Abstract
Background
Health care accounts for almost 10% of the United States’ greenhouse gas emissions, accounting for a loss of 470,000 disability-adjusted life years based on the health effects of climate change. Telemedicine has the potential to decrease health care’s carbon footprint by reducing patient travel and clinic-related emissions. At our institution, telemedicine visits for evaluation of benign foregut disease were implemented for patient care during the COVID-19 pandemic. We aimed to estimate the environmental impact of telemedicine usage for these clinic encounters.
Methods
We used life cycle assessment (LCA) to compare greenhouse gas (GHG) emissions for an in-person and a telemedicine visit. For in-person visits, travel distances to clinic were retrospectively assessed from 2020 visits as a representative sample, and prospective data were gathered on materials and processes related to in-person clinic visits. Prospective data on the length of telemedicine encounters were collected and environmental impact was calculated for equipment and internet usage. Upper and lower bounds scenarios for emissions were generated for each type of visit.
Results
For in-person visits, 145 patient travel distances were recorded with a median [IQR] distance travel distance of 29.5 [13.7, 85.1] miles resulting in 38.22–39.61 carbon dioxide equivalents (kgCO2-eq) emitted. For telemedicine visits, the mean (SD) visit time was 40.6 (17.1) min. Telemedicine GHG emissions ranged from 2.26 to 2.99 kgCO2-eq depending on the device used. An in-person visit resulted in 25 times more GHG emissions compared to a telemedicine visit (p < 0.001).
Conclusion
Telemedicine has the potential to decrease health care’s carbon footprint. Policy changes to facilitate telemedicine use are needed, as well as increased awareness of potential disparities of and barriers to telemedicine use. Moving toward telemedicine preoperative evaluations in appropriate surgical populations is a purposeful step toward actively addressing our role in health care’s large carbon footprint.
Keywords: Telemedicine, Environmental impact, Carbon footprint, Foregut clinic, Telehealth
Health care is a major contributor to environmental pollution. In 2009, one study found that the US health care sector was estimated to contribute 8% of US emissions [1]. Several years later, another study estimated that in 2013, the US health care greenhouse gas (GHG) emissions had increased to 9.8% of the national total [2]. Other countries such as Australia and Canada have found similar results [3, 4]. Studies have shown that a large component of emissions come from the inpatient hospital setting. A review on CO2 emissions of operating rooms found annual emissions as high as 5 million kg of CO2 [5]. With this known impact of health care on the environment, multiple researchers have published articles with calls to action and proposed solutions, including diligent quantification of carbon emissions, hospital infrastructure updates, and decreasing waste in the supply chain [6–11].
Telemedicine has been proposed by several researchers as a means of reducing carbon emissions. In pediatric surgical and pre-anesthesia clinics, the use of telemedicine significantly decreased CO2 emissions [12]. A French study found a 99% decrease in GHG emissions with the use of telemedicine for Urology clinic visits during COVID compared to in-person visits prior to COVID prior usage [13]. Lastly, researchers in Sweden investigated the use of telemedicine in rehabilitation units and found a 97.5–98.5% decrease in GHG emissions with the implementation of telemedicine compared to in-person visits [14]. Applications of telemedicine sharply increased during the COVID pandemic. In 2020, telemedicine visits rose from 0.3 to 23.6% of contacts the prior year [15]. Our institution found similar results with an increase in telemedicine visits from 0.8 to 38% [16]. While there has been a more recent return to in-person clinic visits with relaxing of COVID-related restrictions, telemedicine use has continued due to the many advantages it confers to patients and institutions. Telemedicine has been shown to decrease costs across different specialties [17, 18], while also harboring the potential to decrease health care’s carbon footprint.
Although some have argued that preoperative visits are not suitable for surgical patients due to the need for a physical exam, our institution found that it is feasible to conduct the preoperative work-up and evaluation for operative benign foregut disease virtually [16]. This patient population undergoes a robust diagnostic work-up prior to consultation with a surgeon that includes endoscopic, imaging, and functional studies; therefore, the in-person portions of the preoperative exam have less bearing on operative decision-making.
While it can be assumed that telemedicine reduces carbon emissions through reductions in travel and consequent fossil fuel usage, rigorous quantification of the impact of telemedicine are still required to understand the potential broader effects telemedicine can have on climate change. Telemedicine itself requires GHG-producing infrastructure, such as hardware (computers, phones), internet connectivity, and electricity usage. Life cycle assessment (LCA) is a validated technique used to estimate the environmental impact of various industrial and commercial processes [19]. The use of LCA in the health care sector has been growing because of its ability to capture the environmental impact of products, systems, and processes from cradle to grave in order to provide a comprehensive summary of waste and GHG emissions associated with various health care activities [20]. To assess environmental sustainability, LCA evaluates the complete life cycle of the studied process, accounting for all phases of a process, including materials extraction, production of disposable and reusable equipment, transportation, utilization of products and materials, energy consumption, and disposal. This study utilized LCA to quantify the current usage and carbon footprint of telemedicine in a general surgery subspecialty clinic.
Methods
The functional unit of our study was one preoperative visit to benign foregut clinic. The GHG emissions for a telemedicine visit and an in-person visit were calculated using LCA based on the emissions of determined inputs for each type of visit. In this study, the scope of the LCA for telemedicine visits was defined as the full-patient visit from the start of the virtual encounter to its completion. Inputs used to determine emissions included the equipment used for video conferencing, energy requirements for broadband internet, and the length of the visit. For in-person visits, the scope encompassed patient travel to and from clinic as well as products used during the visit. The ecoinvent database, an internationally recognized database of environmental assessments of products and services, was accessed [21]. When a specific product’s LCA was not available, economic input–output LCA utilizing known economic information to estimate associated emissions was used. Using these inputs, a Monte Carlo Analysis (MCA) was used with 10,000 simulations to account for variability in the data. MCA generates simulations based on a distribution of known data points. In our study, we also used MCA to simulate low and high endpoints of possible GHG emissions for various inputs to generate upper and lower bounds scenarios.
Telemedicine inputs: computer usage
Telemedicine visit times were collected prospectively. It is assumed that the telemedicine conference call times follow a normal distribution and that the patients can use any of the following devices for their telemedicine session: desktop, laptop, tablet, or phone. The provider was assumed to have used a desktop computer as this was standard during all observed telemedicine visits. The environmental impact for the production and end-of-life disposal of the computer devices was determined from information provided by the leading manufacturer’s website. The total environmental impact of the manufacturing and end-of-life disposal of the devices used for telemedicine was then divided by the lifespan of the devices to determine the per-hour environmental impact of computer usage. This quantity was then multiplied by the telemedicine visit time to determine the device’s per-visit environmental impact. We assumed that the patients use their devices for 5 h per week for three years, and the providers use their computers for 5 h per day for four years. The following Eq. (1) shows the computer usage:
| 1 |
In Eq. (1), N is the number of devices, CF is the carbon footprint of the production and end-of-life disposal of the device, t is the duration of telemedicine conference call, and DLF is the life span of the considered device.
Network data usage
Internet usage during telemedicine is a potentially important source of GHG emissions. The teleconference call may be routed through a number of servers. In this study, it is assumed that the calls are routed through a single server. Equation (2) is used to calculate the environmental impact of internet data transfer and server usage.
| 2 |
| 3 |
| 4 |
In Eqs. (3) and (4), E is the GHG emission per kWh of electricity use, taken to be 0.6 kgCO2-eq. (1), I is the energy density of internet (kWh/GB), D is the internet data transfer rate (Mbps), S is the server number, and W is the wattage of server. In this study, the following values of I, D, and W were considered 0.64 kWh/GB, 5.5 Mbps, and 0.6 kWh/server, respectively (2).
In-person visit calculations
For in-person visits, round-trip travel distance data were collected retrospectively from a representative sample of patient visits in the third quarter of 2020. These data were fitted to several distributions to find the best-fit distribution, which produces a minimum error. It was found that a log-normal distribution best described the travel distance data. It was assumed that patients would travel the one-way distance to the clinic by car if the distance was less than 300 miles and by air, if the distance was 300 miles or greater. Based on the data from Holmner et al. [14] and ecoinvent database, we determined that per kilometer of travel, a car produces 0.5 kgCO2-eq and a kilometer traveled by air produces 0.0245 kgCO2-Eq. (1, 3). Additional inputs for in-person visits included disposable items (e.g., paper handouts, exam table paper sheets, hand sanitizer) and durable medical equipment (DME, e.g., blood pressure cuff, weight scale, pulse oximeter, digital thermometer). Calculated GHG emissions of disposable products are based on material type, and emissions attributable to DME are based on LCA inventory data from Ecoinvent. We excluded facilities-related inputs, such as hospital building electricity use, heating, ventilation, and cooling, as well as clinic electricity use as these are a part of the larger hospital structure and are not altered by telemedicine vs. in-person appointments.
Results
For in-person visits, 145 patient round-trip travel distances were recorded. The median [IQR] distance traveled was 29.5 [13.7, 85.1] miles. For telemedicine visits, prospective data from 10 visits were recorded and when fit to a normal distribution, the mean (SD) was 40.6 (17.1) minutes. The GHG emissions from telemedicine visits and from in-person visits were determined after running 10,000 simulations using Monte Carlo method. For telemedicine, if patients used desktop computers, the GHG emissions were 2.99 kgCO2-eq; if they used all-in-one computers (AIO) or laptops, the GHG emissions were 2.62 kgCO2-eq; if they used tablets, the GHG emissions were 2.26 kgCO2-eq; and if they used cell phones, the GHG emissions were 2.22 kg CO2-eq (Fig. 1). For in-person visits, based on the log-normal distribution of travel distance inputs for the Monte Carlo simulation, one visit via car travel emitted 38.22 kgCO2-eq and one visit via plane travel emitted 39.61 kgCO2-eq (Fig. 1). The GHG emissions for paper products, hand sanitizer, gloves, cleaning wipes, and durable medical equipment that were utilized during in-person visits were negligible compared to GHG emissions for patient travel and are listed in Table 1. Telemedicine visits resulted in less GHG emissions than in-person visits (2.22–2.99 kgCO2-eq vs. 38.22–39.61 kgCO2-eq, p < 0.001). There were no canceled cases in the telemedicine group due to lack of preoperative physical exam.
Fig. 1.
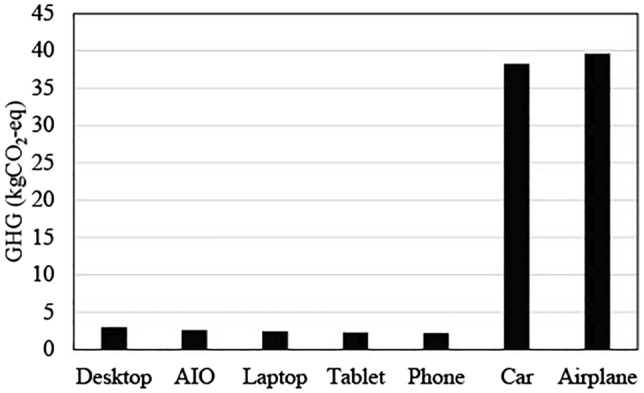
GHG emissions across different telemedicine visit choices and in-person visit travel types. GHG = greenhouse gas, kgCO2-eq = carbon dioxide equivalents, AIO = all-in-one device
Table 1.
GHG emissions for materials and durable medical equipment used during an in-person visit
| Product | GHG (kgCO2-eq) |
|---|---|
| Hand sanitizer | 0.015 |
| Table Sheet | 0.028 |
| Paper sheet | 0.026 |
| Gloves | 0.065 |
| Cleaning wipe | 0.039 |
| BP cuff | 0.011 |
| Thermometer | 0.070 |
| Pulse oximeter | 0.009 |
| Weight scale | 0.045 |
GHG greenhouse gas, kgCO2-eq carbon dioxide equivalents, BP blood pressure
Discussion
Increasing carbon emissions from provision of health care in the USA continues to endanger the environment and human health, with surgical care being a major contributor. This study augments prior research using LCA to quantify the reduction in GHG emissions associated with using telemedicine to conduct preoperative patient evaluations for benign foregut disease. While our study was limited to benign foregut clinic, these findings could be extrapolated to other surgical subspecialties and diseases. Our data provide a compelling case to advocate for expanded use of virtual visits across our health care system in order to reduce carbon emissions. We chose this specialized clinic as the tactile portions of the physical exam have less bearing on operative decision-making than other portions of the evaluation. For a patient with GERD, for example, we rely on a detailed patient history as well as functional and anatomic foregut testing that includes pH testing, esophageal manometry, upper endoscopy, and barium esophagram.
In addition to environmental impact, telemedicine may be of significant benefit to patients. There may be an overall decrease in referral to first appointment times across specialties with telemedicine use [22, 23]. Virtual visits also provide overall shorter time commitment with median overall postoperative visit time being 27.5 min shorter [24]. A vascular surgery clinic found that patients were 2.3 times more likely to complete virtual postoperative visits compared to in-person visits [25].
It is important to note that telemedicine can create “intervention-generated inequalities” [26]. It is well established that there are patient populations who have limited access to telemedicine or who have limited use of telemedicine [12, 27–33]. In fact, the year prior to the onset of the COVID-19 pandemic, the National Health Interview Survey conducted by the CDC found that 18% of responders did not use the internet [34]. Ethical use of telemedicine requires awareness of these disparities. One group aimed to create a telemedicine literacy index using data from the United States Census and Pew Research Institute survey to determine which factors were associated with telemedicine literacy [35]. They found that lower income, lower educational attainment, residing in a rural setting, self-identification as Black, widowed status, and presence of a disability were all associated with lower telemedicine use and access. Similarly, pediatric surgical clinics have found that patients with public insurance or without insurance and non-white patients were more likely to miss telemedicine appointments [36, 37]. In addition to socioeconomic differences, older age was found in some studies to be associated with lower telemedicine usage [38, 39]. However, telemedicine may reduce barriers to care in certain complex and lengthy surgical evaluations, such as living kidney donors. Donors with a low income or of racial minorities face greater barriers to completing the multidisciplinary evaluation and facilitating telemedicine evaluations may mitigate this [40]. Understanding and identifying these disparities is only the first step. Taking the next step to mitigate disparities requires our health care system to adopt inclusive language, facilitate access to telemedicine interpreters, and provide resources to help vulnerable populations access care despite potential limitations in health and technological literacy [41].
In our study, 11% of all visits were out-of-state patients. Patients who must travel a far distance for care are more likely to use telemedicine [12, 37]. Currently, there are policy restrictions on conducting telemedicine visits across state lines. This was mitigated during the pandemic due to emergency measures that were implemented. However, these emergency measures were temporary and for many states these measures have expired or are soon to expire. As Ortega et al. summarized, there are three main barriers: inequitable access to the internet, lack of reimbursement, and lack of institutional buy-in [42]. Permanent federal and state policies that support telemedicine reimbursement and expand affordable broadband internet to rural and undeserved communities will play a key role in dismantling existing barriers and improving access to health care [42, 43].
Our study had several strengths and we acknowledge certain weaknesses. There are certain assumptions that must be made to define inputs for our analysis. For example, the exact types of devices that our patients are using for telemedicine visits is not known. However, a benefit of the MCA is that we can vary the usage percentages of each type of device to create a range from lowest carbon emissions to highest and account for this unknown. We also assume based on known averages, the emissions of patients’ car and plane travel. While our results are not an exact measurement of emissions for each individual patient visit, the Monte Carlo analysis provides an estimate that accounts for the input variability observed in our processes. Despite our relatively conservative estimate of GHG emissions generated from car and air travel, telemedicine visits had significantly lower GHG emissions when compared to in-person visits. Using methods such as LCA to analyze and compare the environmental impact of health care processes allows physicians and policy leaders to develop strategies to minimize health care’s environmental waste and GHG emissions.
A limitation of this study is that we focused on preoperative evaluations to further the discussion that virtual preoperative visits may be appropriate for specific patient populations. There is clearly potential to extend this model to additional perioperative visits across surgical subspecialties without compromising quality of care to further reduce health care’s carbon footprint. However, more investigation needs to be done to achieve consensus on which diseases can be appropriately evaluated using telemedicine. Additionally, we did not quantify the cost associated with patients taking time-off to attend appointments. Many patients do not have paid time-off and in-person visits may place a larger burden on these patients when considering loss of work productivity. In addition, our patient population is unique in that our specialized clinic serves many out-of-state patients. The amount of time-off required to attend an appointment is likely higher for those traveling further and using air travel as their means of transportation. Other costs that we did not factor into our analysis include childcare costs for patients with children. As telemedicine use becomes more prevalent, further research regarding surgeon and patient attitudes toward completely virtual preoperative evaluation is warranted.
Conclusion
Telemedicine has the potential to decrease health care’s carbon footprint and therefore benefit individual and population health. Policy changes are needed to facilitate broader use of telemedicine while reducing disparities in access to health care and technology Moving toward telemedicine preoperative evaluations in select surgical populations is a purposeful step toward actively mitigating health care’s significant carbon footprint.
Declarations
Disclosures
Drs. Sillcox, Meiklejohn, Wright, Oelschlager, Bryant, Tarefder and Zhu, Baraka Gitonga, and Zafrul Khan have no conflicts of interest to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chung JW, Meltzer DO. Estimate of the carbon footprint of the US health care sector. JAMA. 2009;302(18):1970–1972. doi: 10.1001/jama.2009.1610. [DOI] [PubMed] [Google Scholar]
- 2.Eckelman MJ, Sherman J. Environmental impacts of the US health care system and effects on public health. PLoS ONE. 2016;11(6):e0157014. doi: 10.1371/journal.pone.0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malik A, et al. The carbon footprint of Australian health care. Lancet. 2018;2(1):e27–e35. doi: 10.1016/S2542-5196(17)30180-8. [DOI] [PubMed] [Google Scholar]
- 4.Eckelman MJ, Sherman JD, MacNeill AJ. Life cycle environmental emissions and health damages from the Canadian healthcare system: an economic-environmental-epidemiological analysis. PLoS Med. 2018;15(7):e1002623. doi: 10.1371/journal.pmed.1002623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drew J, Christie SD, Tyedmers P, Smith-Forrester J, Rainham D. Operating in a climate crisis: a state-of-the-science review of life cycle assessment within surgical and anesthetic care. Environ Health Perspect. 2021;129(7):76001. doi: 10.1289/EHP8666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schoen J, Chopra V. The harm we do: the environmental impact of medicine. J Hosp Med. 2018;13(5):353–355. doi: 10.12788/jhm.2947. [DOI] [PubMed] [Google Scholar]
- 7.Mortimer F, Pencheon D. Do no harm: addressing the environmental impact of health care. Nat Rev Dis Primers. 2022;8(1):38. doi: 10.1038/s41572-022-00372-8. [DOI] [PubMed] [Google Scholar]
- 8.Capon A, Madden DL, Truskett PG. Environmentally sustainable health care: now is the time for action. Med J Aust. 2020;213(10):479–479.e1. doi: 10.5694/mja2.50825. [DOI] [PubMed] [Google Scholar]
- 9.Stuart N. Environmental sustainability must be on our agenda for healthcare. Healthc Pap. 2020;19(3):4–7. doi: 10.12927/hcpap.2020.26378. [DOI] [PubMed] [Google Scholar]
- 10.Barratt AL, Bell KJ, Charlesworth K, McGain F. High value health care is low carbon health care. Med J Aust. 2022;216(2):67–68. doi: 10.5694/mja2.51331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilkinson E. Reaching net zero carbon emissions in health systems. Lancet. 2021;398(10315):1953–1954. doi: 10.1016/S0140-6736(21)02642-8. [DOI] [PubMed] [Google Scholar]
- 12.Cockrell HC, Maine RG, Hansen EE, Mehta K, Salazar DR, Stewart BT, Greenberg SLM. Environmental impact of telehealth use for pediatric surgery. J Pediatr Surg. 2022;57(12):865–869. doi: 10.1016/j.jpedsurg.2022.06.023. [DOI] [PubMed] [Google Scholar]
- 13.Filfilan A, Anract J, Chartier-Kastler E, Parra J, Vaessen C, de La Taille A, Roupret M, Pinar U. Positive environmental impact of remote teleconsultation in urology during the COVID-19 pandemic in a highly populated area. Prog Urol. 2021;31(16):1133–1138. doi: 10.1016/j.purol.2021.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holmner A, Ebi KL, Lazuardi L, Nilsson M. Carbon footprint of telemedicine solutions–unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE. 2014;9(9):e105040. doi: 10.1371/journal.pone.0105040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiner JP, Bandeian S, Hatef E, Lans D, Liu A, Lemke KW. In-person and telehealth ambulatory contacts and costs in a large US insured cohort before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e212618. doi: 10.1001/jamanetworkopen.2021.2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu J, Lois AW, Gitonga B, Chen-Meekin JY, Williams EJ, Khandelwal S, Carrera Ceron R, Oelschlager BK, Wright AS. The impact of socioeconomic status on telemedicine utilization during the COVID-19 pandemic among surgical clinics at an academic tertiary care center. Surg Endosc. 2022;36(12):9304–9312. doi: 10.1007/s00464-022-09186-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zholudev V, Safir IJ, Painter MN, Petros JA, Filson CP, Issa MM. Comparative cost analysis: teleurology vs conventional face-to-face clinics. Urology. 2018;113:40–44. doi: 10.1016/j.urology.2017.07.034. [DOI] [PubMed] [Google Scholar]
- 18.Cabrera CI, Ning AY, Cai Y, D'Anza B. Systematic review of telehealth cost minimization for patients and health systems in otolaryngology. Laryngoscope. 2021;131(8):1741–1748. doi: 10.1002/lary.29321. [DOI] [PubMed] [Google Scholar]
- 19.Hauschild MZ, Huijbregts MAJ. Life cycle impact assessment. Dordrecht, the Netherlands: Springer; 2015. [Google Scholar]
- 20.Seifert C, Koep L, Wolf P, Guenther E. Life cycle assessment as decision support tool for environmental management in hospitals: a literature review. Health Care Manag Rev. 2021;46(1):12–24. doi: 10.1097/HMR.0000000000000248. [DOI] [PubMed] [Google Scholar]
- 21.Ecoinvent database. https://ecoinvent.org/the-ecoinvent-database Accessed Dec 2022.
- 22.Silverstein RG, McClurg AB, Moore KJ, Fliss MD, Louie M. Patient characteristics associated with access to minimally invasive gynecologic surgery: changes during the COVID-19 pandemic. J Minim Invasive Gynecol. 2022;29(9):1110–1118. doi: 10.1016/j.jmig.2022.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Emmett SD, Platt A, Turner EL, Gallo JJ, Labrique AB, Inglis SM, Jenson CD, Parnell HE, Wang NY, Hicks KL, Egger JR, Halpin PF, Yong M, Ballreich J, Robler SK. Mobile health school screening and telemedicine referral to improve access to specialty care in rural Alaska: a cluster- randomised controlled trial. Lancet Glob Health. 2022;10(7):e1023–e1033. doi: 10.1016/S2214-109X(22)00184-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harkey K, Kaiser N, Zhao J, et al. Postdischarge virtual visits for low-risk surgeries: A randomized noninferiority clinical trial. JAMA Surg. 2021 doi: 10.1001/jamasurg.2020.6265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abou Ali AN, Abdul Malak OM, Hafeez MS, Habib S, Cherfan P, Salem KM, Hager E, Avgerinos E, Sridharan N. Improved outpatient medical visit compliance with sociodemographic discrepancies in vascular telehealth evaluations. J Vasc Surg. 2022;S0741–5214(22):02515. doi: 10.1016/j.jvs.2022.11.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Veinot TC, Mitchell H, Ancker JS. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc. 2018;25(8):1080–1088. doi: 10.1093/jamia/ocy052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carlisle EM, Shakhsheer BA. Ethical issues related to the COVID-19 pandemic that have influenced pediatric surgery. Pediatr Ann. 2022;51(8):e306–e310. doi: 10.3928/19382359-20220606-03. [DOI] [PubMed] [Google Scholar]
- 28.Asare EA, Andreae MH, Stewart JH., 4th Bridging the disparity gap in surgical oncology access: does telehealth hold a key? Ann Surg Oncol. 2022;29(12):7235–7236. doi: 10.1245/s10434-022-12262-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruberto RA, Schweppe EA, Ahmed R, Swindell HW, Cordero CA, Lanham NS, Jobin CM. Disparities in telemedicine utilization during COVID-19 pandemic: analysis of demographic data from a large academic orthopaedic practice. JBJS Open Access. 2022;7(2):e21.00116. doi: 10.2106/JBJS.OA.21.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haynes N, Ezekwesili A, Nunes K, Gumbs E, Haynes M, Swain J. "Can you see my screen?" Addressing racial and ethnic disparities in telehealth. Curr Cardiovasc Risk Rep. 2021;15(12):23. doi: 10.1007/s12170-021-00685-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lattimore CM, Kane WJ, Fleming MA, 2nd, Martin AN, Mehaffey JH, Smolkin ME, Ratcliffe SJ, Zaydfudim VM, Showalter SL, Hedrick TL. Disparities in telemedicine utilization among surgical patients during COVID-19. PLoS ONE. 2021;16(10):e0258452. doi: 10.1371/journal.pone.0258452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poeran J, Cho LD, Wilson L, Zhong H, Mazumdar M, Liu J, Memtsoudis SG. Pre-existing disparities and potential implications for the rapid expansion of telemedicine in response to the coronavirus disease 2019 pandemic. Med Care. 2021;59(8):694–698. doi: 10.1097/MLR.0000000000001585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lott A, Campbell KA, Hutzler L, Lajam CM. Telemedicine utilization at an academic medical center during covid-19 pandemic: are some patients being left behind? Telemed J E Health. 2022;28(1):44–50. doi: 10.1089/tmj.2020.0561. [DOI] [PubMed] [Google Scholar]
- 34.Chagpar AB. Sociodemographic factors affecting telemedicine access: a population-based analysis. Surgery. 2022;171(3):793–798. doi: 10.1016/j.surg.2021.08.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harris A, Jain A, Dhanjani SA, Wu CA, Helliwell L, Mesfin A, Menga E, Aggarwal S, Pusic A, Ranganathan K. Disparities in telemedicine literacy and access in the United States. Plast Reconstr Surg. 2022 doi: 10.1097/PRS.0000000000009939. [DOI] [PubMed] [Google Scholar]
- 36.Tartarilla AB, Tennermann N, Melvin P, Ward VL, Bauer AS. Sociodemographic missed-care predictors for pediatric orthopaedic telemedicine during COVID-19. J Pediatr Orthop. 2022;42(6):e688–e695. doi: 10.1097/BPO.0000000000002112. [DOI] [PubMed] [Google Scholar]
- 37.Gross K, Georgeades C, Farazi M, Calaway L, Gourlay D, Van Arendonk KJ. Utilization and adequacy of telemedicine for outpatient pediatric surgical care. J Surg Res. 2022;278:179–189. doi: 10.1016/j.jss.2022.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Braswell M, Wally MK, Kempton LB, Seymour RB, Hsu JR, Karunakar M, Afetse KE, Bailey G, Bosse M, Brownrigg M, Cuadra M, Dixon A, Girardi C, Grochowski E, Hysong A, Jolissaint J, Macknet D, Mayberry RM, Moody P, Peterson K, Phelps KD, Pollock H, Posey SL, Reid R, Roe K, Scannell B, Sims S, Stanley A, Wohler AD. Age and socioeconomic status affect access to telemedicine at an urban level 1 trauma center. OTA Int. 2021;4(4):e155. doi: 10.1097/OI9.0000000000000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gmunder KN, Ruiz JW, Franceschi D, Suarez MM. Demographics associated with US healthcare disparities are exacerbated by the telemedicine surge during the COVID-19 pandemic. J Telemed Telecare. 2021 doi: 10.1177/1357633X211025939. [DOI] [PubMed] [Google Scholar]
- 40.Al Ammary F, Muzaale AD, Tantisattamoa E, Hanna RM, Reddy UG, Bunnapradist S, Kalantar-Zadeh K. Changing landscape of living kidney donation and the role of telemedicine. Curr Opin Nephrol Hypertens. 2023;32(1):81–88. doi: 10.1097/MNH.0000000000000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc. 2019;26(8–9):855–870. doi: 10.1093/jamia/ocz023.PMID:30958532;PMCID:PMC6696508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ortega G, Rodriguez JA, Maurer LR, Witt EE, Perez N, Reich A, Bates DW. Telemedicine, COVID-19, and disparities: policy implications. Health Policy Technol. 2020;9(3):368–371. doi: 10.1016/j.hlpt.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eruchalu CN, Bergmark RW, Smink DS, Tavakkoli A, Nguyen LL, Bates DW, Cooper Z, Ortega G. Demographic disparity in use of telemedicine for ambulatory general surgical consultation during the COVID-19 pandemic: analysis of the initial public health emergency and second phase periods. J Am Coll Surg. 2022;234(2):191–202. doi: 10.1097/XCS.0000000000000030. [DOI] [PubMed] [Google Scholar]


