.395* | 0.519* | −0.081 | −0.331* |
| Deaths rate (per 100,000 pn.) | −0.135 | −0.170 | −0.246 | −0.281* | −0.199 | −0.147 | −0.063 |
| Malaria | |||||||
| Cases (n) | −0.162 | −0.353* | −0.469* | −0.519* | −0.402* | −0.262 | −0.402* |
| NCDs | |||||||
| DM death (n) | 0.046 | 0.053 | 0.002 | −0.055 | 0.711* | −0.075 | −0.143 |
| CVD death (n) | −0.022 | 0.005 | −0.025 | −0.084 | 0.673* | −0.147 | −0.201 |
| RD death (n) | −0.030 | −0.017 | −0.068 | −0.110 | 0.651* | −0.165 | −0.244 |
| MN death (n) | −0.027 | 0.002 | −0.035 | −0.104 | 0.669* | −0.127 | −0.201 |
|
Total NCD death (n) |
−0.022 | −0.003 | −0.037 | −0.098 | 0.685* | −0.150 | −0.206 |
r Spearman’s correlation, *P-value < 0.05, US$ United States Dollar, GDP Gross domestic product, pn Population, DM Diabetes mellitus, CVD Cardiovascular diseases, RD Respiratory diseases, MN Malignant neoplasms, NCD Non-communicable diseases.
Digital health ecosystem mapping of all 54 countries
Finally, the digital health ecosystem of the 54 countries of Africa was characterized and mapped based on their rank on the WLC model that provides a one-point weighted linear combination of disease burden, mobile/internet subscriptions, and GDP per capita. For NCD-related outcome variables, running a correlation among the five NCD variables, we found a correlation coefficient greater than 0.95, indicating nearly perfect positive colinearity among the NCD outcome variables at a cut-off of > 0.80 (refer to Supplementary Table 2). Hence, in prioritizing and developing a map for NCDs, we considered total NCD deaths as it provided relatively better information about the NCD burden compared to single NCDs. For ID-related outcome variables (refer to Supplementary Table 3), since the correlation coefficient among the two HIV-related outcome variables was 0.967, the number of PWH was considered in the mapping. The correlation among TB-related burdens was greater than 0.88, TB incidence was considered in the mapping. Number of malaria cases was not highly correlated with the other IDs. Therefore, IDs burdens were represented separately by PWH, TB incidence, and number of malaria cases.
For IDs, the highest-priority countries for implementation of digital health technologies were South Africa, Nigeria, and Tanzania for HIV; Nigeria, South Africa, and DROC for TB; and DROC, Nigeria, and Uganda for malaria. For NCDs, Egypt, Nigeria, and Ethiopia were the highest-priority countries for digital health interventions. For details about each specific NCD, refer to Supplementary Table 4. Table 2 lists countries ranked top and least three for digital health interventions on IDs and NCDs.
Table 2.
Countries in Africa ranked top and least three for digital health ecosystem on endemic infectious and non-communicable diseases.
| Countries | South Africa | Nigeria | UR Tanzania | ST & Principe | Comoros | Mozambique |
|---|---|---|---|---|---|---|
|
PWH r, n |
1 5250731.8 |
2 1330228.3 |
3 1190130.8 |
52 960.7 |
53 307.5 |
54 59.8 |
| Nigeria | South Africa | DR Congo | Cape Verde | ST & Principe | Comoros | |
|
TB incidence r, n |
1 316628.3 |
2 230331.8 |
3 200267.6 |
52 518.2 |
53 442.7 |
54 377.5 |
| DR Congo | Nigeria | Uganda | Cape Verde | Lesotho | Togo | |
|
Malaria cases r, n |
1 17472065.5 |
2 15106266.8 |
3 10739890.7 |
52 371.2 |
53 131.3 |
54 115.0 |
| Egypt | Nigeria | Ethiopia | Cape Verde | Comoros | ST & Principe | |
|
TNCD death r, n |
1 345141.5 |
2 313665.2 |
3 190010.9 |
52 1765.6 |
53 1739.7 |
54 665.5 |
r Rank, n Number of cases, PWH People living with HIV, DR Congo Democratic Republic of Congo, ST & Principle Sao Tome and Principle, TB Tuberculosis, TNCD Total non-communicable diseases.
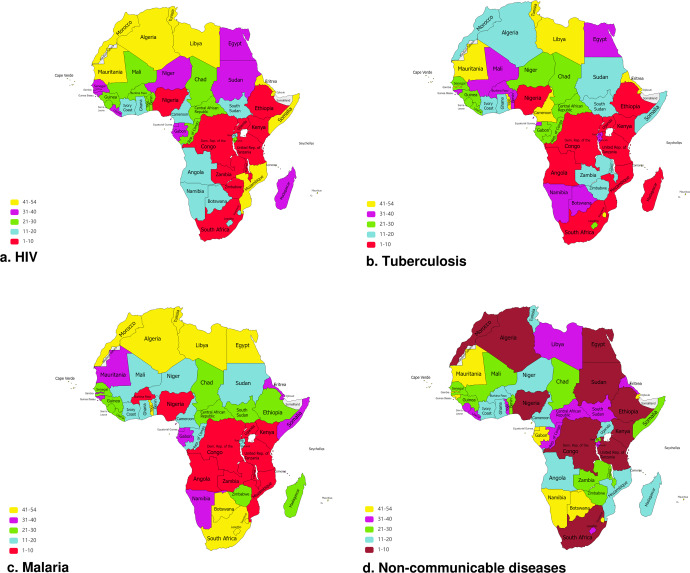
Figure 5 mapped the 54 countries of Africa based on their rank for digital health ecosystem on IDs (HIV, TB, malaria) and NCDs, with a higher rank representing countries of high priority.
Fig. 5. Map of Africa illustrating ranks of countries that should prioritize digital health investments against endemic infectious and non-communicable diseases.
Maps illustrating all 54 countries of Africa, based on their ranks in descending order, that should prioritize digital health investments against (a) HIV, (b) Tuberculosis, (c) Malaria, (d) Non-communicable diseases across.
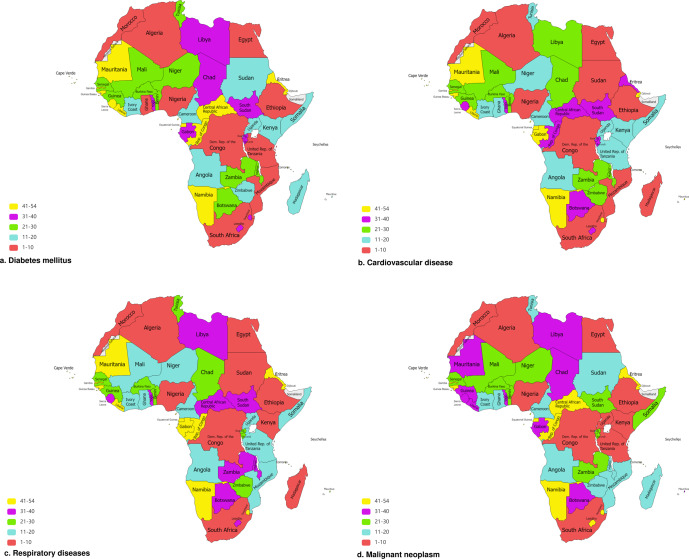
Figure 6 mapped the 54 countries of Africa based on their rank for digital health ecosystem of each specific NCD.
Fig. 6. Map of Africa illustrating ranks of countries that should prioritize digital health investments against specific non-communicable diseases.
Maps illustrating all 54 countries of Africa, based on their ranks in descending order, that should prioritize digital health investments against (a) Diabetes mellitus, (b) Cardiovascular disease, (c) Respiratory diseases, (d) Malignant neoplasm.
Discussion
Here, we report current digital health ecosystems in Africa and the countries that should prioritize digital health investments against endemic IDs and NCDs. The findings demonstrate that in the last 20 years, critical infrastructure and drivers of digital health interventions have been steadily growing in Africa, including the number of individuals using the internet, mobile cellular subscriptions, fixed broadband subscriptions, high-technology manufacturing, GDP per capita, and adult literacy rate. However, these technology developments varied across countries, with Seychelles, Morocco, Tunisia, South Africa, Mauritius, and Botswana at the top, thus developments concentrate mainly in the Northern part of Africa, followed by Southern Africa. Many African countries were overwhelmed by the dual burden of endemic IDs and NCDs. There were inverse correlations between technology characteristics and IDs, such as fixed broadband subscription and incidence of tuberculosis and malaria, GDP per capita and incidence of tuberculosis and malaria, and access to electricity and prevalence of HIV and malaria. On the WLC ranking, which provides a one-point weighted linear combination of disease burden, existing infrastructure, and economy, the highest-priority countries for implementation of digital health technologies were South Africa, Nigeria, and Tanzania for HIV; Nigeria, South Africa, and Democratic Republic of the Congo (DROC) for tuberculosis; DROC, Nigeria, and Uganda for malaria; and Egypt, Nigeria, and Ethiopia for endemic NCDs (diabetes mellitus, cardiovascular diseases, respiratory diseases, cancer). Countries such as Kenya, Ethiopia, Zambia, Zimbabwe, Angola, Zambia, and Mozambique also were highly affected by endemic IDs but were not on the list of countries with high priority as they had comparably lower technology access and economy.
The returns on digital health investments rely mainly on country-specific demands and enabling environments. In the current study, South Africa, Nigeria, Tanzania, DR Congo, and Uganda were the most prepared and most likely to benefit from digital health interventions on IDs. This finding amplifies the previous report from the WHO Digital Health Atlas platform that listed 12 countries, which exhibited a relatively greater number of digital health projects, including four countries similarly identified by this analysis24. However, countries with better performance at the macro-level of the digital health ecosystem may not necessarily experience optimal deployment and implementation of digital health programs in actuality. Previous studies issued cautionary notes on the digital health space in South Africa, including restrictive legislative and regulatory processes25, underinvestment26, urban-rural divide27,28, and disintegration from the multi-sectorial health systems backing SDG 329. South Africa was one of the first countries globally to adopt telehealth/medicine but, because of poor connectivity in rural areas, the program did not flourish26–28,30,31. Similarly, in Nigeria, digital health technologies offer profound opportunities to materialize SDG 3 but were concentrated as pilot projects32. In general, robust digital health capabilities are lacking in Africa as this is an emerging and consistently evolving technology33,34. In addition, even if the supply of digital health technologies exists, it is not clear that it will be adopted optimally by those in the health sector. On the other hand, countries such as Kenya, Ethiopia, Zambia, Zimbabwe, Angola, Zambia, and Mozambique also were highly overwhelmed by endemic IDs but were not on the list for their relatively lower digital infrastructure and economy. Further, by prioritizing certain countries with existing infrastructure, there is a possibility of worsening the existing inequities even if the weight formulation processes were matched by countries with the highest burden. Hence, those countries with a high burden of IDs but lack the needed digital infrastructure should be prioritized for economic development. Poorer countries would most likely invest relatively less in health and hence would be prone to IDs associated with poverty. Therefore mechanisms that broadly uplift economic development are necessary for digital health technologies to become effective.
In the current study, Egypt, South Africa, Nigeria, Morocco, Ethiopia, and DROC were top priority countries for digital health investments in NCDs. They had the highest burden of different types of endemic NCDs and a comparatively better enabling environment for investment in digital health technologies for NCDs. The data also showed that the majority of these countries are ranked the highest in Africa for high-technology exports, which would provide opportunities for in-country digital health technology development and startups. Digital health technologies supporting the management of NCDs are rapidly evolving in the developed world35–40, and those African countries highly susceptible to NCDs would need to investigate the effectiveness of such technologies in local contexts to adapt or develop locally and implement sustainably.
In this study, countries that had relatively better economies, IT infrastructure, and electric power supply were less vulnerable to IDs, which was aligned with previous studies that documented a significant association between under-development and infectious diseases41–43. This was not the case for NCDs, where the data showed a higher burden of specific NCDs in countries with comparatively better economies and infrastructure, which was comparable with previous findings44–47. As technology becomes accessible for a country, this correlates with improved public health practices including water, sanitation and hygiene (WASH), thereby reducing infectious diseases but increasing exposure to unhealthy lifestyles including physical inactivity, unhealthy diet, and other sedentary lifestyles that increase the risk of NCDs48–51. Countries in the northern part of Africa including Egypt, Tunisia, Morocco, and Libya are in a relatively better economic and infrastructural situation, but bear a significant share of the NCD burden in Africa.
Africa’s economies are smaller than the economies in other continents of the world and this may hamper Africa’s significant contributions to the digital health ecosystem; however, untapped opportunities exist for strategic actions. Global health initiatives may have significant contributions toward bridging the knowledge and investment gaps, both through technology transfer for local production of digital health technologies and price negotiation for large-scale deployment of the most impactful technologies. The long-term financial and technical support that global health partners such as the United States President’s Emergency Plan for AIDS Relief (PEPFAR) brought to Africa in the fight against endemic IDs52–57 could serve as a fertile ground to transform digital health interventions in the area, extend to NCD programs, and avert digital health inequities ahead. This is with full understanding that many of the infrastructure developments alongside digital health technologies remain on the shoulders of local African governments. WHO recommends countries to actively work towards universal health coverage (UHC), and hence, investments in digital health technologies should go beyond vertical disease programs to help strengthen the overall healthcare system. Resilient governance, stewardship, health systems, and societies are all important for wide-scale deployment of digital health technologies through the lens of UHC16,17,58–60. Resource-limited countries may initially start with high-burden diseases using tailored digital health technologies within existing resources. Then over time, these same technologies could be leveraged and adapted to respond to other health priorities thereby creating broader access to digital health. This is precisely how countries used HIV-specific resources, technologies, programs, services, and systems to address other priorities such as Ebola, COVID-19, measles, and now NCDs53,61–63.
This study uses rigorous methods, addressing all 54 countries of Africa, to unlock information gaps in the digital health ecosystem in the context of IDs and NCDs of global importance in Africa. However, this study has some limitations. The study explored the macro-level digital health ecosystem to understand the broader forces that impact investments in digital health technologies in Africa, hence, insights from micro- and meso-level analyses including patient- and provider-reported usability and satisfaction results are also needed to understand individual forces that could be observed in the implementation of a specific digital health technology. The study mapped the digital health ecosystem and underlying facets in the context of endemic IDs and NCDs, and thus may not necessarily address non-endemic diseases.
In conclusion, this study provides substantial insight into where governments should prioritize efforts in digital health interventions in Africa as an important accelerator of the UN SDG 3 targets by 2030 and the WHO global strategy on digital health 2020–2025. Many African countries were overwhelmed by a double burden of infectious and non-communicable diseases. Conversely, in the last 20 years, infrastructure important to digital health interventions hase been steadily growing in Africa, including the number of individuals using the internet, mobile cellular subscriptions, fixed broadband subscriptions, high-technology exports, adult literacy rate, and GDP per capita. Digital health technology investments in Africa, including clinical utility trials, require preliminary analyses of the enabling environments to bring about sustainable health and economic returns. Equally, African countries with a high burden of endemic diseases but lacking digital infrastructure should be prioritized for economic development not to worsen existing inequities. Building digital infrastructure should be a key part of economic development programs in countries with high disease burdens to ensure more equitable health outcomes. Though infrastructure developments alongside digital health interventions remain on the shoulders of governments, global health initiatives can cultivate digital health interventions substantially by bridging knowledge and investment gaps, both through technology transfer for local production and negotiation of prices for large-scale deployment of the most impactful digital health technologies.
Methods
Design and data sources
For 54 countries across Africa, we conducted a cross-national ecological analysis using data collected from four credible open-access sources: The World Bank Open Data64, the WHO Global Health Observatory65, Africa United Nations Data for Development of the United Nations Economic Commission for Africa66, and the Global Data on HIV Epidemiology and Response of the Joint United Nations Programme on HIV/AIDS (UNAIDS)67. A minimum of 20 years of consecutive annual data, from January 2000 to September 2022 (latest date available), was extracted for 38 independent variables on technology characteristics and incidence or mortality of endemic IDs and NCDs. The World Bank Open Data consists of 5,443 global development datasets and the WHO Global Health Observatory data repository provides credible data on over 1000 indicators on priority health topics. The Africa UN Data for Development platform provides a regional online portal to bring together all African countries with high-quality data and statistical progress on SDG 3030 as a one-stop-shop repository. The UNAIDS provides the world’s most credible and large-scale datasets on epidemiology, program coverage, and finance relevant to HIV/AIDS.
We adapted the WHO digital health interventions framework68 to provide a conceptual framework that helps operationalize and interpret the findings of this study. Our underlying focus was to study if a country’s maturity of the digital ecosystem comprising the technology infrastructure and economy (i.e., the exposure) has a critical influence on the relevance and impact of digital health interventions in reducing the incidence and mortality of endemic IDs and NCDs (i.e., the outcome).
Variables
Using the World Bank Open Data, 20-year data were collected for each African country on nine key exposure variables including economic size, IT infrastructure, electricity infrastructure, technology intensity, and population literacy that drive digital health implementation. Using the WHO Global Health Observatory data repository, data were collected for each African country on 17 key variables on endemic IDs and NCDs. Using the Africa UN Data for Development portal, analyses were made on key SDG 3 trends and progress so far in Africa, and data were used to understand the progress toward SDG 3 in Africa. The UNAIDS database was used to analyze trends in key HIV/AIDS indicators and to compare the burden of HIV/AIDS in Africa against the globe and among sub-regions within Africa based on the latest (2022) data as available. These variables were selected following a review of the complete list of variables in each database. Those that provide the best fit to the study of interest were pooled in line with WHO’s digital health interventions framework and WHO’s definitions of endemic IDs and NCDs. The variables pooled from the four database platforms are summarized in Supplementary Table 5.
Data analysis
Spearman’s rank correlation coefficients were used to characterize the ecological associations between exposures (technology characteristics) and outcomes (incidence or mortality of endemic IDs and NCDs).
The variables used to define the exposure were mobile cellular subscriptions (per 100 people); individuals using the internet (% of the population); fixed broadband subscriptions (per 100 people); access to electricity (% of the population); high-technology exports (US$); adult literacy rate (%); and GDP per capita (US$).
The variables used to define the outcome had two categories: IDs and NCDs. Thus, outcome variables included incidence or mortality of IDs (HIV, TB, malaria) and NCDs (diabetes mellitus, cardiovascular diseases, malignant neoplasm, respiratory diseases, the four NCDs in total). Additional programmatic aspects including treatment success, drug resistance, and financing were included. We used descriptive statistics to characterize the variables.
We conducted a colinearity test at a cut-off value of Spearman’s rank correlation coefficient of > 0.80 to identify and exclude variables providing similar information and minimize the number of variables accordingly. Descriptive analyses were conducted to display in bar charts the top ten countries for each exposure and outcome variable and to show, using line charts, the patterns over 20 years of the variables. Incidence and mortality of outcome variables were compared between Africa and globally as well as between sub-regions within Africa which were East and Southern Africa, West and Central Africa, and the Middle East and North Africa. The findings were summarized in tables.
A weighted linear combination (WLC) model69 was used as the decision rule, combining disease burden, technology access, and GDP per capita, to explain, rank, and map the digital health ecosystem of a given country. Informed by the WHO digital health framework68, a counterfactual scenario was formulated that combined three attributes from the exposure and outcome variables: 1) countries with the highest burden of infectious or NCDs should have priority for digital health technologies in line with the specific disease and the related digital health intervention; 2) all countries with the highest burden of IDs or NCDs may not have favorable access to the internet or mobile services for successful digital health interventions, and hence the high-burden countries would need to also have relatively high access to the internet or mobile phone subscription rate depending on the nature of the digital health technology; and 3) all countries with the highest burdens of IDs or NCDs and better access to the internet or mobile subscriptions may not have the economy to import or locally produce digital health technologies and hence would also need to have a competitive economy. Hence, disease burden (incidence or mortality of IDs and NCDs), digital infrastructure (access to the internet or mobile phone subscription), and economy (GDP per capita) were identified as the main attributes defining the digital health ecosystem of a given country. Based on the WLC model, weights were determined by an expert group using multiple attribute decision-making (MADM)69. With these, a one-point linear combination was developed: [0.7*incidence/mortality of the disease] + [0.2*mobile/internet subscriptions] + [0.1*country GDP per capita] of a given country. Using the WLC procedure, we then ranked all 54 countries according to their overall values, and for each ID and NCD and considering colinearity. We developed map charts using an online map creation platform70 to illustrate countries based on their ranks and in descending order.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
The work was supported by the Fogarty International Center of the US National Institutes of Health (D43TW011404) and the Emory Center for AIDS Research (P30AI050409). The content is solely the responsibility of the authors and does not necessarily represent the official views of the US National Institutes of Health or the Emory Center for AIDS Research. The authors thank Dr. Solveig Argeseanu Cunningham and Emily Chuba of the Rollins School of Public Health, Emory University, US, for their technical support.
Author contributions
Study conception and Principal Investigator: T.M.; Study design: T.M., M.K.A., T.K., T.G., M.J.M., S.A.P., D.H., C.E., Y.W., N.M., S.S., W.A., V.C.M., A.F.; Statistical Analysis: T.M., T.G.; Funding acquisition: M.K.A., A.F., V.C.M., D.H., T.M.; Draft the manuscript: T.M.; Reviewed and revised the manuscript: T.M., M.K.A., T.K., T.G., M.J.M., S.A.P., D.H., C.E., Y.W., N.M., S.S., W.A., V.C.M., A.F.; All authors read and approved the final manuscript.
Data availability
The data that support the findings of this study were derived from the following open-access public domain resources: The World Bank Open Data, the WHO Global Health Observatory, Africa United Nations Data for Development of the United Nations Economic Commission for Africa, and the Global Data on HIV Epidemiology and Response of the UNAIDS.
Competing interests
V.C.M. has received investigator-initiated research grants (to the institution) and consultation fees (both unrelated to the current work) from Eli Lilly, Bayer, Gilead Sciences, and ViiV. M.K.A. has received investigator-initiated research grants to the institution from Merck and consultation fees (both unrelated to the current work) from Eli Lilly and Bayer. All other authors report no potential conflicts.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41746-023-00839-2.
References
- 1.Taha TE, et al. Effects of long-term antiretroviral therapy in reproductive-age women in sub-Saharan Africa (the PEPFAR PROMOTE study): a multi-country observational cohort study. Lancet HIV. 2022;9:e394–e403. doi: 10.1016/S2352-3018(22)00037-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Payne CF, et al. Differences in healthy longevity by HIV status and viral load among older South African adults: an observational cohort modelling study. Lancet Healthy Longevity. 2022;3:S1. doi: 10.1016/S2666-7568(22)00062-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tromp J, et al. World Heart Federation Roadmap for Digital Health in Cardiology. Glob. Heart. 2022;17:61. doi: 10.5334/gh.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global Burden of Disease Health Financing Collaborator Network. Health sector spending and spending on HIV/AIDS, tuberculosis, and malaria, and development assistance for health: progress towards Sustainable Development Goal 3. Lancet. 2020;396:693–724. doi: 10.1016/S0140-6736(20)30608-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis K, et al. Association between HIV infection and hypertension: a global systematic review and meta-analysis of cross-sectional studies. BMC Med. 2021;19:105. doi: 10.1186/s12916-021-01978-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agan BK, Marconi VC. Noncommunicable Diseases: Yet Another Challenge for Human Immunodeficiency Virus Treatment and Care in Sub-Saharan Africa. Clin. Infect. Dis. 2020;71:1874–1876. doi: 10.1093/cid/ciz1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kajogoo VD, et al. HIV Protease Inhibitors and Insulin Sensitivity: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 2021;12:635089. doi: 10.3389/fphar.2021.635089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Getachew E, et al. Digital health in the era of COVID-19: Reshaping the next generation of healthcare. Front. Public Health. 2023;11:942703. doi: 10.3389/fpubh.2023.942703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guan G, et al. Higher sensitivity monitoring of reactions to COVID-19 vaccination using smartwatches. NPJ Digit. Med. 2022;5:140. doi: 10.1038/s41746-022-00683-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olusanya OA, White B, Melton CA, Shaban-Nejad A. Examining the Implementation of Digital Health to Strengthen the COVID-19 Pandemic Response and Recovery and Scale up Equitable Vaccine Access in African Countries. JMIR Form Res. 2022;6:e34363. doi: 10.2196/34363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Digital Health - Worldwide. Statista Inc. (n.d.), New York, USA; 2022. Retrieved September 4, 2022. Available at https://www.statista.com/outlook/dmo/digital-health/worldwide.
- 12.van Stam G. Conceptualization and practices in digital health: Voices from Africa. Afr. Health Sci. 2022;22:664–672. doi: 10.4314/ahs.v22i1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ibeneme S, et al. Strengthening Health Systems Using Innovative Digital Health Technologies in Africa. Front. Digit. Health. 2022;4:854339. doi: 10.3389/fdgth.2022.854339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manyazewal T, Matlakala MC. Implementing health care reform: implications for performance of public hospitals in central Ethiopia. J. Glob. Health. 2018;8:010403. doi: 10.7189/jogh.08.010403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manyazewal T, Woldeamanuel Y, Blumberg HM, Fekadu A, Marconi VC. The potential use of digital health technologies in the African context: a systematic review of evidence from Ethiopia. NPJ Digit. Med. 2021;4:125. doi: 10.1038/s41746-021-00487-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization (WHO). Global strategy on digital health 2020–2025. (World Health Organization, Geneva, Switzerland, 2021. https://www.who.int/publications/i/item/9789240020924.
- 17.Holly L, Smith RD, Ndili N, Franz C, Stevens EAG. A Review of Digital Health Strategies in 10 Countries With Young Populations: Do They Serve the Health and Wellbeing of Children and Youth in a Digital Age? Front. Digit. Health. 2022;4:817810. doi: 10.3389/fdgth.2022.817810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shahil Feroz A, Afzal N, Seto E. Exploring digital health interventions for pregnant women at high risk for pre-eclampsia and eclampsia in low-income and-middle-income countries: a scoping review. BMJ Open. 2022;12:e056130. doi: 10.1136/bmjopen-2021-056130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Haan K, et al. Automated screening of sickle cells using a smartphone-based microscope and deep learning. NPJ Digit. Med. 2020;3:76. doi: 10.1038/s41746-020-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manyazewal T, Woldeamanuel Y, Fekadu A, Holland DP, Marconi VC. Effect of digital medication event reminder and monitor-observed therapy vs standard directly observed therapy on health-related quality of life and catastrophic costs in patients with tuberculosis: A secondary analysis of a randomized clinical trial. JAMA Netw. Open. 2022;5:e2230509. doi: 10.1001/jamanetworkopen.2022.30509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.LeFevre A, et al. Avoiding the road to nowhere: Policy insights on scaling up and sustaining digital health. Glob. Policy. 2021;12:110–114. doi: 10.1111/1758-5899.12909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manyazewal T, et al. Patient-reported usability and satisfaction with electronic medication event reminder and monitor device for tuberculosis: A multicentre, randomised controlled trial. E Clin. Med. 2023;56:101820. doi: 10.1016/j.eclinm.2022.101820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fehr J, et al. Computer-aided interpretation of chest radiography reveals the spectrum of tuberculosis in rural South Africa. NPJ Digit. Med. 2021;4:106. doi: 10.1038/s41746-021-00471-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization Digital Health Atlas (WHO DHA). Digital Health Atlas in Africa: Analysis of digital health products in Africa. Geneva, Switzerland; WHO DHA 2022. Accessed 16 September 2022. Available at https://stories.digitalhealthatlas.org/post/f8a48940-2f77-418b-b722-c4cd42f8ebcc.
- 25.Donnelly, D. L. First Do No Harm: Legal Principles Regulating the Future of Artificial Intelligence in Health Care in South Africa. Potchefstroom Electron Law J. 25 (2022), 10.17159/1727-3781/2022/v25ia11118. [DOI] [PMC free article] [PubMed]
- 26.Swartz A, LeFevre AE, Perera S, Kinney MV, George AS. Multiple pathways to scaling up and sustainability: an exploration of digital health solutions in South Africa. Global Health. 2021;17:77. doi: 10.1186/s12992-021-00716-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Visagie J, Turok I. Rural–urban inequalities amplified by COVID-19: evidence from South Africa. Area Development Policy. 2021;6:50–62. doi: 10.1080/23792949.2020.1851143. [DOI] [Google Scholar]
- 28.Mbunge E, Batani J, Gaobotse G, Muchemwa B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: a systematic review. Glob. Health J. 2022;6:102–113. doi: 10.1016/j.glohj.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sibuyi IN, de la Harpe R, Nyasulu P. A Stakeholder-Centered mHealth Implementation Inquiry Within the Digital Health Innovation Ecosystem in South Africa: MomConnect as a Demonstration Case. JMIR Mhealth Uhealth. 2022;10:e18188. doi: 10.2196/18188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhamjee A, et al. Perceptions of Telehealth Services for Hearing Loss in South Africa’s Public Healthcare System. Int. J. Environ. Res. Public Health. 2022;19:7780. doi: 10.3390/ijerph19137780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehl GL, Tamrat T, Bhardwaj S, Blaschke S, Labrique A. Digital health vision: could MomConnect provide a pragmatic starting point for achieving universal health coverage in South Africa and elsewhere? BMJ Glob. Health. 2018;3:e000626. doi: 10.1136/bmjgh-2017-000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ibeneme S, et al. Strengthening capacities among digital health leaders for the development and implementation of national digital health programs in Nigeria. BMC Proc. 2020;14:9. doi: 10.1186/s12919-020-00193-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Badran MF. Digital platforms in Africa: A case-study of Jumia Egypt’s digital platform. Telecommun. Policy. 2021;45:102077. doi: 10.1016/j.telpol.2020.102077. [DOI] [Google Scholar]
- 34.Getachew E, Woldeamanuel Y, Manyazewal T. Digital health interventions in the clinical care and treatment of tuberculosis and hiv in central Ethiopia: An initial provider perceptions and acceptability study using the unified theory of acceptance and use of technology model. Int. J. Mycobacteriol. 2022;11:1–9. doi: 10.4103/ijmy.ijmy_235_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wannheden C, et al. Digital health technologies enabling partnerships in chronic care management: Scoping review. J. Med. Internet Res. 2022;24:e38980. doi: 10.2196/38980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patel SA, et al. A model for national assessment of barriers for implementing digital technology interventions to improve hypertension management in the public health care system in India. BMC Health Serv. Res. 2021;21:1101. doi: 10.1186/s12913-021-06999-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Getachew E, Woldeamanuel Y, Manyazewal T. Capacity and Readiness Assessment of Healthcare Facilities for Digital Health Interventions Against Tuberculosis and HIV in Addis Ababa, Ethiopia. Front Digit Health. 2022;4:821390. doi: 10.3389/fdgth.2022.821390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Auster-Gussman LA, et al. Engagement in Digital Health App-Based Prevention Programs Is Associated With Weight Loss Among Adults Age 65. Front Digit Health. 2022;4:886783. doi: 10.3389/fdgth.2022.886783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kvedar JC, Mittermaier M, Pritzker J. The industry impact of the American Medical Association’s Digital Medicine Payment Advisory Group (DMPAG) NPJ Digit Med. 2022;5:193. doi: 10.1038/s41746-022-00743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mussie KM, et al. Exploring local realities: Perceptions and experiences of healthcare workers on the management and control of drug-resistant tuberculosis in Addis Ababa, Ethiopia. PLoS One. 2019;14:e0224277. doi: 10.1371/journal.pone.0224277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mussie KM, Gradmann C, Manyazewal T. Bridging the gap between policy and practice: a qualitative analysis of providers’ field experiences tinkering with directly observed therapy in patients with drug-resistant tuberculosis in Addis Ababa, Ethiopia. BMJ Open. 2020;10:e035272. doi: 10.1136/bmjopen-2019-035272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tesfahunei HA, et al. Human papillomavirus self-sampling versus standard clinician-sampling for cervical cancer screening in sub-Saharan Africa: a systematic review and meta-analysis of randomized controlled trials. Infect Agent Cancer. 2021;16:43. doi: 10.1186/s13027-021-00380-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Modjadji P. Communicable and non-communicable diseases coexisting in South Africa. Lancet Glob. Health. 2021;9:e889–e890. doi: 10.1016/S2214-109X(21)00271-0. [DOI] [PubMed] [Google Scholar]
- 44.Adeyeye SAO, Ashaolu TJ, Bolaji OT, Abegunde TA, Omoyajowo AO. Africa and the Nexus of poverty, malnutrition and diseases. Crit. Rev. Food Sci. Nutr. 2023;63:641–656. doi: 10.1080/10408398.2021.1952160. [DOI] [PubMed] [Google Scholar]
- 45.Chikowore T, Kamiza AB, Oduaran OH, Machipisa T, Fatumo S. Non-communicable diseases pandemic and precision medicine: Is Africa ready? EBioMed. 2021;65:103260. doi: 10.1016/j.ebiom.2021.103260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Adeyemi O, et al. Integration of non-communicable disease and HIV/AIDS management: a review of healthcare policies and plans in East Africa. BMJ Glob. Health. 2021;6:e004669. doi: 10.1136/bmjgh-2020-004669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Park JH, Moon JH, Kim HJ, Kong MH, Oh YH. Sedentary lifestyle: Overview of updated evidence of potential health risks. Korean J. Fam. Med. 2020;41:365–373. doi: 10.4082/kjfm.20.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lin X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci. Rep. 2020;10:14790. doi: 10.1038/s41598-020-71908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee JH, Duster M, Roberts T, Devinsky O. United States Dietary Trends Since 1800: Lack of Association Between Saturated Fatty Acid Consumption and Non-communicable Diseases. Front Nutr. 2022;8:748847. doi: 10.3389/fnut.2021.748847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Galaviz KI, et al. Interventions for reversing prediabetes: A systematic review and meta-analysis. Am. J. Prev. Med. 2022;62:614–625. doi: 10.1016/j.amepre.2021.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Manyazewal T, Paterniti AD, Redfield RR, Marinucci F. Role of secondary level laboratories in strengthening quality at primary level health facilities’ laboratories: an innovative approach to ensure accurate HIV, tuberculosis, and malaria test results in resource-limited settings. Diagn. Microbiol. Infect. Dis. 2013;75:55–59. doi: 10.1016/j.diagmicrobio.2012.09.020. [DOI] [PubMed] [Google Scholar]
- 52.Marinucci F, et al. Impact of horizontal approach in vertical program: Continuous quality improvement of malaria and tuberculosis diagnostic services at primary-level medical laboratories in the context of HIV care and treatment program in Ethiopia. Am. J. Trop. Med. Hyg. 2013;88:547–551. doi: 10.4269/ajtmh.12-0628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manyazewal T, et al. Implementation and evaluation of a blended learning course on tuberculosis for front-line health care professionals. Am. J. Clin. Pathol. 2017;147:285–291. doi: 10.1093/ajcp/aqx002. [DOI] [PubMed] [Google Scholar]
- 54.Qiu M, et al. Exploring perceived effects from loss of PEPFAR support for outreach in Kenya and Uganda. Glob. Health. 2021;17:80. doi: 10.1186/s12992-021-00729-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Manyazewal T, Woldeamanuel Y, Holland DP, Fekadu A, Marconi VC. Effectiveness of a digital medication event reminder and monitor device for patients with tuberculosis (SELFTB): a multicenter randomized controlled trial. BMC Med. 2022;20:310. doi: 10.1186/s12916-022-02521-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Manyazewal T, Oosthuizen MJ, Matlakala MC. Proposing evidence-based strategies to strengthen implementation of healthcare reform in resource-limited settings: a summative analysis. BMJ Open. 2016;6:e012582. doi: 10.1136/bmjopen-2016-012582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Olu O, et al. How Can Digital Health Technologies Contribute to Sustainable Attainment of Universal Health Coverage in Africa? A Perspective. Front. Public Health. 2019;7:341. doi: 10.3389/fpubh.2019.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kickbusch I, et al. The Lancet and financial times commission on governing health futures 2030: Growing up in a digital world. Lancet. 2021;398:1727–1776. doi: 10.1016/S0140-6736(21)01824-9. [DOI] [PubMed] [Google Scholar]
- 59.Karamagi HC, et al. eHealth or e-Chaos: The use of Digital Health Interventions for Health Systems Strengthening in sub-Saharan Africa over the last 10 years: A scoping review. J. Glob. Health. 2022;12:04090. doi: 10.7189/jogh.12.04090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fauci AS, Eisinger RW. PEPFAR - 15 Years and Counting the Lives Saved. N. Engl. J. Med. 2018;378:314–316. doi: 10.1056/NEJMp1714773. [DOI] [PubMed] [Google Scholar]
- 61.Nkengasong J. Let Africa into the market for COVID-19 diagnostics. Nature. 2020;580:565. doi: 10.1038/d41586-020-01265-0. [DOI] [PubMed] [Google Scholar]
- 62.Farmer, P. Fevers, feuds, and diamonds: Ebola and the ravages of history. Farrar, Straus and Giroux; New York, 2020.
- 63.The World Bank Group. World Bank Open Data. Washington DC, USA; The World Bank Grouup 2022. Accessed 02 September 2022. Available at https://data.worldbank.org/.
- 64.World Health Organization (WHO). WHO Global Health Observatory. Geneva, Switzerland; WHO 2022. Accessed 02 September 2022. Available at https://www.who.int/data/gho.
- 65.United Nations Economic Commision for Africa (UNECA). Africa UN Data for Development. Addis Ababa, Ethiopia; 2022. Accessed 02 September 2022. Available at https://ecastats.uneca.org/africaundata.
- 66.The Joint United Nations Programme on HIV/AIDS (UNAIDS). AIDSInfo: Global data on HIV epidemiology and response. Geneva, Switzerland; UNAIDS 2022. Accessed 02 September 2022. Available at https://aidsinfo.unaids.org/.
- 67.World Health Organization (WHO). WHO guideline: recommendations on digital interventions for health system strengthening. Geneva, Switzerland; WHO 2019. Accessed 17 February 2022. Available at https://www.who.int/publications/i/item/9789241550505. [PubMed]
- 68.Yue Z. Approach to group decision making based on determining the weights of experts by using projection method. Appl. Mathematical Modelling. 2012;36:2900–2910. doi: 10.1016/j.apm.2011.09.068. [DOI] [Google Scholar]
- 69.Paintmaps.com. Color maps with statistical data. Accessed 09 September 2022. Available at https://paintmaps.com/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study were derived from the following open-access public domain resources: The World Bank Open Data, the WHO Global Health Observatory, Africa United Nations Data for Development of the United Nations Economic Commission for Africa, and the Global Data on HIV Epidemiology and Response of the UNAIDS.