Abstract
Objective:
Parkinson's disease (PD) is a progressive neurodegenerative disease that can reduce quality of life (QOL). Previous research has explored patient specific factors that influence QOL; but understanding external factors that may also affect patient QOL, such as caregiver characteristics, can provide additional intervention targets that may improve QOL for both the person with PD and their caregiver.
Methods:
We conducted a systematic review of existing literature on caregiver factors that are related to QOL for the person with PD. We developed a tailored search strategy in six databases and performed a screening procedure according to PRISMA guidelines. We synthesized findings from articles that met inclusion criteria using a narrative approach and identified themes categorizing caregiver factors associated with PD QOL.
Results:
We found 32 full-text articles that fulfilled the inclusion criteria and passed the quality appraisal. Seven themes were identified, including: (1) burden, (2) strain, (3) QOL and satisfaction, (4) demographic factors, (5) psychological factors, (6) relationship factors, and (7) caregiver input.
Conclusions:
Our review presents critical insights into the role of the caregiver in the QOL of a person with PD. Findings reveal several targets for intervention to improve QOL in this population.
Keywords: burden, caregiver, Parkinson's disease, quality of life, strain
1 ∣. INTRODUCTION
Parkinson's disease (Parkinson's disease (PD)) is a progressive neurodegenerative disease characterized by motor and non-motor symptoms that impair functioning and reduce QOL.1-3 A previous systematic review of QOL in PD identified several patient-level factors that contribute to QOL, including depression, mobility limitations, problems in psychosocial functioning, attitude, and living environment.4 However, models of QOL frequently reference influences outside of the individual, such as social relationships and environmental factors.5-7 Therefore, to understand what affects QOL, we examined factors beyond patient-level factors.
One important social relationship to evaluate in PD is the relationship between the person with PD and their caregiver. With advancing disease severity, patients with PD frequently require a caregiver.8 Caregivers provide physical and emotional care for the patient and often help with adherence to medical regimens for PD.9-11 Caregiver support can also delay formal home care or residential nursing home placement.12
In other disease populations, several studies have revealed the influence of a caregiver on the QOL of the care recipient. Hoe et al. found that people with dementia who lived at home with a caregiver had higher QOL than people living in 24-h care facilities.13 Burgener and Twigg also found that the quality of the caregiver-care recipient relationship predicted QOL and psychological wellbeing of the care recipient.14 Another study demonstrated that caregiver burden, or the level of multidimensional burden resulting from caring for a family member and/or loved one over time that a caregiver perceives, contributed to worse QOL for the care recipient.15,16 Caregiver strain, defined as the caregiver's experience of persistent problems and a feeling of reduced well-being that results from providing prolonged care for someone, is also associated with worse QOL for both care recipient and caregiver.17,18
These findings have translated to interventions targeting caregivers that improve patient outcomes. A review of dementia caregiver interventions reported on several interventions that successfully improved patient functioning and QOL.19 Thus, improvement in QOL for PD patients may hinge on identifying and addressing modifiable caregiver characteristics that impact QOL for PD patients.
Several reviews have examined PD patient factors that affect QOL of the care recipient.4,20,21 However, no review has examined caregiver-specific factors associated with QOL for the person with PD. The purpose of this review is to identify caregiver characteristics that influence PD patient QOL to inform the development of interventions to improve QOL in this population.
2 ∣. METHODS
2.1 ∣. Search strategy
A systematic review of research-based literature cataloged in PubMed, CINAHL, EMBASE, PsychINFO, Cochrane, and Web of Science was performed. The entire available time range of databases was used until January 24, 2022. The search strategy can be found in Appendix A.
2.2 ∣. Study selection
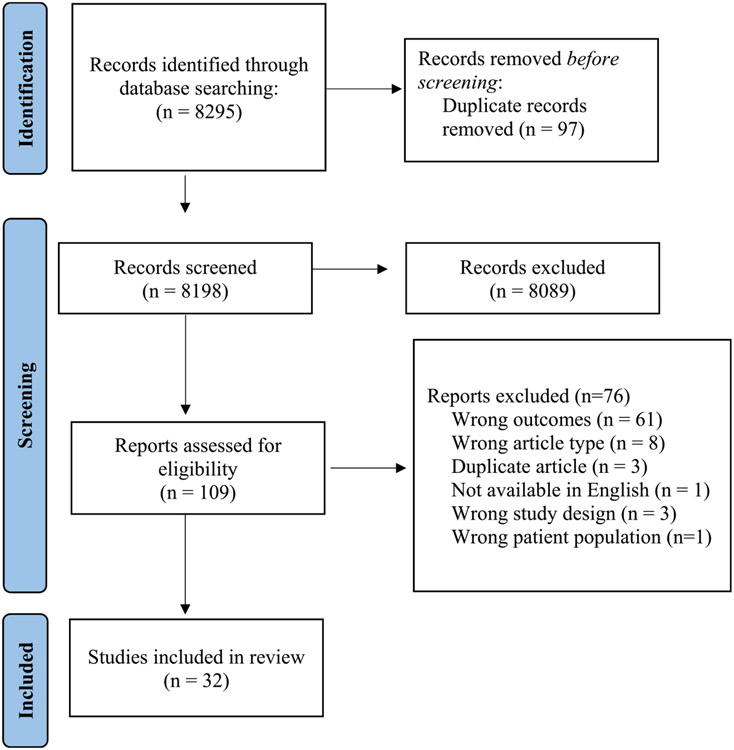
After removing duplicates (n = 97), the titles and abstracts of the remaining 8, 295 articles were independently screened by two reviewers (KP and JH), consistent with PRISMA guidelines.22 Articles were excluded during screening if they did not meet inclusion criteria or if they were not available in English. Discrepancies were resolved by a third reviewer (EF). Articles meeting the inclusion criteria and not meeting exclusion criteria were selected for full-text review (Table 1).
TABLE 1.
Exclusion and inclusion criteria for a systematic review of quality of life (QOL) in Parkinson's disease and the caregiver
| Inclusion criteria | Exclusion criteria |
|---|---|
| Article topic relates to Parkinson's disease and quality of life | Article topic was not related to Parkinson's disease and quality of life. |
| Study sample included both caregivers and people with Parkinson's disease | Article did not include both caregivers and PWP in their sample. |
| Peer-reviewed articles available in English. | Articles is not peer-review, not in English. The record type is a review, book, abstracts only/conference proceedings. |
| Measured and reported on quality of life for the person with Parkinson's disease. | Study design uses an animal model. |
| Evaluated the relationship between a caregiver factor and PWP QOL. |
After the title and abstract screening was complete, 8098 articles were excluded, leaving 109 full-text articles for further screening (Figure 1). These articles were read by two reviewers (KP and JH) to determine if they met inclusion criteria. Any discrepancies were resolved again by the third reviewer (EF). After full-text review, 72 articles were excluded, leaving 32 articles for quality appraisal and data extraction. The reasons for exclusion during the full-text screening stage can be found in Figure 1.
FIGURE 1.
Study selection process (CONSORT diagram)
2.3 ∣. Quality appraisal
One reviewer (KP) used the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies to evaluate the articles that were included after full-text review.23 Table 2 displays the questions that informed the quality appraisal. The results for the quality appraisal can be found in Appendix B.
TABLE 2.
Quality Appraisal criteria
| Criteria |
|---|
| 1. Was the research question or objective in this paper clearly stated? |
| 2. Was the study population clearly specified and defined? |
| 3. Was the participation rate of eligible persons at least 50%? |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? |
| 5. Was a sample size justification, power description, or variance and effect estimates provided? |
| 6. For the analyses in this paper, were the exposure(s) of interest measured before the outcome(s) were measured? |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? |
| 8. For exposures that can vary in amount or level, did the study examine different levels of exposure as related to the outcome (e.g., categories of exposure or exposure measured as a continuous variable)? |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
| 10. Was the exposure(s) assessed more than once over time? |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? |
| 12. Were the outcome assessors blinded to the exposure status of participants? |
| 13. Was loss to follow-up after baseline 20% or less? |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure (s) and outcome(s)? |
2.4 ∣. Data extraction and synthesis
Following quality appraisal, data were extracted from articles using a form that can be found in Appendix C. The study aim, sample size of participants with PD and their caregivers, and the study setting were recorded for all included papers. The QOL measures for the person with PD and the measures of caregiver factors were also noted. Lastly, the relationship between the caregiver factors and QOL measure and the type of analysis used were documented for each study. The data extracted from studies is presented in Table 3.
TABLE 3.
Methodological characteristics of included articles
| Study | Study Aim | Sample | Study design | Sample size (PWP) |
Sample Size (CG) |
Caregiver Measures | Quality of Life Measures |
Analysis Method | Relationship between CG factor and PWP QOL |
|---|---|---|---|---|---|---|---|---|---|
| Bartolomei 2018 | To examine the relationship of sleep quality and depression in patients with PD with burden, mood, and quality of life of their caregivers. | Outpatient clinic | Cross sectional study | 57 | 57 | CBI, BDI | PDQ-39 | Pearson correlation and Spearman correlation | Caregivers' burden and depression were interrelated (Pearson's correlation p < 0.001) and both correlated with PD quality of life. |
| Caap-Ahlgren 2002 | To identify various factors in PD patients and their caregivers that are of supposed importance with respect to caregiver burden. | Outpatient clinic | Longitudinal study | 65 | 65 | CBI | PDQ-39 | Spearman correlation | The correlation between PDQ-39 and caregiver burden: 0.48 (p < 0.005) |
| Chu 2019 | To determine the relationships between QOL and life satisfaction among PD patients and their caregiver. | Active members of the Malaysia Parkinson's Disease Association (MPDA) | Cross sectional study | 20 | 20 | Life satisfaction Scale | PDQ-39 | Pearson Correlation | Correlation between PDQ-39 and life satisfaction scale was 0.46 (significant 2-tailed) |
| Dahodwala 2018 | To compare access to caregiving between men and women with Parkinson's disease (PD). | Participants enrolled in the National Parkinson Foundation Parkinson's Outcomes Project | Cross-sectional | 6154 | 7209 | Caregiver attending visit MCSI | PDQ-39 | Linear regression (Cross-sectional) | Higher PDQ-39 score was related to higher odds of having a caregiver accompany to baseline visit (1.02; 95% CI: 1.01–1.02) and MCSI score (0.34; 95% CI: 0.30–0.37). |
| daSilva 2008 | To evaluate the quality of life of patients with PD; measure the caregivers stress level; and to confront the caregivers stress levels with the patient's quality of life, relating them to the disease gradation. | Outpatient clinic | Cross-sectional | 43 | 43 | CSS | PDQ-39 | Chi-Square test Spearman Correlation | PDQ-39 versus CSS (p = 0.0017, r = 0.4646). |
| Demeulemeester 2015 | To investigate the perception of patients and partners of their own as well as of each other present and former quality of life and to explore a possible correlation of these estimates with measures of disease burden. | Outpatient clinic | Cross sectional study | 50 | 50 | VAS | VAS | Pearson correlation | Quality of life of the PD patient was correlated with caregiver QOL (0.395, p = 0.005) |
| Hand 2018 | To examine the baseline care needs of the cohort living at home and detail the levels of formal and informal care required to meet these needs. | Participants in the Northumbria Care Needs Project. | Cross-sectional | 132 | 115 | Presence of caregiver Duration of caregiving Tasks performed Current health problems they had which they felt negatively affected their ability to fulfill their caring role. |
PDQ-39 | Chi-squared Test | There was a significant difference in PDQ-39 score for those with informal caregiver (32.97; 22.71–42.86 compared to those without an informal caregiver (18.7; 14.455–30.295), p < 0.001. |
| Henry 2020 | To assess the relationship among a range of PD symptoms and four measures of caregiver QOL. | Outpatient clinic | Cross sectional study | 181 | 181 | PDQ-Carer Demographic information (age, sex, relationship to care recipient, how often they see the care recipient, and how many hours per week they spend with the care recipient) |
PDQ-39 | Correlation | All subscales of the PDQ-39 were correlated with PDQ-Carer subscales (p < 0.01 or lower). |
| Karlstedt 2017 | To identify factors associated with mutuality, HRQOL, and caregiver burden. | Baseline data from a longitudinal study. | Cross sectional study | 51 | 51 | CBI MS Caregiver gender and age |
PDQ-8 | Multiple linear regression | The significant predictors of PDQ-8 Total score were MS score (beta = 433, = 0.001) and NMSQuest score (beta = 0.498, p < 0.001) contributed significantly to the explained variance of PDQ8SI scores. Caregiver gender (−4.329; 95% CI −11.565–2.907) and caregiver age (−0.190; 95% CI: −0.551–0.171) were not significant predictors of PDQ-8 total score. |
| Karlstedt 2018 | To disentangle different pathways that could explain the effect of PD specific symptoms on patients' HRQOL. | Outpatient clinic | Cross sectional study | 51 | 51 | CBI MS Caregiver gender and age |
PDQ-8 | Structural equation modeling | With increasing severity of motor and nonmotor symptoms, patients' mutuality decreased which leads to worse PDQ-8. |
| Kelly 2012 | To consider the relationship between HRQOL in people with PD and their caregivers. | Participants were drawn from general medical practitioners, neurologists, Parkinson's Victoria network and advertisements in local papers. | Cross sectional study | 97 | 97 | MCSI | EQ-5D PDQ-39 VAS | Spearman rank correlations coefficient | A small but significant negative relationship was found using the EQ-5D and VAS, but not the unweighted VAS, suggesting that poorer HRQOL in people with PD is associated with higher caregiver strain experienced by their caregivers. The correlation of PDQ-39 with MCSI scores (rs = 0.3 at p < 0.001) confirmed that poorer self-rated health in people with PD was associated with increased strain in their caregivers. |
| Kudlicka 2014 | To evaluate how EF contributes to QOL and health status for the PwPD and caregiver burden. | Outpatient clinic | Cross sectional study | 50 | 65 | CBI caregiver rating of BRIEF-A | LSS PDQ-39 | Multiple regression analyses | The BRIEF-A caregiver rating was the strongest and the only individually significant predictor of QOL-health, whereas the depression rating only approached significance. The model explained 32% of the variance in QOL-health. The BRIEF-A caregiver rating was the strongest and the only individually significant predictor of QOL movement disorders. The model explained 26% of the variance in QOL-movement disorders. The BRIEF-A self-rating was the strongest and the only individually significant predictor of PDQ-39. The model explained 34% of the variance in health status. |
| Lubomski 2021 | To examine MCI in PD patients and their caregivers to determine if caregiver cognition affected their PD relative. | Outpatient clinic | Cross-sectional study | 103 | 81 | MoCA | SF-36 | T-tests | PD patients without MCI were noted to experience an even lower QOL when their caregiver had MCI, compared to a caregiver with no MCI. This difference was observed on the physical component of the SF-36 [PCS 50.9 (SD 22.3) versus 55.8 (SD 16.1), t = −2.5, p = 0.015 and the mental components 60.5 (SD 18.4) versus 64.8 (SD 19.3), t = −2.3, p = 0.028]. |
| Ma 2018 | To explore neuroticism and conscientiousness personality factors of the patient and family caregiver associated with quality of life (QOL) of PD patients | Outpatient clinic | Cross sectional study | 134 | 134 | NEO-FFI | PDQ-39 | Multivariate stepwise linear regression analysis with a forward selection. | The neuroticism of the caregiver was not significantly related to the three domains of QOL, while conscientiousness of the caregiver was added to the predictor of PDQ-39 (beta = −0.22). |
| Martinez-Martin 2005 | To assess the impact of PD on informal caregivers of patients and identify the main factors related to caregiver strain. | Outpatient Clinic | Cross sectional study | 64 | 64 | PDQ-39 | Spearman Correlation | Caregiver quality of life was correlated with patient quality of life (r = −0.600, p < 0.001). | |
| Miyashita 2011 | To clarify the QOL of patients with intractable neurological diseases and their caregivers. | Survey sent to homes | Cross sectional study | 418 | 418 | SF-8 | SF-36 | correlation and regression | The patients' mental health and caregivers' mental component summary were moderately correlated (standardized beta [SB] = 0.34, p < 0.001). |
| Muller 2010 | To report the analysis of the survey outcomes on QOL, insurance, disability and caregiver burden in patients with PD and their carers. | Not described. | Cross sectional study | 2603 | 2603 | BSFC | PDQ-8 | Spearman Correlation | Correlation between PDQ-8 & BSFC = 0.25 (p < 0.0001) |
| Navarta-Sanchez 2016 | To explore potential clinical, social and attitudinal determinants of psychosocial adjustment and QOL in PD patients and informal caregivers | Three settings in a community context: The Navarre association of Parkinson's patients, a Neurology outpatient clinic and a primary care practice in Pamplona (Spain) | Cross sectional study | 83 | 91 | SQLC | PDQ-39 | Multiple linear regression | The presence of a caregiver was not a significant predictor of PDQ-39 (−1.61 (−9.14,5.90) p = 0.67)) after controlling for age, gender, brief coping, benefit finding, disease severity, psychosocial adjustment, and resources. |
| Oguh 2013 | To determine what measures of PD disability, demographics, and patient quality of life are associated with caregiver strain among caregivers of patients with PD. | Data was obtained from the National Parkinson Foundation's quality Improvement Registry (NPF-QII) | Cross sectional study | 826 | 826 | MCSI | PDQ-39 | Spearman Correlation | The total PDQ-39 score was correlated with MCSI score (r = 0.567, p < 0.00). |
| Peters 2011 | To explore to what extent patient self-reported health, as measured on the disease-specific Parkinson's Disease Questionnaire (PDQ-39), is associated with carer strain and self-reported quality of life. | A postal survey was carried out of both patients and caregivers through local branches of Parkinson's UK. | Cross sectional study | 704 | 901 | CSI | PDQ-39 | Correlation | The PD Index was found to be highly associated with caregiver burden as measured on the CSI (r = 0.56, p < 0.001, n = 422). |
| Prizer 2020 | To assess whether caregiver presence was associated with variations in patient presentation and outcomes in a palliative PD and atypical PD population. | Baseline data from a 3-site randomized controlled trial | Cross-sectional | 210 | 175 | Presence of a caregiver | PDQ-39, PROMIS-29, McGill QOL, QOL-AD | Regression | Quality of life as measured by the QOL-AD questionnaire was better for individuals with caregivers compared to those without caregivers (p < 0.0001). Differences in QOL between people with caregivers and those without caregivers as measured by other scales did not reach significance. |
| Rajiah 2017 | To examine the impact of clinical features on PD patients' QOL, and the impact of PD patients' QOL on their caregivers' burden. | Malaysian Parkinson's Disease Association | Cross-sectional | 122 | 122 | ZBI | PDQ-39 | Correlation | ZBI score was correlated with PDQ-39 score (r = 0.76, p < 0.005). |
| Ricciardi 2015 | To evaluate the relationship quality and satisfaction in couples, in which one partner had PD, obtaining the perspective of both patients and partner and examine the impact of alexithymia, empathy, depression, and anxiety on ratings of relationship quality and satisfaction. | PD patients and their spousal caregivers were recruited at “Centro Studi Lorenzon” in Treviso, Italy, in the context of a free workshop series | Cross sectional study | 15 | 15 | DAS,CoSI | PDQ-39 | Backward Step-wise regression | CoSI was a significant predictor of PDQ-39 social support subscale (beta = −0.606, p = 0.004). |
| Rodriguez-Violante 2015 | To analyze the relationship between caregiver burden and PD patients' quality of life. | Outpatient clinic | Cross sectional study | 201 | 250 | ZBI | PDQ-8 | t-test correlation | PDQ-8 score was higher for patients who had caregivers with burden (44.3+/−31) compared to those without burden (28.3 +/−20.6), p = 0.004. A moderate correlation was observed between PDQ-8 and ZBI (r = 0.35, p < 0.001) |
| Rosqvist 2019 | To describe and assess satisfaction with care in a sample of patients with late stage PD in Sweden and to identify factors associated with patient satisfaction with care as well as to describe and assess their informal caregivers' satisfaction with support and to identify factors associated with caregivers' satisfaction with support. | Outpatient clinic | Cross sectional study | 76 | 107 | Caregiver satisfaction with support | SEIQOL | logistic regression | PWP quality of life was not significantly associated with caregiver satisfaction with support (p = 0.623). |
| Tan 2019 | To investigate the characteristics of PD patients related to different levels of caregiver burden. | Outpatient clinic | Cross sectional study | 104 | 104 | ZBI | PDQ-39 | ANOVA | The median PDQ-39 scores was significantly higher in the high caregiver burden group compared to no-or little group (30.7 vs. 16.2, p-value 0.002). The high caregiver burden group had significantly higher median scores for domain 2 (ADL, p-value 0.005), domain 4 (stigma, p-value 0.005), and domain 6 (cognition, p-value 0.002) compared to no-or little group. |
| Tanji 2008 | To assess the association between mutuality of the marital relationship in Parkinson's disease with disease severity, disability, mental health, quality of life, and caregiver burden. | Outpatient clinic | Cross sectional study | 96 | 96 | MS | SF-12v2 | Correlation | Spouse reported mutuality was not significantly correlated with physical health QOL (p = 0.20) or mental health QOL (p = 0.10). |
| Torny 2018 | To determine correlations between the intensity of disease burden and characteristics of patients and their spouses. | Outpatient clinic | Cross sectional study | 38 | 38 | ZBI | PDQ-8 | Correlation | PDQ-8 was correlated with ZBI score (r = 0.27, p = 0.007). |
| Trang 2020 | To determine predictors of general QOL in a population of PDRD patients with high needs and advanced disease and to compare patient ratings of general QOL to health-related QOL and general patient QOL as reported by caregivers. | Baseline data obtained from a multisite randomized controlled trial of outpatient palliative care | Cross-sectional | 210 | 175 | HADS, FACIT, QOL-AD, ZBI | QOL-AD, PDQ-39 | Regression (Elastic Nets Model) | Caregiver burden (ZBI) was associated with PDQ-39 (r = 0.1105, p = 0.0394). |
| Valldeoriola 2021 | To assess, the effect of 6-month treatment with LCIG on the QOL of patients with APD using the self-reported PDQ-39. | Outpatient clinics | Longitudinal | 62 | 62 | SQLC, ZBI, CSI, GAS, GDS | PDQ-39 | Regression | Improvements in patients' QOL (PDQ-39) did not correspond with improvements in caregivers' QOL (SQLC) or caregiver burden (ZBI). |
| Viwattanakulvanid 2014 | To determine and analyze the main determinants of caregiver burden and examine the impact of nocturnal dis-abilities of PD patients on their caregivers. | Multicenter, national outpatient centers | Cross sectional study | 89 | 89 | ZBI | PDQ-8 | Correlation | PDQ-8 was correlated with ZBI score (r = 0.38, p < 0.001). |
| Yuksel 2018 | To assess the impact of early-stage PD on caregiver burden with disease severity, duration, disability and psychiatric symptoms. | Outpatient clinic | Cross sectional study | 30 | 30 | ZBI | SF-36 | Student t test, Mann Whitney U test | Lower caregiver education was related to SF-36 subdomains of the patients (emotional role, social functioning, and pain), p < 0.05). |
Abbreviations: BDI, Beck Depression Inventory; BRIEF-A, Behavior Rating Inventory of EF-Adult Version; BSFC, Burden Scale for Family Caregivers; CBI, Caregiver Burden Inventory; CoSI, Couple Satisfaction Index; CSI, Caregiver Strain Index; CSS, Caregiver Stress Scale; DAS, Dyadic Adjustment Scale; EQ-5D, EuroQOL; FACIT, Functional Assessment of Chronic Illness Therapy; GAS, Goldberg Anxiety Scale; GDS, Goldberg Depression Scale; HADS, Hospital Anxiety and Depression Scale; HRQOL, Health Related Quality of Life; LCIG, Levodopa-Carbidopa Intestinal Gel; LSS, Life Satisfaction Scale; MCI, Mild Cognitive Impairment; MCSI, Multidimensional Caregiver Strain Index; McGill QOL, McGill Quality of Life Questionnaire; MoCA, Montreal Cognitive Assessment; MS, Mutuality Scale; NEO-FFI, Neuroticism Extraversion Openness Five-Factor Inventory; Outpatient clinics, Clinic that provides care for patients without requiring a hospital stay; PDQ-Carer, Parkinson's disease Questionnaire for Caregivers; PDQ-39, Parkinson's disease Questionnaire-39; PDQ-8, Parkinson's disease Questionnaire-8; PDRD, Parkinson's Disease and Related Disorders; PROMIS-29, Patient-Reported Outcomes Measurement Information System; QOL-AD, Quality of Life in Alzheimer's Disease; SEIQOL, Schedule for the Evaluation of Individual QOL Questionnaire; SF-36, Short Form-36 Health Survey; SF-8, Short Form-8 Health Survey; SF-12v2, Short Form-12 Health Survey; SQLC, Scale of Quality of Life of Caregivers; VAS, Visual Analog Scale; WPAI, Work Productivity and Activity Impairment.
We employed a narrative approach to describe and synthesize the results of the included articles.24 The results section was divided into themes characterized by caregiver factors that were associated with the QOL of people with PD. These themes included: burden, strain, QOL and satisfaction, psychological factors, demographics, and relationship factors. Next, we followed a process that has been described in previous reviews to create a “summary of association” score for each theme.24-26 We determined if the association between the caregiver factor within each theme and PD QOL was significant and whether the factors were positively or negatively related to QOL. A summary score was used to describe the proportion of evidence within each theme that supported an association (i.e. a significant relationship). We then classified the evidence based on this “summary of association” score according to categories defined in previous reviews: unrelated (0%–33% of studies supporting association), unclear (34%–59% of studies supporting association) or related (60%–100% of studies supporting association).24-26
3 ∣. RESULTS
3.1 ∣. Participant and study characteristics
We identified 32 papers to include in our review. These articles were published between 2002 and 2021. All included papers used a quantitative analysis method. Most papers (n = 17) used correlation analysis, 12 papers used regression analysis, two papers used a chi-square test, two papers used t-tests, one paper used structural equation modeling, and one paper used an ANOVA. Most study designs were cross-sectional (n = 30) and two studies were longitudinal. The median sample size for caregivers was 87 (range: 15–6154). The median sample size for people with PD was 91 (range: 15–7209).
Several different instruments were used to measure QOL in people with PD. The most frequently used instrument was the Parkinson's Disease Questionnaire-39 (PDQ-39) (n = 20).27 Other measures of QOL included the Parkinson's Disease Questionnaire-8 (PDQ-8)28 (n = 6), the 36-Item Short Form Survey (SF-36)29 (n = 3), Visual Analogue Scale (VAS)30 (n = 2), QOL in Alzheimer's disease (Quality of Life in Alzheimer's Disease)31 (n = 2), 12-Item Short Form Survey (SF-12)32 (n = 1), Schedule for the Evaluation of Individual QOL Questionnaire33 (n = 1), Questions on Life Satisfaction scale34 (n = 1), McGill QOL Questionnaire35 (n = 1), Patient-Reported Outcomes Measurement Information System36 (n = 1), and the Euroqol (EQ-5D) (n = 1).37
3.2 ∣. Narrative synthesis
After identifying similar caregiver factors across included studies, we developed seven themes that represented the findings reported in the included studies. These themes included: (1) burden, (2) strain, (3) QOL and satisfaction, (4) demographics, (5) psychological factors, (6) relationship factors, and (7) caregiver input. The following sections describe the key findings for each theme and the summary of association score.
3.3 ∣. Caregiver burden
The most frequently reported caregiver factor was caregiver burden (n = 10). Nine studies reported a significant relationship between caregiver burden and PD QOL, resulting in a summary of association of 90% which indicates caregiver burden is related to PD QOL.38-47 In most studies (n = 8), worse caregiver burden was associated with worse QOL for the PD patient. One article did not report the direction of the association between caregiver burden and PD QOL, only reporting a significant p-value.38
Importantly, all the articles that did report a significant association between these variables relied on univariable analyses (e.g., correlations, t-test, ANOVA) and therefore did not account for potential confounders of the relationship between caregiver burden and PD QOL. The article that did not find a significant relationship between these variables did employ regression, controlling for scores on the Parkinson Fatigue Scale, Nonmotor Symptom Scale, and caregiver QOL.47 However, this study focused on advanced PD patients using levodopa-carbidopa intestinal gel and therefore the findings may not be transferable to the general PD population.
3.4 ∣. Caregiver strain
Another caregiver measure that was evaluated was caregiver strain (n = 6). All six studies identified a significant relationship between caregiver strain and PD QOL (summary of association = 100%).38,48-58 In these studies, higher caregiver strain was associated with worse QOL for the PD patient. Most articles examined this relationship with univariable analyses; however, one article did report the results of a regression analysis that accounted for patient sex, age, comorbidities, Hoehn and Yahr stage, mobility, verbal fluency, recall scores, and the use of treatments for depression, psychosis, and cognition.48 This study still found a significant relationship between caregiver strain and QOL among a large, national sample of people with PD.
3.5 ∣. Quality of life and satisfaction
Another theme that was identified during this narrative approach was caregiver QOL and satisfaction. Findings motivating this theme reported on overall caregiver QOL as measured by a QOL scale and caregiver satisfaction with life and support. Six articles reported on the relationship between this caregiver factor and PD QOL, with most articles (n = 4) revealing a positive relationship.50,59-64 Two articles did not find significant associations between these variables.47,54 Most articles (n = 4) relied on univariable analyses, however, one article that did not report a significant relationship between caregiver QOL and PD QOL, employed a regression analysis, controlling for scores on the Parkinson Fatigue Scale, Nonmotor Symptom Scale, and caregiver burden among a sample with advanced PD who used levodopa-carbidopa intestinal gel. The summary of association score for findings contributing to this theme was 60%, indicating these factors are related.
3.6 ∣. Demographics
There were two papers that reported on three caregiver demographic factors and their relationship to PD QOL. One study examined the relationship between caregiver age and gender on PD QOL and found no significant relationship.55 This study used a regression analysis, controlling for patient mutuality score, UPDRS Part 3 score, Nonmotor Symptom Scale score, and Montreal Cognitive Assessment score. Another study evaluated the relationship between caregiver education and PD QOL. These authors did find that lower caregiver education was related to worse scores on PD patient SF-36 subdomains (emotional role, social functioning, and pain).65 The summary of association score for caregiver demographics is 33% indicating these factors are unrelated.
3.7 ∣. Psychological factors
There were five different psychological factors (e.g. cognitive status, depression, personality, perception of patient anxiety and depression) that were investigated in the articles included in this review. Most of these factors were found to have a relationship with PD QOL, resulting in a summary of association score of 66% (related). Lubomski et al. found that care recipients who had caregivers with mild cognitive impairment also had worse QOL.57 Bartolomei et al. revealed that caregiver depression was correlated with worse PD QOL.49 Another study investigated the relationship between specific caregiver personality traits and care recipient QOL. Ma et al. found that caregiver neuroticism was not significantly associated with PD QOL, while higher caregiver conscientiousness scores associated with better PD QOL.66 The authors also controlled for patient age, gender, disease duration, UPDRS score, and patient neuroticism and conscientiousness in this analysis. Lastly, Kudlicka et al. reported on the relationship between caregivers' rating of their care recipient's anxiety and depression. The caregiver rating of anxiety was found to be significantly related to PD QOL, while the rating of depression was not.67
3.8 ∣. Relationship factors
In addition to identifying individual caregiver factors that contributed to QOL for the care recipient, some papers looked at factors related to the relationship between the caregiver and care recipient and how they affect PD QOL. Three papers investigated the quality of interactions between the caregiver and care recipient, labeled as mutuality score or couple satisfaction.68-73 From the analyses conducted in these included articles, the quality of interactions and PD QOL was found to be unrelated (summary of association = 33%). The only paper that had a significant association between the relationship quality and PD QOL, conducted this analysis with PD QOL subscales.73 The authors only reported a significant association between relationship satisfaction and the social support subscale on the PDQ-39.
3.9 ∣. Caregiver input
Four papers examined the relationship between having a caregiver and PD QOL. Three papers found a negative relationship between having a caregiver or having higher carer input and PD QOL (summary of association score = 75%, related).54,74,75 While these authors did report a significant negative relationship between these variables, it is important to consider the cross-sectional nature of these relationships. All studies reporting on this factor were cross-sectional and therefore, it is impossible to determine the directionality of this association and, therefore, causality. It is likely that people with PD are more likely to need a caregiver when their QOL deteriorates. In fact, a couple of studies included in this section support this idea. Hand et al. found that QOL score was worse for people with PD who had high care input compared to moderate or low care input.74 These researchers also observed significant differences on both the mobility and activities of daily living subscales of the PDQ-39, with people with PD who had high caregiver input also having worse scores on those subscales. This finding suggests that lower QOL scores contribute to the need for a caregiver due to increased disability. Additionally, Navarta-Sanchez et al. found no significant relationship between presence of a caregiver and PD QOL after controlling for age, gender, brief coping, benefit finding, disease severity, psychosocial adjustment, and resources.75 Similarly, Dahodwala et al. found that worse QOL was related to higher odds of having a caregiver present during a clinical visit, however, caregiver presence was also more likely with higher disease severity (Hoehn & Yahr stage 4-5 compared to stage 1).48 These analyses suggest that having a caregiver is more strongly associated with worse disability and longer disease duration which can affect QOL, rather than worse QOL resulting from having a caregiver.
4 ∣. DISCUSSION
We aimed to identify and describe the literature exploring the role of the caregiver in QOL for people with PD. We synthesized research examining caregiver factors associated with care recipient QOL, including caregiver burden, strain, QOL and satisfaction, psychological factors, demographic factors, relationship factors, and caregiver input. Our analysis revealed that one of the most influential and commonly studied caregiver factors was caregiver strain. All articles that investigated the relationship between caregiver strain and PD QOL found a significant relationship between these two variables. Additionally, caregiver burden, psychological factors, and caregiver input were also found to be associated with PD QOL, whereas demographic factors and relationship quality were not. These studies provide some insight into the influential role of a caregiver, however, many relied on univariable analyses and cross-sectional study designs. More research is needed on this topic to better understand the relationship between caregiver factors and QOL for people with PD.
Our systematic review is the first to summarize studies examining the role of the caregiver in the QOL of people with PD. We followed Cochrane's robust methodological procedures during the review process and had more than one reviewer at each stage to reduce bias. We also performed a search in six databases for relevant papers but acknowledge the potential to miss other sources in the gray literature. However, given the observational nature of these studies, we focused on manuscripts whose methods would withstand the scrutiny of peer review.
One major implication of the findings of this review is that several potential targets for interventions that can improve QOL for people with PD were identified. Existing treatments and interventions to improve QOL in this population typically target the person with Parkinson's disease62,63; however, caregivers are common and highly affected by the disease as well.8 This review identified several caregiver characteristics and qualities that could be addressed with an existing intervention known to improve patient QOL in other disease states or could justify and inform the development of a new caregiver intervention.
In addition to informing the design of interventions to improve QOL for people with PD, this review also highlights the importance of evaluating caregiver health and needs during regular clinical visits. Routine caregiver evaluations during care recipient clinic visits have been proposed.52,64 A study by Riffin, Wolff, and Pillemer surveyed US primary care physicians to assess the current practices and barriers to evaluating caregivers during primary care visits. This study revealed how rare caregiver evaluations are in this setting and found that a lack of time was the most common barrier to conducting such an assessment.76 Participants in the study also identified facilitators of routine caregiver evaluation, such as better referral options and an easier referral mechanism.76 PD demands a multi-disciplinary approach to care, with many patients having a movement disorders specialist, psychiatrist/psychologist, physical therapist, occupational therapist, speech-language therapist, and social worker on their medical care team.77-79 However, referrals for caregivers are less common.80 Future research should evaluate the feasibility of incorporating caregiver assessments into movement disorder specialist visits. Several low-burden, self-administered questionnaires are available to assess caregiver burden or strain.17,81,82 Incorporating these measures into routine clinical visits could have implications for caregiver and care recipient health outcomes. Caregivers who fall within a risk category could be referred to additional services to prevent worsening of their own health and the health of their care recipients.
The findings of review also point to a dearth of research examining the relationship between caregiver factors and PD QOL using rigorous methods. Most articles included in this review only evaluated the relationship between the caregiver factor and PD QOL, without accounting for other influential factors. Future research is needed to more systematically study this relationship using multivariate approach to control for potential confounders of the caregiver factor-PD QOL relationship. There are several variables that have previously been shown to influence both PD QOL and the caregiver. For example, most people with PD experience a worsening of symptoms and that require greater caregiver involvement and a reduction in QOL around disease durations of 10 years65,66,83 Additionally, other variables such as level of disability and cognitive status have also been shown to influence both PD QOL and the caregiver.71-73
Furthermore, all studies included in this review were cross-sectional, which only allows us to determine associations between variables and prevents any investigation of causality. Within the caregiver input theme, the reliance on cross-sectional analyses demands a cautious interpretation of the findings. The results reported in this section differ from what has been observed in other caregiving literature, namely, several articles contained findings that having a caregiver was associated with worse QOL. In contrast, in the general caregiving literature the presence of a caregiver has been associated with better outcomes for the care recipient. This discrepancy highlights the need for further, longitudinal investigation of this relationship to determine directionality.
5 ∣. LIMITATIONS
We broadly defined our search strategy to capture all measures of QOL in PD and all study designs. While this approach likely increased the number of articles we included in the review and provided a more comprehensive overview of this topic, it also prevented us from conducting a meta-analysis84 making direct comparison across studies more challenging. One general requirement for a meta-analysis is that the studies are “sufficiently homogenous in terms of subjects involved, interventions, and outcomes to provide a meaningful summary.”85 Unfortunately, even though we had similar outcomes across studies (QOL), the study designs and participant characteristics varied greatly, meaning the results of a meta-analysis would be less meaningful (see Table 3). However, as this is the first review looking at the role of the caregiver in PD QOL, we believe that a narrative summary provides the best method to synthesize information across the studies that were included. We also employed the Popay framework,24 which has been used in other systemic reviews to synthesize information and compare the level of evidence, to address this limitation.
6 ∣. CONCLUSION
Caregivers play a critical role in the management of Parkinson's disease. Our review reveals that caregiver strain is one of the most influential caregiver-level factors that contributed to QOL for people with PD. Caregiver burden, psychological factors, caregiver presence were also found to be associated with PD QOL, whereas demographic factors and relationship quality were not. The findings from this review can inform novel interventions targeting these modifiable caregiver factors. Our research emphasizes the importance of considering the caregiver and their health during clinical visits for people with Parkinson's disease. Our review also indicates the need of additional research investigating the relationship between caregiver factors and PD QOL.
Key points.
Several caregiver-specific characteristics are associated with quality of life (QOL) for the care recipient with Parkinson's disease, including caregiver QOL, burden, strain, conscientiousness, and education level.
Findings reveal several targets for interventions to improve QOL in this population.
The findings of this review uncover a dearth of research examining the relationship between caregiver factors and QOL for the care recipient using rigorous, longitudinal methods. Future research is needed to study this relationship more systematically.
ACKNOWLEDGMENTS
Kate Perepezko is supported by the NIH/NIA F31AG066316 and the Center for Innovative Care in Aging at Johns Hopkins School of Nursing. Jared T. Hinkle is supported by the NIH/NIA F30AG067643 and MSTP at Johns Hopkins (NIH/NIGMS T32 GM136577). Gregory M. Pontone serves on the Parkinson Study Group Scientific Review Committee and consults with Acadia Pharmaceuticals, Inc. Kelly A. Mills is supported by the Parkinson's Foundation.
APPENDIX A
Search Strategy
(“Parkinson Disease”[Mesh] OR parkinson[tiab] OR parkinson's [tiab] OR parkinsons[tiab])
#2 (“Caregivers”[Mesh] OR “Spouses”[Mesh] OR caregiver*[tiab] OR “caring intervention”[tiab] OR “care giver*”[tiab] OR “caregiving”[tiab] OR “care giving”[tiab] OR spouse*[tiab] OR “significant other*”[tiab] OR “family caring”[tiab] OR “family caregiver*”[tiab] OR “family partner*”[tiab] OR husband*[tiab] OR wives[tiab] OR wife[tiab] OR partner[tiab] OR “adult children” [tiab] OR relatives[tiab] OR sibling*[tiab] OR spouse*[tiab] OR carer*[tiab] OR “informal care*”[tiab])
#3 (animals[mh] NOT humans [mh])
#4 (#1 AND #2) NOT #3
APPENDIX B
Quality Appraisal Results
| Research question |
Study population |
Response rate |
Inclusion criteria |
Sample size |
Exposure measure |
Timeframe | Different exposure levels |
Exposure measurement |
Repeated exposure |
Outcome measures |
Blinding of outcome assessors |
Follow- up rate |
Statistical analysis |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bartolomei 2018 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Caap-Ahlgren 2002 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Chu 2019 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Dahodwala 2018 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| daSilva 2008 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Demeulemeester 2015 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Hand 2018 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Henry 2020 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Karlstedt 2017 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Karlstedt 2018 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Kelly 2012 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Kudlicka 2014 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Lubomski 2021 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Ma 2018 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Martinez-Martin 2005 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Miyashita 2011 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Muller 2010 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Navarta-Sanchez 2016 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Oguh 2013 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Peters 2011 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Prizer 2020 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Rajiah 2017 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Ricciardi 2015 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Rodriguez-Violante 2015 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Rosqvist 2019 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Tan 2019 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Tanji 2008 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Torny 2018 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Trang 2020 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Valldeoriola 2021 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 1 |
| Viwattanakulvanid 2014 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
| Yuksel 2018 | 1 | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | N/A | 1 | 0 | N/A | 0 |
APPENDIX C
Data Extraction Form
| Title |
|---|
| Lead author |
| Country in which the study conducted |
| Aim of study |
| Study design |
| Inclusion criteria |
| Exclusion criteria |
| Total number of caregiver participants |
| Total number of participants with PD |
| Analysis used |
| Primary findings |
| Additional notes (optional) |
Footnotes
CONFLICTS OF INTEREST
The author declares that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
- 1.Jankovic J Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatr. 2008;79(4):368–376. 10.1136/jnnp.2007.131045 [DOI] [PubMed] [Google Scholar]
- 2.Schrag A, Jahanshahi M, Quinn N. How does Parkinson's disease affect quality of life? A comparison with quality of life in the general population. Mov Disord. 2000;15(6):1112–1118. [DOI] [PubMed] [Google Scholar]
- 3.Perepezko K, Hinkle JT, Shepard MD, et al. Social role functioning in Parkinson's disease: a mixed-methods systematic review. Int J Geriatr Psychiatr. 2019;34(8):1128–1138. 10.1002/gps.5137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soh S, Morris ME, McGinley JL. Determinants of health-related quality of life in Parkinson’s disease: a systematic review. Park Relat Disord. 2011;17(1):1–9. 10.1016/j.parkreldis.2010.08.012 [DOI] [PubMed] [Google Scholar]
- 5.Saxena S, Saraceno B. WHOQOL User Manual. World Health Organization; 2005. [Google Scholar]
- 6.Halpern AS. Quality of life as a conceptual framework for evaluating transition outcomes. Except Child. 1993;59(6):486–498. 10.1177/001440299305900602 [DOI] [Google Scholar]
- 7.Ventegodt S, Hilden J, Merrick J. Measurement of quality of life I. A methodological framework. TheScientificWorldJOURNAL. 2003;3: 950–961. 10.1100/tsw.2003.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong SL, Gilmour H, Ramage-Morin P. Parkinson's disease: prevalence, diagnosis, and impact. 2014. 10.13140/2.1.4842.9767 [DOI] [PubMed] [Google Scholar]
- 9.Van Houtven CH, Voils CI, Weinberger M. An organizing framework for informal caregiver interventions: detailing caregiving activities and caregiver and care recipient outcomes to optimize evaluation efforts. BMC Geriatr. 2011;11(1):77. 10.1186/1471-2318-11-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldsworthy B, Knowles S. Caregiving for Parkinson's disease patients: an exploration of a stress-appraisal model for quality of life and burden. J Gerontology. Ser b, Psychol Sci Soc Sci. 2008;63(6):P372–P376. 10.1093/geronb/63.6.p372 [DOI] [PubMed] [Google Scholar]
- 11.Martinez-Martin P, Rodriguez-Blazquez C, Forjaz MJ. Quality of life and burden in caregivers for patients with Parkinson's disease: concepts, assessment and related factors. Expert Rev Pharmacoecon Outcomes Res. 2012;12(2):221–230. 10.1586/erp.11.106 [DOI] [PubMed] [Google Scholar]
- 12.Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with alzheimer disease. Neurology. 2006;67(9):1592–1599. 10.1212/01.wnl.0000242727.81172.91 [DOI] [PubMed] [Google Scholar]
- 13.Hoe J, Katona C, Orrell M, Livingston G. Quality of life in dementia: care recipient and caregiver perceptions of quality of life in dementia: the LASER-AD study. Int J Geriatr Psychiatr. 2007;22(10):1031–1036. 10.1002/gps.1786 [DOI] [PubMed] [Google Scholar]
- 14.Burgener S, Twigg P. Relationships among caregiver factors and quality of life in care recipients with irreversible dementia. Alzheimer Dis Assoc Disord. 2002;16(2):88–102. 10.1097/01.WAD.0000015567.76518.5C [DOI] [PubMed] [Google Scholar]
- 15.Brodaty H, Berman K. Interventions for family caregivers of people with dementia. Handbook of the Clinical Psychology of Ageing:549–569. 10.1002/9780470773185.ch32 [DOI] [Google Scholar]
- 16.Liu Z, Heffernan C, Tan J. Caregiver burden: a concept analysis. Int J Nur Sci. 2020;7(4):438–445. 10.1016/j.ijnss.2020.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onega LL. The modified caregiver strain index (MCSI). J Gerontol Nurs. 2013;33(11):19–26. [Google Scholar]
- 18.Khan F, Pallant J, Brand C. Caregiver strain and factors associated with caregiver self-efficacy and quality of life in a community cohort with multiple sclerosis. Disabil Rehabil. 2007;29(16):1241–1250. 10.1080/01443610600964141 [DOI] [PubMed] [Google Scholar]
- 19.Pinquart M, Sörensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects? Int Psychogeriatr. 2006;18(4):577–595. 10.1017/S1041610206003462 [DOI] [PubMed] [Google Scholar]
- 20.van Uem JM, Marinus J, Canning C, et al. Health-related quality of life in patients with Parkinson's disease—a systematic review based on the ICF model. Neurosci Biobehav Rev. 2016;61:26–34. 10.1016/j.neubiorev.2015.11.014 [DOI] [PubMed] [Google Scholar]
- 21.Den Oudsten BL, Van Heck GL, De Vries J. Quality of life and related concepts in Parkinson's disease: a systematic review. Mov Disord. 2007;22(11):1528–1537. 10.1002/mds.21567 [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Institutes of Health. National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies; 2016. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 24.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006;1(1):b92. [Google Scholar]
- 25.Farina N, Page TE, Daley S, et al. Factors associated with the quality of life of family carers of people with dementia: a systematic review. Alzheimer's & Dementia. 2017;13(5):572–581. 10.1016/j.jalz.2016.12.010 [DOI] [PubMed] [Google Scholar]
- 26.Stubbs B, Eggermont L, Soundy A, Probst M, Vandenbulcke M, Vancampfort D. What are the factors associated with physical activity (PA) participation in community dwelling adults with dementia? A systematic review of PA correlates. Arch Gerontol Geriatr. 2014;59(2):195–203. 10.1016/j.archger.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 27.Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The Parkinson's disease questionnaire (PDQ-39): development and validation of a Parkinson's disease summary index score. Age ageing. 1997;26(5):353–357. 10.1093/ageing/26.5.353 [DOI] [PubMed] [Google Scholar]
- 28.Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The PDQ-8: development and validation of a short-form Parkinson's disease questionnaire. Psychol Health. 1997;12(6):805–814. 10.1080/08870449708406741 [DOI] [Google Scholar]
- 29.Patel AA, Donegan D, Albert T. The 36-item short form. JAAOS-Journal Am Acad Orthop Surg. 2007;15(2):126–134. 10.5435/00124635-200702000-00007 [DOI] [PubMed] [Google Scholar]
- 30.Crichton N Visual analogue scale (VAS). J Clin Nurs. 2001;10(5):706. [Google Scholar]
- 31.Thorgrimsen L, Selwood A, Spector A, et al. Whose quality of life is it anyway?: the validity and reliability of the quality of life-alzheimer's disease (QoL-AD) scale. Alzheimer Dis Assoc Disord. 2003;17(4):201–208. 10.1097/00002093-200310000-00002 [DOI] [PubMed] [Google Scholar]
- 32.Ware JE Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 33.Mcgee H Schedule for the evaluation of individual quality of life (SEIQoL): a direct weighting procedure for quality of life domains (SEIQoL-DW) quality of life of patients with breast cancer view project latent structure of the hospital anxiety and depression scale view project ciaran O'boyle royal college of surgeons in Ireland. 1993. [Google Scholar]
- 34.Henrich G, Herschbach P. Questions on life satisfaction (FLZM): a short questionnaire for assessing subjective quality of life. Eur J Psychol Assess. 2000;16(3):150–159. 10.1027/1015-5759.16.3.150 [DOI] [Google Scholar]
- 35.Cohen SR, Mount BM, Strobel MG, Bui F. The McGill quality of life questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliat Med. 1995;9(3):207–219. 10.1177/026921639500900306 [DOI] [PubMed] [Google Scholar]
- 36.Ader DN. Developing the patient-reported outcomes measurement information system (PROMIS). Med Care. 2007;45(5):S1–S2. 10.1097/01.mlr.0000260537.45076.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balestroni G, Bertolotti G. ARTICOLO ORIGINALE L'EuroQol-5D (EQ-5D): uno strumento per la misura della qualità della vita EuroQol-5D (EQ-5D): an instrument for measuring quality of life. 1975. [DOI] [PubMed] [Google Scholar]
- 38.Bartolomei L, Pastore A, Meligrana L, et al. Relevance of sleep quality on caregiver burden in Parkinson's disease. Neurol Sci. 2018;39(5):835–839. 10.1007/s10072-018-3252-2 [DOI] [PubMed] [Google Scholar]
- 39.Caap-Ahlgren M, Dehlin O. Factors of importance to the caregiver burden experienced by family caregivers of Parkinson’s disease patients. Aging Exp Res. 2002;5. [DOI] [PubMed] [Google Scholar]
- 40.Rajiah K, Maharajan MK, Yeen SJ, Lew S. Quality of life and caregivers' burden of Parkinson's disease. Neuroepidemiology. 2017;48(3–4):131–137. 10.1159/000479031 [DOI] [PubMed] [Google Scholar]
- 41.Rodríguez-Violante M, Camacho-Ordoñez A, Cervantes-Arriaga A, González-Latapí P, Velázquez-Osuna S. Factors associated with the quality of life of subjects with Parkinson's disease and burden on their caregivers. Neurologia. 2015;30(5):257–263. 10.1016/j.nrleng.2014.01.002 [DOI] [PubMed] [Google Scholar]
- 42.Müller T, Woitalla D. Quality of life, caregiver burden and insurance in patients with Parkinson’s disease in Germany. Eur J Neurol. 2010;17(11):1365–1369. 10.1111/j.1468-1331.2010.03033.x [DOI] [PubMed] [Google Scholar]
- 43.Trang I, Katz M, Galifianakis N, et al. Predictors of general and health-related quality of life in Parkinson's disease and related disorders including caregiver perspectives. Park Relat Disord. 2020;77:5–10. 10.1016/j.parkreldis.2020.05.036 [DOI] [PubMed] [Google Scholar]
- 44.Torny F, Videaud H, Chatainier P, Tarrade C, Meissner WG, Couratier P. Factors associated with spousal burden in Parkinson's disease. Rev Neurol. 2018;174(10):711–715. 10.1016/j.neurol.2018.01.372 [DOI] [PubMed] [Google Scholar]
- 45.Tan MM, Lim EC, Nadkarni NV, Lye WK, Tan EK, Prakash KM. The characteristics of patients associated with high caregiver burden in Parkinson's disease in Singapore. Front Neurol. 2019;10:561. 10.3389/fneur.2019.00561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Viwattanakulvanid P, Kaewwilai L, Jitkritsadakul O, et al. The impact of the nocturnal disabilities of Parkinson’s disease on caregivers’ burden: implications for interventions. J Neural Transm. 2014;121(1):15–24. 10.1007/s00702-014-1200-8 [DOI] [PubMed] [Google Scholar]
- 47.Valldeoriola F, Catalán MJ, Escamilla-Sevilla F, et al. Patient and caregiver outcomes with levodopa-carbidopa intestinal gel in advanced Parkinson’s disease. NPJ Parkinson's Dis. 2021;108(1):7. 10.1038/s41531-021-00246-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dahodwala N, Shah K, He Y, et al. Sex disparities in access to caregiving in Parkinson disease. Neurology. 2018;90(1):e48–e54. 10.1212/wnl.0000000000004764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.da Silva EG, Cuziol K, Viana MA, Barasnevicius EMA. Quality of life in patients with Parkinson's disease and their caregivers’ stress levels. Revista Neurociências. 2008;16(2):113–117. 10.34024/rnc.2008.v16.8647 [DOI] [Google Scholar]
- 50.Demeulemeester F, De Letter M, Miatton M, Santens P. Quality of life in patients with PD and their caregiving spouses: a view from both sides. Clin Neurol Neurosurg. 2015;139:24–28. 10.1016/j.clineuro.2015.08.027 [DOI] [PubMed] [Google Scholar]
- 51.Kelly DH, McGinley JL, Huxham FE, et al. Health-related quality of life and strain in caregivers of Australians with Parkinson's disease: an observational study. BMC Neurol. 2012;12(1):1–7. 10.1186/1471-2377-12-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oguh O, Kwasny M, Carter J, Stell B, Simuni T. Caregiver strain in Parkinson's disease: national Parkinson foundation quality initiative study. Park Relat Disord. 2013;19(11):975–979. 10.1016/j.parkreldis.2013.06.015 [DOI] [PubMed] [Google Scholar]
- 53.Peters M, Fitzpatrick R, Doll H, Playford D, Jenkinson C. Does self-reported well-being of patients with Parkinson's disease influence caregiver strain and quality of life? Park Relat Disord. 2011;17(5):348–352. 10.1016/j.parkreldis.2011.02.009 [DOI] [PubMed] [Google Scholar]
- 54.Rosqvist K, Hagell P, Iwarsson S, Nilsson MH, Odin P. Satisfaction with care in late stage Parkinson's disease. Parkinson's Dis. 2019;2019:1–10. 10.1155/2019/2593547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Karlstedt M, Fereshtehnejad S, Aarsland D, Lökk J. Determinants of dyadic relationship and its psychosocial impact in patients with Parkinson's disease and their spouses. Parkinson's Dis. 2017;2017: 1–9. 10.1155/2017/4697052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yuksel B, Ak PD, Sen A, Sariahmetoglu H, Uslu SC, Atakli D. Eredeti közlemény caregiver burden and quality of life in early stages of idiopathic Parkinson’s disease. SZEMLE. 2018;71(9-10):343–350. 10.18071/isz.71.0343 [DOI] [PubMed] [Google Scholar]
- 57.Lubomski M, Davis RL, Sue CM. Cognitive influences in Parkinson's disease patients and their caregivers: perspectives from an australian cohort. Front Neurol. 2021;12. 10.3389/fneur.2021.673816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ma X, Meng G, Tan Y, et al. Patient and family caregiver's neuroticism and conscientiousness personality in relation to quality of life of patient with Parkinson's disease: a cross-sectional study neuroticism and conscientiousness personality in relation to QoL of patient with PD. Front Neurol. 2018;9:754. 10.3389/fneur.2018.00754. https://www.ncbi.nlm.nih.gov/pubmed/30254602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chu SY, Tan CL. Perception on the quality of life, communication and life satisfaction among individuals with parkison’s and their caregivers. Ethiopian J Health Sci. 2019;29(5). 10.4314/ejhs.v29i5.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martinez-Martin P, Benito-Leon J, Alonso F, et al. Quality of life of caregivers in Parkinson's disease. Qual Life Res. 2005;14(2):463–472. 10.1007/s11136-004-6253-y [DOI] [PubMed] [Google Scholar]
- 61.Henry RS, Lageman SK, Perrin PB. The relationship between Parkinson’s disease symptoms and caregiver quality of life. Rehabil Psychol. 2020;65(2):137–144. 10.1037/rep0000313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Martinez-Martin P, Deuschl G. Effect of medical and surgical interventions on health-related quality of life in Parkinson's disease. Mov Disord. 2007;22(6):757–765. 10.1002/mds.21407 [DOI] [PubMed] [Google Scholar]
- 63.Chen K, Tan Y, Lu Y, Wu J, Liu X, Zhao Y. Effect of exercise on quality of life in Parkinson's disease: a systematic review and meta-analysis. Parkinson's Dis. 2020;2020:1–10. 10.1155/2020/3257623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brown LJ, Potter JF, Foster BG. Caregiver burden should be evaluated during geriatric assessment. J Am Geriatr Soc. 1990;38(4):455–460. 10.1111/j.1532-5415.1990.tb03545.x [DOI] [PubMed] [Google Scholar]
- 65.Lokk J Caregiver strain in Parkinson's disease and the impact of disease duration. Eur J Phys Rehabil Med. 2007;44(1). [PubMed] [Google Scholar]
- 66.Auyeung M, Tsoi TH, Mok V, et al. Ten year survival and outcomes in a prospective cohort of new onset Chinese Parkinson's disease patients. J Neurol Neurosurg Psychiatr. 2012;83(6):607–611. 10.1136/jnnp-2011-301590 [DOI] [PubMed] [Google Scholar]
- 67.Kudlicka A, Clare L, Hindle JV. Quality of life, health status and caregiver burden in Parkinson's disease: relationship to executive functioning. Int J Geriatr Psychiatr. 2014;29(1):68–76. 10.1002/gps.3970 [DOI] [PubMed] [Google Scholar]
- 68.Karlstedt M, Fereshtehnejad S, Aarsland D, Lökk J. Mediating effect of mutuality on health-related quality of life in patients with Parkinson’s disease. Parkinson's Dis. 2018;2018:9548681–9548688. 10.1155/2018/9548681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tanji H, Anderson KE, Gruber-Baldini AL, et al. Mutuality of the marital relationship in Parkinson's disease. Mov Disord. 2008;23(13):1843–1849. 10.1002/mds.22089 [DOI] [PubMed] [Google Scholar]
- 70.Ricciardi L, Pomponi M, Demartini B, et al. Emotional awareness, relationship quality, and satisfaction in patients with Parkinson’s disease and their spousal caregivers. J Nerv Ment Dis. 2015;203(8):646–649. 10.1097/nmd.0000000000000342 [DOI] [PubMed] [Google Scholar]
- 71.Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: three-step approaches using M plus. Struct Equ Model A Multidiscip J. 2014;21(3):329–341. 10.1080/10705511.2014.915181 [DOI] [Google Scholar]
- 72.Bolck A, Croon M, Hagenaars J. Estimating latent structure models with categorical variables: one-step versus three-step estimators. Polit Anal. 2004;12(1):3–27. 10.1093/pan/mph001 [DOI] [Google Scholar]
- 73.Kuhlman GD, Flanigan JL, Sperling SA, Barrett MJ. Predictors of health-related quality of life in Parkinson's disease. Park Relat Disord. 2019;65:86–90. 10.1016/j.parkreldis.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 74.Hand A, Oates LL, Gray WK, Walker RW. The role and profile of the informal carer in meeting the needs of people with advancing Parkinson's disease. Aging Ment Health. 2018;23(3):337–344. 10.1080/13607863.2017.1421612 [DOI] [PubMed] [Google Scholar]
- 75.Navarta-Sanchez MV, Senosiain Garcia JM, Riverol M, et al. Factors influencing psychosocial adjustment and quality of life in Parkinson patients and informal caregivers. Qual Life Res. 2016;25(8):1959–1968. 10.1007/s11136-015-1220-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Riffin C, Wolff JL, Pillemer KA. Assessing and addressing family caregivers' needs and risks in primary care. J Am Geriatr Soc. 2021;69(2):432–440. 10.1111/jgs.16945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Van Der Marck MA, Kalf JG, Sturkenboom IHWM, Nijkrake MJ, Munneke M, Bloem BR. Multidisciplinary care for patients with Parkinson's disease. Park Relat Disord. 2009;15:S219–S223. 10.1016/s1353-8020(09)70819-3 [DOI] [PubMed] [Google Scholar]
- 78.van der Marck MA, Bloem BR, Borm GF, Overeem S, Munneke M, Guttman M. Effectiveness of multidisciplinary care for Parkinson's disease: a randomized, controlled trial. Mov Disord. 2013;28(5):605–611. 10.1002/mds.25194 [DOI] [PubMed] [Google Scholar]
- 79.Post B, van der Eijk M, Munneke M, Bloem BR. Multidisciplinary care for Parkinson's disease: not if, but how. Practical Neurol. 2011;11(2):58–61. 10.1136/jnnp.2011.241604 [DOI] [PubMed] [Google Scholar]
- 80.Lageman SK, Mickens MN, Cash TV. Caregiver-identified needs and barriers to care in Parkinson's disease. Geriatr Nurs. 2015;36(3):197–201. 10.1016/j.gerinurse.2015.01.002 [DOI] [PubMed] [Google Scholar]
- 81.Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O'Donnell M. 830 O’Donnell M (2001) the zarit burden interview: a new short 831 version and screening version. Gerontol. 2001;41(5):652–657. 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- 82.Jenkinson C, Dummett S, Kelly L, et al. The development and validation of a quality of life measure for the carers of people with Parkinson’s disease (the PDQ-carer). Park Relat Disord. 2012;18(5):483–487. 10.1016/j.parkreldis.2012.01.007 [DOI] [PubMed] [Google Scholar]
- 83.Boersma I, Jones J, Coughlan C, et al. Palliative care and Parkinson's disease: caregiver perspectives. J Palliat Med. 2017;20(9):930–938. 10.1089/jpm.2016.0325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Deeks JJ, Higgins JP, Altman DG. Analysing data and undertaking meta-analyses. In: Higgins J, Thomas J, Chandler J, et al. , eds. Cochrane handbook for systematic reviews of interventions; 2022. [Google Scholar]
- 85.Haidich A Meta-analysis in medical research. Hippokratia. 2010;14((Suppl 1)):29. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.