Abstract
Female reproductive health is strongly associated with healthy vaginal microbiota, which is thought to be ensured by the dominance of certain Lactobacillus species. Lactobacilli control the vaginal microenvironment through several factors and mechanisms. One of them is their ability to produce hydrogen peroxide (H2O2). The role of Lactobacillus-derived H2O2 in the vaginal microbial community has been intensively investigated in several studies with many designs. However, results and data are controversial and challenging to interpret in vivo. Defining the underlying mechanisms responsible for a physiological vaginal ecosystem is crucial since it could directly affect probiotic treatment attempts. This review aims to summarize current knowledge on the topic, focusing on probiotic treatment possibilities.
Keywords: vaginal microbiota, lactobacilli, hydrogen peroxide, probiotics, reproductive health
1. Introduction
The unique vaginal microbial community with the dominance of Lactobacillus species, described by Döderlein more than a century ago, is considered the hallmark of the healthy vaginal microenvironment and the guarantee of overall vaginal health in women of reproductive age [1,2,3,4,5,6]. According to the predominant lactobacilli, vaginal microbiota composition is characterized by community state types (CSTs) [1]. Currently, CSTs are grouped in 6 bacterial configurations: CST I–Lactobacillus crispatus, CST II–Lactobacillus gasseri, CST III–Lactobacillus iners, CST V–Lactobacillus jensenii [1,7]. The CST IV lacks the significant abundance of a certain Lactobacillus species, and it can be divided into subgroups CST IV-A (modest proportion of L. iners and anaerobic bacteria: Corynebacterium, Finegoldia, Streptococcus, Anaerococcus) and CST IV-B (bacterial vaginosis associated bacteria: Gardnerella, Atopobium, Prevotella [7]. In approximately 90% of women of fertile age, the most prevalent configurations are CSTs I, III and IV [1].
An association between ethnicity and vaginal bacterial community composition was also demonstrated. CST IV (diverse group lacking Lactobacillus dominance) is significantly overrepresented and considered as common and normal in Hispanic and black women as compared with Asian and white women [1]. The reasons for the observed differences among ethnic groups are unknown but suggest host genetic factors determining vaginal bacterial colonization.
Changes and variations in community composition could be mainly affected during the menstrual cycle, by sexual activity or by other unknown factors. However, the vaginal microbiota of some individuals does not demonstrate temporal fluctuation and remains stable over several menstrual cycles [7]. In most cases, altered community composition did not affect community function since changes were observed in the relative abundance of a small number of different lactic acid-producing bacterial species [2,7].
During pregnancy, the diversity and richness of vaginal microbiota decrease compared to the non-pregnant vagina, with a higher abundance of Lactobacillus species [8,9,10]. Additionally, the stability of vaginal microbiota was significantly higher in the early stages of pregnancy and further increased with gestational age [11].
CST I with vaginal L. crispatus dominance is thought to be associated with a healthy vagina, while L. iners-dominance (CST III) is more prone to vaginal dysbiosis [12,13]. Multiple studies have shown the protective effect of L. crispatus against bacterial vaginosis (BV), vulvovaginal candidiasis (VVC), and sexually transmitted infections (STIs) [12,13].
There are several factors and mechanisms how lactobacilli contribute to maintaining a healthy vaginal ecosystem and preserving their dominance over other vaginal microorganisms (summarized in Table 1). It is most likely the combination of these lactobacilli-derived factors responsible for vaginal health and for the prevention of BV, VVC and STIs primarily [2].
Table 1.
Contribution of lactobacilli to a healthy vaginal microbiota.
|
|---|
| Lactic acid production |
|
| Hydrogene peroxide generation |
|
| Bacteriocin synthesis |
|
| Epithelial cell adhesion |
|
| S-layer protein expression |
|
To which extent each mechanism can contribute to a healthy vaginal mucosal microenvironment needs further investigation. For example, the production of lactate acid by vaginal lactobacilli and, thus, the reduced pH in the vagina directly inhibits the growth of a significant proportion of microorganisms occurring in or entering the vagina.
Since the main species of vaginal Lactobacillus can generate hydrogen peroxide (H2O2) and considering the chemical character of the molecule, H2O2 could be another critical element ensuring vaginal Lactobacillus abundance [14,15]. However, findings of clinical and experimental studies revealed inconsistent data and therefore, the significance of vaginal H2O2 is often doubted. This review aims to summarize current knowledge on the possible role of Lactobacillus-derived H2O2 in vaginal health.
2. Characteristics of Hydrogen Peroxide as a Chemical Compound and Oxidizing Agent
Hydrogen peroxide is a water-soluble liquid with an ashen blue color. Besides exogenous sources, such as microbial synthesis, which is the topic of this review, it can be produced in vivo as well, both enzymatically and non-enzymatically. H2O2 is generated by superoxide dismutase through the dismutation of the superoxide anion, or it can be produced directly by different oxidases in the human body (e.g., monoamine oxidase). Non-enzymatically formation of hydrogen peroxide occurs in the mitochondrial matrix as a result of the reduction of the superoxide anion by protons and electrons during terminal oxidation of the glucose metabolic pathway [16,17].
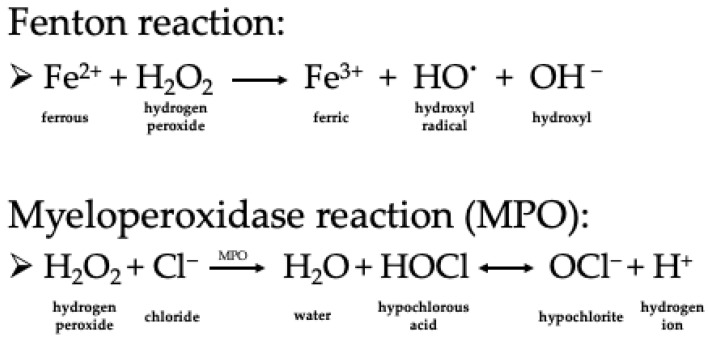
Once present in human tissue, H2O2 can easily cross the cell membrane and act as an oxidizing agent in redox reactions. However, its oxidative capacity remains low, and it is instead an exception with its relatively stable character among reactive oxygen species occurring physiologically in humans [18]. The significant negative impact of hydrogen peroxide is its conversion into the dangerous hydroxyl radical, which rapidly oxidizes cellular macromolecules like DNA, proteins and lipids, acting thereby mutagen/carcinogen and/or direct cytotoxic. The Fenton reaction (soluble Fe(II) donates an electron to a hydrogen peroxide molecule, which splits then into hydroxyl anion and hydroxyl radical spontaneously) is thought to be responsible for the conversion in vivo, as shown in Figure 1 [17,19]. Moreover, H2O2 can release iron from the protein-bound form (heme proteins) and accelerate Fenton chemistry [17,20,21]. Another possible mechanism in humans is the enzyme myeloperoxidase (MPO), which in the presence of halides (like Cl−), is also able to convert H2O2 to hypochlorite (HOCl)(see Figure 1) [22]. It has been shown that cervicovaginal fluids contain adequate levels of MPO, and chloride is also present in the vaginal mucus [14,22].
Figure 1.
Conversion mechanisms of hydrogen peroxide in vivo.
Interestingly, the relative stability of hydrogen peroxide allows the molecule to exert essential and valuable functions for the organism before its spontaneous conversion into a harmful agent. In recent years, a growing body of evidence supported the role of hydrogen peroxide as a signaling molecule, more precisely, as a second messenger. After the formation of H2O2, there is an undefined period for the molecule to communicate the circumstances, namely the oxidative stress in its local environment, by binding to signaling proteins in the cascade [23,24,25,26,27,28]. One of the known targets is the important ubiquitous inflammation mediator, NFκB regulating cell proliferation, apoptosis and tissue repair [27,29,30,31].
3. Bacterial Hydrogen Peroxide Production
Besides endogenous sources of H2O2 in the human body, the occurrence of the molecule in the mucosa is mainly of microbial origin produced by local microbiota members. Lactic acid-producing bacteria, like lactobacilli, streptococci and pneumococci, can release detectable amounts of H2O2 in their environment. These bacteria lack heme and cytochrome proteins for terminal oxidation and utilize flavoproteins which synthesize H2O2 from O2 by oxidizing lactate, pyruvate or NADH with the corresponding enzymes [32,33,34,35]. Bacterial H2O2 can accumulate to a certain extent on mucous membranes since lactic acid bacteria cannot convert it with enzymes like catalase or peroxidase (e.g., NADH peroxidase) by themselves [14,15]. Hydrogen peroxide generating enzymes of bacterial origin were shown to be constitutively expressed, suggesting that H2O2 synthesis mainly depends on environmental O2 [36]
3.1. Hydrogen Peroxide Production in the Vaginal Microbiota
The healthy vaginal microbiota is dominated by the Lactobacillus genus. Although hydrogen peroxide formation by vaginal lactobacilli is a standard feature, it is an exception among intestinal and environmental strains [15]. Synthesis of H2O2 by vaginal lactobacilli is not species-specific but only characteristic of those with facultative anaerobe metabolism [37]. Vaginal colonization by H2O2-producing lactobacilli is as high as 106–107 organisms per ml [15]. Since different levels of H2O2 formation were shown for L. crispatus, there is a variation in hydrogen peroxide production between strains from the same species varying from excellent to non-H2O2 producers [38,39]. According to measurements of cultivated lactobacilli with different detection methods, amounts of H2O2 produced by the most active strains vary from 1.5–2 to 28–30 mg/L, and its detection is only possible after oxygenation of anaerobic cultures or under aerobic culture conditions, which is however, not characteristic for the vaginal lumen microenvironment [40,41,42]. Notably, the L. iners does not generate H2O2 [4,12].
The physiological hydrogen peroxide concentration of the cervicovaginal fluid is 23 ± 5 μM, which is considered low due to the relative oxygen shortage in the vaginal mucosa. Oxygen tension of [43,44] the vagina and consequentially enhanced H2O2 production by lactobacilli may increase, for example, during sexual intercourse, menstruation, inflammation and with the usage of intrauterine devices ([39,41]). Additionally, colonization by H2O2-producing L. crispatus or L. jensenii was more abundant in white women compared to other ethnical groups. [4].
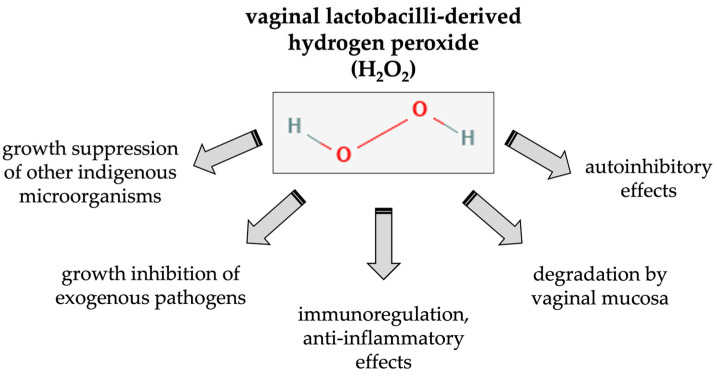
In vitro studies demonstrated the cooperative actions of the primary metabolites of Lactobacillus, lactic acid and hydrogen peroxide. In the presence of lactic acid, H2O2 displayed enhanced antimicrobial killing activity against urogenital and enteric pathogens [42,45,46]. Since lactobacilli do not produce H2O2-inactivating enzymes (e.g., catalase) accumulation of hydrogen peroxide in the immediate area of the lactobacilli themselves may occur. This, in turn, may lead to autoinhibitory effects in lactobacilli caused by self-produced H2O2 [40].
3.2. Effects of Lactobacillus-Derived H2O2 on the Host
In the context of the vaginal microenvironment, locally produced H2O2 by lactobacilli may interact not only with other microorganisms but with vaginal mucosa and its components like epithelial and immune cells. Harmful effects of H2O2 as an oxidizing agent may occur in the host tissue. However, due to unpreventable endogenous H2O2 formations in eukaryotic cells, they are best equipped with neutralizing enzymes, e.g., catalase and peroxidase. As a part of the mucosa-associated lymphatic tissue (MALT), the vaginal mucosa harbors macrophages, natural killer (NK) cells, dendritic cells (DC) and neutrophils in variable distribution influenced mainly by hormonal changes [47,48,49]. The most abundant leukocytes are T lymphocytes, but γδ and mucosal-associated invariant T (MAIT) cells are also present in the vaginal mucosa [50,51,52,53]. IgG and IgA are also found in the vagina; interestingly, in cervicovaginal fluids, IgG concentration is higher than IgA [54]. B cells are found mainly in the ectocervix [53,55].
Possible immunomodulatory effects of H2O2 were suggested in a population-based study: cytokine concentrations were determined in cervicovaginal fluids revealing lower levels of vaginal interleukin (IL)-1β by the dominance of H2O2-producing lactobacilli [56]. IL-1β is a crucial mediator of inflammatory responses. It is released upon intracellular inflammasome activation, mainly by macrophages and dendritic cells. An innate immune subversion through inflammasome inhibition was demonstrated in a recent study showing that the oral commensal H2O2-producing bacterium Streptococcus oralis can block inflammasome activation, which is mediated by hydrogen peroxide [57].
In eukaryotes, hydrogen peroxide has important roles as a signaling molecule regulating various biological processes, like cell proliferation, differentiation, migration, or apoptosis [58]. Although hydrogen peroxide can diffuse across membranes, exogenously produced H2O2 is less effective at eliciting a signaling response than endogenously produced hydrogen peroxide [59]. The concentration of exogenous hydrogen peroxide sufficient to act as a second messenger varies significantly between cells [59,60]. Furthermore, different concentration-specific responses can occur in eukaryotic cells [61]. A large group of redox-regulated proteins is found in almost all cell types, including transcription factors, kinases, phosphatases, and ion channels [58]. A probiotic strain of L. crispatus M247 uses H2O2 as a signal-transducing molecule to induce PPAR-γ (peroxisome proliferator-activated receptors) activation in IEC, directly modulating epithelial cell responsiveness to inflammatory stimuli. PPAR-γ is an endogenous regulator of intestinal inflammation; its activation prevents inflammatory damage in colitis [62].
Figure 2 summarizes the possible main effects of Lactobacillus-derived H2O2 in the vaginal mucosa and microbial community.
Figure 2.
Suggested effects of Lactobacillus-derived H2O2 in the vaginal mucosa and microbial community.
4. The Possible Contribution of Lactobacillus-Derived Hydrogen Peroxide to Vaginal Health: Pros and Cons
In the vaginal micro-ecosystem, the primary impact of hydrogen peroxide on living organisms at the cellular level is believed to be predominantly antimicrobial. The control of the growth of specific microbial populations could contribute to the physiological composition of the vaginal microbiota and ensure the dominance of H2O2-producing lactobacilli. There are mainly two types of studies investigating the effects of vaginal H2O2. Epidemiological studies focused on the presence and ratio of H2O2-producing lactobacilli and its possible association with vaginal dysbiosis and/or infection. Experimental studies were of the microbiological type, investigating characteristics and requirements of bacterial H2O2 synthesis in the culture of vagina-derived Lactobacillus species and its effect on other microbial populations. While epidemiological investigations rather support the protective role of hydrogen peroxide-producing lactobacilli in vaginal health, many in vitro studies failed to demonstrate a significant role of H2O2 in maintaining physiological vaginal microbiota composition.
4.1. Antimicrobial Effects of H2O2: Epidemiological Studies on Bacterial Vaginosis
The first studies focusing on this topic were in vivo observational studies beginning from the late 1980s. Their provide the most supporting data about the positive correlation between the vaginal presence and dominance of H2O2-producing Lactobacillus species and healthy vaginal microbiota. One group of these studies focused on the association between H2O2 lactobacilli and bacterial vaginosis. BV is thought to be a vaginal dysbacteriosis with anaerobic overgrowth (e.g., Gardnerella, Atopobium) with or without symptoms [63,64]. Women with bacterial vaginosis have higher risks for preterm birth, late miscarriage, and HIV infection [65,66,67].
The epidemiological studies on bacterial vaginosis demonstrated a remarkable difference in the prevalence of isolated H2O2-producing lactobacilli in healthy, nonpregnant women and women with bacterial vaginosis. Hydrogen peroxide-generating lactobacilli were detected in the large majority of healthy women whereas only in a small part of women with BV [15,68]. Moreover, differences in vaginal colonization by lactobacilli in healthy women and those with BV were only observed in the H2O2-producing group of Lactobacillus [68,69]. Since the absence of these bacteria in women with bacterial vaginosis was more prevalent than the increased colonization rates of anaerobic bacteria (Gardnerella, Mobiluncus, Mycoplasma), the theory of the presence of H2O2 producing lactobacilli as a critical protective factor in the healthy vaginal microbiota was reasonable [15].
These findings also raised an important question regarding the pathogenesis of BV and the chronology of microbial events resulting in the disease. Do H2O2-positive Lactobacillus species first disappear, and do obligate anaerobic bacteria take over their place or the other way round? A possible answer was provided by longitudinal studies of healthy, nonpregnant women with follow-up visits. They confirmed the lack of H2O2-forming lactobacilli as a primary risk factor for bacterial vaginosis [70]. BV development was four times higher in women without Lactobacillus species producing H2O2 than in women colonized by these bacteria. Harboring any lactobacilli reduced the risk of BV twofold [70]. The acquisition of bacterial vaginosis was significantly higher among women initially colonized with H2O2-producing strains and lost colonization of these species later, compared to persistently colonized women [71]. H2O2-positive strains of L. crispatus and L. jensenii were the most likely to maintain persistent vaginal colonization over the period of the study, suggesting optimized host-microbiota interactions.
Interestingly, vaginal and rectal co-colonization by H2O2-producing L. crispatus species is suggested as another protective factor against BV development. In a cross-sectional study, co-colonization by H2O2-positive lactobacilli was shown to occur very often and was associated with a reduced risk of BV 4-fold compared with vaginal colonization only [72]. According to this observation, H2O2-producing lactobacilli in the distal gastrointestinal tract could contribute to maintaining the dominance and supplying eventual shortages of vaginal lactobacilli.
Epidemiological studies also helped identify several demographic and behavioral factors correlated either positively or negatively with vaginal colonization of H2O2-producing Lactobacillus species. Certainly, several of these factors are also correlated to the development of bacterial vaginosis. Vaginal colonization with H2O2-forming Lactobacillus strains was associated with white race, higher education, the use of barrier contraception and less smoking [70]. Older age, parity, alcohol use, having ≥1 act of vaginal intercourse per week, vaginal cleansing, current BV, and recent use of antibiotics were associated with decreased H2O2+ Lactobacillus isolation. women having ≥1 act of vaginal intercourse per week (no information about condom use) or antibiotic treatment were more likely to lose colonization [71,73]. The possible association with host-specific health issues (e.g., hormone and immunologic status) has not been investigated.
When determining the levels of H2O2 in vaginal secretions, women with BV had lower levels of H2O2 than healthy women’s concentrations (0.04 μg/mL vs. 0.17 μg/mL) [74].
The hypothesis of the protective role of H2O2-producing lactobacilli in the vagina was questioned by some studies suggesting that bacterial vaginosis may develop despite the presence of lactobacilli with H2O2 formation [75,76]. For example, in most of the investigated BV cases with large numbers of BV-associated species, simultaneous colonization of vaginal lactobacilli in large numbers (105–106 colony forming units (CFU)/mL) was demonstrated. Moreover, as shown in vitro, strong H2O2 producers were identified in BV cases as well [75,76]. However, due to the more significant number of lactobacilli observed in healthy women, it might be the case that overall higher amounts of vaginal H2O2 would be generated in them than in women with bacterial vaginosis [76,77].
4.2. Antimicrobial Effects of H2O2: Epidemiological Studies on Vulvovaginal Candidiasis (VVC)
One of the most frequent vaginal disorders is vulvovaginal candidiasis, caused by several species of the yeast Candida, predominantly by C. albicans. Candidal vulvovaginitis occurs when Candida species members of vaginal microbiota superficially penetrate the mucosal lining of the vagina leading to a secondary inflammatory response [78]. An association between Candida overgrowth and levels of lactobacilli overall, neither a deficiency nor colonization with unusual Lactobacillus species could be observed [79]. Most women with candidiasis had the highest lactobacilli counts; even previous antibiotic treatment did not affect lactobacilli density [80]. Similar results were shown later: hydrogen peroxide-producing Lactobacillus species were almost equally isolated in women with normal microbiota and women with VVC [80]. Furthermore, a longitudinal study showed no correlation between initial H2O2−/H2O2+ Lactobacillus colonization with the development of symptomatic candidiasis. The demonstration of the protective role of H2O2-positive lactobacilli against the acquisition of VVC failed and therefore a possible correlation was questioned [37]. Vaginal Candida propagation may be facilitated by fungal intrinsic and/or local extrinsic factors more powerful than Lactobacillus-related defense.
4.3. Antimicrobial Effects of H2O2: Epidemiological Studies on STI Pathogens
Hydrogen peroxide produced by lactobacilli in the vagina may not only maintain their dominance and control the physiological composition of the vaginal microbiota, but they may protect against colonization of pathogens. Preventing sexually transmitted diseases and ascending infection of the chorioamniotic membranes and uterine cavity in pregnant women is of great medical importance. Compared to in vitro studies, there are just a few investigations dealing with epidemiologic correlation between H2O2-producing lactobacilli and vaginal infection [37,70,80,81,82]. Most of these epidemiological studies are complex, analyzing normal microbiota, bacterial vaginosis, and the most frequent infections simultaneously.
Infections by the protozoon Trichomonas vaginalis belong to the group of sexually transmitted diseases, with having a new sex partner as the most important risk factor. Since T. vaginalis is able to the phagocytosis and indirect killing of vaginal lactobacilli with its toxic metabolic products, abnormal vaginal flora and/or reduction of lactobacilli are thought to be additional risk factors for the infection [80,83,84]. Most epidemiological studies investigating the possible role of H2O2-producing Lactobacillus species in normal vaginal flora, bacterial vaginosis and VVC failed to show any correlation of the bacteria with trichomoniasis [37,70,80].
In the case of the STI caused by Neisseria gonorrhoeae, Lactobacillus-dominant vaginal microbial community was shown to protect individuals from lower genital tract infection with N. gonorrhoeae [85]. Furthermore, women colonized by H2O2-generating Lactobacillus species were less frequently infected by gonococci than women lacking H2O2+ lactobacilli [70].
The association between HIV infections and vaginal colonization by H2O2-forming lactobacilli was investigated in HIV seronegative and seropositive women. Compared with African female sexual workers carrying H2O2+ Lactobacillus, women without lactobacilli had a 2.5-fold higher risk of HIV-1 infection. Women with only H2O2-negative strains were at intermediate risk. The abundance of H2O2-generating lactobacilli in HIV-positive women was significantly reduced than in HIV-negative women [81]. Analyzing the occurrence of different hydrogen peroxide-producing Lactobacillus species in HIV seropositive women, it was demonstrated that H2O2-producing L. gasseri is more prevalent in the population of HIV-1 infected women [82]. Moreover, it was the predominant species detected among women who had high quantities of H2O2-producing Lactobacillus but were negative for both L. crispatus and L. jensenii, suggesting an alteration of Lactobacillus species in the vaginal flora of HIV-positive women [82].
4.4. Antimicrobial Effects of H2O2: Experimental Studies
Alongside the population-based studies, the hypothesized direct antimicrobial role of vaginal lactobacilli-derived hydrogen peroxide was investigated in a series of experiments. In these microbiological in vitro studies, the H2O2-mediated killing/inhibition of target pathogens was observed by co-culturing them either with different types of lactobacilli or with its supernatants or with cervicovaginal fluid.
The most convincing epidemiological correlation was demonstrated in women with bacterial vaginosis, where vaginal colonization by H2O2-producing Lactobacillus strains was reduced. The key bacterium of BV is thought to be Gardnerella vaginalis, with its overgrowth potential beside certain other anaerobes. Initial findings of in vivo studies assumed the control of H2O2-forming Lactobacillus species over other members of the vaginal microbiota, especially over G. vaginalis with the, at least partially, direct bactericidal effect of H2O2.
In a liquid co-culture assay with lactobacilli and BV-associated organisms, G. vaginalis and P. bivia at pH 5 resembling vaginal acidic conditions, killing of the pathogens could be observed only when H2O2-producing lactobacilli were added to the system, H2O2-negative lactobacilli showed no effect [14]. The H2O2-dependent antibacterial mechanism was demonstrated by adding catalase to the assay, which abandoned the reduction of G. vaginalis and P. bivia. Moreover, toxic effects on G. vaginalis could be augmented by adding peroxidase and a halide to the co-culture [14]. However, the study has some limitations in its interpretation in vivo. First, as shown in studies later, reduced pH alone can inhibit the growth of several vaginal microbiota members, including G. vaginalis [86]. Therefore, bacterial depletion should have also occurred in the test system with H2O2-nonproducer lactobacilli. Furthermore, experiments were carried out under fully aerobic conditions, which is questionable in the vaginal mucosa. At toxic concentrations of H2O2 complemented with peroxidase and a halide in the experiments, there was a fall in the viable cell count of the H2O2-producing lactobacilli, suggesting autoinhibitory effects. Since lactobacilli dominate the vaginal microbiota, this suggests more reduced H2O2 concentrations in vivo and a rather subordinate role of oxidative stress caused by H2O2 in controlling the growth of BV-associated bacteria.
Another study of the same year with co-culture test systems, although on solid agar media, supported these concerns regarding in vitro experiments [86]. 5 of 20 H2O2-positive lactobacilli isolated from healthy women or women with bacterial vaginosis exerted some inhibitory effects against a few Mobiluncus and Peptostreptococcus strains. In contrast, others failed to reduce the growth of Gardnerella vaginalis, Bacteroides spp. and other strains of Mobiluncus and Peptostreptococcus. Similar results were observed with H2O2-negative lactobacilli. The observed antimicrobial effect was hardly influenced by the pH of the medium, suggesting rather pH-dependent growth inhibition. A growth inhibitory activity of H2O2 alone at different concentrations (0.0003–0.3%) was not observed either. It should be noted that these experiments were carried out under anaerobic conditions, and concentrations of target bacteria were chosen arbitrarily and, therefore, probably too high for inhibition detection (106 CFU/mL) [63].
A more complex study provided detailed data about the circumstances of H2O2 production and H2O2-mediated toxicity by vaginal lactobacilli [87]. In these experiments, the inhibitory effects of 22 isolated H2O2-producing vaginal lactobacilli were determined on different G. vaginalis strains. Agar well diffusion assay measured the cell growth reduction induced by Lactobacillus culture filtrates. The influence of several culture parameters (pH, H2O2 presence, anaerobic/aerobic conditions) was tested independently. A low pH of around four and lactic acid accounted for 60 to 95% Lactobacillus-derived inhibitory activity, and H2O2 accounted for only 0 to 30% after its denaturation with catalase treatment. H2O2 production was not detectable under anaerobic or static aerobic conditions. This study also confirmed the enhancement of killing with additional peroxidase and halide under aerobic conditions. These findings suggest that lactic acid and a low pH are more critical for G. vaginalis growth inhibition than H2O2 in vitro [87].
Comparison of the antimicrobial effect of pure H2O2 and culture supernatants of H2O2-producing vaginal lactobacilli against BV-associated microorganisms demonstrated significant H2O2 sensitivity of Gardnerella and Prevotella, however, experiment conditions are unlikely to occur in vivo [39]. Catalase treatment neutralized growth inhibition of pure H2O2 but did not affect the toxicity of culture supernatants proposing other toxic mechanisms than H2O2. Cultured media of Lactobacillus species with moderate or low H2O2 production appeared to be less effective or ineffective on the growth of G. vaginalis, indicating dose-dependent toxicity and varying levels of H2O2 and at least in vitro [38].
In the case of candidiasis, as seen in the epidemiological studies, the protective role of lactobacilli-derived hydrogen peroxide is rather doubtful since different Candida species were found to be resistant to relatively high concentrations of H2O2 [40]. 30 g/L H2O2 was necessary to kill all Candida yeast cells, and 3 g/L was inhibitory for only some Candida cells [40]. No Lactobacillus strain was found to produce H2O2 in this high concentration. Moreover, this concentration of H2O2 would also act as an autoinhibitory [40]. In contrast to these results, using Lactobacillus culture supernatants, in which H2O2 reached concentrations from 0.05 to 1.0 mM, they effectively could inhibit Candida growth. Still, it could not be neutralized with catalase, suggesting other toxic mechanisms [39]. Furthermore, Candida species can produce their catalase for H2O2 degradation, which, in turn, could be further stimulated by Lactobacillus-derived H2O2 [39]. In another study of the same year, the minimal bactericidal concentration of H2O2 on a single C. albicans strain was 2.52 mmol/L; Candida albicans appeared to be approximately six times more tolerant than G. vaginalis to H2O2-mediated inhibition [38]. Supernatants of vaginal H2O2-producing lactobacilli, treated with proteinase K to neutralize antimicrobial peptides but with maintained H2O2 activity, showed insufficient eradication of C. albicans [38].
Liquid co-culture experiments demonstrated pH-dependent growth inhibitory effects of vaginal lactobacilli on the pathogen Neisseria gonorrhoeae with the enhancement of toxicity under acidic conditions [88]. Gonococcal growth was significantly more inhibited by H2O2-producing lactobacilli. Moreover, H2O2-positive lactobacilli could increase catalase production by N. gonorrhoeae at least at neutral pH, and catalase activity parallel decreased with pH, probably due to the bactericide effect of low pH on gonococci [88]. Co-culture experiments obtained similar results based on the sandwich method with agar plates investigating the inhibitory effect of four isolated Lactobacillus strains (L. crispatus, L. jensenii, L. gasseri, L. acidophilus) on two Gonococcal laboratory strains [42]. All four Lactobacillus strains inhibited the growth of all Gonococcal strains tested at low pH. Since adding catalase could effectively neutralize Lactobacillus-mediated Gonococcal killing, H2O2 was suggested as the primary mediator of inhibition [42].
In one study, supernatants of H2O2-producing Lactobacillus species were shown to inactivate elementary bodies of Chlamydia trachomatis mainly through a lactate acid-dependent mechanism since catalase-treatment could not reverse the inhibition by neutralizing H2O2 [43]. It was hypothesized that the rigid outer membrane of Chlamydia could prevent H2O2 from entering the cell [43].
The antiviral potential of H2O2 was studied for Herpes Simplex Virus Type 2 (HSV-2) and Human Immunodeficiency Virus Type 1 (HIV-1) [89,90]. Inhibition of HSV-2 multiplication by lactobacilli was demonstrated on HSV-2-infected Vero cells incubated with bacteria. However, culture supernatants of H2O2-forming lactobacilli could neither modify the infectivity of HSV-2 virions nor affect intracellular events of virus multiplication. Investigation of the effects of pure H2O2 in cell culture experiments was hindered by the fact that H2O2 was metabolized promptly in the cell culture, and maintaining constant levels of H2O2 was not possible. Incubating HSV-2 virions with H2O2, hydrogen peroxide showed a dose-dependent reduction of the infection capacity with a 50% inhibition at 184 μM after one h incubation. Still, that high activity level in the vagina is rather unlikely [43,44,89]. In a simple, early study on HIV-1, H2O2-producing L. acidophilus at a concentration of 107 CFU/mL was viricidal to HIV-1 virions in lactate buffer with pH 5.0 [90]. The role of H2O2 was demonstrated with the addition of myeloperoxidase and chloride to lower concentrations of the Lactobacillus with ineffective viricidal activity alone, showing enhancement of viral reduction in the in vitro test system [90].
The correlation of these studies with physiological conditions in the vaginal mucosa is challenging to estimate since in vitro studies contain several limiting factors for their proper interpretation. Most of the studies worked with isolated Lactobacillus strains and not with bacterial communities; concentrations of lactobacilli and target bacteria varied in the experiments, as was the case of O2 tension and sometimes pH values during incubation periods. Using pure H2O2 in inhibitory experiments, it should always be remembered that lactobacilli are H2O2-sensitive as well. Furthermore, cervical mucosa may harbor additional molecules able to react with and inactivate hydrogen peroxide. Using cervicovaginal fluid (CVF) from healthy women as the natural source of lactobacilli-derived compounds in in vitro experiments could eliminate some significant issues regarding microbiological tests [91,92]. Under hypoxic conditions, CVF lost its H2O2 content within one hour, significantly suggesting inactivating mechanism present in CVF [91]. The mean hydrogen peroxide content in CVF samples after aeration was only 23 ± 5 μM, one hundred times lower than maximal aerobic in vitro production (~2 mM). But even 50 μM hydrogen peroxide could not contain inactive pathogens like HSV-2, N. gonorrhoeae, H. ducreyii and several BV-associated bacteria. Additionally, adding 1% CVF reversed the in vitro inactivation of G. vaginalis and P. bivia by H2O2-producing L. crispatus, suggesting vigorous H2O2-blocking activity of CVF and questioning the dominant role of hydrogen peroxide in the maintenance of healthy vaginal microenvironment [91]. In contrast, a strong inhibitory effect was observed with physiological concentrations of lactic acid (56 mM) at pH 4.5 [92]. Although the advantage of examining CVF by the interpretation of the results, limitations of the experiments still exist. Localization, distribution, and stability of H2O2 in the vaginal mucosa and bacterial interactions in proximity in the tissue are still unknown characteristics of H2O2-producing lactobacilli in the vaginal microbiota.
4.5. Impact of H2O2-Producing Lactobacilli on Fertility and Pregnancy Outcome
In healthy pregnancy, the abundance of vaginal H2O2-producing lactobacilli was lower than that in nonpregnant females [93]. The proportion of H2O2+ strains decreased with the gravidae’s age and increased with pregnancy trimesters [93].
Several studies demonstrated the association of vaginal dysbiosis with the negative outcome of fertility treatments suggesting altered vaginal microbiota and bacterial vaginosis as independent risk factors with a predictive value [94,95,96,97,98]. Moreover, investigating 135 vaginal Lactobacillus strains belonging to the species L. crispatus, L. jensenii and L. gasseri, lactobacilli strains from healthy women generated significantly higher amounts of H2O2 than strains of infertile women [99]. Colonization with Lactobacillus species that produce hydrogen peroxide (H2O2) and bacterial vaginosis have been associated with lower rates of preterm birth as well, suggesting the protective role of these strains against ascending infections [100]. Furthermore, the presence of H2O2-producing species (L. jensenii and/or L. vaginalis) during pregnancy was associated with significantly reduced rates of preterm birth and/or chorioamnionitis [101].
5. H2O2-Producing Lactobacilli as Therapeutic Agents in Vaginal Probiotics
Considering the Lactobacillus dominance of the healthy vaginal microflora, efforts to modulate the pathological composition of vaginal microbiota with probiotics have been made in the last decades in varying studies [2,64]. Most of these trials focused on treating the most common bacterial vaginosis with its dysbiotic character, and a few studies focused on vulvovaginal candidiasis [102,103]. Probiotic treatment can be either primary, in combination, or following antibiotic therapy, or probiotics can be administered orally or vaginally.
Interestingly, the effects of vaginal douching with 3% H2O2 alone for treating BV have been investigated in two studies with contradictory findings [104]. In recurrent cases of bacterial vaginosis, daily vaginal irrigations with 30 mL of 3% hydrogen peroxide for seven days could eliminate the main symptoms of BV three months after treatment. This result was comparable to that achieved with local antibiotic therapy. Moreover, H2O2 was found to facilitate the restoration of normal vaginal bacterial flora and normal acid pH in 98% of cases and led to the disappearance of clue cells from vaginal smears [104]. In a randomized controlled trial, 3% H2O2 single vaginal douching was significantly less effective than a single oral dose of metronidazole (62.5% versus 78.6%) in treating bacterial vaginosis [105].
In studies aiming to characterize and select vaginal Lactobacillus species with probiotic potential, one of the primary criteria (e.g., lactic acid formation, epithelial adhesion, inhibitory activity against BV-associated bacterial species) is the H2O2-producing capacity of lactobacilli tested in vitro. Certain strains of several Lactobacillus species (L. crispatus, L. acidophilus, L. jenseni, L. gasseri, L. brevis, L. salivarius) were considered probiotic candidates based partly on strong H2O2 generation [99,106,107,108,109].
Local administration of an H2O2-producing probiotic strain of L. crispatus in healthy, sexually active women could establish Lactobacillus colonization in women lacking lactobacilli [110]. Furthermore, the introduction of exogenous L. crispatus increased vaginal colonization by other H2O2-producing lactobacilli in female participants. Failure of colonization with the probiotic strain was associated with sexual intercourse [110].
One of the first studies using probiotic strains (H2O2-producing L. acidophilus) in vaginal capsules (for the treatment of BV could not demonstrate any efficacy for the treatment of BV probably because of losing a significant proportion of patients during the trial [111,112]. In a multicentric, randomized, placebo-controlled clinical trial, locally administered estradiol-combined H2O2-producing L. acidophilus achieved significantly higher cure rate in non-menopausal women with BV [112]. Further trials showed varying results [113,114].
Combination therapies with different, mostly H2O2 Lactobacillus species revealed controversial results as well [115,116,117].
Interestingly, the high efficiency of oral probiotic therapy of bacterial vaginosis was demonstrated in clinical trials using well-characterized intestinal Lactobacillus strains: L. rhamnosus GR-1 and L. reuteri RC-14 either alone or in combination with antibiotic treatment. Vaginal Lactobacillus recovery suggests the ability of Lactobacillus GR-1 and RC-14 to colonize the vagina after oral intake [108,118,119,120]. Vaginal administration of these intestinal probiotic strains combined with antibiotic treatment demonstrated high efficiency in curing vaginal BV and stabilizing the vaginal ecosystem in a few studies [121,122,123,124,125]. Additionally, oral probiotic L. reuteri RC-14 and L. rhamnosus GR-1 strains increased the relative abundance of indigenous vaginal lactobacilli, like H2O2-producing L. crispatus [126].
Some trials have also investigated the efficiency of combination therapy of vulvovaginal candidiasis with antifungals and probiotics compared to antifungals alone, but no information was available about the H2O2 production of the administered probiotic strains in the studies [108,127,128,129,130,131,132].
Despite the strong negative association between vaginal dysbiosis and IVF outcome, probiotic therapy (L. acidophilus and bifidobacterial; H2O2 production not known) of infertile women was carried out only in two studies reporting treatment failure [133,134,135].
6. Conclusions
Several species of the genus Lactobacillus constitute a significant component of the human microbiota at various body sites, like the oral, intestinal, and vaginal flora. However, the abundance of hydrogen peroxide-producing lactobacilli is unique for the vaginal microbial community suggesting the importance of Lactobacillus-derived exogenous H2O2 in the vaginal microenvironment. Most epidemiological studies could support this theory and reveal the protective role of H2O2 against dysbiosis and pathogen colonization. In vitro studies contradicted these findings and demonstrated other possible effects of H2O2. Since these microbiological experiments were conducted under artificial circumstances with several arbitrary settings, it became apparent that interpreting the results referring to in vivo conditions is complicated and nearly impossible. Although in studies, aiming at the selection of vaginal Lactobacillus species with probiotic potential, selection criteria included the ability of the strain to produce H2O2, this was often not in the focus of the clinical trials with probiotic lactobacilli and the administration of many different Lactobacillus species and strains made challenging to draw valuable conclusions. However, going through all the studies with many aspects and designs, Lactobacillus-derived H2O2 still seems important in vaginal health. H2O2 production may play an antimicrobial role in the vaginal microenvironment, probably limited to local cell-cell interactions in close proximity, embedded in a biofilm that is not reproducible in vitro. Furthermore, H2O2-producing lactobacilli may possess a favorable, more efficient phenotype than their non-producer counterparts contributing significantly to a healthy vaginal ecosystem. Since altered vaginal microbiota is strongly associated with disorders of infective character (BV, VVC, STIs) and certain pregnancy-related complications (infertility, pre-term birth), further investigations are needed to explore the possible background and to improve probiotic treatment.
Acknowledgments
This work was supported by the National Laboratory on Human Reproduction as part of the “Establishment of National Laboratories 2020” program (RRF-2.3.1-21-2022-00012).
Author Contributions
E.M.: conceptualization and writing; A.B.: review; figures and table. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the University of Pecs Medical School Research Grant (PTE-ÁOK KA 2021-38, KA 2021-20, KA-2019-37, KA-2018-07, KA-2018-18).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Ravel J., Gajer P., Abdo Z., Schneider G.M., Koenig S.S.K., McCulle S.L., Karlebach S., Gorle R., Russell J., Tacket C.O., et al. Vaginal Microbiome of Reproductive-Age Women. Proc. Natl. Acad. Sci. USA. 2011;108:4680–4687. doi: 10.1073/pnas.1002611107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.France M., Alizadeh M., Brown S., Ma B., Ravel J. Towards a Deeper Understanding of the Vaginal Microbiota. Nat. Microbiol. 2022;7:367–378. doi: 10.1038/s41564-022-01083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma B., Forney L.J., Ravel J. Vaginal Microbiome: Rethinking Health and Disease. Annu. Rev. Microbiol. 2012;66:371–389. doi: 10.1146/annurev-micro-092611-150157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Antonio M.A., Hawes S.E., Hillier S.L. The Identification of Vaginal Lactobacillus Species and the Demographic and Microbiologic Characteristics of Women Colonized by These Species. J. Infect. Dis. 1999;180:1950–1956. doi: 10.1086/315109. [DOI] [PubMed] [Google Scholar]
- 5.Zhou X., Bent S.J., Schneider M.G., Davis C.C., Islam M.R., Forney L.J. Characterization of Vaginal Microbial Communities in Adult Healthy Women Using Cultivation-Independent Methods. Microbiology. 2004;150:2565–2573. doi: 10.1099/mic.0.26905-0. [DOI] [PubMed] [Google Scholar]
- 6.Galask R.P., Larsen B., Ohm M.J. Vaginal Flora and Its Role in Disease Entities. Clin. Obstet. Gynecol. 1976;19:61–81. doi: 10.1097/00003081-197603000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Gajer P., Brotman R.M., Bai G., Sakamoto J., Schütte U.M.E., Zhong X., Koenig S.S.K., Fu L., Ma Z., Zhou X., et al. Temporal Dynamics of the Human Vaginal Microbiota. Sci. Transl. Med. 2012;4:132ra52. doi: 10.1126/scitranslmed.3003605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freitas A.C., Chaban B., Bocking A., Rocco M., Yang S., Hill J.E., Money D.M., Hemmingsen S., Reid G., Dumonceaux T., et al. The Vaginal Microbiome of Pregnant Women Is Less Rich and Diverse, with Lower Prevalence of Mollicutes, Compared to Non-Pregnant Women. Sci. Rep. 2017;7:9212. doi: 10.1038/s41598-017-07790-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta P., Singh M.P., Goyal K. Diversity of Vaginal Microbiome in Pregnancy: Deciphering the Obscurity. Front. Public Health. 2020;8:326. doi: 10.3389/fpubh.2020.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aagaard K., Riehle K., Ma J., Segata N., Mistretta T.A., Coarfa C., Raza S., Rosenbaum S., van den Veyver I., Milosavljevic A., et al. A Metagenomic Approach to Characterization of the Vaginal Microbiome Signature in Pregnancy. PLoS ONE. 2012;7:e36466. doi: 10.1371/journal.pone.0036466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Romero R., Hassan S.S., Gajer P., Tarca A.L., Fadrosh D.W., Nikita L., Galuppi M., Lamont R.F., Chaemsaithong P., Miranda J., et al. The Composition and Stability of the Vaginal Microbiota of Normal Pregnant Women Is Different from That of Non-Pregnant Women. Microbiome. 2014;2:4. doi: 10.1186/2049-2618-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jakobsson T., Forsum U. Lactobacillus Iners: A Marker of Changes in the Vaginal Flora? J. Clin. Microbiol. 2007;45:3145. doi: 10.1128/JCM.00558-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verstraelen H., Verhelst R., Claeys G., de Backer E., Temmerman M., Vaneechoutte M. Longitudinal Analysis of the Vaginal Microflora in Pregnancy Suggests That L. Crispatus Promotes the Stability of the Normal Vaginal Microflora and That L. Gasseri and/or L. Iners Are More Conducive to the Occurrence of Abnormal Vaginal Microflora. BMC Microbiol. 2009;9:116. doi: 10.1186/1471-2180-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klebanoff S.J., Hillier S.L., Eschenbach D.A., Waltersdorph M. Control of the Microbial Flora of the Vagina by H202-Generating Lactobacilli. J. Infect. Dis. 1991;164:94–100. doi: 10.1093/infdis/164.1.94. [DOI] [PubMed] [Google Scholar]
- 15.Eschenbach D.A., Davick P.R., Williams B.L., Klebanoff S.J., Young-Smith K., Critchlow C.M., Holmes K.K. Prevalence of Hydrogen Peroxide-Producing Lactobacillus Species in Normal Women and Women with Bacterial Vaginosis. J. Clin. Microbiol. 1989;27:251–256. doi: 10.1128/jcm.27.2.251-256.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andrés C.M.C., Pérez de la Lastra J.M., Juan C.A., Plou F.J., Pérez-Lebeña E. Chemistry of Hydrogen Peroxide Formation and Elimination in Mammalian Cells, and Its Role in Various Pathologies. Stresses. 2022;2:256–274. doi: 10.3390/stresses2030019. [DOI] [Google Scholar]
- 17.Halliwell B., Clement M.V., Long L.H. Hydrogen Peroxide in the Human Body. FEBS Lett. 2000;486:10–13. doi: 10.1016/S0014-5793(00)02197-9. [DOI] [PubMed] [Google Scholar]
- 18.Castagna R., Eiserich J.P., Budamagunta M.S., Stipa P., Cross C.E., Proietti E., Voss J.C., Greci L. Hydroxyl Radical from the Reaction between Hypochlorite and Hydrogen Peroxide. Atmos. Environ. 2008;42:6551–6554. doi: 10.1016/j.atmosenv.2008.04.029. [DOI] [Google Scholar]
- 19.Mahaseth T., Kuzminov A. Potentiation of Hydrogen Peroxide Toxicity: From Catalase Inhibition to Stable DNA-Iron Complexes. Mutat. Res. Rev. Mutat. Res. 2017;773:274–281. doi: 10.1016/j.mrrev.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halliwell B., Gutteridge J.M.C. The Antioxidants of Human Extracellular Fluids. Arch. Biochem. Biophys. 1990;280:1–8. doi: 10.1016/0003-9861(90)90510-6. [DOI] [PubMed] [Google Scholar]
- 21.Halliwell B., Gutteridge J.M.C. Role of Free Radicals and Catalytic Metal Ions in Human Disease: An Overview. Methods Enzymol. 1990;186:1–85. doi: 10.1016/0076-6879(90)86093-B. [DOI] [PubMed] [Google Scholar]
- 22.Klebanoff S.J. Myeloperoxidase: Friend and Foe. J. Leukoc. Biol. 2005;77:598–625. doi: 10.1189/jlb.1204697. [DOI] [PubMed] [Google Scholar]
- 23.Wang X., Martindale J.L., Liu Y., Holbrook N.J. The Cellular Response to Oxidative Stress: Influences of Mitogen-Activated Protein Kinase Signalling Pathways on Cell Survival. Pt 2Biochem. J. 1998;333:291–300. doi: 10.1042/bj3330291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Griendling K.K., Harrison D.G. Dual Role of Reactive Oxygen Species in Vascular Growth. Circ. Res. 1999;85:562–563. doi: 10.1161/01.RES.85.6.562. [DOI] [PubMed] [Google Scholar]
- 25.Abe J.I., Berk B.C. Fyn and JAK2 Mediate Ras Activation by Reactive Oxygen Species. J. Biol. Chem. 1999;274:21003–21010. doi: 10.1074/jbc.274.30.21003. [DOI] [PubMed] [Google Scholar]
- 26.Dalton T.P., Shertzer H.G., Puga A. Regulation of Gene Expression by Reactive Oxygen. Annu. Rev. Pharmacol. Toxicol. 1999;39:67–101. doi: 10.1146/annurev.pharmtox.39.1.67. [DOI] [PubMed] [Google Scholar]
- 27.Sies H. Hydrogen Peroxide as a Central Redox Signaling Molecule in Physiological Oxidative Stress: Oxidative Eustress. Redox Biol. 2017;11:613–619. doi: 10.1016/j.redox.2016.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D’Autréaux B., Toledano M.B. ROS as Signalling Molecules: Mechanisms That Generate Specificity in ROS Homeostasis. Nat. Rev. Mol. Cell Biol. 2007;8:813–824. doi: 10.1038/nrm2256. [DOI] [PubMed] [Google Scholar]
- 29.Burdon R.H., Gill V., Alliangana D. Hydrogen Peroxide in Relation to Proliferation and Apoptosis in BHK-21 Hamster Fibroblasts. Free Radic. Res. 1996;24:81–93. doi: 10.3109/10715769609088004. [DOI] [PubMed] [Google Scholar]
- 30.Poli G., Parola M. Oxidative Damage and Fibrogenesis. Free Radic. Biol. Med. 1997;22:287–305. doi: 10.1016/S0891-5849(96)00327-9. [DOI] [PubMed] [Google Scholar]
- 31.Schreck R., Rieber P., Baeuerle P.A. Reactive Oxygen Intermediates as Apparently Widely Used Messengers in the Activation of the NF-Kappa B Transcription Factor and HIV-1. EMBO J. 1991;10:2247–2258. doi: 10.1002/j.1460-2075.1991.tb07761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hertzberger R., Arents J., Dekker H.L., Pridmore R.D., Gysler C., Kleerebezem M., de Mattos M.J.T. H(2)O(2) Production in Species of the Lactobacillus Acidophilus Group: A Central Role for a Novel NADH-Dependent Flavin Reductase. Appl. Environ. Microbiol. 2014;80:2229–2239. doi: 10.1128/AEM.04272-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Condon S. Responses of Lactic Acid Bacteria to Oxygen. FEMS Microbiol. Lett. 1987;46:269–280. doi: 10.1111/j.1574-6968.1987.tb02465.x. [DOI] [Google Scholar]
- 34.Kawasaki S., Satoh T., Todoroki M., Niimura Y. B-Type Dihydroorotate Dehydrogenase Is Purified as a H2O2-Forming NADH Oxidase from Bifidobacterium Bifidum. Appl. Environ. Microbiol. 2009;75:629–636. doi: 10.1128/AEM.02111-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marty-Teysset C., de la Torre F., Garel J. Increased Production of Hydrogen Peroxide by Lactobacillus Delbrueckii Subsp. Bulgaricus upon Aeration: Involvement of an NADH Oxidase in Oxidative Stress. Appl. Environ. Microbiol. 2000;66:262–267. doi: 10.1128/AEM.66.1.262-267.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martín R., Soberón N., Vaneechoutte M., Flórez A.B., Vázquez F., Suárez J.E. Characterization of Indigenous Vaginal Lactobacilli from Healthy Women as Probiotic Candidates. Int. Microbiol. 2008;11:261–266. doi: 10.2436/20.1501.01.70. [DOI] [PubMed] [Google Scholar]
- 37.Hillier S.L., Krohn M.E., Klebanoff S.J., Eschenbach D.A. The Relationship of Hydrogen Peroxide-Producing Lactobacilli to Bacterial Vaginosis and Genital Microflora in Pregnant Women. Obstet. Gynecol. 1992;79:369–373. doi: 10.1097/00006250-199203000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Kaewsrichan J., Peeyananjarassri K., Kongprasertkit J. Selection and Identification of Anaerobic Lactobacilli Producing Inhibitory Compounds against Vaginal Pathogens. FEMS Immunol. Med. Microbiol. 2006;48:75–83. doi: 10.1111/j.1574-695X.2006.00124.x. [DOI] [PubMed] [Google Scholar]
- 39.Strus M., Brzychczy-Włoch M., Gosiewski T., Kochan P., Heczko P.B. The in Vitro Effect of Hydrogen Peroxide on Vaginal Microbial Communities. FEMS Immunol. Med. Microbiol. 2006;48:56–63. doi: 10.1111/j.1574-695X.2006.00120.x. [DOI] [PubMed] [Google Scholar]
- 40.Strus M., Kucharska A., Kukla G., Brzychczy-Włoch M., Maresz K., Heczko P.B. The in Vitro Activity of Vaginal Lactobacillus with Probiotic Properties against Candida. Infect. Dis. Obstet. Gynecol. 2005;13:69–75. doi: 10.1080/10647440400028136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rashad A.L., Toffler W.L., Wolf N., Thornburg K., Kirk E.P., Ellis G., Whitehead W.E. Vaginal PO2 in Healthy Women and in Women Infected with Trichomonas Vaginalis: Potential Implications for Metronidazole Therapy. Am. J. Obstet. Gynecol. 1992;166:620–624. doi: 10.1016/0002-9378(92)91687-6. [DOI] [PubMed] [Google Scholar]
- 42.St Amant D.C., Valentin-Bon I.E., Jerse A.E. Inhibition of Neisseria Gonorrhoeae by Lactobacillus Species That Are Commonly Isolated from the Female Genital Tract. Infect. Immun. 2002;70:7169–7171. doi: 10.1128/IAI.70.12.7169-7171.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gong Z., Luna Y., Yu P., Fan H. Lactobacilli Inactivate Chlamydia Trachomatis through Lactic Acid but Not H2O2. PLoS ONE. 2014;9:e107758. doi: 10.1371/journal.pone.0107758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O’Hanlon D.E., Moench T.R., Cone R.A. Vaginal PH and Microbicidal Lactic Acid When Lactobacilli Dominate the Microbiota. PLoS ONE. 2013;8:e80074. doi: 10.1371/journal.pone.0080074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cadieux P.A., Burton J.P., Devillard E., Reid G. Lactobacillus By-Products Inhibit the Growth and Virulence of Uropathogenic Escherichia coli. J. Physiol. Pharmacol. 2009;60((Suppl. S6)):13–18. [PubMed] [Google Scholar]
- 46.Atassi F., Servin A.L. Individual and Co-Operative Roles of Lactic Acid and Hydrogen Peroxide in the Killing Activity of Enteric Strain Lactobacillus Johnsonii NCC933 and Vaginal Strain Lactobacillus Gasseri KS120.1 against Enteric, Uropathogenic and Vaginosis-Associated Pathogens. FEMS Microbiol. Lett. 2010;304:29–38. doi: 10.1111/j.1574-6968.2009.01887.x. [DOI] [PubMed] [Google Scholar]
- 47.Hickey D.K., Patel M.V., Fahey J.V., Wira C.R. Innate and Adaptive Immunity at Mucosal Surfaces of the Female Reproductive Tract: Stratification and Integration of Immune Protection against the Transmission of Sexually Transmitted Infections. J. Reprod. Immunol. 2011;88:185–194. doi: 10.1016/j.jri.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reis Machado J., da Silva M.V., Cavellani C.L., Antônia Dos Reis M., Monteiro M.L.G.D.R., Teixeira V.D.P.A., Rosa Miranda Corrêa R. Mucosal Immunity in the Female Genital Tract, HIV/AIDS. Biomed. Res. Int. 2014;2014:350195. doi: 10.1155/2014/350195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adapen C., Réot L., Menu E. Role of the Human Vaginal Microbiota in the Regulation of Inflammation and Sexually Transmitted Infection Acquisition: Contribution of the Non-Human Primate Model to a Better Understanding? Front. Reprod. Health. 2022;4:992176. doi: 10.3389/frph.2022.992176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Strbo N., Alcaide M.L., Romero L., Bolivar H., Jones D., Podack E.R., Fischl M.A. Loss of Intra-Epithelial Endocervical Gamma Delta (GD) 1 T Cells in HIV-Infected Women. Am. J. Reprod. Immunol. 2016;75:134–145. doi: 10.1111/aji.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gibbs A., Leeansyah E., Introini A., Paquin-Proulx D., Hasselrot K., Andersson E., Broliden K., Sandberg J.K., Tjernlund A. MAIT Cells Reside in the Female Genital Mucosa and Are Biased towards IL-17 and IL-22 Production in Response to Bacterial Stimulation. Mucosal Immunol. 2017;10:35–45. doi: 10.1038/mi.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Benjelloun F., Quillay H., Cannou C., Marlin R., Madec Y., Fernandez H., Chrétien F., le Grand R., Barré-Sinoussi F., Nugeyre M.T., et al. Activation of Toll-Like Receptors Differentially Modulates Inflammation in the Human Reproductive Tract: Preliminary Findings. Front. Immunol. 2020;11:1655. doi: 10.3389/fimmu.2020.01655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Trifonova R.T., Lieberman J., van Baarle D. Distribution of Immune Cells in the Human Cervix and Implications for HIV Transmission. Am. J. Reprod. Immunol. 2014;71:252–264. doi: 10.1111/aji.12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sullivan D.A., Richardson G.S., MacLaughlin D.T., Wira C.R. Variations in the Levels of Secretory Component in Human Uterine Fluid during the Menstrual Cycle. J. Steroid Biochem. 1984;20:509–513. doi: 10.1016/0022-4731(84)90263-2. [DOI] [PubMed] [Google Scholar]
- 55.Wira C.R., Rodriguez-Garcia M., Patel M.V. The Role of Sex Hormones in Immune Protection of the Female Reproductive Tract. Nat. Rev. Immunol. 2015;15:217–230. doi: 10.1038/nri3819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mitchell C., Fredricks D., Agnew K., Hitti J. Hydrogen Peroxide-Producing Lactobacilli Are Associated with Lower Levels of Vaginal Interleukin-1β, Independent of Bacterial Vaginosis. Sex. Transm. Dis. 2015;42:358–363. doi: 10.1097/OLQ.0000000000000298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Erttmann S.F., Gekara N.O. Hydrogen Peroxide Release by Bacteria Suppresses Inflammasome-Dependent Innate Immunity. Nat. Commun. 2019;10:3493. doi: 10.1038/s41467-019-11169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Veal E.A., Day A.M., Morgan B.A. Hydrogen Peroxide Sensing and Signaling. Mol. Cell. 2007;26:1–14. doi: 10.1016/j.molcel.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 59.Choi S.E., Min S.H., Shin H.C., Kim H.E., Jung M.W., Kang Y. Involvement of Calcium-Mediated Apoptotic Signals in H2O2-Induced MIN6N8a Cell Death. Eur. J. Pharmacol. 2006;547:1–9. doi: 10.1016/j.ejphar.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 60.Chen Q., Espey M.G., Krishna M.C., Mitchell J.B., Corpe C.P., Buettner G.R., Shaded E., Levine M. Pharmacologic Ascorbic Acid Concentrations Selectively Kill Cancer Cells: Action as a pro-Drug to Deliver Hydrogen Peroxide to Tissues. Proc. Natl. Acad. Sci. USA. 2005;102:13604–13609. doi: 10.1073/pnas.0506390102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sablina A.A., Budanov A.V., Ilyinskaya G.V., Agapova L.S., Kravchenko J.E., Chumakov P.M. The Antioxidant Function of the P53 Tumor Suppressor. Nat. Med. 2005;11:1306–1313. doi: 10.1038/nm1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Voltan S., Martines D., Elli M., Brun P., Longo S., Porzionato A., Macchi V., D’Incà R., Scarpa M., Palù G., et al. Lactobacillus Crispatus M247-Derived H2O2 Acts as a Signal Transducing Molecule Activating Peroxisome Proliferator Activated Receptor-Gamma in the Intestinal Mucosa. Gastroenterology. 2008;135:1216–1227. doi: 10.1053/j.gastro.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 63.Pybus V., Onderdonk A.B. Microbial Interactions in the Vaginal Ecosystem, with Emphasis on the Pathogenesis of Bacterial Vaginosis. Microbes Infect. 1999;1:285–292. doi: 10.1016/S1286-4579(99)80024-0. [DOI] [PubMed] [Google Scholar]
- 64.Fredricsson B., Englund K., Weintraub L., Ölund A., Nord C.E. Ecological Treatment of Bacterial Vaginosis. Lancet. 1987;1:276. doi: 10.1016/S0140-6736(87)90096-1. [DOI] [PubMed] [Google Scholar]
- 65.Hillier S.L., Nugent R.P., Eschenbach D.A., Krohn M.A., Gibbs R.S., Martin D.H., Cotch M.F., Edelman R., Pastorek J.G., Rao A.V., et al. Association between Bacterial Vaginosis and Preterm Delivery of a Low-Birth-Weight Infant. N. Engl. J. Med. 1995;333:1737–1742. doi: 10.1056/NEJM199512283332604. [DOI] [PubMed] [Google Scholar]
- 66.Hay P.E., Lamont R.F., Taylor-Robinson D., Morgan D.J., Ison C., Pearson J. Abnormal Bacterial Colonisation of the Genital Tract and Subsequent Preterm Delivery and Late Miscarriage. BMJ. 1994;308:295. doi: 10.1136/bmj.308.6924.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Armstrong E., Kaul R. Beyond bacterial vaginosis: Vaginal lactobacilli and HIV risk. Microbiome. 2021;9:239. doi: 10.1186/s40168-021-01183-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hillier S.L. Diagnostic Microbiology of Bacterial Vaginosis. Am. J. Obstet. Gynecol. 1993;169:455–459. doi: 10.1016/0002-9378(93)90340-O. [DOI] [PubMed] [Google Scholar]
- 69.Hillier S.L., Krohn M.A., Rabe L.K., Klebanoff S.J., Eschenbach D.A. The Normal Vaginal Flora, H2O2-Producing Lactobacilli, and Bacterial Vaginosis in Pregnant Women. Clin. Infect. Dis. 1993;16:S273–S281. doi: 10.1093/clinids/16.Supplement_4.S273. [DOI] [PubMed] [Google Scholar]
- 70.Hawes S.E., Hillier S.L., Benedetti J., Stevens C.E., Koutsky L.A., Wølner-Hanssen P., Holmes K.K. Hydrogen Peroxide-Producing Lactobacilli and Acquisition of Vaginal Infections. J. Infect. Dis. 1996;174:1058–1063. doi: 10.1093/infdis/174.5.1058. [DOI] [PubMed] [Google Scholar]
- 71.Vallor A.C., Antonio M.A.D., Hawes S.E., Hillier S.L. Factors Associated with Acquisition of, or Persistent Colonization by, Vaginal Lactobacilli: Role of Hydrogen Peroxide Production. J. Infect. Dis. 2001;184:1431–1436. doi: 10.1086/324445. [DOI] [PubMed] [Google Scholar]
- 72.Antonio M.A.D., Rabe L.K., Hillier S.L. Colonization of the Rectum by Lactobacillus Species and Decreased Risk of Bacterial Vaginosis. J. Infect. Dis. 2005;192:394–398. doi: 10.1086/430926. [DOI] [PubMed] [Google Scholar]
- 73.Baeten J.M., Hassan W.M., Chohan V., Richardson B.A., Mandaliya K., Ndinya-Achola J.O., Jaoko W., McClelland R.S. Prospective Study of Correlates of Vaginal Lactobacillus Colonisation among High-Risk HIV-1 Seronegative Women. Sex. Transm. Infect. 2009;85:348–353. doi: 10.1136/sti.2008.035451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Al-Mushrif S., Jones B.M. A Study of the Prevalence of Hydrogen Peroxide Generating Lactobacilli in Bacterial Vaginosis: The Determination of H2O2 Concentrations Generated, in Vitro, by Isolated Strains and the Levels Found in Vaginal Secretions of Women with and without Infection. J. Obstet. Gynaecol. 1998;18:63–67. doi: 10.1080/01443619868325. [DOI] [PubMed] [Google Scholar]
- 75.Rosenstein U., Fontaine E.A., Morgan D.J., Sheehan M., Lament R.F., Taylor-Robinson D. Relationship between Hydrogen Peroxide-Producing Strains of Lactobacilli and Vaginosis-Associated Bacterial Species in Pregnant Women. Eur. J. Clin. Microbiol. Infect. Dis. 1997;16:517–522. doi: 10.1007/BF01708235. [DOI] [PubMed] [Google Scholar]
- 76.Fontaine E.A., Claydon E., Taylor-Robinson D., Fontainet E.A., Claydons E., Taylor-Robinsonts D. Lactobacilli from Women with or without Bacterial Vaginosis and Observations on the Significance of Hydrogen Peroxide. Microb. Ecol. Health Dis. 2009;9:135–141. doi: 10.3109/08910609609166454. [DOI] [Google Scholar]
- 77.Beigi R.H., Wiesenfeld H.C., Hillier S.L., Straw T., Krohn M.A. Factors Associated with Absence of H2O2-Producing Lactobacillus among Women with Bacterial Vaginosis. J. Infect. Dis. 2005;191:924–929. doi: 10.1086/428288. [DOI] [PubMed] [Google Scholar]
- 78.Jeanmonod R., Jeanmonod D. Vaginal Candidiasis. StatPearls; Treasure Island, FL, USA: 2022. [Google Scholar]
- 79.Sobel J.D., Chaim W. Vaginal Microbiology of Women with Acute Recurrent Vulvovaginal Candidiasis. J. Clin. Microbiol. 1996;34:2497–2499. doi: 10.1128/jcm.34.10.2497-2499.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mijač V.D., Dukić S.V., Opavski N.Z., Dukić M.K., Ranin L.T. Hydrogen Peroxide Producing Lactobacilli in Women with Vaginal Infections. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006;129:69–76. doi: 10.1016/j.ejogrb.2005.11.036. [DOI] [PubMed] [Google Scholar]
- 81.Knežević A., Stepanović S., Ćupić M., Jevtović D., Ranin J., Jovanović T. Reduced Quantity and Hydrogen-Peroxide Production of Vaginal Lactobacilli in HIV Positive Women. Biomed. Pharmacother. 2005;59:521–523. doi: 10.1016/j.biopha.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 82.Balkus J.E., Mitchell C., Agnew K., Liu C., Fiedler T., Cohn S.E., Luque A., Coombs R., Fredricks D.N., Hitti J. Detection of Hydrogen Peroxide-Producing Lactobacillus Species in the Vagina: A Comparison of Culture and Quantitative PCR among HIV-1 Seropositive Women. BMC Infect. Dis. 2012;12:188. doi: 10.1186/1471-2334-12-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Martin H.L., Richardson B.A., Nyange P.M., Lavreys L., Hillier S.L., Chohan B., Mandaliya K., Ndinya-Achola J.O., Bwayo J., Kreiss J. Vaginal Lactobacilli, Microbial Flora, and Risk of Human Immunodeficiency Virus Type 1 and Sexually Transmitted Disease Acquisition. J. Infect. Dis. 1999;180:1863–1868. doi: 10.1086/315127. [DOI] [PubMed] [Google Scholar]
- 84.Petrin D., Delgaty K., Bhatt R., Garber G. Clinical and Microbiological Aspects of Trichomonas Vaginalis. Clin. Microbiol. Rev. 1998;11:300–317. doi: 10.1128/CMR.11.2.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lovett A., Seña A.C., Macintyre A.N., Sempowski G.D., Duncan J.A., Waltmann A. Cervicovaginal Microbiota Predicts Neisseria Gonorrhoeae Clinical Presentation. Front. Microbiol. 2022;12:4171. doi: 10.3389/fmicb.2021.790531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nagy E., Petterson M., MÅRdh P.-A. Antibiosis between Bacteria Isolated from the Vagina of Women with and without Signs of Bacterial Vaginosis. Apmis. 1991;99:739–744. doi: 10.1111/j.1699-0463.1991.tb01253.x. [DOI] [PubMed] [Google Scholar]
- 87.McLean N.W., McGroarty J.A. Growth Inhibition of Metronidazole-Susceptible and Metronidazole-Resistant Strains of Gardnerella Vaginalis by Lactobacilli in Vitro. Appl. Environ. Microbiol. 1996;62:1089–1092. doi: 10.1128/aem.62.3.1089-1092.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zheng H.Y., Alcorn T.M., Cohen M.S. Effects of H2O2-Producing Lactobacilli on Neisseria Gonorrhoeae Growth and Catalase Activity. J. Infect. Dis. 1994;170:1209–1215. doi: 10.1093/infdis/170.5.1209. [DOI] [PubMed] [Google Scholar]
- 89.Conti C., Malacrino C., Mastromarino P. Inhibition of Herpes Simplex Virus Type 2 by Vaginal Lactobacilli. J. Physiol. Pharmacol. 2009;60((Suppl. S6)):19–26. [PubMed] [Google Scholar]
- 90.Klebanoff S.J., Coombs R.W. Viricidal Effect of Lactobacillus Acidophilus on Human Immunodeficiency Virus Type 1: Possible Role in Heterosexual Transmission. J. Exp. Med. 1991;174:289–292. doi: 10.1084/jem.174.1.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.O’Hanlon D.E., Lanier B.R., Moench T.R., Cone R.A. Cervicovaginal Fluid and Semen Block the Microbicidal Activity of Hydrogen Peroxide Produced by Vaginal Lactobacilli. BMC Infect. Dis. 2010;10:120. doi: 10.1186/1471-2334-10-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.O’Hanlon D.E., Moench T.R., Cone R.A. In Vaginal Fluid, Bacteria Associated with Bacterial Vaginosis Can Be Suppressed with Lactic Acid but Not Hydrogen Peroxide. BMC Infect. Dis. 2011;11:200. doi: 10.1186/1471-2334-11-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Xu H.Y., Tian W.H., Wan C.X., Jia L.J., Wang L.Y., Yuan J., Liu C.M., Zeng M., Wei H. Antagonistic Potential against Pathogenic Microorganisms and Hydrogen Peroxide Production of Indigenous Lactobacilli Isolated from Vagina of Chinese Pregnant Women. Biomed. Environ. Sci. 2008;21:365–371. doi: 10.1016/S0895-3988(08)60056-2. [DOI] [PubMed] [Google Scholar]
- 94.Bracewell-Milnes T., Saso S., Nikolaou D., Norman-Taylor J., Johnson M., Thum M.Y. Investigating the Effect of an Abnormal Cervico-Vaginal and Endometrial Microbiome on Assisted Reproductive Technologies: A Systematic Review. Am. J. Reprod. Immunol. 2018;80:e13037. doi: 10.1111/aji.13037. [DOI] [PubMed] [Google Scholar]
- 95.Singer M., Borg M., Ouburg S., Morré S.A. The Relation of the Vaginal Microbiota to Early Pregnancy Development during in Vitro Fertilization Treatment-A Meta-Analysis. J. Gynecol. Obstet. Hum. Reprod. 2019;48:223–229. doi: 10.1016/j.jogoh.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 96.Hyman R.W., Herndon C.N., Jiang H., Palm C., Fukushima M., Bernstein D., Vo K.C., Zelenko Z., Davis R.W., Giudice L.C. The Dynamics of the Vaginal Microbiome during Infertility Therapy with in Vitro Fertilization-Embryo Transfer. J. Assist. Reprod. Genet. 2012;29:105–115. doi: 10.1007/s10815-011-9694-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bernabeu A., Lledo B., Díaz M.C., Lozano F.M., Ruiz V., Fuentes A., Lopez-Pineda A., Moliner B., Castillo J.C., Ortiz J.A., et al. Effect of the Vaginal Microbiome on the Pregnancy Rate in Women Receiving Assisted Reproductive Treatment. J. Assist. Reprod. Genet. 2019;36:2111–2119. doi: 10.1007/s10815-019-01564-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Haahr T., Jensen J.S., Thomsen L., Duus L., Rygaard K., Humaidan P. Abnormal Vaginal Microbiota May Be Associated with Poor Reproductive Outcomes: A Prospective Study in IVF Patients. Hum. Reprod. 2016;31:795–803. doi: 10.1093/humrep/dew026. [DOI] [PubMed] [Google Scholar]
- 99.Hütt P., Lapp E., Štšepetova J., Smidt I., Taelma H., Borovkova N., Oopkaup H., Ahelik A., Rööp T., Hoidmets D., et al. Characterisation of Probiotic Properties in Human Vaginal Lactobacilli Strains. Microb. Ecol. Health Dis. 2016;27:30484. doi: 10.3402/mehd.v27.30484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Martius J., Krohn M.A., Hillier S.L., Stamm W.E., Holmes K.K., Eschenbach D.A. Relationships of Vaginal Lactobacillus Species, Cervical Chlamydia Trachomatis, and Bacterial Vaginosis to Preterm Birth. Obstet. Gynecol. 1988;71:89–95. [PubMed] [Google Scholar]
- 101.Wilks M., Wiggins R., Whiley A., Hennessy E., Warwick S., Porter H., Corfield A., Millar M. Identification and H2O2 Production of Vaginal Lactobacilli from Pregnant Women at High Risk of Preterm Birth and Relation with Outcome. J. Clin. Microbiol. 2004;42:713. doi: 10.1128/JCM.42.2.713-717.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.López-Moreno A., Aguilera M. Vaginal Probiotics for Reproductive Health and Related Dysbiosis: Systematic Review and Meta-Analysis. J. Clin. Med. 2021;10:1461. doi: 10.3390/jcm10071461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Petrova M.I., Lievens E., Malik S., Imholz N., Lebeer S. Lactobacillus Species as Biomarkers and Agents That Can Promote Various Aspects of Vaginal Health. Front. Physiol. 2015;6:81. doi: 10.3389/fphys.2015.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cardone A., Zarcone R., Borrelli A., Di Cunzolo A., Russo A., Tartaglia E. Utilisation of Hydrogen Peroxide in the Treatment of Recurrent Bacterial Vaginosis. Minerva Ginecol. 2003;55:483–492. [PubMed] [Google Scholar]
- 105.Chaithongwongwatthana S., Limpongsanurak S., Sitthi-Amorn C. Single Hydrogen Peroxide Vaginal Douching versus Single-Dose Oral Metronidazole for the Treatment of Bacterial Vaginosis: A Randomized Controlled Trial. J. Med. Assoc. Thail. 2003;86((Suppl. S2)):S379–S384. [PubMed] [Google Scholar]
- 106.Ocaña V.S., Pesce de Ruiz Holgado A.A., Nader-Macías M.E. Selection of Vaginal H2O2-Generating Lactobacillus Species for Probiotic Use. Curr. Microbiol. 1999;38:279–284. doi: 10.1007/PL00006802. [DOI] [PubMed] [Google Scholar]
- 107.McLEAN N.W., Rosenstein I.J. Characterisation and Selection of a Lactobacillus Species to Re-Colonise the Vagina of Women with Recurrent Bacterial Vaginosis. J. Med. Microbiol. 2000;49:543–552. doi: 10.1099/0022-1317-49-6-543. [DOI] [PubMed] [Google Scholar]
- 108.Martinez R.C.R., Franceschini S.A., Patta M.C., Quintana S.M., Candido R.C., Ferreira J.C., De Martinis E.C.P., Reid G. Improved Treatment of Vulvovaginal Candidiasis with Fluconazole plus Probiotic Lactobacillus Rhamnosus GR-1 and Lactobacillus Reuteri RC-14. Lett. Appl. Microbiol. 2009;48:269–274. doi: 10.1111/j.1472-765X.2008.02477.x. [DOI] [PubMed] [Google Scholar]
- 109.Mastromarino P., Brigidi P., Macchia S., Maggi L., Pirovano F., Trinchieri V., Conte U., Matteuzzi D. Characterization and Selection of Vaginal Lactobacillus Strains for the Preparation of Vaginal Tablets. J. Appl. Microbiol. 2002;93:884–893. doi: 10.1046/j.1365-2672.2002.01759.x. [DOI] [PubMed] [Google Scholar]
- 110.Antonio M.A.D., Meyn L.A., Murray P.J., Busse B., Hillier S.L. Vaginal Colonization by Probiotic Lactobacillus Crispatus CTV-05 Is Decreased by Sexual Activity and Endogenous Lactobacilli. J. Infect. Dis. 2009;199:1506–1513. doi: 10.1086/598686. [DOI] [PubMed] [Google Scholar]
- 111.Hallén A., Jarstrand C., Påhlson C. Treatment of Bacterial Vaginosis with Lactobacilli. Sex. Transm. Dis. 1992;19:146–148. doi: 10.1097/00007435-199205000-00007. [DOI] [PubMed] [Google Scholar]
- 112.Parent D., Bossens M., Bayot D., Kirkpatrick C., Graf F., Wilkinson F.E., Kaiser R.R. Therapy of bacterial vaginosis using exogenously-applied Lactobacilli acidophili and a low dose of estriol: A placebo-controlled multicentric clinical trial. Arzneim.-Forsch. 1996;46:68–73. [PubMed] [Google Scholar]
- 113.Bradshaw C.S., Pirotta M., de Guingand D., Hocking J.S., Morton A.N., Garland S.M., Fehler G., Morrow A., Walker S., Vodstrcil L.A., et al. Efficacy of Oral Metronidazole with Vaginal Clindamycin or Vaginal Probiotic for Bacterial Vaginosis: Randomised Placebo-Controlled Double-Blind Trial. PLoS ONE. 2012;7:e34540. doi: 10.1371/journal.pone.0034540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bohbot J.M., Daraï E., Bretelle F., Brami G., Daniel C., Cardot J.M. Efficacy and Safety of Vaginally Administered Lyophilized Lactobacillus Crispatus IP 174178 in the Prevention of Bacterial Vaginosis Recurrence. J. Gynecol. Obstet. Hum. Reprod. 2018;47:81–86. doi: 10.1016/j.jogoh.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 115.Eriksson K., Carlsson B., Forsum U., Larsson P.G. A Double-Blind Treatment Study of Bacterial Vaginosis with Normal Vaginal Lactobacilli after an Open Treatment with Vaginal Clindamycin Ovules. Acta Derm. Venereol. 2005;85:42–46. doi: 10.1080/00015550410022249. [DOI] [PubMed] [Google Scholar]
- 116.Larsson P.G., Stray-Pedersen B., Ryttig K.R., Larsen S. Human Lactobacilli as Supplementation of Clindamycin to Patients with Bacterial Vaginosis Reduce the Recurrence Rate; a 6-Month, Double-Blind, Randomized, Placebo-Controlled Study. BMC Womens Health. 2008;8:3. doi: 10.1186/1472-6874-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mastromarino P., Cacciotti F., Masci A., Mosca L. Antiviral Activity of Lactobacillus Brevis towards Herpes Simplex Virus Type 2: Role of Cell Wall Associated Components. Anaerobe. 2011;17:334–336. doi: 10.1016/j.anaerobe.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 118.Reid G., Jass J., Sebulsky M.T., McCormick J.K. Potential Uses of Probiotics in Clinical Practice. Clin. Microbiol. Rev. 2003;16:658–672. doi: 10.1128/CMR.16.4.658-672.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Anukam K., Osazuwa E., Ahonkhai I., Ngwu M., Osemene G., Bruce A.W., Reid G. Augmentation of Antimicrobial Metronidazole Therapy of Bacterial Vaginosis with Oral Probiotic Lactobacillus Rhamnosus GR-1 and Lactobacillus Reuteri RC-14: Randomized, Double-Blind, Placebo Controlled Trial. Microbes Infect. 2006;8:1450–1454. doi: 10.1016/j.micinf.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 120.Petricevic L., Witt A. The Role of Lactobacillus Casei Rhamnosus Lcr35 in Restoring the Normal Vaginal Flora after Antibiotic Treatment of Bacterial Vaginosis. BJOG. 2008;115:1369–1374. doi: 10.1111/j.1471-0528.2008.01882.x. [DOI] [PubMed] [Google Scholar]
- 121.Anukam K.C., Osazuwa E., Osemene G.I., Ehigiagbe F., Bruce A.W., Reid G. Clinical Study Comparing Probiotic Lactobacillus GR-1 and RC-14 with Metronidazole Vaginal Gel to Treat Symptomatic Bacterial Vaginosis. Microbes Infect. 2006;8:2772–2776. doi: 10.1016/j.micinf.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 122.Marcone V., Rocca G., Lichtner M., Calzolari E. Long-Term Vaginal Administration of Lactobacillus Rhamnosus as a Complementary Approach to Management of Bacterial Vaginosis. Int. J. Gynaecol. Obstet. 2010;110:223–226. doi: 10.1016/j.ijgo.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 123.Gardiner G.E., Heinemann C., Bruce A.W., Beuerman D., Reid G. Persistence of Lactobacillus Fermentum RC-14 and Lactobacillus Rhamnosus GR-1 but Not L. Rhamnosus GG in the Human Vagina as Demonstrated by Randomly Amplified Polymorphic DNA. Clin. Diagn. Lab. Immunol. 2002;9:92–96. doi: 10.1128/CDLI.9.1.92-96.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Marcotte H., Larsson P.G., Andersen K.K., Zuo F., Mikkelsen L.S., Brandsborg E., Gray G., Laher F., Otwombe K. An Exploratory Pilot Study Evaluating the Supplementation of Standard Antibiotic Therapy with Probiotic Lactobacilli in South African Women with Bacterial Vaginosis. BMC Infect. Dis. 2019;19:824. doi: 10.1186/s12879-019-4425-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bisanz J.E., Seney S., McMillan A., Vongsa R., Koenig D., Wong L.F., Dvoracek B., Gloor G.B., Sumarah M., Ford B., et al. A Systems Biology Approach Investigating the Effect of Probiotics on the Vaginal Microbiome and Host Responses in a Double Blind, Placebo-Controlled Clinical Trial of Post-Menopausal Women. PLoS ONE. 2014;9:e104511. doi: 10.1371/journal.pone.0104511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Macklaim J.M., Clemente J.C., Knight R., Gloor G.B., Reid G. Changes in Vaginal Microbiota Following Antimicrobial and Probiotic Therapy. Microb. Ecol. Health Dis. 2015;26:27799. doi: 10.3402/mehd.v26.27799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Oerlemans E.F.M., Bellen G., Claes I., Henkens T., Allonsius C.N., Wittouck S., van den Broek M.F.L., Wuyts S., Kiekens F., Donders G.G.G., et al. Impact of a Lactobacilli-Containing Gel on Vulvovaginal Candidosis and the Vaginal Microbiome. Sci. Rep. 2020;10:7976. doi: 10.1038/s41598-020-64705-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Donders G., Bellen G., Oerlemans E., Claes I., Ruban K., Henkens T., Kiekens F., Lebeer S. The Use of 3 Selected Lactobacillary Strains in Vaginal Probiotic Gel for the Treatment of Acute Candida Vaginitis: A Proof-of-Concept Study. Eur. J. Clin. Microbiol. Infect. Dis. 2020;39:1551–1558. doi: 10.1007/s10096-020-03868-x. [DOI] [PubMed] [Google Scholar]
- 129.Kovachev S.M., Vatcheva-Dobrevska R.S. Local Probiotic Therapy for Vaginal Candida Albicans Infections. Probiotics Antimicrob. Proteins. 2015;7:38–44. doi: 10.1007/s12602-014-9176-0. [DOI] [PubMed] [Google Scholar]
- 130.Zeng X., An R., Li H., Zhang Y. Improved Treatment of Vulvovaginal Candidiasis with Clotrimazole plus Probiotic Lacidophilin Vaginal Capsules: A Prospective, Real-World Study. Medicine. 2023;102:e32664. doi: 10.1097/MD.0000000000032664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nouraei S., Amir Ali Akbari S., Jorjani M., Alavi Majd H., Afrakhteh M., Ghafoorian A., Tafazzoli Harandi H. Comparison between Fluconazole with Oral Protexin Combination and Fluconazole in the Treatment of Vulvovaginal Candidiasis. ISRN Obstet. Gynecol. 2012;2012:1–10. doi: 10.5402/2012/375806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.De Seta F., Parazzini F., De Leo R., Banco R., Maso G.P., De Santo D., Sartore A., Stabile G., Inglese S., Tonon M., et al. Lactobacillus Plantarum P17630 for Preventing Candida Vaginitis Recurrence: A Retrospective Comparative Study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014;182:136–139. doi: 10.1016/j.ejogrb.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 133.Corbett G.A., Crosby D.A., McAuliffe F.M. Probiotic Therapy in Couples with Infertility: A Systematic Review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021;256:95–100. doi: 10.1016/j.ejogrb.2020.10.054. [DOI] [PubMed] [Google Scholar]
- 134.Gilboa Y., Bar-Hava I., Fisch B., Ashkenazi J., Voliovitch I., Borkowski T., Orvieto R. Does Intravaginal Probiotic Supplementation Increase the Pregnancy Rate in IVF-Embryo Transfer Cycles? Reprod. BioMed. Online. 2005;11:71–75. doi: 10.1016/S1472-6483(10)61301-6. [DOI] [PubMed] [Google Scholar]
- 135.Jepsen I.E., Saxtorph M.H., Englund A.L.M., Petersen K.B., Wissing M.L.M., Hviid T.V.F., Macklon N. Probiotic Treatment with Specific Lactobacilli Does Not Improve an Unfavorable Vaginal Microbiota Prior to Fertility Treatment-A Randomized, Double-Blinded, Placebo-Controlled Trial. Front. Endocrinol. 2022;13:1057022. doi: 10.3389/fendo.2022.1057022. [DOI] [PMC free article] [PubMed] [Google Scholar]